Antibacterial Effect of Acoustic Cavitation Promoted by Mesoporous Silicon Nanoparticles
Abstract
1. Introduction
2. Results and Discussion
2.1. Characterization of m-PSi NPs
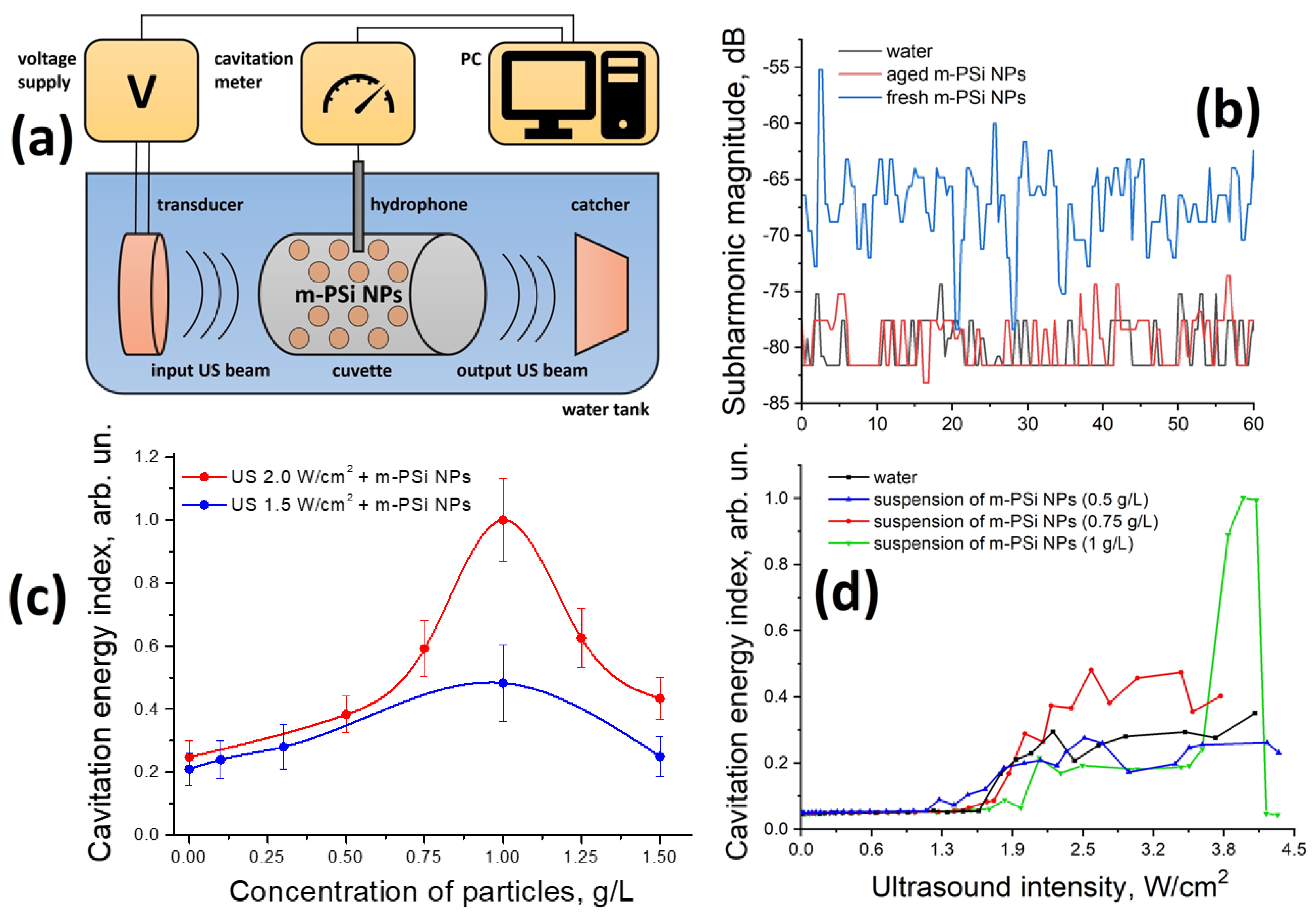
2.2. Cavitation Activity in Suspensions of m-PSi NPs
2.3. Antibacterial Effect of Ultrasound in the Presence of m-PSi NPs
3. Materials and Methods
3.1. Preparation of m-PSi NPs
3.2. Measurements of m-PSi NPs’ Sizes and Crystallinity
3.3. FTIR Measurement
3.4. Setup for the Cavitation Activity Detection
3.5. In Vitro Studies
3.6. Scanning Electron Microscopy of Bacteria
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vouga, M.; Greub, G. Emerging bacterial pathogens: The past and beyond. Clin. Microbiol. Infect. 2016, 22, 12–21. [Google Scholar] [CrossRef]
- Urban-Chmiel, R.; Marek, A.; Stępień-Pyśniak, D.; Wieczorek, K.; Dec, M.; Nowaczek, A.; Osek, J. Antibiotic resistance in bacteria—A review. Antibiotics 2022, 11, 1079. [Google Scholar] [CrossRef] [PubMed]
- De Dicastillo, C.L.; Correa, M.G.; Martínez, F.B.; Streitt, C.; Galotto, M.J. Antimicrobial effect of titanium dioxide nanoparticles. In Antimicrobial Resistance—A One Health Perspective; Mareș, M., Lim, S.H.E., Lai, K., Cristina, R., Eds.; IntechOpen: London, UK, 2020. [Google Scholar] [CrossRef]
- Sirelkhatim, A.; Mahmud, S.; Seeni, A.; Kaus, H.N.M.; Ann, L.C.; Bakhori, S.K.M.; Hasan, H.; Mohamad, D. Review on zinc oxide nanoparticles: Antibacterial activity and toxicity mechanism. Nanomicro Lett. 2015, 7, 219–242. [Google Scholar] [CrossRef] [PubMed]
- Bezza, F.A.; Tichapondwa, S.M.; Chirwa, E.M.N. Fabrication of monodispersed copper oxide nanoparticles with potential application as antimicrobial agents. Sci. Rep. 2020, 10, 16680. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Xu, Z.; Gu, L.; Xu, H.; Han, F.; Chen, B.; Pan, X. Preparation and antibacterial properties of gold nanoparticles: A review. Environ. Chem. Lett. 2020, 19, 167–187. [Google Scholar] [CrossRef]
- Bruna, T.; Maldonado-Bravo, F.; Jara, P.; Caro, N. Silver nanoparticles and their antibacterial applications. Int. J. Mol. Sci. 2021, 22, 7202. [Google Scholar] [CrossRef]
- Guo, L.; Wang, H.; Wang, Y.; Liu, F.; Feng, L. Organic polymer nanoparticles with primary ammonium salt as potent antibacterial nanomaterials. ACS Appl. Mater. Interfaces 2020, 12, 21254–21262. [Google Scholar] [CrossRef]
- Divya, K.; Vijayan, S.; George, T.K.; Jisha, M.S. Antimicrobial properties of chitosan nanoparticles: Mode of action and factors affecting activity. Fibers Polym. 2017, 18, 221–230. [Google Scholar] [CrossRef]
- Pang, Q.; Wu, K.; Jiang, Z.; Shi, Z.; Si, Z.; Wang, Q.; Cao, Y.; Hou, R.; Zhu, Y. A Polyaniline nanoparticles crosslinked hydrogel with excellent photothermal antibacterial and mechanical properties for wound dressing. Macromol. Biosci. 2021, 22, 2100386. [Google Scholar] [CrossRef]
- Hajipour, M.J.; Fromm, K.M.; Ashkarran, A.A.; de Aberasturi, D.J.; de Larramendi, I.R.; Rojo, T.; Serpooshan, V.; Parak, W.J.; Mahmoudi, M. Antibacterial properties of nanoparticles. Trends Biotechnol. 2012, 30, 499–511. [Google Scholar] [CrossRef]
- Wang, C.; Makvandi, P.; Zare, E.N.; Tay, F.R.; Niu, L. Advances in antimicrobial organic and inorganic nanocompounds in biomedicine. Adv. Ther. 2020, 3, 2000024. [Google Scholar] [CrossRef]
- Low, S.P.; Voelcker, N.H.; Canham, L.T.; Williams, K.A. The biocompatibility of porous silicon in tissues of the eye. Biomaterials 2009, 30, 2873–2880. [Google Scholar] [CrossRef] [PubMed]
- Canham, L.T. Nanoscale semiconducting silicon as a nutritional food additive. Nanotechnology 2007, 18, 185704. [Google Scholar] [CrossRef]
- Park, J.-H.; Gu, L.; von Maltzahn, G.; Ruoslahti, E.; Bhatia, S.N.; Sailor, M.J. Biodegradable luminescent porous silicon nanoparticles for in vivo applications. Nat. Mat. 2009, 8, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Timoshenko, V.Y.; Kudryavtsev, A.A.; Osminkina, L.A.; Vorontzov, A.S.; Ryabchikov, Y.V.; Belogorokhov, I.A.; Kovalev, D.; Kashkarov, P.K. Silicon nanocrystals as photosensitizers of active oxygen for biomedical applications. JETP Lett. 2006, 83, 423–426. [Google Scholar] [CrossRef]
- Santos, H.A. Porous Silicon for Biomedical Applications, 2nd ed.; Woodhead Publishing: Sawston, UK, 2021. [Google Scholar]
- Hill, C.R.; Bamber, J.C.; ter Haar, G.R. Physical Principles of Medical Ultrasonics, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2004. [Google Scholar]
- Canavese, G.; Ancona, A.; Racca, L.; Canta, M.; Dumontel, B.; Barbaresco, F.; Limongi, T.; Cauda, V. Nanoparticle-assisted ultrasound: A special focus on sonodynamic therapy against cancer. J. Chem. Eng. 2018, 340, 155–172. [Google Scholar] [CrossRef]
- Costley, D.; Ewan, C.M.; Fowley, C.; McHale, A.P.; Atchison, J.; Nomikou, N.; Callan, J.F. Treating cancer with sonodynamic therapy: A review. Int. J. Hyperthermia 2015, 31, 107–117. [Google Scholar] [CrossRef]
- Ter Haar, G. HIFU tissue ablation: Concept and devices. Adv. Exp. Med. Biol. 2016, 880, 3–20. [Google Scholar] [CrossRef]
- Kessel, D.; Lo, J.; Jeffers, R.; Fowlkes, J.B.; Cain, C. Modes of photodynamic vs sonodynamic cytotoxicity. J. Photochem. Photobiol. B. 1995, 28, 219–221. [Google Scholar] [CrossRef]
- Serpe, L.; Foglietta, F.; Canaparo, R. Nanosonotechnology: The next challenge in cancer sonodynamic therapy. Nanotechnol. Rev. 2012, 1, 173–182. [Google Scholar] [CrossRef]
- Yildirimer, L.; Thanh, N.T.K.; Loizidou, M.; Seifalian, A.M. Toxicological considerations of clinically applicable nanoparticles. Nano Today 2011, 6, 585–607. [Google Scholar] [CrossRef] [PubMed]
- Osminkina, L.A.; Sivakov, V.A.; Mysov, G.A.; Georgobiani, V.A.; Natashina, U.A.; Talkenberg, F.; Solovyev, V.V.; Kudryavtsev, A.A.; Timoshenko, V.Y. Nanoparticles prepared from porous silicon nanowires for bio-imaging and sonodynamic therapy. Nanoscale Res. Lett. 2014, 9, 463. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Lewis, G.D.; Ashokkumar, M.; Hemar, Y. Inactivation of microorganisms by low-frequency high-power ultrasound: 2. A simple model for the inactivation mechanism. Ultrason. Sonochem. 2014, 21, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Brayman, A.A.; MacConaghy, B.E.; Wang, Y.-N.; Chan, K.T.; Monsky, W.L.; Chernikov, V.P.; Buravkov, S.V.; Khokhlova, V.A.; Matula, T.J. Inactivation of planktonic Escherichia coli by focused 1-MHz ultrasound pulses with shocks: Efficacy and kinetics upon volume scale-up. Ultrasound Med. Biol. 2018, 44, 1996–2008. [Google Scholar] [CrossRef]
- Fu, Y.; Zhang, L.; Yang, Y.; Liu, C.; He, Y.; Li, P.; Yu, X. Synergistic antibacterial effect of ultrasound microbubbles combined with chitosan-modified polymyxin B-loaded liposomes on biofilm-producing Acinetobacter baumannii. Int. J. Nanomed. 2019, 14, 1805–1815. [Google Scholar] [CrossRef]
- McCorkell, G.; Nakayama, M.; Feltis, B.; Piva, T.; Geso, M. Ultrasound-stimulated microbubbles enhance radiation-induced cell killing. Ultrasound Med. Biol. 2022, 48, 2449–2460. [Google Scholar] [CrossRef]
- Roy, J.; Pandey, V.; Gupta, I.; Shekhar, H. Antibacterial sonodynamic therapy: Current status and future perspectives. ACS Biomater. Sci. Eng. 2021, 7, 219–221. [Google Scholar] [CrossRef]
- Wang, R.; Liu, Q.; Gao, A.; Tang, N.; Zhang, Q.; Zhang, A.; Cui, D. Recent developments of sonodynamic therapy in antibacterial application. Nanoscale 2022, 36, 12999–13017. [Google Scholar] [CrossRef]
- Sviridov, A.; Tamarov, K.; Fesenko, I.; Xu, W.; Andreev, V.; Timoshenko, V.; Lehto, V.P. Cavitation induced by Janus-like mesoporous silicon nanoparticles enhances ultrasound hyperthermia. Front. Chem. 2019, 7, 393. [Google Scholar] [CrossRef]
- Tamarov, K.; Sviridov, A.; Xu, W.; Malo, M.; Andreev, V.; Timoshenko, V.; Lehto, V.P. Nano air seeds trapped in mesoporous Janus nanoparticles facilitate cavitation and enhance ultrasound imaging. ACS Appl. Mater. Interfaces 2017, 9, 35234–35243. [Google Scholar] [CrossRef]
- Osminkina, L.A.; Nikolaev, A.L.; Sviridov, A.P.; Andronova, N.V.; Tamarov, K.P.; Gongalsky, M.B.; Kudryavtsev, A.A.; Treshalina, H.M.; Timoshenko, V.Y. Porous silicon nanoparticles as efficient sensitizers for sonodynamic therapy of cancer. Microporous Mesoporous Mater. 2015, 210, 169–175. [Google Scholar] [CrossRef]
- Shevchenko, S.N.; Burkhardt, M.; Sheval, E.V.; Natashina, U.A.; Grosse, C.; Nikolaev, A.L.; Gopin, A.V.; Neugebauer, U.; Kudryavtsev, A.A.; Sivakov, V.; et al. Antimicrobial Effect of Biocompatible Silicon Nanoparticles Activated Using Therapeutic Ultrasound. Langmuir 2017, 33, 2603–2609. [Google Scholar] [CrossRef] [PubMed]
- Mira, J.M.; Wu, L.; Sabuncu, S.; Sapre, A.; Civitci, F.; Ibsen, S.; Esener, S.; Yildirim, A. Gas-stabilizing sub-100 nm mesoporous silica nanoparticles for ultrasound theranostics. ACS Omega 2017, 5, 24762–24772. [Google Scholar] [CrossRef] [PubMed]
- Egoshina, V.D.; Gongalsky, M.B.; Tsurikova, U.A.; Sviridov, A.P.; Osminkina, L.A.; Andreev, V.G. The cavitation activity of aqueous suspensions of porous silicon nanoparticles with different degrees of surface hydrophobicity. Acoust. Phys. 2022, 68, 649–656. [Google Scholar] [CrossRef]
- Eremina, A.S.; Kargina, Y.V.; Kharin, A.Y.; Petukhov, D.I.; Timoshenko, V.Y. Mesoporous silicon nanoparticles covered with PEG molecules by mechanical grinding in aqueous suspensions. Microporous Mesoporous Mater. 2022, 331, 111641. [Google Scholar] [CrossRef]
- Konoplyannikov, M.; Eremina, A.; Kargina, Y.; Le-Deygen, I.; Kharin, A.; Bazylenko, T.; Yusubalieva, G.; Revkova, V.; Matchuk, O.; Zamulaeva, I.; et al. Mesoporous silicon nanoparticles loaded with salinomycin for cancer therapy applications. Microporous Mesoporous Mater. 2021, 328, 111473. [Google Scholar] [CrossRef]
- Bimbo, L.M.; Sarparanta, M.; Santos, H.A.; Airaksinen, A.J.; Makila, E.; Laaksonen, T.; Peltonen, L.; Lehto, V.-P.; Hirvonen, J.; Salonen, J. Biocompatibility of thermally hydrocarbonized porous silicon nanoparticles and their biodistribution in rats. ACS Nano 2009, 4, 3023–3032. [Google Scholar] [CrossRef]
- Gan, Q.; Dai, D.; Yuan, Y.; Qian, J.; Sha, S.; Shi, J.; Liu, C. Effect of size on the cellular endocytosis and controlled release of mesoporous silica nanoparticles for intracellular delivery. Biomed. Microdevices 2012, 14, 259–270. [Google Scholar] [CrossRef]
- Tolstik, E.; Osminkina, L.A.; Matthäus, C.; Burkhardt, M.; Tsurikov, K.E.; Natashina, U.A.; Timoshenko, V.Y.; Heintzmann, R.; Popp, J.; Sivakov, V. Studies of silicon nanoparticles uptake and biodegradation in cancer cells by Raman spectroscopy. Nanomed. NBM 2016, 12, 1931–1940. [Google Scholar] [CrossRef]
- Sviridov, A.P.; A Osminkina, L.; Kharin, A.Y.; Gongalsky, M.B.; Kargina, J.V.; A Kudryavtsev, A.; I Bezsudnova, Y.; Perova, T.S.; Geloen, A.; Lysenko, V.; et al. Cytotoxicity control of silicon nanoparticles by biopolymer coating and ultrasound irradiation for cancer theranostic applications. Nanotechnology 2017, 28, 105102. [Google Scholar] [CrossRef]
- Kumar, A.; Dixit, C.K. Methods for characterization of nanoparticles. In Advances in Nanomedicine for the Delivery of Therapeutic Nucleic Acids, 1st ed.; Nimesh, S., Chandra, R., Gupta, N., Eds.; Woodhead Publishing: Sawston, UK, 2021; pp. 43–58. [Google Scholar] [CrossRef]
- Brasili, F.; Capocefalo, A.; Palmieri, D.; Capitani, F.; Chiessi, E.; Paradossi, G.; Bordi, F.; Domenici, F. Assembling patchy plasmonic nanoparticles with aggregation-dependent antibacterial activity. J. Colloid Interface Sci. 2020, 580, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Canham, L. Handbook of Porous Silicon, 2nd ed.; Springer: Berlin, Germany, 2018. [Google Scholar]
- Riikonen, J.; Salomaki, M.; van Wonderen, J.; Kemell, M.; Xu, W.; Korhonen, O.; Ritala, M.; MacMillan, F.; Salonen, J.; Lehto, V.-P. Surface chemistry, reactivity, and pore structure of porous silicon oxidized by various methods. Langmuir 2012, 28, 10573–10583. [Google Scholar] [CrossRef] [PubMed]
- Sheng, X.; Zhang, J. Air layer on superhydrophobic surface underwater. Colloids Surf. A Physicochem. Eng. Asp. 2011, 377, 374–378. [Google Scholar] [CrossRef]
- Cullis, A.G.; Canham, L.T.; Calcott, P.D.J. The structural and luminescence properties of porous silicon. J. Appl. Phys. 1997, 82, 909–965. [Google Scholar] [CrossRef]
- Kharin, A.Y.; Kargina, Y.V.; Timoshenko, V.Y. Evolution of nanocrystal size distribution in porous silicon nanoparticles during storage in aqueous media: X-ray diffraction analysis. J. Nanopart. Res. 2019, 21, 27. [Google Scholar] [CrossRef]
- Salcedo, W.J.; Fernandez, F.J.R.; Galeazzo, E. Structural characterization of photoluminescent porous silicon with FTIR spectroscopy. Braz. J. Phys. 1997, 27, 158–161. [Google Scholar]
- Mawhinney, D.B.; Glass, J.A.; Yates, J.T. FTIR study of the oxidation of porous silicon. J. Electrochem. Soc. 1995, 142, 195–201. [Google Scholar] [CrossRef]
- Ogata, Y.; Niki, H.; Sakka, T.; Iwasaki, M. Hydrogen in porous silicon: Vibrational analysis of SiHx species. J. Phys. Chem. B 1997, 101, 1202–1206. [Google Scholar] [CrossRef]
- Benesi, H.A.; Jones, A.C. An infrared study of the water-silica gel system. J. Phys. Chem. 1959, 63, 179–182. [Google Scholar] [CrossRef]
- Cheng, M.; Li, F.; Han, T.; Yu, A.C.H.; Qin, P. Effects of ultrasound pulse parameters on cavitation properties of flowing microbubbles under physiologically relevant conditions. Ultrason. Sonochem. 2019, 52, 512–521. [Google Scholar] [CrossRef]
- Neppiras, E.A. Subharmonic and other low-frequency signals from sound-irradiated liquids. J. Sound Vib. 1969, 10, 176–186. [Google Scholar] [CrossRef]
- Bader, K.B.; Holland, C.K. Gauging the likelihood of stable cavitation from ultrasound contrast agents. Phys. Med. Biol. 2013, 58, 127–144. [Google Scholar] [CrossRef] [PubMed]
- Abbas, S.; Hayat, K.; Karangwa, E.; Bashari, M.; Zhang, X. An overview of ultrasound-assisted food-grade nanoemulsions. Food Eng. Rev. 2013, 5, 139–157. [Google Scholar] [CrossRef]
- Maiga, M.A.; Coutier-Delgosha, O.; Buisine, D. A new cavitation model based on bubble-bubble interactions. Phys. Fluids 2018, 30, 123301. [Google Scholar] [CrossRef]
- Leighton, T. The Acoustic Bubble, 1st ed.; Academic Press: Cambridge, UK, 1997. [Google Scholar]
- Morton, K.I.; ter Haar, G.R.; Stratford, I.J.; Hill, C.R. Subharmonic emission as an indicator of ultrasonically-induced biological damage. Ultrasound Med. Biol. 1983, 9, 629–633. [Google Scholar] [CrossRef]
- Ngo, D.; Liu, H.; Chen, Z.; Kaya, H.; Zimudzi, T.J.; Gin, S.; Mahadevan, T.; Du, J.; Kim, S.H. Hydrogen bonding interactions of H2O and SiOH on a boroaluminosilicate glass corroded in aqueous solution. NPJ Mater. Degrad. 2020, 4, 1. [Google Scholar] [CrossRef]
- Gongalsky, M.B.; Sviridov, A.P.; Bezsudnova, Y.I.; Osminkina, L.A. Biodegradation model of porous silicon nanoparticles. Colloids Surf. B Biointerfaces 2020, 190, 110946. [Google Scholar] [CrossRef]
- Brujan, E.A. The role of cavitation microjets in the therapeutic applications of ultrasound. Ultrasound Med. Biol. 2004, 30, 381–387. [Google Scholar] [CrossRef]
- Rich, J.; Tian, Z.; Huang, T.J. Sonoporation: Past, present, and future. Adv. Mater. Technol. 2021, 7, 2100885. [Google Scholar] [CrossRef]
- Domenici, F.; Brasili, F.; Giantulli, S.; Cerroni, B.; Bedini, A.; Giliberti, C.; Palomba, R.; Silvestri, I.; Morrone, S.; Paradossi, G.; et al. Differential effects on membrane permeability and viability of human keratinocyte cells undergoing very low intensity megasonic fields. Sci. Rep. 2017, 7, 16536. [Google Scholar] [CrossRef]
- Herino, R.; Bomchil, G.; Barla, K.; Bertrand, C.; Ginoux, J.L. Porosity and pore size distributions of porous silicon layers. J. Electrochem. Soc. 1994, 134, 1994–2000. [Google Scholar] [CrossRef]
- Sviridov, A.P.; Osminkina, L.A.; Nikolaev, A.L.; Kudryavtsev, A.A.; Vasiliev, A.N.; Timoshenko, V.Y. Lowering of the cavitation threshold in aqueous suspensions of porous silicon nanoparticles for sonodynamic therapy applications. Appl. Phys. Lett. 2015, 107, 123107. [Google Scholar] [CrossRef]


| Group | Wavenumber (cm−1) | Vibration Mode |
|---|---|---|
| Si-H | 626 | Wagging |
| Si-H2 | 662 | Rolling |
| Si-H2 | 908 | Scissoring |
| Si-O-Si | 1080 | Assym. stretching |
| Si-O-Si | 1170 | Sym. stretching |
| Si-H2 | 2082 | Stretching |
| Si-H | 2112 | Stretching |
| Si-H3 | 2138 | Stretching |
| SiO-H | 3740, 3700–2700, 1640 | Stretching |
| H2O | 3700–2700, 1620 | Stretching |
| C-H | 2850–2950 | Stretching |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sviridov, A.; Mazina, S.; Ostapenko, A.; Nikolaev, A.; Timoshenko, V. Antibacterial Effect of Acoustic Cavitation Promoted by Mesoporous Silicon Nanoparticles. Int. J. Mol. Sci. 2023, 24, 1065. https://doi.org/10.3390/ijms24021065
Sviridov A, Mazina S, Ostapenko A, Nikolaev A, Timoshenko V. Antibacterial Effect of Acoustic Cavitation Promoted by Mesoporous Silicon Nanoparticles. International Journal of Molecular Sciences. 2023; 24(2):1065. https://doi.org/10.3390/ijms24021065
Chicago/Turabian StyleSviridov, Andrey, Svetlana Mazina, Anna Ostapenko, Alexander Nikolaev, and Victor Timoshenko. 2023. "Antibacterial Effect of Acoustic Cavitation Promoted by Mesoporous Silicon Nanoparticles" International Journal of Molecular Sciences 24, no. 2: 1065. https://doi.org/10.3390/ijms24021065
APA StyleSviridov, A., Mazina, S., Ostapenko, A., Nikolaev, A., & Timoshenko, V. (2023). Antibacterial Effect of Acoustic Cavitation Promoted by Mesoporous Silicon Nanoparticles. International Journal of Molecular Sciences, 24(2), 1065. https://doi.org/10.3390/ijms24021065






