Mediterranean Diet and Oxidative Stress: A Relationship with Pain Perception in Endometriosis
Abstract
:1. Introduction
2. Results
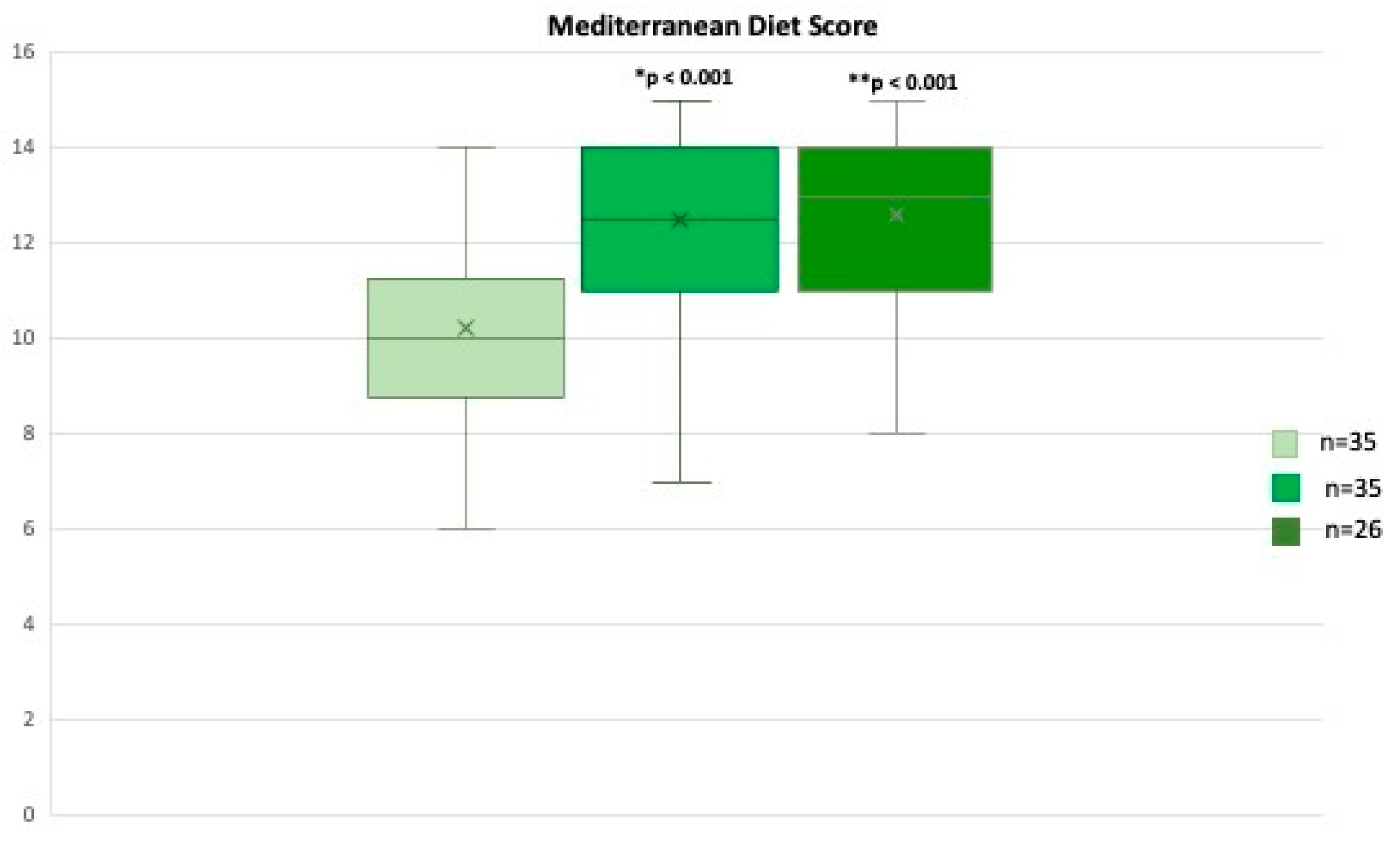
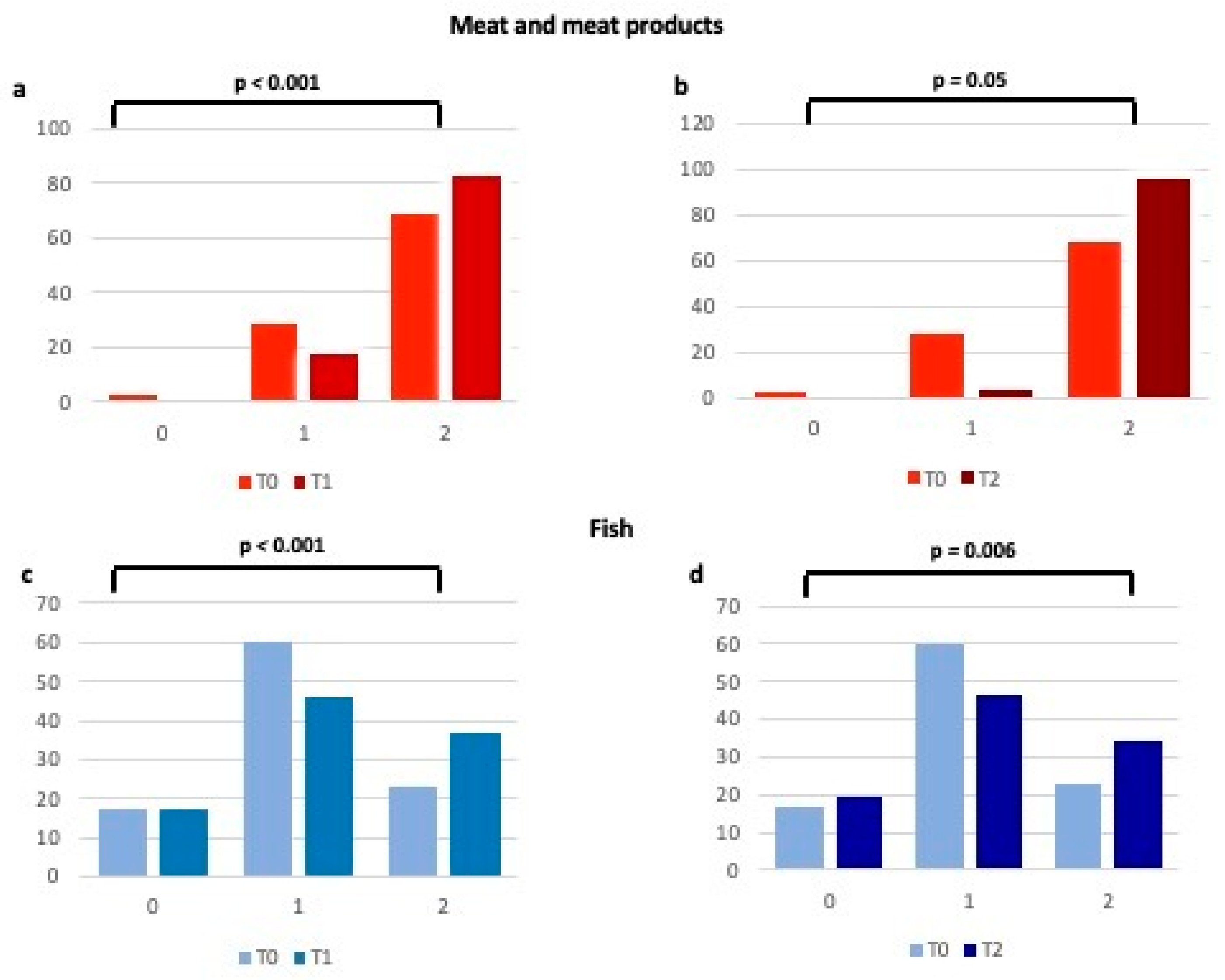
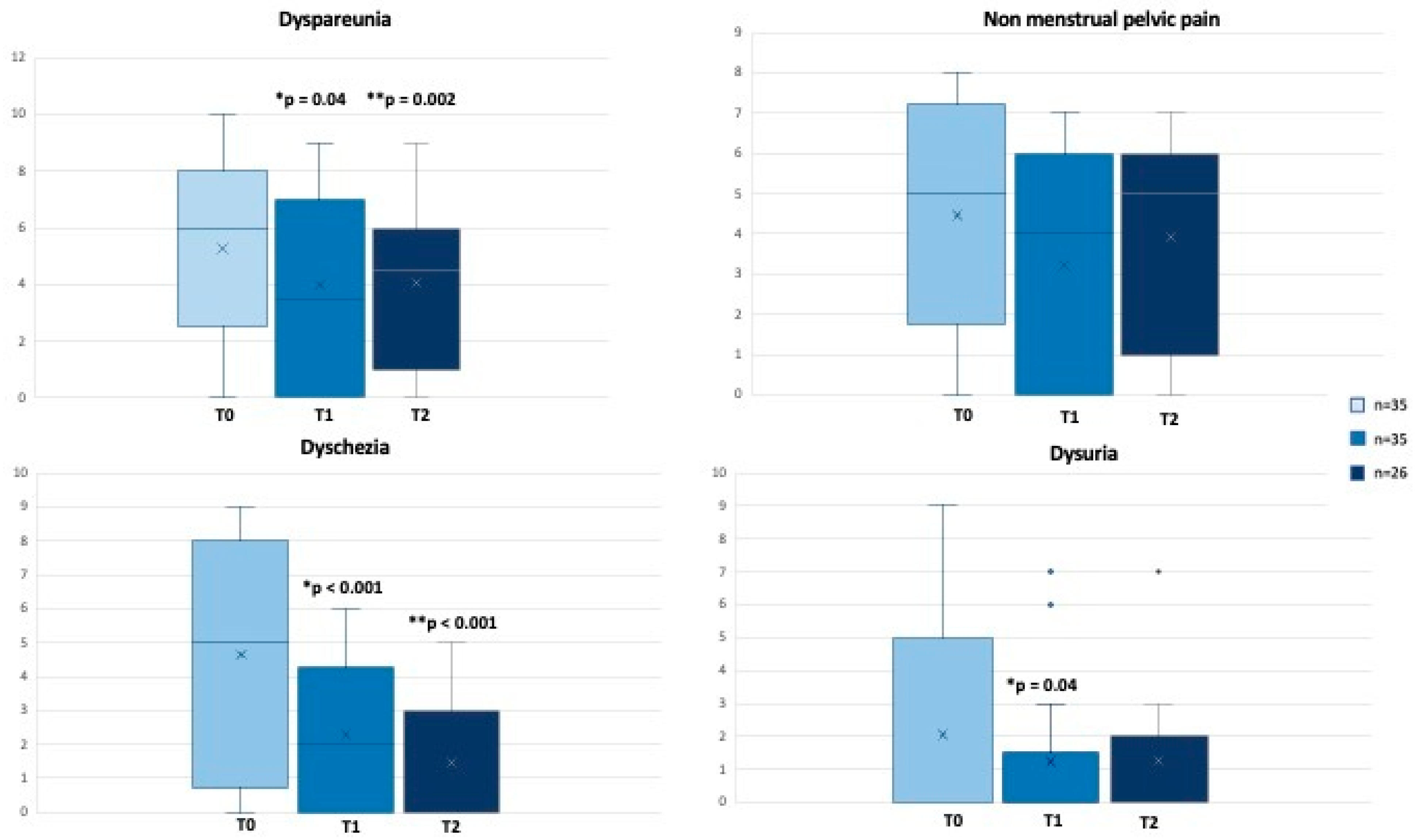
2.1. Mediterranean Diet and Pain Perception
2.2. Oxidative Stress, Mediterranean Diet and Pain Perception
3. Discussion
4. Materials and Methods
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giudice, L.C. Clinical practice. Endometriosis. N. Engl. J. Med. 2010, 362, 2389–2398. [Google Scholar] [CrossRef]
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef]
- Agarwal, S.K.; Chapron, C.; Giudice, L.C.; Laufer, M.R.; Leyland, N.; Missmer, S.A.; Singh, S.S.; Taylor, H.S. Clinical diagnosis of endometriosis: A call to action. Am. J. Obstet. Gynecol. 2019, 220, 354.e1–354.e12. [Google Scholar] [CrossRef]
- As-Sanie, S.; Black, R.; Giudice, L.C.; Valbrun, T.G.; Gupta, J.; Jones, B.; Laufer, M.R.; Milspaw, A.T.; Missmer, S.A.; Norman, A.; et al. Assessing research gaps and unmet needs in endometriosis. Am. J. Obstet. Gynecol. 2019, 221, 86–94. [Google Scholar] [CrossRef]
- Becker, C.M.; Gattrell, W.T.; Gude, K.; Singh, S.S. Reevaluating response and failure of medical treatment of endometriosis: A systematic review. Fertil Steril. 2017, 108, 125–136. [Google Scholar] [CrossRef]
- Sverrisdóttir, U.; Hansen, S.; Rudnicki, M. Impact of diet on pain perception in women with endometriosis: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 271, 245–249. [Google Scholar] [CrossRef]
- World Health Organization. Endometriosis. Key Facts 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/endometriosis (accessed on 20 July 2023).
- Izetbegovic, S.; Alajbegovic, J.; Mutevelic, A.; Pasagic, A.; Masic, I. Prevention of Diseases in Gynecology. Int. J. Prev. Med. 2013, 4, 1347–1358. [Google Scholar]
- Karlsson, J.V.; Patel, H.; Premberg, A. Experiences of health after dietary changes in endometriosis: A qualitative interview study. BMJ Open 2020, 10, e032321. [Google Scholar] [CrossRef]
- Galland, L. Diet and inflammation. Nutr. Clin. Pract. 2010, 25, 634–640. [Google Scholar] [CrossRef]
- Ott, J.; Nouri, K.; Hrebacka, D.; Gutschelhofer, S.; Huber, J.; Wenzl, R. Endometriosis and nutrition-recommending a Mediterranean diet decreases endometriosis-associated pain: An experimental observational study. J. Aging Res. Clin. Pract. 2012, 1, 162. [Google Scholar]
- Nirgianakis, K.; Egger, K.; Kalaitzopoulos, D.R.; Lanz, S.; Bally, L.; Mueller, M.D. Effectiveness of Dietary Interventions in the Treatment of Endometriosis: A Systematic Review. Reprod. Sci. 2022, 29, 26–42. [Google Scholar] [CrossRef] [PubMed]
- Cirillo, M.; Argento, F.R.; Attanasio, M.; Becatti, M.; Ladisa, I.; Fiorillo, C.; Coccia, M.E.; Fatini, C. Atherosclerosis and Endometriosis: The Role of Diet and Oxidative Stress in a Gender-Specific Disorder. Biomedicines 2023, 11, 450. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2013, 17, 2769–2782. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Marcucci, R.; Casini, A. Validation of a literature-based adherence score to Mediterranean diet: The MEDI-LITE score. Int. J. Food Sci. Nutr. 2017, 68, 757–762. [Google Scholar] [CrossRef] [PubMed]
- Fjerbaek, A.; Knudsen, U.B. Endometriosis, dysmenorrhea, and diet—What is the evidence? Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 132, 140–147. [Google Scholar] [CrossRef]
- Pagliai, G.; Russo, E.; Niccolai, E.; Dinu, M.; Di Pilato, V.; Magrini, A.; Bartolucci, G.; Baldi, S.; Menicatti, M.; Giusti, B.; et al. Influence of a 3-month low-calorie Mediterranean diet compared to the vegetarian diet on human gut microbiota and SCFA: The CARDIVEG Study. Eur. J. Nutr. 2020, 59, 2011–2024. [Google Scholar] [CrossRef]
- Santanam, N.; Kavtaradze, N.; Murphy, A.; Dominguez, C.; Parthasarathy, S. Antioxidant supplementation reduces endometriosis-related pelvic pain in humans. Transl. Res. 2013, 161, 189–195. [Google Scholar] [CrossRef]
- Parazzini, F.; Viganò, P.; Candiani, M.; Fedele, L. Diet, and endometriosis risk: A literature review. Reprod. Biomed. Online 2013, 26, 323–336. [Google Scholar] [CrossRef]
- Saguyod, S.J.U.; Kelley, A.S.; Velarde, M.C.; Simmen, R.C. Diet and endometriosis-revisiting the linkages to inflammation. J. Endometr. Pelvic. Pain Disord. 2018, 10, 51–58. [Google Scholar] [CrossRef]
- Harris, H.R.; Chavarro, J.E.; Malspeis, S.; Willett, W.C.; Missmer, S.A. Dairy-Food, calcium, magnesium, and Vitamin D intake and endometriosis: A prospective cohort study. Am. J. Epidemiol. 2013, 177, 420–430. [Google Scholar] [CrossRef]
- Sesti, F.; Capozzolo, T.; Pietropolli, A.; Collalti, M.; Bollea, M.R.; Piccione, E. Dietary therapy: A new strategy for management of chronic pelvic pain. Nutr. Res. Rev. 2011, 24, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, A.; Harris, H.R.; Vitonis, A.F.; Chavarro, J.E.; Missmer, S.A. A prospective cohort study of meat and fish consumption and endometriosis risk. Am. J. Obstet. Gynecol. 2018, 219, e1–e178. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Scialli, A.R.; Hurlock, D.; Bertron, P. Diet and sex-hormone binding globulin, dysmenorrhea, and premenstrual symptoms. Obstet. Gynecol. 2000, 95, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, M.T.; Baglietto, L.; Krishnan, K.; English, D.R.; Severi, G.; Morris, H.A.; Hopper, J.L.; Giles, G.G. Consumption of animal products, their nutrient components and postmenopausal circulating steroid hormone concentrations. Eur. J. Clin. Nutr. 2010, 64, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.D.; Dizdaroglu, M.; Cooke, M.S. Oxidative DNA damage and disease: Induction, repair and significance. Mutat. Res. Mol. Mech. Mutagen. 2004, 567, 1–61. [Google Scholar] [CrossRef] [PubMed]
- Huijs, E.; Nap, A. The effects of nutrients on symptoms in women with endometriosis: A systematic review. Reprod. Biomed. Online 2020, 41, 317–328. [Google Scholar] [CrossRef]
- Parazzini, F.; Chiaffarino, F.; Surace, M.; Chatenoud, L.; Cipriani, S.; Chiantera, V.; Benzi, G.; Fedele, L. Selected food intake and risk of endometriosis. Hum. Reprod. 2004, 19, 1755–1759. [Google Scholar] [CrossRef]
- Joshi, R.; Adhikari, S.; Patro, B.S.; Chattopadhyay, S.; Mukherjee, T. Free radical scavenging behavior of folic acid: Evidence for possible antioxidant activity. Free Radic. Biol. Med. 2001, 30, 1390–1399. [Google Scholar] [CrossRef]
- O’Connor, J.M. Trace elements and DNA damage. Biochem. Soc. Trans. 2001, 29, 354–357. [Google Scholar] [CrossRef]
- Mehdizadehkashi, A.; Rokhgireh, S.; Tahermanesh, K.; Eslahi, N.; Minaeian, S.; Samimi, M. The effect of vitamin D supplementation on clinical symptoms and metabolic profiles in patients with endometriosis. Gynecol. Endocrinol. 2021, 37 Pt 2, 640–645. [Google Scholar] [CrossRef]


| Variables at T0 (n = 35) | VAS Dyspareunia | VAS Non-Menstrual Pelvic Pain | VAS Dyschezia | VAS Dysuria |
|---|---|---|---|---|
| Lipid peroxidation | - | rho = 0.369 p = 0.029 | - | rho = 0.416 p = 0.013 |
| ORAC | - | rho = −0.394 p = 0.019 | rho = −0.515 p = 0.002 | - |
| M-derived ROS | - | - | - | rho = 0.589 p < 0.001 |
| N-derived ROS | - | - | - | rho = 0.607 p < 0.001 |
| L-derived ROS | - | - | - | rho = 0.534 p = 0.001 |
| Variables | T0 | T1 | T2 | p (T0 vs. T1) | p (T0 vs. T2) |
|---|---|---|---|---|---|
| (n = 35) | (n = 35) | (n = 26) | |||
| Folate, ng/mL | 5.6 (1–14.4) | 7.2 (3.9–20) | 7.1 (3.7–19.8) | 0.01 | 0.006 |
| Vitamin B12, pg/mL | 310 (99–709) | 366 (123–760) | 336 (199–749) | 0.1 | 0.3 |
| Vitamin E, µg/dL | 1285 (720–2612) | 1322.5 (889–2828) | 1415.5 (952–2615) | 0.1 | 0.1 |
| Zinc, µg/dL | 114 (76–193) | 125 (89–233) | 120 (95–186) | 0.1 | 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cirillo, M.; Argento, F.R.; Becatti, M.; Fiorillo, C.; Coccia, M.E.; Fatini, C. Mediterranean Diet and Oxidative Stress: A Relationship with Pain Perception in Endometriosis. Int. J. Mol. Sci. 2023, 24, 14601. https://doi.org/10.3390/ijms241914601
Cirillo M, Argento FR, Becatti M, Fiorillo C, Coccia ME, Fatini C. Mediterranean Diet and Oxidative Stress: A Relationship with Pain Perception in Endometriosis. International Journal of Molecular Sciences. 2023; 24(19):14601. https://doi.org/10.3390/ijms241914601
Chicago/Turabian StyleCirillo, Michela, Flavia Rita Argento, Matteo Becatti, Claudia Fiorillo, Maria Elisabetta Coccia, and Cinzia Fatini. 2023. "Mediterranean Diet and Oxidative Stress: A Relationship with Pain Perception in Endometriosis" International Journal of Molecular Sciences 24, no. 19: 14601. https://doi.org/10.3390/ijms241914601
APA StyleCirillo, M., Argento, F. R., Becatti, M., Fiorillo, C., Coccia, M. E., & Fatini, C. (2023). Mediterranean Diet and Oxidative Stress: A Relationship with Pain Perception in Endometriosis. International Journal of Molecular Sciences, 24(19), 14601. https://doi.org/10.3390/ijms241914601








