Effects of Electrical Stimulation on Articular Cartilage Regeneration with a Focus on Piezoelectric Biomaterials for Articular Cartilage Tissue Repair and Engineering
Abstract
1. Introduction
2. A Basic Outline of the Pathogenesis and Treatment of Articular Cartilage Injury
2.1. Pathogenesis of Articular Cartilage Injuries
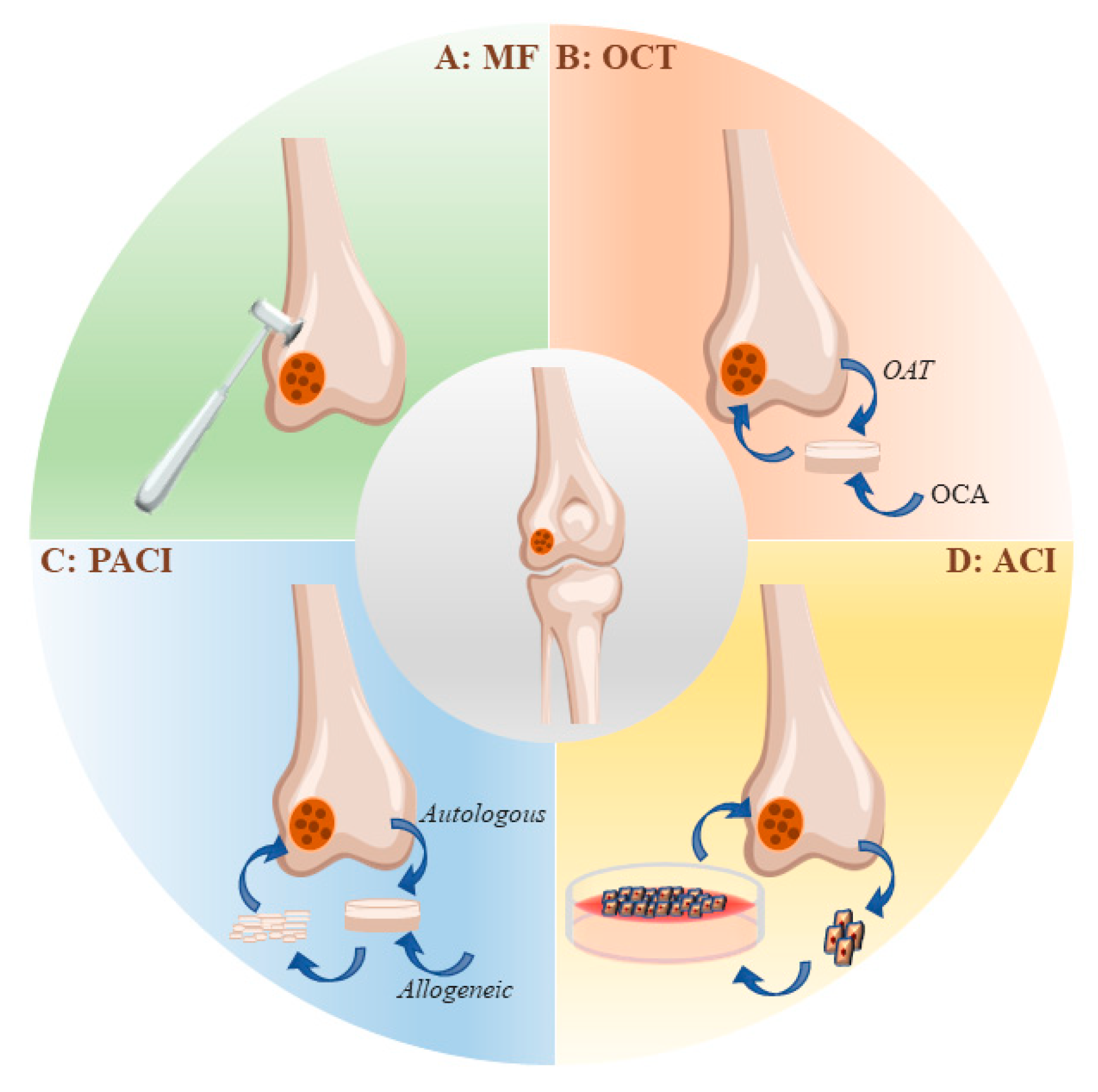
2.2. Strategies for the Clinical Treatment of Articular Cartilage Injuries
2.2.1. Microfracture
2.2.2. Autologous Chondrocyte Implantation (ACI)
- Invasive surgery is required for obtaining chondrocytes;
- A limited number of chondrocytes are available at the donor site;
- The morbidity of the donor site;
- Loss of chondrocytes due to the fact of collagen/periosteal membrane detachment;
- Chondrocytes expansion in vitro is prone to dedifferentiation, and the maintenance of the chondrocyte phenotype is difficult;
- The proliferation and differentiation potential of autologous chondrocytes in aged patients are reduced, limiting their application;
- Joint replacement surgery is often unavoidable due to the generation of mechanically inferior fibrocartilage.
2.2.3. Osteochondral Transplantation (OCT)
2.2.4. Particulate Articular Cartilage Implantation (PACI)
2.2.5. Nonoperative Conservative Treatment
Viscosupplementation with Hyaluronic Acid
Intra-Articular Platelet-Rich Plasma (PRP)
2.2.6. Physical Therapy
3. ES Promotes the In Vivo Repair of Articular Cartilage
4. ES Promotes Chondrogenic Differentiation In Vitro
5. Possible Molecular Mechanisms Involved in ES-Promoted Cartilage Injury Repair and Cell Differentiation
6. Application of ES on Cartilage Tissue Engineering
6.1. Three Main Categories of Cartilage Tissue Engineering
6.2. Conductive Scaffolds
6.2.1. Hydrogels
6.2.2. Polyaniline
6.2.3. Poly(3,4-ethylenedioxythiophene)
6.2.4. Polypyrrole
6.3. Materials with Piezoelectric Properties for Cartilage Repair and Tissue Engineering
6.3.1. Natural Piezoelectric Polymer
6.3.2. Synthetic Piezoelectric Polymer
6.3.3. Composite Piezoelectric Materials
6.3.4. Piezoelectric Scaffolds for Cartilage Tissue Engineering
7. Conclusions and Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barbour, K.E.; Helmick, C.G.; Boring, M.; Brady, T.J. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation--United States, 2010–2012. MMWR Morb. Mortal. Wkly. Rep. 2013, 62, 869–873. [Google Scholar]
- Hootman, J.M.; Helmick, C.G. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006, 54, 226–229. [Google Scholar] [CrossRef]
- Armiento, A.R.; Stoddart, M.J.; Alini, M.; Eglin, D. Biomaterials for articular cartilage tissue engineering: Learning from biology. Acta Biomater 2018, 65, 1–20. [Google Scholar] [CrossRef]
- Rojas-Murillo, J.A.; Simental-Mendía, M.A.; Moncada-Saucedo, N.K.; Delgado-Gonzalez, P.; Islas, J.F.; Roacho-Pérez, J.A.; Garza-Treviño, E.N. Physical, Mechanical, and Biological Properties of Fibrin Scaffolds for Cartilage Repair. Int. J. Mol. Sci. 2022, 23, 9879. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, Y.; Grodzinsky, A.J. Cartilage diseases. Matrix. Biol. 2018, 71, 51–69. [Google Scholar] [CrossRef]
- Chen, S.; Fu, P.; Wu, H.; Pei, M. Meniscus, articular cartilage and nucleus pulposus: A comparative review of cartilage-like tissues in anatomy, development and function. Cell. Tissue Res. 2017, 370, 53–70. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Pan, Q.; Dong, W.; Yao, Y. Progress in Osteochondral Regeneration with Engineering Strategies. Ann. Biomed. Eng. 2022, 50, 1232–1242. [Google Scholar] [CrossRef]
- Steadman, J.R.; Rodkey, W.G.; Briggs, K.K.; Rodrigo, J.J. The microfracture technic in the management of complete cartilage defects in the knee joint. Orthopade 1999, 28, 26–32. [Google Scholar]
- Na, Y.; Shi, Y.; Liu, W.; Jia, Y.; Kong, L.; Zhang, T.; Han, C.; Ren, Y. Is implantation of autologous chondrocytes superior to microfracture for articular-cartilage defects of the knee? A systematic review of 5-year follow-up data. Int. J. Surg. 2019, 68, 56–62. [Google Scholar] [CrossRef]
- Gao, Y.; Gao, J.; Li, H.; Du, D.; Jin, D.; Zheng, M.; Zhang, C. Autologous costal chondral transplantation and costa-derived chondrocyte implantation: Emerging surgical techniques. Ther. Adv. Musculoskelet Dis. 2019, 11, 1759720X19877131. [Google Scholar] [CrossRef]
- Christensen, B.B.; Olesen, M.L.; Hede, K.T.C.; Bergholt, N.L.; Foldager, C.B.; Lind, M. Particulated Cartilage for Chondral and Osteochondral Repair: A Review. Cartilage 2021, 13, 1047S–1057S. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, A.; Bathan, L. Biological approaches for cartilage repair. J. Knee Surg. 2009, 22, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Cui, J.; Wu, S.; Geng, Z.; Su, J. Silk fibroin-based biomaterials for cartilage/osteochondral repair. Theranostics 2022, 12, 5103–5124. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.A.; Little, D.; Toth, A.P.; Moorman, C.T.; Tucker, B.S.; Ciccotti, M.G.; Guilak, F. Stem cell therapies for knee cartilage repair: The current status of preclinical and clinical studies. Am. J. Sport. Med. 2014, 42, 2253–2261. [Google Scholar] [CrossRef]
- Pearson, R.G.; Bhandari, R.; Quirk, R.A.; Shakesheff, K.M. Recent Advances in Tissue Engineering. J. Long Term Eff. Med. Implant. 2017, 27, 199–231. [Google Scholar] [CrossRef]
- Chung, C.; Burdick, J.A. Engineering cartilage tissue. Adv. Drug. Deliv. Rev. 2008, 60, 243–262. [Google Scholar]
- Niu, X.; Li, N.; Du, Z.; Li, X. Integrated gradient tissue-engineered osteochondral scaffolds: Challenges, current efforts and future perspectives. Bioact. Mater. 2023, 20, 574–597. [Google Scholar] [CrossRef]
- Housmans, B.A.C.; van den Akker, G.G.H.; Neefjes, M.; Timur, U.T.; Cremers, A.; Peffers, M.J.; Caron, M.M.J.; van Rhijn, L.W.; Emans, P.J.; Boymans, T.A.E.J.; et al. Direct comparison of non-osteoarthritic and osteoarthritic synovial fluid-induced intracellular chondrocyte signaling and phenotype changes. Osteoarthr. Cartil. 2022, 31, 60–71. [Google Scholar] [CrossRef]
- Schlegel, W.; Nürnberger, S.; Hombauer, M.; Albrecht, C.; Vécsei, V.; Marlovits, S. Scaffold-dependent differentiation of human articular chondrocytes. Int. J. Mol. Med. 2008, 22, 691–699. [Google Scholar] [CrossRef]
- Massari, L.; Benazzo, F.; De Mattei, M.; Setti, S.; Fini, M. Effects of electrical physical stimuli on articular cartilage. J. Bone Jt. Surg. Am. 2007, 89 (Suppl. S3), 152–161. [Google Scholar]
- Vaca-González, J.J.; Guevara, J.M.; Moncayo, M.A.; Castro-Abril, H.; Hata, Y.; Garzón-Alvarado, D.A. Biophysical Stimuli: A Review of Electrical and Mechanical Stimulation in Hyaline Cartilage. Cartilage 2019, 10, 157–172. [Google Scholar] [CrossRef] [PubMed]
- Lippiello, L.; Chakkalakal, D.; Connolly, J.F. Pulsing direct current-induced repair of articular cartilage in rabbit osteochondral defects. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1990, 8, 266–275. [Google Scholar]
- de Campos Ciccone, C.; Zuzzi, D.C.; Neves, L.M.G.; Mendonça, J.S.; Joazeiro, P.P.; Esquisatto, M.A.M. Effects of microcurrent stimulation on hyaline cartilage repair in immature male rats (Rattus norvegicus). BMC Complement. Altern. Med. 2013, 13, 17. [Google Scholar] [CrossRef] [PubMed]
- Victoria, G.; Petrisor, B.; Drew, B.; Dick, D. Bone stimulation for fracture healing: What’s all the fuss? Indian J. Orthop. 2009, 43, 117–120. [Google Scholar] [CrossRef]
- Najjari, A.; Mehdinavaz Aghdam, R.; Ebrahimi, S.A.S.; Suresh, K.S.; Krishnan, S.; Shanthi, C.; Ramalingam, M. Smart piezoelectric biomaterials for tissue engineering and regenerative medicine: A review. Biomed. Tech. 2022, 67, 71–88. [Google Scholar] [CrossRef]
- Kamel, N.A. Bio-piezoelectricity: Fundamentals and applications in tissue engineering and regenerative medicine. Biophys. Rev. 2022, 14, 717–733. [Google Scholar] [CrossRef]
- Cafarelli, A.; Marino, A.; Vannozzi, L.; Puigmartí-Luis, J.; Pané, S.; Ciofani, G.; Ricotti, L. Piezoelectric Nanomaterials Activated by Ultrasound: The Pathway from Discovery to Future Clinical Adoption. ACS Nano 2021, 15, 11066–11086. [Google Scholar] [CrossRef]
- Liu, Y.; Dzidotor, G.; Le, T.T.; Vinikoor, T.; Morgan, K.; Curry, E.J.; Das, R.; McClinton, A.; Eisenberg, E.; Apuzzo, L.N.; et al. Exercise-induced piezoelectric stimulation for cartilage regeneration in rabbits. Sci. Transl. Med. 2022, 14, eabi7282. [Google Scholar] [CrossRef]
- Pauli, C.; Grogan, S.P.; Patil, S.; Otsuki, S.; Hasegawa, A.; Koziol, J.; Lotz, M.K.; D’Lima, D.D. Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthr. Cartil. 2011, 19, 1132–1141. [Google Scholar] [CrossRef]
- Liu, W.; Madry, H.; Cucchiarini, M. Application of Alginate Hydrogels for Next-Generation Articular Cartilage Regeneration. Int. J. Mol. Sci. 2022, 23, 1147. [Google Scholar] [CrossRef]
- Attur, M.; Krasnokutsky, S.; Statnikov, A.; Samuels, J.; Li, Z.; Friese, O.; Hellio Le Graverand-Gastineau, M.-P.; Rybak, L.; Kraus, V.B.; Jordan, J.M.; et al. Low-grade inflammation in symptomatic knee osteoarthritis: Prognostic value of inflammatory plasma lipids and peripheral blood leukocyte biomarkers. Arthritis Rheumatol. 2015, 67, 2905–2915. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Bonafè, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000, 908, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Lotz, M.; Loeser, R.F. Effects of aging on articular cartilage homeostasis. Bone 2012, 51, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.P. Redox theory of aging. Redox. Biol. 2015, 5, 71–79. [Google Scholar] [CrossRef]
- Hui, W.; Young, D.A.; Rowan, A.D.; Xu, X.; Cawston, T.E.; Proctor, C.J. Oxidative changes and signalling pathways are pivotal in initiating age-related changes in articular cartilage. Ann. Rheum. Dis. 2016, 75, 449–458. [Google Scholar] [CrossRef]
- Yin, W.; Park, J.-I.; Loeser, R.F. Oxidative stress inhibits insulin-like growth factor-I induction of chondrocyte proteoglycan synthesis through differential regulation of phosphatidylinositol 3-Kinase-Akt and MEK-ERK MAPK signaling pathways. J. Biol. Chem. 2009, 284, 31972–31981. [Google Scholar] [CrossRef]
- Loeser, R.F.; Gandhi, U.; Long, D.L.; Yin, W.; Chubinskaya, S. Aging and oxidative stress reduce the response of human articular chondrocytes to insulin-like growth factor 1 and osteogenic protein 1. Arthritis Rheumatol. 2014, 66, 2201–2209. [Google Scholar] [CrossRef]
- Loeser, R.F.; Collins, J.A.; Diekman, B.O. Ageing and the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 2016, 12, 412–420. [Google Scholar] [CrossRef]
- Berenbaum, F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr. Cartil. 2013, 21, 16–21. [Google Scholar] [CrossRef]
- Scotti, C.; Osmokrovic, A.; Wolf, F.; Miot, S.; Peretti, G.M.; Barbero, A.; Martin, I. Response of human engineered cartilage based on articular or nasal chondrocytes to interleukin-1β and low oxygen. Tissue Eng. Part A 2012, 18, 362–372. [Google Scholar] [CrossRef]
- Leong, D.J.; Gu, X.I.; Li, Y.; Lee, J.Y.; Laudier, D.M.; Majeska, R.J.; Schaffler, M.B.; Cardoso, L.; Sun, H.B. Matrix metalloproteinase-3 in articular cartilage is upregulated by joint immobilization and suppressed by passive joint motion. Matrix Biol. 2010, 29, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Jaime, P.; García-Guerrero, N.; Estella, R.; Pardo, J.; García-Álvarez, F.; Martinez-Lostao, L. CD56/CD16 Natural Killer cells expressing the inflammatory protease granzyme A are enriched in synovial fluid from patients with osteoarthritis. Osteoarthr. Cartil. 2017, 25, 1708–1718. [Google Scholar] [CrossRef]
- Nigrovic, P.A.; Lee, D.M. Mast cells in inflammatory arthritis. Arthritis Res. Ther. 2005, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Dai, H. Articular cartilage and osteochondral tissue engineering techniques: Recent advances and challenges. Bioact. Mater. 2021, 6, 4830–4855. [Google Scholar] [CrossRef] [PubMed]
- Madry, H.; Grün, U.W.; Knutsen, G. Cartilage repair and joint preservation: Medical and surgical treatment options. Dtsch. Arztebl. Int. 2011, 108, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.; Jakob, R.P. Review of K.H. Pridie (1959) on “A method of resurfacing osteoarthritic knee joints”. J. ISAKOS 2022, 7, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Case, J.M.; Scopp, J.M. Treatment of Articular Cartilage Defects of the Knee With Microfracture and Enhanced Microfracture Techniques. Sport. Med. Arthrosc. Rev. 2016, 24, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Kalson, N.S.; Gikas, P.D.; Briggs, T.W.R. Current strategies for knee cartilage repair. Int. J. Clin. Pract. 2010, 64, 1444–1452. [Google Scholar] [CrossRef]
- Moran, C.J.; Pascual-Garrido, C.; Chubinskaya, S.; Potter, H.G.; Warren, R.F.; Cole, B.J.; Rodeo, S.A. Restoration of articular cartilage. J. Bone. Jt. Surg. Am. 2014, 96, 336–344. [Google Scholar] [CrossRef]
- Kurenkova, A.D.; Romanova, I.A.; Kibirskiy, P.D.; Timashev, P.; Medvedeva, E.V. Strategies to Convert Cells into Hyaline Cartilage: Magic Spells for Adult Stem Cells. Int. J. Mol. Sci. 2022, 23, 11169. [Google Scholar] [CrossRef]
- Grande, D.A.; Pitman, M.I.; Peterson, L.; Menche, D.; Klein, M. The repair of experimentally produced defects in rabbit articular cartilage by autologous chondrocyte transplantation. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1989, 7, 208–218. [Google Scholar] [CrossRef] [PubMed]
- Welch, T.; Mandelbaum, B.; Tom, M. Autologous Chondrocyte Implantation: Past, Present, and Future. Sport. Med. Arthrosc. Rev. 2016, 24, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Brittberg, M.; Peterson, L.; Sjögren-Jansson, E.; Tallheden, T.; Lindahl, A. Articular cartilage engineering with autologous chondrocyte transplantation. A review of recent developments. J. Bone Jt. Surg. Am. 2003, 85 (Suppl. S3), 109–115. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Guo, W.; Tian, G.; Luo, X.; Peng, L.; Liu, S.; Sui, X.; Guo, Q.; Li, X. Clinical Application Status of Articular Cartilage Regeneration Techniques: Tissue-Engineered Cartilage Brings New Hope. Stem Cells Int. 2020, 2020, 5690252. [Google Scholar] [CrossRef]
- Redondo, M.L.; Beer, A.J.; Yanke, A.B. Cartilage Restoration: Microfracture and Osteochondral Autograft Transplantation. J. Knee Surg. 2018, 31, 231–238. [Google Scholar] [CrossRef]
- Hangody, L.; Ráthonyi, G.K.; Duska, Z.; Vásárhelyi, G.; Füles, P.; Módis, L. Autologous osteochondral mosaicplasty. Surgical technique. J. Bone Jt. Surg. Am. 2004, 86 (Suppl. S1), 65–72. [Google Scholar] [CrossRef]
- Liu, Y.; Shah, K.M.; Luo, J. Strategies for Articular Cartilage Repair and Regeneration. Front. Bioeng. Biotech. 2021, 9, 770655. [Google Scholar] [CrossRef]
- Lu, Y.; Dhanaraj, S.; Wang, Z.; Bradley, D.M.; Bowman, S.M.; Cole, B.J.; Binette, F. Minced cartilage without cell culture serves as an effective intraoperative cell source for cartilage repair. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2006, 24, 1261–1270. [Google Scholar] [CrossRef]
- Farr, J.; Tabet, S.K.; Margerrison, E.; Cole, B.J. Clinical, Radiographic, and Histological Outcomes After Cartilage Repair With Particulated Juvenile Articular Cartilage: A 2-Year Prospective Study. Am. J. Sport. Med. 2014, 42, 1417–1425. [Google Scholar] [CrossRef]
- Wilson, M.G.; Michet, C.J.; Ilstrup, D.M.; Melton, L.J. Idiopathic symptomatic osteoarthritis of the hip and knee: A population-based incidence study. Mayo Clin. Proc. 1990, 65, 1214–1221. [Google Scholar] [CrossRef]
- Shokri, A.; Ramezani, K.; Jamalpour, M.R.; Mohammadi, C.; Vahdatinia, F.; Irani, A.D.; Sharifi, E.; Haddadi, R.; Jamshidi, S.; Amirabad, L.M.; et al. In vivo efficacy of 3D-printed elastin-gelatin-hyaluronic acid scaffolds for regeneration of nasal septal cartilage defects. J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110, 614–624. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef]
- Kraeutler, M.J.; Garabekyan, T.; Mei-Dan, O. The use of platelet-rich plasma to augment conservative and surgical treatment of hip and pelvic disorders. Muscles Ligaments Tendons J. 2016, 6, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.; Johnson, V.M.; Murray, M.M. Effects of age and platelet-rich plasma on ACL cell viability and collagen gene expression. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2012, 30, 79–85. [Google Scholar] [CrossRef]
- Cavallo, C.; Roffi, A.; Grigolo, B.; Mariani, E.; Pratelli, L.; Merli, G.; Kon, E.; Marcacci, M.; Filardo, G. Platelet-Rich Plasma: The Choice of Activation Method Affects the Release of Bioactive Molecules. Biomed. Res. Int. 2016, 2016, 6591717. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Rohlfing, B.; Schneider, U.; Goost, H.; Silny, J. Mechanically induced electrical potentials of articular cartilage. J. Biomech. 2002, 35, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Farooqi, A.R.; Bader, R.; van Rienen, U. Numerical Study on Electromechanics in Cartilage Tissue with Respect to Its Electrical Properties. Tissue Eng. Part B Rev. 2019, 25, 152–166. [Google Scholar] [CrossRef]
- Xu, J.; Wang, W.; Clark, C.C.; Brighton, C.T. Signal transduction in electrically stimulated articular chondrocytes involves translocation of extracellular calcium through voltage-gated channels. Osteoarthr. Cartil. 2009, 17, 397–405. [Google Scholar] [CrossRef]
- Snyder, M.J.; Wilensky, J.A.; Fortin, J.D. Current applications of electrotherapeutics in collagen healing. Pain. Physician 2002, 5, 172–181. [Google Scholar]
- Jahr, H.; Matta, C.; Mobasheri, A. Physicochemical and biomechanical stimuli in cell-based articular cartilage repair. Curr. Rheumatol. Rep. 2015, 17, 22. [Google Scholar] [CrossRef] [PubMed]
- Krueger, S.; Riess, A.; Jonitz-Heincke, A.; Weizel, A.; Seyfarth, A.; Seitz, H.; Bader, R. Establishment of a New Device for Electrical Stimulation of Non-Degenerative Cartilage Cells In Vitro. Int. J. Mol. Sci. 2021, 22, 394. [Google Scholar] [CrossRef] [PubMed]
- Matta, C.; Mobasheri, A. Regulation of chondrogenesis by protein kinase C: Emerging new roles in calcium signalling. Cell Signal 2014, 26, 979–1000. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.J.; Lee, G.S.; Chun, H. Electrical stimulation drives chondrogenesis of mesenchymal stem cells in the absence of exogenous growth factors. Sci. Rep. 2016, 6, 39302. [Google Scholar] [CrossRef] [PubMed]
- Baker, B.; Spadaro, J.; Marino, A.; Becker, R.O. Electrical stimulation of articular cartilage regeneration. Ann. N. Y. Acad. Sci. 1974, 238, 491–499. [Google Scholar] [CrossRef]
- Hronik-Tupaj, M.; Kaplan, D.L. A review of the responses of two- and three-dimensional engineered tissues to electric fields. Tissue Eng. Part B Rev. 2012, 18, 167–180. [Google Scholar] [CrossRef]
- Brighton, C.T.; Pfeffer, G.B.; Pollack, S.R. In vivo growth plate stimulation in various capacitively coupled electrical fields. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1983, 1, 42–49. [Google Scholar] [CrossRef]
- Ciombor, D.M.; Aaron, R.K.; Wang, S.; Simon, B. Modification of osteoarthritis by pulsed electromagnetic field--a morphological study. Osteoarthr. Cartil. 2003, 11, 455–462. [Google Scholar] [CrossRef]
- Fini, M.; Giavaresi, G.; Torricelli, P.; Cavani, F.; Setti, S.; Canè, V.; Giardino, R. Pulsed electromagnetic fields reduce knee osteoarthritic lesion progression in the aged Dunkin Hartley guinea pig. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2005, 23, 899–908. [Google Scholar] [CrossRef]
- Chen, C.-H.; Lin, Y.-S.; Fu, Y.-C.; Wang, C.-K.; Wu, S.-C.; Wang, G.-J.; Eswaramoorthy, R.; Wang, Y.-H.; Wang, C.-Z.; Wang, Y.-H.; et al. Electromagnetic fields enhance chondrogenesis of human adipose-derived stem cells in a chondrogenic microenvironment in vitro. J. Appl. Physiol. 2013, 114, 647–655. [Google Scholar] [CrossRef]
- Nisbet, H.O.; Akar, A.; Nisbet, C.; Gulbahar, M.Y.; Ozak, A.; Yardimci, C.; Comlekci, S. Effects of electromagnetic field (1.8/0.9 GHz) exposure on growth plate in growing rats. Res. Vet. Sci. 2016, 104, 24–29. [Google Scholar] [CrossRef] [PubMed]
- De Mattei, M.; Fini, M.; Setti, S.; Ongaro, A.; Gemmati, D.; Stabellini, G.; Pellati, A.; Caruso, A. Proteoglycan synthesis in bovine articular cartilage explants exposed to different low-frequency low-energy pulsed electromagnetic fields. Osteoarthr. Cartil. 2007, 15, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Hiemer, B.; Krogull, M.; Bender, T.; Ziebart, J.; Krueger, S.; Bader, R.; Jonitz-Heincke, A. Effect of electric stimulation on human chondrocytes and mesenchymal stem cells under normoxia and hypoxia. Mol. Med. Rep. 2018, 18, 2133–2141. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Meng, X.; Pei, Z.; Wang, G.; Liu, R.; Qi, M.; Zhou, J.; Wang, F. Physiological Electric Field: A Potential Construction Regulator of Human Brain Organoids. Int. J. Mol. Sci. 2022, 23, 3877. [Google Scholar] [CrossRef]
- Nogami, H.; Aoki, H.; Okagawa, T.; Mimatsu, K. Effects of electric current on chondrogenesis in vitro. Clin. Orthop. Relat. Res. 1982, 163, 243–247. [Google Scholar] [CrossRef]
- Ross, C.L.; Siriwardane, M.; Almeida-Porada, G.; Porada, C.D.; Brink, P.; Christ, G.J.; Harrison, B.S. The effect of low-frequency electromagnetic field on human bone marrow stem/progenitor cell differentiation. Stem Cell Res. 2015, 15, 96–108. [Google Scholar] [CrossRef]
- Mayer-Wagner, S.; Passberger, A.; Sievers, B.; Aigner, J.; Summer, B.; Schiergens, T.S.; Jansson, V.; Müller, P.E. Effects of low frequency electromagnetic fields on the chondrogenic differentiation of human mesenchymal stem cells. Bioelectromagnetics 2011, 32, 283–290. [Google Scholar] [CrossRef]
- Parate, D.; Franco-Obregón, A.; Fröhlich, J.; Beyer, C.; Abbas, A.A.; Kamarul, T.; Hui, J.H.P.; Yang, Z. Enhancement of mesenchymal stem cell chondrogenesis with short-term low intensity pulsed electromagnetic fields. Sci. Rep. 2017, 7, 9421. [Google Scholar] [CrossRef]
- Iwasa, K.; Reddi, A.H. Pulsed Electromagnetic Fields and Tissue Engineering of the Joints. Tissue Eng. Part B Rev. 2018, 24, 144–154. [Google Scholar] [CrossRef]
- Chang, C.-H.; Loo, S.-T.; Liu, H.-L.; Fang, H.-W.; Lin, H.-Y. Can low frequency electromagnetic field help cartilage tissue engineering? J. Biomed. Mater. Res. Part A 2010, 92, 843–851. [Google Scholar] [CrossRef]
- Mardani, M.; Roshankhah, S.; Hashemibeni, B.; Salahshoor, M.; Naghsh, E.; Esfandiari, E. Induction of chondrogenic differentiation of human adipose-derived stem cells by low frequency electric field. Adv. Biomed. Res. 2016, 5, 97. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Balooch, G.; Chiou, M.; Bekerman, E.; Ritchie, R.O.; Longaker, M.T. Analysis of the material properties of early chondrogenic differentiated adipose-derived stromal cells (ASC) using an in vitro three-dimensional micromass culture system. Biochem. Biophys. Res. Commun. 2007, 359, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Fan, L.; Lin, J.; Heng, B.C.; Deng, Z.; Zheng, Q.; Zhang, J.; Jiang, Y.; Ge, Z. Nanosecond pulsed electric fields prime mesenchymal stem cells to peptide ghrelin and enhance chondrogenesis and osteochondral defect repair in vivo. Sci. China Life Sci. 2022, 65, 927–939. [Google Scholar] [CrossRef] [PubMed]
- Bai, B.; Hou, M.; Hao, J.; Liu, Y.; Ji, G.; Zhou, G. Research progress in seed cells for cartilage tissue engineering. Regen. Med. 2022, 17, 659–675. [Google Scholar] [CrossRef]
- Ciobanu, F.; Golzio, M.; Kovacs, E.; Teissié, J. Control by Low Levels of Calcium of Mammalian Cell Membrane Electropermeabilization. J. Membr. Biol. 2018, 251, 221–228. [Google Scholar] [CrossRef]
- McCullen, S.D.; McQuilling, J.P.; Grossfeld, R.M.; Lubischer, J.L.; Clarke, L.I.; Loboa, E.G. Application of low-frequency alternating current electric fields via interdigitated electrodes: Effects on cellular viability, cytoplasmic calcium, and osteogenic differentiation of human adipose-derived stem cells. Tissue Eng. Part C Methods 2010, 16, 1377–1386. [Google Scholar] [CrossRef]
- Pall, M.L. Electromagnetic fields act via activation of voltage-gated calcium channels to produce beneficial or adverse effects. J. Cell. Mol. Med. 2013, 17, 958–965. [Google Scholar] [CrossRef]
- Matta, C.; Zákány, R.; Mobasheri, A. Voltage-dependent calcium channels in chondrocytes: Roles in health and disease. Curr. Rheumatol. Rep. 2015, 17, 43. [Google Scholar] [CrossRef]
- Zhang, Y.; Pizzute, T.; Pei, M. A review of crosstalk between MAPK and Wnt signals and its impact on cartilage regeneration. Cell Tissue Res. 2014, 358, 633–649. [Google Scholar] [CrossRef]
- Ning, T.; Guo, J.; Zhang, K.; Li, K.; Zhang, J.; Yang, Z.; Ge, Z. Nanosecond pulsed electric fields enhanced chondrogenic potential of mesenchymal stem cells via JNK/CREB-STAT3 signaling pathway. Stem Cell Res. Ther. 2019, 10, 45. [Google Scholar] [CrossRef]
- Hwang, S.-G.; Yu, S.-S.; Poo, H.; Chun, J.-S. c-Jun/activator protein-1 mediates interleukin-1beta-induced dedifferentiation but not cyclooxygenase-2 expression in articular chondrocytes. J. Biol. Chem. 2005, 280, 29780–29787. [Google Scholar] [CrossRef] [PubMed]
- Novak, A.; Dedhar, S. Signaling through beta-catenin and Lef/Tcf. Cell. Mol. Life Sci. 1999, 56, 523–537. [Google Scholar] [CrossRef]
- Fodor, J.; Matta, C.; Juhász, T.; Oláh, T.; Gönczi, M.; Szíjgyártó, Z.; Gergely, P.; Csernoch, L.; Zákány, R. Ionotropic purinergic receptor P2X4 is involved in the regulation of chondrogenesis in chicken micromass cell cultures. Cell Calcium 2009, 45, 421–430. [Google Scholar] [CrossRef]
- Gabler, J.; Ruetze, M.; Kynast, K.L.; Grossner, T.; Diederichs, S.; Richter, W. Stage-Specific miRs in Chondrocyte Maturation: Differentiation-Dependent and Hypertrophy-Related miR Clusters and the miR-181 Family. Tissue Eng. Part A 2015, 21, 2840–2851. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.-E.; Koh, P.-S.; Seo, B.-K.; Park, Y.-C.; Baek, Y.-H.; Lee, J.-D.; Park, D.-S. Mangiferin reduces the inhibition of chondrogenic differentiation by IL-1β in mesenchymal stem cells from subchondral bone and targets multiple aspects of the Smad and Sox9 SOX9 pathways. Int. J. Mol. Sci. 2014, 15, 16025–16042. [Google Scholar] [CrossRef] [PubMed]
- Tam, W.L.; Freitas Mendes, L.; Chen, X.; Lesage, R.; Van Hoven, I.; Leysen, E.; Kerckhofs, G.; Bosmans, K.; Chai, Y.C.; Yamashita, A.; et al. Human pluripotent stem cell-derived cartilaginous organoids promote scaffold-free healing of critical size long bone defects. Stem Cell Res. Ther. 2021, 12, 513. [Google Scholar] [CrossRef]
- Scotti, C.; Piccinini, E.; Takizawa, H.; Todorov, A.; Bourgine, P.; Papadimitropoulos, A.; Barbero, A.; Manz, M.G.; Martin, I. Engineering of a functional bone organ through endochondral ossification. Proc. Natl. Acad. Sci. USA 2013, 110, 3997–4002. [Google Scholar] [CrossRef] [PubMed]
- Decker, R.S. Articular cartilage and joint development from embryogenesis to adulthood. Semin. Cell. Dev. Biol. 2017, 62, 50–56. [Google Scholar] [CrossRef]
- Hall, G.N.; Tam, W.L.; Andrikopoulos, K.S.; Casas-Fraile, L.; Voyiatzis, G.A.; Geris, L.; Luyten, F.P.; Papantoniou, I. Patterned, organoid-based cartilaginous implants exhibit zone specific functionality forming osteochondral-like tissues in vivo. Biomaterials 2021, 273, 120820. [Google Scholar] [CrossRef]
- Rowland, C.R.; Glass, K.A.; Ettyreddy, A.R.; Gloss, C.C.; Matthews, J.R.L.; Huynh, N.P.T.; Guilak, F. Regulation of decellularized tissue remodeling via scaffold-mediated lentiviral delivery in anatomically-shaped osteochondral constructs. Biomaterials 2018, 177, 161–175. [Google Scholar] [CrossRef]
- Hong, H.; Seo, Y.B.; Kim, D.Y.; Lee, J.S.; Lee, Y.J.; Lee, H.; Ajiteru, O.; Sultan, M.T.; Lee, O.J.; Kim, S.H.; et al. Digital light processing 3D printed silk fibroin hydrogel for cartilage tissue engineering. Biomaterials 2020, 232, 119679. [Google Scholar] [CrossRef]
- Turnbull, G.; Clarke, J.; Picard, F.; Riches, P.; Jia, L.; Han, F.; Li, B.; Shu, W. 3D bioactive composite scaffolds for bone tissue engineering. Bioact. Mater. 2018, 3, 278–314. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, A.J.; Converse, G.L.; Hopkins, R.A.; Detamore, M.S. The bioactivity of cartilage extracellular matrix in articular cartilage regeneration. Adv. Healthc. Mater. 2015, 4, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Ma, Y.; Min, Y.; Sun, J.; Shi, X.; Gao, G.; Sun, L.; Wang, J. Progress and prospect of technical and regulatory challenges on tissue-engineered cartilage as therapeutic combination product. Bioact. Mater. 2023, 20, 501–518. [Google Scholar] [CrossRef] [PubMed]
- Lammi, M.J.; Piltti, J.; Prittinen, J.; Qu, C. Challenges in Fabrication of Tissue-Engineered Cartilage with Correct Cellular Colonization and Extracellular Matrix Assembly. Int. J. Mol. Sci. 2018, 19, 2700. [Google Scholar] [CrossRef] [PubMed]
- Ode, A.; Duda, G.N.; Geissler, S.; Pauly, S.; Ode, J.-E.; Perka, C.; Strube, P. Interaction of age and mechanical stability on bone defect healing: An early transcriptional analysis of fracture hematoma in rat. PLoS ONE 2014, 9, e106462. [Google Scholar] [CrossRef] [PubMed]
- Saberi, A.; Jabbari, F.; Zarrintaj, P.; Saeb, M.R.; Mozafari, M. Electrically Conductive Materials: Opportunities and Challenges in Tissue Engineering. Biomolecules 2019, 9, 448. [Google Scholar] [CrossRef] [PubMed]
- Breukers, R.D.; Gilmore, K.J.; Kita, M.; Wagner, K.K.; Higgins, M.J.; Moulton, S.E.; Clark, G.M.; Officer, D.L.; Kapsa, R.M.I.; Wallace, G.G. Creating conductive structures for cell growth: Growth and alignment of myogenic cell types on polythiophenes. J. Biomed. Mater. Res. Part A 2010, 95, 256–268. [Google Scholar] [CrossRef] [PubMed]
- Balint, R.; Cassidy, N.J.; Cartmell, S.H. Conductive polymers: Towards a smart biomaterial for tissue engineering. Acta Biomater. 2014, 10, 2341–2353. [Google Scholar] [CrossRef]
- Marsudi, M.A.; Ariski, R.T.; Wibowo, A.; Cooper, G.; Barlian, A.; Rachmantyo, R.; Bartolo, P.J.D.S. Conductive Polymeric-Based Electroactive Scaffolds for Tissue Engineering Applications: Current Progress and Challenges from Biomaterials and Manufacturing Perspectives. Int. J. Mol. Sci. 2021, 22, 11543. [Google Scholar] [CrossRef]
- Drury, J.L.; Mooney, D.J. Hydrogels for tissue engineering: Scaffold design variables and applications. Biomaterials 2003, 24, 4337–4351. [Google Scholar] [CrossRef] [PubMed]
- Yuk, H.; Lu, B.; Zhao, X. Hydrogel bioelectronics. Chem. Soc. Rev. 2019, 48, 1642–1667. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Fan, L.; Yi, X.; Zhou, Z.; Liu, C.; Fu, R.; Dai, C.; Wang, Z.; Chen, X.; Yu, P.; et al. Soft Conducting Polymer Hydrogels Cross-Linked and Doped by Tannic Acid for Spinal Cord Injury Repair. ACS Nano 2018, 12, 10957–10967. [Google Scholar] [CrossRef] [PubMed]
- Hosoyama, K.; Ahumada, M.; Goel, K.; Ruel, M.; Suuronen, E.J.; Alarcon, E.I. Electroconductive materials as biomimetic platforms for tissue regeneration. Biotechnol. Adv. 2019, 37, 444–458. [Google Scholar] [CrossRef]
- Li, D.; Huang, J.; Kaner, R.B. Polyaniline nanofibers: A unique polymer nanostructure for versatile applications. Acc. Chem. Res. 2009, 42, 135–145. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, T.; Zhang, Q.; Feng, Z.; Zhu, C.; Yu, Y.; Li, K.; Zhao, M.; Yang, J.; Liu, J.; et al. Three-Dimensional BC/PEDOT Composite Nanofibers with High Performance for Electrode-Cell Interface. ACS Appl. Mater. Interfaces 2015, 7, 28244–28253. [Google Scholar] [CrossRef]
- Niu, X.; Rouabhia, M.; Chiffot, N.; King, M.W.; Zhang, Z. An electrically conductive 3D scaffold based on a nonwoven web of poly(L-lactic acid) and conductive poly(3,4-ethylenedioxythiophene). J. Biomed. Mater. Res. Part A 2015, 103, 2635–2644. [Google Scholar] [CrossRef]
- Abidian, M.R.; Corey, J.M.; Kipke, D.R.; Martin, D.C. Conducting-polymer nanotubes improve electrical properties, mechanical adhesion, neural attachment, and neurite outgrowth of neural electrodes. Small Weinh. Bergstr. Ger. 2010, 6, 421–429. [Google Scholar] [CrossRef]
- Ateh, D.D.; Navsaria, H.A.; Vadgama, P. Polypyrrole-based conducting polymers and interactions with biological tissues. J. R. Soc. Interface 2006, 3, 741–752. [Google Scholar] [CrossRef]
- Bendrea, A.-D.; Cianga, L.; Cianga, I. Review paper: Progress in the field of conducting polymers for tissue engineering applications. J. Biomater. Appl. 2011, 26, 3–84. [Google Scholar] [CrossRef]
- Collier, J.H.; Camp, J.P.; Hudson, T.W.; Schmidt, C.E. Synthesis and characterization of polypyrrole-hyaluronic acid composite biomaterials for tissue engineering applications. J. Biomed. Mater. Res. 2000, 50, 574–584. [Google Scholar] [CrossRef]
- Guo, B.; Ma, P.X. Conducting Polymers for Tissue Engineering. Biomacromolecules 2018, 19, 1764–1782. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Yang, Y.; Chen, Y.; Zhou, Q. Ultrasound-Induced Wireless Energy Harvesting: From Materials Strategies to Functional Applications. Nano Energy 2020, 77, 105131. [Google Scholar] [CrossRef] [PubMed]
- Han, J.K.; Jeon, D.H.; Cho, S.Y.; Kang, S.W.; Yang, S.A.; Bu, S.D.; Myung, S.; Lim, J.; Choi, M.; Lee, M.; et al. Nanogenerators consisting of direct-grown piezoelectrics on multi-walled carbon nanotubes using flexoelectric effects. Sci. Rep. 2016, 6, 29562. [Google Scholar] [CrossRef] [PubMed]
- Rajabi, A.H.; Jaffe, M.; Arinzeh, T.L. Piezoelectric materials for tissue regeneration: A review. Acta Biomater. 2015, 24, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Ansari, S.; Khorshidi, S.; Karkhaneh, A. Engineering of gradient osteochondral tissue: From nature to lab. Acta Biomater. 2019, 87, 41–54. [Google Scholar] [CrossRef]
- Zheng, T.; Huang, Y.; Zhang, X.; Cai, Q.; Deng, X.; Yang, X. Mimicking the electrophysiological microenvironment of bone tissue using electroactive materials to promote its regeneration. J. Mater. Chem. B 2020, 8, 10221–10256. [Google Scholar] [CrossRef]
- Kwon, J.; Cho, H. Piezoelectric Heterogeneity in Collagen Type I Fibrils Quantitatively Characterized by Piezoresponse Force Microscopy. ACS Biomater. Sci. Eng. 2020, 6, 6680–6689. [Google Scholar] [CrossRef]
- Nguyen, T.D.; Mao, S.; Yeh, Y.-W.; Purohit, P.K.; McAlpine, M.C. Nanoscale flexoelectricity. Adv. Mater. 2013, 25, 946–974. [Google Scholar] [CrossRef]
- Tandon, B.; Blaker, J.J.; Cartmell, S.H. Piezoelectric materials as stimulatory biomedical materials and scaffolds for bone repair. Acta Biomater. 2018, 73, 1–20. [Google Scholar] [CrossRef]
- Pärssinen, J.; Hammarén, H.; Rahikainen, R.; Sencadas, V.; Ribeiro, C.; Vanhatupa, S.; Miettinen, S.; Lanceros-Méndez, S.; Hytönen, V.P. Enhancement of adhesion and promotion of osteogenic differentiation of human adipose stem cells by poled electroactive poly(vinylidene fluoride). J. Biomed. Mater. Res. Part A 2015, 103, 919–928. [Google Scholar] [CrossRef] [PubMed]
- Yao, T.; Chen, J.; Wang, Z.; Zhai, J.; Li, Y.; Xing, J.; Hu, S.; Tan, G.; Qi, S.; Chang, Y.; et al. The antibacterial effect of potassium-sodium niobate ceramics based on controlling piezoelectric properties. Colloids Surf. B Biointerfaces 2019, 175, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Z.-L.; Sun, Y.; Wang, D.; Chen, K.-Q.; Tang, L.-M. A review of ultra-thin ferroelectric films. J. Phys. Condens. Matter. 2021, 33. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.; Pärssinen, J.; Sencadas, V.; Correia, V.; Miettinen, S.; Hytönen, V.P.; Lanceros-Méndez, S. Dynamic piezoelectric stimulation enhances osteogenic differentiation of human adipose stem cells. J. Biomed. Mater. Res. Part A 2015, 103, 2172–2175. [Google Scholar] [CrossRef]
- Weber, N.; Lee, Y.S.; Shanmugasundaram, S.; Jaffe, M.; Arinzeh, T.L. Characterization and in vitro cytocompatibility of piezoelectric electrospun scaffolds. Acta Biomater. 2010, 6, 3550–3556. [Google Scholar] [CrossRef]
- Santos, D.; Correia, C.O.; Silva, D.M.; Gomes, P.S.; Fernandes, M.H.; Santos, J.D.; Sencadas, V. Incorporation of glass-reinforced hydroxyapatite microparticles into poly(lactic acid) electrospun fibre mats for biomedical applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 75, 1184–1190. [Google Scholar] [CrossRef] [PubMed]
- Fukada, E. History and recent progress in piezoelectric polymers. IEEE Trans. Ultrason Ferroelectr. Freq. Control 2000, 47, 1277–1290. [Google Scholar] [CrossRef] [PubMed]
- Köse, G.T.; Korkusuz, F.; Ozkul, A.; Soysal, Y.; Ozdemir, T.; Yildiz, C.; Hasirci, V. Tissue engineered cartilage on collagen and PHBV matrices. Biomaterials 2005, 26, 5187–5197. [Google Scholar] [CrossRef]
- Ghosh, S.; Mei, B.Z.; Lubkin, V.; Scheinbeim, J.I.; Newman, B.A.; Kramer, P.; Bennett, G.; Feit, N. Piezoelectric response of scleral collagen. J. Biomed. Mater. Res. 1998, 39, 453–457. [Google Scholar] [CrossRef]
- Fukada, E. Piezoelectricity of biopolymers. Biorheology 1995, 32, 593–609. [Google Scholar] [CrossRef]
- Hsu, H.H.; Zhong, W. Nanocellulose-Based Conductive Membranes for Free-Standing Supercapacitors: A Review. Membranes 2019, 9, 74. [Google Scholar] [CrossRef] [PubMed]
- Zaborowska, M.; Bodin, A.; Bäckdahl, H.; Popp, J.; Goldstein, A.; Gatenholm, P. Microporous bacterial cellulose as a potential scaffold for bone regeneration. Acta Biomater. 2010, 6, 2540–2547. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Sun, M.; Hu, X.; Ren, B.; Cheng, J.; Li, C.; Duan, X.; Fu, X.; Zhang, J.; Chen, H.; et al. Structurally and Functionally Optimized Silk-Fibroin-Gelatin Scaffold Using 3D Printing to Repair Cartilage Injury In Vitro and In Vivo. Adv. Mater. 2017, 29, 1701089. [Google Scholar] [CrossRef] [PubMed]
- Rajala, S.; Siponkoski, T.; Sarlin, E.; Mettänen, M.; Vuoriluoto, M.; Pammo, A.; Juuti, J.; Rojas, O.J.; Franssila, S.; Tuukkanen, S. Cellulose Nanofibril Film as a Piezoelectric Sensor Material. ACS Appl. Mater. Interfaces 2016, 8, 15607–15614. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.R.; Varma, A.J. Functional nanoparticles obtained from cellulose: Engineering the shape and size of 6-carboxycellulose. Chem. Commun. 2013, 49, 8818–8820. [Google Scholar] [CrossRef]
- Hickey, R.J.; Pelling, A.E. Cellulose Biomaterials for Tissue Engineering. Front. Bioeng. Biotech. 2019, 7, 45. [Google Scholar] [CrossRef]
- Klemm, D.; Heublein, B.; Fink, H.-P.; Bohn, A. Cellulose: Fascinating biopolymer and sustainable raw material. Angew. Chem. Int. Ed. Engl. 2005, 44, 3358–3393. [Google Scholar] [CrossRef]
- Donnaloja, F.; Jacchetti, E.; Soncini, M.; Raimondi, M.T. Natural and Synthetic Polymers for Bone Scaffolds Optimization. Polymers 2020, 12, 905. [Google Scholar] [CrossRef]
- Saravanan, S.; Leena, R.S.; Selvamurugan, N. Chitosan based biocomposite scaffolds for bone tissue engineering. Int. J. Biol. Macromol. 2016, 93, 1354–1365. [Google Scholar] [CrossRef]
- Fang, J.; Liao, J.; Zhong, C.; Lu, X.; Ren, F. High-Strength, Biomimetic Functional Chitosan-Based Hydrogels for Full-Thickness Osteochondral Defect Repair. ACS Biomater. Sci. Eng. 2022, 8, 4449–4461. [Google Scholar] [CrossRef]
- Raghav, P.K.; Mann, Z.; Ahlawat, S.; Mohanty, S. Mesenchymal stem cell-based nanoparticles and scaffolds in regenerative medicine. Eur. J. Pharm. 2022, 918, 174657. [Google Scholar] [CrossRef] [PubMed]
- Jiao, F.; Wei, P.; Li, Y. Wave propagation through a flexoelectric piezoelectric slab sandwiched by two piezoelectric half-spaces. Ultrasonics 2018, 82, 217–232. [Google Scholar] [CrossRef] [PubMed]
- Singhvi, M.S.; Zinjarde, S.S.; Gokhale, D.V. Polylactic acid: Synthesis and biomedical applications. J. Appl. Microbiol. 2019, 127, 1612–1626. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.; Sencadas, V.; Costa, C.M.; Gómez Ribelles, J.L.; Lanceros-Méndez, S. Tailoring the morphology and crystallinity of poly(L-lactide acid) electrospun membranes. Sci. Technol. Adv. Mater. 2011, 12, 015001. [Google Scholar] [CrossRef]
- Hoop, M.; Chen, X.-Z.; Ferrari, A.; Mushtaq, F.; Ghazaryan, G.; Tervoort, T.; Poulikakos, D.; Nelson, B.; Pané, S. Ultrasound-mediated piezoelectric differentiation of neuron-like PC12 cells on PVDF membranes. Sci. Rep. 2017, 7, 4028. [Google Scholar] [CrossRef]
- Li, W.-J.; Jiang, Y.J.; Tuan, R.S. Chondrocyte phenotype in engineered fibrous matrix is regulated by fiber size. Tissue Eng. 2006, 12, 1775–1785. [Google Scholar] [CrossRef]
- Jacob, J.; More, N.; Kalia, K.; Kapusetti, G. Piezoelectric smart biomaterials for bone and cartilage tissue engineering. Inflamm. Regen. 2018, 38, 2. [Google Scholar] [CrossRef]
- Xie, M.; Wang, L.; Guo, B.; Wang, Z.; Chen, Y.E.; Ma, P.X. Ductile electroactive biodegradable hyperbranched polylactide copolymers enhancing myoblast differentiation. Biomaterials 2015, 71, 158–167. [Google Scholar] [CrossRef]
- Pereira, J.D.A.S.; Camargo, R.C.T.; Filho, J.C.S.C.; Alves, N.; Rodriguez-Perez, M.A.; Constantino, C.J.L. Biomaterials from blends of fluoropolymers and corn starch-implant and structural aspects. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 36, 226–236. [Google Scholar] [CrossRef]
- Cheng, Y.; Xu, Y.; Qian, Y.; Chen, X.; Ouyang, Y.; Yuan, W.-E. 3D structured self-powered PVDF/PCL scaffolds for peripheral nerve regeneration. Nano Energy 2020, 69, 104411. [Google Scholar] [CrossRef]
- Vannozzi, L.; Gouveia, P.; Pingue, P.; Canale, C.; Ricotti, L. Novel Ultrathin Films Based on a Blend of PEG-PCL and PLLA and Doped with ZnO Nanoparticles. ACS Appl. Mater. Interfaces 2020, 12, 21398–21410. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Su, M.; Li, K.; Jiang, L.; Song, Y.; Doi, M.; Wang, J. Preparation of patterned ultrathin polymer films. Langmuir 2014, 30, 9436–9441. [Google Scholar] [CrossRef] [PubMed]
- Borodina, T.N.; Grigoriev, D.O.; Andreeva, D.V.; Möhwald, H.; Shchukin, D.G. Polyelectrolyte multilayered nanofilms as a novel approach for the protection of hydrogen storage materials. ACS Appl. Mater. Interfaces 2009, 1, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Ho, Q.-P.; Wang, S.-L.; Wang, M.-J. Creation of biofunctionalized micropatterns on poly(methyl methacrylate) by single-step phase separation method. ACS Appl. Mater. Interfaces 2011, 3, 4496–4503. [Google Scholar] [CrossRef]
- Banks, T.A.; Luckman, P.S.B.; Frith, J.E.; Cooper-White, J.J. Effects of electric fields on human mesenchymal stem cell behaviour and morphology using a novel multichannel device. Integr. Biol. 2015, 7, 693–712. [Google Scholar] [CrossRef]
- Huang, X.; Das, R.; Patel, A.; Nguyen, T.D. Physical Stimulations for Bone and Cartilage Regeneration. Regen. Eng. Transl. Med. 2018, 4, 216–237. [Google Scholar] [CrossRef]
- Damaraju, S.M.; Shen, Y.; Elele, E.; Khusid, B.; Eshghinejad, A.; Li, J.; Jaffe, M.; Arinzeh, T.L. Three-dimensional piezoelectric fibrous scaffolds selectively promote mesenchymal stem cell differentiation. Biomaterials 2017, 149, 51–62. [Google Scholar] [CrossRef]
- Samadi, A.; Salati, M.A.; Safari, A.; Jouyandeh, M.; Barani, M.; Singh Chauhan, N.P.; Golab, E.G.; Zarrintaj, P.; Kar, S.; Seidi, F.; et al. Comparative review of piezoelectric biomaterials approach for bone tissue engineering. J. Biomater. Sci. Polym. Ed. 2022, 33, 1555–1594. [Google Scholar] [CrossRef]
- Kong, L.; Gao, X.; Qian, Y.; Sun, W.; You, Z.; Fan, C. Biomechanical microenvironment in peripheral nerve regeneration: From pathophysiological understanding to tissue engineering development. Theranostics 2022, 12, 4993–5014. [Google Scholar] [CrossRef]
- Zaszczynska, A.; Sajkiewicz, P.; Gradys, A. Piezoelectric Scaffolds as Smart Materials for Neural Tissue Engineering. Polymer 2020, 12, 161. [Google Scholar] [CrossRef]
- Khan, H.M.; Liao, X.; Sheikh, B.A.; Wang, Y.; Su, Z.; Guo, C.; Li, Z.; Zhou, C.; Cen, Y.; Kong, Q. Smart biomaterials and their potential applications in tissue engineering. J. Mater. Chem. B 2022, 10, 6859–6895. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wan, X.; Wang, Z.L.; Li, L. Electroactive Biomaterials and Systems for Cell Fate Determination and Tissue Regeneration: Design and Applications. Adv. Mater. 2021, 33, e2007429. [Google Scholar] [CrossRef] [PubMed]
- Grayson, W.L.; Chao, P.-H.G.; Marolt, D.; Kaplan, D.L.; Vunjak-Novakovic, G. Engineering custom-designed osteochondral tissue grafts. Trends Biotechnol. 2008, 26, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Fallahiarezoudar, E.; Ahmadipourroudposht, M.; Idris, A.; Mohd Yusof, N. A review of: Application of synthetic scaffold in tissue engineering heart valves. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 48, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Tandon, B.; Kamble, P.; Olsson, R.T.; Blaker, J.J.; Cartmell, S.H. Fabrication and Characterisation of Stimuli Responsive Piezoelectric PVDF and Hydroxyapatite-Filled PVDF Fibrous Membranes. Molecules 2019, 24, 1903. [Google Scholar] [CrossRef]
- Jacob, J.; More, N.; Mounika, C.; Gondaliya, P.; Kalia, K.; Kapusetti, G. Smart Piezoelectric Nanohybrid of Poly(3-hydroxybutyrate--3-hydroxyvalerate) and Barium Titanate for Stimulated Cartilage Regeneration. Acs. Appl. Bio Mater. 2019, 2, 4922–4931. [Google Scholar] [CrossRef]
- Sadeghi, D.; Karbasi, S.; Razavi, S.; Mohammadi, S.; Shokrgozar, M.A.; Bonakdar, S. Electrospun poly(hydroxybutyrate)/chitosan blend fibrous scaffolds for cartilage tissue engineering. J. Appl. Polym. Sci. 2016, 133. [Google Scholar] [CrossRef]
- Barbosa, F.; Ferreira, F.C.; Silva, J.C. Piezoelectric Electrospun Fibrous Scaffolds for Bone, Articular Cartilage and Osteochondral Tissue Engineering. Int. J. Mol. Sci. 2022, 23, 2907. [Google Scholar] [CrossRef]
- Lay, R.; Deijs, G.S.; Malmström, J. The intrinsic piezoelectric properties of materials—A review with a focus on biological materials. RSC Adv. 2021, 11, 30657–30673. [Google Scholar] [CrossRef]

| Type of Stimulation | Animal Model | ES Parameters | Electrode/Distance of the EFs/EMFs | Results | Reference |
|---|---|---|---|---|---|
| EFs | Femoral condyles of New Zealand white rabbits. | 70 mV; 1–9 weeks | Bimetallic silver platinum electrochemical device; 3 mm silver electrodes. | Increase in cellular response, proliferation, and matrix production. | [75] |
| Epiphyseal plate from rabbit femur. | 1.5 V; 20 μA; 6 weeks | Two 8 cm long, twisted stainless-steel wire electrodes. | Experimental animals showed longer and broader femur on the operating side after surgery. | [76] | |
| Proximal tibia of the rabbit. | 5 V; 60 kHz | Fitted with 1.8 × 1.8 cm stainless-steel capacitor plates over the right proximal tibial growth plate. | Small amount of electric current stimulates the epiphyseal plate to accelerate bone growth; distribution of current results in regular growth of epiphyseal. | [77] | |
| EMFs | Knee of Hartley guinea pigs. | 1.5 Hz; 1 h/day for 6 months | The applied magnetic field consisted of a pulse-burst of a 4.5 ms duration repeated at 15 burst and with a peak magnetic field of 16 G. | EMF retarded the development of osteoarthritic lesions; an increased amount of cartilage ECM, chondrocyte hypertrophy, and calcification. | [78] |
| Joint knee from Hartley guinea pigs. | 75 Hz; 1.5 mT; 6 h a day for 3 months | Magnetic field of 20 G, pulsed period of 67.1 ms. | Cartilage thickness (CT) was significantly higher (p < 0.001) in the medial tibia plateaus; significant reduction of chondroplasty progression. | [79,80] | |
| Distal femoral growth plates of male Wistar rats. | 110 Hz; 2 mT; 2 h/day for 90 days | A 0.2 mm copper wire, 0.5 cm internal diameter of the coil probe. | Rats treated with ES experienced more rapid weight gain; chondrocytes rapidly proliferated, matured, and transformed into hypertrophic cells in the growth plate calcium; growth hormone levels were higher. | [81,82] |
| Stem Cell Type | ES Modality | Parameters | Differentiation Medium | Results | Reference(s) |
|---|---|---|---|---|---|
| ADSCs | EFs | 1 KHz, 20 mV/cm, 20 min/day, 7 days | Chondrogenic differentiation media DMEM-high glucose; penicillin and streptomycin: 1%; dexamethasone: 10−7 M; ascorbat-2-phosphate: 50 μg/mL; bovine serum albumin: 0.5 mg/mL; linoleic acid: 5 μg/mL; insulin: 10 mg/mL; transferrin: 5.5 mg/L; selenium (insulin-transferrin-selenium): 5 μg/L. | Increase in the expression of COL2α1 and Sox9 genes; decrease in the expression of type I and type X collagen genes. | [91,92] |
| BMSCs | EMFs | 15 Hz, 5 mT, 45 min every 8 h | Chondrogenic differentiation media DMEM-high glucose; insulin: 10 mg/mL; transferrin: 5.5 mg/L; selenium: 5 mg/L; bovine serum albumin: 0.5 mg/mL; linoleic acid: 4.7 mg/mL; dexamethasone: 0.1 mM; L-ascorbic acid-2-phosphate: 0.2 mM; L-proline: 0.35 mM; penicillin/streptomycin: 30 U/mL; FGF-2: 5 ng/mL. | Increased in COL2α1 expression, decrease in collagen type X expression. | [87] |
| BMSCs | PEMFs | 15 Hz, 2 mT, 10 min, daily | Chondrogenic differentiation media DMEM-high glucose; proline: 4 mM; ascorbic acid: 50 µg/mL; sodium pyruvate: 1 mM; dexamethasone: 10−7 M; transforming growth factor-β3 (TGFβ3): 10 ng/mL. | Moderate enhancement in the gene expression of Sox9, aggrecan, and COL2α1 and the deposition of GAGs. | [88] |
| Category | Material | Piezoelectric Coefficient | Material Biological Advantages | Restoration Result | Reference(s) |
|---|---|---|---|---|---|
| Synthetic piezoelectric materials | PVDF | d31 = 20 pC/N | Highly elastic; nontoxic; biocompatible. | Promotes cell adhesion and proliferation of chondrogenic cells. | [143,144] |
| P(VDF-TrFE) | d33 = 30 pC/N | Cytocompatible. | Piezoelectric fibers can stimulate the differentiable cells into a mature phenotype and promote tissue repair. | [145,146] | |
| PHBV | d33 = 1.3 pC/N | Biocompatible; more extended biodegradation rate. | Formed hyaline such as cartilage and neocartilage was integrated into the adjacent cartilage. | [147,148] | |
| PLLA | d14 = −10 pC/N | Biodegradable; biocompatible; strong mechanical properties; nontoxic; water soluble. | Rapid bone and cartilage regeneration by consuming the piezoelectric property. | [149,150] | |
| Natural piezoelectric materials | Cellulose | d14 = 0.2 pC/N | Excellent biocompatibility. | Offers biological signaling, cell adhesion, and remodeling. | [151,152] |
| Chitin | d14 = 0.2–1.5 pC/N | Natural polysaccharide; hydrophilic material; biocompatible. | Carriers for controlled drug delivery; promote cell adhesion, proliferation, and differentiation, providing support for cartilage regeneration; favor integration to the subchondral region. | [153] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Z.; Zheng, J.; Meng, X.; Wang, F. Effects of Electrical Stimulation on Articular Cartilage Regeneration with a Focus on Piezoelectric Biomaterials for Articular Cartilage Tissue Repair and Engineering. Int. J. Mol. Sci. 2023, 24, 1836. https://doi.org/10.3390/ijms24031836
Zhou Z, Zheng J, Meng X, Wang F. Effects of Electrical Stimulation on Articular Cartilage Regeneration with a Focus on Piezoelectric Biomaterials for Articular Cartilage Tissue Repair and Engineering. International Journal of Molecular Sciences. 2023; 24(3):1836. https://doi.org/10.3390/ijms24031836
Chicago/Turabian StyleZhou, Zhengjie, Jingtong Zheng, Xiaoting Meng, and Fang Wang. 2023. "Effects of Electrical Stimulation on Articular Cartilage Regeneration with a Focus on Piezoelectric Biomaterials for Articular Cartilage Tissue Repair and Engineering" International Journal of Molecular Sciences 24, no. 3: 1836. https://doi.org/10.3390/ijms24031836
APA StyleZhou, Z., Zheng, J., Meng, X., & Wang, F. (2023). Effects of Electrical Stimulation on Articular Cartilage Regeneration with a Focus on Piezoelectric Biomaterials for Articular Cartilage Tissue Repair and Engineering. International Journal of Molecular Sciences, 24(3), 1836. https://doi.org/10.3390/ijms24031836







