TNAP and P2X7R: New Plasma Biomarkers for Alzheimer’s Disease
Abstract
1. Introduction
2. Results
2.1. Study Population Characteristics
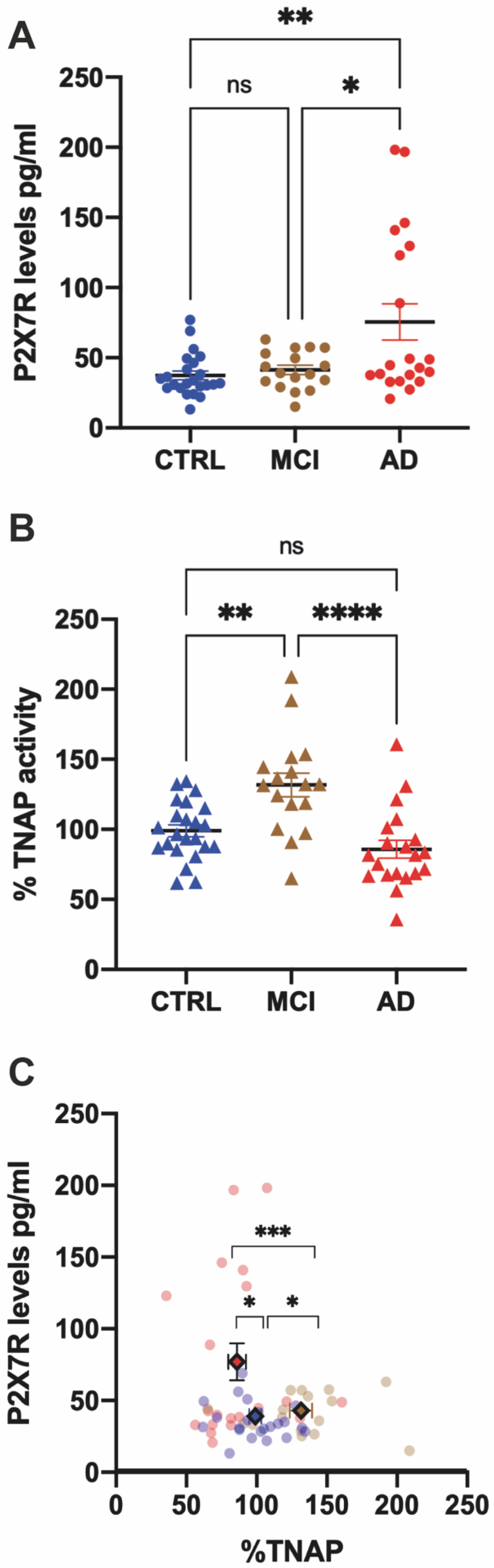
2.2. P2X7R Plasma Levels Are Increased in AD but Not in MCI Patients
2.3. TNAP Activity Is Increased in MCI but Not in AD Patients
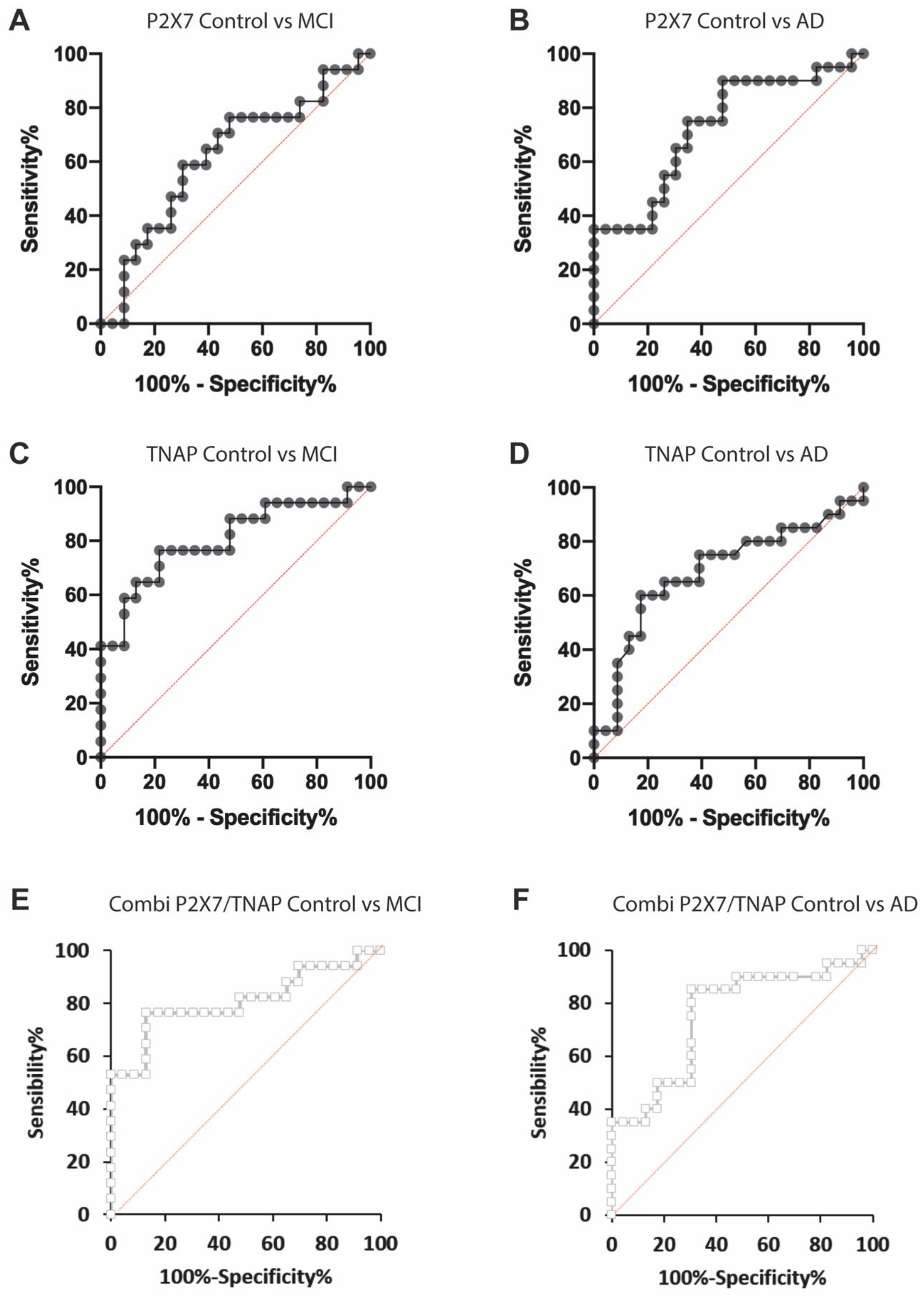
2.4. Measuring Both P2X7R and TNAP Activity Has a Reasonable Discrimination Capability to Diagnose MCI and AD Conditions
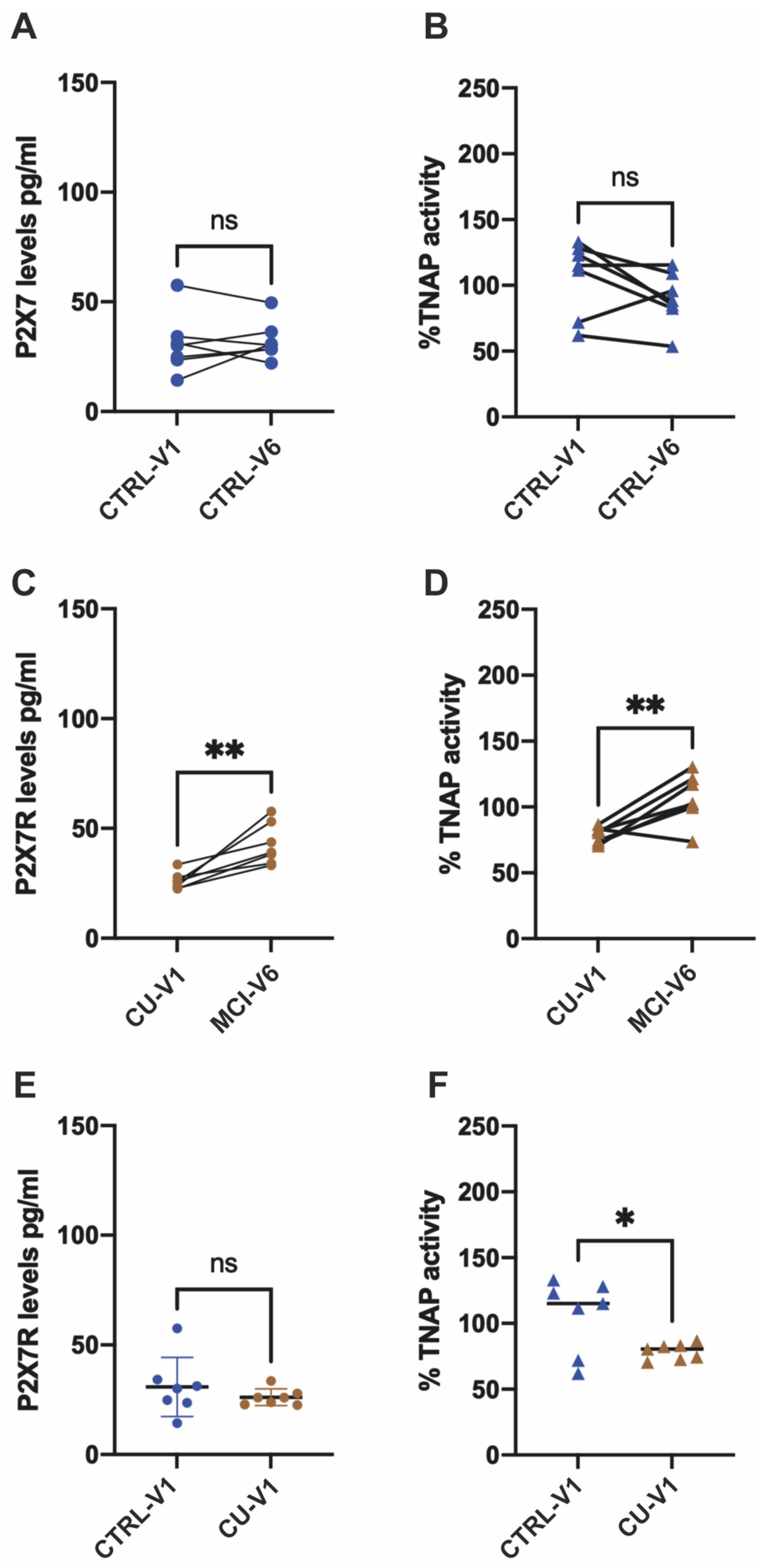
2.5. Longitudinal Studies Confirm That Patients Progressing to MCI Condition Experience Changes in Their Plasma TNAP Activity and P2X7 Levels
3. Discussion
4. Materials and Methods
4.1. Human Subjects/Participants
4.2. Neurological and Neuropsychological Assessments
4.3. Neuroimaging
4.4. Human Blood Sample Collection
4.5. APOE Genotyping
4.6. ELISA
4.7. TNAP Activity
4.8. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anonymous. 2022 Alzheimer’s disease facts and figures. Alzheimers Dement 2022, 18, 700–789. [Google Scholar]
- Selkoe, D.J. Alzheimer’s disease: Genes, proteins, and therapy. Physiol. Rev. 2001, 81, 741–766. [Google Scholar] [CrossRef] [PubMed]
- Avila, J. Tau protein, the main component of paired helical filaments. J. Alzheimers Dis. 2006, 9, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Dubois, B.; Feldman, H.H.; Jacova, C.; Hampel, H.; Molinuevo, J.L.; Blennow, K.; DeKosky, S.T.; Gauthier, S.; Selkoe, D.; Bateman, R.; et al. Advancing research diagnostic criteria for Alzheimer’s disease: The IWG-2 criteria. Lancet. Neurol. 2014, 13, 614–629. [Google Scholar] [CrossRef]
- Jack, C.R., Jr.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlein, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Karlawish, J.; et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement 2018, 14, 535–562. [Google Scholar] [CrossRef]
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R., Jr.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 2011, 7, 263–269. [Google Scholar] [CrossRef]
- Duits, F.H.; Martinez-Lage, P.; Paquet, C.; Engelborghs, S.; Lleo, A.; Hausner, L.; Molinuevo, J.L.; Stomrud, E.; Farotti, L.; Ramakers, I.; et al. Performance and complications of lumbar puncture in memory clinics: Results of the multicenter lumbar puncture feasibility study. Alzheimers Dement 2016, 12, 154–163. [Google Scholar] [CrossRef]
- Leuzy, A.; Mattsson-Carlgren, N.; Palmqvist, S.; Janelidze, S.; Dage, J.L.; Hansson, O. Blood-based biomarkers for Alzheimer’s disease. EMBO Mol. Med. 2022, 14, e14408. [Google Scholar] [CrossRef]
- Schindler, S.E.; Bollinger, J.G.; Ovod, V.; Mawuenyega, K.G.; Li, Y.; Gordon, B.A.; Holtzman, D.M.; Morris, J.C.; Benzinger, T.L.S.; Xiong, C.; et al. High-precision plasma beta-amyloid 42/40 predicts current and future brain amyloidosis. Neurology 2019, 93, e1647–e1659. [Google Scholar] [CrossRef]
- Janelidze, S.; Mattsson, N.; Palmqvist, S.; Smith, R.; Beach, T.G.; Serrano, G.E.; Chai, X.; Proctor, N.K.; Eichenlaub, U.; Zetterberg, H.; et al. Plasma P-tau181 in Alzheimer’s disease: Relationship to other biomarkers, differential diagnosis, neuropathology and longitudinal progression to Alzheimer’s dementia. Nat. Med. 2020, 26, 379–386. [Google Scholar] [CrossRef]
- Karikari, T.K.; Pascoal, T.A.; Ashton, N.J.; Janelidze, S.; Benedet, A.L.; Rodriguez, J.L.; Chamoun, M.; Savard, M.; Kang, M.S.; Therriault, J.; et al. Blood phosphorylated tau 181 as a biomarker for Alzheimer’s disease: A diagnostic performance and prediction modelling study using data from four prospective cohorts. Lancet. Neurol. 2020, 19, 422–433. [Google Scholar] [CrossRef]
- Mattsson, N.; Andreasson, U.; Zetterberg, H.; Blennow, K.; Alzheimer’s Disease Neuroimaging, I. Association of Plasma Neurofilament Light With Neurodegeneration in Patients With Alzheimer Disease. JAMA Neurol. 2017, 74, 557–566. [Google Scholar] [CrossRef]
- Rozga, M.; Bittner, T.; Batrla, R.; Karl, J. Preanalytical sample handling recommendations for Alzheimer’s disease plasma biomarkers. Alzheimers Dement 2019, 11, 291–300. [Google Scholar] [CrossRef]
- Sperling, R.A.; Rentz, D.M.; Johnson, K.A.; Karlawish, J.; Donohue, M.; Salmon, D.P.; Aisen, P. The A4 study: Stopping AD before symptoms begin? Sci. Transl. Med. 2014, 6, 228fs213. [Google Scholar] [CrossRef]
- Francistiova, L.; Bianchi, C.; Di Lauro, C.; Sebastian-Serrano, A.; de Diego-Garcia, L.; Kobolak, J.; Dinnyes, A.; Diaz-Hernandez, M. The Role of P2X7 Receptor in Alzheimer’s Disease. Front. Mol. Neurosci. 2020, 13, 94. [Google Scholar] [CrossRef]
- Diaz-Hernandez, J.I.; Gomez-Villafuertes, R.; Leon-Otegui, M.; Hontecillas-Prieto, L.; Del Puerto, A.; Trejo, J.L.; Lucas, J.J.; Garrido, J.J.; Gualix, J.; Miras-Portugal, M.T.; et al. In vivo P2X7 inhibition reduces amyloid plaques in Alzheimer’s disease through GSK3beta and secretases. Neurobiol. Aging 2012, 33, 1816–1828. [Google Scholar] [CrossRef]
- Carvalho, K.; Martin, E.; Ces, A.; Sarrazin, N.; Lagouge-Roussey, P.; Nous, C.; Boucherit, L.; Youssef, I.; Prigent, A.; Faivre, E.; et al. P2X7-deficiency improves plasticity and cognitive abilities in a mouse model of Tauopathy. Prog. Neurobiol. 2021, 206, 102139. [Google Scholar] [CrossRef]
- Di Lauro, C.; Bianchi, C.; Sebastian-Serrano, A.; Soria-Tobar, L.; Alvarez-Castelao, B.; Nicke, A.; Diaz-Hernandez, M. P2X7 receptor blockade reduces tau induced toxicity, therapeutic implications in tauopathies. Prog. Neurobiol. 2022, 208, 102173. [Google Scholar] [CrossRef]
- Martinez-Frailes, C.; Di Lauro, C.; Bianchi, C.; de Diego-Garcia, L.; Sebastian-Serrano, A.; Bosca, L.; Diaz-Hernandez, M. Amyloid Peptide Induced Neuroinflammation Increases the P2X7 Receptor Expression in Microglial Cells, Impacting on Its Functionality. Front. Cell Neurosci. 2019, 13, 143. [Google Scholar] [CrossRef]
- Diez-Zaera, M.; Diaz-Hernandez, J.I.; Hernandez-Alvarez, E.; Zimmermann, H.; Diaz-Hernandez, M.; Miras-Portugal, M.T. Tissue-nonspecific alkaline phosphatase promotes axonal growth of hippocampal neurons. Mol. Biol. Cell 2011, 22, 1014–1024. [Google Scholar] [CrossRef]
- Sebastian-Serrano, A.; de Diego-Garcia, L.; Martinez-Frailes, C.; Avila, J.; Zimmermann, H.; Millan, J.L.; Miras-Portugal, M.T.; Diaz-Hernandez, M. Tissue-nonspecific Alkaline Phosphatase Regulates Purinergic Transmission in the Central Nervous System During Development and Disease. Comput. Struct. Biotechnol. J. 2015, 13, 95–100. [Google Scholar] [CrossRef]
- Diaz-Hernandez, M.; Gomez-Ramos, A.; Rubio, A.; Gomez-Villafuertes, R.; Naranjo, J.R.; Miras-Portugal, M.T.; Avila, J. Tissue-nonspecific alkaline phosphatase promotes the neurotoxicity effect of extracellular tau. J. Biol. Chem. 2010, 285, 32539–32548. [Google Scholar] [CrossRef] [PubMed]
- Sebastian-Serrano, A.; Merchan-Rubira, J.; Di Lauro, C.; Bianchi, C.; Soria-Tobar, L.; Narisawa, S.; Millan, J.L.; Avila, J.; Hernandez, F.; Diaz-Hernandez, M. TNAP upregulation is a critical factor in Tauopathies and its blockade ameliorates neurotoxicity and increases life-expectancy. Neurobiol. Dis. 2022, 165, 105632. [Google Scholar] [CrossRef] [PubMed]
- Vardy, E.R.; Kellett, K.A.; Cocklin, S.L.; Hooper, N.M. Alkaline phosphatase is increased in both brain and plasma in Alzheimer’s disease. Neurodegener. Dis. 2012, 9, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Kellett, K.A.; Williams, J.; Vardy, E.R.; Smith, A.D.; Hooper, N.M. Plasma alkaline phosphatase is elevated in Alzheimer’s disease and inversely correlates with cognitive function. Int. J. Mol. Epidemiol. Genet. 2011, 2, 114–121. [Google Scholar]
- Conte, G.; Menendez-Mendez, A.; Bauer, S.; El-Naggar, H.; Alves, M.; Nicke, A.; Delanty, N.; Rosenow, F.; Henshall, D.C.; Engel, T. Circulating P2X7 Receptor Signaling Components as Diagnostic Biomarkers for Temporal Lobe Epilepsy. Cells 2021, 10, 2444. [Google Scholar] [CrossRef]
- Garcia-Villalba, J.; Hurtado-Navarro, L.; Penin-Franch, A.; Molina-Lopez, C.; Martinez-Alarcon, L.; Angosto-Bazarra, D.; Baroja-Mazo, A.; Pelegrin, P. Soluble P2X7 Receptor is Elevated in the Plasma of COVID-19 Patients and Correlates with Disease Severity. Front. Immunol. 2022, 13, 894470. [Google Scholar] [CrossRef]
- Giuliani, A.L.; Berchan, M.; Sanz, J.M.; Passaro, A.; Pizzicotti, S.; Vultaggio-Poma, V.; Sarti, A.C.; Di Virgilio, F. The P2X7 Receptor is Shed into Circulation: Correlation with C-Reactive Protein Levels. Front. Immunol. 2019, 10, 793. [Google Scholar] [CrossRef]
- Saunders, A.M.; Strittmatter, W.J.; Schmechel, D.; George-Hyslop, P.H.; Pericak-Vance, M.A.; Joo, S.H.; Rosi, B.L.; Gusella, J.F.; Crapper-MacLachlan, D.R.; Alberts, M.J.; et al. Association of apolipoprotein E allele epsilon 4 with late-onset familial and sporadic Alzheimer’s disease. Neurology 1993, 43, 1467–1472. [Google Scholar] [CrossRef]
- Sebastian-Serrano, A.; Engel, T.; de Diego-Garcia, L.; Olivos-Ore, L.A.; Arribas-Blazquez, M.; Martinez-Frailes, C.; Perez-Diaz, C.; Millan, J.L.; Artalejo, A.R.; Miras-Portugal, M.T.; et al. Neurodevelopmental alterations and seizures developed by mouse model of infantile hypophosphatasia are associated with purinergic signalling deregulation. Hum. Mol. Genet. 2016, 25, 4143–4156. [Google Scholar] [CrossRef]
- Liang, Y.; Mao, Y.; Liang, W.; Liang, L.; Suo, M.; Xue, J.; Yang, H. Association of serum alkaline phosphatase and depression in US adults: A population-based cross-sectional study. Front. Psychiatry 2023, 14, 1131105. [Google Scholar] [CrossRef]
- Arun, P.; Oguntayo, S.; Albert, S.V.; Gist, I.; Wang, Y.; Nambiar, M.P.; Long, J.B. Acute decrease in alkaline phosphatase after brain injury: A potential mechanism for tauopathy. Neurosci. Lett. 2015, 609, 152–158. [Google Scholar] [CrossRef]
- Zetterberg, H.; Bendlin, B.B. Biomarkers for Alzheimer’s disease-preparing for a new era of disease-modifying therapies. Mol. Psychiatry 2021, 26, 296–308. [Google Scholar] [CrossRef]
- Martinez-Garcia, J.J.; Martinez-Banaclocha, H.; Angosto-Bazarra, D.; de Torre-Minguela, C.; Baroja-Mazo, A.; Alarcon-Vila, C.; Martinez-Alarcon, L.; Amores-Iniesta, J.; Martin-Sanchez, F.; Ercole, G.A.; et al. P2X7 receptor induces mitochondrial failure in monocytes and compromises NLRP3 inflammasome activation during sepsis. Nat. Commun. 2019, 10, 2711. [Google Scholar] [CrossRef]
- Wu, H.; Nie, Y.; Xiong, H.; Liu, S.; Li, G.; Huang, A.; Guo, L.; Wang, S.; Xue, Y.; Wu, B.; et al. P2X7 Receptor Expression in Peripheral Blood Monocytes is Correlated with Plasma C-Reactive Protein and Cytokine Levels in Patients with Type 2 Diabetes Mellitus: A Preliminary Report. Inflammation 2015, 38, 2076–2081. [Google Scholar] [CrossRef]
- Calsolaro, V.; Edison, P. Neuroinflammation in Alzheimer’s disease: Current evidence and future directions. Alzheimers Dement 2016, 12, 719–732. [Google Scholar] [CrossRef]
- Fan, Z.; Brooks, D.J.; Okello, A.; Edison, P. An early and late peak in microglial activation in Alzheimer’s disease trajectory. Brain 2017, 140, 792–803. [Google Scholar] [CrossRef]
- Beaino, W.; Janssen, B.; Kooij, G.; van der Pol, S.M.A.; van Het Hof, B.; van Horssen, J.; Windhorst, A.D.; de Vries, H.E. Purinergic receptors P2Y12R and P2X7R: Potential targets for PET imaging of microglia phenotypes in multiple sclerosis. J. Neuroinflammation 2017, 14, 259. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Huang, X.; Fowler, C.; Lim, Y.Y.; Laws, S.M.; Faux, N.; Doecke, J.D.; Trounson, B.; Pertile, K.; Rumble, R.; et al. Identification of Leukocyte Surface P2X7 as a Biomarker Associated with Alzheimer’s Disease. Int. J. Mol. Sci. 2022, 23, 7867. [Google Scholar] [CrossRef]
- Lioi, A.B.; Ferrari, B.M.; Dubyak, G.R.; Weinberg, A.; Sieg, S.F. Human beta Defensin-3 Increases CD86 Expression on Monocytes by Activating the ATP-Gated Channel P2X7. J. Immunol. 2015, 195, 4438–4445. [Google Scholar] [CrossRef]
- Rizzo, R.; Ferrari, D.; Melchiorri, L.; Stignani, M.; Gulinelli, S.; Baricordi, O.R.; Di Virgilio, F. Extracellular ATP acting at the P2X7 receptor inhibits secretion of soluble HLA-G from human monocytes. J. Immunol. 2009, 183, 4302–4311. [Google Scholar] [CrossRef] [PubMed]
- Gourine, A.V.; Dale, N.; Llaudet, E.; Poputnikov, D.M.; Spyer, K.M.; Gourine, V.N. Release of ATP in the central nervous system during systemic inflammation: Real-time measurement in the hypothalamus of conscious rabbits. J. Physiol. 2007, 585, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Janelidze, S.; Teunissen, C.E.; Zetterberg, H.; Allue, J.A.; Sarasa, L.; Eichenlaub, U.; Bittner, T.; Ovod, V.; Verberk, I.M.W.; Toba, K.; et al. Head-to-Head Comparison of 8 Plasma Amyloid-beta 42/40 Assays in Alzheimer Disease. JAMA Neurol 2021, 78, 1375–1382. [Google Scholar] [CrossRef] [PubMed]
- Simren, J.; Leuzy, A.; Karikari, T.K.; Hye, A.; Benedet, A.L.; Lantero-Rodriguez, J.; Mattsson-Carlgren, N.; Scholl, M.; Mecocci, P.; Vellas, B.; et al. The diagnostic and prognostic capabilities of plasma biomarkers in Alzheimer’s disease. Alzheimers Dement 2021, 17, 1145–1156. [Google Scholar] [CrossRef]
- Olazaran, J.; Valenti, M.; Frades, B.; Zea-Sevilla, M.A.; Avila-Villanueva, M.; Fernandez-Blazquez, M.A.; Calero, M.; Dobato, J.L.; Hernandez-Tamames, J.A.; Leon-Salas, B.; et al. The Vallecas Project: A Cohort to Identify Early Markers and Mechanisms of Alzheimer’s Disease. Front. Aging Neurosci. 2015, 7, 181. [Google Scholar] [CrossRef]
- Petersen, R.C.; Smith, G.E.; Waring, S.C.; Ivnik, R.J.; Tangalos, E.G.; Kokmen, E. Mild cognitive impairment: Clinical characterization and outcome. Arch. Neurol. 1999, 56, 303–308. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Pfeffer, R.I.; Kurosaki, T.T.; Harrah, C.H., Jr.; Chance, J.M.; Filos, S. Measurement of functional activities in older adults in the community. J. Gerontol. 1982, 37, 323–329. [Google Scholar] [CrossRef]
- Peavy, G.M.; Salmon, D.P.; Rice, V.A.; Galasko, D.; Samuel, W.; Taylor, K.I.; Ernesto, C.; Butters, N.; Thal, L. Neuropsychological assessment of severely demeted elderly: The severe cognitive impairment profile. Arch. Neurol. 1996, 53, 367–372. [Google Scholar] [CrossRef]
- Mitchell, A.J. A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. J. Psychiatr. Res. 2009, 43, 411–431. [Google Scholar] [CrossRef]
- Harrell, L.E.; Marson, D.; Chatterjee, A.; Parrish, J.A. The Severe Mini-Mental State Examination: A new neuropsychologic instrument for the bedside assessment of severely impaired patients with Alzheimer disease. Alzheimer Dis. Assoc. Disord. 2000, 14, 168–175. [Google Scholar] [CrossRef]
- Mougias, A.A.; Christidi, F.; Kiosterakis, G.; Messinis, L.; Politis, A. Dealing with severe dementia in clinical practice: A validity and reliability study of Severe Mini-Mental State Examination in Greek population. Int. J. Geriatr. Psychiatry 2018, 33, 1236–1242. [Google Scholar] [CrossRef]
- Fazekas, F.; Chawluk, J.B.; Alavi, A.; Hurtig, H.I.; Zimmerman, R.A. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am. J. Roentgenol. 1987, 149, 351–356. [Google Scholar] [CrossRef]
- Calero, O.; Hortiguela, R.; Bullido, M.J.; Calero, M. Apolipoprotein E genotyping method by real time PCR, a fast and cost-effective alternative to the TaqMan and FRET assays. J. Neurosci. Methods 2009, 183, 238–240. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef]
| Control n = 23 | MCI n = 17 | AD n = 20 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | Mean | SEM | ||
| Age (years) | 77.0 | 0.5 | 79.9 | 0.7 | 78.6 | 1.3 | PANOVA = 0.09 (ns) |
| Sex F/M % | 60/40 | 41/59 | 55/45 | ||||
| Fazekas scale value | 0.8 | 0.2 | 1.2 | 0.2 | 1.6 | 0.2 | PANOVA = 0.045 (*) |
| %FS = 0 | 35 | 29 | 13 | ||||
| %FS = 1 | 52 | 29 | 38 | ||||
| %FS = 2 | 9 | 35 | 31 | ||||
| %FS = 3 | 4 | 6 | 19 | ||||
| MMSE | 29.1 | 1.1 | 27.3 | 1.4 | - | - | PMW < 0.0001 |
| FAQ | 0.6 | 0.9 | 3.0 | 1.8 | - | - | PMW < 0.0001 |
| CDT | 9.5 | 1.0 | 8.5 | 1.7 | - | - | PMW = 0.0171 |
| GDS | 1.0 | 1.4 | 1.8 | 2.1 | - | - | PMW = 0.106 |
| CDR | 0.0 | 0.0 | 0.5 | 0.0 | - | - | PMW < 0.0001 |
| APOEƐ3Ɛ4 allele, % | 8.7 | 23.5 | 40 | ||||
| APOEƐ4Ɛ4 allele, % | 0 | 0 | 15 | ||||
| AUC (±SE) | IC95% | Cut-Off Value | Sensitivity % | Specificity % | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| CTRL vs. MCI | P2X7R pg/mL | 0.65 ± 0.09 | 0.46–0.83 | >32.5 | 78.6 | 50.0 | 0.144 | |
| TNAP activity | 0.75 ± 0.09 | 0.58–0.92 | >112.6 | 71.4 | 72.3 | 0.011 | * p < 0.05 | |
| CTRL vs. AD | P2X7R pg/mL | 0.73 ± 0.08 | 0.58–0.89 | >32.3 | 90.00 | 50.22 | 0.009 | ** p < 0.01 |
| TNAP activity | 0.69 ± 0.08 | 0.53–0.86 | <92.9 | 75.00 | 68.18 | 0.029 | * p < 0.05 |
| AUC (±SE) | IC95% | Cut-Off Predicted Probability | Sensitivity % | Specificity % | ||
|---|---|---|---|---|---|---|
| CTRL vs. MCI | Probability of the combined variable | 0.76 ± 0.09 | 0.59–0.94 | <0.49 | 71.4 | 86.4 |
| CTRL vs. AD | Probability of the combined variable | 0.77 ± 0.07 | 0.63–0.92 | <0.40 | 80.00 | 72.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aivar, P.; Bianchi, C.; Di Lauro, C.; Soria-Tobar, L.; Alvarez-Castelao, B.; Calero, M.; Medina, M.; Diaz-Hernandez, M. TNAP and P2X7R: New Plasma Biomarkers for Alzheimer’s Disease. Int. J. Mol. Sci. 2023, 24, 10897. https://doi.org/10.3390/ijms241310897
Aivar P, Bianchi C, Di Lauro C, Soria-Tobar L, Alvarez-Castelao B, Calero M, Medina M, Diaz-Hernandez M. TNAP and P2X7R: New Plasma Biomarkers for Alzheimer’s Disease. International Journal of Molecular Sciences. 2023; 24(13):10897. https://doi.org/10.3390/ijms241310897
Chicago/Turabian StyleAivar, Paloma, Carolina Bianchi, Caterina Di Lauro, Lucia Soria-Tobar, Beatriz Alvarez-Castelao, Miguel Calero, Miguel Medina, and Miguel Diaz-Hernandez. 2023. "TNAP and P2X7R: New Plasma Biomarkers for Alzheimer’s Disease" International Journal of Molecular Sciences 24, no. 13: 10897. https://doi.org/10.3390/ijms241310897
APA StyleAivar, P., Bianchi, C., Di Lauro, C., Soria-Tobar, L., Alvarez-Castelao, B., Calero, M., Medina, M., & Diaz-Hernandez, M. (2023). TNAP and P2X7R: New Plasma Biomarkers for Alzheimer’s Disease. International Journal of Molecular Sciences, 24(13), 10897. https://doi.org/10.3390/ijms241310897









