Effect of the Cannabinoid Agonist WIN 55,212-2 on Neuropathic and Visceral Pain Induced by a Non-Diarrheagenic Dose of the Antitumoral Drug 5-Fluorouracil in the Rat
Abstract
1. Introduction
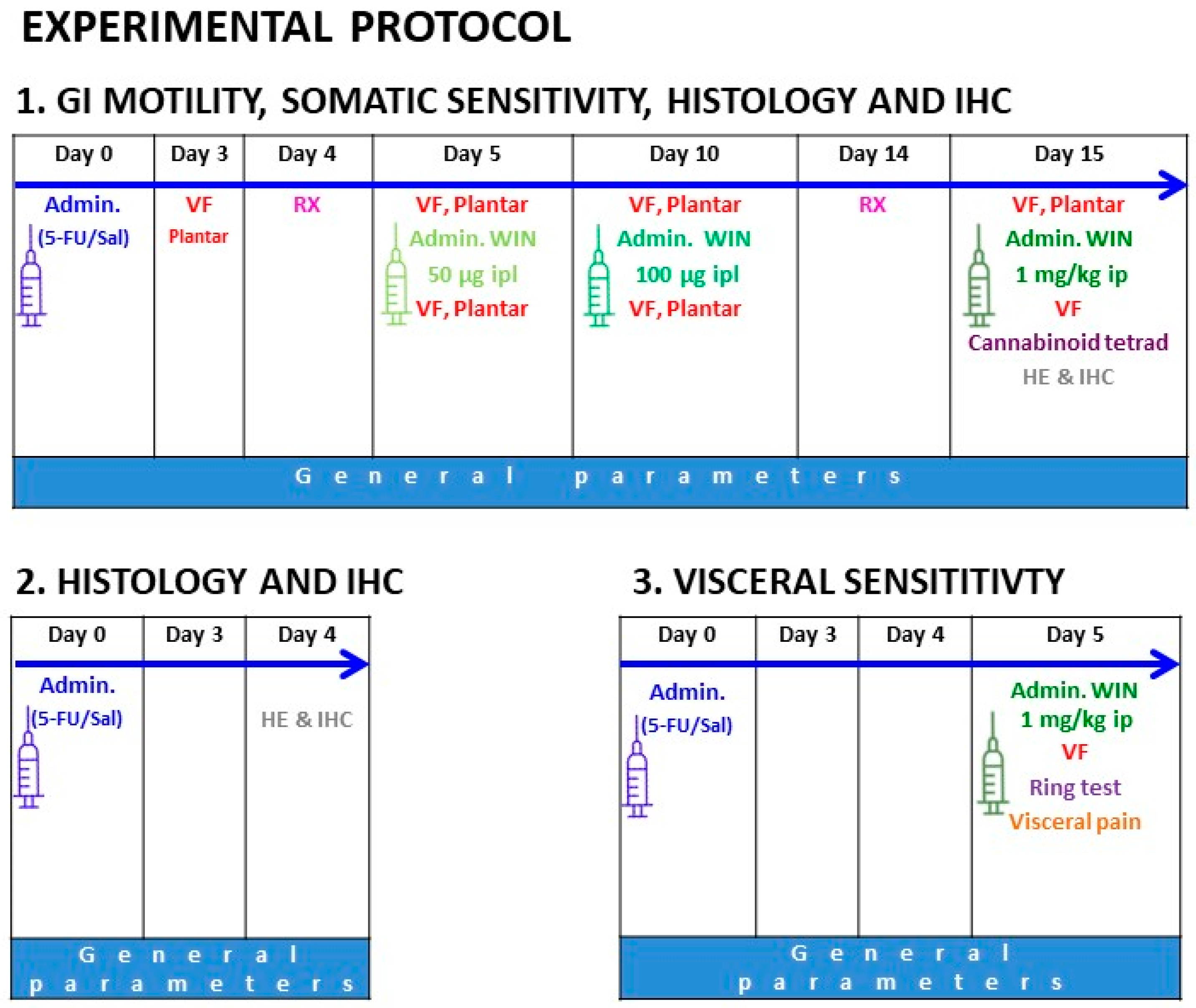
- To characterize in the rat the effects of a relatively low dose of 5-FU on body weight, food and water intakes, gastrointestinal motor function, tactile mechanical and thermal sensitivity, colonic mechanical sensitivity, and the general structure of the gut (ileum, colon) wall;
- To evaluate the effects of WIN on the somatic and visceral nociceptive thresholds altered in the rat by 5-FU. In addition, the possible central effects of WIN, which could be seen as a drawback of cannabinoid treatment, were analyzed.
2. Results
2.1. General Health Parameters
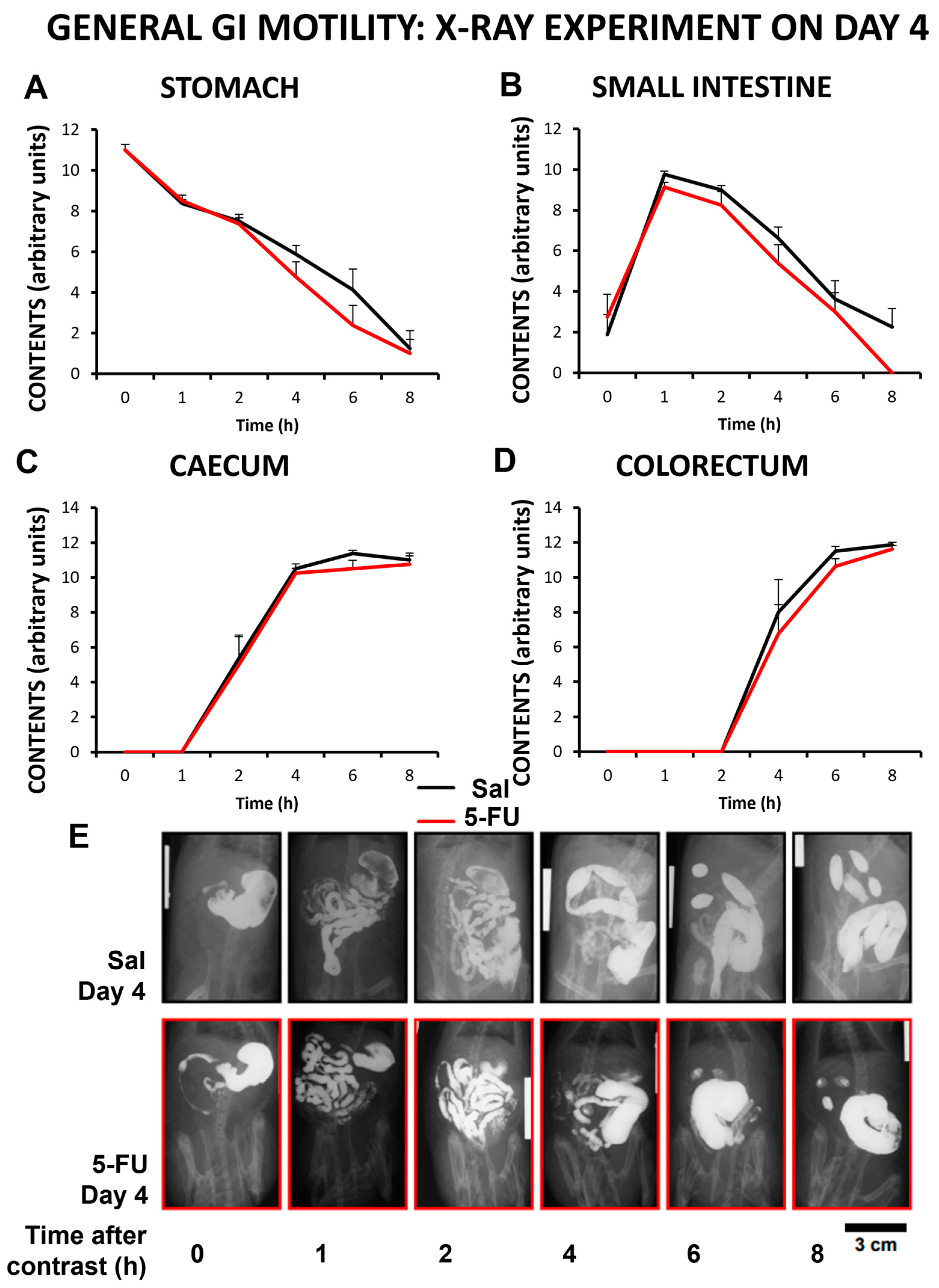
2.2. Gastrointestinal Motor Activity
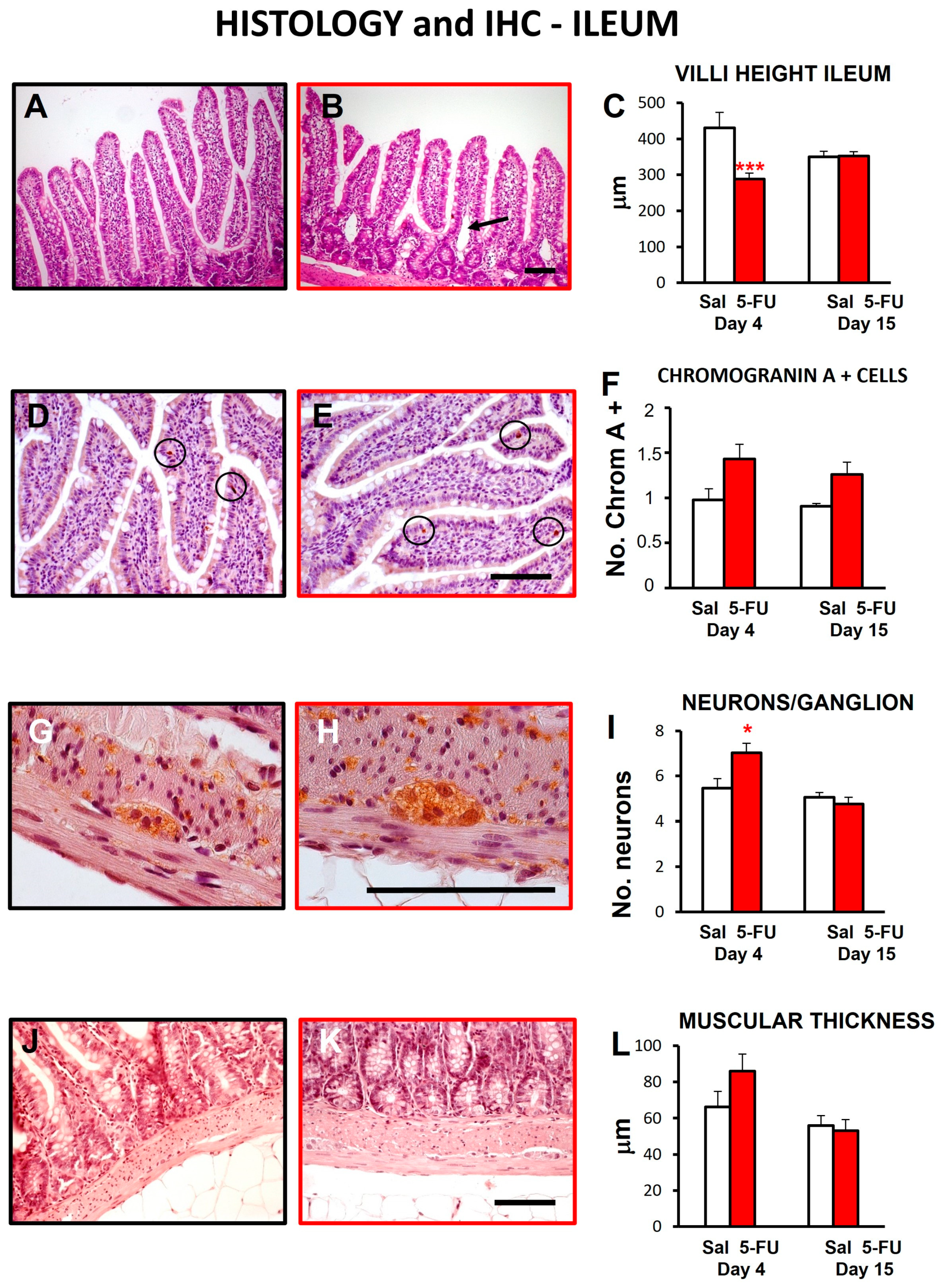
2.3. Gut Wall Histology
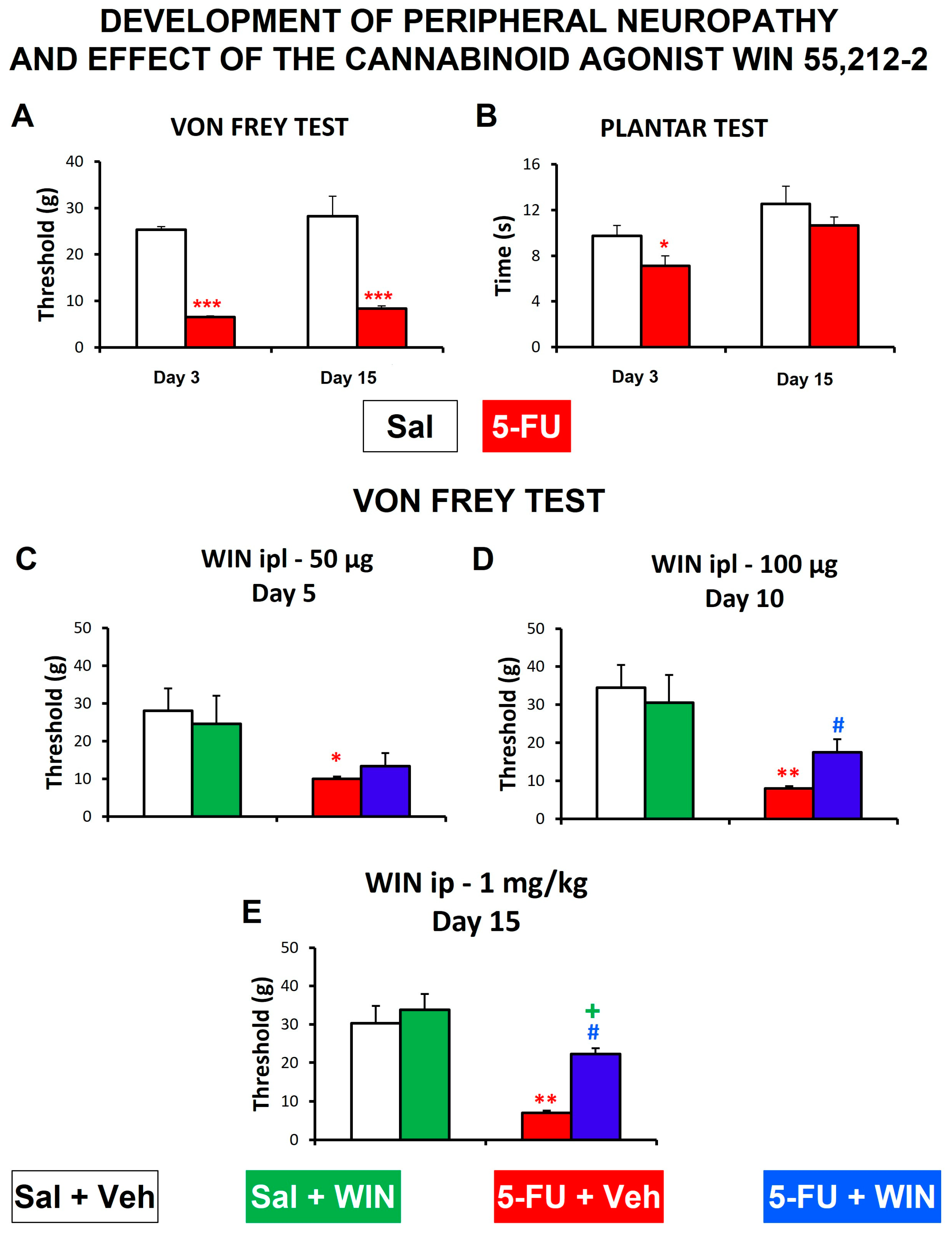
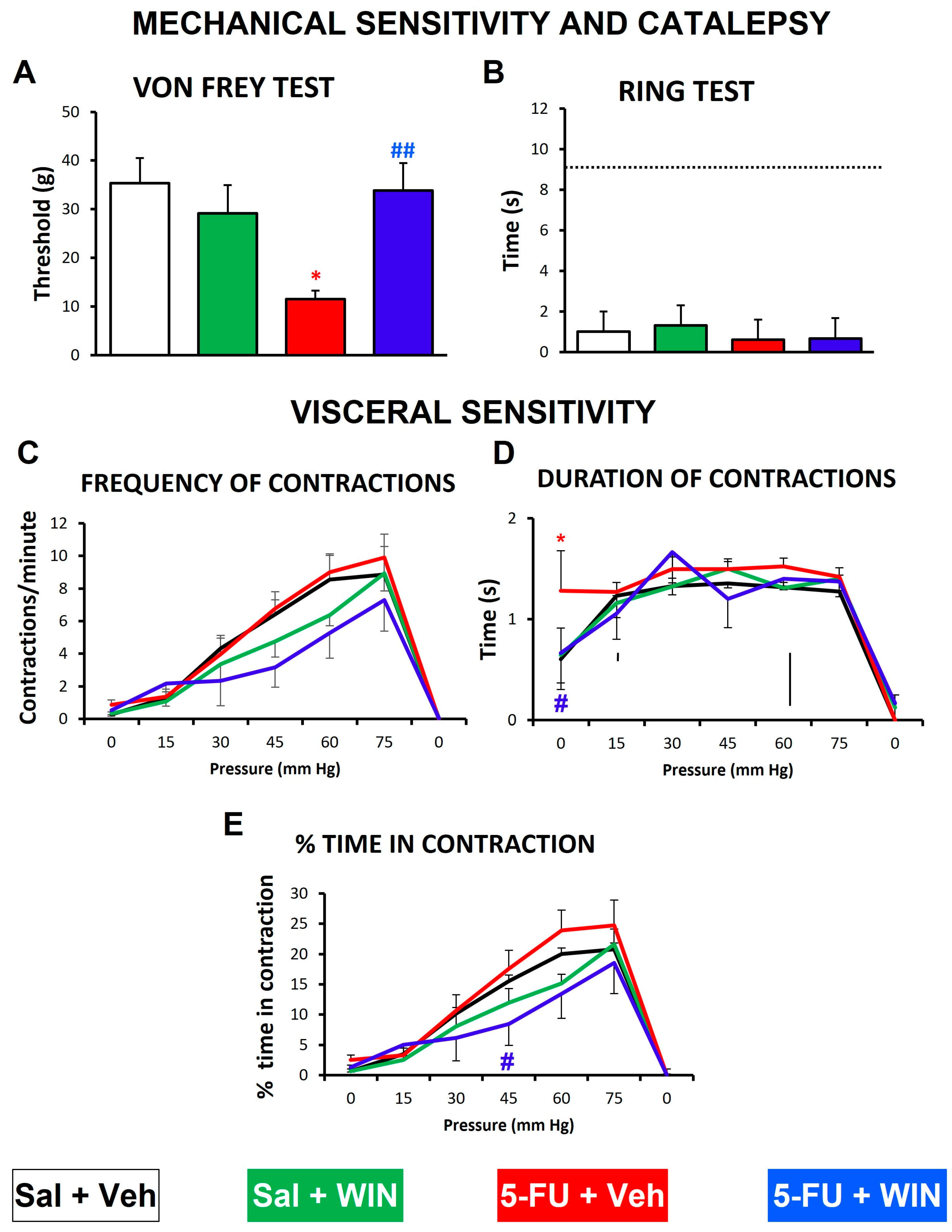
2.4. Development of Peripheral Neuropathy and Effect of WIN
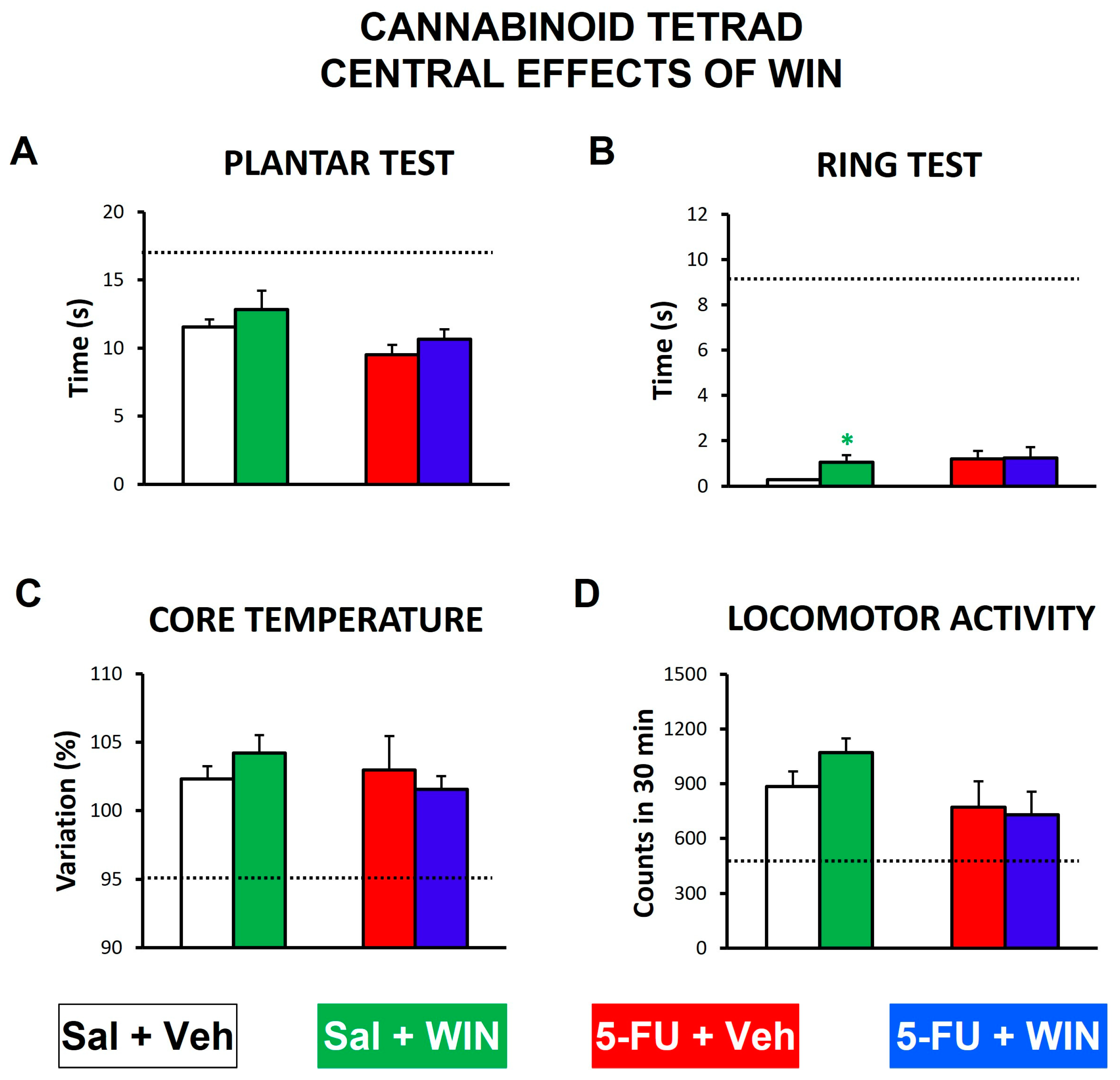
2.5. Cannabinoid Tetrad
2.6. Visceral Sensitivity
3. Discussion
4. Materials and Methods
4.1. Animals and Treatments
4.2. General Health Parameters
4.3. Gastrointestinal Motility Experiments
4.4. Histopathological Analysis of Gastrointestinal Regions
4.5. Assessment of Somatic Nociceptive Thresholds
4.6. Effect of WIN 55,212-2 on Tactile Sensitivity
4.7. Cannabinoid Tetrad
4.8. Assessment of Visceral Sensitivity
4.9. Effect of WIN 55,212-2 on Visceral Sensitivity
4.10. Compounds and Drugs
4.11. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, N.; Yin, Y.; Xu, S.J.; Chen, W.S. 5-Fluorouracil: Mechanisms of resistance and reversal strategies. Molecules 2008, 13, 1551–1569. [Google Scholar] [CrossRef] [PubMed]
- Mafi, A.; Rezaee, M.; Hedayati, N.; Hogan, S.D.; Reiter, R.J.; Aarabi, M.H.; Asemi, Z.A. Melatonin and 5-fluorouracil combination chemotherapy: Opportunities and efficacy in cancer therapy. Cell Commun. Signal. 2023, 21, 33. [Google Scholar] [CrossRef] [PubMed]
- Christensen, S.; Van der Roest, B.; Besselink, N.; Janssen, R.; Boymans, S.; Martens, J.W.M.; Yaspo, M.L.; Priestley, P.; Kuijk, E.; Cuppen, E.; et al. 5-Fluorouracil treatment induces characteristic T>G mutations in human cancer. Nat. Commun. 2019, 10, 4571. [Google Scholar] [CrossRef] [PubMed]
- Spencer, N.J. Motility patterns in mouse colon: Gastrointestinal dysfunction induced by anticancer chemotherapy. Neurogastroenterol. Motil. 2016, 28, 1759–1764. [Google Scholar] [CrossRef]
- Korver, S.K.; Bowen, J.M.; Gibson, R.J.; Ball, I.A.; Secombe, K.R.; Wain, T.J.; Logan, R.M.; Tuke, J.; Mead, K.R.; Richards, A.M.; et al. Advanced statistics identification of participant and treatment predictors associated with severe adverse effects induced by fluoropyrimidine-based chemotherapy. Cancer Chemother. Pharmacol. 2023, 91, 507–521. [Google Scholar] [CrossRef]
- Schneider, E.C.; Malin, J.L.; Kahn, K.L.; Ko, C.Y.; Adams, J.; Epstein, A.M. Surviving colorectal cancer: Patient-reported symptoms 4 years after diagnosis. Cancer 2007, 110, 2075–2082. [Google Scholar] [CrossRef]
- Denlinger, C.S.; Barsevick, A.M. The challenges of colorectal cancer survivorship. J. Natl. Compr. Canc. Netw. 2009, 7, 883–894. [Google Scholar] [CrossRef]
- Soares, P.M.; Mota, J.M.; Souza, E.P.; Justino, P.F.; Franco, A.X.; Cunha, F.Q.; Ribeiro, R.A.; Souza, M.H. Inflammatory intestinal damage induced by 5-fluorouracil requires IL-4. Cytokine 2013, 61, 46–49. [Google Scholar] [CrossRef]
- Duncan, M.; Grant, G. Oral and intestinal mucositis–Causes and possible treatments. Aliment. Pharmacol. Ther. 2003, 18, 853–874. [Google Scholar] [CrossRef]
- Sougiannis, A.T.M.; VanderVeen, B.N.; Davis, J.M.; Fan, D.; Murphy, E.A. Understanding chemotherapy-induced intestinal mucositis and strategies to improve gut resilience. Am. J. Physiol. Gastrointest. Liver Physiol. 2021, 320, G712–G719. [Google Scholar] [CrossRef]
- Keefe, D.M.; Brealey, J.; Goland, G.J.; Cummins, A.G. Chemotherapy for cancer causes apoptosis that precedes hypoplasia in crypts of the small intestine in humans. Gut 2000, 47, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.M.; Mota, J.M.; Gomes, A.S.; Oliveira, R.B.; Assreuy, A.M.; Brito, G.A.; Santos, A.A.; Ribeiro, R.A.; Souza, M.H. Gastrointestinal dysmotility in 5-fluorouracil-induced intestinal mucositis outlasts inflammatory process resolution. Cancer Chemother. Pharmacol. 2008, 63, 91–98. [Google Scholar] [CrossRef] [PubMed]
- McQuade, R.M.; Stojanovska, V.; Donald, E.; Abalo, R.; Bornstein, J.C.; Nurgali, K. Gastrointestinal dysfunction and enteric neurotoxicity following treatment with anticancer chemotherapeutic agent 5-fluorouracil. Neurogastroenterol. Motil. 2016, 28, 1861–1875. [Google Scholar] [CrossRef] [PubMed]
- Carozzi, V.A.; Canta, A.; Chirazzi, A. Chemotherapy-induced periphetal neuropathy: What do we know about mechanisms? Neurosci. Lett. 2015, 596, 90–107. [Google Scholar] [CrossRef]
- Ibrahim, E.Y.; Ehrlich, B.E. Prevention of chemotherapy-induced peripheral neuropathy: A review of recent findings. Crit. Rev. Oncol. Hematol. 2020, 145, 102831. [Google Scholar] [CrossRef]
- Ruskh, L.; Ali, G.; Ullah, R.; Islam, N.U.; Shahid, M. Efficacy assessment of salicylidene salicylhydrazide in chemotherapy associated peripheral neuropathy. Eur. J. Pharmacol. 2020, 888, 173481. [Google Scholar] [CrossRef]
- Saif, M.W.; Wood, T.E.; McGee, P.J.; Diasio, R.B. Peripheral neuropathy associated with capecitabine. Anticancer. Drugs. 2004, 15, 767–771. [Google Scholar] [CrossRef]
- Werbrouck, B.F.; Pauwels, W.J.; De Bleecker, J.L. A case of 5-fluorouracil-induced peripheral neuropathy. Clin. Toxicol. 2008, 46, 264–266. [Google Scholar] [CrossRef][Green Version]
- Bielefeldt, K.; Christianson, J.A.; Davis, B.M. Basic and clinical aspects of visceral sensation: Transmission in the CNS. Neurogastroenterol. Motil. 2005, 7, 488–499. [Google Scholar] [CrossRef]
- Sikandar, S.; Dickenson, A.H. Visceral pain: The ins and outs, the ups and downs. Curr. Opin. Support. Palliat. Care 2012, 6, 17–26. [Google Scholar] [CrossRef]
- Martín-Ruíz, M.; Uranga, J.A.; Mosinska, P.; Fichna, J.; Nurgali, K.; Martín-Fontelles, M.I.; Abalo, R. Alterations of colonic sensitivity and gastric dysmotility after acute cisplatin and granisetron. Neurogastroenterol. Motil. 2019, 31, e13499. [Google Scholar] [CrossRef] [PubMed]
- Rossato, M.F.; Rigo, F.K.; Oliveira, S.M.; Guerra, G.P.; Silva, C.R.; Cunha, T.M.; Gomez, M.V.; Ferreira, J.; Trevisan, G. Participation of transient receptor potential vanilloid 1 in paclitaxel-induced acute visceral and peripheral nociception in rodents. Eur. J. Pharmacol. 2018, 828, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Cinausero, M.; Aprile, G.; Ermacora, P.; Basile, D.; Vitale, M.G.; Fanotto, V.; Parisi, G.; Calvetti, L.; Sonis, S.T. New Frontiers in the Pathobiology and Treatment of Cancer Regimen-Related Mucosal Injury. Front. Pharmacol. 2017, 8, 354. [Google Scholar] [CrossRef] [PubMed]
- George, R.P.; Howarth, G.S.; Whittaker, A.L. Use of the Rat Grimace Scale to Evaluate Visceral Pain in a Model of Chemotherapy-Induced Mucositis. Animals 2019, 9, 678. [Google Scholar] [CrossRef] [PubMed]
- Vera, G.; Castillo, M.; Cabezos, P.A.; Chiarlone, A.; Martín, M.I.; Gori, A.; Pasquinelli, G.; Barbara, G.; Stanghellini, V.; Corinaldesi, R.; et al. Enteric neuropathy evoked by repeated cisplatin in the rat. Neurogastroenterol. Motil. 2011, 23, 370.e163. [Google Scholar] [CrossRef]
- Wafai, L.; Taher, M.; Jovanovska, V.; Bornstein, J.C.; Dass, C.R.; Nurgali, K. Effects of oxaliplatin on mouse myenteric neurons and colonic motility. Front. Neurosci. 2013, 7, 30. [Google Scholar] [CrossRef]
- Guzmán, M. Cannabinoids: Potential anticancer agents. Nat. Rev. Cancer 2003, 3, 745–755. [Google Scholar] [CrossRef]
- Abrams, D.I. Integrating cannabis into clinical cancer care. Curr. Oncol. 2016, 23, S8–S14. [Google Scholar] [CrossRef]
- Dariš, B.; Tancer Verboten, M.; Knez, Ž.; Ferk, P. Cannabinoids in cancer treatment: Therapeutic potential and legislation. Bosn. J. Basic Med. Sci. 2019, 19, 14–23. [Google Scholar] [CrossRef]
- Abalo, R.; Uranga, J.A.; Pérez-García, I.; de Andrés, R.; Girón, R.; Vera, G.; López-Pérez, A.E.; Martín-Fontelles, M.I. May cannabinoids prevent the development of chemotherapy-induced diarrhea and intestinal mucositis? Experimental study in the rat. Neurogastroenterol. Motil. 2017, 29, 12952. [Google Scholar] [CrossRef]
- Pascual, D.; Goicoechea, C.; Suardíaz, M.; Martín, M.I. A cannabinoid agonist, WIN 55,212-2, reduces neuropathic nociception induced by paclitaxel in rats. Pain 2005, 118, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Vera, G.; Cabezos, P.A.; Martín, M.I.; Abalo, R. Characterization of cannabinoid-induced relief of neuropathic pain in a rat model of cisplatin-induced neuropathy. Pharmacol. Biochem. Behav. 2013, 105, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Rahn, E.J.; Makriyannis, A.; Hohmann, A.G. Activation of cannabinoid CB1 and CB2 receptors suppresses neuropathic nociception evoked by the chemotherapeutic agent vincristine in rats. Br. J. Pharmacol. 2007, 152, 765–777. [Google Scholar] [CrossRef] [PubMed]
- King, K.M.; Myers, A.M.; Soroka-Monzo, A.J.; Tuma, R.F.; Tallarida, R.J.; Walker, E.A.; Ward, S.J. Single and combined effects of Δ9-tetrahydrocannabinol and cannabidiol in a mouse model of chemotherapy-induced neuropathic pain. Br. J. Pharmacol. 2017, 174, 2832–2841. [Google Scholar] [CrossRef] [PubMed]
- Çengelli Ünel, Ç.; Ayaz, B.; Aydın, Ş.; Ulupınar, E.; Özatik, O.; Kaygısız, B.; Yıldırım, E.; Erol, K. Protective effects of anandamide against cisplatin-induced peripheral neuropathy in rats. Turk. J. Med. Sci. 2021, 51, 3098–3107. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Guindon, J.; Vemuri, V.K.; Thakur, G.A.; White, F.A.; Makriyannis, A.; Hohmann, A.G. The maintenance of cisplatin- and paclitaxel-induced mechanical and cold allodynia is suppressed by cannabinoid CB2 receptor activation and independent of CXCR4 signaling in models of chemotherapy-induced peripheral neuropathy. Mol. Pain 2012, 8, 71. [Google Scholar] [CrossRef]
- Pereira, A.F.; Lisboa MR, P.; de Freitas Alves, B.W.; da Silva CM, P.; Dias DB, S.; de Menezes KL, S.; Cesário FR, A.S.; de França, J.C.; de Oliveira, A.R.; Hallak JE, C.; et al. Endocannabinoid System Attenuates Oxaliplatin-Induced Peripheral Sensory Neuropathy Through the Activation of CB1 Receptors. Neurotox. Res. 2021, 39, 1782–1799. [Google Scholar] [CrossRef]
- Torres, D.M.; Tooley, K.L.; Butler, R.N.; Smith, C.L.; Geier, M.S.; Howa, S. Lyprinol only partially improves indicators of small intestinal integrity in a rat model of 5-fluorouracil-induced mucositis. Cancer Biol. Ther. 2008, 7, 295–302. [Google Scholar] [CrossRef]
- Yazbeck, R.; Lindsay, R.J.; Geier, M.S.; Butler, R.N.; Howarth, G.S. Prebiotics Fructo-, Galacto-, and Mannan-Oligosaccharide Do Not Protect against 5-Fluorouracil-Induced Intestinal Mucositis in Rats. J. Nutr. 2019, 149, 2164–2173. [Google Scholar] [CrossRef]
- Yazbeck, R.; Howarth, G.S.; Borges, L.; Geier, M.S.; Smith, C.L.; Davidson, G.P.; Butler, R.N. Non-invasive detection of a palifermin-mediated adaptive response following chemotherapy-induced damage to the distal small intestine of rats. Cancer Biol. Ther. 2011, 12, 399–406. [Google Scholar] [CrossRef][Green Version]
- Kamar, S.S.; Baky, M.H.; Omar, A.I. The beneficial influence of rhubarb on 5-fluorouracil-induced ileal mucositis and the combined role of aquaporin-4, tumour necrosis factor-α, nuclear factor-kappa B & matrix metalloproteinase-9 in rat model: Histological study. Anat. Cell Biol. 2020, 53, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Cool, J.C.; Dyer, J.L.; Xian, C.J.; Butler, R.N.; Geier, M.S.; Howarth, G.S. Pre-treatment with insulin-like growth factor-I partially ameliorates 5-fluorouracil-induced intestinal mucositis in rats. Growth Horm. IGF Res. 2005, 15, 72–82. [Google Scholar] [CrossRef]
- Oh, N.S.; Lee, J.Y.; Lee, J.M.; Lee, K.W.; Kim, Y. Mulberry leaf extract fermented with Lactobacillus acidophilus A4 ameliorates 5-fluorouracil-induced intestinal mucositis in rats. Lett. Appl. Microbiol. 2017, 64, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Keefe, D.M.; Gibson, R.J. The combination of oral and small intestinal mucositis, pediatrics and biomarkers: A particularly tricky problem! Cancer Biol. Ther. 2006, 5, 1282–1284. [Google Scholar] [CrossRef]
- Mikawa, S.; Kondo, M.; Kaji, N.; Mihara, T.; Yoshitake, R.; Nakagawa, T.; Takamoto, M.; Nishimura, R.; Shimada, S.; Ozaki, H.; et al. Serotonin 3 receptor signaling regulates 5-fluorouracil-mediated apoptosis indirectly via TNF-α production by enhancing serotonin release from enterochromaffin cells. FASEB J. 2019, 33, 1669–1680. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, M.; Kato, S.; Yamanaka, N.; Iimori, M.; Matsumoto, K.; Utsumi, D.; Kitahara, Y.; Amagase, K.; Horie, S.; Takeuchi, K. 5-HT3 receptor antagonists ameliorate 5-fluorouracil-induced intestinal mucositis by suppression of apoptosis in murine intestinal crypt cells. Br. J. Pharmacol. 2013, 168, 1388–1400. [Google Scholar] [CrossRef]
- Cubeddu, L.X.; O’Connor, D.T.; Parmer, R.J. Plasma chromogranin A: A marker of serotonin release and of emesis associated with cisplatin chemotherapy. J. Clin. Oncol. 1995, 13, 681–687. [Google Scholar] [CrossRef]
- Cetin, Y. Secretin-cells of the mammalian intestine contain serotonin. Histochemistry 1990, 93, 601–606. [Google Scholar] [CrossRef]
- Starobova, H.; Vetter, I. Pathophysiology of Chemotherapy-Induced Peripheral Neuropathy. Front. Mol. Neurosci. 2017, 10, 174. [Google Scholar] [CrossRef]
- Kerckhove, N.; Collin, A.; Condé, S.; Chaleteix, C.; Pezet, D.; Balayssac, D. Long-Term Effects, Pathophysiological Mechanisms, and Risk Factors of Chemotherapy-Induced Peripheral Neuropathies: A Comprehensive Literature Review. Front. Pharmacol. 2017, 8, 86. [Google Scholar] [CrossRef]
- Authier, N.; Gillet, J.P.; Fialip, J.; Eschalier, A.; Coudore, F. An animal model of nociceptive peripheral neuropathy following repeated cisplatin injections. Exp. Neurol. 2003, 182, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Ling, B.; Authier, N.; Balayssac, D.; Eschalier, A.; Coudore, F. Behavioral and pharmacological description of oxaliplatin-induced painful neuropathy in rat. Pain 2007, 128, 225–234. [Google Scholar] [CrossRef] [PubMed]
- López-Gómez, L.; Díaz-Ruano, S.; Girón, R.; López-Pérez, A.E.; Vera, G.; Herradón Pliego, E.; López-Miranda, V.; Nurgali, K.; Martín-Fontelles, M.I.; Uranga, J.A.; et al. Preclinical evaluation of the effects on the gastrointestinal tract of the antineoplastic drug vincristine repeatedly administered to rats. Neurogastroenterol. Motil. 2018, 30, e13399. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Ono, K.; Hitomi, S.; Ito, M.; Nodai, T.; Goto, T.; Harano, N.; Watanabe, S.; Inoue, H.; Miyano, K.; et al. Distinct TRPV1- and TRPA1-based mechanisms underlying enhancement of oral ulcerative mucositis-induced pain by 5-fluorouracil. Pain 2016, 157, 1004–1020. [Google Scholar] [CrossRef]
- Feng, C.C.; Yan, X.J.; Chen, X.; Wang, E.M.; Liu, Q.; Zhang, L.Y.; Chen, J.; Fang, J.Y.; Chen, S.L. Vagal anandamide signaling via cannabinoid receptor 1 contributes to luminal 5-HT modulation of visceral nociception in rats. Pain 2014, 155, 1591–1604. [Google Scholar] [CrossRef]
- McQuade, R.M.; Al Thaalibi, M.; Nurgali, K. Impact of chemotherapy-induced enteric nervous system toxicity on gastrointestinal mucositis. Curr. Opin. Support. Palliat. Care 2020, 14, 293–300. [Google Scholar] [CrossRef]
- Bujalska, M. Effect of cannabinoid receptor agonists on streptozotocin-induced hyperalgesia in diabetic neuropathy. Pharmacology 2008, 82, 193–200. [Google Scholar] [CrossRef]
- Galeazzi, F.; Blennerhassett, P.A.; Qiu, B.; O’Byrne, P.M.; Collins, S.M. Cigarette smoke aggravates experimental colitis in rats. Gastroenterology 1999, 117, 877–883. [Google Scholar] [CrossRef]
- Saccani, F.; Anselmi, L.; Jaramillo, I.; Bertoni, S.; Barocelli, E.; Sternini, C. Protective role of μ opioid receptor activation in intestinal inflammation induced by mesenteric ischemia/reperfusion in mice. J. Neurosci. Res. 2012, 90, 2146–2153. [Google Scholar] [CrossRef]
- Compton, D.R.; Rice, K.C.; De Costa, B.R.; Razdan, R.K.; Melvin, L.S.; Johnson, M.R.; Martin, B.R. Cannabinoid structure-activity relationships: Correlation of receptor binding and in vivo activities. J. Pharmacol. Exp. Ther. 1993, 265, 218–226. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vera, G.; López-Gómez, L.; Girón, R.; Martín-Fontelles, M.I.; Nurgali, K.; Abalo, R.; Uranga, J.A. Effect of the Cannabinoid Agonist WIN 55,212-2 on Neuropathic and Visceral Pain Induced by a Non-Diarrheagenic Dose of the Antitumoral Drug 5-Fluorouracil in the Rat. Int. J. Mol. Sci. 2023, 24, 14430. https://doi.org/10.3390/ijms241914430
Vera G, López-Gómez L, Girón R, Martín-Fontelles MI, Nurgali K, Abalo R, Uranga JA. Effect of the Cannabinoid Agonist WIN 55,212-2 on Neuropathic and Visceral Pain Induced by a Non-Diarrheagenic Dose of the Antitumoral Drug 5-Fluorouracil in the Rat. International Journal of Molecular Sciences. 2023; 24(19):14430. https://doi.org/10.3390/ijms241914430
Chicago/Turabian StyleVera, Gema, Laura López-Gómez, Rocío Girón, María Isabel Martín-Fontelles, Kulmira Nurgali, Raquel Abalo, and José Antonio Uranga. 2023. "Effect of the Cannabinoid Agonist WIN 55,212-2 on Neuropathic and Visceral Pain Induced by a Non-Diarrheagenic Dose of the Antitumoral Drug 5-Fluorouracil in the Rat" International Journal of Molecular Sciences 24, no. 19: 14430. https://doi.org/10.3390/ijms241914430
APA StyleVera, G., López-Gómez, L., Girón, R., Martín-Fontelles, M. I., Nurgali, K., Abalo, R., & Uranga, J. A. (2023). Effect of the Cannabinoid Agonist WIN 55,212-2 on Neuropathic and Visceral Pain Induced by a Non-Diarrheagenic Dose of the Antitumoral Drug 5-Fluorouracil in the Rat. International Journal of Molecular Sciences, 24(19), 14430. https://doi.org/10.3390/ijms241914430







