The Yin and Yang of Breast Cancer: Ion Channels as Determinants of Left–Right Functional Differences
Abstract
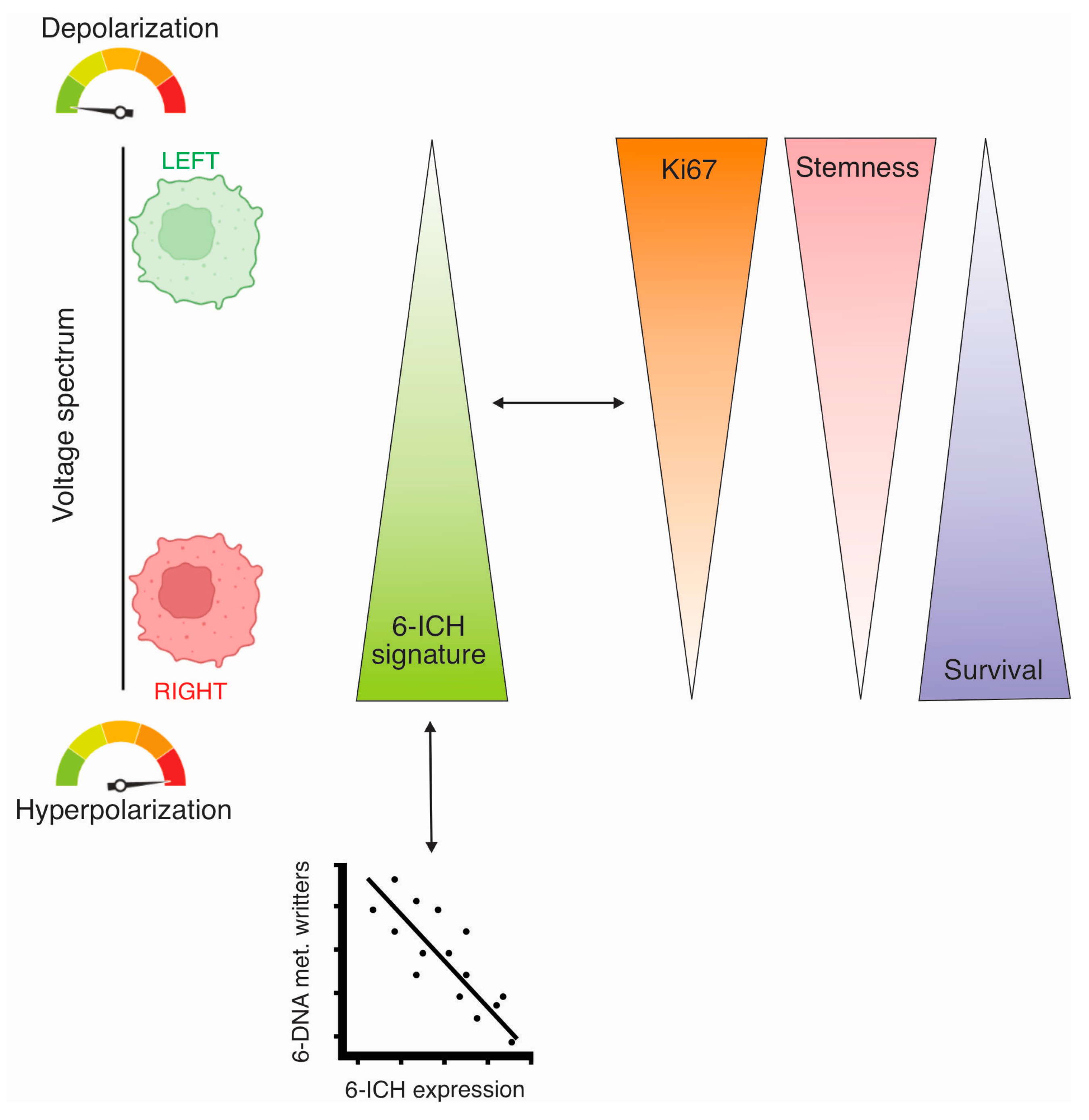
1. Introduction
2. Results
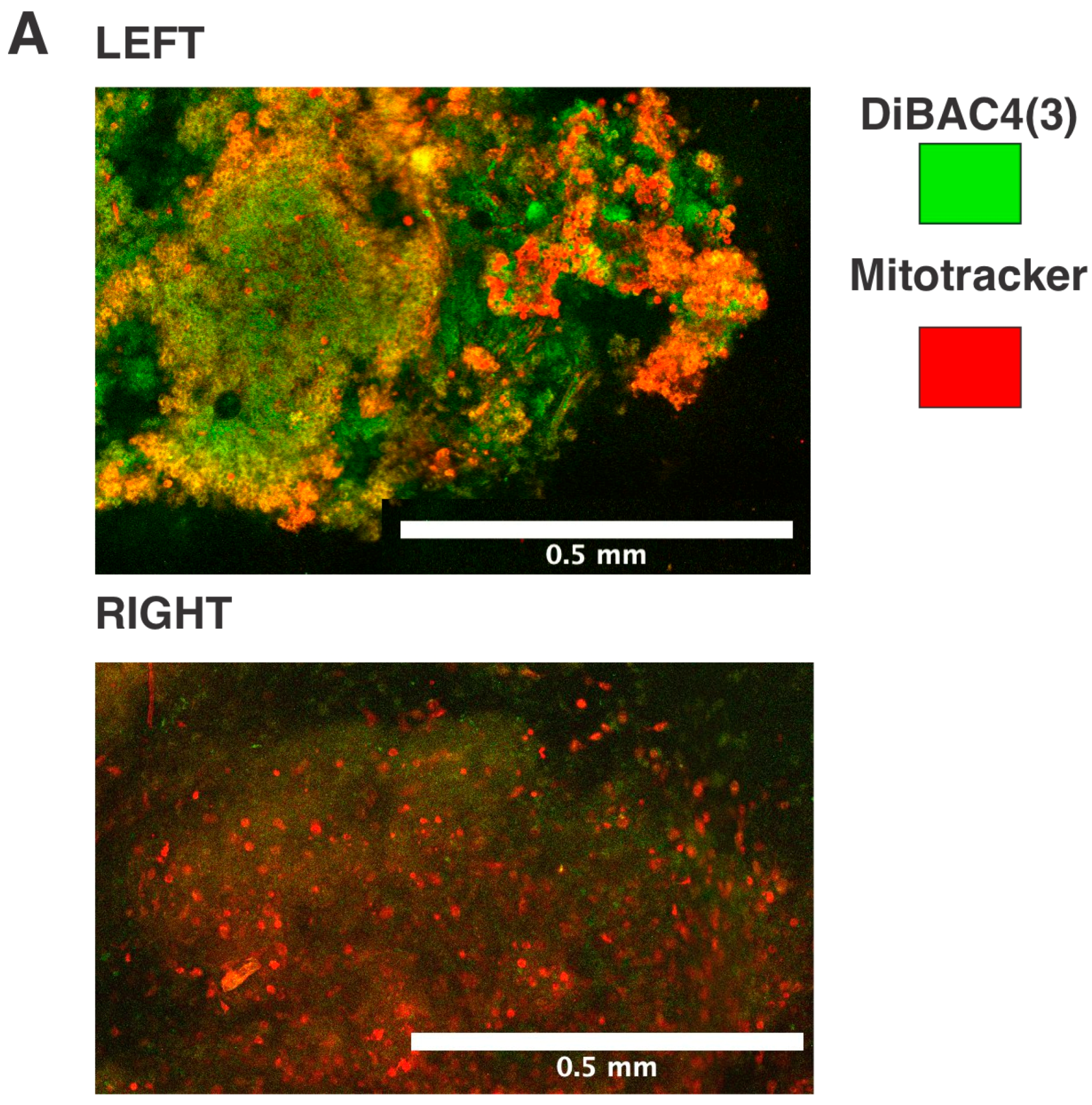
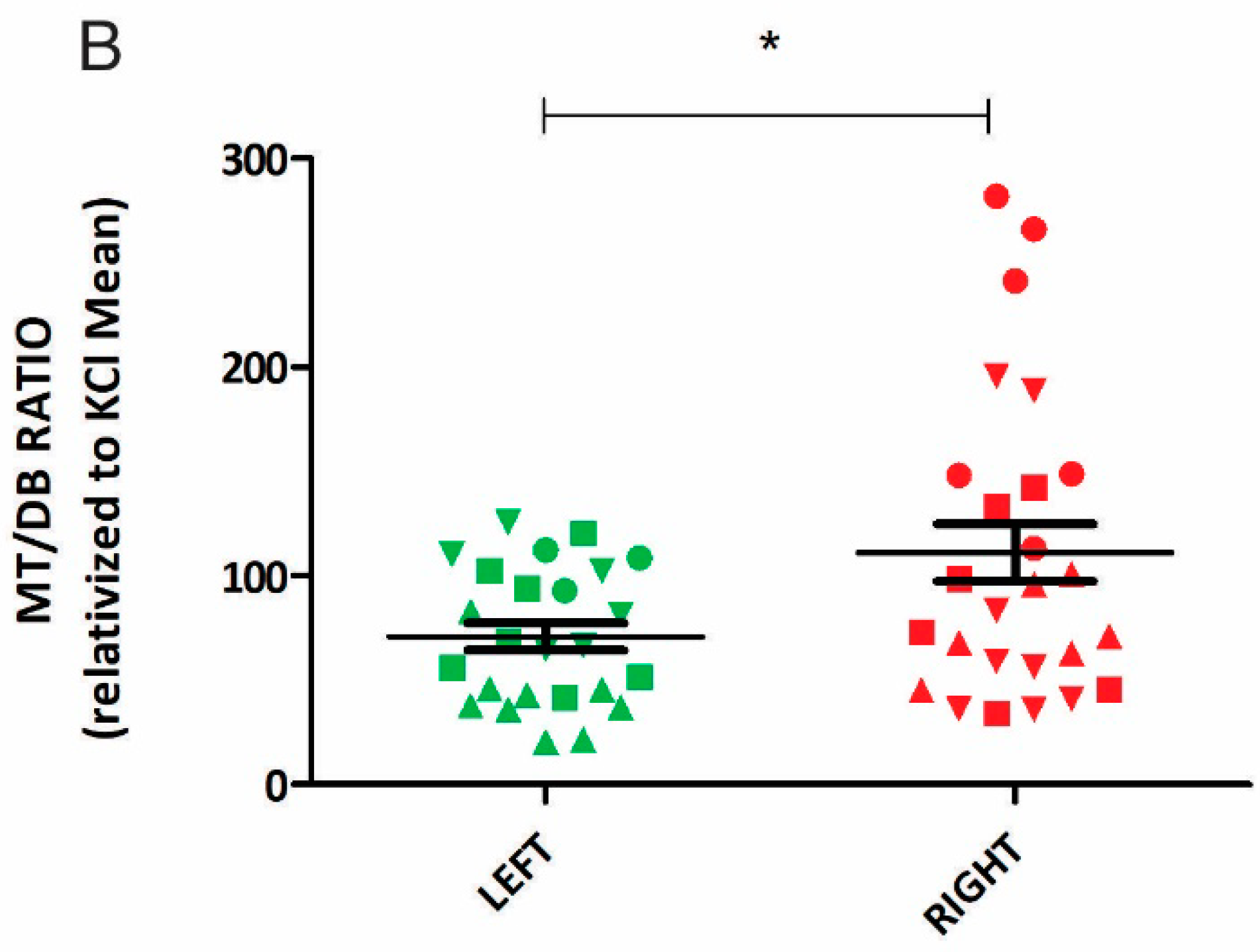
2.1. Left-Sided Mice Tumors Exhibit Greater Depolarization
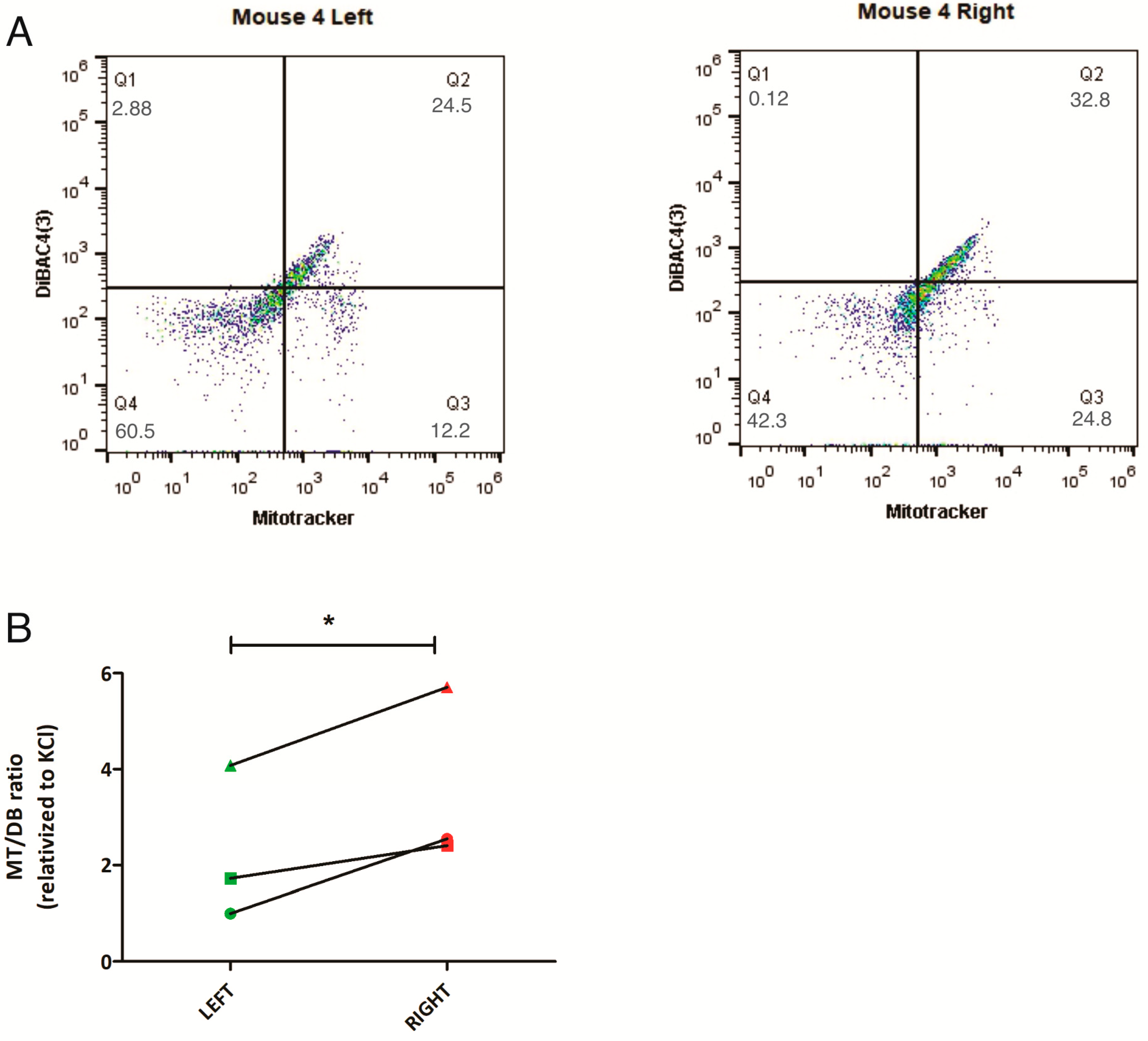
2.2. Bioinformatic Approach: ICH Gene Signature Involved in L-R Bioelectric Differences
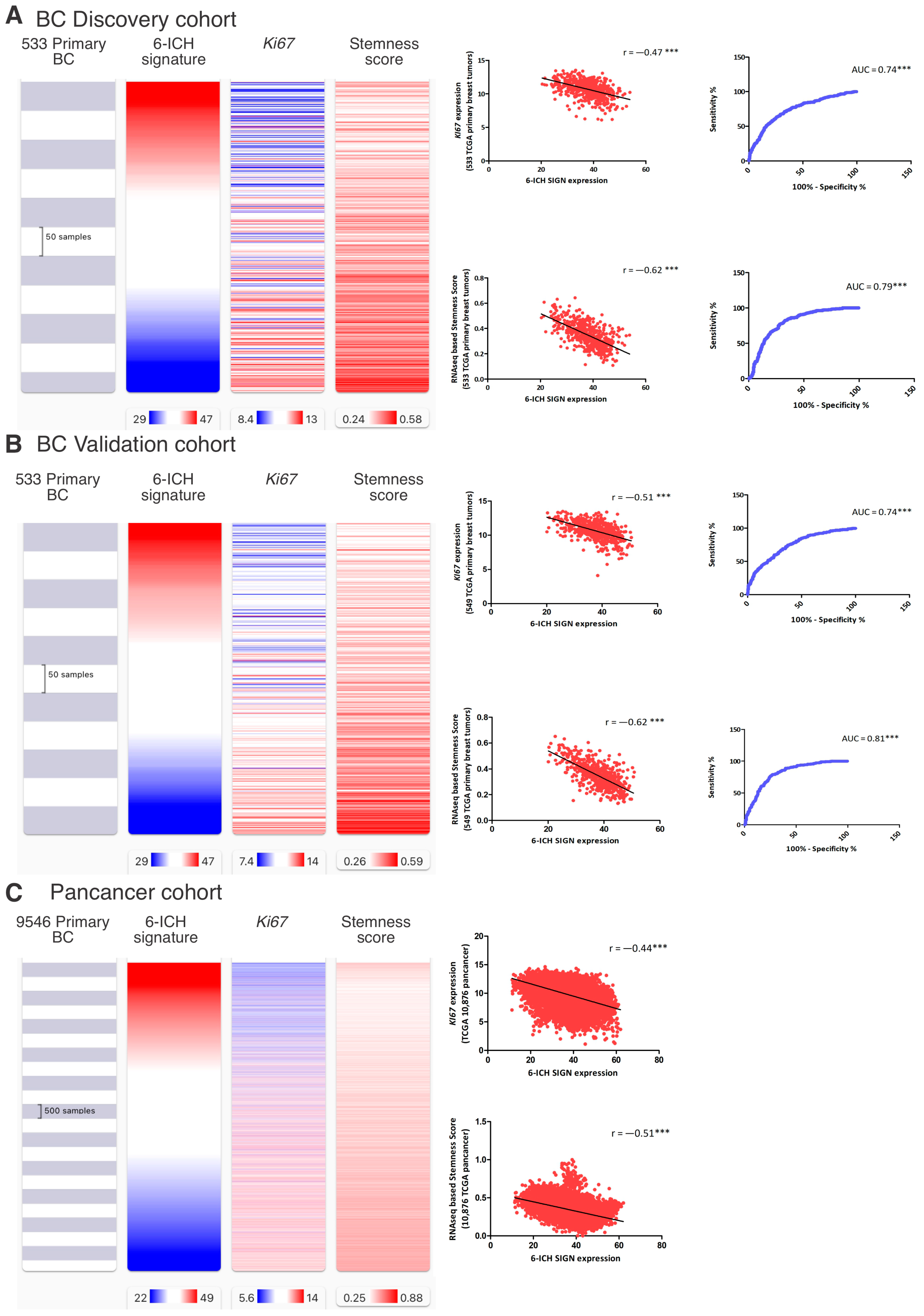
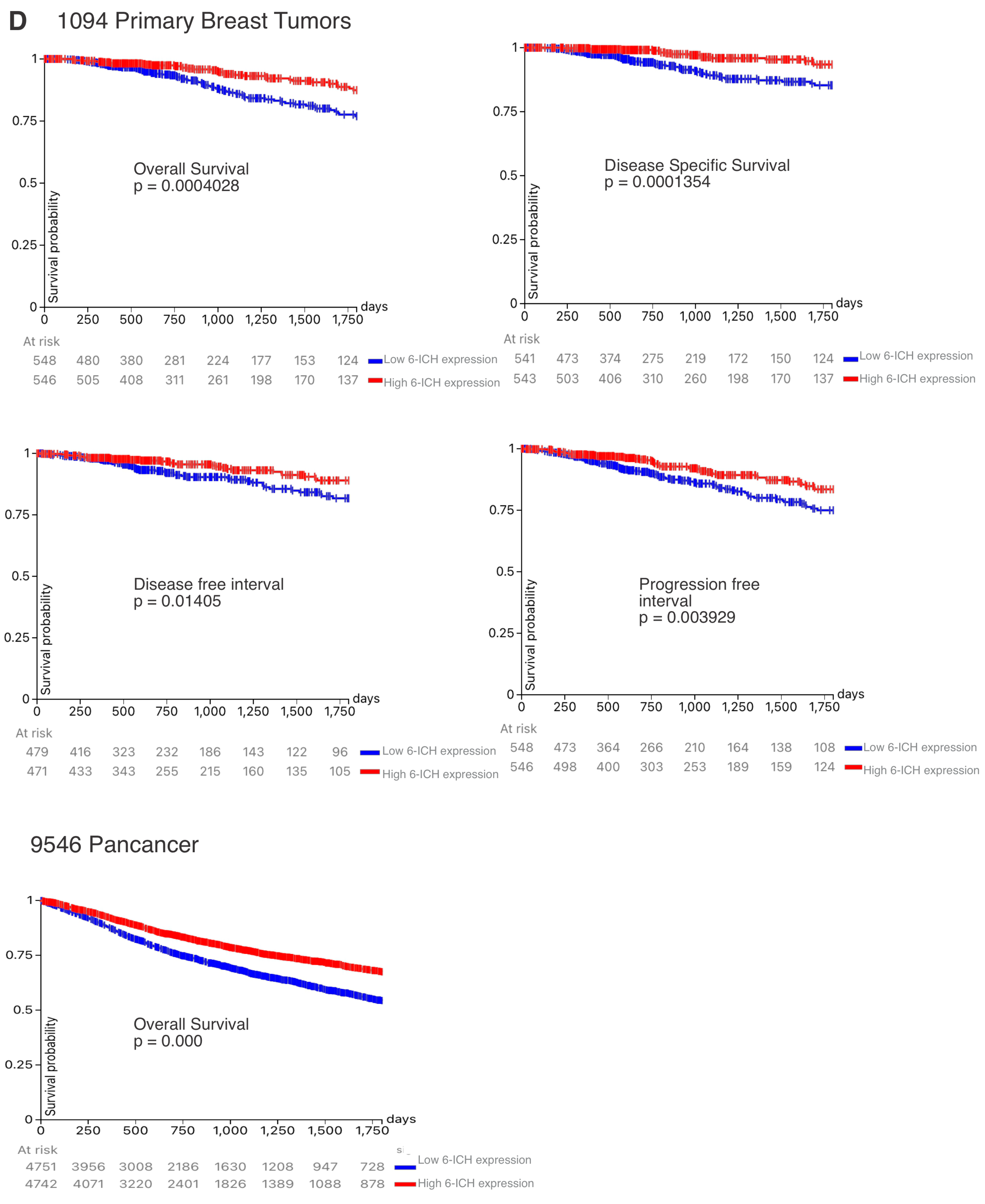
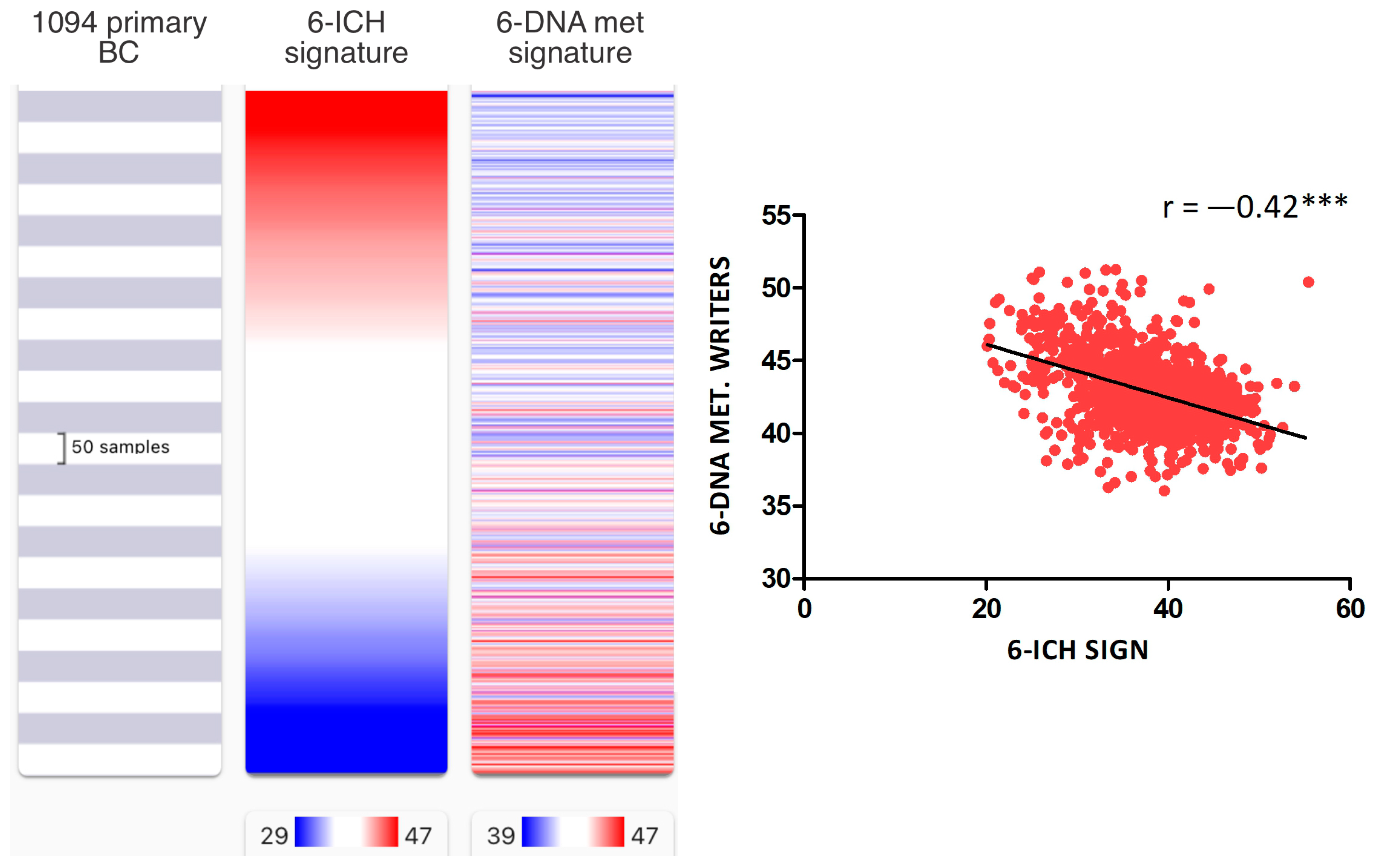
2.3. In Silico: The 6-ICH Signature Inversely Correlates with Pro-Mitotic and Stemness Markers and Survival Rates
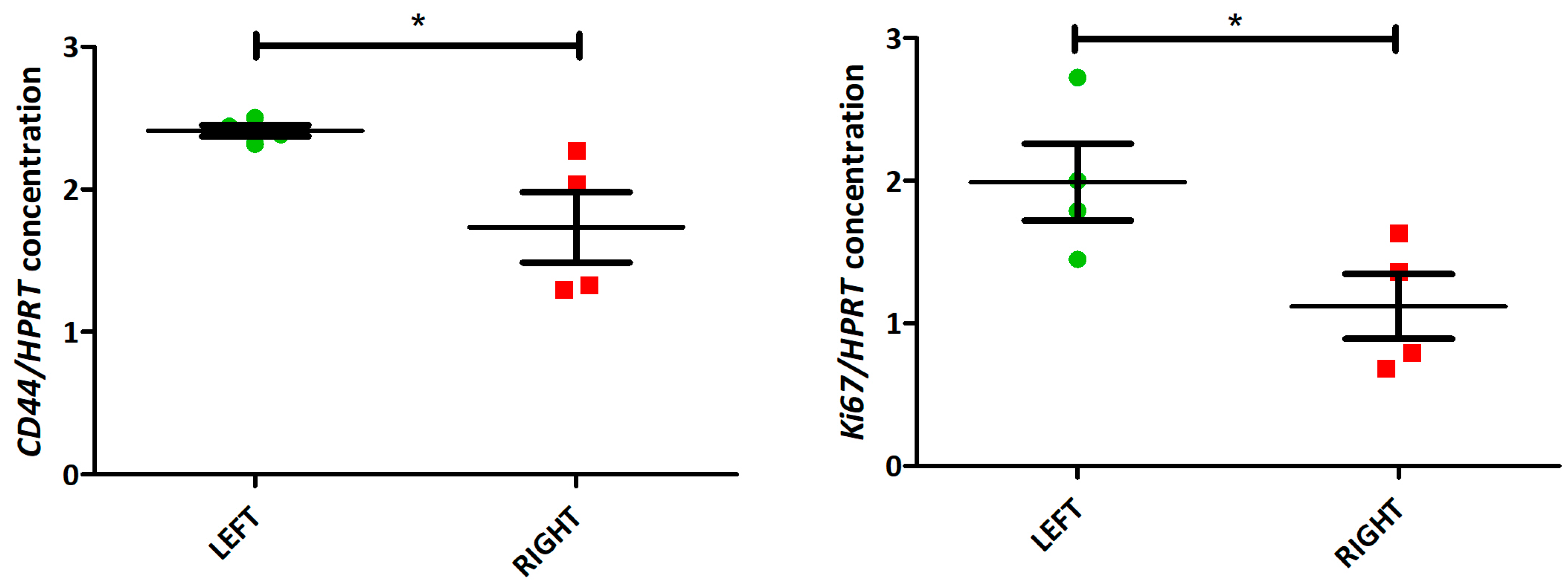
2.4. In Vivo: The 6-ICH Signature Inversely Correlates with Proliferation Marker and Stemness Scores
3. Discussion
4. Methods
4.1. Human Primary Breast Tumors
4.2. Mouse Model MMTV-PYMT
4.3. Membrane Potential Measured by Flow Cytometry
4.4. Membrane Potential Measured by Confocal Microscopy
4.5. RNA Extraction
4.6. Gene Expression Analysis in Mice Tumors by Droplet Digital PCR (ddPCR)
4.7. Gene Expression Analysis in Human Tumors by qPCR
4.8. Public Datasets and Platforms Used
4.9. Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fields, C.; Levin, M. Competency in Navigating Arbitrary Spaces as an Invariant for Analyzing Cognition in Diverse Embodiments. Entropy 2022, 24, 819. [Google Scholar] [CrossRef] [PubMed]
- Mathews, J.; Levin, M. Gap Junctional Signaling in Pattern Regulation: Physiological Network Connectivity Instructs Growth and Form. Dev. Neurobiol. 2017, 77, 643–673. [Google Scholar] [CrossRef] [PubMed]
- Hirata, E.; Sahai, E. Tumor Microenvironment and Differential Responses to Therapy. Cold Spring Harb. Perspect. Med. 2017, 7, a026781. [Google Scholar] [CrossRef]
- Blackiston, D.; Adams, D.S.; Lemire, J.M.; Lobikin, M.; Levin, M. Transmembrane Potential of GlyCl-Expressing Instructor Cells Induces a Neoplastic-like Conversion of Melanocytes via a Serotonergic Pathway. Dis. Model. Mech. 2011, 4, 67–85. [Google Scholar] [CrossRef] [PubMed]
- Morokuma, J.; Blackiston, D.; Adams, D.S.; Seebohm, G.; Trimmer, B.; Levin, M. Modulation of Potassium Channel Function Confers a Hyperproliferative Invasive Phenotype on Embryonic Stem Cells. Proc. Natl. Acad. Sci. USA 2008, 105, 16608–16613. [Google Scholar] [CrossRef] [PubMed]
- Trigos, A.S.; Pearson, R.B.; Papenfuss, A.T.; Goode, D.L. Altered Interactions between Unicellular and Multicellular Genes Drive Hallmarks of Transformation in a Diverse Range of Solid Tumors. Proc. Natl. Acad. Sci. USA 2017, 114, 6406–6411. [Google Scholar] [CrossRef]
- Levin, M. Bioelectrical Approaches to Cancer as a Problem of the Scaling of the Cellular Self. Prog. Biophys. Mol. Biol. 2021, 165, 102–113. [Google Scholar] [CrossRef]
- Chernet, B.T.; Levin, M. Transmembrane Voltage Potential Is an Essential Cellular Parameter for the Detection and Control of Tumor Development in a Xenopus Model. Dis. Model. Mech. 2013, 6, 595–607. [Google Scholar] [CrossRef]
- Mathews, J.; Kuchling, F.; Baez-Nieto, D.; Diberardinis, M.; Pan, J.Q.; Levin, M. Ion Channel Drugs Suppress Cancer Phenotype in NG108-15 and U87 Cells: Toward Novel Electroceuticals for Glioblastoma. Cancers 2022, 14, 1499. [Google Scholar] [CrossRef]
- Arcangeli, A.; Crociani, O.; Bencini, L. Interaction of Tumour Cells with Their Microenvironment: Ion Channels and Cell Adhesion Molecules. A Focus on Pancreatic Cancer. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130101. [Google Scholar] [CrossRef]
- Arcangeli, A. Ion Channels and Transporters in Cancer. 3. Ion Channels in the Tumor Cell-Microenvironment Cross Talk. Am. J. Physiol. Cell Physiol. 2011, 301, C762–C771. [Google Scholar] [CrossRef]
- Lanni, J.S.; Peal, D.; Ekstrom, L.; Chen, H.; Stanclift, C.; Bowen, M.E.; Mercado, A.; Gamba, G.; Kahle, K.T.; Harris, M.P. Integrated K+ Channel and K+Cl- Cotransporter Functions Are Required for the Coordination of Size and Proportion during Development. Dev. Biol. 2019, 456, 164–178. [Google Scholar] [CrossRef]
- Srivastava, P.; Kane, A.; Harrison, C.; Levin, M. A Meta-Analysis of Bioelectric Data in Cancer, Embryogenesis, and Regeneration. Bioelectricity 2020, 3, 42–67. [Google Scholar] [CrossRef]
- Prevarskaya, N.; Skryma, R.; Shuba, Y. Ion Channels in Cancer: Are Cancer Hallmarks Oncochannelopathies? Physiol. Rev. 2018, 98, 559–621. [Google Scholar] [CrossRef]
- Perkins, C.I.; Hotes, J.; Kohler, B.A.; Howe, H.L. Association between Breast Cancer Laterality and Tumor Location, United States, 1994–1998. Cancer Causes Control 2004, 15, 637–645. [Google Scholar] [CrossRef]
- Petitprez, F.; Sun, C.M.; Lacroix, L.; Sautès-Fridman, C.; de Reyniès, A.; Fridman, W.H. Quantitative Analyses of the Tumor Microenvironment Composition and Orientation in the Era of Precision Medicine. Front. Oncol. 2018, 8, 390. [Google Scholar] [CrossRef]
- Levin, M.; Klar, A.J.S.; Ramsdell, A.F. Introduction to Provocative Questions in Left–Right Asymmetry. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150399. [Google Scholar] [CrossRef] [PubMed]
- Levin, M.; Thorlin, T.; Robinson, K.R.; Nogi, T.; Mercola, M. Asymmetries in H+/K+-ATPase and Cell Membrane Potentials Comprise a Very Early Step in Left-Right Patterning. Cell 2002, 111, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Hu, C.; Zhou, Y.; Cui, C.; Yang, J.; Cui, Q. MicroRNA Profiling in Paired Left and Right Eyes, Lungs, and Testes of Normal Mice. Mol. Ther. Nucleic Acids 2020, 21, 687–695. [Google Scholar] [CrossRef]
- Sughrue, T.; Brody, J.P. Breast Tumor Laterality in the United States Depends upon the Country of Birth, but Not Race. PLoS ONE 2014, 9, e103313. [Google Scholar] [CrossRef] [PubMed]
- Titus-Ernstoff, L.; Newcomb, P.A.; Egan, K.M.; Baron, J.A.; Greenberg, E.R.; Trichopoulos, D.; Willett, W.C.; Stampfer, M.J. Left-Handedness in Relation to Breast Cancer Risk in Postmenopausal Women. Epidemiology 2000, 11, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Roychoudhuri, R.; Putcha, V.; Møller, H. Cancer and Laterality: A Study of the Five Major Paired Organs (UK). Cancer Causes Control 2006, 17, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.; Yu, K.D.; Jiang, Y.Z.; Shao, Z.M.; Di, G.H. The Effect of Laterality and Primary Tumor Site on Cancer-Specific Mortality in Breast Cancer: A SEER Population-Based Study. PLoS ONE 2014, 9, e94815. [Google Scholar] [CrossRef] [PubMed]
- Mittwoch, U. Different Gene Expressions on the Left and the Right: A Genotype/Phenotype Mismatch in Need of Attention. Ann. Hum. Genet. 2008, 72, 2–9. [Google Scholar] [CrossRef]
- Robichaux, J.P.; Hallett, R.M.; Fuseler, J.W.; Hassell, J.A.; Ramsdell, A.F. Mammary Glands Exhibit Molecular Laterality and Undergo Left-Right Asymmetric Ductal Epithelial Growth in MMTV-CNeu Mice. Oncogene 2015, 34, 2003–2010. [Google Scholar] [CrossRef]
- Huang, Y.; Duanmu, J.; Liu, Y.; Yan, M.; Li, T.; Jiang, Q. Analysis of Multi-Omics Differences in Left-Side and Right-Side Colon Cancer. PeerJ 2021, 9, e11433. [Google Scholar] [CrossRef]
- Zhang, L.; Zhao, Y.; Dai, Y.; Cheng, J.N.; Gong, Z.; Feng, Y.; Sun, C.; Jia, Q.; Zhu, B. Immune Landscape of Colorectal Cancer Tumor Microenvironment from Different Primary Tumor Location. Front. Immunol. 2018, 9, 1578. [Google Scholar] [CrossRef]
- Abdou, Y.; Gupta, M.; Asaoka, M.; Attwood, K.; Mateusz, O.; Gandhi, S.; Takabe, K. Left Sided Breast Cancer Is Associated with Aggressive Biology and Worse Outcomes than Right Sided Breast Cancer. Sci. Rep. 2022, 12, 13377. [Google Scholar] [CrossRef]
- Al Saad, S.; Al Shenawi, H.; Almarabheh, A.; Al Shenawi, N.; Mohamed, A.I.; Yaghan, R. Is Laterality in Breast Cancer Still Worth Studying? Local Experience in Bahrain. BMC Cancer 2022, 22, 968. [Google Scholar] [CrossRef]
- Campoy, E.M.; Laurito, S.R.; Branham, M.T.; Urrutia, G.; Mathison, A.; Gago, F.; Orozco, J.; Urrutia, R.; Mayorga, L.S.; Roqué, M. Asymmetric Cancer Hallmarks in Breast Tumors on Different Sides of the Body. PLoS ONE 2016, 11, e157416. [Google Scholar] [CrossRef]
- Masuelli, S.; Real, S.; Campoy, E.; Branham, M.T.; Marzese, D.M.; Salomon, M.; De Blas, G.; Arias, R.; Levin, M.; Roque, M. Correction to: When Left Does Not Seem Right: Epigenetic and Bioelectric Differences between Left and Right-sided Breast Cancer (Molecular Medicine, (2022), 28, 1, (15), 10.1186/S10020-022-00440-5). Mol. Med. 2022, 28, 10020. [Google Scholar] [CrossRef]
- Goldman, M.J.; Craft, B.; Hastie, M.; Repečka, K.; McDade, F.; Kamath, A.; Banerjee, A.; Luo, Y.; Rogers, D.; Brooks, A.N.; et al. Visualizing and Interpreting Cancer Genomics Data via the Xena Platform. Nat. Biotechnol. 2020, 38, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Malta, T.M.; Sokolov, A.; Gentles, A.J.; Burzykowski, T.; Poisson, L.; Weinstein, J.N.; Kamińska, B.; Huelsken, J.; Omberg, L.; Gevaert, O.; et al. Machine Learning Identifies Stemness Features Associated with Oncogenic Dedifferentiation. Cell 2018, 173, 338–354. [Google Scholar] [CrossRef] [PubMed]
- Nolan, E.; Lindeman, G.J.; Visvader, J.E. Deciphering Breast Cancer: From Biology to the Clinic. Cell 2023, 186, 1708–1728. [Google Scholar] [CrossRef]
- Ma, K. Embryonic Left-Right Separation Mechanism Allows Confinement of Mutation-Induced Phenotypes to One Lateral Body Half of Bilaterians. Am. J. Med. Genet. Part A 2013, 161, 3095–3114. [Google Scholar] [CrossRef] [PubMed]
- Onjiko, R.M.; Morris, S.E.; Moody, S.A.; Nemes, P. Single-Cell Mass Spectrometry with Multi-Solvent Extraction Identifies Metabolic Differences between Left and Right Blastomeres in the 8-Cell Frog (Xenopus) Embryo. Analyst 2016, 141, 3648–3656. [Google Scholar] [CrossRef]
- Monsoro-Burq, A.H.; Levin, M. Avian Models and the Study of Invariant Asymmetry: How the Chicken and the Egg Taught Us to Tell Right from Left. Int. J. Dev. Biol. 2018, 62, 63–77. [Google Scholar] [CrossRef]
- Robichaux, J.P.; Fuseler, J.W.; Patel, S.S.; Kubalak, S.W.; Hartstone-Rose, A.; Ramsdell, A.F. Left-Right Analysis of Mammary Gland Development in Retinoid X Receptor-A+/- Mice. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2016, 371, 2015041. [Google Scholar] [CrossRef]
- Busk, T.; Clemmesen, J. The Frequencies of Left- and Right-Sided Breast Cancer. Br. J. Cancer 1947, 1, 345–351. [Google Scholar] [CrossRef]
- Karunasekara, Y.; Dulhunty, A.F.; Casarotto, M.G. The Voltage-Gated Calcium-Channel Beta Subunit: More than Just an Accessory. Eur. Biophys. J. 2009, 39, 75–81. [Google Scholar] [CrossRef]
- Rizvi, S.; Raza, S.T.; Rahman, Q.; Mahdi, F. Role of GNB3, NET, KCNJ11, TCF7L2 and GRL Genes Single Nucleotide Polymorphism in the Risk Prediction of Type 2 Diabetes Mellitus. 3 Biotech 2016, 6, 255. [Google Scholar] [CrossRef] [PubMed]
- Payne, S.L.; Ram, P.; Srinivasan, D.H.; Le, T.T.; Levin, M.; Oudin, M.J. Potassium Channel-Driven Bioelectric Signalling Regulates Metastasis in Triple-Negative Breast Cancer. EBioMedicine 2022, 75, 103767. [Google Scholar] [CrossRef]
- Luiz, A.P.; Wood, J.N. Sodium Channels in Pain and Cancer: New Therapeutic Opportunities. Adv. Pharmacol. 2016, 75, 153–178. [Google Scholar] [CrossRef] [PubMed]
- Leslie, T.K.; Brackenbury, W.J. Sodium Channels and the Ionic Microenvironment of Breast Tumours. J. Physiol. 2023, 601, 1543–1553. [Google Scholar] [CrossRef]
- Blackiston, D.J.; McLaughlin, K.A.; Levin, M. Bioelectric Controls of Cell Proliferation: Ion Channels, Membrane Voltage and the Cell Cycle. Cell Cycle 2009, 8, 3527–3536. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Brackenbury, W.J. Membrane Potential and Cancer Progression. Front. Physiol. 2013, 4, 185. [Google Scholar] [CrossRef]
- Binggeli, R.; Weinstein, R.C. Membrane Potentials and Sodium Channels: Hypotheses for Growth Regulation and Cancer Formation Based on Changes in Sodium Channels and Gap Junctions. J. Theor. Biol. 1986, 123, 377–401. [Google Scholar] [CrossRef]
- Sundelacruz, S.; Levin, M.; Kaplan, D.L. Depolarization Alters Phenotype, Maintains Plasticity of Predifferentiated Mesenchymal Stem Cells. Tissue Eng. Part A 2013, 19, 1889–1908. [Google Scholar] [CrossRef]
- Visvader, J.E.; Lindeman, G.J. Cancer Stem Cells: Current Status and Evolving Complexities. Cell Stem Cell 2012, 10, 717–728. [Google Scholar] [CrossRef]
- Lashen, A.G.; Toss, M.S.; Ghannam, S.F.; Makhlouf, S.; Green, A.; Mongan, N.P.; Rakha, E. Expression, Assessment and Significance of Ki67 Expression in Breast Cancer: An Update. J. Clin. Pathol. 2023, 76, 357–364. [Google Scholar] [CrossRef]
- Place, A.E.; Jin Huh, S.; Polyak, K. The Microenvironment in Breast Cancer Progression: Biology and Implications for Treatment. Breast Cancer Res. 2011, 13, 227. [Google Scholar] [CrossRef]
- Flavahan, W.A.; Gaskell, E.; Bernstein, B.E. Epigenetic Plasticity and the Hallmarks of Cancer. Science 2017, 357, eaal2380. [Google Scholar] [CrossRef]
- Błaszczyk, M.; Kozioł, A.; Palko-Łabuz, A.; Środa-Pomianek, K.; Wesołowska, O. Modulators of Cellular Cholesterol Homeostasis as Antiproliferative and Model Membranes Perturbing Agents. Biochim. Biophys. Acta Biomembr. 2023, 1865, 184163. [Google Scholar] [CrossRef] [PubMed]
- Wills, R.C.; Hammond, G.R.V. PI(4,5)P2: Signaling the Plasma Membrane. Biochem. J. 2022, 479, 2311–2325. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Zaman, M.K.; Das, S.; Goyary, D.; Pathak, M.P.; Chattopadhyay, P. Transient Receptor Potential Vanilloid (TRPV4) Channel Inhibition: A Novel Promising Approach for the Treatment of Lung Diseases. Biomed. Pharmacother. 2023, 163, 114861. [Google Scholar] [CrossRef]
- Pantziarka, P.; Verbaanderd, C.; Sukhatme, V.; Rica Capistrano, I.; Crispino, S.; Gyawali, B.; Rooman, I.; Van Nuffel, A.M.T.; Meheus, L.; Sukhatme, V.P.; et al. ReDO_DB: The Repurposing Drugs in Oncology Database. Ecancermedicalscience 2018, 12, 886. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Awasthi, R.; Malviya, R. Bioelectronic Medicines: Therapeutic Potential and Advancements in next-Generation Cancer Therapy. Biochim. Biophys. Acta Rev. Cancer 2022, 1877, 188808. [Google Scholar] [CrossRef]
- Marzese, D.M.; Hoon, D.S.; Chong, K.K.; Gago, F.E.; Orozco, J.I.; Tello, O.M.; Vargas-Roig, L.M.; Roque, M. DNA Methylation Index and Methylation Profile of Invasive Ductal Breast Tumors. J. Mol. Diagn. 2012, 14, 613–622. [Google Scholar] [CrossRef]
- Mandalà, M.; Serck-Hanssen, G.; Martino, G.; Helle, K.B. The Fluorescent Cationic Dye Rhodamine 6G as a Probe for Membrane Potential in Bovine Aortic Endothelial Cells. Anal. Biochem. 1999, 274, 1–6. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masuelli, S.; Real, S.; McMillen, P.; Oudin, M.; Levin, M.; Roqué, M. The Yin and Yang of Breast Cancer: Ion Channels as Determinants of Left–Right Functional Differences. Int. J. Mol. Sci. 2023, 24, 11121. https://doi.org/10.3390/ijms241311121
Masuelli S, Real S, McMillen P, Oudin M, Levin M, Roqué M. The Yin and Yang of Breast Cancer: Ion Channels as Determinants of Left–Right Functional Differences. International Journal of Molecular Sciences. 2023; 24(13):11121. https://doi.org/10.3390/ijms241311121
Chicago/Turabian StyleMasuelli, Sofía, Sebastián Real, Patrick McMillen, Madeleine Oudin, Michael Levin, and María Roqué. 2023. "The Yin and Yang of Breast Cancer: Ion Channels as Determinants of Left–Right Functional Differences" International Journal of Molecular Sciences 24, no. 13: 11121. https://doi.org/10.3390/ijms241311121
APA StyleMasuelli, S., Real, S., McMillen, P., Oudin, M., Levin, M., & Roqué, M. (2023). The Yin and Yang of Breast Cancer: Ion Channels as Determinants of Left–Right Functional Differences. International Journal of Molecular Sciences, 24(13), 11121. https://doi.org/10.3390/ijms241311121







