Genetic Influence on Treatment Response in Psoriasis: New Insights into Personalized Medicine
Abstract
1. Introduction
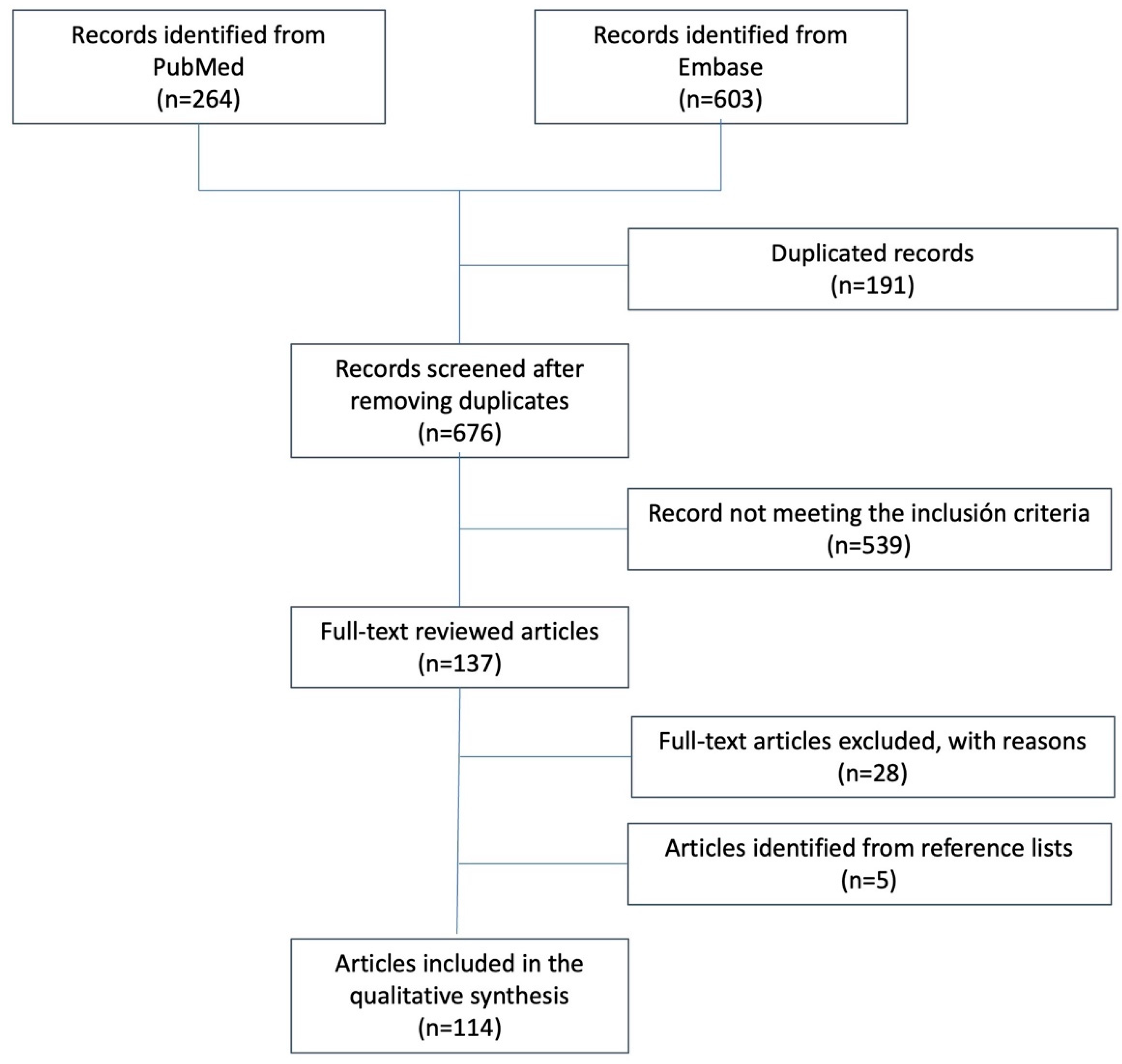
2. Literature Search
3. Therapeutic Options
3.1. Topical Therapies
3.2. Phototherapy
3.3. Conventional Systemic Drugs
3.3.1. Methotrexate
3.3.2. Cyclosporine
3.3.3. Acitretin
3.4. Small Molecules
Apremilast
3.5. Biologics
3.5.1. Anti-TNF-α Drugs
3.5.2. Ustekinumab
| Author | Year | Country | Drug | Gen | SNP (Allele/Genotype) | Responsive Allele or Genotype | n | Follow-Up | Outcome | Response |
|---|---|---|---|---|---|---|---|---|---|---|
| Nani et al. [133] | 2023 | Greece | IFX, ADA and ETN | MIR155 | rs767649 | A | 100 | 24 weeks | PASI75 | (+) |
| Ren et al. γ [112] | 2022 | China | ETN ± MTX | IQGAP2-F2RL2 | rs2431355 | T | 209 | 12 and 24 weeks | PASI75 | (+) |
| SDC3 | rs11801616 | G | (−) | |||||||
| IRF1-AS1 | rs13166823 | G | (−) | |||||||
| NPAP1 | rs10220768 | C | (+) | |||||||
| KRT31 | rs4796752 | C | (+) | |||||||
| CTSZ | rs4796752 | T | (−) | |||||||
| CNOT11 | rs3754679 | G | (−) | |||||||
| Sanz-Garcia et al. [116] | 2021 | Spain | IFX, ADA, and ETN | CPM | CVN | - | 70 | 24 weeks | PASI90 | (+) δ |
| Ovejero-Benito et al. γ [111] | 2020 | Spain | IFX, ADA, and ETN | AKAP13 | rs28461892 | A | 243 | 3 months | PASI75 | (+) |
| SUPT3H | rs9472377 | G | (+) | |||||||
| CDH12 | rs1487419 | A | (+) | |||||||
| rs77497886 | T | (+) | ||||||||
| HNRNPKP3 | rs11037360 | A | (+) | |||||||
| rs7481533 | C | (+) | ||||||||
| rs11037342 | C | (+) | ||||||||
| rs145304743 | T | (+) | ||||||||
| rs1845821 | C | (+) | ||||||||
| Hassan Hadi et al. [104] | 2020 | Iraq | ETN | TNFAIP3 | rs610604 | C | 100 | 6 months | Not specified | (−) |
| Coto-Segura et al. [79] | 2019 | Spain | ADA | NFKBIZ | rs3217713 (indel) | Ins/Del and Del/Del | 169 | 24 weeks | PASI75 | (+) |
| HLA-C | HLA-Cw*06 | Positive | (+) | |||||||
| Ovejero-Benito et al. [98] | 2019 | Spain | anti-TNF | TNFAIP3 | rs610604 | AC/CC | 20 | 3 months | EQ-VAS | (+) |
| rs6920220 | AA | (+) | ||||||||
| Dand et al. [82] | 2019 | United Kingdom and Ireland | ADA | HLA-C | HLA-Cw*06 | Positive | 1326 (839 ADA and 487 ustekinumab) | 6 months | PASI90 | (−) |
| Guarene et al. [93] | 2018 | Italy | IFX, ADA, ETN, and UTK | HLA-A | HLA-A Bw480I | Positive | 48 | 6 months | PASI75 | (−) |
| Ovejero-Benito et al. [134] | 2018 | Spain | IFX and ADA | IVL | rs6661932 | CT-TT | 95 | 3 months | PASI75 | (−) |
| IL-12B | rs2546890 | AG-AA | (+) | |||||||
| NFKBIA | rs2145623 | CG-GG | (−) | |||||||
| ZNF816A | rs9304742 | CT-CC | (+) | |||||||
| SLC9A8 | rs645544 | GG | (−) | |||||||
| Batalla et al. [135] | 2018 | Spain | IFX, ADA, and ETN | IL17RA | rs4819554 | A | 238 | 24 weeks | PASI75 | (+) |
| Prieto-Pérez et al. [106] | 2018 | Spain | IFX, ADA, and ETN | PGLYRP-4-24 | rs2916205 | AG/GG | 144 | 3 months | PASI75 | (−) |
| ZNF816A | rs9304742 | CC | 3 months | (−) | ||||||
| CTNNA2 | rs11126740 | AA | 3 months | (−) | ||||||
| IL-12B | rs2546890 | AG/GG | 3 months | (−) | ||||||
| 6 months | (−) | |||||||||
| MAP3K1 | rs96844 | CT/CC | 3 months | (+) | ||||||
| 6 months | (+) | |||||||||
| HLA-C | rs12191877 | CT/TT | 3 months | (+) | ||||||
| FCGR2A | rs1801274 | CT/CC | 6 months | (−) | ||||||
| HTR2A | rs6311 | CT/TT | 6 months | (−) | ||||||
| CDKAL1 | rs6908425 | CT/TT | 6 months | (+) | ||||||
| Loft et al. [130] | 2018 | Denmark | IFX, ADA, and ETN | IL-1B | rs1143623 | G/C | 376 | 3 months | PASI75 | (−) |
| rs1143627 | T/C | (−) | ||||||||
| LY96 | rs11465996 | C/G | (−) | |||||||
| TLR2 | rs11938228 | C/A | (−) | |||||||
| rs4696480 | A/T | (−) | ||||||||
| van den Reek et al. [83] | 2017 | Netherlands | ADA and ETN | CD84 | rs6427528 | GA | 282 ϕ | 3 months | Change in PASI | (+) |
| HLA-C | HLA-Cw*06 | Positive | (−) δ | |||||||
| Ovejero-Benito et al. [92] | 2017 | Spain | ETN | HLA-B/MICA | rs13437088 | TT | 78 | 3 months | PASI75 | (+) |
| MAP3K1 | rs96844 | CT-CC | (+) | |||||||
| PTTG1 | rs2431697 | CT-CC | (+) | |||||||
| ZNF816A | rs9304742 | CC | (+) | |||||||
| IL12B | rs2546890 | AG-GG | 6 months | (−) | ||||||
| GBP6 | rs928655 | AG-GG | (+) | |||||||
| Coto-Segura et al. [136] | 2016 | Spain | IFX, ADA, and ETN | CARD14 | rs11652075 | CC | 116 | 24 weeks | PASI75 | (+) |
| LCE3 | indel | Ins | (+) | |||||||
| Nishikawa et al. γ [110] | 2016 | Japan | IFX and ADA | SPEN | rs6701290 | G | 65 | 12 weeks | PASI75 | (−) |
| JAG2 | rs3784240 | A | (−) | |||||||
| MACC1 | rs2390256 | A | (−) | |||||||
| GUCY1B3 | rs2219538 | A | (−) | |||||||
| PDE6A | rs10515637 | G | (−) | |||||||
| CDH23 | rs10823825 | G | (−) | |||||||
| SHOC2 | rs1927159 | A | (+) | |||||||
| LOC728724 | rs7820834 | A | (−) | |||||||
| ADRA2A | rs553668 | A | (+) | |||||||
| KCNIP1 | rs4867965 | C | (−) | |||||||
| Mendrinou et al. [107] | 2016 | Greek | IFX, ADA, and ETN | FCGR3A | rs396991 | G | 100 | 6 months | PASI75 | (+) ε |
| Masouri et al. [90] | 2016 | Greece | IFX, ADA, and ETN | HLA-C | rs10484554 | C | 228 | 6 months | PASI75 | (+) |
| TRAF3IP2 | rs13190932 | G | (+) λ | |||||||
| TNFAIP3 | rs610604 | A | (+) ε | |||||||
| HLA-A | rs9260313 | T | (+) δ | |||||||
| Coto-Segura et al. [137] | 2015 | Spain | IFX, ADA, and ETN | CDKAL12 | rs6908435 | CC | 116 | 24 weeks | PASI75 | (+) |
| Batalla et al. [108] | 2015 | Spain | IFX, ADA, and ETN | FCGR3A | rs396991 | FF | 115 | 6 months | PASI75 | (+) ε |
| Prieto-Pérez et al. [131] | 2015 | Spain | IFX, ADA, and ETN | IL17F | rs763780 | CT | 180 | 28 weeks | PASI75 | (−) δ/(+) λ |
| De Simone et al. [96] | 2015 | Italy | ETN | TNF-alfa | rs361525 (-238) | GG | 97 | 12 weeks | PASI75 | (+) |
| rs1800629 (-308) | GG | (+) | ||||||||
| Batalla et al. [80] | 2015 | Spain | anti-TNF | LCE3C_LCE3B | indel | Del | 116 | 24 weeks | PASI75 | (−) |
| Julià et al. [138] | 2015 | Spain | IFX, ADA, and ETN | PDE3A-SLCO1C1 | rs3794271 | G | 130 | 12 weeks | Change in PASI | (+) |
| González-Lara et al. [101] | 2015 | Spain | IFX, ADA, ETN, and UTK | TNFRSFB1 | rs1061622 | G | 90 | 24 weeks | PASI75 | (−) |
| Gallo et al. [81] | 2013 | Spain | IFX, ADA, and ETN | HLA-C | HLA-Cw*06 | Positive | 109 | 6 months | PASI75 | (−) |
| TNF-alfa | rs361525 (-238) | GG | (+) | |||||||
| rs1799724 (-857) | CT/TT | (+) | ||||||||
| rs1799964 (-1031) | TT | (+) | ||||||||
| IL23R | rs11209026 | GG | (+) | |||||||
| Julià et al. [105] | 2013 | Spain | IFX, ADA, and ETN | FCGR2A | rs1801274 (H131R) | HH | 70 | 6 weeks | change in BSA | (+) |
| FCGR3A | rs396991 (V158F) | VV | (+) | |||||||
| Vasilopoulos et al. [95] | 2012 | Greek | IFX, ADA, and ETN | TNFA | rs1799724 (-857) | C | 80 | 6 months | PASI75 | (+) ε |
| TNFRSF1B | rs1061622 | T | (+) | |||||||
| Tejasvi et al. [103] | 2012 | USA and Canada | IFX, ADA, and ETN | TNFAIP3 | rs610604 | G | 632 | Not specified | Self-evaluated/PASI50 * | (+) ε |
| rs2230926/rs610604 (haplotype analysis) | TG | (+) | ||||||||
| Di Renzo et al. [139] | 2012 | Italy | IFX, ADA, and ETN | IL-6 | rs1800795 (-174) | C | 80 | 24 weeks | PASI75 | (+) |
| Author | Year | Country | Gen | Allele/SNP | Responsive Allele or Genotype | n | Follow-Up | Outcome | Response |
|---|---|---|---|---|---|---|---|---|---|
| Morelli et al. [141] | 2022 | Italy | CCHCR1 | rs2073719 | Not provided | 152 | 12, 28, 64, 76, and 88 weeks | PASI90 | (+) |
| TNFA | rs1800610 | 64, 76, 88, and 100 weeks | PASI100 | (−) | |||||
| Intergenic region upstream of HLA-C | rs12189871 (HLA-Cw*06_LD1) | 12, 28, 76, and 88 weeks | PASI90 | (+) | |||||
| rs4406273 (HLA-Cw*06_LD3) | 12, 28, 76, and 88 weeks | PASI90 | (+) | ||||||
| rs9348862 | 12, 28, 40, and 52 | PASI90 | (−) | ||||||
| rs9368670 | 12, 28, 40, and 52 | PASI90 | (−) | ||||||
| PSORS1C3 | rs1265181 | 12, 28, 52, 76, and 88 weeks | PASI90 | (+) | |||||
| MICA | rs2523497 | 64, 76, 88, and 100 weeks | PASI100 | (−) | |||||
| Intergenic region between LCE3B and LCE3A | rs12030223 | 12, 40,52, and 64 weeks | PASI100 | (+) | |||||
| rs6701730 | 12, 40, 52, and 64 weeks | PASI100 | (+) | ||||||
| CDSN | rs1042127 | 52, 64, 88, and 100 weeks | PASI100 | (−) | |||||
| rs4713436 | 52, 64, 88, and 100 weeks | PASI100 | (−) | ||||||
| Connell et al. [140] γ | 2022 | Europe | Intergenic region upstream WDR1 | rs35569429 | Deletion allele | 439 | 12 weeks | Change in PASI | (−) |
| Dand et al. [82] | 2019 | UK and Ireland | HLA-C | HLA-Cw*06 | Positive | 487 | 6 months | PASI90 | (+) |
| Loft et al. [130] | 2018 | Denmark | IL1B | rs1143623 | G/C | 230 | 12 weeks | PASI reduction | (−) |
| rs1143627 | T/C | (−) | |||||||
| TIRAP | rs8177374 | C/T | (+) | ||||||
| TLR5 | rs5744174 | T/C | (+) | ||||||
| Prieto-Pérez et al. [132] | 2017 | Spain | AGBL4 | rs191190 | TT | 69 | 16 weeks | PASI75 | (−) |
| HTR2A | rs6311 | TT | (−) | ||||||
| NFKB1A | rs2145623 | CC | (−) | ||||||
| ADAM33 | rs2787094 | CC | (−) | ||||||
| IL13 | rs848 | TT | (−) | ||||||
| CHUK | rs11591741 | GC | (+) | ||||||
| C17orf51 | rs1975974 | AG | (+) | ||||||
| ZNF816A | rs9304742 | CT | (+) | ||||||
| STAT4 | rs7574865 | GT | (+) | ||||||
| SLCC22A4 | rs1050152 | CT | (+) | ||||||
| C9orf72 | rs774359 | CT | (+) | ||||||
| van den Reek et al. [83] | 2017 | Netherlands | IL12B | rs3213094 | CT | 66 ϕ | 3 months | Change in PASI | (+) |
| TNFAIP3 | rs610604 | GG | Change in PASI | (−) | |||||
| Raposo et al. [125] | 2017 | Portugal | HLA-C | HLA-Cw*06 | Positive | 116 | 12 and 24 | PASI75 | (+) |
| Talamonti et al. [122] | 2017 | Italy | HLA-C | HLA-Cw*06 | Positive | 255 | 4, 12, 28, 40, and 52 | PASI50, PASI75, PASI90 and PASI100 | (+) |
| Talamonti et al. [121] | 2016 | Italy | HLA-C | HLA-Cw*06 | Positive | 134 | 12, 28, 52, and104 | PASI75 | (+) |
| Galluzo et al. [124] | 2016 | Italy | HLA-C | HLA-Cw*06 | Positive | 64 | 4, 28, 40, and 52 | PASI75 | (+) |
| Li et al. [127] | 2016 | USA | HLA-C | HLA-Cw*96 | Positive | 332 | 4 and 12 weeks | PASI50 and PASI75 | (+) |
| Masouri et al. [90] | 2016 | Greece | ERAP1 | rs151823 | CC | 22 | 24 weeks | PASI75 | (+) |
| rs26653 | GG | (+) | |||||||
| Prieto-Pérez et al. [131] | 2015 | Spain | IL-17F | rs763780 | TC | 70 | 12 and 24 weeks | PASI75 | (−) |
| Chiu et al. [123] | 2014 | China | HLA-C | HLA-Cw*06 | Positive | 66 | 4 and 28 weeks | PASI75 and PASI90 | (+) |
| Talamonti et al. [120] | 2013 | Italy | HLA-C | HLA-Cw*06 | Positive | 51 | 4, 12, 28, and 40 weeks | PASI75 | (+) |
3.5.3. Other Biologics
4. Conclusions and Future Directions
5. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boehncke, W.H.; Schön, M.P. Psoriasis. Lancet 2015, 386, 983–994. [Google Scholar] [CrossRef]
- Parisi, R.; Symmons, D.P.M.; Griffiths, C.E.M.; Ashcroft, D.M. Global Epidemiology of Psoriasis: A Systematic Review of Incidence and Prevalence. J. Investig. Dermatol. 2013, 133, 377–385. [Google Scholar] [CrossRef]
- Damiani, G.; Bragazzi, N.L.; Aksut, C.K.; Wu, D.; Alicandro, G.; McGonagle, D.; Guo, C.; Dellavalle, R.; Grada, A.; Wong, P.; et al. The Global, Regional, and National Burden of Psoriasis: Results and Insights From the Global Burden of Disease 2019 Study. Front. Med. 2021, 8, 743180. [Google Scholar] [CrossRef] [PubMed]
- Santus, P.; Rizzi, M.; Radovanovic, D.; Airoldi, A.; Cristiano, A.; Conic, R.; Petrou, S.; Pigatto, P.D.M.; Bragazzi, N.; Colombo, D.; et al. Psoriasis and Respiratory Comorbidities: The Added Value of Fraction of Exhaled Nitric Oxide as a New Method to Detect, Evaluate, and Monitor Psoriatic Systemic Involvement and Therapeutic Efficacy. BioMed Res. Int. 2018, 2018, 3140682. [Google Scholar] [CrossRef] [PubMed]
- Conic, R.R.; Damiani, G.; Schrom, K.P.; Ramser, A.E.; Zheng, C.; Xu, R.; McCormick, T.S.; Cooper, K.D. Psoriasis and Psoriatic Arthritis Cardiovascular Disease Endotypes Identified by Red Blood Cell Distribution Width and Mean Platelet Volume. J. Clin. Med. 2020, 9, 186. [Google Scholar] [CrossRef] [PubMed]
- Takeshita, J.; Grewal, S.; Langan, S.M.; Mehta, N.N.; Ogdie, A.; Van Voorhees, A.S.; Gelfand, J.M. Psoriasis and comorbid diseases. J. Am. Acad. Dermatol. 2017, 76, 377–390. [Google Scholar] [CrossRef]
- Feldman, S.R. Psoriasis causes as much disability as other major medical diseases. J. Am. Acad. Dermatol. 2020, 82, 256–257. [Google Scholar] [CrossRef] [PubMed]
- Dhana, A.; Yen, H.; Yen, H.; Cho, E. All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2019, 80, 1332–1343. [Google Scholar] [CrossRef] [PubMed]
- Abuabara, K.; Azfar, R.S.; Shin, D.B.; Neimann, A.L.; Troxel, A.B.; Gelfand, J.M. Cause-specific mortality in patients with severe psoriasis: A population-based cohort study in the U.K.: Cause-specific mortality in patients with severe psoriasis. Br. J. Dermatol. 2010, 163, 586–592. [Google Scholar] [CrossRef]
- Harden, J.L.; Krueger, J.G.; Bowcock, A.M. The immunogenetics of Psoriasis: A comprehensive review. J. Autoimmun. 2015, 64, 66–73. [Google Scholar] [CrossRef]
- Nair, R.P.; Stuart, P.E.; Nistor, I.; Hiremagalore, R.; Chia, N.V.; Jenisch, S.; Weichenthal, M.; Abecasis, G.R.; Lim, H.W.; Christophers, E.; et al. Sequence and Haplotype Analysis Supports HLA-C as the Psoriasis Susceptibility 1 Gene. Am. J. Hum. Genet. 2006, 78, 827–851. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Song, G.G. Associations between interleukin-23R and interleukin-12B polymorphisms and psoriasis susceptibility: A meta-analysis. Immunol. Investig. 2013, 42, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Caputo, V.; Strafella, C.; Termine, A.; Dattola, A.; Mazzilli, S.; Lanna, C.; Cosio, T.; Campione, E.; Novelli, G.; Giardina, E.; et al. Overview of the molecular determinants contributing to the expression of Psoriasis and Psoriatic Arthritis phenotypes. J. Cell. Mol. Med. 2020, 24, 13554–13563. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Pérez, R.; Cabaleiro, T.; Daudén, E.; Ochoa, D.; Roman, M.; Abad-Santos, F. Genetics of Psoriasis and Pharmacogenetics of Biological Drugs. Autoimmune Dis. 2013, 2013, 613086. [Google Scholar] [CrossRef] [PubMed]
- Rendon, A.; Schäkel, K. Psoriasis Pathogenesis and Treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef]
- Membrive Jiménez, C.; Pérez Ramírez, C.; Sánchez Martín, A.; Vieira Maroun, S.; Arias Santiago, S.A.; Ramírez Tortosa, M.D.C.; Jiménez Morales, A. Influence of Genetic Polymorphisms on Response to Biologics in Moderate-to-Severe Psoriasis. J. Pers. Med. 2021, 11, 293. [Google Scholar] [CrossRef] [PubMed]
- Daudén, E.; Puig, L.; Ferrándiz, C.; Sánchez-Carazo, J.L.; Hernanz-Hermosa, J.M.; the Spanish Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Consensus document on the evaluation and treatment of moderate-to-severe psoriasis: Psoriasis Group of the Spanish Academy of Dermatology and Venereology. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 1–18. [Google Scholar] [CrossRef]
- Sbidian, E.; Chaimani, A.; Garcia-Doval, I.; Do, G.; Hua, C.; Mazaud, C.; Droitcourt, C.; Hughes, C.; Ingram, J.R.; Naldi, L.; et al. Systemic pharmacological treatments for chronic plaque psoriasis: A network meta-analysis. Cochrane Skin Group, editor. Cochrane Database Syst. Rev. 2022, 8, CD011535. [Google Scholar]
- Farhangian, M.E.; Feldman, S.R. Immunogenicity of Biologic Treatments for Psoriasis: Therapeutic Consequences and the Potential Value of Concomitant Methotrexate. Am. J. Clin. Dermatol. 2015, 16, 285–294. [Google Scholar] [CrossRef]
- Muñoz-Aceituno, E.; Martos-Cabrera, L.; Ovejero-Benito, M.C.; Reolid, A.; Abad-Santos, F.; Daudén, E. Pharmacogenetics Update on Biologic Therapy in Psoriasis. Medicina 2020, 56, 719. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Muñoz-Aceituno, E.; Reolid, A.; Saiz-Rodríguez, M.; Abad-Santos, F.; Daudén, E. Pharmacogenetics and Pharmacogenomics in Moderate-to-Severe Psoriasis. Am. J. Clin. Dermatol. 2018, 19, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Caputo, V.; Strafella, C.; Cosio, T.; Lanna, C.; Campione, E.; Novelli, G.; Giardina, E.; Cascella, R. Pharmacogenomics: An Update on Biologics and Small-Molecule Drugs in the Treatment of Psoriasis. Genes 2021, 12, 1398. [Google Scholar] [CrossRef] [PubMed]
- Van Vugt, L.J.; Van Den Reek, J.M.P.A.; Coenen, M.J.H.; De Jong, E.M.G.J. A systematic review of pharmacogenetic studies on the response to biologics in patients with psoriasis. Br. J. Dermatol. 2018, 178, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Mee, J.B.; Cork, M.J. Vitamin D Receptor Polymorphism and Calcipotriol Response in Patients with Psoriasis. J. Investig. Dermatol. 1998, 110, 301–302. [Google Scholar] [CrossRef]
- Giomi, B.; Ruggiero, M.; Fabbri, P.; Gulisano, M.; Peruzzi, B.; Caproni, M.; Pacini, S. Does the determination of the Bb vitamin D receptor genotype identify psoriasis vulgaris patients responsive to topical tacalcitol? J. Dermatol. Sci. 2005, 37, 180–181. [Google Scholar] [CrossRef]
- Saeki, H.; Asano, N.; Tsunemi, Y.; Takekoshi, T.; Kishimoto, M.; Mitsui, H.; Tada, Y.; Torii, H.; Komine, M.; Asahina, A.; et al. Polymorphisms of vitamin D receptor gene in Japanese patients with psoriasis vulgaris. J. Dermatol. Sci. 2002, 30, 167–171. [Google Scholar] [CrossRef]
- Halsall, J.A.; Osborne, J.E.; Pringle, J.H.; Hutchinson, P.E. Vitamin D receptor gene polymorphisms, particularly the novel A-1012G promoter polymorphism, are associated with vitamin D3 responsiveness and non-familial susceptibility in psoriasis. Pharm. Genom. 2005, 15, 349–355. [Google Scholar] [CrossRef]
- Dayangac-Erden, D.; Karaduman, A.; Erdem-Yurter, H. Polymorphisms of vitamin D receptor gene in Turkish familial psoriasis patients. Arch. Dermatol. Res. 2007, 299, 487–491. [Google Scholar] [CrossRef]
- Acikbas, I.; Sanlı, B.; Tepeli, E.; Ergin, S.; Aktan, S.; Bagci, H. Vitamin D receptor gene polymorphisms and haplotypes (Apa I, Bsm I, Fok I, Taq I) in Turkish psoriasis patients. Med. Sci. Monit. 2012, 18, CR661–CR666. [Google Scholar] [CrossRef]
- Zhao, Y.; Chen, X.; Li, J.; He, Y.; Su, J.; Chen, M.; Zhang, W.; Chen, W.; Zhu, W. VDR gene polymorphisms are associated with the clinical response to calcipotriol in psoriatic patients. J. Dermatol. Sci. 2015, 79, 305–307. [Google Scholar] [CrossRef]
- Elmets, C.A.; Lim, H.W.; Stoff, B.; Connor, C.; Cordoro, K.M.; Lebwohl, M.; Armstrong, A.W.; Davis, D.M.; Elewski, B.E.; Gelfand, J.M.; et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J. Am. Acad. Dermatol. 2019, 81, 775–804. [Google Scholar] [CrossRef] [PubMed]
- Seleit, I.; Bakry, O.; Abd El Gayed, E.; Ghanem, M. Peroxisome proliferator-activated receptor-γ gene polymorphism in psoriasis and its relation to obesity, metabolic syndrome, and narrowband ultraviolet B response: A case–control study in Egyptian patients. Indian J. Dermatol. 2019, 64, 192. [Google Scholar] [PubMed]
- Youssef, R.; Abdel-Halim, M.R.; Kamel, M.; Khorshied, M.; Fahim, A. Effect of polymorphisms in IL-12B p40, IL-17A and IL-23 A/G genes on the response of psoriatic patients to narrowband UVB. Photodermatol. Photoimmunol. Photomed. 2018, 34, 347–349. [Google Scholar] [CrossRef] [PubMed]
- Bojko, A.; Ostasz, R.; Białecka, M.; Klimowicz, A.; Malinowski, D.; Budawski, R.; Bojko, P.; Drozdzik, M.; Kurzawski, M. IL12B, IL23A, IL23R and HLA-C*06 genetic variants in psoriasis susceptibility and response to treatment. Hum. Immunol. 2018, 79, 213–217. [Google Scholar] [CrossRef]
- Białecka, M.; Ostasz, R.; Kurzawski, M.; Klimowicz, A.; Fabiańczyk, H.; Bojko, P.; Dziedziejko, V.; Safranow, K.; Machoy-Mokrzyńska, A.; Droździk, M. IL17A and IL17F Gene Polymorphism Association with Psoriasis Risk and Response to Treatment in a Polish Population. Dermatology 2016, 232, 592–596. [Google Scholar] [CrossRef]
- Białecka, M.; Ostasz, R.; Kurzawski, M.; Klimowicz, A.; Fabiańczyk, H.; Bojko, P.; Dziedziejko, V.; Safranow, K.; Droździk, M. IL6 −174G>C polymorphism is associated with an increased risk of psoriasis but not response to treatment. Exp. Dermatol. 2015, 24, 146–147. [Google Scholar] [CrossRef]
- Smith, G.; Wilkie, M.; Deeni, Y.; Farr, P.; Ferguson, J.; Wolf, C.; Ibbotson, S. Melanocortin 1 receptor (MC1R) genotype influences erythemal sensitivity to psoralen–ultraviolet A photochemotherapy. Br. J. Dermatol. 2007, 157, 1230–1234. [Google Scholar] [CrossRef]
- Lesiak, A.; Wódz, K.; Ciążyńska, M.; Skibinska, M.; Waszczykowski, M.; Ciążyński, K.; Olejniczak-Staruch, I.; Sobolewska-Sztychny, D.; Narbutt, J. TaaI/Cdx-2 AA Variant of VDR Defines the Response to Phototherapy amongst Patients with Psoriasis. Life 2021, 11, 567. [Google Scholar] [CrossRef]
- Ryan, C.; Renfro, L.; Collins, P.; Kirby, B.; Rogers, S. Clinical and genetic predictors of response to narrowband ultraviolet B for the treatment of chronic plaque psoriasis: Predictors of response to NB-UVB for psoriasis. Br. J. Dermatol. 2010, 163, 1056–1063. [Google Scholar] [CrossRef]
- Menter, A.; Gelfand, J.M.; Connor, C.; Armstrong, A.W.; Cordoro, K.M.; Davis, D.M.; Elewski, B.E.; Gordon, K.B.; Gottlieb, A.B.; Kaplan, D.H.; et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J. Am. Acad. Dermatol. 2020, 82, 1445–1486. [Google Scholar] [CrossRef]
- Campalani, E.; Arenas, M.; Marinaki, A.M.; Lewis, C.; Barker, J.; Smith, C.H. Polymorphisms in Folate, Pyrimidine, and Purine Metabolism Are Associated with Efficacy and Toxicity of Methotrexate in Psoriasis. J. Investig. Dermatol. 2007, 127, 1860–1867. [Google Scholar] [CrossRef] [PubMed]
- Warren, R.B.; Smith, R.L.; Campalani, E.; Eyre, S.; Smith, C.H.; Barker, J.N.; Worthington, J.; Griffiths, C.E. Genetic Variation in Efflux Transporters Influences Outcome to Methotrexate Therapy in Patients with Psoriasis. J. Investig. Dermatol. 2008, 128, 1925–1929. [Google Scholar] [CrossRef] [PubMed]
- Duan, C.; Yu, M.; Xu, J.; Li, B.-Y.; Zhao, Y.; Kankala, R.K. Overcoming Cancer Multi-drug Resistance (MDR): Reasons, mechanisms, nanotherapeutic solutions, and challenges. Biomed. Pharmacother. 2023, 162, 114643. [Google Scholar] [CrossRef] [PubMed]
- Indhumathi, S.; Rajappa, M.; Chandrashekar, L.; Ananthanarayanan, P.H.; Thappa, D.M.; Negi, V.S. Pharmacogenetic markers to predict the clinical response to methotrexate in south Indian Tamil patients with psoriasis. Eur. J. Clin. Pharmacol. 2017, 73, 965–971. [Google Scholar] [CrossRef]
- West, J.; Ogston, S.; Berg, J.; Palmer, C.; Fleming, C.; Kumar, V.; Foerster, J. HLA-Cw6-positive patients with psoriasis show improved response to methotrexate treatment. Clin. Exp. Dermatol. 2017, 42, 651–655. [Google Scholar] [CrossRef]
- Mao, M.; Kuang, Y.; Chen, M.; Yan, K.; Lv, C.; Liu, P.; Lu, Y.; Chen, X.; Zhu, W.; Chen, W. The HLA-Cw*06 allele may predict the response to methotrexate (MTX) treatment in Chinese arthritis-free psoriasis patients. Arch. Dermatol. Res. 2023, 315, 1241–1247. [Google Scholar] [CrossRef]
- Chen, M.; Chen, W.; Liu, P.; Yan, K.; Lv, C.; Zhang, M.; Lu, Y.; Qin, Q.; Kuang, Y.; Zhu, W.; et al. The impacts of gene polymorphisms on methotrexate in Chinese psoriatic patients. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2059–2065. [Google Scholar] [CrossRef]
- Giletti, A.; Esperon, P. Genetic markers in methotrexate treatments. Pharmacogenom. J. 2018, 18, 689–703. [Google Scholar] [CrossRef]
- Grželj, J.; Mlinarič-Raščan, I.; Marko, P.B.; Marovt, M.; Gmeiner, T.; Šmid, A. Polymorphisms in GNMT and DNMT3b are associated with methotrexate treatment outcome in plaque psoriasis. Biomed. Pharmacother. 2021, 138, 111456. [Google Scholar] [CrossRef]
- Yang, W.; Huang, Q.; Han, L.; Wang, B.; Yawalkar, N.; Zhang, Z.; Yan, K. B7-H4 Polymorphism Influences the Prevalence of Diabetes Mellitus and Pro-Atherogenic Dyslipidemia in Patients with Psoriasis. J. Clin. Med. 2022, 11, 6235. [Google Scholar] [CrossRef]
- Fan, Z.; Zhang, Z.; Huang, Q.; Han, L.; Fang, X.; Yang, K.; Wu, S.; Zheng, Z.; Yawalkar, N.; Wang, Z.; et al. The Impact of ANxA6 Gene Polymorphism on the Efficacy of Methotrexate Treatment in Psoriasis Patients. Dermatology 2021, 237, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Hamza, A.; Abo Elwafa, R.; Ramadan, N.; Omar, S. Il17A (rs2275913 G>A) and IL17F (rs2397084 T>C) gene polymorphisms: Relation to psoriasis risk and response to methotrexate. J. Egypt. Womens Dermatol. Soc. 2021, 18, 167. [Google Scholar]
- Yan, K.X.; Zhang, Y.J.; Han, L.; Huang, Q.; Zhang, Z.H.; Fang, X.; Zheng, Z.Z.; Yawalkar, N.; Chang, Y.L.; Zhang, Q.; et al. TT genotype of rs10036748 in TNIP 1 shows better response to methotrexate in a Chinese population: A prospective cohort study. Br. J. Dermatol. 2019, 181, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Kuang, Y.H.; Lu, Y.; Yan, K.X.; Liu, P.P.; Chen, W.Q.; Shen, M.X.; He, Y.J.; Wu, L.S.; Qin, Q.S.; Zhou, X.C.; et al. Genetic polymorphism predicting Methotrexate efficacy in Chinese patients with psoriasis vulgaris. J. Dermatol. Sci. 2019, 93, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ding, X.; Meng, Z.; Chen, M.; Zheng, X.; Cai, M.; Wu, J.; Chang, Y.; Zhang, Q.; Jin, L.; et al. A Genome-wide association study identified HLA-C associated with the effectiveness of methotrexate for psoriasis treatment. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e898–e900. [Google Scholar] [CrossRef]
- Vasilopoulos, Y.; Sarri, C.; Zafiriou, E.; Patsatsi, A.; Stamatis, C.; Ntoumou, E.; Fassos, I.; Tsalta, A.; Karra, A.; Roussaki-Schulze, A.; et al. A pharmacogenetic study of ABCB1 polymorphisms and cyclosporine treatment response in patients with psoriasis in the Greek population. Pharmacogenom. J. 2014, 14, 523–525. [Google Scholar] [CrossRef]
- Chernov, A.; Kilina, D.; Smirnova, T.; Galimova, E. Pharmacogenetic Study of the Impact of ABCB1 Single Nucleotide Polymorphisms on the Response to Cyclosporine in Psoriasis Patients. Pharmaceutics 2022, 14, 2441. [Google Scholar] [CrossRef]
- Antonatos, C.; Patsatsi, A.; Zafiriou, E.; Stavrou, E.F.; Liaropoulos, A.; Kyriakoy, A.; Evangelou, E.; Digka, D.; Roussaki-Schulze, A.; Sotiriadis, D.; et al. Protein network and pathway analysis in a pharmacogenetic study of cyclosporine treatment response in Greek patients with psoriasis. Pharmacogenom. J. 2023, 23, 8–13. [Google Scholar] [CrossRef]
- Nofal, A.; Al-Makhzangy, I.; Attwa, E.; Nassar, A.; Abdalmoati, A. Vascular endothelial growth factor in psoriasis: An indicator of disease severity and control. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 803–806. [Google Scholar] [CrossRef]
- Young, H.S.; Summers, A.M.; Read, I.R.; Fairhurst, D.A.; Plant, D.J.; Campalani, E.; Smith, C.H.; Barker, J.N.; Detmar, M.J.; Brenchley, P.E.; et al. Interaction between Genetic Control of Vascular Endothelial Growth Factor Production and Retinoid Responsiveness in Psoriasis. J. Investig. Dermatol. 2006, 126, 453–459. [Google Scholar] [CrossRef]
- Chen, W.; Wu, L.; Zhu, W.; Chen, X. The polymorphisms of growth factor genes (VEGFA & EGF) were associated with response to acitretin in psoriasis. Pers. Med. 2018, 15, 181–188. [Google Scholar]
- Bozduman, T.; Evans, S.E.; Karahan, S.; Hayran, Y.; Akbiyik, F.; Lay, I. Genetic Risk Factors for Psoriasis in Turkish Population: -1540 C/A, -1512 Ins18, and +405 C/G Polymorphisms within the Vascular Endothelial Growth Factor Gene. Ann. Dermatol. 2016, 28, 30. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, X.; Zhang, W.; Peng, C.; Zhu, W.; Chen, X. Polymorphisms of SLCO1B1 rs4149056 and SLC22A1 rs2282143 are associated with responsiveness to acitretin in psoriasis patients. Sci. Rep. 2018, 8, 13182. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Wang, Y.; Lu, X.; Wang, T.; Li, Q.; Wang, R.; Wu, J.; Xu, J.; Du, J. The Inflammatory Factor SNP May Serve as a Promising Biomarker for Acitretin to Alleviate Secondary Failure of Response to TNF-a Monoclonal Antibodies in Psoriasis. Front. Pharmacol. 2022, 13, 937490. [Google Scholar] [CrossRef] [PubMed]
- Borghi, A.; Rizzo, R.; Corazza, M.; Bertoldi, A.M.; Bortolotti, D.; Sturabotti, G.; Virgili, A.; Di Luca, D. HLA-G 14-bp polymorphism: A possible marker of systemic treatment response in psoriasis vulgaris? Preliminary results of a retrospective study: HLA-G 14-bp polymorphism and therapy in psoriasis. Dermatol. Ther. 2014, 27, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; He, Y.; Kuang, Y.; Chen, W.; Zhu, W. HLA-DQA1 and DQB1 Alleles are Associated with Acitretin Response in Patients with Psoriasis. Front. Biosci.-Landmark 2022, 27, 266. [Google Scholar] [CrossRef]
- Zhou, X.; He, Y.; Kuang, Y.; Li, J.; Zhang, J.; Chen, M.; Chen, W.; Su, J.; Zhao, S.; Liu, P.; et al. Whole Exome Sequencing in Psoriasis Patients Contributes to Studies of Acitretin Treatment Difference. Int. J. Mol. Sci. 2017, 18, 295. [Google Scholar] [CrossRef] [PubMed]
- Campalani, E.; Allen, M.H.; Fairhurst, D.; Young, H.S.; Mendonca, C.O.; Burden, A.D.; Griffiths, C.E.; Crook, M.A.; Barker, J.N.; Smith, C.H. Apolipoprotein E gene polymorphisms are associated with psoriasis but do not determine disease response to acitretin: ApoE gene polymorphisms, psoriasis and acitretin. Br. J. Dermatol. 2006, 154, 345–352. [Google Scholar] [CrossRef]
- Zhu, T.; Jin, H.; Shu, D.; Li, F.; Wu, C. Association of IL36RN mutations with clinical features, therapeutic response to acitretin, and frequency of recurrence in patients with generalized pustular psoriasis. Eur. J. Dermatol. 2018, 28, 217–224. [Google Scholar] [CrossRef]
- Papp, K.; Reich, K.; Leonardi, C.L.; Kircik, L.; Chimenti, S.; Langley, R.G.; Hu, C.; Stevens, R.M.; Day, R.M.; Gordon, K.B.; et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: Results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J. Am. Acad. Dermatol. 2015, 73, 37–49. [Google Scholar] [CrossRef]
- Verbenko, D.A.; Karamova, A.E.; Artamonova, O.G.; Deryabin, D.G.; Rakitko, A.; Chernitsov, A.; Krasnenko, A.; Elmuratov, A.; Solomka, V.S.; Kubanov, A.A. Apremilast Pharmacogenomics in Russian Patients with Moderate-to-Severe and Severe Psoriasis. J. Pers. Med. 2020, 11, 20. [Google Scholar] [CrossRef] [PubMed]
- Reich, K.; Nestle, F.O.; Papp, K.; Ortonne, J.P.; Evans, R.; Guzzo, C.; Li, S.; Dooley, L.T.; Griffiths, C.E.; EXPRESS study investigators. Infliximab induction and maintenance therapy for moderate-to-severe psoriasis: A phase III, multicentre, double-blind trial. Lancet 2005, 366, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Papp, K.A.; Armstrong, A.W.; Reich, K.; Karunaratne, M.; Valdecantos, W. Adalimumab Efficacy in Patients with Psoriasis Who Received or Did Not Respond to Prior Systemic Therapy: A Pooled Post Hoc Analysis of Results from Three Double-Blind, Placebo-Controlled Clinical Trials. Am. J. Clin. Dermatol. 2016, 17, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Menter, A.; Tyring, S.K.; Gordon, K.; Kimball, A.B.; Leonardi, C.L.; Langley, R.G.; Strober, B.E.; Kaul, M.; Gu, Y.; Okun, M.; et al. Adalimumab therapy for moderate to severe psoriasis: A randomized, controlled phase III trial. J. Am. Acad. Dermatol. 2008, 58, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Saurat, J.-H.; Stingl, G.; Dubertret, L.; Papp, K.A.; Langley, R.G.; Ortonne, J.-P.; Unnebrink, K.; Kaul, M.; Camez, A.; for the CHAMPION Study Investigators. Efficacy and safety results from the randomized controlled comparative study of adalimumab vs. methotrexate vs. placebo in patients with psoriasis (CHAMPION): Adalimumab vs. methotrexate in psoriasis. Br. J. Dermatol. 2007, 158, 558–566. [Google Scholar] [CrossRef] [PubMed]
- Papp, K.; Tyring, S.; Lahfa, M.; Prinz, J.; Griffiths, C.; Nakanishi, A.; Zitnik, R.; van de Kerkhof, P. A global phase III randomized controlled trial of etanercept in psoriasis: Safety, efficacy, and effect of dose reduction. Br. J. Dermatol. 2005, 152, 1304–1312. [Google Scholar] [CrossRef]
- Carrascosa, J.M.; Puig, L.; Belinchón Romero, I.; Salgado-Boquete, L.; del Alcázar, E.; Andrés Lencina, J.J.; Moreno, D.; Cueva, P.D.L. Actualización práctica de las recomendaciones del Grupo de Psoriasis de la Academia Española de Dermatología y Venereología (GPS) para el tratamiento de la psoriasis con terapia biológica. Parte 1. «Conceptos y manejo general de la psoriasis con terapia biológica». Actas Dermo-Sifiliográficas 2022, 113, 261–277. [Google Scholar]
- Amin, M.; No, D.J.; Egeberg, A.; Wu, J.J. Choosing First-Line Biologic Treatment for Moderate-to-Severe Psoriasis: What Does the Evidence Say? Am. J. Clin. Dermatol. 2018, 19, 1–13. [Google Scholar] [CrossRef]
- Coto-Segura, P.; González-Lara, L.; Batalla, A.; Eiris, N.; Quiero, R.; Coto, E. NFKBIZ and CW6 in Adalimumab Response among Psoriasis Patients: Genetic Association and Alternative Transcript Analysis. Mol. Diagn. Ther. 2019, 23, 627–633. [Google Scholar] [CrossRef]
- Batalla, A.; Coto, E.; González-Fernández, D.; González-Lara, L.; Gómez, J.; Santos-Juanes, J.; Quiero, R.; Coto-Segura, P. The Cw6 and late-cornified envelope genotype plays a significant role in anti-tumor necrosis factor response among psoriatic patients. Pharmacogenet. Genom. 2015, 25, 313–316. [Google Scholar] [CrossRef]
- Gallo, E.; Cabaleiro, T.; Román, M.; Solano-López, G.; Abad-Santos, F.; García-Díez, A.; Daudén, E. The relationship between tumour necrosis factor (TNF)-α promoter and IL12B/IL-23R genes polymorphisms and the efficacy of anti-TNF-α therapy in psoriasis: A case-control study. Br. J. Dermatol. 2013, 169, 819–829. [Google Scholar] [CrossRef]
- Dand, N.; Duckworth, M.; Baudry, D.; Russell, A.; Curtis, C.J.; Lee, S.H.; Evans, I.; Mason, K.J.; Alsharqi, A.; Becher, G.; et al. HLA-C*06:02 genotype is a predictive biomarker of biologic treatment response in psoriasis. J. Allergy Clin. Immunol. 2019, 143, 2120–2130. [Google Scholar] [CrossRef]
- van den Reek, J.M.P.A.; Coenen, M.J.H.; van de L’Isle Arias, M.; Zweegers, J.; Rodijk-Olthuis, D.; Schalkwijk, J.; Vermeulen, S.H.; Joosten, I.; van de Kerkhof, P.C.M.; Seyger, M.M.B.; et al. Polymorphisms in CD84, IL12B and TNFAIP3 are associated with response to biologics in patients with psoriasis. Br. J. Dermatol. 2017, 176, 1288–1296. [Google Scholar] [CrossRef]
- Ryan, C.; Kelleher, J.; Fagan, M.F.; Rogers, S.; Collins, P.; Barker, J.N.; Allen, M.; Hagan, R.; Renfro, L.; Kirby, B. Genetic markers of treatment response to tumour necrosis factor-α inhibitors in the treatment of psoriasis. Clin. Exp. Dermatol. 2014, 39, 519–524. [Google Scholar] [CrossRef]
- Chiu, H.Y.; Huang, P.Y.; Jee, S.H.; Hu, C.Y.; Chou, C.T.; Chang, Y.T.; Hwang, C.Y.; Tsai, T.F. HLA polymorphism among Chinese patients with chronic plaque psoriasis: Subgroup analysis: HLA polymorphism among Chinese patients with psoriasis. Br. J. Dermatol. 2012, 166, 288–297. [Google Scholar] [CrossRef]
- Talamonti, M.; Galluzzo, M.; Zangrilli, A.; Papoutsaki, M.; Egan, C.G.; Bavetta, M.; Tambone, S.; Fargnoli, M.C.; Bianchi, L. HLA-C*06:02 Does Not Predispose to Clinical Response Following Long-Term Adalimumab Treatment in Psoriatic Patients: A Retrospective Cohort Study. Mol. Diagn. Ther. 2017, 21, 295–301. [Google Scholar] [CrossRef]
- Talamonti, M.; Galluzzo, M.; Botti, E.; Pavlidis, A.; Spallone, G.; Chimenti, S.; Antonio, C. Potential role of HLA-Cw6 in clinical response to anti-tumour necrosis factor alpha and T-cell targeting agents in psoriasis patients. Clin. Drug. Investig. 2013, 33, S71–S73. [Google Scholar]
- Caldarola, G.; Sgambato, A.; Fanali, C.; Moretta, G.; Farina, M.; Lucchetti, D.; Peris, K.; De Simone, C. HLA-Cw6 allele, NFkB1 and NFkBIA polymorphisms play no role in predicting response to etanercept in psoriatic patients. Pharmacogenet. Genom. 2016, 26, 423–427. [Google Scholar] [CrossRef]
- Burlando, M.; Russo, R.; Clapasson, A.; Carmisciano, L.; Stecca, A.; Cozzani, E.; Parodi, A. The HLA-Cw6 Dilemma: Is It Really an Outcome Predictor in Psoriasis Patients under Biologic Therapy? A Monocentric Retrospective Analysis. J. Clin. Med. 2020, 9, 3140. [Google Scholar] [CrossRef]
- Masouri, S.; Stefanaki, I.; Ntritsos, G.; Kypreou, K.P.; Drakaki, E.; Evangelou, E.; Nicolaidou, E.; Stratigos, A.J.; Antoniou, C. A Pharmacogenetic Study of Psoriasis Risk Variants in a Greek Population and Prediction of Responses to Anti-TNF-α and Anti-IL-12/23 Agents. Mol. Diagn. Ther. 2016, 20, 221–225. [Google Scholar] [CrossRef]
- Prieto-Pérez, R.; Solano-López, G.; Cabaleiro, T.; Román, M.; Ochoa, D.; Talegón, M.; Baniandrés, O.; López-Estebaranz, J.L.; de la Cueva, P.; Daudén, E.; et al. Polymorphisms Associated with Age at Onset in Patients with Moderate-to-Severe Plaque Psoriasis. J. Immunol. Res. 2015, 2015, 101879. [Google Scholar] [CrossRef] [PubMed]
- Ovejero-Benito, M.C.; Prieto-Pérez, R.; Llamas-Velasco, M.; Belmonte, C.; Cabaleiro, T.; Román, M.; Ochoa, D.; Talegón, M.; Saiz-Rodríguez, M.; Daudén, E.; et al. Polymorphisms associated with etanercept response in moderate-to-severe plaque psoriasis. Pharmacogenomics 2017, 18, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Guarene, M.; Pasi, A.; Bolcato, V.; Cananzi, R.; Piccolo, A.; Sbarsi, I.; Klersy, C.; Cacciatore, R.; Brazzelli, V. The Presence of HLA-A Bw4-80I KIR Ligands Could Predict “Difficult-to-Treat” Psoriasis and Poor Response to Etanercept. Mol. Diagn. Ther. 2018, 22, 471–474. [Google Scholar] [CrossRef] [PubMed]
- Song, G.G.; Seo, Y.H.; Kim, J.H.; Choi, S.J.; Ji, J.D.; Lee, Y.H. Association between TNF-α (-308 A/G, -238 A/G, -857 C/T) polymorphisms and responsiveness to TNF-α blockers in spondyloarthropathy, psoriasis and Crohn’s disease: A meta-analysis. Pharmacogenomics 2015, 16, 1427–1437. [Google Scholar] [CrossRef]
- Vasilopoulos, Y.; Manolika, M.; Zafiriou, E.; Sarafidou, T.; Bagiatis, V.; Krüger-Krasagaki, S.; Tosca, A.; Patsatsi, A.; Sotiriadis, D.; Mamuris, Z.; et al. Pharmacogenetic Analysis of TNF, TNFRSF1A, and TNFRSF1B Gene Polymorphisms and Prediction of Response to Anti-TNF Therapy in Psoriasis Patients in the Greek Population. Mol. Diagn. Ther. 2012, 16, 29–34. [Google Scholar] [CrossRef]
- De Simone, C.; Farina, M.; Maiorino, A.; Fanali, C.; Perino, F.; Flamini, A.; Caldarola, G.; Sgambato, A. TNF-alpha gene polymorphisms can help to predict response to etanercept in psoriatic patients. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1786–1790. [Google Scholar] [CrossRef]
- Daprà, V.; Ponti, R.; Lo Curcio, G.; Archetti, M.; Dini, M.; Gavatorta, M.; Quaglino, P.; Fierro, M.T.; Bergallo, M. Functional study of TNF-α as a promoter of polymorphisms in psoriasis. Ital. J. Dermatol. Venereol. 2022, 157, 146–153. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Muñoz-Aceituno, E.; Reolid, A.; Fisas, L.H.; Llamas-Velasco, M.; Prieto-Pérez, R.; Abad-Santos, F.; Daudén, E. Polymorphisms associated with anti-TNF drugs response in patients with psoriasis and psoriatic arthritis. J. Eur. Acad. Dermatol. Venereol. 2019, 33, e175–e177. [Google Scholar] [CrossRef]
- Ito, M.; Hirota, T.; Momose, M.; Ito, T.; Umezawa, Y.; Fukuchi, O.; Asahina, A.; Nakagawa, H.; Tamari, M.; Saeki, H. Lack of association of TNFA, TNFRSF1B and TNFAIP3 gene polymorphisms with response to anti-tumor necrosis factor therapy in Japanese patients with psoriasis. J. Dermatol. 2020, 47, e110–e111. [Google Scholar] [CrossRef]
- Fischer, R.; Kontermann, R.E.; Pfizenmaier, K. Selective Targeting of TNF Receptors as a Novel Therapeutic Approach. Front. Cell Dev. Biol. 2020, 8, 401. [Google Scholar] [CrossRef]
- González-Lara, L.; Batalla, A.; Coto, E.; Gómez, J.; Eiris, N.; Santos-Juanes, J.; Queiro, R.; Coto-Segura, P. The TNFRSF1B rs1061622 polymorphism (p.M196R) is associated with biological drug outcome in Psoriasis patients. Arch. Dermatol. Res. 2015, 307, 405–412. [Google Scholar] [CrossRef]
- Chen, W.; Xu, H.; Wang, X.; Gu, J.; Xiong, H.; Shi, Y. The tumor necrosis factor receptor superfamily member 1B polymorphisms predict response to anti-TNF therapy in patients with autoimmune disease: A meta-analysis. Int. Immunopharmacol. 2015, 28, 146–153. [Google Scholar] [CrossRef]
- Tejasvi, T.; Stuart, P.E.; Chandran, V.; Voorhees, J.J.; Gladman, D.D.; Rahman, P.; Elder, J.T.; Nair, R.P. TNFAIP3 Gene Polymorphisms Are Associated with Response to TNF Blockade in Psoriasis. J. Investig. Dermatol. 2012, 132, 593–600. [Google Scholar] [CrossRef]
- Hassan Hadi, A.M.; Abbas, A.A.; Abdulamir, A.S.; Fadheel, B.M. The effect of TNFAIP3 gene polymorphism on disease susceptibility and response of etanercept in psoriatic patients. Eur. J. Mol. Clin. Med. 2020, 7, 240–246. [Google Scholar]
- Julià, M.; Guilabert, A.; Lozano, F.; Suarez-Casasús, B.; Moreno, N.; Carrascosa, J.M.; Ferrándiz, C.; Pedrosa, E.; Alsina-Gibert, M.; Mascaró, J.M., Jr. The Role of Fcγ Receptor Polymorphisms in the Response to Anti–Tumor Necrosis Factor Therapy in Psoriasis: A Pharmacogenetic Study. JAMA Dermatol. 2013, 149, 1033. [Google Scholar] [CrossRef]
- Prieto-Pérez, R.; Solano-López, G.; Cabaleiro, T.; Román, M.; Ochoa, D.; Talegón, M.; Baniandrés, O.; López-Estebaranz, J.L.; de la Cueva, P.; Daudén, E.; et al. New polymorphisms associated with response to anti-TNF drugs in patients with moderate-to-severe plaque psoriasis. Pharmacogenom. J. 2018, 18, 70–75. [Google Scholar] [CrossRef]
- Mendrinou, E.; Patsatsi, A.; Zafiriou, E.; Papadopoulou, D.; Aggelou, L.; Sarri, C.; Mamuris, Z.; Kyriakou, A.; Sotiriadis, D.; Roussaki-Schulze, A.; et al. FCGR3A-V158F polymorphism is a disease-specific pharmacogenetic marker for the treatment of psoriasis with Fc-containing TNFα inhibitors. Pharmacogenom. J. 2017, 17, 237–241. [Google Scholar] [CrossRef]
- Batalla, A.; Coto, E.; Coto-Segura, P. Influence of Fcγ Receptor Polymorphisms on Response to Anti–Tumor Necrosis Factor Treatment in Psoriasis. JAMA Dermatol. 2015, 151, 1376. [Google Scholar] [CrossRef]
- Antonatos, C.; Stavrou, E.F.; Evangelou, E.; Vasilopoulos, Y. Exploring pharmacogenetic variants for predicting response to anti-TNF therapy in autoimmune diseases: A meta-analysis. Pharmacogenomics 2021, 22, 435–445. [Google Scholar] [CrossRef]
- Nishikawa, R.; Nagai, H.; Bito, T.; Ikeda, T.; Horikawa, T.; Adachi, A.; Matsubara, T.; Nishigori, C. Genetic prediction of the effectiveness of biologics for psoriasis treatment. J. Dermatol. 2016, 43, 1273–1277. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Muñoz-Aceituno, E.; Sabador, D.; Almoguera, B.; Prieto-Pérez, R.; Hakonarson, H.; Coto-Segura, P.; Carretero, G.; Reolid, A.; Llamas-Velasco, M.; et al. Genome-wide association analysis of psoriasis patients treated with anti-TNF drugs. Exp. Dermatol. 2020, 29, 1225–1232. [Google Scholar] [CrossRef]
- Ren, Y.; Wang, L.; Dai, H.; Qiu, G.; Liu, J.; Yu, D.; Liu, J.; Lyu, C.Z.; Liu, L.; Zheng, M. Genome-wide association analysis of anti-TNF-α treatment response in Chinese patients with psoriasis. Front. Pharmacol. 2022, 13, 968935. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Muñoz-Aceituno, E.; Sabador, D.; Reolid, A.; Llamas-Velasco, M.; Prieto-Pérez, R.; Abad-Santos, F.; Daudén, E. Polymorphisms associated with optimization of biological therapy through drug dose reduction in moderate-to-severe psoriasis. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e271–e275. [Google Scholar] [CrossRef]
- Bucalo, A.; Rega, F.; Zangrilli, A.; Silvestri, V.; Valentini, V.; Scafetta, G.; Marraffa, F.; Grassi, S.; Rogante, E.; Piccolo, A.; et al. Paradoxical Psoriasis Induced by Anti-TNFα Treatment: Evaluation of Disease-Specific Clinical and Genetic Markers. Int. J. Mol. Sci. 2020, 21, 7873. [Google Scholar] [CrossRef]
- Cabaleiro, T.; Prietoperez, R.; Navarro, R.M.; Solano, G.; Roman, M.J.; Ochoa, D.; Abad-Santos, F.; Dauden, E. Paradoxical psoriasiform reactions to anti-TNFα drugs are associated with genetic polymorphisms in patients with psoriasis. Pharmacogenom. J. 2016, 16, 336–340. [Google Scholar] [CrossRef]
- Sanz-Garcia, A.; Reolid, A.; Fisas, L.; Muñoz-Aceituno, E.; Llamas-Velasco, M.; Sahuquillo-Torralba, A.; Botella-Estrada, R.; García-Martínez, J.; Navarro, R.; Daudén, E.; et al. DNA Copy Number Variation Associated with Anti-tumour Necrosis Factor Drug Response and Paradoxical Psoriasiform Reactions in Patients with Moderate-to-severe Psoriasis. Acta Derm. Venereol. 2021, 101, adv00448. [Google Scholar] [CrossRef]
- Leonardi, C.L.; Kimball, A.B.; Papp, K.A.; Yeilding, N.; Guzzo, C.; Wang, Y.; Li, S.; Dooley, L.T.; Gordon, K.B.; PHOENIX 1 study investigators. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet 2008, 371, 1665–1674. [Google Scholar] [CrossRef]
- Papp, K.A.; Langley, R.G.; Lebwohl, M.; Krueger, G.G.; Szapary, P.; Yeilding, N.; Guzzo, C.; Hsu, M.C.; Wang, Y.; Li, S.; et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet 2008, 371, 1675–1684. [Google Scholar] [CrossRef]
- Zweegers, J.; Groenewoud, J.M.M.; van den Reek, J.M.P.A.; Otero, M.E.; van de Kerkhof, P.C.M.; Driessen, R.J.B.; van Lümig, P.P.M.; Njoo, M.D.; Ossenkoppele, P.M.; Mommers, J.M.; et al. Comparison of the 1- and 5-year effectiveness of adalimumab, etanercept and ustekinumab in patients with psoriasis in daily clinical practice: Results from the prospective BioCAPTURE registry. Br. J. Dermatol. 2017, 176, 1001–1009. [Google Scholar] [CrossRef]
- Talamonti, M.; Botti, E.; Galluzzo, M.; Teoli, M.; Spallone, G.; Bavetta, M.; Chimenti, S.; Costanzo, A. Pharmacogenetics of psoriasis: HLA-Cw6 but not LCE3B/3C deletion nor TNFAIP3 polymorphism predisposes to clinical response to interleukin 12/23 blocker ustekinumab. Br. J. Dermatol. 2013, 169, 458–463. [Google Scholar] [CrossRef]
- Talamonti, M.; Galluzzo, M.; Chimenti, S.; Costanzo, A. HLA-C*06 and response to ustekinumab in Caucasian patients with psoriasis: Outcome and long-term follow-up. J. Am. Acad. Dermatol. 2016, 74, 374–375. [Google Scholar] [CrossRef]
- Talamonti, M.; Galluzzo, M.; van den Reek, J.M.; de Jong, E.M.; Lambert, J.L.W.; Malagoli, P.; Bianchi, L.; Costanzo, A. Role of the HLA-C*06 allele in clinical response to ustekinumab: Evidence from real life in a large cohort of European patients. Br. J. Dermatol. 2017, 177, 489–496. [Google Scholar] [CrossRef]
- Chiu, H.-Y.; Wang, T.-S.; Chan, C.-C.; Cheng, Y.-P.; Lin, S.-J.; Tsai, T.-F. Human leucocyte antigen-Cw6 as a predictor for clinical response to ustekinumab, an interleukin-12/23 blocker, in C hinese patients with psoriasis: A retrospective analysis. Br. J. Dermatol. 2014, 171, 1181–1188. [Google Scholar] [CrossRef]
- Galluzzo, M.; Boca, A.N.; Botti, E.; Potenza, C.; Malara, G.; Malagoli, P.; Vesa, S.; Chimenti, S.; Buzoianu, A.D.; Talamonti, M.; et al. IL12B (p40) Gene Polymorphisms Contribute to Ustekinumab Response Prediction in Psoriasis. Dermatology 2016, 232, 230–236. [Google Scholar] [CrossRef]
- Raposo, I.; Carvalho, C.; Bettencourt, A.; Da Silva, B.M.; Leite, L.; Selores, M.; Torres, T. Psoriasis pharmacogenetics: HLA-Cw*0602 as a marker of therapeutic response to ustekinumab. Eur. J. Dermatol. 2017, 27, 528–530. [Google Scholar] [CrossRef]
- Griffiths, C.E.M.; Strober, B.E.; van de Kerkhof, P.; Ho, V.; Fidelus-Gort, R.; Yeilding, N.; Guzzo, C.; Xia, Y.; Zhou, B.; Li, S.; et al. Comparison of Ustekinumab and Etanercept for Moderate-to-Severe Psoriasis. N. Engl. J. Med. 2010, 362, 118–128. [Google Scholar] [CrossRef]
- Li, K.; Huang, C.C.; Randazzo, B.; Li, S.; Szapary, P.; Curran, M.; Campbell, K.; Brodmerkel, C. HLA-C*06:02 Allele and Response to IL-12/23 Inhibition: Results from the Ustekinumab Phase 3 Psoriasis Program. J. Investig. Dermatol. 2016, 136, 2364–2371. [Google Scholar] [CrossRef]
- van Vugt, L.J.; van den Reek, J.M.P.A.; Hannink, G.; Coenen, M.J.H.; de Jong, E.M.G.J. Association of HLA-C*06:02 Status with Differential Response to Ustekinumab in Patients with Psoriasis: A Systematic Review and Meta-analysis. JAMA Dermatol. 2019, 155, 708. [Google Scholar] [CrossRef]
- Anzengruber, F.; Ghosh, A.; Maul, J.T.; Drach, M.; Navarini, A.A. Limited clinical utility of HLA-Cw6 genotyping for outcome prediction in psoriasis patients under ustekinumab therapy: A monocentric, retrospective analysis. Psoriasis Targets Ther. 2018, 8, 7–11. [Google Scholar] [CrossRef]
- Loft, N.D.; Skov, L.; Iversen, L.; Gniadecki, R.; Dam, T.N.; Brandslund, I.; Hoffmann, H.J.; Andersen, M.R.; Dessau, R.; Bergmann, A.C.; et al. Associations between functional polymorphisms and response to biological treatment in Danish patients with psoriasis. Pharmacogenom. J. 2018, 18, 494–500. [Google Scholar] [CrossRef]
- Prieto-Pérez, R.; Solano-López, G.; Cabaleiro, T.; Román, M.; Ochoa, D.; Talegón, M.; Baniandrés, O.; Estebaranz, J.L.L.; de la Cueva, P.; Daudén, E.; et al. The polymorphism rs763780 in the IL-17F gene is associated with response to biological drugs in patients with psoriasis. Pharmacogenomics 2015, 16, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Pérez, R.; Llamas-Velasco, M.; Cabaleiro, T.; Solano-López, G.; Márquez, B.; Román, M.; Ochoa, D.; Talegón, M.; Daudén, E.; Abad-Santos, F. Pharmacogenetics of ustekinumab in patients with moderate-to-severe plaque psoriasis. Pharmacogenomics 2017, 18, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Nani, P.; Ladopoulou, M.; Papaioannou, E.H.; Papagianni, E.D.; Antonatos, C.; Xiropotamos, P.; Kapsoritakis, A.; Potamianos, P.S.; Karmiris, K.; Tzathas, C.; et al. Pharmacogenetic Analysis of the MIR146A rs2910164 and MIR155 rs767649 Polymorphisms and Response to Anti-TNF Treatment in Patients with Crohn’s Disease and Psoriasis. Genes 2023, 14, 445. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Prieto-Pérez, R.; Llamas-Velasco, M.; Muñoz-Aceituno, E.; Reolid, A.; Saiz-Rodríguez, M.; Belmonte, C.; Román, M.; Dolores Ochoa, D.; Talegón, M.; et al. Polymor-phisms associated with adalimumab and infliximab response in moderate-to-severe plaque psoriasis. Pharmacogenomics 2018, 19, 7–16. [Google Scholar] [CrossRef]
- Batalla, A.; Coto, E.; Gómez, J.; Eiris, N.; González-Fernández, D.; Castro, C.G.-D.; Daudén, E.; Llamas-Velasco, M.; Prieto-Perez, R.; Abad-Santos, F.; et al. IL17RA gene variants and anti-TNF response among psoriasis patients. Pharmacogenom. J. 2018, 18, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Coto-Segura, P.; González-Fernández, D.; Batalla, A.; Gómez, J.; González-Lara, L.; Queiro, R.; Alonso, B.; Iglesias, S.; Coto, E. Common and rare CARD14 gene variants affect the antitumour necrosis factor response among patients with psoriasis. Br. J. Dermatol. 2016, 175, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Coto-Segura, P.; Batalla, A.; González-Fernández, D.; Gómez, J.; Santos-Juanes, J.; Queiro, R.; Alonso, B.; Iglesias, S.; Coto, E. CDKAL1 gene variants affect the anti-TNF response among Psoriasis patients. Int. Immunopharmacol. 2015, 29, 947–949. [Google Scholar] [CrossRef] [PubMed]
- Julià, A.; Ferrándiz, C.; Dauden, E.; Fonseca, E.; Fernández-López, E.; Sanchez-Carazo, J.L.; Vanaclocha, F.; Puig, L.; Moreno-Ramírez, D.; Lopez-Estebaranz, J.L.; et al. Association of the PDE3A-SLCO1C1 locus with the response to anti-TNF agents in psoriasis. Pharmacogenom. J. 2015, 15, 322–325. [Google Scholar] [CrossRef]
- Di Renzo, L.; Bianchi, A.; Saraceno, R.; Calabrese, V.; Cornelius, C.; Iacopino, L.; Chimenti, S.; De Lorenzo, A. −174G/C IL-6 gene promoter polymorphism predicts therapeutic response to TNF-α blockers. Pharm. Genom. 2012, 22, 134–142. [Google Scholar] [CrossRef]
- Connell, W.T.; Hong, J.; Liao, W. Genome-Wide Association Study of Ustekinumab Response in Psoriasis. Front. Immunol. 2022, 12, 815121. [Google Scholar] [CrossRef]
- Morelli, M.; Galluzzo, M.; Scarponi, C.; Madonna, S.; Scaglione, G.L.; Girolomoni, G.; Talamonti, M.; Bianchi, L.; Albanesi, C. Allelic Variants of HLA-C Upstream Region, PSORS1C3, MICA, TNFA and Genes Involved in Epidermal Homeostasis and Barrier Function Influence the Clinical Response to Anti-IL-12/IL-23 Treatment of Patients with Psoriasis. Vaccines 2022, 10, 1977. [Google Scholar] [CrossRef]
- Sawyer, L.M.; Malottki, K.; Sabry-Grant, C.; Yasmeen, N.; Wright, E.; Sohrt, A.; Borg, E.; Warren, R.B. Assessing the relative efficacy of interleukin-17 and interleukin-23 targeted treatments for moderate-to-severe plaque psoriasis: A systematic review and network meta-analysis of PASI response. PLoS ONE 2019, 14, e0220868. [Google Scholar] [CrossRef]
- Bai, F.; Li, G.G.; Liu, Q.; Niu, X.; Li, R.; Ma, H. Short-Term Efficacy and Safety of IL-17, IL-12/23, and IL-23 Inhibitors Brodalumab, Secukinumab, Ixekizumab, Ustekinumab, Guselkumab, Tildrakizumab, and Risankizumab for the Treatment of Moderate to Severe Plaque Psoriasis: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. J. Immunol. Res. 2019, 2019, 2546161. [Google Scholar]
- Costanzo, A.; Bianchi, L.; Flori, M.L.; Malara, G.; Stingeni, L.; Bartezaghi, M.; Carraro, L.; Castellino, G. Secukinumab shows high efficacy irrespective of HLA-Cw6 status in patients with moderate-to-severe plaque-type psoriasis: SUPREME study. Br. J. Dermatol. 2018, 179, 1072–1080. [Google Scholar] [CrossRef]
- Papini, M.; Cusano, F.; Romanelli, M.; Burlando, M.; Stinco, G.; Girolomoni, G.; Peris, K.; Potenza, C.; Offidani, A.; Bartezaghi, M.; et al. Secukinumab shows high efficacy irrespective of HLA-Cw6 status in patients with moderate-to-severe plaque-type psoriasis: Results from extension phase of the SUPREME study. Br. J. Dermatol. 2019, 181, 413–414. [Google Scholar] [CrossRef]
- Anzengruber, F.; Drach, M.; Maul, J.-T.; Kolios, A.; Meier, B.; Navarini, A.A. Therapy response was not altered by HLA-Cw6 status in psoriasis patients treated with secukinumab: A retrospective case series. J. Eur. Acad. Dermatol. Venereol. 2018, 32, e274–e276. [Google Scholar] [CrossRef]
- Galluzzo, M.; D’Adamio, S.; Silvaggio, D.; Lombardo, P.; Bianchi, L.; Talamonti, M. In which patients the best efficacy of secukinumab? Update of a real-life analysis after 136 weeks of treatment with secukinumab in moderate-to-severe plaque psoriasis. Expert Opin. Biol. Ther. 2020, 20, 173–182. [Google Scholar] [CrossRef]
- Morelli, M.; Galluzzo, M.; Madonna, S.; Scarponi, C.; Scaglione, G.L.; Galluccio, T.; Andreani, M.; Pallotta, S.; Girolomoni, G.; Bianchi, L.; et al. HLA-Cw6 and other HLA-C alleles, as well as MICB-DT, DDX58, and TYK2 genetic variants associate with optimal response to anti-IL-17A treatment in patients with psoriasis. Expert Opin. Biol. Ther. 2021, 21, 259–270. [Google Scholar] [CrossRef]
- Van Vugt, L.; Reek, J.V.D.; Meulewaeter, E.; Hakobjan, M.; Heddes, N.; Traks, T.; Kingo, K.; Galluzzo, M.; Talamonti, M.; Lambert, J.; et al. Response to IL -17A inhibitors secukinumab and ixekizumab cannot be explained by genetic variation in the protein-coding and untranslated regions of the IL -17A gene: Results from a multicentre study of four European psoriasis cohorts. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 112–118. [Google Scholar] [CrossRef]
- Verbelen, M.; Weale, M.E.; Lewis, C.M. Cost-effectiveness of pharmacogenetic-guided treatment: Are we there yet? Pharmacogenom. J. 2017, 17, 395–402. [Google Scholar] [CrossRef]
- Ivanov, M.; Barragan, I.; Ingelman-Sundberg, M. Epigenetic mechanisms of importance for drug treatment. Trends Pharmacol. Sci. 2014, 35, 384–396. [Google Scholar] [CrossRef]
- Zhou, F.; Wang, W.; Shen, C.; Li, H.; Zuo, X.; Zheng, X.; Yue, M.; Zhang, C.; Yu, L.; Chen, M.; et al. Epigenome-Wide Association Analysis Identified Nine Skin DNA Methylation Loci for Psoriasis. J. Investig. Dermatol. 2016, 136, 779–787. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Cabaleiro, T.; Sanz-García, A.; Llamas-Velasco, M.; Saiz-Rodríguez, M.; Prieto-Pérez, R.; Talegón, M.; Román, M.; Ochoa, D.; Reolid, A.; et al. Epigenetic biomarkers associated with antitumour necrosis factor drug response in moderate-to-severe psoriasis. Br. J. Dermatol. 2018, 178, 798–800. [Google Scholar] [CrossRef]
- Ovejero-Benito, M.C.; Reolid, A.; Sánchez-Jiménez, P.; Saiz-Rodríguez, M.; Muñoz-Aceituno, E.; Llamas-Velasco, M.; Martín-Vilchez, S.; Cabaleiro, T.; Román, M.; Ochoa, D.; et al. Histone modifications associated with biological drug response in moderate-to-severe psoriasis. Exp. Dermatol. 2018, 27, 1361–1371. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berna-Rico, E.; Perez-Bootello, J.; Abbad-Jaime de Aragon, C.; Gonzalez-Cantero, A. Genetic Influence on Treatment Response in Psoriasis: New Insights into Personalized Medicine. Int. J. Mol. Sci. 2023, 24, 9850. https://doi.org/10.3390/ijms24129850
Berna-Rico E, Perez-Bootello J, Abbad-Jaime de Aragon C, Gonzalez-Cantero A. Genetic Influence on Treatment Response in Psoriasis: New Insights into Personalized Medicine. International Journal of Molecular Sciences. 2023; 24(12):9850. https://doi.org/10.3390/ijms24129850
Chicago/Turabian StyleBerna-Rico, Emilio, Javier Perez-Bootello, Carlota Abbad-Jaime de Aragon, and Alvaro Gonzalez-Cantero. 2023. "Genetic Influence on Treatment Response in Psoriasis: New Insights into Personalized Medicine" International Journal of Molecular Sciences 24, no. 12: 9850. https://doi.org/10.3390/ijms24129850
APA StyleBerna-Rico, E., Perez-Bootello, J., Abbad-Jaime de Aragon, C., & Gonzalez-Cantero, A. (2023). Genetic Influence on Treatment Response in Psoriasis: New Insights into Personalized Medicine. International Journal of Molecular Sciences, 24(12), 9850. https://doi.org/10.3390/ijms24129850






