ATRX Loss in the Development and Prognosis of Conjunctival Melanoma
Abstract
:1. Introduction
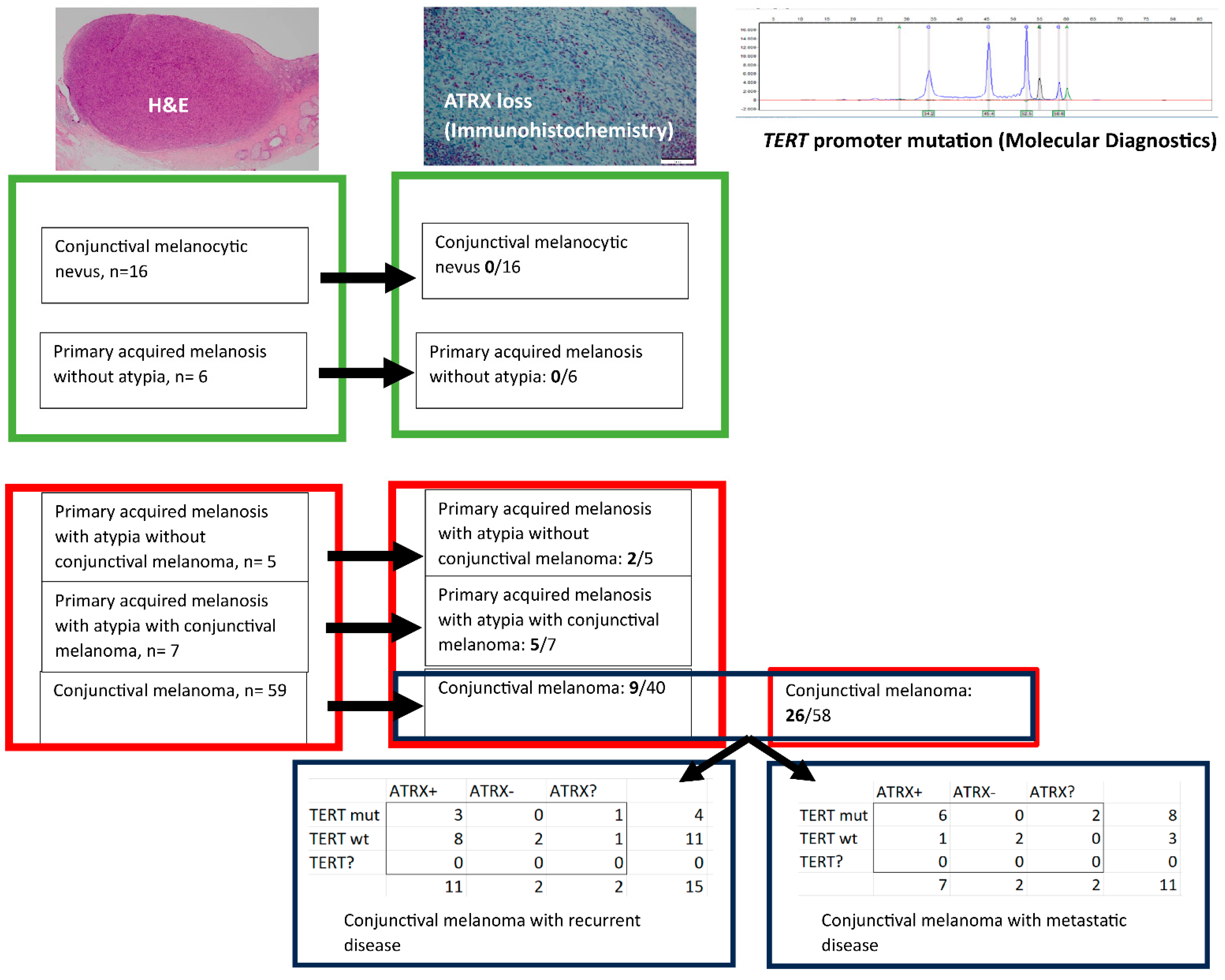
2. Results
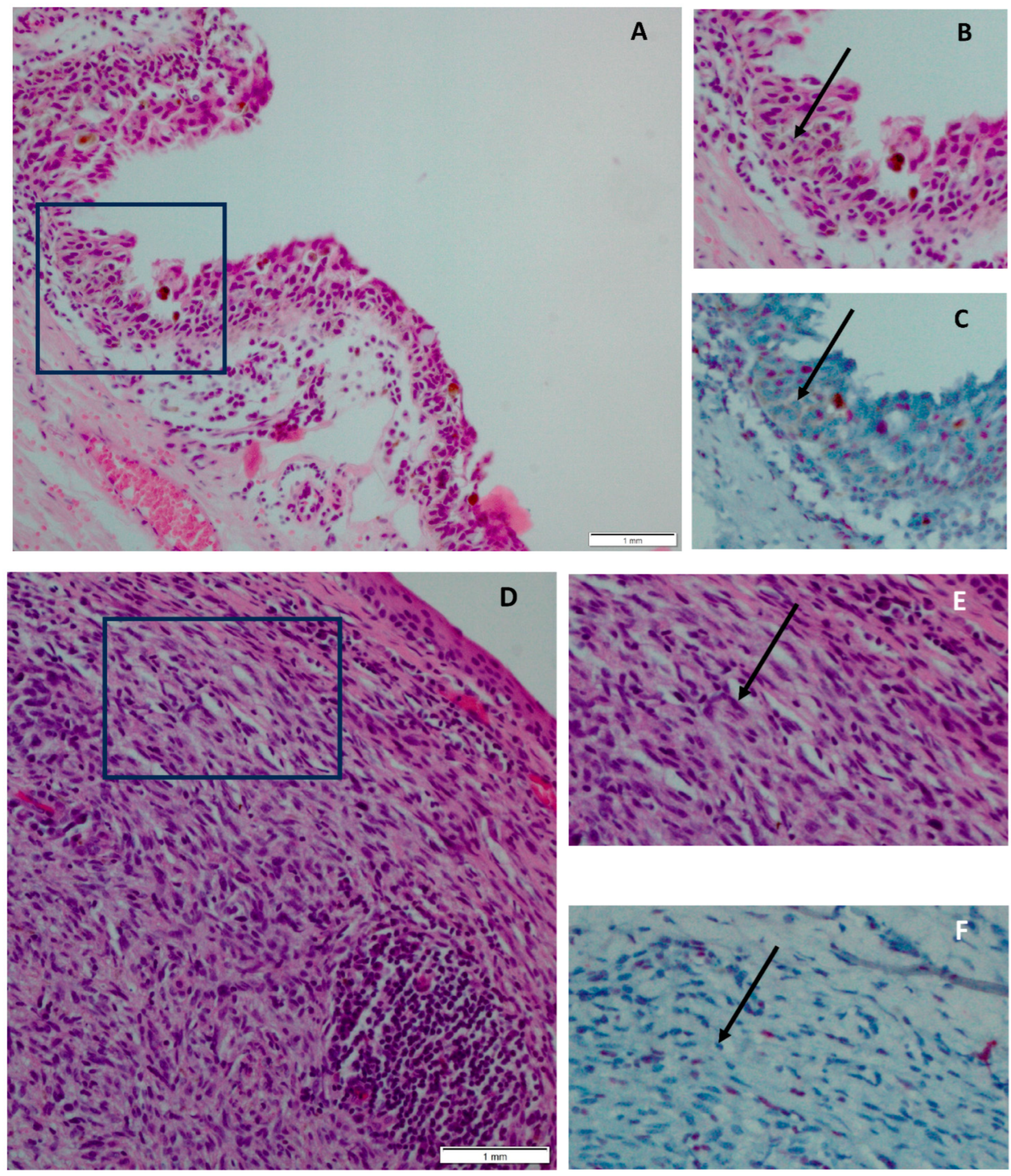
2.1. ATRX Status in Conjunctival Melanocytic Nevi versus CM
2.2. ATRX Status in PAM− versus PAM+
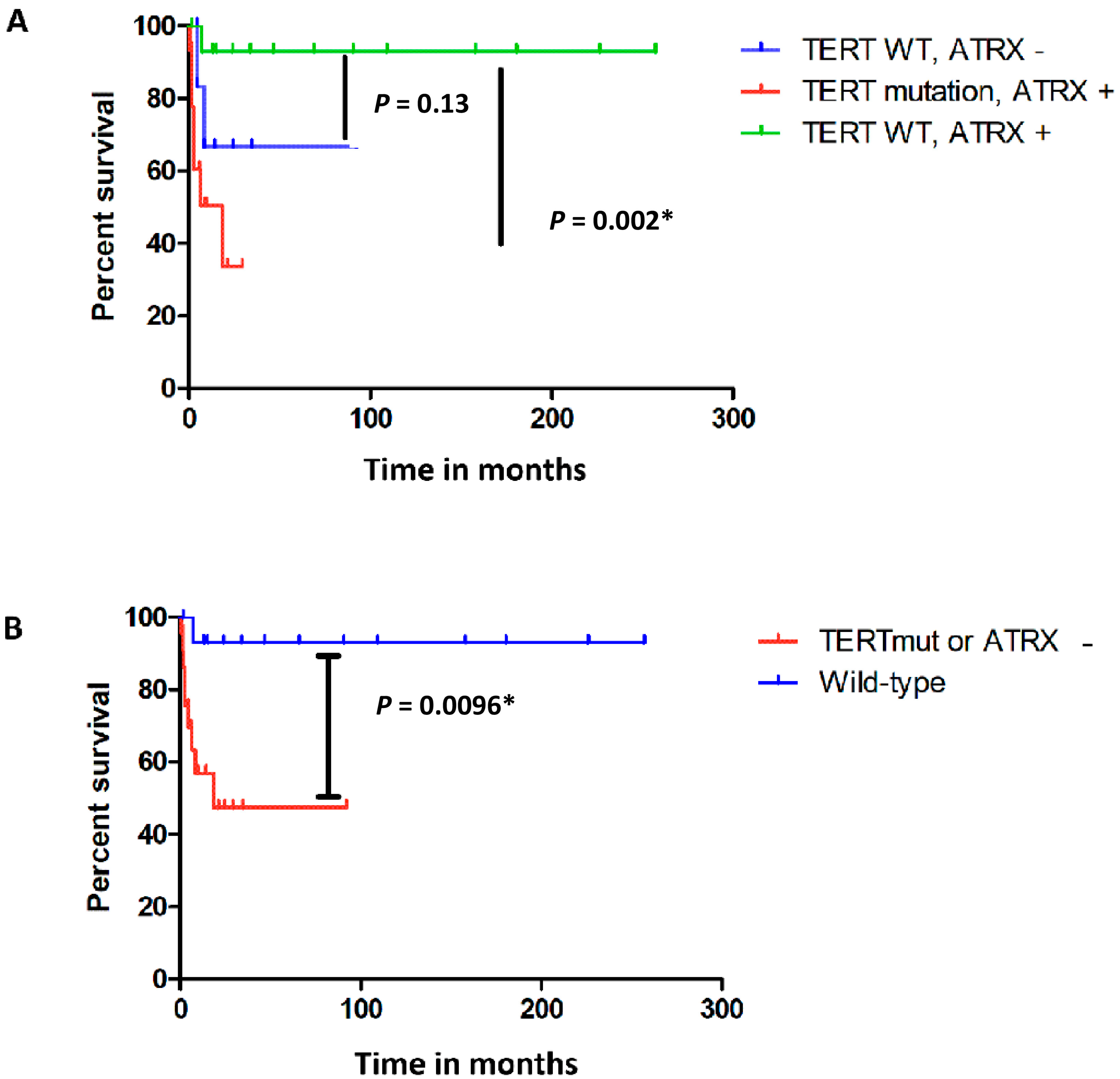
2.3. ATRX Status and CM with Recurrent Disease
2.4. ATRX Status and CM with Metastatic Disease
2.5. TERT Promoter Mutation and ATRX Loss in CM
3. Discussion
4. Materials and Methods
4.1. Material Selection
4.2. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kaštelan, S.; Antunica, A.G.; Orešković, L.B.; Rabatić, J.S.; Kasun, B.; Bakija, I. Conjunctival Melanoma—Epidemiological Trends and Features. Pathol. Oncol. Res. 2018, 24, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Weppelmann, T.A.; Zimmerman, K.T.; Rashidi, V. Trends in Incidence of Conjunctival Melanoma in the US. JAMA Netw. Open 2022, 5, e2237229. [Google Scholar] [CrossRef] [PubMed]
- Virgili, G.; Parravano, M.; Gatta, G.; Capocaccia, R.; Mazzini, C.; Mallone, S.; Botta, L.; RARECAREnet Working Group. Incidence and Survival of Patients With Conjunctival Melanoma in Europe. JAMA Ophthalmol. 2020, 138, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Anastassiou, G.; Heiligenhaus, A.; Bechrakis, N.; Bader, E.; Bornfeld, N.; Steuhl, K.-P. Prognostic value of clinical and histopathological parameters in conjunctival melanomas: A retrospective study. Br. J. Ophthalmol. 2002, 86, 163–167. [Google Scholar] [CrossRef]
- Zhou, C.; Wang, Y.; Jia, R.; Fan, X. Conjunctival Melanoma in Chinese Patients: Local Recurrence, Metastasis, Mortality, and Comparisons With Caucasian Patients. Investig. Opthalmol. Vis. Sci. 2017, 58, 5452–5459. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, L.H.; Maag, E.; Andersen, M.K.; Kruhøffer, M.; Larsen, A.-C.; Melchior, L.C.; Toft, P.B.; von Buchwald, C.; Wadt, K.; Heegaard, S. The molecular profile of mucosal melanoma. Melanoma Res. 2020, 30, 533–542. [Google Scholar] [CrossRef]
- Gkiala, A.; Palioura, S. Conjunctival Melanoma: Update on Genetics, Epigenetics and Targeted Molecular and Immune-Based Therapies. Clin. Ophthalmol. 2020, 14, 3137–3152. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas Network. Genomic Classification of Cutaneous Melanoma. Cell 2015, 161, 1681–1696. [Google Scholar] [CrossRef]
- Pipek, O.; Vizkeleti, L.; Doma, V.; Alpár, D.; Bödör, C.; Kárpáti, S.; Timar, J. The Driverless Triple-Wild-Type (BRAF, RAS, KIT) Cutaneous Melanoma: Whole Genome Sequencing Discoveries. Cancers 2023, 15, 1712. [Google Scholar] [CrossRef]
- Griewank, K.G.; Westekemper, H.; Murali, R.; Mach, M.; Schilling, B.; Wiesner, T.; Schimming, T.; Livingstone, E.; Sucker, A.; Grabellus, F.; et al. Conjunctival melanomas harbor BRAF and NRAS mutations and copy number changes similar to cutaneous and mucosal melanomas. Clin. Cancer Res. 2013, 19, 3143–3152. [Google Scholar] [CrossRef]
- Van Ipenburg, J.A.; Naus, N.C.; Dubbink, H.J.; Van Ginderdeuren, R.; Missotten, G.S.; Paridaens, D.; Verdijk, R.M. Prognostic value of TERT promoter mutations in conjunctival melanomas in addition to clinicopathological features. Br. J. Ophthalmol. 2021, 105, 1454–1461. [Google Scholar] [CrossRef] [PubMed]
- Barthel, F.P.; Wei, W.; Tang, M.; Martinez-Ledesma, E.; Hu, X.; Amin, S.B.; Akdemir, K.C.; Seth, S.; Song, X.; Wang, Q.; et al. Systematic analysis of telomere length and somatic alterations in 31 cancer types. Nat. Genet. 2017, 49, 349–357. [Google Scholar] [CrossRef]
- Newell, F.; Kong, Y.; Wilmott, J.S.; Johansson, P.A.; Ferguson, P.M.; Cui, C.; Li, Z.; Kazakoff, S.H.; Burke, H.; Dodds, T.J.; et al. Whole-genome landscape of mucosal melanoma reveals diverse drivers and therapeutic targets. Nat. Commun. 2019, 10, 3163. [Google Scholar] [CrossRef] [PubMed]
- Aguilera, P.; López-Contreras, A.J. ATRX, a guardian of chromatin. Trends Genet. 2023, 39, 505–519. [Google Scholar] [CrossRef] [PubMed]
- Koelsche, C.; Sahm, F.; Capper, D.; Reuss, D.; Sturm, D.; Jones, D.T.W.; Kool, M.; Northcott, P.A.; Wiestler, B.; Böhmer, K.; et al. Distribution of TERT promoter mutations in pediatric and adult tumors of the nervous system. Acta Neuropathol. 2013, 126, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Lally, S.E.; Milman, T.; Orloff, M.; Dalvin, L.A.; Eberhart, C.G.; Heaphy, C.M.; Rodriguez, F.J.; Lin, C.-C.; Dockery, P.W.; Shields, J.A.; et al. Mutational Landscape and Outcomes of Conjunctival Melanoma in 101 Patients. Ophthalmology 2022, 129, 679–693. [Google Scholar] [CrossRef]
- MacKenzie, D.; Watters, A.K.; To, J.T.; Young, M.W.; Muratori, J.; Wilkoff, M.H.; Abraham, R.G.; Plummer, M.M.; Zhang, D. ALT Positivity in Human Cancers: Prevalence and Clinical Insights. Cancers 2021, 13, 2384. [Google Scholar] [CrossRef]
- Chami, R.; Marrano, P.M.; Teerapakpinyo, C.; Arnoldo, A.; Shago, M.; Shuangshoti, S.; Thorner, P.S. Immunohistochemistry for ATRX Can Miss ATRX Mutations. Am. J. Surg. Pathol. 2019, 43, 1203–1211. [Google Scholar] [CrossRef]
- Yuan, G.; Song, J.; Li, N.; Song, Q.; Li, Y.; Du, Y.; Wang, X.; Jiao, Y.; Wu, L. Telomere Maintenance Associated Mutations in the Genetic Landscape of Gynecological Mucosal Melanoma. Front. Oncol. 2020, 10, 1707. [Google Scholar] [CrossRef]
- Van Poppelen, N.M.; van Ipenburg, J.A.; van den Bosch, Q.; Vaarwater, J.; Brands, T.; Eussen, B.; Magielsen, F.; Dubbink, H.J.; Paridaens, D.; Brosens, E.; et al. Molecular Genetics of Conjunctival Melanoma and Prognostic Value of TERT Promoter Mutation Analysis. Int. J. Mol. Sci. 2021, 22, 5784. [Google Scholar] [CrossRef]
- Eckel-Passow, J.E.; Lachance, D.H.; Molinaro, A.M.; Walsh, K.M.; Decker, P.A.; Sicotte, H.; Pekmezci, M.; Rice, T.W.; Kosel, M.L.; Smirnov, I.V.; et al. Glioma Groups Based on 1p/19q, IDH, and TERTPromoter Mutations in Tumors. N. Engl. J. Med. 2015, 372, 2499–2508. [Google Scholar] [CrossRef] [PubMed]
- Hayward, N.K.; Wilmott, J.S.; Waddell, N.; Johansson, P.A.; Field, M.A.; Nones, K.; Patch, A.-M.; Kakavand, H.; Alexandrov, L.B.; Burke, H.; et al. Whole-genome landscapes of major melanoma subtypes. Nature 2017, 545, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Parikh, D.; Fouquerel, E.; Murphy, C.T.; Wang, H.; Opresko, P.L. Telomeres are partly shielded from ultraviolet-induced damage and proficient for nucleotide excision repair of photoproducts. Nat. Commun. 2015, 6, 8214. [Google Scholar] [CrossRef]
- Shen, E.; Xiu, J.; Lopez, G.Y.; Bentley, R.; Jalali, A.; Heimberger, A.B.; Bainbridge, M.N.; Bondy, M.L.; Walsh, K.M. POT1 mutation spectrum in tumour types commonly diagnosed among POT1-associated hereditary cancer syndrome families. J. Med. Genet. 2020, 57, 664–670. [Google Scholar] [CrossRef]
- Beaudoux, O.; Oudart, J.-B.; Riffaud, L.; Visseaux, L.; Marchal, A.; Lebre, A.-S.; Grange, F. Mutational Characteristics of Primary Mucosal Melanoma: A Systematic Review. Mol. Diagn. Ther. 2022, 26, 189–202. [Google Scholar] [CrossRef]
- Koopmans, A.E.; Ober, K.; Dubbink, H.J.; Paridaens, D.; Naus, N.C.; Belunek, S.; Krist, B.; Post, E.; Zwarthoff, E.C.; De Klein, A.; et al. Prevalence and implications of TERT promoter mutation in uveal and conjunctival melanoma and in benign and premalignant conjunctival melanocytic lesions. Investig. Opthalmol. Vis. Sci. 2014, 55, 6024–6030. [Google Scholar] [CrossRef] [PubMed]
- Harford, E.; Palmer, J.M.; Glasson, W.J.; Warrier, S.K.; Whitehead, K.J.; Brooks, K.M.; Johansson, P.A.; Hayward, N.K.; McGrath, L.A. Choroidal melanoma with synchronous Fuchs’ adenoma and novel ATRX mutation. Int. J. Retin. Vitr. 2022, 8, 24. [Google Scholar] [CrossRef] [PubMed]
| Age at Time of Diagnosis (y) | Gender | Recurrent Disease, Months after Diagnosis | Metastasis, Months after Diagnosis | Breslow (mm) | Ulceration | Presence of Mitotic Figure (s) | Presence of Epithelioid Cells | pT Status | Origin | Diameter (mm) | Bulbar Involvement | Follow-Up (Months after Diagnosis) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 43 | M | 20 | 47 | UK | Yes | Yes | Mixed | pT2b | UK | 7 | UK | 68 |
| 2 | 62 | M | No | No | UK | Yes | Yes | Mixed | UK | UK | 17 | UK | 4 |
| 3 | 44 | M | No | 38 | 1.7 | Yes | Yes | Mixed | pT1a | Nevus | 21 * | UK | 38 |
| 4 | 65 | F | 55 | No | 3.46 | Yes | Yes | Mixed | pT2b | PAM+ | 7 * | UK | 257 |
| 5 | 60 | F | No | No | 0.4 | No | Yes | Mixed | UK | De novo | 6 * | UK | 1 |
| 6 | 68 | F | No | 8 | 7 | Yes | Yes | Mixed | UK | PAM+ | 18 | UK | 54 |
| 7 | 84 | M | No | No | 2.6 * | Yes | Yes | Mixed | pT1b | De novo | 6 * | UK | 1 |
| 8 | 65 | M | No | No | 3 | Yes | Yes | Spindle cells | pT1b | PAM+ | 6 | UK | 6 |
| 9 | 64 | M | No | No | 1.55 * | No | Yes | Mixed | pT1a | Nevus | 6 | UK | 29 |
| 10 | 51 | M | 8 | 9 | 0.96 * | No | Yes | Spindle cells | UK | De novo | 12 * | UK | 22 |
| 11 | 49 | M | No | 49 | 2.3 * | Yes | Yes | Mixed | UK | PAM+ | 3 | UK | 86 |
| 12 | 84 | M | 23 | No | 2.3 * | UK | UK | Epithelioid | UK | PAM+ | UK | UK | 35 |
| 13 | 73 | F | 157 | No | 3 | UK | Yes | Spindle cells | UK | PAM+ | UK | UK | 158 |
| 14 | 53 | M | No | 14 | 3.69 | Yes | Yes | Epithelioid | UK | Nevus | 7 | UK | 36 |
| 15 | 64 | M | 81 | No | 1.1 | No | Yes | Spindle cells | pT1a | PAM+ | UK | UK | 109 |
| 16 | 49 | F | No | No | 0.3 | No | No | Mixed | pT1a | PAM+ | 3 | UK | 166 |
| 17 | 79 | F | No | No | UK | UK | UK | UK | UK | PAM+ | UK | UK | 21 |
| 18 | 66 | M | No | No | 2 | Yes | No | Mixed | pT1a | De novo | 4 | UK | 9 |
| 19 | 83 | F | 87 | No | 5.1 | No | Yes | Mixed | pT2b | PAM+ | 6 * | UK | 90 |
| 20 | 46 | F | No | 2 | 7 * | Yes | Yes | Mixed | UK | PAM+ | 11 | UK | 69 |
| 21 | 65 | M | 11 | 15 | 1.9 * | Yes | Yes | Mixed | UK | De novo | 4.2 | UK | 58 |
| 22 | 63 | M | No | No | UK | UK | UK | UK | UK | PAM+ | 5 | UK | 24 |
| 23 | 40 | M | No | No | 0.3 | No | No | Spindle cells | pT1a | PAM+ | 1.3 | Yes | 3 |
| 24 | 55 | F | No | No | 0.35 | No | No | Spindle cells | pT1a | PAM+ | 10 | Yes | 187 |
| 25 | 75 | F | 5 | No | 0.37 | No | No | Spindle cells | pT1a | PAM+ | 2 | Yes | 226 |
| 26 | 71 | F | No | No | 0.5 | No | No | Spindle cells | UK | PAM+ | UK | UK | 1 |
| 27 | 85 | M | No | No | 0.5 | Yes | Yes | Spindle cells | pT1a | De novo | UK | Yes | 0 |
| 28 | 54 | M | No | No | 0.5 | No | No | UK | pT1a | PAM+ | UK | Yes | 142 |
| 29 | 72 | M | No | No | 0.6 | No | No | Mixed | pT1a | PAM+ | 9 * | Yes | 92 |
| 30 | 56 | F | No | No | 0.62 | No | No | Mixed | UK | Nevus | 4.5 * | UK | 185 |
| 31 | 68 | M | No | No | 0.7 | Yes | No | Spindle cells | pT1a | PAM+ | UK | Yes | 112 |
| 32 | 43 | M | No | No | 0.78 | No | No | Spindle cells | pT2a | De novo | 2.5 | No | 69 |
| 33 | 52 | M | No | No | 0.9 | No | No | Epithelioid | UK | PAM+ | UK | UK | 15 |
| 34 | 84 | M | No | No | 0.9 | UK | UK | Mixed | pT1a | PAM+ | UK | Yes | 24 |
| 35 | 73 | M | No | No | 1.3 | Yes | Yes | Mixed | pT1a | De novo | UK | Yes | 3 |
| 36 | 67 | F | No | No | 1 | Yes | Yes | Epithelioid | pT1a | PAM+ | 6 * | Yes | 2 |
| 37 | 16 | F | No | 18 | 1.04 | Yes | Yes | Mixed | pT1a | Nevus | 0.5 | Yes | 180 |
| 38 | 57 | M | No | No | 1.05 | No | Yes | Epithelioid | pT2a | UK | UK | No | 2 |
| 39 | 63 | F | No | No | 1.1 | No | No | UK | pT1a | Nevus | 3 | Yes | 54 |
| 40 | 56 | M | No | No | 1.3 | No | Yes | Mixed | pT1a | PAM+ | 4.5 * | Yes | 0 |
| 41 | 76 | F | No | No | 2.3 | Yes | Yes | Mixed | pT1b | PAM+ | 17 * | Yes | 2 |
| 42 | 51 | F | No | No | 3 | Yes | Yes | Spindle cells | pT2b | De novo | 10 | No | 95 |
| 43 | 89 | M | No | No | 7.7 * | Yes | Yes | Mixed | pT3a | PAM+ | 14 | No | 13 |
| 44 | 41 | M | No | No | 1 * | No | Yes | Spindle cells | UK | Nevus | 6 | Yes | 14 |
| 45 | 69 | F | 8 | No | 1.1 * | No | No | Mixed | UK | PAM+ | UK | Yes | 34 |
| 46 | 66 | M | No | No | 1.1 * | No | Yes | Spindle cells | UK | PAM+ | 4 * | yes | 81 |
| 47 | 70 | F | No | No | 1.2 * | No | No | Mixed | UK | UK | 4 | Yes | 13 |
| 48 | 71 | M | No | No | 2.7 * | Yes | Yes | Mixed | pT1b | De novo | 6 | Yes | 179 |
| 49 | 57 | M | No | No | 2.5 * | Yes | UK | Mixed | pT1b | PAM+ | 6 | Yes | 15 |
| 50 | 79 | F | No | No | 2.3 | UK | UK | UK | UK | PAM+ | 0.7 | Yes | 0 |
| 51 | 73 | M | No | No | 6.2 | UK | UK | UK | UK | PAM+ | 1.2 | No | 22 |
| 52 | 83 | F | No | No | 3 | UK | UK | UK | UK | Nevus | 1 | Yes | 0 |
| 53 | 80 | F | 29 | No | 0.2 | UK | UK | UK | UK | PAM+ | 0.8 | Yes | 73 |
| 54 | 74 | F | No | 45 | UK | UK | UK | UK | UK | PAM+ | UK | Yes | 49 |
| 55 | 37 | F | No | 7 | 4 | UK | UK | UK | UK | UK | UK | No (though the caruncle is involved) | 66 |
| 56 | 56 | M | 7 | No | 3.5 | UK | UK | UK | UK | PAM+ | UK | Yes | 47 |
| 57 | 58 | M | 42 | No | 3 | UK | UK | UK | UK | PAM+ | 0.6 | Yes | 174 |
| 58 | 60 | M | No | No | 1.1 | UK | UK | UK | UK | UK | 0.6 | No | 5 |
| 59 | 55 | M | No | No | 2.5 | UK | UK | UK | UK | UK | 0.7 | UK | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Ipenburg, J.A.; van den Bosch, Q.C.C.; Paridaens, D.; Dubbink, H.J.; Kiliç, E.; Naus, N.; Verdijk, R.M., on behalf of the Rotterdam Ocular Melanoma Study Group. ATRX Loss in the Development and Prognosis of Conjunctival Melanoma. Int. J. Mol. Sci. 2023, 24, 12988. https://doi.org/10.3390/ijms241612988
van Ipenburg JA, van den Bosch QCC, Paridaens D, Dubbink HJ, Kiliç E, Naus N, Verdijk RM on behalf of the Rotterdam Ocular Melanoma Study Group. ATRX Loss in the Development and Prognosis of Conjunctival Melanoma. International Journal of Molecular Sciences. 2023; 24(16):12988. https://doi.org/10.3390/ijms241612988
Chicago/Turabian Stylevan Ipenburg, Jolique A., Quincy C. C. van den Bosch, Dion Paridaens, Hendrikus J. Dubbink, Emine Kiliç, Nicole Naus, and Robert M. Verdijk on behalf of the Rotterdam Ocular Melanoma Study Group. 2023. "ATRX Loss in the Development and Prognosis of Conjunctival Melanoma" International Journal of Molecular Sciences 24, no. 16: 12988. https://doi.org/10.3390/ijms241612988
APA Stylevan Ipenburg, J. A., van den Bosch, Q. C. C., Paridaens, D., Dubbink, H. J., Kiliç, E., Naus, N., & Verdijk, R. M., on behalf of the Rotterdam Ocular Melanoma Study Group. (2023). ATRX Loss in the Development and Prognosis of Conjunctival Melanoma. International Journal of Molecular Sciences, 24(16), 12988. https://doi.org/10.3390/ijms241612988






