Pesticides and Bladder Cancer: Mechanisms Leading to Anti-Cancer Drug Chemoresistance and New Chemosensitization Strategies
Abstract
1. Introduction
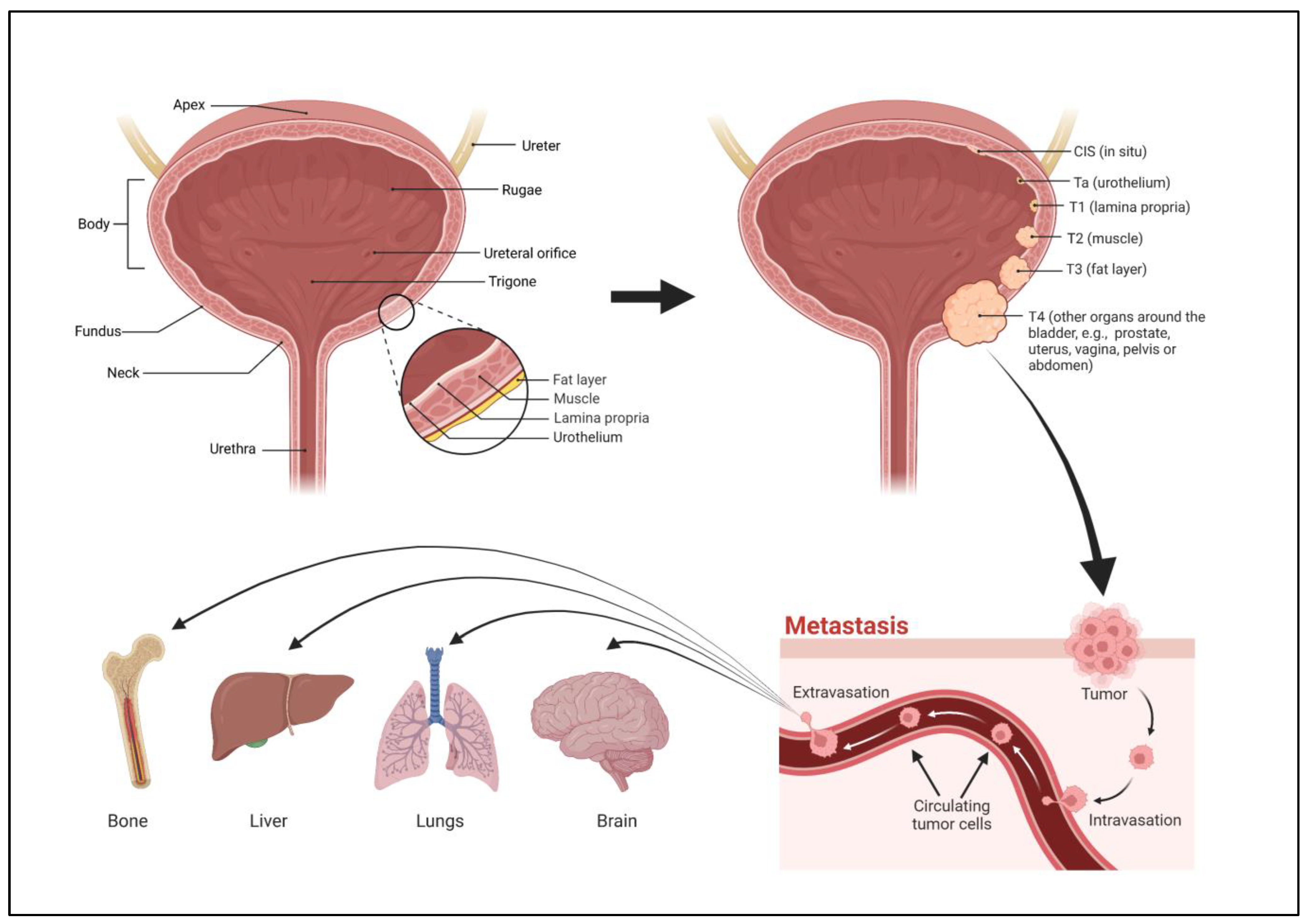
2. Structure of the Bladder
3. Stages of Bladder Cancer
4. Grades of Bladder Cancer
5. Types of Bladder Cancer
6. Pesticides
7. Routes of Pesticide Exposure That May Promote Bladder Cancer
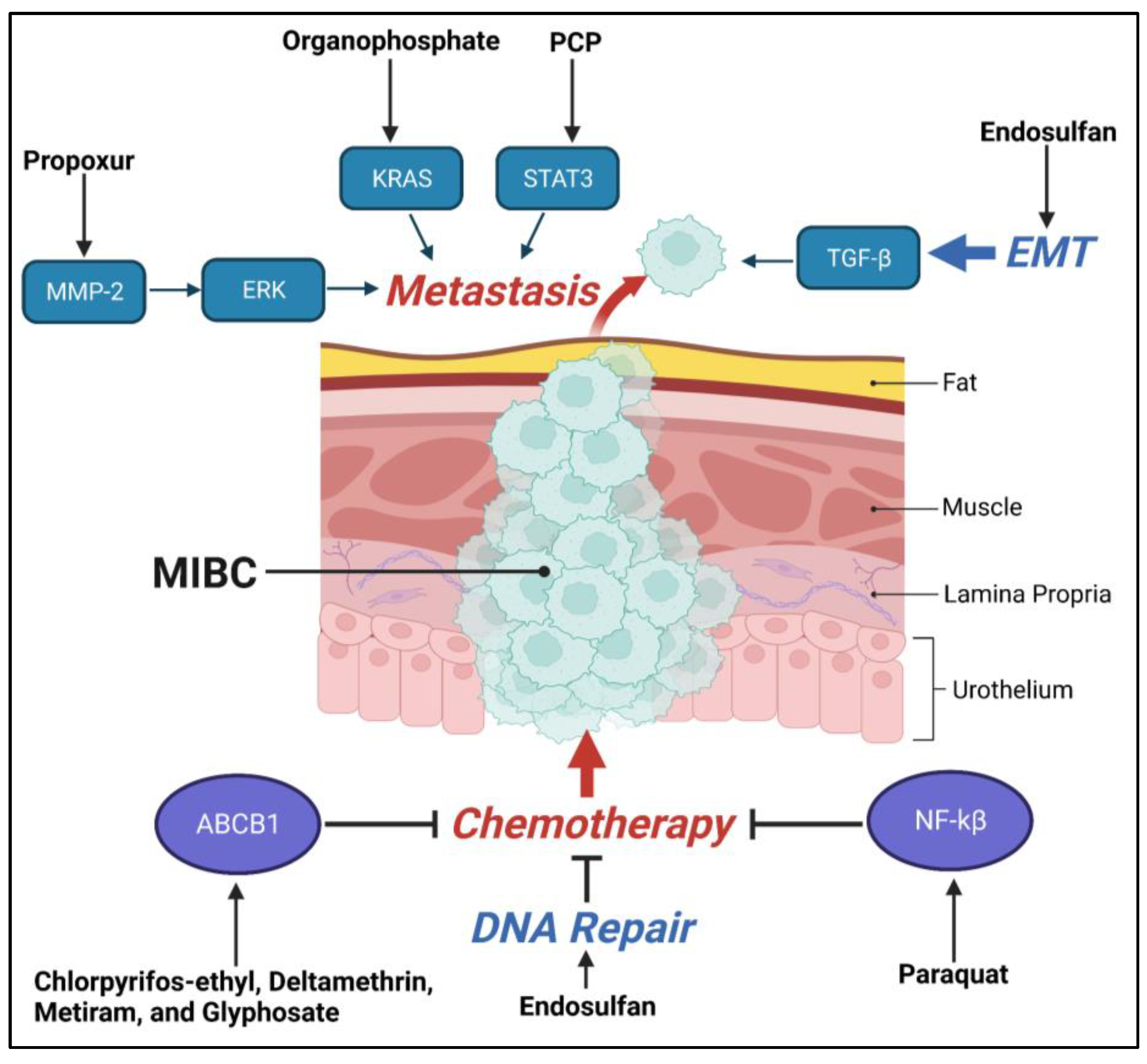
8. Role of Pesticides in Oncogenesis
9. Role of Pesticides in EMT and Metastasis
10. Chemoresistance Due to Pesticide Exposure
11. Pesticide Effects on Other Therapies for Bladder Cancer
12. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Martin, P.; Hooker, M.; Aktar, M.; Stockton, M. How many workers are employed in California agriculture? Calif. Agric. 2016, 71, 30–34. [Google Scholar] [CrossRef]
- Isharwal, S.; Konety, B. Non-muscle invasive bladder cancer risk stratification. Indian J. Urol. 2015, 31, 289–296. [Google Scholar] [CrossRef]
- Bilim, V.; Kuroki, H.; Shirono, Y.; Murata, M.; Hiruma, K.; Tomita, Y. Advanced Bladder Cancer: Changing the Treatment Landscape. J. Pers. Med. 2022, 12, 1745. [Google Scholar] [CrossRef]
- Park, J.C.; Citrin, D.E.; Agarwal, P.K.; Apolo, A.B. Multimodal management of muscle-invasive bladder cancer. Curr. Probl. Cancer 2014, 38, 80–108. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Halaseh, S.A.; Halaseh, S.; Alali, Y.; Ashour, M.E.; Alharayzah, M.J. A Review of the Etiology and Epidemiology of Bladder Cancer: All You Need to Know. Cureus 2022, 14, e27330. [Google Scholar] [CrossRef] [PubMed]
- Baan, R.; Straif, K.; Grosse, Y.; Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Cogliano, V. Carcinogenicity of some aromatic amines, organic dyes, and related exposures. Lancet Oncol. 2008, 9, 322–323. [Google Scholar] [CrossRef]
- Cumberbatch, M.G.K.; Jubber, I.; Black, P.C.; Esperto, F.; Figueroa, J.D.; Kamat, A.M.; Kiemeney, L.; Lotan, Y.; Pang, K.; Silverman, D.T.; et al. Epidemiology of Bladder Cancer: A Systematic Review and Contemporary Update of Risk Factors in 2018. Eur. Urol. 2018, 74, 784–795. [Google Scholar] [CrossRef]
- Rosiello, G.; Palumbo, C.; Deuker, M.; Stolzenbach, L.F.; Martin, T.; Tian, Z.; Gallina, A.; Montorsi, F.; Black, P.; Kassouf, W.; et al. Racial differences in the distribution of bladder cancer metastases: A population-based analysis. Cent. Eur. J. Urol. 2020, 73, 407–415. [Google Scholar] [CrossRef]
- Wang, Y.; Chang, Q.; Li, Y. Racial differences in Urinary Bladder Cancer in the United States. Sci. Rep. 2018, 8, 12521. [Google Scholar] [CrossRef] [PubMed]
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Padala, S.A.; Barsouk, A. Epidemiology of Bladder Cancer. Med. Sci. 2020, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Sui, X.; Lei, L.; Chen, L.; Xie, T.; Li, X. Inflammatory microenvironment in the initiation and progression of bladder cancer. Oncotarget 2017, 8, 93279–93294. [Google Scholar] [CrossRef] [PubMed]
- Manley, K.V.; Hubbard, R.; Swallow, D.; Finch, W.; Wood, S.J.; Biers, S.M. Risk factors for development of primary bladder squamous cell carcinoma. Ind. Mark. Manag. 2017, 99, 155–160. [Google Scholar] [CrossRef]
- Mostafa, M.H.; Sheweita, S.A.; O’connor, P.J. Relationship between Schistosomiasis and Bladder Cancer. Clin. Microbiol. Rev. 1999, 12, 97–111. [Google Scholar] [CrossRef]
- Sharma, P.K.; Pandey, P.K.; Vijay, M.K.; Bera, M.K.; Singh, J.P.; Saha, K. Squamous cell carcinoma in exstrophy of the bladder. Korean J. Urol. 2013, 54, 555–557. [Google Scholar] [CrossRef]
- Talar-Williams, C.; Hijazi, Y.M.; Walther, M.M.; Linehan, W.M.; Hallahan, C.W.; Lubensky, I.; Kerr, G.S.; Hoffman, G.S.; Fauci, A.S.; Sneller, M.C. Cyclophosphamide-Induced Cystitis and Bladder Cancer in Patients with Wegener Granulomatosis. Ann. Intern. Med. 1996, 124, 477–484. [Google Scholar] [CrossRef]
- Suriano, F.; Altobelli, E.; Sergi, F.; Buscarini, M. Bladder cancer after radiotherapy for prostate cancer. Rev. Urol. 2013, 15, 108–112. [Google Scholar]
- Bhat, S.; Sathyanarayanaprasad, M.; Paul, F. Primary squamous cell carcinoma of bladder exstrophy in an adult. Indian J. Urol. 2015, 31, 142–143. [Google Scholar] [CrossRef]
- Omidakhsh, N.; Heck, J.E.; Cockburn, M.; Ling, C.; Hershman, J.M.; Harari, A. Thyroid Cancer and Pesticide Use in a Central California Agricultural Area: A Case Control Study. J. Clin. Endocrinol. Metab. 2022, 107, e3574–e3582. [Google Scholar] [CrossRef]
- Pedroso, T.M.A.; Benvindo-Souza, M.; de Araújo Nascimento, F.; Woch, J.; Dos Reis, F.G.; de Melo e Silva, D. Cancer and occupational exposure to pesticides: A bibliometric study of the past 10 years. Environ. Sci. Pollut. Res. 2022, 29, 17464–17475. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.S.; George, D.M.S.; Loffredo, C.A.; Amr, S. Nonoccupational exposure to agricultural work and risk of urinary bladder cancer among Egyptian women. Arch. Environ. Occup. Health 2017, 72, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Viel, J.F.; Challier, B. Bladder cancer among French farmers: Does exposure to pesticides in vineyards play a part? Occup. Environ. Med. 1995, 52, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Boulanger, M.; Tual, S.; LeMarchand, C.; Guizard, A.-V.; Velten, M.; Marcotullio, E.; Baldi, I.; Clin, B.; LeBailly, P. Agricultural exposure and risk of bladder cancer in the AGRIculture and CANcer cohort. Int. Arch. Occup. Environ. Health 2017, 90, 169–178. [Google Scholar] [CrossRef]
- Liang, Z.; Wang, X.; Xie, B.; Zhu, Y.; Wu, J.; Li, S.; Meng, S.; Zheng, X.; Ji, A.; Xie, L. Pesticide exposure and risk of bladder cancer: A meta-analysis. Oncotarget 2016, 7, 66959–66969. [Google Scholar] [CrossRef]
- Koutros, S.; Alavanja, M.C.; Lubin, J.H.; Sandler, D.P.; Hoppin, J.A.; Lynch, C.F.; Knott, C.; Blair, A.; Freeman, L.E.B. An Update of Cancer Incidence in the Agricultural Health Study. J. Occup. Environ. Med. 2010, 52, 1098–1105. [Google Scholar] [CrossRef]
- Acquavella, J.; Olsen, G.; Cole, P.; Ireland, B.; Kaneene, J.; Schuman, S.; Holden, L. Cancer among Farmers: A Meta-Analysis. Ann. Epidemiol. 1998, 8, 64–74. [Google Scholar] [CrossRef]
- Kabat, G.C.; Dieck, G.S.; Wynder, E.L. Bladder Cancer in Nonsmokers. Cancer 1986, 57, 362–367. [Google Scholar] [CrossRef]
- Amr, S.; Dawson, R.; Saleh, D.A.; Magder, L.S.; Mikhail, N.N.; George, D.M.S.; Squibb, K.; Khaled, H.; Loffredo, C.A. Agricultural Workers and Urinary Bladder Cancer Risk in Egypt. Arch. Environ. Occup. Health 2013, 69, 3–10. [Google Scholar] [CrossRef]
- Koutros, S.; Silverman, D.T.; Alavanja, M.C.; Andreotti, G.; Lerro, C.C.; Heltshe, S.; Lynch, C.F.; Sandler, D.P.; Blair, A.; Freeman, L.E.B. Occupational exposure to pesticides and bladder cancer risk. Int. J. Epidemiol. 2016, 45, 792–805. [Google Scholar] [CrossRef]
- Shermadou, E.S.; Rahman, S.; Leslie, S.W. Anatomy, Abdomen and Pelvis: Bladder; StatPearls: Tampa, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK531465/ (accessed on 16 April 2023).
- Bolla, S.R.; Odeluga, N.; Amraei, R.; Jetti, R. Histology, Bladder; StatPearls: Tampa, FL, USA, 2023. [Google Scholar]
- Dalghi, M.G.; Montalbetti, N.; Carattino, M.D.; Apodaca, G. The Urothelium: Life in a Liquid Environment. Physiol. Rev. 2020, 100, 1621–1705. [Google Scholar] [CrossRef]
- Andersson, K.; McCloskey, K.D. Lamina propria: The functional center of the bladder? Neurourol. Urodyn. 2014, 33, 9–16. [Google Scholar] [CrossRef]
- Andersson, K.-E.; Arner, A. Urinary Bladder Contraction and Relaxation: Physiology and Pathophysiology. Physiol. Rev. 2004, 84, 935–986. [Google Scholar] [CrossRef]
- Miyazaki, J.; Nishiyama, H. Epidemiology of urothelial carcinoma. Int. J. Urol. 2017, 24, 730–734. [Google Scholar] [CrossRef]
- Yin, P.N.; Kc, K.; Wei, S.; Yu, Q.; Li, R.; Haake, A.R.; Miyamoto, H.; Cui, F. Histopathological distinction of non-invasive and invasive bladder cancers using machine learning approaches. BMC Med. Inform. Decis. Mak. 2020, 20, 162. [Google Scholar] [CrossRef]
- Adamczyk, P.; Pobłocki, P.; Kadlubowski, M.; Ostrowski, A.; Wróbel, A.; Mikołajczak, W.; Adamowicz, J.; Drewa, T.; Juszczak, K. A Comprehensive Approach to Clinical Staging of Bladder Cancer. J. Clin. Med. 2022, 11, 761. [Google Scholar] [CrossRef]
- Blanca, A.; Lopez-Beltran, A.; Lopez-Porcheron, K.; Gomez-Gomez, E.; Cimadamore, A.; Bilé-Silva, A.; Gogna, R.; Montironi, R.; Cheng, L. Risk Classification of Bladder Cancer by Gene Expression and Molecular Subtype. Cancers 2023, 15, 2149. [Google Scholar] [CrossRef]
- Lopez-Beltran, A. Bladder cancer: Clinical and pathological profile. Scand. J. Urol. Nephrol. 2008, 42, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.; Porten, S.; Kim, S.; Willis, D.; Plimack, E.R.; Hoffman-Censits, J.; Roth, B.; Cheng, T.; Tran, M.; Lee, I.-L.; et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 2014, 25, 152–165. [Google Scholar] [CrossRef] [PubMed]
- Apollo, A.; Ortenzi, V.; Scatena, C.; Zavaglia, K.; Aretini, P.; Lessi, F.; Franceschi, S.; Tomei, S.; Sepich, C.A.; Viacava, P.; et al. Molecular characterization of low grade and high grade bladder cancer. PLoS ONE 2019, 14, e0210635. [Google Scholar] [CrossRef] [PubMed]
- Kirkali, Z.; Chan, T.; Manoharan, M.; Algaba, F.; Busch, C.; Cheng, L.; Kiemeney, L.; Kriegmair, M.; Montironi, R.; Murphy, W.M.; et al. Bladder cancer: Epidemiology, staging and grading, and diagnosis. Urology 2005, 66, 4–34. [Google Scholar] [CrossRef]
- Neuzillet, Y.; Paoletti, X.; Ouerhani, S.; Mongiat-Artus, P.; Soliman, H.; de The, H.; Sibony, M.; Denoux, Y.; Molinie, V.; Herault, A.; et al. A meta-analysis of the relationship between FGFR3 and TP53 mutations in bladder cancer. PLoS ONE 2012, 7, e48993. [Google Scholar] [CrossRef] [PubMed]
- Kaseb, H.; Aeddula, N.R. Bladder Cancer; StatPearls: Tampa, FL, USA, 2023. [Google Scholar]
- Minato, A.; Noguchi, H.; Tomisaki, I.; Fukuda, A.; Kubo, T.; Nakayama, T.; Fujimoto, N. Clinical Significance of Squamous Differentiation in Urothelial Carcinoma of the Bladder. Cancer Control 2018, 25, 1073274818800269. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B. Histological variants of urothelial carcinoma: Diagnostic, therapeutic and prognostic implications. Mod. Pathol. 2009, 22 (Suppl. S2), S96–S118. [Google Scholar] [CrossRef]
- Makise, N.; Morikawa, T.; Kawai, T.; Nakagawa, T.; Kume, H.; Homma, Y.; Fukayama, M. Squamous differentiation and prognosis in upper urinary tract urothelial carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 7203–7209. [Google Scholar]
- Warrick, J.I. Clinical Significance of Histologic Variants of Bladder Cancer. J. Natl. Compr. Cancer Netw. 2017, 15, 1268–1274. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.W.; Carballido, E.M.; Ahmed, A.; Farhan, B.; Dutta, R.; Smith, C.; Youssef, R.F. Squamous cell carcinoma of the urinary bladder: Systematic review of clinical characteristics and therapeutic approaches. Arab. J. Urol. 2016, 14, 183–191. [Google Scholar] [CrossRef]
- Ho, C.-H.; Sung, K.-C.; Lim, S.-W.; Liao, C.-H.; Liang, F.-W.; Wang, J.-J.; Wu, C.-C. Chronic Indwelling Urinary Catheter Increase the Risk of Bladder Cancer, Even in Patients Without Spinal Cord Injury. Medicine 2015, 94, e1736. [Google Scholar] [CrossRef]
- PDQ Supportive and Palliative Care Editorial Board. PDQ Cancer Information Summaries. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK65883/ (accessed on 9 May 2023).
- Bandini, M.; Pederzoli, F.; Madison, R.; Briganti, A.; Ross, J.S.; Niegisch, G.; Yu, E.Y.; Bamias, A.; Agarwal, N.; Sridhar, S.S.; et al. Unfavorable Cancer-specific Survival After Neoadjuvant Chemotherapy and Radical Cystectomy in Patients with Bladder Cancer and Squamous Cell Variant: A Multi-institutional Study. Clin. Genitourin. Cancer 2020, 18, e543–e556. [Google Scholar] [CrossRef]
- Dadhania, V.; Czerniak, B.; Guo, C.C. Adenocarcinoma of the urinary bladder. Am. J. Clin. Exp. Urol. 2015, 3, 51–63. [Google Scholar]
- Ismaili, N. A rare bladder cancer—Small cell carcinoma: Review and update. Orphanet J. Rare Dis. 2011, 6, 75. [Google Scholar] [CrossRef]
- Weiss, B.; Amler, S.; Amler, R.W. Pesticides. Pediatrics 2004, 113, 1030–1036. [Google Scholar] [CrossRef]
- Cohen, M. Environmental toxins and health—The health impact of pesticides. Aust. Fam. Physician 2007, 36, 1002–1004. [Google Scholar]
- MacFarlane, E.; Carey, R.; Keegel, T.; El-Zaemay, S.; Fritschi, L. Dermal exposure associated with occupational end use of pesticides and the role of protective measures. Saf. Health Work. 2013, 4, 136–141. [Google Scholar] [CrossRef]
- Latif, Y.; Sherazi, S.T.H.; Bhanger, M.I.; Nizamani, S. Evaluation of Pesticide Residues in Human Blood Samples of Agro Professionals and Non-Agro Professionals. Am. J. Anal. Chem. 2012, 3, 587–595. [Google Scholar] [CrossRef]
- Ali, T.; Ismail, M.; Asad, F.; Ashraf, A.; Waheed, U.; Khan, Q.M. Pesticide genotoxicity in cotton picking women in Pakistan evaluated using comet assay. Drug Chem. Toxicol. 2018, 41, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Kapeleka, J.A.; Sauli, E.; Ndakidemi, P.A. Pesticide exposure and genotoxic effects as measured by DNA damage and human monitoring biomarkers. Int. J. Environ. Health Res. 2021, 31, 805–822. [Google Scholar] [CrossRef]
- Singh, S.; Kumar, V.; Thakur, S.; Banerjee, B.D.; Chandna, S.; Rautela, R.S.; Grover, S.S.; Rawat, D.S.; Pasha, S.T.; Jain, S.K.; et al. DNA damage and cholinesterase activity in occupational workers exposed to pesticides. Environ. Toxicol. Pharmacol. 2011, 31, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Connolly, A.; Jones, K.; Galea, K.S.; Basinas, I.; Kenny, L.; McGowan, P.; Coggins, M. Exposure assessment using human biomonitoring for glyphosate and fluroxypyr users in amenity horticulture. Int. J. Hyg. Environ. Healrh 2017, 220, 1064–1073. [Google Scholar] [CrossRef]
- Sokoloff, K.; Fraser, W.; Arbuckle, T.E.; Fisher, M.; Gaudreau, E.; LeBlanc, A.; Morisset, A.-S.; Bouchard, M.F. Determinants of urinary concentrations of dialkyl phosphates among pregnant women in Canada—Results from the MIREC study. Environ. Int. 2016, 94, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-H.; Kabir, E.; Jahan, S.A. Exposure to pesticides and the associated human health effects. Sci. Total Environ. 2017, 575, 525–535. [Google Scholar] [CrossRef]
- Hayat, K.; Afzal, M.; Aqueel, M.A.; Ali, S.; Khan, Q.M.; Ashfaq, U. Determination of insecticide residues and their adverse effects on blood profile of occupationally exposed individuals. Ecotoxicol. Environ. Saf. 2018, 163, 382–390. [Google Scholar] [CrossRef]
- Parrón, T.; Requena, M.; Hernández, A.F.; Alarcón, R. Environmental exposure to pesticides and cancer risk in multiple human organ systems. Toxicol. Lett. 2014, 230, 157–165. [Google Scholar] [CrossRef]
- Hu, R.; Huang, X.; Huang, J.; Li, Y.; Zhang, C.; Yin, Y.; Chen, Z.; Cai, J.; Cui, F. Long- and short-term health effects of pesticide exposure: A cohort study from China. PLoS ONE 2015, 10, e0128766. [Google Scholar] [CrossRef]
- Rohlman, D.S.; Anger, W.K.; Lein, P.J. Correlating neurobehavioral performance with biomarkers of organophosphorous pesticide exposure. Neurotoxicology 2011, 32, 268–276. [Google Scholar] [CrossRef]
- Faria, N.M.X.; Fassa, A.G.; Meucci, R.D.; Fiori, N.S.; Miranda, V.I. Occupational exposure to pesticides, nicotine and minor psychiatric disorders among tobacco farmers in southern Brazil. Neurotoxicology 2014, 45, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Bolognesi, C. Genotoxicity of pesticides: A review of human biomonitoring studies. Mutat. Res. Mol. Mech. Mutagen. 2003, 543, 251–272. [Google Scholar] [CrossRef] [PubMed]
- Band, P.R.; Abanto, Z.; Bert, J.; Lang, B.; Fang, R.; Gallagher, R.P.; Le, N.D. Prostate cancer risk and exposure to pesticides in British Columbia Farmers. Prostate 2011, 71, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Alavanja, M.C.R.; Hofmann, J.; Lynch, C.F.; Hines, C.J.; Barry, K.H.; Barker, J.; Buckman, D.W.; Thomas, K.; Sandler, D.P.; Hoppin, J.; et al. Non-hodgkin lymphoma risk and insecticide, fungicide and fumigant use in the agricultural health study. PLoS ONE 2014, 9, e109332. [Google Scholar] [CrossRef]
- Koutros, S.; Lynch, C.F.; Ma, X.; Lee, W.J.; Hoppin, J.A.; Christensen, C.H.; Andreotti, G.; Freeman, L.B.; Rusiecki, J.A.; Hou, L.; et al. Heterocyclic aromatic amine pesticide use and human cancer risk: Results from the U.S. Agricultural Health Study. Int. J. Cancer 2009, 124, 1206–1212. [Google Scholar] [CrossRef]
- Jung, I.; Messing, E. Molecular mechanisms and pathways in bladder cancer development and progression. Cancer Control 2000, 7, 325–334. [Google Scholar] [CrossRef]
- Glickman, L.T.; Raghavan, M.; Knapp, D.W.; Bonney, P.L.; Dawson, M.H. Herbicide exposure and the risk of transitional cell carcinoma of the urinary bladder in Scottish Terriers. J. Am. Veter.-Med. Assoc. 2004, 224, 1290–1297. [Google Scholar] [CrossRef]
- Loomis, D.; Guyton, K.; Grosse, Y.; El Ghissasi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Mattock, H.; Straif, K. Carcinogenicity of lindane, DDT, and 2,4-dichlorophenoxyacetic acid. Lancet Oncol. 2015, 16, 891–892. [Google Scholar] [CrossRef]
- Ünal, F.; Yüzbaşıoğlu, D.; Yılmaz, S.; Akıncı, N.; Aksoy, H. Genotoxic effects of chlorophenoxy herbicide diclofop-methyl in micein vivoand in human lymphocytesin vitro. Drug Chem. Toxicol. 2011, 34, 390–395. [Google Scholar] [CrossRef]
- Yamada, A.; Aki, T.; Unuma, K.; Funakoshi, T.; Uemura, K. Paraquat Induces Epithelial-Mesenchymal Transition-Like Cellular Response Resulting in Fibrogenesis and the Prevention of Apoptosis in Human Pulmonary Epithelial Cells. PLoS ONE 2015, 10, e0120192. [Google Scholar] [CrossRef]
- Doğanlar, O.; Doğanlar, Z.B.; Kurtdere, A.K.; Chasan, T.; Ok, E.S. Chronic exposure of human glioblastoma tumors to low concentrations of a pesticide mixture induced multidrug resistance against chemotherapy agents. Ecotoxicol. Environ. Saf. 2020, 202, 110940. [Google Scholar] [CrossRef]
- Freeman, L.E.B.; Bonner, M.R.; Blair, A.; Hoppin, J.A.; Sandler, D.P.; Lubin, J.H.; Dosemeci, M.; Lynch, C.F.; Knott, C.; Alavanja, M.C.R. Cancer Incidence among Male Pesticide Applicators in the Agricultural Health Study Cohort Exposed to Diazinon. Am. J. Epidemiol. 2005, 162, 1070–1079. [Google Scholar] [CrossRef] [PubMed]
- Ferri, G.M.; Specchia, G.; Mazza, P.; Ingravallo, G.; Intranuovo, G.; Guastadisegno, C.M.; Congedo, M.L.; Lagioia, G.; Loparco, M.C.; Giordano, A.; et al. Risk of lymphoma subtypes by occupational exposure in Southern Italy. J. Occup. Med. Toxicol. 2017, 12, 31. [Google Scholar] [CrossRef] [PubMed]
- Piel, C.; Pouchieu, C.; Tual, S.; Migault, L.; LeMarchand, C.; Carles, C.; Boulanger, M.; Gruber, A.; Rondeau, V.; Marcotullio, E.; et al. Central nervous system tumors and agricultural exposures in the prospective cohort AGRICAN. Int. J. Cancer 2017, 141, 1771–1782. [Google Scholar] [CrossRef] [PubMed]
- Piel, C.; Pouchieu, C.; Carles, C.; Béziat, B.; Boulanger, M.; Bureau, M.; Busson, A.; Grüber, A.; Lecluse, Y.; Migault, L.; et al. Agricultural exposures to carbamate herbicides and fungicides and central nervous system tumour incidence in the cohort AGRICAN. Environ. Int. 2019, 130, 104876. [Google Scholar] [CrossRef]
- Liu, S.; Hu, Y.; Wang, Y.; Sun, Y.; Qin, S.-L.; Xu, D. Endosulfan promotes cell proliferation and extracellular matrix accumulation through TGF-β/Smad signaling pathway in HRMCs. Ecotoxicol. Environ. Saf. 2021, 228, 113040. [Google Scholar] [CrossRef]
- Arrebola, J.P.; Belhassen, H.; Artacho-Cordón, F.; Ghali, R.; Ghorbel, H.; Boussen, H.; Perez-Carrascosa, F.M.; Expósito, J.; Hedhili, A.; Olea, N. Risk of female breast cancer and serum concentrations of organochlorine pesticides and polychlorinated biphenyls: A case–control study in Tunisia. Sci. Total Environ. 2015, 520, 106–113. [Google Scholar] [CrossRef]
- Lerro, C.C.; Koutros, S.; Andreotti, G.; Hines, C.J.; Blair, A.; Lubin, J.; Ma, X.; Zhang, Y.; Freeman, L.E.B. Use of acetochlor and cancer incidence in the Agricultural Health Study. Int. J. Cancer 2015, 137, 1167–1175. [Google Scholar] [CrossRef]
- Cabello, G.; Galaz, S.; Botella, L.; Calaf, G.; Pacheco, M.; Stockert, J.C.; Villanueva, A.; Cañete, M.; Juarranz, A. The pesticide malathion induces alterations in actin cytoskeleton and in cell adhesion of cultured breast carcinoma cells. Int. J. Oncol. 2003, 23, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; An, D.; Liu, Y.; Feng, Q.; Fang, X.; Pan, G.; Wang, Q. Propoxur enhances MMP-2 expression and the corresponding invasion of human breast cancer cells via the ERK/Nrf2 signaling pathway. Oncotarget 2017, 8, 87107–87123. [Google Scholar] [CrossRef]
- Lasagna, M.; Hielpos, M.; Ventura, C.; Mardirosian, M.; Martín, G.; Miret, N.; Randi, A.; Núñez, M.; Cocca, C. Chlorpyrifos subthreshold exposure induces epithelial-mesenchymal transition in breast cancer cells. Ecotoxicol. Environ. Saf. 2020, 205, 111312. [Google Scholar] [CrossRef]
- Lee, W.J.; Alavanja, M.C.; Hoppin, J.A.; Rusiecki, J.A.; Kamel, F.; Blair, A.; Sandler, D.P. Mortality among pesticide applicators exposed to chlorpyrifos in the agricultural health study. Environ. Health Perspect. 2007, 115, 528–534. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.; Tian, Y.; DU, Y.; Huang, L.; Chen, J.; Li, N.; Liu, W.; Liang, Z.; Zhao, L. Atrazine promotes RM1 prostate cancer cell proliferation by activating STAT3 signaling. Int. J. Oncol. 2016, 48, 2166–2174. [Google Scholar] [CrossRef] [PubMed]
- Thota, S.; Begum, R.; Kaur, G.; Bagam, P.; Dorsey, W.; Batra, S. Pentachlorophenol mediated regulation of DAMPs and inflammation: In vitro study. Toxicol. Vitr. 2022, 83, 105378. [Google Scholar] [CrossRef]
- Andreotti, G.; Freeman, L.E.B.; Hou, L.; Coble, J.; Rusiecki, J.; Hoppin, J.A.; Silverman, D.T.; Alavanja, M.C. Agricultural pesticide use and pancreatic cancer risk in the Agricultural Health Study Cohort. Int. J. Cancer 2009, 124, 2495–2500. [Google Scholar] [CrossRef]
- van Bemmel, D.M.; Visvanathan, K.; Freeman, L.E.B.; Coble, J.; Hoppin, J.A.; Alavanja, M.C. S -Ethyl- N,N -dipropylthiocarbamate exposure and cancer incidence among male pesticide applicators in the agricultural health study: A prospective cohort. Environ. Health Perspect. 2008, 116, 1541–1546. [Google Scholar] [CrossRef]
- Samanic, C.; Rusiecki, J.; Dosemeci, M.; Hou, L.; Hoppin, J.A.; Sandler, D.P.; Lubin, J.; Blair, A.; Alavanja, M.C. Cancer incidence among pesticide applicators exposed to dicamba in the agricultural health study. Environ. Health Perspect. 2006, 114, 1521–1526. [Google Scholar] [CrossRef]
- Purdue, M.P.; Hoppin, J.A.; Blair, A.; Dosemeci, M.; Alavanja, M.C. Occupational exposure to organochlorine insecticides and cancer incidence in the Agricultural Health Study. Int. J. Cancer 2007, 120, 642–649. [Google Scholar] [CrossRef]
- Hou, L.; Lee, W.J.; Rusiecki, J.; Hoppin, J.A.; Blair, A.; Bonner, M.R.; Lubin, J.H.; Samanic, C.; Sandler, D.P.; Dosemeci, M.; et al. Pendimethalin exposure and cancer incidence among pesticide applicators. Epidemiology 2006, 17, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Park, S.K.; Beane-Freeman, L.; Lynch, C.F.; Knott, C.E.; Sandler, D.P.; Hoppin, J.A.; Dosemeci, M.; Coble, J.; Lubin, J.; et al. Cancer incidence among pesticide applicators exposed to trifluralin in the Agricultural Health Study. Environ. Res. 2008, 107, 271–276. [Google Scholar] [CrossRef]
- Multigner, L.; Ndong, J.R.; Giusti, A.; Romana, M.; Delacroix-Maillard, H.; Cordier, S.; Jégou, B.; Thome, J.P.; Blanchet, P. Chlordecone exposure and risk of prostate cancer. J. Clin. Oncol. 2010, 28, 3457–3462. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, R.; Blair, A.; Lynch, C.F.; Schroeder, P.; Hoppin, J.A.; Sandler, D.P.; Alavanja, M.C. Fonofos exposure and cancer incidence in the agricultural health study. Environ. Health Perspect. 2006, 114, 1838–1842. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Hoppin, J.A.; Blair, A.; Lubin, J.H.; Dosemeci, M.; Sandler, D.P.; Alavanja, M.C.R. Cancer incidence among pesticide applicators exposed to alachlor in the agricultural health study. Am. J. Epidemiol. 2004, 159, 373–380. [Google Scholar] [CrossRef]
- Dennis, L.K.; Lynch, C.F.; Sandler, D.P.; Alavanja, M.C. Pesticide use and cutaneous melanoma in pesticide applicators in the agricultural heath study. Environ. Health Perspect. 2010, 118, 812–817. [Google Scholar] [CrossRef]
- Parkash, O.; Kiesswetter, H. The Role of Urine in the Etiology of Cancer of the Urinary Bladder. Urol. Int. 1976, 31, 343–348. [Google Scholar] [CrossRef]
- Damalas, C.A.; Eleftherohorinos, I.G. Pesticide Exposure, Safety Issues, and Risk Assessment Indicators. Int. J. Environ. Res. Public Health 2011, 8, 1402–1419. [Google Scholar] [CrossRef]
- National Research Council. Intentional Human Dosing Studies for EPA Regulatory Purposes; National Academies Press: Washington, DC, USA, 2004. [Google Scholar] [CrossRef]
- Tsamouri, M.M.; Steele, T.M.; Mudryj, M.; Kent, M.S.; Ghosh, P.M. Comparative Cancer Cell Signaling in Muscle-Invasive Urothelial Carcinoma of the Bladder in Dogs and Humans. Biomedicines 2021, 9, 1472. [Google Scholar] [CrossRef]
- Glickman, L.T.; Schofer, F.S.; McKee, L.J.; Reif, J.S.; Goldschmidt, M.H. Epidemiologic study of insecticide exposures, obesity, and risk of bladder cancer in household dogs. J. Toxicol. Environ. Health 1989, 28, 407–414. [Google Scholar] [CrossRef]
- Knapp, D.W.; Peer, W.A.; Conteh, A.; Diggs, A.R.; Cooper, B.R.; Glickman, N.W.; Bonney, P.L.; Stewart, J.C.; Glickman, L.T.; Murphy, A.S. Detection of herbicides in the urine of pet dogs following home lawn chemical application. Sci. Total. Environ. 2013, 456–457, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Knapp, D.W.; Glickman, N.W.; DeNicola, D.B.; Bonney, P.L.; Lin, T.L.; Glickman, L.T. Naturally-occurring canine transitional cell carcinoma of the urinary bladder A relevant model of human invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2000, 5, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Burns, C.; Bodner, K.; Swaen, G.; Collins, J.; Beard, K.; Lee, M. Cancer Incidence of 2,4-D Production Workers. Int. J. Environ. Res. Public Health 2011, 8, 3579–3590. [Google Scholar] [CrossRef] [PubMed]
- Craun, K.; Luethcke, K.R.; Shafer, M.; Stanton, N.; Zhang, C.; Schauer, J.; Faulkes, J.; Sundling, K.E.; Kurtycz, D.; Malecki, K.; et al. Environmental chemical exposures in the urine of dogs and people sharing the same households. J. Clin. Transl. Sci. 2020, 5, 1–27. [Google Scholar] [CrossRef]
- Mortazavi, N.; Asadikaram, G.; Ebadzadeh, M.; Kamalati, A.; Pakmanesh, H.; Dadgar, R.; Moazed, V.; Paydar, P.; Fallah, H.; Abolhassani, M. Organochlorine and organophosphorus pesticides and bladder cancer: A case-control study. J. Cell. Biochem. 2019, 120, 14847–14859. [Google Scholar] [CrossRef]
- Phyu, M.P.; Hlain, Z.T.T.; Zaw, T.; Htway, S.M.; Sein, M.T. Correlation Study Between Erythrocyte Acetylcholinesterase Activity, Serum Malondialdehyde and Insulin Sensitivity in Agricultural Workers and Non-agricultural Workers in Nat-Kan Village, Magway Township. J. ASEAN Fed. Endocr. Soc. 2020, 35, 85–92. [Google Scholar] [CrossRef]
- Piruat, J.I.; Millán-Uclés, Á. Genetically modeled mice with mutations in mitochondrial metabolic enzymes for the study of cancer. Front. Oncol. 2014, 4, 200. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Tseng, L.-M.; Lee, H.-C. Role of mitochondrial dysfunction in cancer progression. Exp. Biol. Med. 2016, 241, 1281–1295. [Google Scholar] [CrossRef]
- Elmore, S.E.; La Merrill, M.A. Oxidative Phosphorylation Impairment by DDT and DDE. Front. Endocrinol. 2019, 10, 122. [Google Scholar] [CrossRef] [PubMed]
- Reuter, S.; Gupta, S.C.; Chaturvedi, M.M.; Aggarwal, B.B. Oxidative stress, inflammation, and cancer: How are they linked? Free Radic. Biol. Med. 2010, 49, 1603–1616. [Google Scholar] [CrossRef]
- Hameed, D.A.; Yassa, H.A.; Agban, M.N.; Hanna, R.T.; Elderwy, A.M.; Zwaita, M.A. Genetic aberrations of the K-ras proto-oncogene in bladder cancer in relation to pesticide exposure. Environ. Sci. Pollut. Res. 2018, 25, 21535–21542. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.I.; Patel, R.; Liu, Y.; Singh, L.B.; Taketo, M.M.; Wu, X.-R.; Leung, H.Y.; Sansom, O.J. Ras mutation cooperates with β-catenin activation to drive bladder tumourigenesis. Cell Death Dis. 2011, 2, e124. [Google Scholar] [CrossRef]
- Masui, T.; Mann, A.M.; Macatee, T.L.; Okamura, T.; Garland, E.M.; Fujii, H.; Pelling, J.C.; Cohen, S.M. H-ras mutations in rat urinary bladder carcinomas induced by N-[4-(5-nitro-2-furyl)-2-thiazolyl]formamide and sodium saccharin, sodium ascorbate, or related salts. Cancer Res. 1991, 51, 3471–3475. [Google Scholar]
- Fares, J.; Fares, M.Y.; Khachfe, H.H.; Salhab, H.A.; Fares, Y. Molecular principles of metastasis: A hallmark of cancer revisited. Signal Transduct. Target. Ther. 2020, 5, 28. [Google Scholar] [CrossRef]
- Chin, J.; Siddiqui, K.; Tran, K.-C. Metastatic Bladder Cancer; Western University: London, ON, Canada, 2017; pp. 177–198. [Google Scholar] [CrossRef]
- Shayan, R.; Achen, M.G.; Stacker, S.A. Lymphatic vessels in cancer metastasis: Bridging the gaps. Carcinog 2006, 27, 1729–1738. [Google Scholar] [CrossRef]
- Massagué, J.; Obenauf, A.C. Metastatic colonization by circulating tumour cells. Nature 2016, 529, 298–306. [Google Scholar] [CrossRef]
- Maitra, A. Molecular envoys pave the way for pancreatic cancer to invade the liver. Nature 2019, 567, 181–182. [Google Scholar] [CrossRef]
- Hall, A. The cytoskeleton and cancer. Cancer Metastasis Rev. 2009, 28, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Kessenbrock, K.; Plaks, V.; Werb, Z. Matrix metalloproteinases: Regulators of the tumor microenvironment. Cell 2010, 141, 52–67. [Google Scholar] [CrossRef]
- Chaffer, C.L.; Weinberg, R.A. A perspective on cancer cell metastasis. Science 2011, 331, 1559–1564. [Google Scholar] [CrossRef]
- Nguyen, D.X.; Bos, P.D.; Massague, J. Metastasis: From dissemination to organ-specific colonization. Nat. Rev. Cancer 2009, 9, 274–284. [Google Scholar] [CrossRef]
- Mittal, V. Epithelial Mesenchymal Transition in Tumor Metastasis. Annu. Rev. Pathol. 2018, 13, 395–412. [Google Scholar] [CrossRef]
- Davis, F.M.; Stewart, T.A.; Thompson, E.W.; Monteith, G.R. Targeting EMT in cancer: Opportunities for pharmacological intervention. Trends Pharmacol. Sci. 2014, 35, 479–488. [Google Scholar] [CrossRef]
- Thiery, J.P.; Acloque, H.; Huang, R.Y.J.; Nieto, M.A. Epithelial-mesenchymal transitions in development and disease. Cell 2009, 139, 871–890. [Google Scholar] [CrossRef]
- Brabletz, T.; Kalluri, R.; Nieto, M.A.; Weinberg, R.A. EMT in cancer. Nat. Rev. Cancer 2018, 18, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Tuomainen, A.; Kangas, J.A.; Meuling, W.J.; Glass, R.C. Monitoring of pesticide applicators for potential dermal exposure to malathion and biomarkers in urine. Toxicol. Lett. 2002, 134, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Shengnan, L.; Fei, W.; Yingli, S.; Qingshan, S.; Wei, S.; Shuhua, X.; Guifan, S.; Lin, Z.; Shengnan, L.; et al. Dimethylarsinic acid (DMAV) changed the expressions of proliferative related factors and secretion of inflammatory cytokines in rat bladder. J. Appl. Toxicol. 2015, 35, 133–141. [Google Scholar] [CrossRef]
- Zhou, Q.; Jin, P.; Liu, J.; Li, S.; Liu, W.; Xi, S. Arsenic-induced HER2 promotes proliferation, migration and angiogenesis of bladder epithelial cells via activation of multiple signaling pathways in vitro and in vivo. Sci. Total Environ. 2021, 753, 141962. [Google Scholar] [CrossRef]
- Yang, W.; Ma, X.; Zhu, Y.; Meng, X.; Tian, R.; Yang, Z. Paraquat but not diquat induces TGF-β expression and thus activates calcium-NFAT axis for epithelial–mesenchymal transition. Toxicol. Res. 2021, 10, 733–741. [Google Scholar] [CrossRef]
- Liu, H.; Wu, Q.; Chu, T.; Mo, Y.; Cai, S.; Chen, M.; Zhu, G. High-dose acute exposure of paraquat induces injuries of swim bladder, gastrointestinal tract and liver via neutrophil-mediated ROS in zebrafish and their relevance for human health risk assessment. Chemosphere 2018, 205, 662–673. [Google Scholar] [CrossRef]
- da Silva, J.C.; Scandolara, T.B.; Kern, R.; Jaques, H.D.S.; Malanowski, J.; Alves, F.M.; Rech, D.; Silveira, G.F.; Panis, C. Occupational Exposure to Pesticides Affects Pivotal Immunologic Anti-Tumor Responses in Breast Cancer Women from the Intermediate Risk of Recurrence and Death. Cancers 2022, 14, 5199. [Google Scholar] [CrossRef]
- Feng, Y.; Yang, Z.; Xu, X. c-Met: A Promising Therapeutic Target in Bladder Cancer. Cancer Manag. Res. 2022, 14, 2379–2388. [Google Scholar] [CrossRef]
- Sim, W.J.; Iyengar, P.V.; Lama, D.; Lui, S.K.L.; Ng, H.C.; Haviv-Shapira, L.; Domany, E.; Kappei, D.; Tan, T.Z.; Saei, A.; et al. c-Met activation leads to the establishment of a TGFβ-receptor regulatory network in bladder cancer progression. Nat. Commun. 2019, 10, 4349. [Google Scholar] [CrossRef]
- Huang, X.; Li, E.; Shen, H.; Wang, X.; Tang, T.; Zhang, X.; Xu, J.; Tang, Z.; Guo, C.; Bai, X.; et al. Targeting the HGF/MET Axis in Cancer Therapy: Challenges in Resistance and Opportunities for Im-provement. Front. Cell Dev. Biol. 2020, 8, 152. [Google Scholar] [CrossRef]
- Kim, B.-G.; Malek, E.; Choi, S.H.; Ignatz-Hoover, J.J.; Driscoll, J.J. Novel therapies emerging in oncology to target the TGF-β pathway. J. Hematol. Oncol. 2021, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Calaf, G.M.; Bleak, T.C.; Muñoz, J.P.; Aguayo, F. Markers of epithelial-mesenchymal transition in an experimental breast cancer model induced by organophosphorous pesticides and estrogen (Review). Oncol. Lett. 2020, 20, 1. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Shen, Y.; Wang, S.; Shen, Q.; Zhou, X. The Role of STAT3 in Leading the Crosstalk between Human Cancers and the Immune System. Cancer Lett. 2018, 415, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-F.; Lin, P.-Y.; Wu, C.-F.; Chen, W.-C.; Wu, C.-T. IL-6 Expression regulates tumorigenicity and correlates with prognosis in bladder cancer. PLoS ONE 2013, 8, e61901. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Xie, R.-Y.; Cao, C.-Z.; Shang, B.-Q.; Shi, H.-Z.; Shou, J.-Z. Disease Management of Clinical Complete Responders to Neoadjuvant Chemotherapy of Muscle-Invasive Bladder Cancer: A Review of Literature. Front. Oncol. 2022, 12, 816444. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Zhang, F.; Chen, W.; Zhang, J.; Li, H. miRNAs: A Promising Target in the Chemoresistance of Bladder Cancer. OncoTargets Ther. 2019, 12, 11805–11816. [Google Scholar] [CrossRef]
- Donat, S.M.; North, A.; Dalbagni, G.; Herr, H.W. Efficacy of office fulguration for recurrent low grade papillary bladder tumors less than 0.5 cm. J. Urol. 2004, 171, 636–639. [Google Scholar] [CrossRef]
- Zacharis, A.; Grüllich, C. Die Erstlinientherapie des metastasierten Urothelkarzinoms. Der Urol. 2020, 59, 797–803. [Google Scholar] [CrossRef]
- Ughachukwu, P.; Unekwe, P. Efflux Pump-Mediated Resistance in Chemotherapy. Ann. Med. Health Sci. Res. 2012, 2, 191–198. [Google Scholar] [CrossRef]
- Giddings, E.L.; Champagne, D.P.; Wu, M.-H.; Laffin, J.M.; Thornton, T.M.; Valenca-Pereira, F.; Culp-Hill, R.; Fortner, K.A.; Romero, N.; East, J.; et al. Mitochondrial ATP fuels ABC transporter-mediated drug efflux in cancer chemoresistance. Nat. Commun. 2021, 12, 2804. [Google Scholar] [CrossRef] [PubMed]
- Bouwman, P.; Jonkers, J. The effects of deregulated DNA damage signalling on cancer chemotherapy response and resistance. Nat. Rev. Cancer 2012, 12, 587–598. [Google Scholar] [CrossRef]
- Li, L.-Y.; Guan, Y.-D.; Chen, X.-S.; Yang, J.-M.; Cheng, Y. DNA Repair Pathways in Cancer Therapy and Resistance. Front. Pharmacol. 2021, 11, 629266. [Google Scholar] [CrossRef]
- Fernald, K.; Kurokawa, M. Evading apoptosis in cancer. Trends Cell Biol. 2013, 23, 620–633. [Google Scholar] [CrossRef]
- Fulda, S. Evasion of Apoptosis as a Cellular Stress Response in Cancer. Int. J. Cell Biol. 2010, 2010, 370835. [Google Scholar] [CrossRef] [PubMed]
- Caracciolo, D.; Riillo, C.; Di Martino, M.T.; Tagliaferri, P.; Tassone, P. Alternative Non-Homologous End-Joining: Error-Prone DNA Repair as Cancer’s Achilles’ Heel. Cancers 2021, 13, 1392. [Google Scholar] [CrossRef] [PubMed]
- Sfeir, A.; Symington, L.S. Microhomology-mediated end joining: A back-up survival mechanism or dedicated pathway? Trends Biochem. Sci. 2015, 40, 701–714. [Google Scholar] [CrossRef] [PubMed]
- Bentley, J. DNA double strand break repair in human bladder cancer is error prone and involves microhomology-associated end-joining. Nucleic Acids Res. 2004, 32, 5249–5259. [Google Scholar] [CrossRef]
- Sebastian, R.; Raghavan, S.C. Induction of DNA damage and erroneous repair can explain genomic instability caused by endosulfan. Carcinog. 2016, 37, 929–940. [Google Scholar] [CrossRef]
- Boada, L.D.; Henriquez-Hernandez, L.A.; Zumbado, M.; Almeida-González, M.; Álvarez-León, E.E.; Navarro, P.; Luzardo, O.P. Organochlorine Pesticides Exposure and Bladder Cancer: Evaluation from a Gene-Environment Perspective in a Hospital-Based Case-Control Study in the Canary Islands (Spain). J. Agromed. 2016, 21, 34–42. [Google Scholar] [CrossRef]
- Sathua, K.; Srivastava, S.; Flora, S. MiADMSA ameliorate arsenic induced urinary bladder carcinogenesis in vivo and in vitro. Biomed. Pharmacother. 2020, 128, 110257. [Google Scholar] [CrossRef]
- Wong, R.S.Y. Apoptosis in cancer: From pathogenesis to treatment. J. Exp. Clin. Cancer Res. 2011, 30, 87. [Google Scholar] [CrossRef]
- Luo, J.-L.; Kamata, H.; Karin, M. IKK/NF- B signaling: Balancing life and death—A new approach to cancer therapy. J. Clin. Investig. 2005, 115, 2625–2632. [Google Scholar] [CrossRef]
- Kucharczak, J.; Simmons, M.J.; Fan, Y.; Gélinas, C. To be, or not to be: NF-κB is the answer—Role of Rel/NF-κB in the regulation of apoptosis. Oncogene 2003, 22, 8961–8982. [Google Scholar] [CrossRef]
- Karin, M.; Lin, A. NF-κB at the crossroads of life and death. Nat. Immunol. 2002, 3, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Shen, D.; Kong, C.; Zhang, Z.; Zeng, Y.; Lin, X.; Liu, X. NF-κB suppresses apoptosis and promotes bladder cancer cell proliferation by upregulating survivin expression in vitro and in vivo. Sci. Rep. 2017, 7, 40723. [Google Scholar] [CrossRef] [PubMed]
- Godwin, P.; Baird, A.M.; Heavey, S.; Barr, M.P.; O’byrne, K.J.; Gately, K. Targeting Nuclear Factor-Kappa B to Overcome Resistance to Chemotherapy. Front. Oncol. 2013, 3, 120. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Misra, H.P. Reactive oxygen species in in vitro pesticide-induced neuronal cell (SH-SY5Y) cytotoxicity: Role of NFκB and caspase-3. Free. Radic. Biol. Med. 2007, 42, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Gargouri, B.; Boukholda, K.; Kumar, A.; Benazzouz, A.; Fetoui, H.; Fiebich, B.L.; Bouchard, M. Bifenthrin insecticide promotes oxidative stress and increases inflammatory mediators in human neuroblastoma cells through NF-kappaB pathway. Toxicol. Vitr. 2020, 65, 104792. [Google Scholar] [CrossRef]
- Williams, C.-A.; Lin, Y.; Maynard, A.; Cheng, S.-Y. Involvement of NF kappa B in potentiated effect of Mn-containing dithiocarbamates on MPP+ induced cell death. Cell. Mol. Neurobiol. 2013, 33, 815–823. [Google Scholar] [CrossRef]
- Pires, B.R.B.; Mencalha, A.L.; Ferreira, G.M.; de Souza, W.F.; Morgado-Díaz, J.A.; Maia, A.M.; Corrêa, S.; Abdelhay, E.S.F.W. NF-kappaB Is Involved in the Regulation of EMT Genes in Breast Cancer Cells. PLoS ONE 2017, 12, e0169622. [Google Scholar] [CrossRef]
- Xia, Y.; Shen, S.; Verma, I.M. NF-κB, an Active Player in Human Cancers. Cancer Immunol. Res. 2014, 2, 823–830. [Google Scholar] [CrossRef]
- Yan, M.; Xu, Q.; Zhang, P.; Zhou, X.-J.; Zhang, Z.-Y.; Chen, W.-T. Correlation of NF-κB signal pathway with tumor metastasis of human head and neck squamous cell carcinoma. BMC Cancer 2010, 10, 437. [Google Scholar] [CrossRef]
- Zhu, J.; Li, Y.; Chen, C.; Ma, J.; Sun, W.; Tian, Z.; Li, J.; Xu, J.; Liu, C.S.; Zhang, D.; et al. NF-κB p65 Overexpression Promotes Bladder Cancer Cell Migration via FBW7-Mediated Degradation of RhoGDIα Protein. Neoplasia 2017, 19, 672–683. [Google Scholar] [CrossRef]
- Geng, H.; Guo, W.; Feng, L.; Xie, D.; Bi, L.; Wang, Y.; Zhang, T.; Liang, Z.; Yu, D. Diallyl trisulfide inhibited tobacco smoke-mediated bladder EMT and cancer stem cell marker expression via the NF-κB pathway in vivo. J. Int. Med. Res. 2021, 49, 0300060521992900. [Google Scholar] [CrossRef] [PubMed]
- Ramadass, V.; Vaiyapuri, T.; Tergaonkar, V. Small Molecule NF-kB Pathway Inhibitors in Clinic. Int. J. Mol. Sci. 2020, 21, 5164. [Google Scholar] [CrossRef] [PubMed]
- Swellam, M.; Abd-Elmaksoud, N.; Halim, M.H.; Khatab, H.; Khiry, H. Incidence of Bcl-2 expression in bladder cancer: Relation to schistosomiasis. Clin. Biochem. 2004, 37, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Miyake, H.; Hanada, N.; Nakamura, H.; Kagawa, S.; Fujiwara, T.; Hara, I.; Eto, H.; Gohji, K.; Arakawa, S.; Kamidono, S.; et al. Overexpression of Bcl-2 in bladder cancer cells inhibits apoptosis induced by cisplatin and adenoviral-mediated p53 gene transfer. Oncogene 1998, 16, 933–943. [Google Scholar] [CrossRef] [PubMed]
- Inoue, S.; Ide, H.; Mizushima, T.; Jiang, G.; Netto, G.J.; Gotoh, M.; Miyamoto, H. Nuclear Factor-κB Promotes Urothelial Tumorigenesis and Cancer Progression via Cooperation with Androgen Receptor Signaling. Mol. Cancer Ther. 2018, 17, 1303–1314. [Google Scholar] [CrossRef]
- Thomas, S.; Quinn, B.A.; Das, S.K.; Dash, R.; Emdad, L.; Dasgupta, S.; Wang, X.-Y.; Dent, P.; Reed, J.C.; Pellecchia, M.; et al. Targeting the Bcl-2 family for cancer therapy. Expert Opin. Ther. Targets 2013, 17, 61–75. [Google Scholar] [CrossRef]
- Roulland, S.; Lebailly, P.; Lecluse, Y.; Briand, M.; Pottier, D.; Gauduchon, P. Characterization of the t(14;18) BCL2-IGH translocation in farmers occupationally exposed to pesticides. Cancer Res. 2004, 64, 2264–2269. [Google Scholar] [CrossRef]
- Qaqish, B.M.; Al-Dalahmah, O.; Al-Motassem, Y.; Battah, A.; Ismail, S.S. Occupational exposure to pesticides and occurrence of the chromosomal translocation t(14;18) among farmers in Jordan. Toxicol. Rep. 2016, 3, 225–229. [Google Scholar] [CrossRef]
- Shin, D.Y.; Kim, G.-Y.; Hwang, H.J.; Kim, W.-J.; Choi, Y.H. Diallyl trisulfide-induced apoptosis of bladder cancer cells is caspase-dependent and regulated by PI3K/Akt and JNK pathways. Environ. Toxicol. Pharmacol. 2014, 37, 74–83. [Google Scholar] [CrossRef]
- Prabhu, B.; Sivakumar, A.; Sundaresan, S. Diindolylmethane and Lupeol Modulates Apoptosis and Cell Proliferation in N-Butyl-N-(4-Hydroxybutyl) Nitrosamine Initiated and Dimethylarsinic Acid Promoted rat Bladder Carcinogenesis. Pathol. Oncol. Res. 2016, 22, 747–754. [Google Scholar] [CrossRef]
- Takara, K.; Sakaeda, T.; Okumura, K. An update on overcoming MDR1-mediated multidrug resistance in cancer chemotherapy. Curr. Pharm. Des. 2006, 12, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Sakaeda, T.; Nakamura, T.; Okumura, K. Pharmacogenetics of MDR1 and its impact on the pharmacokinetics and pharmacodynamics of drugs. Pharmacogenomics 2004, 4, 397–410. [Google Scholar] [CrossRef] [PubMed]
- Conrad, S.; Kauffmann, H.-M.; Ito, K.-I.; Leslie, E.; Deeley, R.G.; Schrenk, D.; Cole, S. A naturally occurring mutation in MRP1 results in a selective decrease in organic anion transport and in increased doxorubicin resistance. Pharmacogenetics 2002, 12, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Leslie, E.M.; Létourneau, I.J.; Deeley, R.G.; Cole, S.P.C. Functional and structural consequences of cysteine substitutions in the NH2 proximal region of the human multidrug resistance protein 1 (MRP1/ABCC1). Biochemistry 2003, 42, 5214–5224. [Google Scholar] [CrossRef]
- Conseil, G.; Cole, S.P. Two Polymorphic Variants of ABCC1Selectively alter drug resistance and inhibitor sensitivity of the multidrug and organic anion transporter multidrug resistance protein 1. Drug Metab. Dispos. 2013, 41, 2187–2196. [Google Scholar] [CrossRef]
- Chen, C.-C.; Huang, C.-H.; Wu, M.-T.M.; Chou, C.-H.; Huang, C.-C.; Tseng, T.-Y.; Chang, F.-Y.; Li, Y.-T.; Tsai, C.-C.; Wang, T.-S.; et al. Multidrug resistance 1 gene variants, pesticide exposure, and increased risk of DNA damage. BioMed Res. Int. 2014, 2014, 1–9. [Google Scholar] [CrossRef]
- Pinto, B.G.S.; Soares, T.K.M.; Linhares, M.A.; Ghisi, N.C. Occupational exposure to pesticides: Genetic danger to farmworkers and manufacturing workers—A meta-analytical review. Sci. Total Environ. 2020, 748, 141382. [Google Scholar] [CrossRef]
- Sun, Y.; Guan, Z.; Liang, L.; Cheng, Y.; Zhou, J.; Li, J.; Xu, Y. HIF-1α/MDR1 pathway confers chemoresistance to cisplatin in bladder cancer. Oncol. Rep. 2016, 35, 1549–1556. [Google Scholar] [CrossRef]
- Garje, R.; An, J.; Obeidat, M.; Kumar, K.; Yasin, H.A.; Zakharia, Y. Fibroblast Growth Factor Receptor (FGFR) Inhibitors in Urothelial Cancer. Oncologist 2020, 25, e1711–e1719. [Google Scholar] [CrossRef]
- Wong, J.L.; Rosenberg, J.E. Targeting nectin-4 by antibody-drug conjugates for the treatment of urothelial carcinoma. Expert Opin. Biol. Ther. 2021, 21, 863–873. [Google Scholar] [CrossRef]
- Guerra, E.; Alberti, S. The anti-Trop-2 antibody-drug conjugate Sacituzumab Govitecan—Effectiveness, pitfalls and promises. Ann. Transl. Med. 2022, 10, 501. [Google Scholar] [CrossRef] [PubMed]
- Shi, F.; Liu, Y.; Zhou, X.; Shen, P.; Xue, R.; Zhang, M. Disitamab vedotin: A novel antibody-drug conjugates for cancer therapy. Drug Deliv. 2022, 29, 1335–1344. [Google Scholar] [CrossRef] [PubMed]
- Potti, A.; Ganti, A.K.; Tuchman, S.A.; Sholes, K.; Langness, E.; Koka, V.; Koch, M. HER-2/neu and CD117 (c-kit) overexpression in patients with pesticide exposure and extensive stage small cell lung carcinoma (ESSCLC). J. Carcinog. 2005, 4, 8. [Google Scholar] [CrossRef]
- Suzuki, S.; Arnold, L.L.; Pennington, K.L.; Chen, B.; Le, X.C.; Cohen, S.M. Effects of an epidermal growth factor receptor inhibitor on arsenic associated toxicity in the rat bladder epithelium. Toxicol. Lett. 2009, 187, 124–129. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, S.-D.; McCRUDDEN, C.; Chan, K.-W.; Lin, Y.; Kwok, H.-F. The prognostic significance of PD-L1 in bladder cancer. Oncol. Rep. 2015, 33, 3075–3084. [Google Scholar] [CrossRef]
- Stenehjem, D.D.; Tran, D.; Nkrumah, M.A.; Gupta, S. PD1/PDL1 inhibitors for the treatment of advanced urothelial bladder cancer. OncoTargets Ther. 2018, 11, 5973–5989. [Google Scholar] [CrossRef] [PubMed]
- Bellmunt, J.; Powles, T.; Vogelzang, N.J. A review on the evolution of PD-1/PD-L1 immunotherapy for bladder cancer: The future is now. Cancer Treat. Rev. 2017, 54, 58–67. [Google Scholar] [CrossRef]
- Zhou, Z.; Liu, Y.; Jiang, X.; Zheng, C.; Luo, W.; Xiang, X.; Qi, X.; Shen, J. Metformin modified chitosan as a multi-functional adjuvant to enhance cisplatin-based tumor chemotherapy efficacy. Int. J. Biol. Macromol. 2023, 224, 797–809. [Google Scholar] [CrossRef]
- Lee, G.-H.; Choi, K.-C. Adverse effects of pesticides on the functions of immune system. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2020, 235, 108789. [Google Scholar] [CrossRef]
- Ihlaseh, S.M.; Bailey, K.A.; Hester, S.D.; Jones, C.; Ren, H.; Cardoso, A.P.F.; Oliveira, M.L.C.S.; Wolf, D.C.; de Camargo, J.L.V. Transcriptional Profile of Diuron-Induced Toxicity on the Urinary Bladder of Male Wistar Rats to Inform Mode of Action. Toxicol. Sci. 2011, 122, 330–338. [Google Scholar] [CrossRef]
- Iatropoulos, M.; Duan, J.-D.; Schmuck, G.; Williams, G. The urinary bladder carcinogen propoxur does not produce genotoxic effects in the urinary bladder of Wistar male rats. Exp. Toxicol. Pathol. 2015, 67, 453–458. [Google Scholar] [CrossRef]
- Faba, O.R.; Palou-Redorta, J.; Fernández-Gómez, J.M.; Algaba, F.; Eiró, N.; Villavicencio, H.; Vizoso, F.J. Matrix Metalloproteinases and Bladder Cancer: What is New? ISRN Urol. 2012, 2012, 581539. [Google Scholar] [CrossRef]
- Fields, G.B. The Rebirth of Matrix Metalloproteinase Inhibitors: Moving Beyond the Dogma. Cells 2019, 8, 984. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.J.; Infante, J.R.; Janku, F.; Wong, D.J.L.; Sosman, J.A.; Keedy, V.; Patel, M.R.; Shapiro, G.I.; Mier, J.W.; Tolcher, A.W.; et al. First-in-Class ERK1/2 Inhibitor Ulixertinib (BVD-523) in Patients with MAPK Mutant Advanced Solid Tumors: Results of a Phase I Dose-Escalation and Expansion Study. Cancer Discov. 2018, 8, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Karlou, M.; Saetta, A.A.; Korkolopoulou, P.; Levidou, G.; Papanastasiou, P.; Boltetsou, E.; Isaiadis, D.; Pavlopoulos, P.; Thymara, I.; Thomas-Tsagli, E.; et al. Activation of extracellular regulated kinases (ERK1/2) predicts poor prognosis in urothelial bladder carcinoma and is not associated with B-Raf gene mutations. Pathology 2009, 41, 327–334. [Google Scholar] [CrossRef]
| Pesticide | Class | Structure | Potential Mode of Action | Reference |
|---|---|---|---|---|
| DDT | Insecticide |  | Oxidative stress, Xenoestrogen | [30,72,73] |
| Imazethapyr | Herbicide | 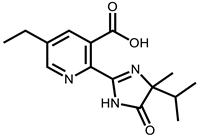 | DNA adducts | [30,74,75] |
| 2,4-Dichlorophenoxyacetic acid | Herbicide | 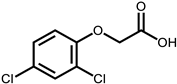 | Oxidative stress | [30,76,77] |
| Bentazon | Herbicide | 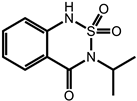 | Mechanisms unknown | [30] |
| Bromoxynil | Herbicide | 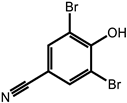 | Mechanisms unknown | [30] |
| Chloramben | Herbicide |  | Mechanisms unknown | [30] |
| Diclofop-methyl | Herbicide | 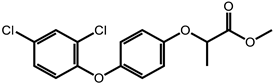 | Genotoxic | [30,78] |
| Imazaquin | Herbicide |  | Mechanisms unknown | [30] |
| Heptachlor | Insecticide | 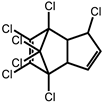 | Mechanisms unknown | [30] |
| Pesticide | Class | Cancer | Reference |
|---|---|---|---|
| Paraquat dichloride | Herbicide | Thyroid and Lung | [20,79] |
| Oxyfluorfen | Herbicide | Thyroid Cancer | [20] |
| Glyphosate | Herbicide | Thyroid Cancer, Glioblastoma | [20,80] |
| DDT | Insecticide | NHL, Prostate | [30,72,73] |
| Lindane | Insecticide | NHL, Prostate | [26,72] |
| Permethrin | Insecticide | NHL | [73] |
| Diazinon | Insecticide | NHL, Lung | [73,81] |
| Terbufos | Insecticide and Nematicide | NHL | [73] |
| Captafol | Fungicide | NHL | [82] |
| Simazine | Herbicide | Prostate | [72] |
| (Dithio/Thio)-carbamates | Fungicide | CNS Cancers | [83,84] |
| Imazethapyr | Herbicide | Colon | [30,74] |
| Cyhalothrin | Insecticide | DNA damage inducing | [60] |
| Endosulfan | Insecticide and Acaricide | Renal cancer, DNA damage inducing | [60,85] |
| Deltamethrin | Insecticide | Glioblastoma, DNA damage inducing | [60,80] |
| Polychlorinated biphenyls | Insecticide | Breast Cancer | [86] |
| Acetochlor | Herbicide | Lung Cancer | [87] |
| Malathion | Insecticide | Breast Cancer | [88] |
| Propoxur | Insecticide | Breast Cancer | [89] |
| Chlorpyrifos | Insecticide and Acaracide | Breast Cancer, Glioblastoma, Lung | [80,90,91] |
| Atrazine | Herbicide | Prostate Cancer | [92] |
| Pentachlorophenol | Termiticide, Fungicide, Herbicide, Molluscicide, Disinfectant | Lung, Liver | [93] |
| Metiram | Fungicide | Glioblastoma | [80] |
| EPTC | Herbicide | Pancreas, Colon | [94,95] |
| Dicamba | Herbicide | Lung, colon | [96] |
| Dieldrin | Insecticide | Lung | [97] |
| Metolachlor | Herbicide | Lung | [96] |
| Pendimethalin | Herbicide | Lung, Colon | [98] |
| Trifluralin | Herbicide | Colon | [99] |
| Chlordane | Insecticide (termiticide) | Colon, Leukemia, Prostate | [97,100] |
| Toxaphene | Insecticide | Colon, Melanoma | [91,97] |
| Fonofos | Insecticide and selective acaricide | Leukemia | [101] |
| Alachlor | Herbicide | Lymphoma | [102] |
| Aldicarb | Insecticide | Colon | [91] |
| Parathion | Insecticide and Miticide | Melanoma | [103] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucchesi, C.A.; Vasilatis, D.M.; Mantrala, S.; Chandrasekar, T.; Mudryj, M.; Ghosh, P.M. Pesticides and Bladder Cancer: Mechanisms Leading to Anti-Cancer Drug Chemoresistance and New Chemosensitization Strategies. Int. J. Mol. Sci. 2023, 24, 11395. https://doi.org/10.3390/ijms241411395
Lucchesi CA, Vasilatis DM, Mantrala S, Chandrasekar T, Mudryj M, Ghosh PM. Pesticides and Bladder Cancer: Mechanisms Leading to Anti-Cancer Drug Chemoresistance and New Chemosensitization Strategies. International Journal of Molecular Sciences. 2023; 24(14):11395. https://doi.org/10.3390/ijms241411395
Chicago/Turabian StyleLucchesi, Christopher A., Demitria M. Vasilatis, Saisamkalpa Mantrala, Thenappan Chandrasekar, Maria Mudryj, and Paramita M. Ghosh. 2023. "Pesticides and Bladder Cancer: Mechanisms Leading to Anti-Cancer Drug Chemoresistance and New Chemosensitization Strategies" International Journal of Molecular Sciences 24, no. 14: 11395. https://doi.org/10.3390/ijms241411395
APA StyleLucchesi, C. A., Vasilatis, D. M., Mantrala, S., Chandrasekar, T., Mudryj, M., & Ghosh, P. M. (2023). Pesticides and Bladder Cancer: Mechanisms Leading to Anti-Cancer Drug Chemoresistance and New Chemosensitization Strategies. International Journal of Molecular Sciences, 24(14), 11395. https://doi.org/10.3390/ijms241411395







