Prognostic Value of the miR-17~92 Cluster in Chronic Lymphocytic Leukemia
Abstract
1. Introduction
2. Results
2.1. Patients’ Characteristics
2.2. Expression of the miR-17∼92 Cluster in Different Risk Groups
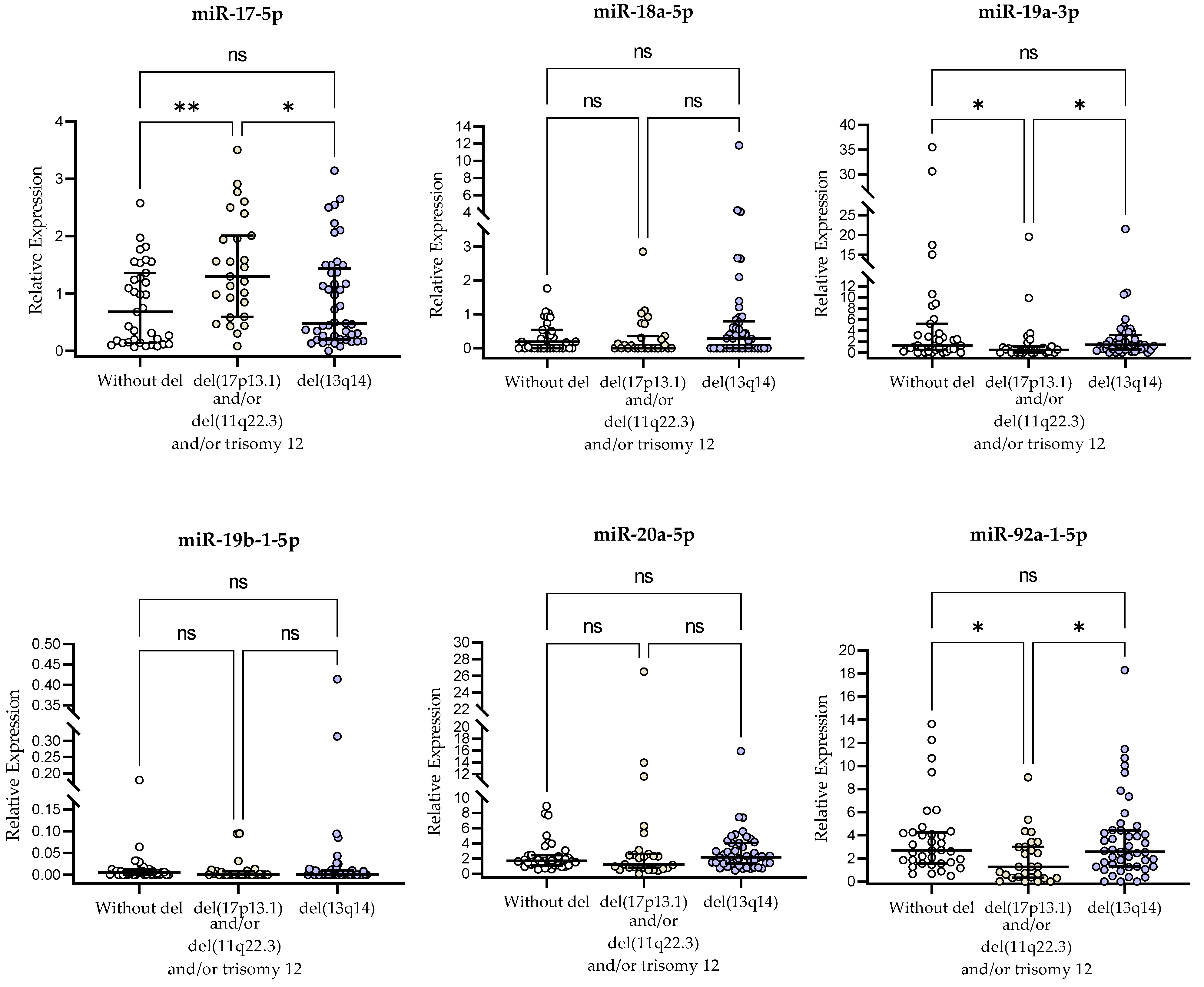
2.3. miR-17∼92-Cluster Expression and Genetic Aberrations
2.4. miR-17∼92-Cluster Expression and Chromosome 13q14 Deletion
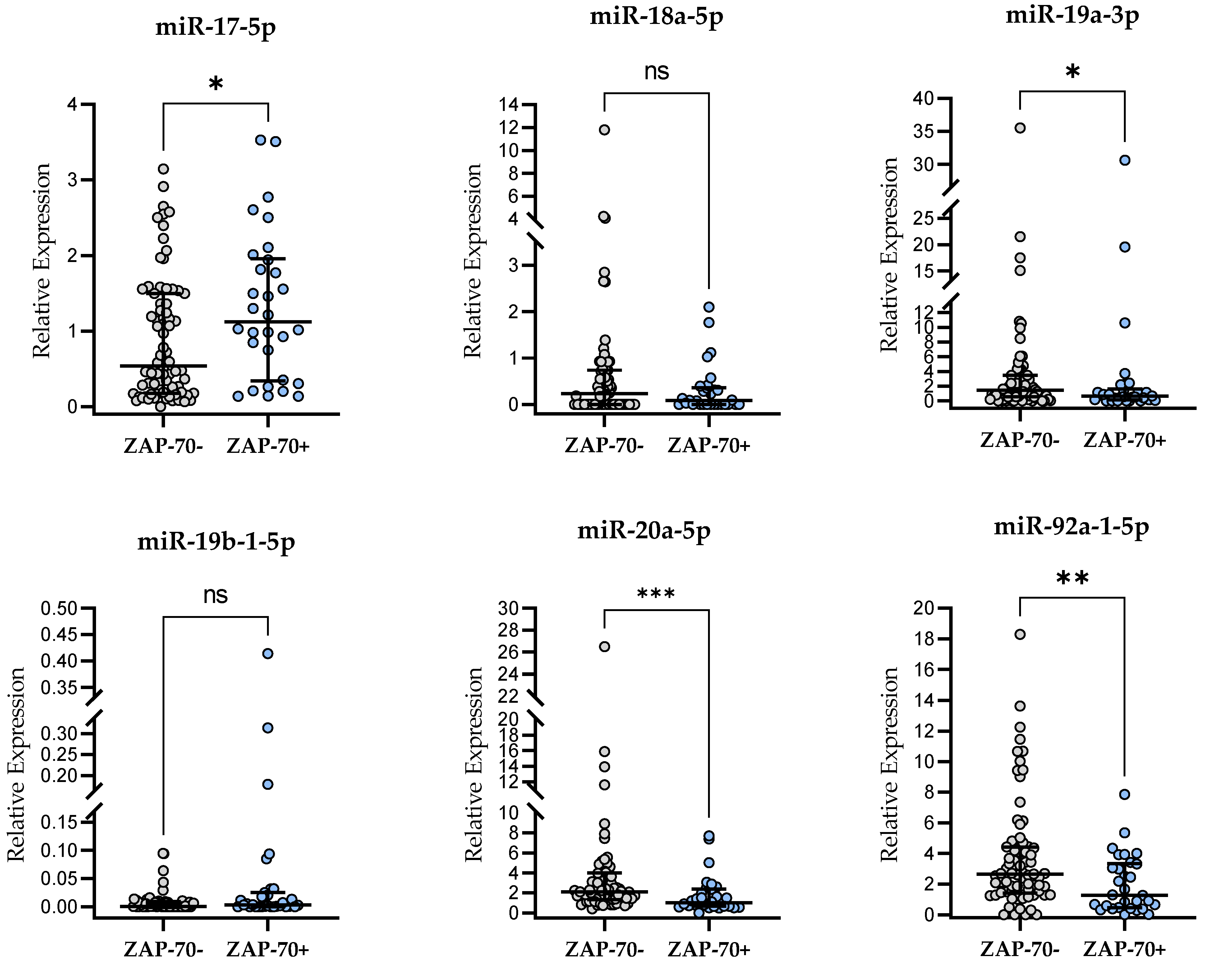
2.5. miR-17∼92-Cluster Expression and ZAP-70 Expression
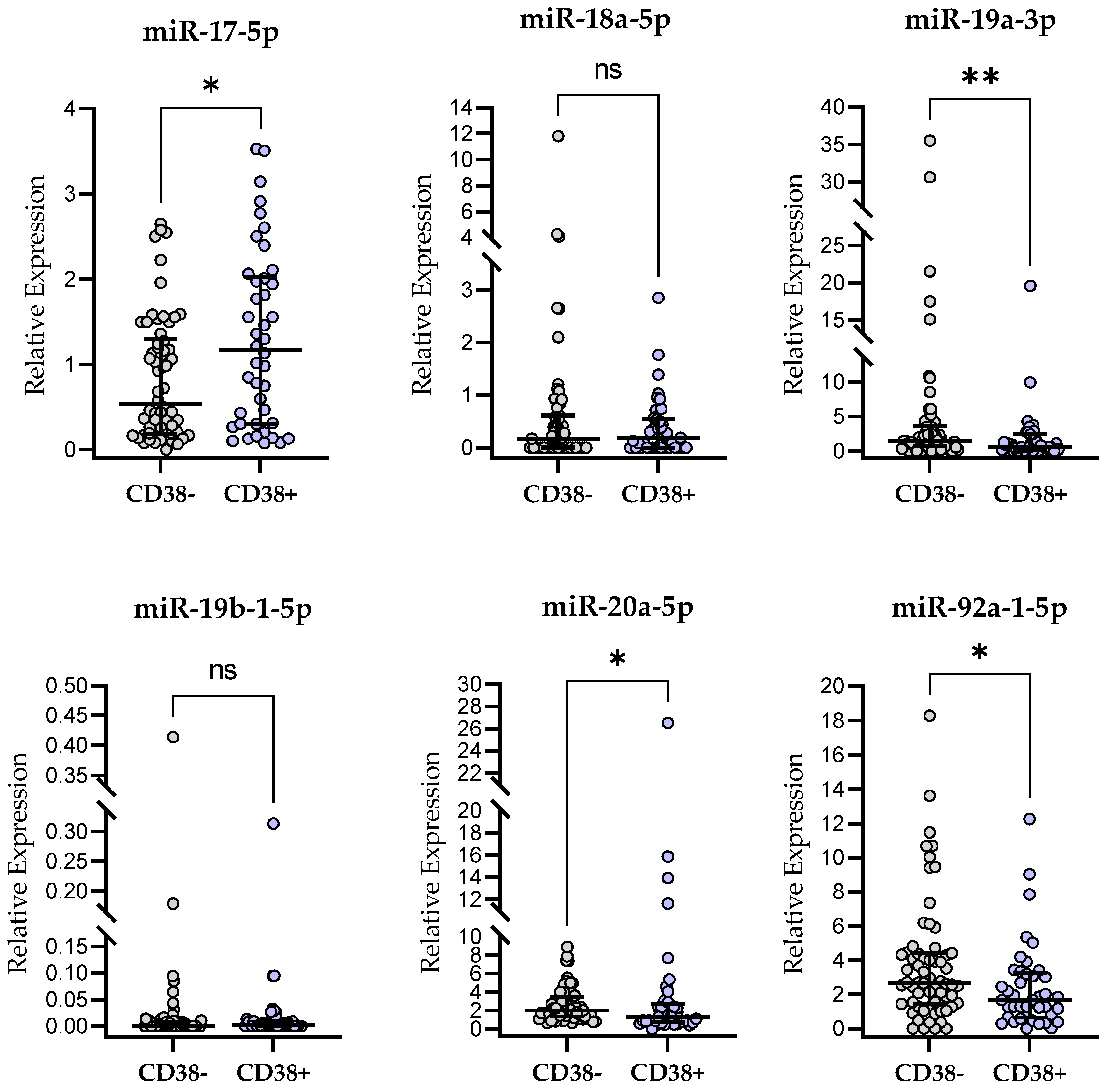
2.6. miR-17∼92-Cluster Expression and CD38 Expression
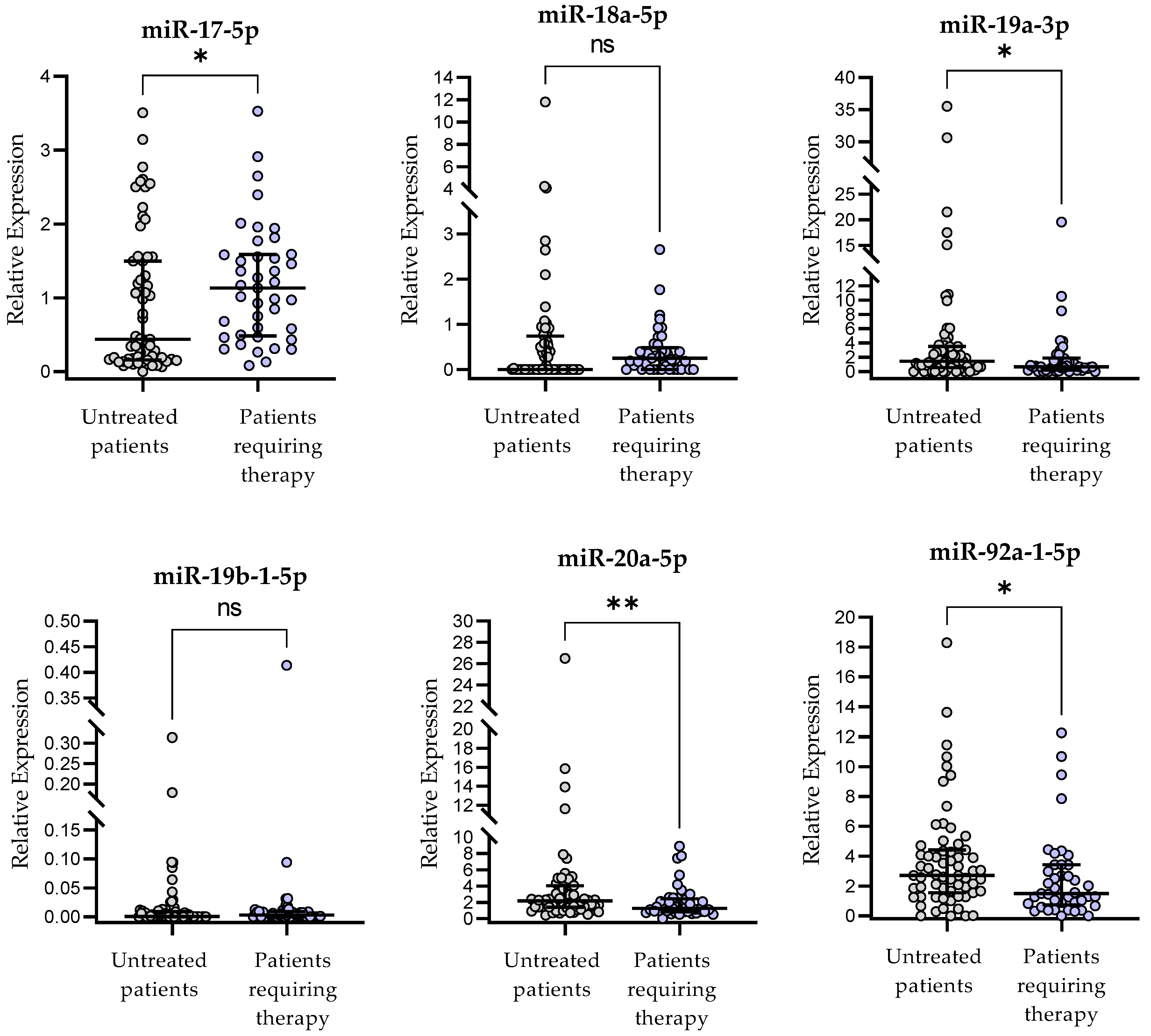
2.7. miR-17∼92-Cluster Expression and Clinical Outcome of CLL Patients
- -
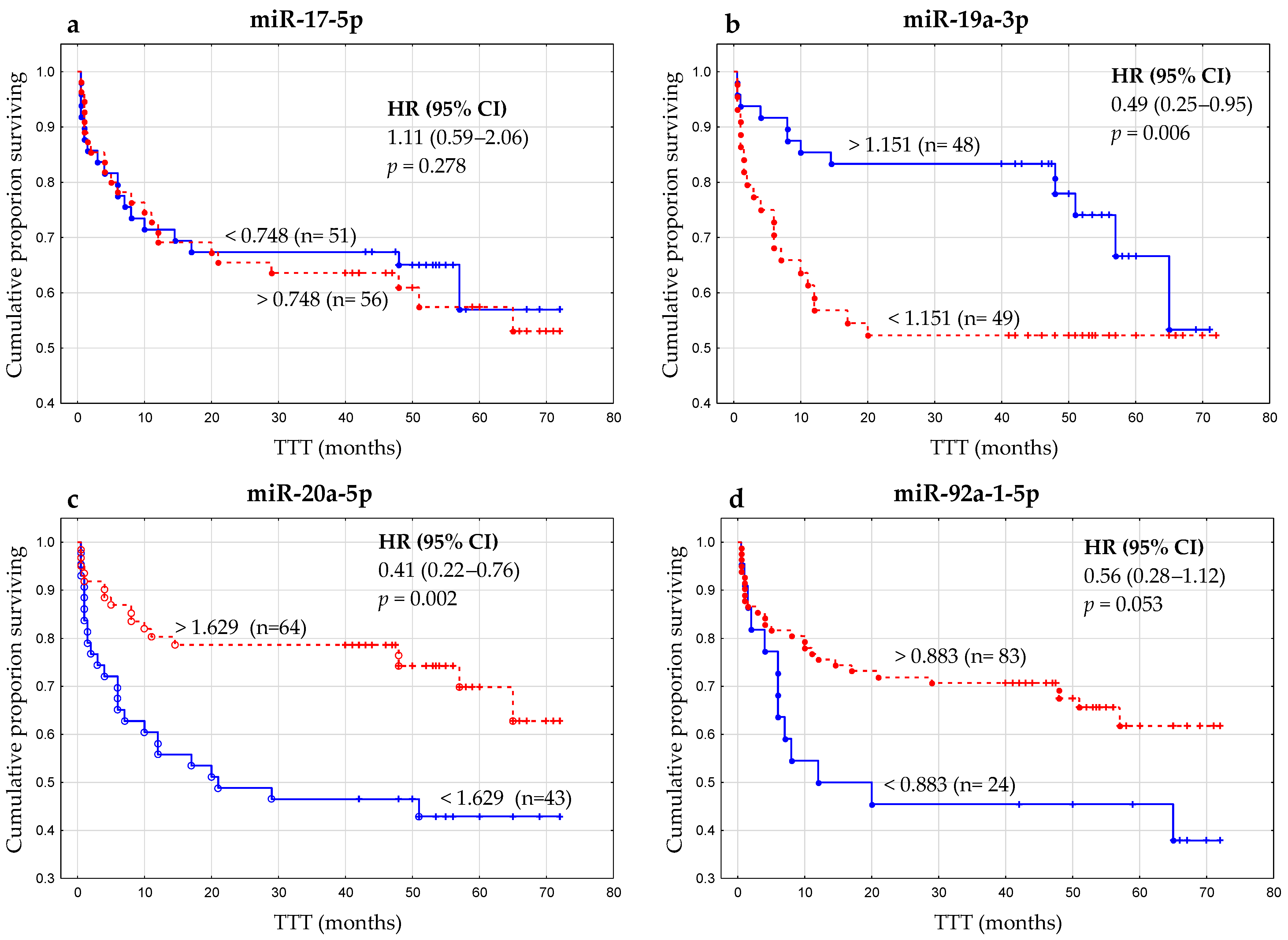
- The cutoff value for miR-17-5p expression was found to be: >0.748 (AUC, 0.752; 95% confidence interval [CI], 0.656–0.842; p < 0.0001; Figure 6a).
- -
- The cutoff for miR-19a-3p expression was found to be: <1.151 (AUC, 0.653; 95% CI, 0.546–0.760; p < 0.01; Figure 6b).
- -
- The cutoff for miR-20a-5p expression was found to be: <1.629 (AUC, 0.719; 95% CI, 0.612–0.825; p < 0.0001; Figure 6c).
- -
- The cutoff for miR-92a-1-5p expression was: <0.883 (AUC, 0.666; 95% CI, 0.547–0.725; p < 0.01; Figure 6d).
- -
- For miR-18a-5p and miR-19b-1-5p, it was not possible to determine the optimal cutoff point with a significance of p < 0.05.
3. Discussion
4. Materials and Methods
4.1. Patients and Samples
4.2. PBMCs Isolation
4.3. I-FISH Analysis
4.4. RNA Preparation and microRNA Expression Analysis
4.5. Flow Cytometric Analysis of CD38 and ZAP-70 Expression in CLL Cells
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kay, N.E.; Hampel, P.J.; Van Dyke, D.L.; Parikh, S.A. CLL Update 2022: A Continuing Evolution in Care. Blood Rev. 2022, 54, 100930. [Google Scholar] [CrossRef] [PubMed]
- Farzadfard, E.; Kalantari, T.; Tamaddon, G. Serum Expression of Seven MicroRNAs in Chronic Lymphocytic Leukemia Patients. J. Blood Med. 2020, 11, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Hallek, M.; Shanafelt, T.D.; Eichhorst, B. Chronic Lymphocytic Leukaemia. Lancet 2018, 391, 1524–1537. [Google Scholar] [CrossRef] [PubMed]
- Kulis, M.; Martin-Subero, J.I. Integrative Epigenomics in Chronic Lymphocytic Leukaemia: Biological Insights and Clinical Applications. Br. J. Haematol. 2022, 00, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Buccheri, V.; Barreto, W.G.; Fogliatto, L.M.; Capra, M.; Marchiani, M.; Rocha, V. Prognostic and Therapeutic Stratification in CLL: Focus on 17p Deletion and P53 Mutation. Ann. Hematol. 2018, 97, 2269–2278. [Google Scholar] [CrossRef]
- Stefaniuk, P.; Onyszczuk, J.; Szymczyk, A.; Podhorecka, M. Therapeutic Options for Patients with TP53 Deficient Chronic Lymphocytic Leukemia: Narrative Review. Cancer Manag. Res. 2021, 13, 1459–1476. [Google Scholar] [CrossRef]
- Mirzaei, H.; Fathullahzadeh, S.; Khanmohammadi, R.; Darijani, M.; Momeni, F.; Masoudifar, A.; Goodarzi, M.; Mardanshah, O.; Stenvang, J.; Jaafari, M.R.; et al. State of the Art in MicroRNA as Diagnostic and Therapeutic Biomarkers in Chronic Lymphocytic Leukemia. J. Cell. Physiol. 2018, 233, 888–900. [Google Scholar] [CrossRef]
- Hadi, N.; Namazi, F.; Ketabchi, F.; Khosravian, F.; Nateghi, B.; Talebi, A.; Baghi, M.; Mianesaz, H.; Zare, F.; Salehi, M. MiR-574, MiR-499, MiR-125b, MiR-106a, and MiR-9 Potentially Target TGFBR-1 and TGFBR-2 Genes Involving in Inflammatory Response Pathway: Potential Novel Biomarkers for Chronic Lymphocytic Leukemia. Pathol. Res. Pract. 2022, 238, 154077. [Google Scholar] [CrossRef]
- Papageorgiou, S.G.; Kontos, C.K.; Tsiakanikas, P.; Stavroulaki, G.; Bouchla, A.; Vasilatou, D.; Bazani, E.; Lazarakou, A.; Scorilas, A.; Pappa, V. Elevated MiR-20b-5p Expression in Peripheral Blood Mononuclear Cells: A Novel, Independent Molecular Biomarker of Favorable Prognosis in Chronic Lymphocytic Leukemia. Leuk. Res. 2018, 70, 1–7. [Google Scholar] [CrossRef]
- Papageorgiou, S.G.; Diamantopoulos, M.A.; Kontos, C.K.; Bouchla, A.; Vasilatou, D.; Bazani, E.; Scorilas, A.; Pappa, V. MicroRNA-92a-3p Overexpression in Peripheral Blood Mononuclear Cells Is an Independent Predictor of Prolonged Overall Survival of Patients with Chronic Lymphocytic Leukemia. Leuk. Lymphoma 2019, 60, 658–667. [Google Scholar] [CrossRef]
- Fang, L.-L.; Wang, X.-H.; Sun, B.-F.; Zhang, X.-D.; Zhu, X.-H.; Yu, Z.-J.; Luo, H. Expression, Regulation and Mechanism of Action of the MiR-17-92 Cluster in Tumor Cells (Review). Int. J. Mol. Med. 2017, 40, 1624–1630. [Google Scholar] [CrossRef] [PubMed]
- Hutter, K.; Rülicke, T.; Szabo, T.G.; Andersen, L.; Villunger, A.; Herzog, S. The MiR-15a/16-1 and MiR-15b/16-2 Clusters Regulate Early B Cell Development by Limiting IL-7 Receptor Expression. Front. Immunol. 2022, 13, 967914. [Google Scholar] [CrossRef]
- Balatti, V.; Pekarky, Y.; Croce, C.M. Role of MicroRNA in Chronic Lymphocytic Leukemia Onset and Progression. J. Hematol. Oncol. 2015, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Hallek, M.; Cheson, B.D.; Catovsky, D.; Caligaris-Cappio, F.; Dighiero, G.; Döhner, H.; Hillmen, P.; Keating, M.J.; Montserrat, E.; Rai, K.R.; et al. Guidelines for the Diagnosis and Treatment of Chronic Lymphocytic Leukemia: A Report from the International Workshop on Chronic Lymphocytic Leukemia Updating the National Cancer Institute-Working Group 1996 Guidelines. Blood 2008, 111, 5446–5456. [Google Scholar] [CrossRef]
- Hallek, M.; Cheson, B.D.; Catovsky, D.; Caligaris-Cappio, F.; Dighiero, G.; Döhner, H.; Hillmen, P.; Keating, M.; Montserrat, E.; Chiorazzi, N.; et al. IwCLL Guidelines for Diagnosis, Indications for Treatment, Response Assessment, and Supportive Management of CLL. Blood 2018, 131, 2745–2760. [Google Scholar] [CrossRef] [PubMed]
- Rai, K.R.; Sawitsky, A.; Cronkite, E.P.; Chanana, A.D.; Levy, R.N.; Pasternack, B.S. Clinical Staging of Chronic Lymphocytic Leukemia. Blood 1975, 46, 219–234. [Google Scholar] [CrossRef]
- Durak Aras, B.; Isik, S.; Uskudar Teke, H.; Aslan, A.; Yavasoglu, F.; Gulbas, Z.; Demirkan, F.; Ozen, H.; Cilingir, O.; Inci, N.S.; et al. Which Prognostic Marker Is Responsible for the Clinical Heterogeneity in CLL with 13q Deletion? Mol. Cytogenet. 2021, 14, 2. [Google Scholar] [CrossRef]
- Ota, A.; Tagawa, H.; Karnan, S.; Tsuzuki, S.; Karpas, A.; Kira, S.; Yoshida, Y.; Seto, M. Identification and Characterization of a Novel Gene, C13orf25, as a Target for 13q31-Q32 Amplification in Malignant Lymphoma. Cancer Res. 2004, 64, 3087–3095. [Google Scholar] [CrossRef]
- He, L.; Thomson, J.M.; Hemann, M.T.; Hernando-Monge, E.; Mu, D.; Goodson, S.; Powers, S.; Cordon-Cardo, C.; Lowe, S.W.; Hannon, G.J.; et al. A MicroRNA Polycistron as a Potential Human Oncogene. Nature 2005, 435, 828–833. [Google Scholar] [CrossRef]
- Mogilyansky, E.; Rigoutsos, I. The MiR-17/92 Cluster: A Comprehensive Update on Its Genomics, Genetics, Functions and Increasingly Important and Numerous Roles in Health and Disease. Cell Death Differ. 2013, 20, 1603–1614. [Google Scholar] [CrossRef]
- Krsmanovic, P.; Mocikova, H.; Chramostova, K.; Klanova, M.; Trnkova, M.; Pesta, M.; Laslo, P.; Pytlik, R.; Stopka, T.; Trneny, M.; et al. Circulating MicroRNAs in Cerebrospinal Fluid and Plasma: Sensitive Tool for Detection of Secondary CNS Involvement, Monitoring of Therapy and Prediction of CNS Relapse in Aggressive B-NHL Lymphomas. Cancers 2022, 14, 2305. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Zhang, L.; Zhang, M.; Zhang, Y.; Fan, D.; Jiang, J.; Ye, L.; Fang, X.; Chen, X.; Fan, S.; et al. Prognostic Value of High-Expression of MiR-17-92 Cluster in Various Tumors: Evidence from a Meta-Analysis. Sci. Rep. 2017, 7, 8375. [Google Scholar] [CrossRef] [PubMed]
- Zanette, D.L.; Rivadavia, F.; Molfetta, G.A.; Barbuzano, F.G.; Proto-Siqueira, R.; Silva, W.A.; Falcão, R.P.; Zago, M.A. MiRNA Expression Profiles in Chronic Lymphocytic and Acute Lymphocytic Leukemia. Braz. J. Med. Biol. Res. 2007, 40, 1435–1440. [Google Scholar] [CrossRef] [PubMed]
- Döhner, H.; Stilgenbauer, S.; Benner, A.; Leupolt, E.; Kröber, A.; Bullinger, L.; Döhner, K.; Bentz, M.; Lichter, P. Genomic Aberrations and Survival in Chronic Lymphocytic Leukemia. N. Engl. J. Med. 2000, 343, 1910–1916. [Google Scholar] [CrossRef] [PubMed]
- Puiggros, A.; Blanco, G.; Espinet, B. Genetic Abnormalities in Chronic Lymphocytic Leukemia: Where We Are and Where We Go. BioMed Res. Int. 2014, 2014, 435983. [Google Scholar] [CrossRef]
- Kuo, G.; Wu, C.-Y.; Yang, H.-Y. MiR-17-92 Cluster and Immunity. J. Formos. Med. Assoc. Taiwan Yi Zhi 2019, 118, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Willimott, S.; Wagner, S.D. Stromal Cells and CD40 Ligand (CD154) Alter the MiRNome and Induce MiRNA Clusters Including, MiR-125b/MiR-99a/Let-7c and MiR-17-92 in Chronic Lymphocytic Leukaemia. Leukemia 2012, 26, 1113–1116. [Google Scholar] [CrossRef] [PubMed]
- Filip, D.; Mraz, M. The Role of MYC in the Transformation and Aggressiveness of “indolent” B-Cell Malignancies. Leuk. Lymphoma 2020, 61, 510–524. [Google Scholar] [CrossRef]
- Psathas, J.N.; Doonan, P.J.; Raman, P.; Freedman, B.D.; Minn, A.J.; Thomas-Tikhonenko, A. The Myc-MiR-17-92 Axis Amplifies B-Cell Receptor Signaling via Inhibition of ITIM Proteins: A Novel Lymphomagenic Feed-Forward Loop. Blood 2013, 122, 4220–4229. [Google Scholar] [CrossRef] [PubMed]
- Mihailovich, M.; Bremang, M.; Spadotto, V.; Musiani, D.; Vitale, E.; Varano, G.; Zambelli, F.; Mancuso, F.M.; Cairns, D.A.; Pavesi, G.; et al. MiR-17-92 Fine-Tunes MYC Expression and Function to Ensure Optimal B Cell Lymphoma Growth. Nat. Commun. 2015, 6, 8725. [Google Scholar] [CrossRef]
- Shen, J.; Pan, J.; Du, C.; Si, W.; Yao, M.; Xu, L.; Zheng, H.; Xu, M.; Chen, D.; Wang, S.; et al. Silencing NKG2D Ligand-Targeting MiRNAs Enhances Natural Killer Cell-Mediated Cytotoxicity in Breast Cancer. Cell Death Dis. 2017, 8, e2740. [Google Scholar] [CrossRef]
- Zarobkiewicz, M.K.; Bojarska-Junak, A.A. The Mysterious Actor-Γδ T Lymphocytes in Chronic Lymphocytic Leukaemia (CLL). Cells 2022, 11, 661. [Google Scholar] [CrossRef]
- Selven, H.; Andersen, S.; Pedersen, M.I.; Lombardi, A.P.G.; Busund, L.-T.R.; Kilvær, T.K. High Expression of MiR-17-5p and MiR-20a-5p Predicts Favorable Disease-Specific Survival in Stage I-III Colon Cancer. Sci. Rep. 2022, 12, 7080. [Google Scholar] [CrossRef]
- Khalifa, M.M.; Zaki, N.E.; Nazier, A.A.; Moussa, M.A.; Haleem, R.A.; Rabie, M.A.; Mansour, A.R. Prognostic Significance of MicroRNA 17-92 Cluster Expression in Egyptian Chronic Lymphocytic Leukemia Patients. J. Egypt. Natl. Cancer Inst. 2021, 33, 37. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Huang, D.; Ma, K.; Deng, X.; Shao, Z. MiR-19a as a Prognostic Indicator for Cancer Patients: A Meta-Analysis. Biosci. Rep. 2019, 39, BSR20182370. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Wu, X.; Xiang, S.; Qiao, M.; Cen, X.; Pan, X.; Huang, X.; Zhao, Z. Regulatory Mechanism of MiR-20a-5p Expression in Cancer. Cell Death Discov. 2022, 8, 262. [Google Scholar] [CrossRef] [PubMed]
- Parker, H.; Rose-Zerilli, M.J.J.; Parker, A.; Chaplin, T.; Wade, R.; Gardiner, A.; Griffiths, M.; Collins, A.; Young, B.D.; Oscier, D.G.; et al. 13q Deletion Anatomy and Disease Progression in Patients with Chronic Lymphocytic Leukemia. Leukemia 2011, 25, 489–497. [Google Scholar] [CrossRef]
- Chena, C.; Avalos, J.S.; Bezares, R.F.; Arrossagaray, G.; Turdó, K.; Bistmans, A.; Slavutsky, I. Biallelic Deletion 13q14.3 in Patients with Chronic Lymphocytic Leukemia: Cytogenetic, FISH and Clinical Studies. Eur. J. Haematol. 2008, 81, 94–99. [Google Scholar] [CrossRef]
- Bomben, R.; Gobessi, S.; Dal Bo, M.; Volinia, S.; Marconi, D.; Tissino, E.; Benedetti, D.; Zucchetto, A.; Rossi, D.; Gaidano, G.; et al. The MiR-17∼92 Family Regulates the Response to Toll-like Receptor 9 Triggering of CLL Cells with Unmutated IGHV Genes. Leukemia 2012, 26, 1584–1593. [Google Scholar] [CrossRef]
- Cao, Y.; Liu, Y.; Shang, L.; Chen, H.; Yue, Y.; Dong, W.; Guo, Y.; Yang, H.; Yang, X.; Liu, Y.; et al. Overexpression of MiR-17 Predicts Adverse Prognosis and Disease Recurrence for Acute Myeloid Leukemia. Int. J. Clin. Oncol. 2022, 27, 1222–1232. [Google Scholar] [CrossRef]
- Moussay, E.; Wang, K.; Cho, J.-H.; van Moer, K.; Pierson, S.; Paggetti, J.; Nazarov, P.V.; Palissot, V.; Hood, L.E.; Berchem, G.; et al. MicroRNA as Biomarkers and Regulators in B-Cell Chronic Lymphocytic Leukemia. Proc. Natl. Acad. Sci. USA 2011, 108, 6573–6578. [Google Scholar] [CrossRef] [PubMed]
- Hus, I.; Podhorecka, M.; Bojarska-Junak, A.; Roliński, J.; Schmitt, M.; Sieklucka, M.; Wasik-Szczepanek, E.; Dmoszyńska, A. The Clinical Significance of ZAP-70 and CD38 Expression in B-Cell Chronic Lymphocytic Leukaemia. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2006, 17, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Woś, J.; Chocholska, S.; Kowalska, W.; Tomczak, W.; Szymańska, A.; Karczmarczyk, A.; Szuster-Ciesielska, A.; Wojciechowska, A.; Bojarska-Junak, A. Prognostic Value of Tie2-Expressing Monocytes in Chronic Lymphocytic Leukemia Patients. Cancers 2021, 13, 2817. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | n (%) |
|---|---|
| Total number of patients | 107 |
| Patient sex | |
| Female (%) | 61 (57.0) |
| Male (%) | 46 (43.0) |
| Rai Stage | |
| 0 (%) | 50 (46.7) |
| I (%) | 18 (16.8) |
| II (%) | 25 (23.4) |
| III (%) | 5 (4.7) |
| IV (%) | 9 (8.4) |
| Risk group | |
| Low | 50 (46.7) |
| Intermediate | 43 (40.2) |
| High | 14 (13.1) |
| ZAP-70 (cutoff 20%) | |
| Positive (%) | 30 (28.0) |
| Negative (%) | 77 (72.0) |
| CD38 (cutoff 30%) | |
| Positive (%) | 42 (39.3) |
| Negative (%) | 65 (60.7) |
| Cytogenetic abnormalities | |
| del(17p13.1) | 4 (3.7) |
| del(11q22.3) | 16 (14.9) |
| Trisomy 12 | 9 (8.4) |
| sole del(13q14) | 45 (42.0) |
| monoallelic del(13q) | 35/45 (77.8) |
| biallelic del(13q) | 10/45 (22.2) |
| Without del(17p13.1), del(11q22.3), trisomy 12, and del(13q14) | 33 (31.0) |
| Patients requiring therapy (%) | 45 (42.1) |
| Untreated patients (%) | 62 (57.9) |
| Median (IQR; interquartile range) | |
| Age at diagnosis (years) | 65 (61–72) |
| WBC count (G/L) | 25 (17.15–54.79) |
| Lymphocyte count (G/L) | 18.32 (10.56–44.96) |
| LDH (IU/L) | 377 (325–424) |
| β2M (mg/dL) | 2.46 (2.06–3.19) |
| CD19+/CD5+/ZAP-70+ cells (%) | 7.85 (3.89–20.73) |
| CD19+/CD5+/CD38+ cells (%) | 6.71 (16.05–37.04) |
| microRNAs | Low-Risk (Stage 0) n = 50 | Intermediate-Risk (Stages I–II) n = 43 | High-Risk (Stages III–IV) n = 14 |
|---|---|---|---|
| miR-17-5p | 0.466 (0.175–1.329) * | 0.495 (0.247–1.511) | 1.097 (0.293–1.945) * |
| miR-18a-5p | 0.000 (0.000–0.555) | 0.2955 (0.000–0.624) | 0.274 (0.153–1.075) |
| miR-19a-3p | 1.568 (0.000–0.009) * | 0.8878 (0.214–2.944) | 0.592 (0.000–1.374) * |
| miR-19b-1-5p | 0.0007 (0.000–0.009) | 0.0012 (0.000–0.006) | 0.006 (0.000–0.015) |
| miR-20a-5p | 2.031 (1.111–3.722) * | 1.626 (0.832–3.204) | 1.372 (1.070–2.348) * |
| miR-92a-1-5p | 2.648 (1.401–4.739) | 1.897 (0.645–3.552) | 2.103 (0.887–4.378) |
| Criterion | miR-17-5p | miR-18a-5p | miR-19a-3p | miR-19b-1-5p | miR-20a-5p | miR-92a-1-5p |
|---|---|---|---|---|---|---|
| Response (CR or PR) | ||||||
| Median | 0.680 ## | 0.315 | 0.665 | 0.003 | 1.213 ^^ | 2.381 ** |
| IQR | 0.419–1.192 | 0.046–0.404 | 0.79–3.248 | 0.000–0.013 | 0.686–2.918 | 0.483–4.130 |
| Stable Disease (SD) | ||||||
| Median | 0.754 | 0.268 | 0.885 | 0.0005 | 1.094 | 2.342 |
| IQR | 0.412–1.812 | 0.00–1.349 | 0.07–5.893 | 0.0001–0.003 | 0.766–2.988 | 0.598–8.560 |
| Progressive Disease (PD) | ||||||
| Median | 1.360 # | 0.276 | 0.676 | 0.003 | 1.097 ^ | 1.289 * |
| IQR | 0.595–1.589 | 0.000–0.719 | 0.511–1.835 | 0.0001–0.012 | 0.832–2.511 | 0.367–2.186 |
| Deaths | ||||||
| Median | 1.676 # | 0.048 | 0.374 | 0.004 | 0.664 ^ | 0.658 ** |
| IQR | 0.869–2.208 | 0.000–0.572 | 0.000–1.261 | 0.000–0.014 | 0.000–1.093 | 0.087–1.824 |
| Univariate | Multivariate | ||||
|---|---|---|---|---|---|
| Variable | Median TTT (Months) | HR (95% CI) | p | HR (95% CI) | p |
| Age | |||||
| ≥65 years | 46 | 2.01 (1.083–3.73) | 0.023 | 1.71 (0.81–3.5) | 0.159 |
| <65 years | 50 | ||||
| ZAP-70 | |||||
| ≥20% | 29 | 2.86 (1.52–5.38) | 0.008 | 0.72 (0.31–1.65) | 0.054 |
| <20% | 48 | ||||
| CD38 | |||||
| ≥30% | 44 | 1.67 (0.90–3.08) | 0.042 | 0.95 (0.41–2.19) | 0.434 |
| <30% | 48 | ||||
| β2M | |||||
| ≥3.5 mg/dL | 16 | 2.65 (1.39–5.08) | 0.003 | 2.30 (1.09–4.87) | 0.008 |
| <3.5 mg/dL | 44 | ||||
| del(17p13.1) or del(11q22.3) | |||||
| Positive | 12 | 2.46 (1.29–4.73) | 0.006 | 0.39 (1.09–4.87) | 0.039 |
| Negative | 49 | ||||
| del(13q14) | |||||
| Positive | 49 | 0.51 (0.26–0.96) | 0.039 | 0.68 (0.33–1.42) | 0.31 |
| Negative | 42 | ||||
| miR-17-5p | |||||
| ≥0.748 | 42 | 1.11 (0.59–2.06) | 0.278 | NA | |
| <0.748 | 50 | ||||
| miR-19a-3p | |||||
| ≥1.151 | 49 | 0.49 (0.25–0.95) | 0.006 | 1.67 (0.76–3.63) | 0.195 |
| <1.151 | 41 | ||||
| miR-20a-5p | |||||
| ≥1.629 | 50 | 0.41 (0.22–0.76) | 0.002 | 2.96 (1.38–6.38) | 0.006 |
| <1.629 | 21 | ||||
| miR-92a-1-5p | |||||
| ≥0.883 | 48 | 0.56 (0.28–1.12) | 0.053 | NA | |
| <0.883 | 20 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chocholska, S.; Zarobkiewicz, M.; Szymańska, A.; Lehman, N.; Woś, J.; Bojarska-Junak, A. Prognostic Value of the miR-17~92 Cluster in Chronic Lymphocytic Leukemia. Int. J. Mol. Sci. 2023, 24, 1705. https://doi.org/10.3390/ijms24021705
Chocholska S, Zarobkiewicz M, Szymańska A, Lehman N, Woś J, Bojarska-Junak A. Prognostic Value of the miR-17~92 Cluster in Chronic Lymphocytic Leukemia. International Journal of Molecular Sciences. 2023; 24(2):1705. https://doi.org/10.3390/ijms24021705
Chicago/Turabian StyleChocholska, Sylwia, Michał Zarobkiewicz, Agata Szymańska, Natalia Lehman, Justyna Woś, and Agnieszka Bojarska-Junak. 2023. "Prognostic Value of the miR-17~92 Cluster in Chronic Lymphocytic Leukemia" International Journal of Molecular Sciences 24, no. 2: 1705. https://doi.org/10.3390/ijms24021705
APA StyleChocholska, S., Zarobkiewicz, M., Szymańska, A., Lehman, N., Woś, J., & Bojarska-Junak, A. (2023). Prognostic Value of the miR-17~92 Cluster in Chronic Lymphocytic Leukemia. International Journal of Molecular Sciences, 24(2), 1705. https://doi.org/10.3390/ijms24021705









