Measurement of Cardiac-Specific Biomarkers in the Emergency Department: New Insight in Risk Evaluation
Abstract
:1. Introduction
2. Article Aim and Structure
3. Cardiac Biomarkers in the Setting of ED
3.1. Clinical Interpretations of Circulating hs-cTnI and hs-cTnT Levels
3.2. Clinical Relevance of the Biological Variation in Cardiac Biomarkers
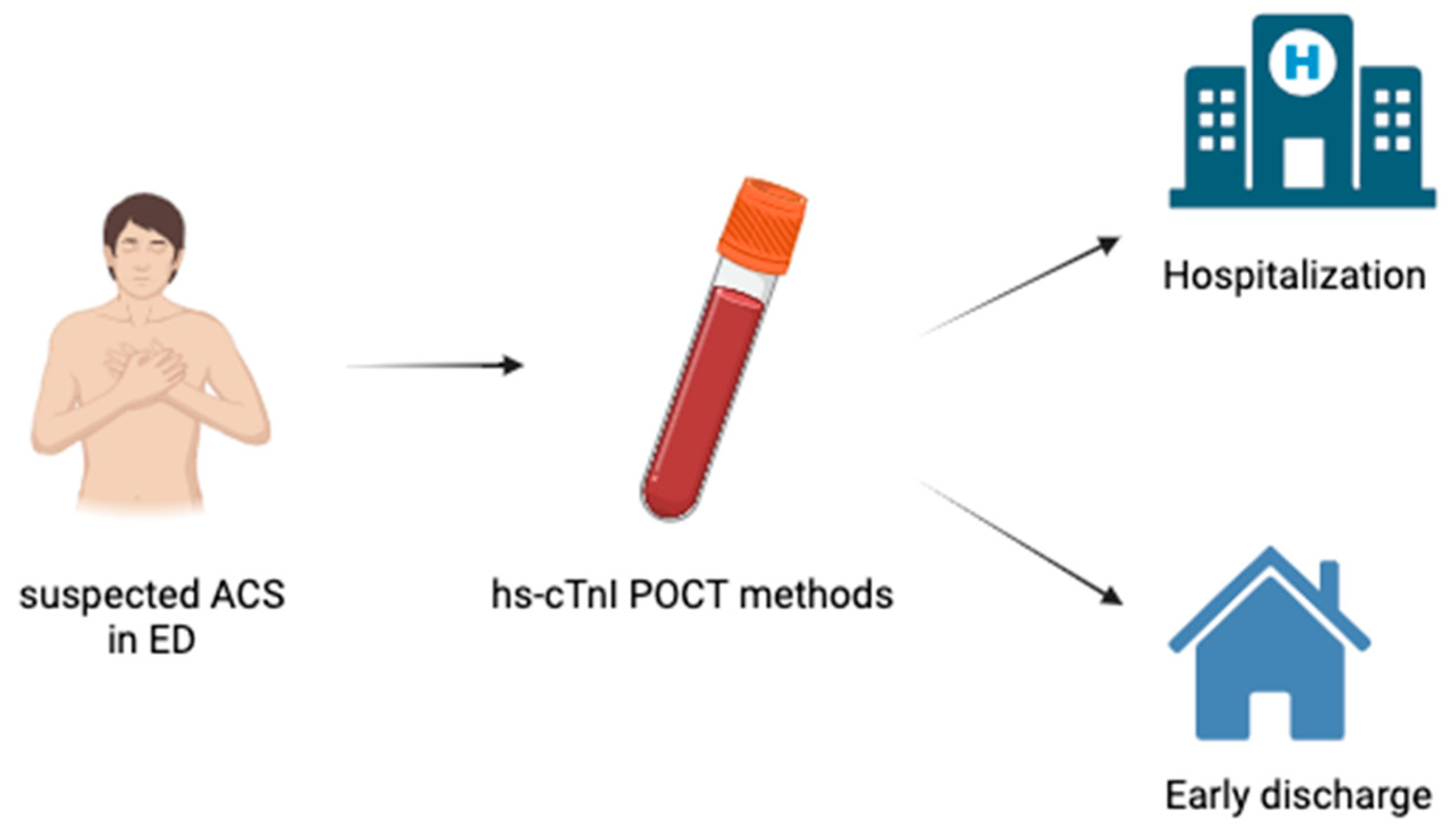
3.3. Role and Advantages of POCT Methods for Cardiac Troponin in Clinical Practice
3.4. Clinical Role of Cardiac-Specific Biomarkers in Patients with AHF Admitted to the ED
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Newman-Toker, D.E.; Peterson, S.M.; Badihian, S.; Hassoon, A.; Nassery, N.; Parizadeh, D.; Wilson, L.M.; Jia, Y.; Omron, R.; Tharmarajah, S.; et al. Diagnostic Errors in the Emergency Department: A Systematic Review; AHRQ Comparative Effectiveness Reviews NO. 258; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2022; 22(23)-EHC043. [Google Scholar]
- Corrales-Medina, V.F.; Musher, D.M.; Shachkina, S.; Chirinos, J.A. Acute pneumonia and cardiovascular system. Lancet 2013, 381, 496–505. [Google Scholar] [CrossRef]
- Desai, A.; Aliberti, S.; Amati, F.; Stainer, A.; Voza, A. Cardiovascular complications in community-acquired pneumonia. Microorganims 2022, 10, 2177. [Google Scholar] [CrossRef]
- Restrepo, M.I.; Reyes, L.F. Pneumonia as a cardiovascular disease. Respirology 2018, 23, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Heit, J.A.; Spencer, F.A.; White, R.H. The epidemiology of thromboembolism. J. Thromb. Thrombolysis 2016, 41, 3–14. [Google Scholar] [CrossRef]
- Sandoval, Y.; Januzzi, J.L., Jr.; Jaffe, A.S. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J. Am. Coll. Cardiol. 2020, 76, 1244–1258. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.Y.; Ma, T.Y.; Zhang, J.Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; The Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef]
- AAEM; RSA; AAEM; ABEM; ACEP; ACOEP; AACEM; CORD; EMRA; SAEM; et al. Multi-Organizational Letter Regarding AHRQ Report on Diagnostic Errors in the Emergency Department; American College of Emergency Physicians: Irving, TX, USA, 2022. [Google Scholar]
- Hendley, N.W.; Moskop, J.; Ashburn, N.P.; Mahler, S.A.; Stopyra, J.P. The ethical dilemma of emergency department patients with low-risk chest pain. Emerg. Med. J. 2021, 38, 85–94. [Google Scholar] [CrossRef]
- Hsia, R.Y.; Hale, Z.; Tabas, J.A. A national study of the prevalence of life-threatening diagnoses in patients with chest pain. JAMA Intern. Med. 2016, 176, 1029–1032. [Google Scholar] [CrossRef]
- Mahler, S.A.; Riley, R.F.; Hiestand, B.C.; Russell, G.B.; Hoekstra, J.W.; Lefebvre, C.W.; Nicks, B.A.; Cline, D.M.; Askew, K.L.; Elliott, S.B.; et al. The heart pathway randomized trial: Identifying emergency department patients with acute chest pain for early discharge. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 195–203. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke Statistics-2019 update: A report from the American Heart Association. Circulation 2019, 139, e56–e66. [Google Scholar] [CrossRef] [PubMed]
- NICE. High-Sensitivity Troponin Tests for the Early Rule out of NSTEMI. Diagnostics Guidance. 2020. Available online: https://www.nice.org.uk/guidance/dg40/resources/highsensitivity-troponin-tests-for-the-early-rule-out-of-nstemi-pdf-1053804469957 (accessed on 18 September 2023).
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1387. [Google Scholar] [PubMed]
- Apple, F.S.; O’Collinson, P.; AKavsak, P.; Body, R.; Ordóñez-Llanos, J.; Saenger, A.K.; Omland, T.; Hammarsten, O.; Jaffe, A.S.; IFCC Committee on Clinical Applications of Cardiac Bio-Markers. Getting cardiac troponin right: Appraisal of the 2020 European Society of Cardiology guidelines for the management of Acute Coronary Syndromes in patients presenting without persistent ST-segment elevation by the International Federation of Clinical Chemistry and Laboratory Medicine Committee on Clinical Applications of Cardiac Bio-Markers. Clin. Chem. 2021, 67, 730–735. [Google Scholar] [PubMed]
- Writing Committee Members; Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/ SCMR guideline for the evaluation and diagnosis of chest pain: A report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2021, 144, e368–e454. [Google Scholar]
- Chen, D.; Zhou, Y.; Yang, Y.; Yao, C.; Gu, G.; Wang, K.; Guo, W.; Shi, D.; Song, Z.; Tong, C. Evaluation of the 0 h/1 h high-sensitivity cardiac troponin T algorithm in diagnosis of non-ST-segment elevation myocardial infarction (NSTEMI) in Han population. Clin Chem Lab Med. 2020, 59, 757–764. [Google Scholar]
- Sandoval, Y.; Apple, F.S.; Mahler, S.A.; Body, R.; Collinson, P.O.; Jaffe, A.S. High-sensitivity cardiac troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guidelines for the evaluation and diagnosis of acute chest pain. Circulation 2022, 146, 569–581. [Google Scholar] [CrossRef]
- Writing Committee; Kontos, M.C.; de Lemos, J.A.; Deitelzweig, S.B.; Diercks, D.B.; Gore, M.O.; Hess, E.P.; McCarthy, C.P.; McCord, J.K.; Musey, P.I., Jr.; et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2022, 80, 1925–1960. [Google Scholar] [CrossRef]
- Kaur, G.; Oliveira-Gomes, D.; Rivera, F.B.; Gulati, M. Chest pain in women: Considerations from the 2021 AHA/ACC Chest Pain Guideline. Curr. Probl. Cardiol. 2023, 48, 101697. [Google Scholar] [CrossRef]
- Altunoz, Y.; Karakus Yilmaz, B.; Topcu, H.; Cetinkal, G.; İkizceli, İ.; Yigit, Y. Improving risk stratification of patients with chest pain in the Emergency Department. Cureus 2023, 15, e33202. [Google Scholar] [CrossRef]
- Maroules, C.D.; Rybicki, F.J.; Ghoshhajra, B.B.; Batlle, J.C.; Branch, K.; Chinnaiyan, K.; Hamilton-Craig, C.; Hoffmann, U.; Litt, H.; Meyersohn, N.; et al. 2022 use of coronary computed tomographic angiography for patients presenting with acute chest pain to the emergency department: An expert consensus document of the Society of cardiovascular computed tomography (SCCT): Endorsed by the American College of Radiology (ACR) and North American Society for cardiovascular Imaging (NASCI). J. Cardiovasc. Comput. Tomogr. 2023, 17, 146–163. [Google Scholar]
- Wu, A.H.; Christenson, R.H.; Greene, D.N.; Jaffe, A.S.; Kavsak, P.A.; Ordonez-Llanos, J.; Apple, F.S. Clinical laboratory practice recommendations for the use of cardiac troponin in acute coronary syndrome: Expert opinion from the Academy of the American Association for Clinical Chemistry and the Task Force on Clinical Applications of Cardiac Bio-Markers of the International Federation of Clinical Chemistry and Laboratory Medicine. Clin. Chem. 2018, 64, 645–655. [Google Scholar] [PubMed]
- Clerico, A.; Zaninotto, M.; Plebani, M. High-sensitivity assay for cardiac troponins with POCT methods. The future is soon. Clim. Chem. Lab. Med. 2021, 59, 1477–1478. [Google Scholar] [CrossRef] [PubMed]
- Clerico, A.; Aimo, A.; Zaninotto, M.; Plebani, M. Transdermal measurement of cardiac troponins: The future is now. Clin. Chem. Lab. Med. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Sörensen, N.A.; Neumann, J.T.; Ojeda, F.; Giannitsis, E.; Spanuth, E.; Blankenberg, S.; Westermann, D.; Zeller, T. Diagnostic evaluation of a high-sensitivity troponin I point-of-care assay. Clin. Chem. 2019, 65, 1592–1601. [Google Scholar] [CrossRef]
- Boeddinghaus, J.; Nestelberger, T.; Koechlin, L.; Wussler, D.; Lopez-Ayala, P.; Walter, J.E.; Troester, V.; Ratmann, P.D.; Seidel, F.; Zimmermann, T.; et al. Early diagnosis of myocardial infarction with point-of-care high-sensitivity cardiac troponin I. J. Am. Coll. Cardiol. 2020, 75, 1111–1124. [Google Scholar] [CrossRef]
- Apple, F.S.; Schulz, K.; Schmidt, C.W.; van Domburg, T.S.Y.; Fonville, J.M.; de Theije, F.K. Determination of sex-specific 99th percentile upper reference limits for a point of care high sensitivity cardiac troponin I assay. Clin. Chem. Lab. Med. 2021, 59, 1574–1578. [Google Scholar] [CrossRef]
- Apple, F.S.; Smith, S.W.; Greenslade, J.H.; Sandoval, Y.; Parsonage, W.; Ranasinghe, I.; Gaikwad, N.; Schulz, K.; Stephensen, L.; Schmidt, C.W.; et al. Single high-sensitivity Point-of-Care whole-blood cardiac troponin I measurement to rule out acute myocardial infarction at low risk. Circulation 2022, 146, 1918–1929. [Google Scholar] [CrossRef]
- Bruinen, A.L.; Frenk, L.D.; de Theije, F.; Kemper, D.W.; Janssen, M.J.; Rahel, B.M.; Meeder, J.G.; Hof, A.W.v. Point-of-care high-sensitivity troponin-I analysis in capillary blood for acute coronary syndrome diagnostics. Clin. Chem. Lab. Med. 2022, 60, 1669–1674. [Google Scholar] [CrossRef]
- Koper, L.H.; Frenk, L.D.S.; Meeder, J.G.; van Osch, F.H.M.; Bruinen, A.L.; Janssen, M.J.W.; van’t Hof, A.W.J.; Rahel, B.M. URGENT 1.5: Diagnostic accuracy of the modified HEART score, with fingerstick point-of-care troponin testing, in ruling out acute coronary syndrome. Neth. Heart J. 2022, 30, 360–369. [Google Scholar] [CrossRef]
- Gunsolus, I.L.; Schulz, K.; Sandoval, Y.; Smith, S.W.; Lindgren, B.; Okeson, B.; Apple, F.S. Diagnostic performance of a rapid, novel, whole blood, point of care high-sensitivity cardiac troponin I assay for myocardial infarction. Clin. Biochem. 2022, 105–106, 70–74. [Google Scholar] [CrossRef]
- Norman, T.; Young, J.; Jones, J.S.; Egan, G.; Pickering, J.; Du Toit, S.; Hamilton, F.; Miller, R.; Frampton, C.; Devlin, G.; et al. Implementation and evaluation of a rural general practice assessment pathway for possible cardiac chest pain using point-of-care troponin testing: A pilot study. BMJ Open 2022, 12, e044801. [Google Scholar] [CrossRef] [PubMed]
- Schols, A.M.R.; Stakenborg, J.P.G.; Dinant, G.J.; Willemsen, R.T.A.; Cals, J.W.L. Point-of-care testing in primary care patients with acute cardiopulmonary symptoms: A systematic review. Fam. Pract. 2018, 35, 4–12. [Google Scholar] [PubMed]
- Collinson, P.O.; Saenger, A.K.; Apple, F.S.; IFCC C-CB. High sensitivity, contemporary and point-of-care cardiac troponin assays: Educational aids developed by the IFCC Committee on Clinical Application of Cardiac Bio-Markers. Clin. Chem. Lab. Med. 2019, 57, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Apple, F.S.; Fantz, C.R.; Collinson, P.O.; on behalf of the IFCC Committee on Clinical Application of Cardiac Bio-Markers. Implementation of high-sensitivity and point-of-care cardiac troponin assays into practice: Some different thoughts. Clin. Chem. 2021, 67, 70–78. [Google Scholar] [CrossRef]
- Giannoni, A.; Giovannini, S.; Clerico, A. Measurement of circulating concentrations of cardiac troponin I and T in healthy subjects: A tool for monitoring myocardial tissue renewal? Clin. Chem. Lab. Med. 2009, 47, 1167–1177. [Google Scholar] [CrossRef]
- Greene, D.N.; Tate, J.R. Establishing consensus-based, assay-specific 99th percentile upper reference limits to facilitate proper utilization of cardiac troponin measurements. Clin Chem Lab Med. 2017, 55, 1675–1682. [Google Scholar]
- Clerico, A.; Ripoli, A.; Zaninotto, M.; Masotti, S.; Musetti, V.; Ciaccio, M.; Aloe, R.; Rizzardi, S.; Dittadi, R.; Carrozza, C.; et al. Head-to-head comparison of plasma cTnI concentration values measured with three high-sensitivity methods in a large Italian population of healthy volunteers and patients admitted to emergency department with acute coronary syndrome: A multi-center study. Clin. Chim. Acta 2019, 496, 25–34. [Google Scholar]
- Franzini, M.; Lorenzoni, V.; Masotti, S.; Prontera, C.; Chiappino, D.; Della Latta, D.; Daves, M.; Deluggi, I.; Zuin, M.; Ferrigno, L.; et al. The calculation of the cardiac troponin T 99th percentile of the reference population is affected by age, gender, and population selection: A multicenter study in Italy. Clin. Chim. Acta 2015, 438, 376–381. [Google Scholar]
- Giannitsis, E.; Mueller-Hennessen, M.; Zeller, T.; Schuebler, A.; Aurich, M.; Biener, M.; Vafaie, M.; Stoyanov, K.M.; Ochs, M.; Riffel, J.; et al. Gender-specific reference values for high-sensitivity cardiac troponin T and I in well-phenotyped healthy individuals and validity of high-sensitivity assay designation. Clin. Biochem. 2020, 78, 18–24. [Google Scholar]
- Zhang, X.; Han, X.; Zhao, M.; Mu, R.; Wang, S.; Yun, K.; Shang, H. Determination of high-sensitivity cardiac troponin T upper reference limits under the improved selection criteria in a Chinese population. J. Clin. Lab. Anal. 2020, 34, e23007. [Google Scholar] [CrossRef]
- Vittorini, S.; Clerico, A. Cardiovascular biomarkers: Increasing impact of laboratory medicine in cardiology practice. Clin. Chem. Lab. Med. 2008, 46, 748–763. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, O.; Zdunek, S.; Felker, A.; Salehpour, M.; Alkass, K.; Bernard, S.; Sjostrom, S.L.; Szewczykowska, M.; Jackowska, T.; dos Remedios, C.; et al. Dynamics of cell generation and turnover in the human heart. Cell 2015, 161, 1566–1575. [Google Scholar] [CrossRef] [PubMed]
- Marjot, J.; Kaier, T.E.; Martin, E.D.; Reji, S.S.; Copeland, O.; Iqbal, M.; Goodson, B.; Hamren, S.; Harding, S.E.; Marber, M.S. Quantifying the release of biomarkers of myocardial necrosis from cardiac myocytes and intact myocardium. Clin. Chem. 2017, 63, 990–996. [Google Scholar]
- Mair, J.; Lindahl, B.; Hammarsten, O.; Müller, C.; Giannitsis, E.; Huber, K.; Möckel, M.; Plebani, M.; Thygesen, K. How is cardiac troponin released from injured myocardium? Eur. Heart J. Acute Cardiovasc. Care 2018, 6, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Fraser, C.G. Biological Variation: From Principles to Practice; AACC Press: Washington, DC, USA, 2001. [Google Scholar]
- Clerico, A.; Zaninotto, M.; Padoan, A.; Masotti, S.; Musetti, V.; Prontera, C.; Ndreu, R.; Zucchelli, G.; Passino, C.; Migliardi, M.; et al. Evaluation of analytical performance of immunoassay methods for cardiac troponin I and T: From theory to practice. Adv. Clin. Chem. 2019, 93, 239–262. [Google Scholar] [PubMed]
- Clerico, A.; Padoan, A.; Zaninotto, M.; Passino, C.; Plebani, M. Clinical relevance of biological variation of cardiac troponins. Clin. Chem. Lab. Med. 2020, 59, 641–652. [Google Scholar] [CrossRef]
- Clerico, A.; Zaninotto, M.; Aimo, A.; Cardinale, D.M.; Dittadi, R.; Sandri, M.T.; Perrone, M.A.; Belloni, L.; Fortunato, A.; Trenti, T.; et al. Variability of cardiac troponin levels in normal subjects and in patients with cardiovascular diseases: Analytical considerations and clinical relevance. Clin. Chem. Lab. Med. 2023, 61, 1209–1229. [Google Scholar]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 267–315. [Google Scholar]
- Chapman, A.R.; Adamson, P.D.; Shah, A.S.V.; Anand, A.; Strachan, F.E.; Ferry, A.V.; Lee, K.K.; Berry, C.; Findlay, I.; Cruikshank, A.; et al. High-sensitivity cardiac troponin and the universal definition of myocardial infarction. Circulation 2020, 141, 161–171. [Google Scholar]
- Emdin, M.; Clerico, A.; Clemenza, F.; Galvani, M.; Latini, R.; Masson, S.; Mulè, P.; Panteghini, M.; Valle, R.; Zaninotto, M.; et al. Recommendations for the clinical use of cardiac natriuretic peptides. Ital. Heart J. 2005, 6, 430–446. [Google Scholar]
- Palazzuoli, A.; Masson, S.; Ronco, C.; Maisel, A. Clinical relevance of biomarkers in heart failure and cardiorenal syndrome: The role of natriuretic peptides and troponin. Heart Fail Rev. 2014, 19, 267–284. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [PubMed]
- Aakre, K.M.; Saenger, A.K.; Body, R.; Collinson, P.; Hammarsten, O.; Jaffe, A.S.; Kavsak, P.; Omland, T.; Ordonez-Lianos, J.; Apple, F.S. Analytical considerations in deriving 99th percentile upper reference limits for high-sensitivity cardiac troponin assays: Educational recommendations from the IFCC Committee on Clinical Application of Cardiac Bio-Markers. Clin. Chem. 2022, 68, 1022–1030. [Google Scholar] [CrossRef] [PubMed]
- Hickman, P.E.; Abhayaratna, W.P.; Potter, J.M.; Koerbin, G. Age-related differences in hs-cTnI concentration in healthy adults. Clin. Biochem. 2019, 69, 26–29. [Google Scholar] [CrossRef]
- Shah, A.S.V.; Griffiths, M.; Lee, K.K.; A McAllister, D.; Hunter, A.L.; Ferry, A.V.; Cruikshank, A.; Reid, A.; Stoddart, M.; Strachan, F.; et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: Prospective cohort study. Br. Med. J. 2015, 350, g7873. [Google Scholar] [CrossRef]
- Slagman, A.; Searle, J.; Vollert, J.O.; Storchmann, H.; Büschenfelde, D.M.Z.; von Recum, J.; Vlasny, D.; Ale-Abaei, A.; Koch, M.; Müller, C.; et al. Sex differences of troponin test performance in chest pain patients. Int. J. Cardiol. 2015, 187, 246–251. [Google Scholar] [CrossRef]
- Shah, A.S.V.; Ferry, A.V.; Mills, N.L. Cardiac biomarkers and the diagnosis of myocardial infarction in women. Curr. Cradiol. Rep. 2017, 19, 40. [Google Scholar] [CrossRef]
- McRae, A.; Graham, M.; Abedin, T.; Ji, Y.; Yang, H.; Wang, D.; Southern, D.; Andruchow, J.; Lang, E.; Innes, G.; et al. Sex-specific, high-sensitivity cardiac troponin T cut-off concentrations for ruling out acute myocardial infarction with a single measurement. CJEM 2019, 21, 26–33. [Google Scholar] [CrossRef]
- Romiti, G.F.; Cangemi, R.; Toriello, F.; Ruscio, E.; Sciomer, S.; Moscucci, F.; Vincenti, M.; Crescioli, C.; Proietti, M.; Basili, S.; et al. Sex-specific cut-offs for hgh-sensitivity cardiac troponin: Is less more? Cardiovasc. Ther. 2019, 2019, 9546931. [Google Scholar] [CrossRef]
- Barakett-Hamadé, V.; Mchantaf, G.; Sleilaty, G. Sex-specific, high-sensitivity cardiac troponin T cut-off concentrations for ruling out acute myocardial infarction with a single measurement. Clin. Chim. Acta 2021, 519, 76–82. [Google Scholar] [CrossRef]
- Kimenai, D.M.; Janssen, E.B.N.J.; Eggers, K.M.; Lindahl, B.; den Ruijter, H.M.; Bekers, O.; Appelman, Y.; Meex, S.J.R. Sex-specific versus overall clinical dcision limits for cardiac troponin I and T for the diagnosis of acute myocardial infarction: A systematic review. Clin. Chem. 2018, 64, 1034–1043. [Google Scholar] [CrossRef]
- Clerico, A.; Masotti, S.; Musetti, V.; Ripoli, A.; Aloe, R.; Di Pietro, M.; Rizzardi, S.; Dittadi, R.; Carrozza, C.; Belloni, L.; et al. Evaluation of 99th percentile and reference change values of the hs-cTnI method using ADVIA Centaur XPT platform: A multicenter study. Clin. Chim. Acta 2019, 495, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Clerico, A.; Ripoli, A.; Masotti, S.; Musetti, V.; Aloe, R.; Dipalo, M.; Rizzardi, S.; Dittadi, R.; Carrozza, C.; Storti, S.; et al. Evaluation of 99th percentile and reference change values of a high sensitivity cTnI method: A multicenter study. Clin. Chim. Acta 2019, 493, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Clerico, A.; Aimo, A.; Zaninotto, M.; Plebani, M. Diagnostic algorithms for non-ST-segment elevation myocardial infarction: Open issues. Clin. Chem. Lab. Med. 2021, 59, 1761–1771. [Google Scholar] [CrossRef] [PubMed]
- Ndreu, R.; Musetti, V.; Masotti, S.; Zaninotto, M.; Prontera, C.; Zucchelli, G.C.; Plebani, M.; Clerico, A. Evaluation of the cTnT immunoassay using quality control samples. Clin. Chim. Acta 2019, 495, 269–270. [Google Scholar] [CrossRef] [PubMed]
- Koerbin, G.; Potter, J.M.; Nascimento, M.P.D.; Cullen, L.; Scanlan, S.L.; Woods, C.; Hickman, P.E. The intra-individual variation of cardiac troponin I: The effects of sex, age, climatic season, and time between samples. Clin. Chem. Lab. Med. 2022, 60, 1001–1009. [Google Scholar] [CrossRef]
- Diaz-Garzon, J.; Fernandez-Calle, P.; Sandberg, S.; Özcürümez, M.; Bartlett, W.A.; Coskun, A.; Carobene, A.; Perich, C.; Simon, M.; Marques, F.; et al. Biological variation of cardiac troponins in health and disease: A systematic review and meta-analysis. Clin. Chem. 2021, 67, 256–264. [Google Scholar] [CrossRef]
- Dawson, L.P.; Nehme, E.; Nehme, Z.; Zomer, E.; Bloom, J.; Cox, S.; Anderson, D.; Stephenson, M.; Ball, J.; Zhou, J.; et al. Chest pain management using prehospital Point-of-Care Troponin and paramedic risk assessment. JAMA Inter. Med. 2023, 183, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Fabre-Estremera, B.; Smith, S.W.; Sandoval, Y.; Schulz, K.; Okeson, B.; Cullen, L.; Apple, F.S. Rapid rule-out of myocardial infarction Using a single high-sensitivity cardiac troponin I measurement strategy at presentation to the emergency department: The SAFETY study. Clin. Chem. 2023, 69, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Collinson, P.; Aakre, K.M.; Saenger, A.; Body, R.; Hammarsten, O.; Jaffe, A.S.; Kavsak, P.; Omland, T.; Ordonez-Lianos, J.; Karon, B.; et al. Cardiac troponin measurement at the point of care: Educational recommendations on analytical and clinical aspects by the IFCC Committee on Clinical Applications of Cardiac Bio-Markers (IFCC C-CB). Clin. Chem. Lab. Med. 2023, 61, 989–998. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart disease and stroke statistics-2022 update: A report from the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef]
- Fountoulaki, K.; Ventoulis, I.; Drokou, A.; Georgarakou, K.; Parissis, J.; Polyzogopoulou, E. Emergency department risk assessment and disposition of acute heart failure patients: Existing evidence and ongoing challenges. Heart Fail. Rev. 2023, 28, 781–793. [Google Scholar] [CrossRef]
- CCollins, S.P.; Storrow, A.B.; Levy, P.D.; Albert, N.; Butler, J.; Ezekowitz, J.A.; Felker, G.M.; Fermann, G.J.; Fonarow, G.C.; Givertz, M.M.; et al. Early management of patients with acute heart failure: State of the art and future directions: A consensus document from the SAEM/HFSA acute heart failure working group. Acad. Emerg. Med. 2015, 22, 94–112. [Google Scholar] [CrossRef] [PubMed]
- Mebazaa, A.; Yilmaz, M.B.; Levy, P.; Ponikowski, P.; Peacock, W.F.; Laribi, S.; Ristic, A.D.; Lambrinou, E.; Masip, J.; Riley, J.P.; et al. Recommendations on pre-hospital & early hospital management of acute heart failure: A consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur. J. Heart Fail. 2015, 17, 544–558. [Google Scholar] [CrossRef]
- Kurmani, S.; Squire, I. Acute heart failure: Definition, classification and epidemiology. Curr. Heart Fail. Rep. 2017, 14, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Arrigo, M.; Jessup, M.; Mullens, W.; Reza, N.; Shah, A.M.; Sliwa, K.; Mebazaa, A. Acute heart failure. Nat. Rev. Dis. Primers 2020, 6, 16. [Google Scholar] [CrossRef]
- Januzzi, J.L., Jr.; Chen-Tournoux, A.A.; Christenson, R.H.; Doros, G.; Hollander, J.E.; Levy, P.D.; Nagurney, J.T.; Nowak, R.M.; Pang, P.S.; Patel, D.; et al. N-terminal pro-B-type natriuretic peptide in the emergency department: The ICON-RELOADED study. J. Am. Coll. Cardiol. 2018, 71, 1191–1200. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wen, Z.; Peng, L.; Liu, X.; Luo, Y.; Wu, B.; Li, S. Diagnostic value of MR-proANP for heart failure in patients with acute dyspnea: A meta-analysis. Acta Cardiol. 2020, 75, 68–74. [Google Scholar] [CrossRef]
- Han, J.H.; Hwang, S.O.; Cha, K.-C.; Roh, Y.-I.; Kim, S.J.; Kim, H.S.; Jung, W.J. High-sensitivity Troponin I assay for differential diagnosis of new-onset myocardial infarction in patients with acute decompensated heart failure. Yonsei Med. J. 2021, 62, 129–136. [Google Scholar] [CrossRef]
- Abboud, A.; Kui, N.; Gaggin, H.K.; Ibrahim, N.E.; Chen-Tournoux, A.A.; Christenson, R.H.; Hollander, J.E.; Levy, P.D.; Nagurney, J.T.; Nowak, R.M.; et al. Multiple cardiac biomarker testing among patients with acute dyspnea from the ICON-RELOADED Study. J. Card. Fail. 2022, 28, 226–233. [Google Scholar] [CrossRef]
- Breidthardt, T.; van Doorn, W.P.; van der Linden, N.; Diebold, M.; Wussler, D.; Danier, I.; Zimmermann, T.; Shrestha, S.; Kozhuharov, N.; Belkin, M.; et al. Diurnal variations in natriuretic peptide levels: Clinical implications for the diagnosis of Acute Heart Failure. Circ. Heart Fail. 2022, 15, e009165. [Google Scholar] [CrossRef] [PubMed]
- Castro-Portillo, E.; López-Izquierdo, R.; Sanz-García, A.; Ortega, G.J.; Delgado-Benito, J.F.; Villamor, M.A.C.; Sánchez-Soberón, I.; Vegas, C.d.P.; Martín-Rodríguez, F. Role of prehospital point-of-care N-terminal pro- brain natriuretic peptide in acute life-threatening cardiovascular disease. J. Cardiol. 2022, 364, 126–132. [Google Scholar] [CrossRef]
- Chetran, A.; Costache, A.D.; Ciongradi, C.I.; Duca, S.T.; Mitu, O.; Sorodoc, V.; Cianga, C.M.; Tuchilus, C.; Mitu, I.; Mitea, R.D.; et al. ECG and biomarker profile in patients with Acute Heart Failure: A pilot study. Diagnostics 2022, 12, 3037. [Google Scholar] [CrossRef] [PubMed]
- Crisanti, L.; Valli, G.; Cennamo, E.; Capolino, A.; Fratini, P.; Cesaro, C.; Adducchio, G.; De Magistris, A.; Terlizzi, F.; Ruggieri, M.P.; et al. Usefulness of high-sensitivity troponin I in risk stratification and final disposition of patients with Acute Heart Failure in the Emergency Department: Comparison between HFpEF vs. HFrEF. Medicina 2022, 59, 7. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, Y.; Wettersten, N.; van Veldhuisen, D.J.; Mueller, C.; Filippatos, G.; Nowak, R.; Hogan, C.; Kontos, M.C.; Cannon, C.M.; Müeller, G.A.; et al. Decongestion, kidney injury and prognosis in patients with acute heart failure. Int. J. Cardiol. 2022, 354, 29–37. [Google Scholar] [CrossRef]
- Kozhuharov, N.; Martin, J.; Wussler, D.; Lopez-Ayala, P.; Belkin, M.; Strebel, I.; Flores, D.; Diebold, M.; Shrestha, S.; Nowak, A.; et al. Clinical effect of obesity on N-terminal pro-B-type natriuretic peptide cut-off concentrations for the diagnosis of acute heart failure. Eur. J. Heart Fail. 2022, 24, 1545–1554. [Google Scholar] [CrossRef]
- Lee, K.K.; Doudesis, D.; Anwar, M.; Astengo, F.; Chenevier-Gobeaux, C.; Claessens, Y.-E.; Wussler, D.; Kozhuharov, N.; Strebel, I.; Sabti, Z.; et al. Development and validation of a decision support tool for the diagnosis of acute heart failure: Systematic review, meta-analysis, and modelling study. BMJ 2022, 377, e068424. [Google Scholar] [CrossRef]
- Miftode, R.-S.; Constantinescu, D.; Cianga, C.-M.; Petris, A.-O.; Costache, I.-I.; Mitu, O.; Miftode, I.-L.; Mitu, I.; Timpau, A.-S.; Duca, S.-T.; et al. A rising star of the multimarker panel: Growth Differentiation Factor-15 levels are an independent predictor of mortality in Acute Heart Failure patients admitted to an Emergency Clinical Hospital from eastern Europe. Life 2022, 12, 1948. [Google Scholar] [CrossRef]
- Wang, Z.; Dong, Y.; Gao, Q.; Zhang, Q.; Jiang, H. The role of acute heart failure index (AHFI) combined with emergency heart failure mortality risk grade (EHMRG) in the evaluation of clinical outcomes and prognosis in patients with acute heart failure. Acta Cardiol. 2022, 77, 488–493. [Google Scholar] [CrossRef]
- Wessman, T.; Zorlak, A.; Wändell, P.; Melander, O.; Carlsson, A.C.; Ruge, T. Myocardial injury defined as elevated high-sensitivity cardiac troponin T is associated with higher mortality in patients seeking care at emergency departments with acute dyspnea. BMC Emerg. Med. 2023, 23, 40. [Google Scholar] [CrossRef]
- Krauser, D.G.; Lloyd-Jones, D.M.; Chae, C.U.; Cameron, R.; Anwaruddin, S.; Baggish, A.L.; Chen, A.; Tung, R.; Januzzi, J.L., Jr. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: A ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005, 149, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Clerico, A.; Passino, C.; Franzini, M.; Emdin, M. Cardiac biomarker testing in the clinical laboratory: Where do we stand? General overview of the methodology with special emphasis on natriuretic peptides. Clin. Chim. Acta 2015, 443, 17–24. [Google Scholar] [CrossRef]
- Clerico, A.; Zaninotto, M.; Passino, C.; Plebani, M. Obese phenotype and natriuretic peptides in patients with heart failure with preserved ejection fraction. Clin. Chem. Lab. Med. 2018, 56, 1015–1025. [Google Scholar] [CrossRef]
- Mueller, C.; McDonald, K.; de Boer, R.A.; Maisel, A.; Cleland, J.G.; Kozhuharov, N.; Coats, A.J.; Metra, M.; Mebazaa, A.; Ruschitzka, F.; et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur. J. Heart Fail. 2019, 21, 715–731. [Google Scholar] [CrossRef] [PubMed]
- Clerico, A.; Zucchelli, G.C.; Pilo, A.; Passino, C.; Emdin, M. Clinical relevance of biological variation: The lesson of brain natriuretic peptide (BNP) and NT-proBNP assay. Clin. Chem. Lab. Med. 2006, 44, 366–378. [Google Scholar] [CrossRef] [PubMed]
- Miró, Ò.; Peacock, F.W.; McMurray, J.J.; Bueno, H.; Christ, M.; Maisel, A.S.; Cullen, L.; Cowie, M.R.; Di Somma, S.; Sánchez, F.J.M.; et al. Acute Heart Failure Study Group of the ESC Acute Cardiovascular Care Association. European Society of Cardiology—Acute Cardiovascular Care Association position paper on safe discharge of acute heart failure patients from the emergency department. Eur. Heart J. Acute Cardiovasc. Care 2017, 6, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Masip, J.; Peacok, W.F.; Arrigo, M.; Rossello, X.; Platz, E.; Cullen, L.; Mebazaa, A.; Price, S.; Bueno, H.; Di Somma, S.; et al. Acute Heart Failure Study Group of the Association for Acute Cardiovascular Care (ACVC) of the European Society of Cardiology. Acute Heart Failure in the 2021 ESC Heart Failure Guidelines: A scientific statement from the Association for Acute CardioVascular Care (ACVC) of the European Society of Cardiology. Eur. Heart J. Acute Cardiovasc. Care 2021, 11, 173–185. [Google Scholar]
- Demissei, B.G.; Postmus, D.; Cleland, J.G.; O’Connor, C.M.; Metra, M.; Ponikowski, P.; Teerlink, J.R.; Cotter, G.; Davison, B.A.; Givertz, M.M.; et al. Plasma biomarkers to predict or rule out early post-discharge events after hospitalization for acute heart failure. Eur. J. Heart Fail. 2017, 19, 728–738. [Google Scholar] [CrossRef]
- Gao, Y.; Bai, X.; Lu, J.; Zhang, L.; Yan, X.; Huang, X.; Dai, H.; Wang, Y.; Hou, L.; Wang, S.; et al. Prognostic value of multiple circulating biomarkers for 2-year death in Acute Heart Failure with preserved ejection fraction. Front Cardiovasc. Med. 2021, 8, 779282. [Google Scholar] [CrossRef]
- Zhang, L.; He, G.; Huo, X.; Ji, R.; Tian, A.; Pu, B.; Lei, L.; Li, J.; Peng, Y. Long-term cumulative high-sensitivity cardiac troponin T and mortality among patients with acute heart failure. ESC Heart Fail. 2023, 10, 1781–1792. [Google Scholar] [CrossRef]
- Shafi, A.M.A.; Shaikh, S.A.; Shirke, M.M.; Iddawela, S.; Harky, A. Cardiac manifestations in COVID-19 patients—A systematic review. J. Card. Surg. 2020, 35, 1988–2008. [Google Scholar] [CrossRef]
- Inciardi, R.M.; Adamo, M.; Lupi, L.; Cani, D.S.; Di Pasquale, M.; Tomasoni, D.; Italia, L.; Zaccone, G.; Tedino, C.; Fabbricatore, D.; et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur. Heart J. 2020, 41, 1821–1829. [Google Scholar] [CrossRef]
- De Michieli, L.; Jaffe, A.S.; Sandoval, Y. Use and prognostic implications of cardiac troponin in COVID-19. Cardiol. Clin. 2022, 40, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, C.C.; Ahmed, A.; Burger, A.L.; Muthspiel, M.; Jäger, B.; Wojta, J.; Huber, K. Biomarkers associated with cardiovascular disease in COVID-19. Cells 2022, 11, 922. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo-Marquisá, A.; Cubero-Gallego, H.; Aparisi, Á.; Vaquerizo, B.; Ribas-Barquet, N. Myocardial injury in COVID-19 and its implications in short- and long-term outcomes. Front. Cardiovasc. Med. 2022, 9, 901245. [Google Scholar] [CrossRef] [PubMed]
- Task Force for the management of COVID-19 of the European Society of Cardiology. European Society of Cardiology guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: Part 1-epidemiology, pathophysiology, and diagnosis. Eur. Heart J. 2022, 43, 1033–1058. [Google Scholar] [CrossRef]
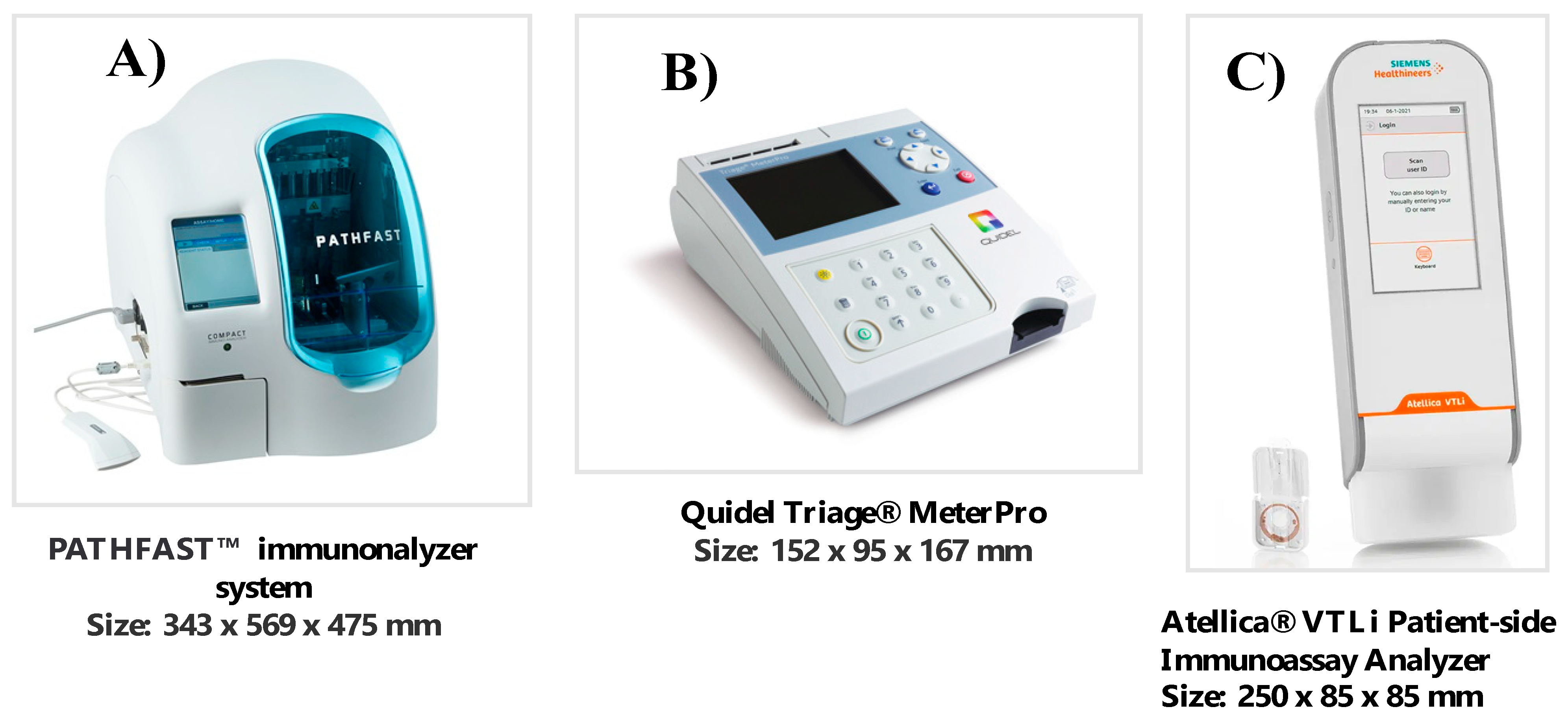
| hs-cTnI POCT Method | Instrument Characteristics | LoD (ng/L) | LoQ 10% (ng/L) | 99th Percentile URL (ng/L) | Reference |
|---|---|---|---|---|---|
| PATHFAST™ POC hs-cTnI (PHC Europe B.V., Nijverheidsweg, The Netherlands). | This method combines the technologies of chemiluminescence for signal detection (enzyme alkaline phosphatase bound to anti-cTnI monclonal antibodies) and magnetic migration for the separation of the bound phase, using antibodies marked by magnetic particles. | 2.9 | 11.0 | W 21.1 (13.4–25.3) * M 27.0 (18.5–27.7) * | Sorensen NA et al. [27] |
| Quidel TriageTrue High Sensitivity Troponin I Test (Quidel Corporation Headquarters, San Diego, CA 92121, USA). | The immunofluorescent Quidel TriageTrue method uses a few drops of whole blood or EDTA plasma for biomarker measurement with the Triage® MeterPro instrument, which has the weight of a cell phone. | 0.7–1.6 | 4.4–8.4 | W 14.4 (13.1–28.7) ** M 25.7 (18.3–37.6) ** | Boeddinghaus J et al. [28] |
| Siemens POC Atellica ® VTLi hs-cTnI (Siemens Healthineers, Erlangen, Germany). | This method uses Magnotech®-type biosensors to separate the cTnI fraction, bound by antibodies to magnetic beads, from the free fraction and detects the signal using the imaging technique called Frustrated Total Internal Reflection (FTIR). This method uses the Atellica® VTLi Patient-side Immunoassay Analyzer instrument, which has the dimensions of a hand-held instrument. | 1.2 | 6.7 | W 18.0 (9.0–78.0) ** M 27.0 (21.0–37.0) ** | Apple FS et al. [29] |
| Study [Reference] | Study Type | N° and Type of Population | POCT Method | Main Clinical Results | Conclusions |
|---|---|---|---|---|---|
| Sörensen NA, et al. 2019 [27] | prospective cohort study (enrolment time: from July 2013 to July 2016) | 669 patients presenting to the ED with suspected MI (STEMI excluded). | POCT hs-cTnI assay (PATHFAST hs-cTnI) | Negative predictive value of 99.7% (95% CI, 98.1–100.0%) and 48.0% of patients ruled out, whereas 14.6% were ruled in with a positive predictive value of 86.5% (95% CI, 77.6–92.8%). | The diagnostic performance of the new POCT assay was highly comparable to that of the laboratory hs-cTnI methods |
| Boeddinghaus J, et al. 2020 [28] | prospective international multicenter study (12 centers, 5 countries) | 1261 adult patients presenting to the ED with symptoms suggestive of MI with an onset or peak within the last 12 h. | POCT hs-cTnI (TriageTrue) assay | The 0/1 h algorithm ruled out 55% of patients (NPV: 100%; 95% CI: 98.8% to 100%), and ruled in 18% of patients (PPV: 76.8%; 95% CI: 67.2% to 84.7%). | The POCT hs-cTnI assay provides high diagnostic accuracy in patients with suspected AMI with a clinical performance that is at least comparable to that of best-validated central laboratory assays. |
| Apple FS, et al. 2022 [30] | 2 prospective observational studies | 1086 patients (8.1% with MI) from a US derivation cohort (SEIGE) and 1486 (5.5% MI) from an Australian validation cohort (SAMIE). All of these patients presented to the ED with suspected acute coronary syndrome. | Whole-blood POC hs-cTnI assay | A derivation whole-blood POC hs-cTnI provided a sensitivity of 98.9% (95% CI, 93.8–100%) and negative predictive value of 99.5% (95% CI, 97.2–100%) for ruling out MI. In the validation cohort, the clinical sensitivity was 98.8% (95% CI, 93.3–100%), and negative predictive value was 99.8% (95% CI, 99.1–100%); 17.8% and 41.8%, respectively, were defined as low risk for discharge. The 30-day adverse cardiac events were 0.1% (n = 1) for SEIGE and 0.8% (n = 5) for SAMIE. | A POC whole-blood hs-cTnI assay permits accessible, rapid, and safe exclusion of MI and may expedite discharge from the emergency department. |
| Bruinen AL, et al. 2022 [31] | prospective, observational cohort study (enrolled from September 2019 until November 2020) | 152 adult patients (55% female, 45% male) referred to the cardiac ED because of acute chest pain suspected for ACS. | Atellica VTLi Patient-side Immunoassay Analyzer (method and sample comparison) using different sample types including capillary blood, in comparison with standard laboratory hs-cTnI testing | No significant difference was observed between venous whole blood vs. plasma analyzed. The difference between capillary blood and venous blood showed a constant bias of 7.1%, for which a correction factor was implemented. | No clinically relevant differences were observed for the capillary POC results compared to plasma analyzed with a standard immunoassay analyzer. |
| Gunsolos IL, et al. 2022 [33] | study cohort | 1089 patients (418 F and 671 M) presenting to ED, with suspected AMI (excluded: age < 21 years, pregnancy, trauma, transferred from an outside hospital). | Whole-blood, point-of-care (POC) high-sensitivity cardiac troponin I (hs-cTnI) assay (Siemens Atellica VTLi) | At baseline (0 h), POC hs-cTnI assay had a sensitivity of 65.7% (95% CI 47.8–80.9) for females and 67.9% (54.0–79.7) for males and NPV of 96.4% (93.9–98.1) for females and 96.7% (94.9–98.0) for males. At 2 h, sensitivity improved to 82.9% (66.4–93.4) for females and 80.4% (67.6–89.8) for males, while NPV improved to 98.2% (96.1–99.3) and 97.9% (96.3–99.0), respectively. | For central laboratory assays (ARCHITECT and Atellica hs-cTnI methods), comparable diagnostics were observed at 2 h. |
| Fabre-Estremera, et al. 2023 [73] | prospective, observationalcohort study | 1171 patients (mean age of 58.9 years and 38.2% female) presenting to an US ED. | Atellica ®IM High-Sensitivity Troponin I assay | AMI occurred in 97 patients (8.3%), 78.3% of which were type 2 AMI. The optimal rule-out POCT hs-cTnI method threshold was <10 ng/L, which identified 519 (44.3%) patients as low-risk at presentation, with sensitivity of 99.0% (95% CI, 94.4–100) and NPV of 99.8% (95% CI, 98.9–100). For type 1 AMI, sensitivity was 100% (95% CI, 83.9–100) and NPV 100% (95% CI, 99.3–100). Regarding myocardial injury, the sensitivity and NPV were 99.5% (95% CI, 97.9–100) and 99.8% (95% CI, 98.9–100), respectively. For 30-day adverse events, sensitivity was 96.8% (95% CI, 94.3–98.4) and NPV 97.9% (95% CI, 96.2–98.9). | A single-measurement strategy using the POCT hs-cTnI method I able to rapidly identify patients at low risk of AMI and 30-day adverse events, allowing potential early discharge after ED presentation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aspromonte, N.; Zaninotto, M.; Aimo, A.; Fumarulo, I.; Plebani, M.; Clerico, A. Measurement of Cardiac-Specific Biomarkers in the Emergency Department: New Insight in Risk Evaluation. Int. J. Mol. Sci. 2023, 24, 15998. https://doi.org/10.3390/ijms242115998
Aspromonte N, Zaninotto M, Aimo A, Fumarulo I, Plebani M, Clerico A. Measurement of Cardiac-Specific Biomarkers in the Emergency Department: New Insight in Risk Evaluation. International Journal of Molecular Sciences. 2023; 24(21):15998. https://doi.org/10.3390/ijms242115998
Chicago/Turabian StyleAspromonte, Nadia, Martina Zaninotto, Alberto Aimo, Isabella Fumarulo, Mario Plebani, and Aldo Clerico. 2023. "Measurement of Cardiac-Specific Biomarkers in the Emergency Department: New Insight in Risk Evaluation" International Journal of Molecular Sciences 24, no. 21: 15998. https://doi.org/10.3390/ijms242115998
APA StyleAspromonte, N., Zaninotto, M., Aimo, A., Fumarulo, I., Plebani, M., & Clerico, A. (2023). Measurement of Cardiac-Specific Biomarkers in the Emergency Department: New Insight in Risk Evaluation. International Journal of Molecular Sciences, 24(21), 15998. https://doi.org/10.3390/ijms242115998







