Molecular Determinants of Species Specificity of α-Conotoxin TxIB towards Rat and Human α6/α3β4 Nicotinic Acetylcholine Receptors
Abstract
1. Introduction
2. Results
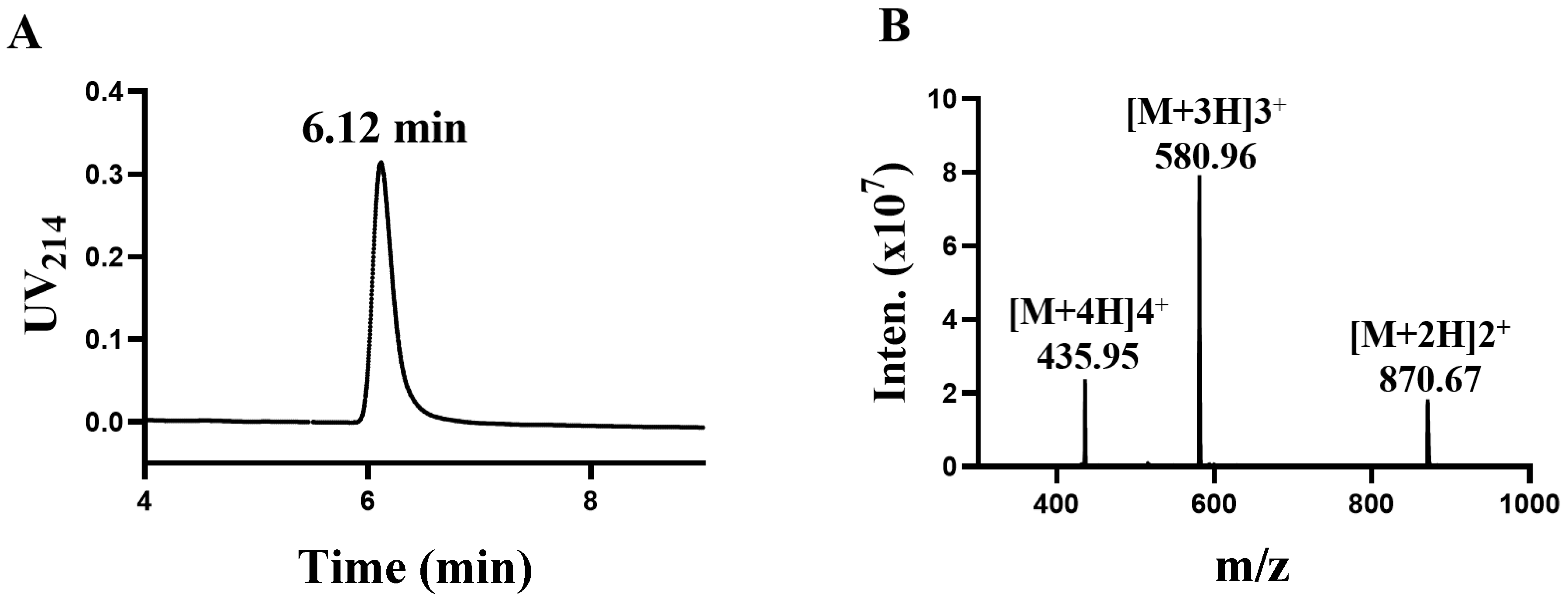
2.1. Synthesis and Identification of TxIB
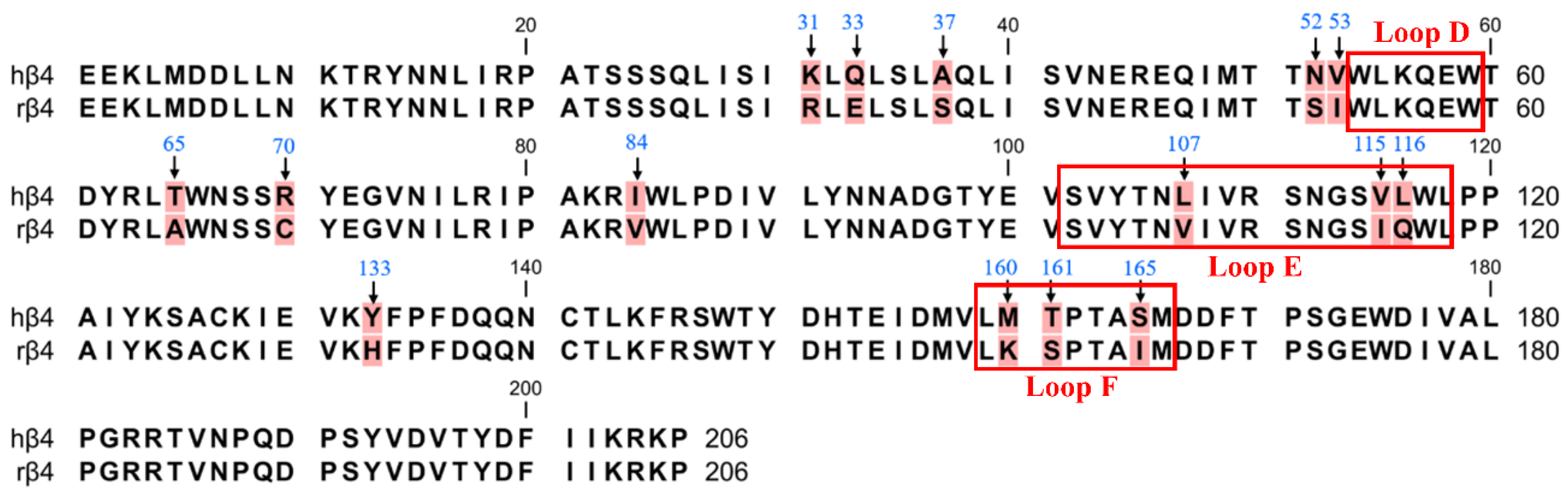
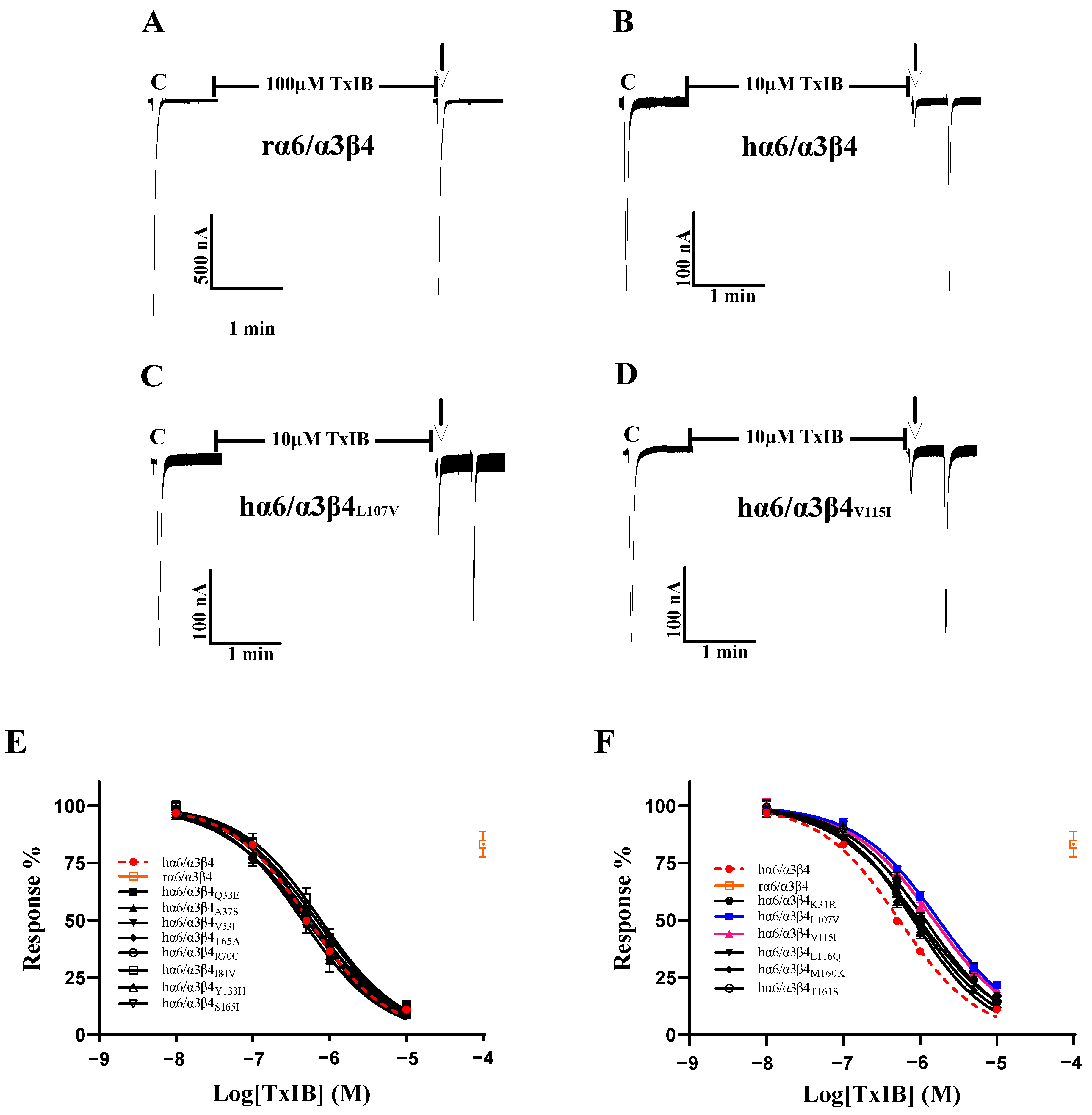
2.2. Identification of Crucial Residues Affecting the Blocking Activity of Human β4 Subunits with TxIB
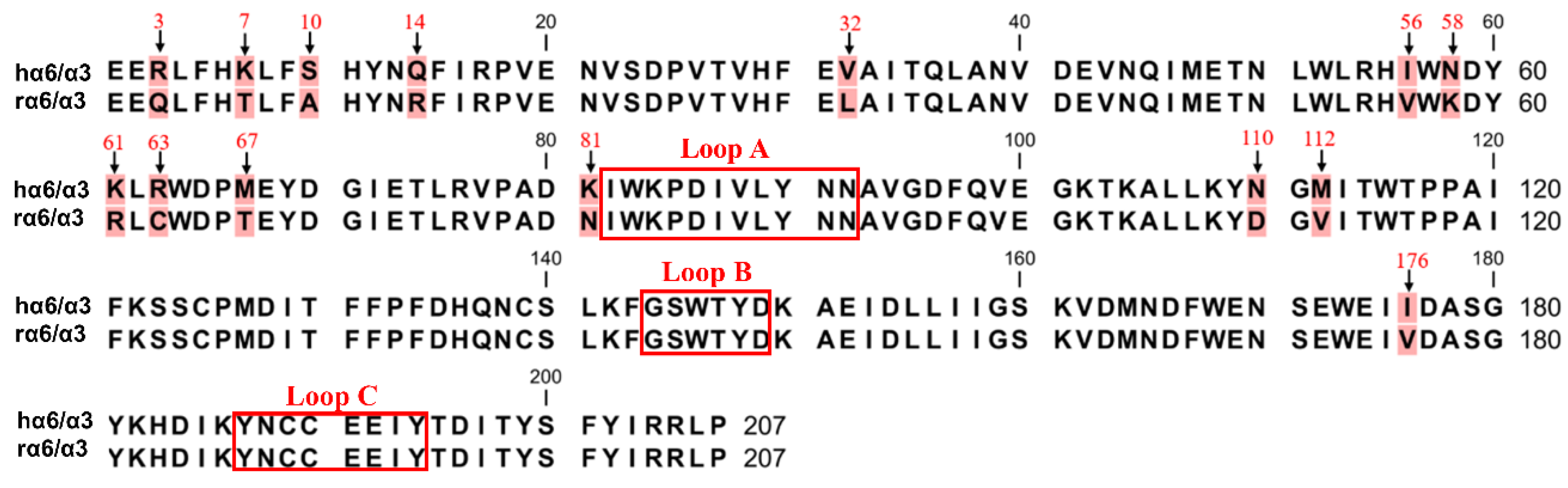
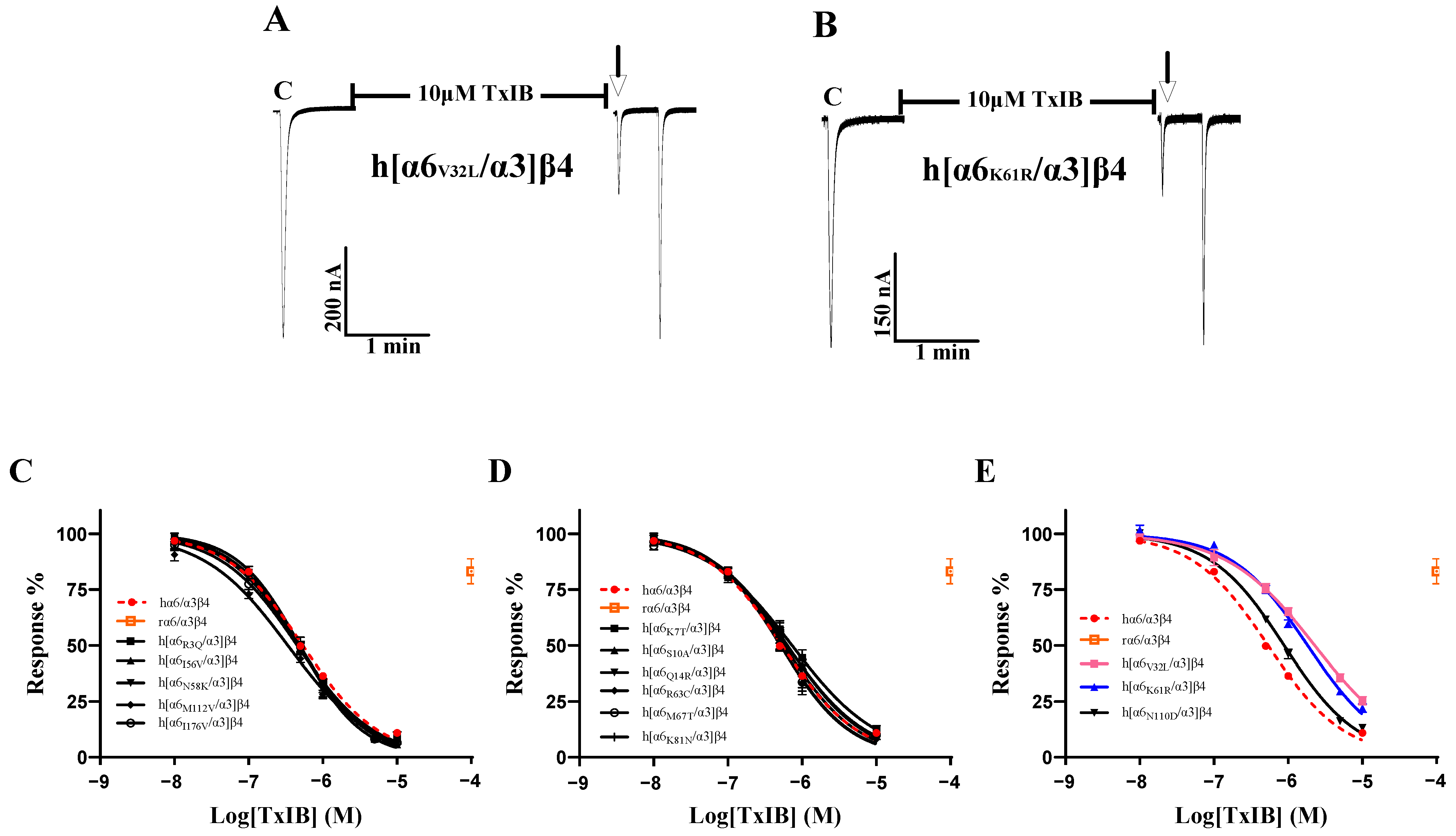
2.3. Identification of Crucial Residues Affecting the Blocking Activity of Human α6/α3 Subunits with TxIB
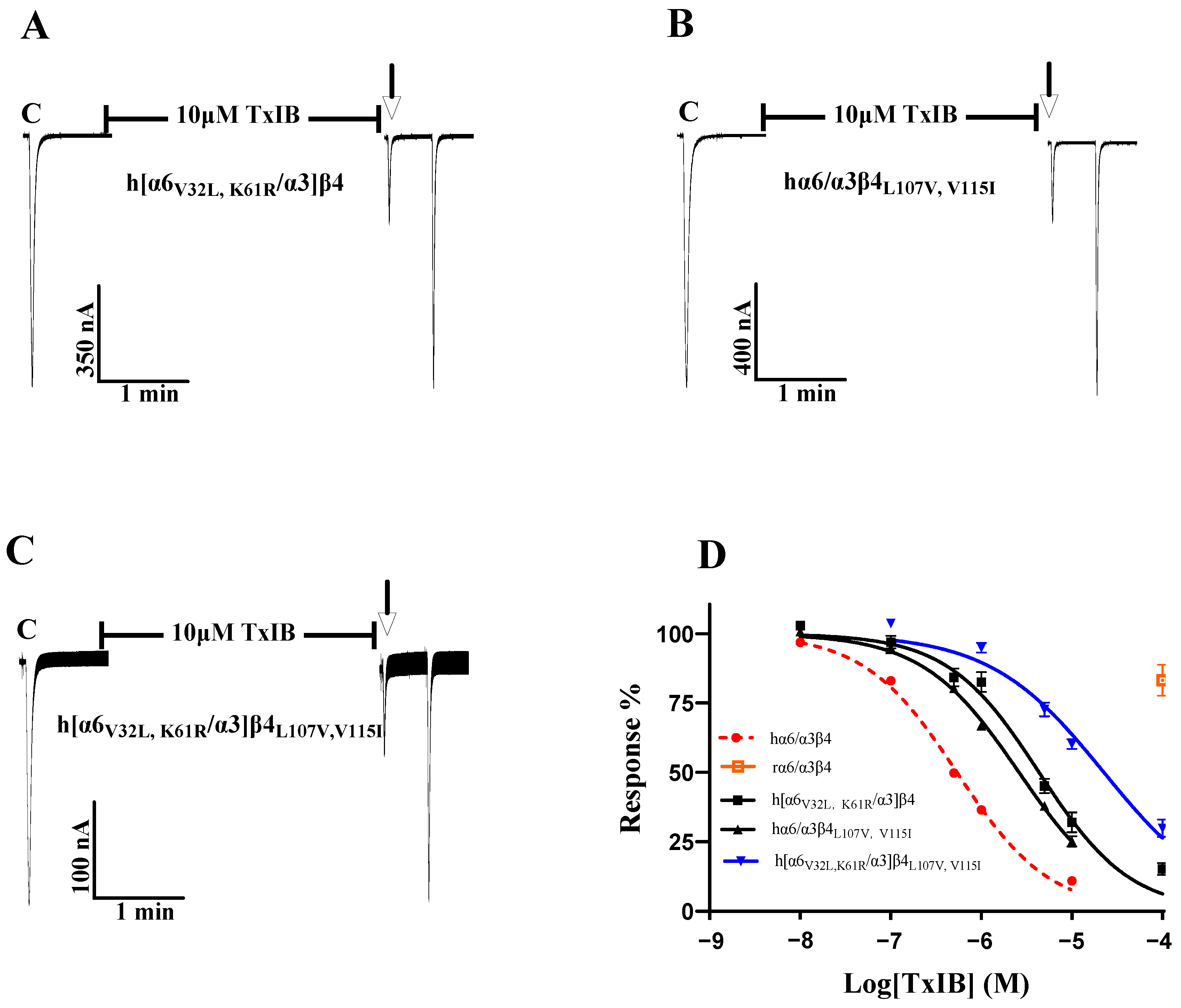
2.4. Identification of Multiple Amino Acid Residues of TxIB That Are Highly Effective against Human α6/α3β4 nAChR
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Peptide Synthesis
4.3. Site-Directed Mutagenesis of α6/α3 and β4 Subunits
4.4. cRNA Synthesis and Injection
4.5. Electrophysiological Assay
4.6. Data Analysis
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Hone, A.J.; Talley, T.T.; Bobango, J.; Melo, C.H.; Hararah, F.; Gajewiak, J.B.; Christensen, S.B.; Harvey, P.J.; Craik, D.J.; McIntosh, J.M. Molecular determinants of α-conotoxin potency for inhibition of human and rat alpha 6 beta 4 nicotinic acetylcholine receptors. J. Biol. Chem. 2018, 293, 17838–17852. [Google Scholar] [CrossRef] [PubMed]
- Sine, S.M.; Engel, A.G. Recent advances in Cys-loop receptor structure and function. Nature 2006, 440, 448–455. [Google Scholar] [CrossRef]
- Cox, B.C.; Marritt, A.M.; Perry, D.C.; Kellar, K.J. Transport of multiple nicotinic acetylcholine receptors in the rat optic nerve: High densities of receptors containing alpha6 and beta3 subunits. J. Neurochem. 2008, 105, 1924–1938. [Google Scholar] [CrossRef] [PubMed]
- Azam, L.; Yoshikami, D.; McIntosh, J.M. Amino acid residues that confer high selectivity of the alpha6 nicotinic acetylcholine receptor subunit to alpha-conotoxin MII[S4A,E11A,L15A]. J. Biol. Chem. 2008, 283, 11625–11632. [Google Scholar] [CrossRef] [PubMed]
- Papke, R.L.; Dwoskin, L.P.; Crooks, P.A.; Zheng, G.; Zhang, Z.; McIntosh, J.M.; Stokes, C. Extending the analysis of nicotinic receptor antagonists with the study of alpha6 nicotinic receptor subunit chimeras. Neuropharmacology 2008, 54, 1189–1200. [Google Scholar] [CrossRef]
- Pons, S.; Fattore, L.; Cossu, G.; Tolu, S.; Porcu, E.; McIntosh, J.M.; Changeux, J.P.; Maskos, U.; Fratta, W. Crucial role of alpha4 and alpha6 nicotinic acetylcholine receptor subunits from ventral tegmental area in systemic nicotine self-administration. J. Neurosci. 2008, 28, 12318–12327. [Google Scholar] [CrossRef] [PubMed]
- Jackson, K.J.; McIntosh, J.M.; Brunzell, D.H.; Sanjakdar, S.S.; Damaj, M.I. The role of alpha6-containing nicotinic acetylcholine receptors in nicotine reward and withdrawal. J. Pharmacol. Exp. Ther. 2009, 331, 547–554. [Google Scholar] [CrossRef]
- You, S.; Li, X.D.; Xiong, J.; Zhu, X.Y.; Zhangsun, D.T.; Zhu, X.P.; Luo, S.L. alpha-Conotoxin TxIB: A Uniquely Selective Ligand for alpha 6/alpha 3 beta 2 beta 3 Nicotinic Acetylcholine Receptor Attenuates Nicotine-Induced Conditioned Place Preference in Mice. Mar. Drugs 2019, 17, 490. [Google Scholar] [CrossRef]
- Yu, J.P.; Zhu, X.P.; Yang, Y.; Luo, S.L.; Zhangsun, D.T. Expression in Escherichia coli of fusion protein comprising -conotoxin TxIB and preservation of selectivity to nicotinic acetylcholine receptors in the purified product. Chem. Biol. Drug Des. 2018, 91, 349–358. [Google Scholar] [CrossRef]
- Quik, M.; Bordia, T.; O’Leary, K. Nicotinic receptors as CNS targets for Parkinson’s disease. Biochem. Pharmacol. 2007, 74, 1224–1234. [Google Scholar] [CrossRef]
- Hone, A.J.; McIntosh, J.M. Nicotinic acetylcholine receptors in neuropathic and inflammatory pain. FEBS Lett. 2018, 592, 1045–1062. [Google Scholar] [CrossRef] [PubMed]
- Hone, A.J.; Meyer, E.L.; McIntyre, M.; McIntosh, J.M. Nicotinic acetylcholine receptors in dorsal root ganglion neurons include the alpha6beta4* subtype. FASEB J. 2012, 26, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Marucci, G.; Dal Ben, D.; Buccioni, M.; Marti Navia, A.; Spinaci, A.; Volpini, R.; Lambertucci, C. Update on novel purinergic P2X3 and P2X2/3 receptor antagonists and their potential therapeutic applications. Expert Opin. Ther. Patents 2019, 29, 943–963. [Google Scholar] [CrossRef] [PubMed]
- Kuryatov, A.; Olale, F.; Cooper, J.; Choi, C.; Lindstrom, J. Human α6 AChR subtypes: Subunit composition, assembly, and pharmacological responses. Neuropharmacology 2000, 39, 2570–2590. [Google Scholar] [CrossRef] [PubMed]
- Cheryl, D.; Baldomero, M.O.; James, E.G.; Sarah, T.S.; Maren, W.; Alexander, K.; Doju, Y.; Jon, M.L.; McIntosh, J.M. α-Conotoxin PIA Is Selective for α6 Subunit-Containing Nicotinic Acetylcholine Receptors. J. Neurosci. 2003, 23, 8445–8452. [Google Scholar] [CrossRef]
- Satkunanathan, N.; Livett, B.; Gayler, K.; Sandall, D.; Down, J.; Khalil, Z. Alpha-conotoxin Vc1.1 alleviates neuropathic pain and accelerates functional recovery of injured neurones. Brain Res. 2005, 1059, 149–158. [Google Scholar] [CrossRef]
- Gao, F.; Chen, D.; Ma, X.; Sudweeks, S.; Yorgason, J.T.; Gao, M.; Turner, D.; Eaton, J.B.; McIntosh, J.M.; Lukas, R.J.; et al. Alpha6-containing nicotinic acetylcholine receptor is a highly sensitive target of alcohol. Neuropharmacology 2019, 149, 45–54. [Google Scholar] [CrossRef]
- Kamens, H.M.; Hoft, N.R.; Cox, R.J.; Miyamoto, J.H.; Ehringer, M.A. The alpha6 nicotinic acetylcholine receptor subunit influences ethanol-induced sedation. Alcohol 2012, 46, 463–471. [Google Scholar] [CrossRef]
- Zhang, B.J.; Ren, M.M.; Xiong, Y.; Li, H.N.; Wu, Y.; Fu, Y.; Zhangsun, D.T.; Dong, S.; Luo, S.L. Cysteine [2,4] Disulfide Bond as a New Modifiable Site of alpha-Conotoxin TxIB. Mar. Drugs 2021, 19, 119. [Google Scholar] [CrossRef]
- Luo, S.; Zhangsun, D.; Wu, Y.; Zhu, X.; Hu, Y.; McIntyre, M.; Christensen, S.; Akcan, M.; Craik, D.J.; McIntosh, J.M. Characterization of a novel alpha-conotoxin from conus textile that selectively targets alpha6/alpha3beta2beta3 nicotinic acetylcholine receptors. J. Biol. Chem. 2013, 288, 894–902. [Google Scholar] [CrossRef]
- Li, X.; Wang, S.; Zhu, X.; Zhangsun, D.; Wu, Y.; Luo, S. Effects of Cyclization on Activity and Stability of alpha-Conotoxin TxIB. Mar. Drugs 2020, 18, 180. [Google Scholar] [CrossRef] [PubMed]
- Wittenberg, R.E.; Wolfman, S.L.; De Biasi, M.; Dani, J.A. Nicotinic acetylcholine receptors and nicotine addiction: A brief introduction. Neuropharmacology 2020, 177, 108256. [Google Scholar] [CrossRef] [PubMed]
- Hone, A.J.; Kaas, Q.; Kearns, I.; Hararah, F.; Gajewiak, J.; Christensen, S.; Craik, D.J.; McIntosh, J.M. Computational and Functional Mapping of Human and Rat alpha6beta4 Nicotinic Acetylcholine Receptors Reveals Species-Specific Ligand-Binding Motifs. J. Med. Chem. 2021, 64, 1685–1700. [Google Scholar] [CrossRef] [PubMed]
- Gharpure, A.; Teng, J.; Zhuang, Y.; Noviello, C.M.; Walsh, R.M., Jr.; Cabuco, R.; Howard, R.J.; Zaveri, N.T.; Lindahl, E.; Hibbs, R.E. Agonist Selectivity and Ion Permeation in the alpha3beta4 Ganglionic Nicotinic Receptor. Neuron 2019, 104, 501–511.e6. [Google Scholar] [CrossRef]
- Dash, B.; Bhakta, M.; Chang, Y.C.; Lukas, R.J. Identification of N-terminal Extracellular Domain Determinants in Nicotinic Acetylcholine Receptor (nAChR) alpha 6 Subunits That Influence Effects of Wild-type or Mutant beta 3 Subunits on Function of alpha 6 beta 2*-or alpha 6 beta 4*-nAChR. J. Biol. Chem. 2011, 286, 37976–37989. [Google Scholar] [CrossRef]
- Noviello, C.M.; Gharpure, A.; Mukhtasimova, N.; Cabuco, R.; Baxter, L.; Borek, D.; Sine, S.M.; Hibbs, R.E. Structure and gating mechanism of the alpha 7 nicotinic acetylcholine receptor. Cell 2021, 184, 2121–2134. [Google Scholar] [CrossRef]
- Hone, A.J.; Fisher, F.; Christensen, S.; Gajewiak, J.; Larkin, D.; Whiteaker, P.; McIntosh, J.M. PeIA-5466: A Novel Peptide Antagonist Containing Non-natural Amino Acids That Selectively Targets alpha3beta2 Nicotinic Acetylcholine Receptors. J. Med. Chem. 2019, 62, 6262–6275. [Google Scholar] [CrossRef]
- Hone, A.J.; Scadden, M.; Gajewiak, J.; Christensen, S.; Lindstrom, J.; McIntosh, J.M. alpha-Conotoxin PeIA[S9H,V10A,E14N] potently and selectively blocks alpha6beta2beta3 versus alpha6beta4 nicotinic acetylcholine receptors. Mol. Pharmacol. 2012, 82, 972–982. [Google Scholar] [CrossRef]
- Zhu, X.P.; Wang, S.; Kaas, Q.; Yu, J.P.; Wu, Y.; Harvey, P.J.; Zhangsun, D.; Craik, D.J.; Luo, S.L. Discovery, Characterization, and Engineering of LvIC, an alpha 4/4-Conotoxin That Selectively Blocks Rat alpha 6/alpha 3 beta 4 Nicotinic Acetylcholine Receptors. J. Med. Chem. 2023, 66, 2020–2031. [Google Scholar] [CrossRef]
- Exley, R.; Maubourguet, N.; David, V.; Eddine, R.; Evrard, A.; Pons, S.; Marti, F.; Threlfell, S.; Cazala, P.; McIntosh, J.M.; et al. Distinct contributions of nicotinic acetylcholine receptor subunit alpha4 and subunit alpha6 to the reinforcing effects of nicotine. Proc. Natl. Acad. Sci. USA 2011, 108, 7577–7582. [Google Scholar] [CrossRef]
- Luo, S.L.; Zhangsun, D.T.; Schroeder, C.I.; Zhu, X.P.; Hu, Y.Y.; Wu, Y.; Weltzin, M.M.; Eberhard, S.; Kaas, Q.; Craik, D.J.; et al. A novel alpha 4/7-conotoxin LvIA from Conus lividus that selectively blocks alpha 3 beta 2 vs. alpha 6/alpha 3 beta 2 beta 3 nicotinic acetylcholine receptors. FASEB J. 2014, 28, 1842–1853. [Google Scholar] [CrossRef] [PubMed]
- Kasheverov, I.E.; Chugunov, A.O.; Kudryavtsev, D.S.; Ivanov, I.A.; Zhmak, M.N.; Shelukhina, I.V.; Spirova, E.N.; Tabakmakher, V.M.; Zelepuga, E.A.; Efremov, R.G.; et al. High-Affinity alpha-Conotoxin PnIA Analogs Designed on the Basis of the Protein Surface Topography Method. Sci. Rep. 2016, 6, 36848. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, S.A.; Christie, M.J. Conotoxin Interactions with alpha9alpha10-nAChRs: Is the alpha9alpha10-Nicotinic Acetylcholine Receptor an Important Therapeutic Target for Pain Management? Toxins 2015, 7, 3916–3932. [Google Scholar] [CrossRef]
- Sandager-Nielsen, K.; Ahring, P.K.; Klein, J.; van Hout, M.; Thaneshwaran, S.; Dos Santos, A.B.; Jacobsen, T.A.; Amrutkar, D.V.; Peters, D.; Jensen, A.A.; et al. Characterization of AN317, a novel selective agonist of alpha6beta2-containing nicotinic acetylcholine receptors. Biochem. Pharmacol. 2020, 174, 113786. [Google Scholar] [CrossRef] [PubMed]
- Hogg, R.C.; Raggenbass, M.; Bertrand, D. Nicotinic acetylcholine receptors: From structure to brain function. Rev. Physiol. Biochem. Pharmacol. 2003, 147, 1–46. [Google Scholar] [CrossRef]
- Gu, S.; Matta, J.A.; Davini, W.B.; Dawe, G.B.; Lord, B.; Bredt, D.S. alpha6-Containing Nicotinic Acetylcholine Receptor Reconstitution Involves Mechanistically Distinct Accessory Components. Cell Rep. 2019, 26, 866–874.e3. [Google Scholar] [CrossRef] [PubMed]
- Knowland, D.; Gu, S.; Eckert, W.A., 3rd; Dawe, G.B.; Matta, J.A.; Limberis, J.; Wickenden, A.D.; Bhattacharya, A.; Bredt, D.S. Functional alpha6beta4 acetylcholine receptor expression enables pharmacological testing of nicotinic agonists with analgesic properties. J. Clin. Investig. 2020, 130, 6158–6170. [Google Scholar] [CrossRef]
- Bernier, L.P.; Ase, A.R.; Seguela, P. P2X receptor channels in chronic pain pathways. Br. J. Pharmacol. 2018, 175, 2219–2230. [Google Scholar] [CrossRef]
- Unwin, N. Refined structure of the nicotinic acetylcholine receptor at 4A resolution. J. Mol. Biol. 2005, 346, 967–989. [Google Scholar] [CrossRef]
- Almouzni, G.; Wolffe, A.P. Nuclear assembly, structure, and function: The use of Xenopus in vitro systems. Exp. Cell Res. 1993, 205, 1–15. [Google Scholar] [CrossRef]
- Wu, X.S.; Wu, Y.; Zhu, F.R.; Yang, Q.Y.; Wu, Q.Q.; Zhangsun, D.T.; Luo, S.L. Optimal Cleavage and Oxidative Folding of alpha-Conotoxin TxIB as a Therapeutic Candidate Peptide. Mar. Drugs 2013, 11, 3537–3553. [Google Scholar] [CrossRef] [PubMed]


| nAChRs | EC50 (95% CI) a (μM) | Hill Slope | Ratio b |
|---|---|---|---|
| hα6/α3β4 | 138 (121–158) | 1.4 (1.2–1.7) | 1 |
| hα6/α3β4K31R | 129 (111–150) | 1.3 (1.1–1.6) | 0.9 |
| hα6/α3β4Q33E | 173 (151–199) | 1.2 (1.1–1.5) | 1.3 |
| hα6/α3β4A37S | 94 (80.6–111) | 1.1 (1.0–1.4) | 0.7 |
| hα6/α3β4V53I | 95 (86–108) | 1.6 (1.2–2.3) | 0.7 |
| hα6/α3β4T65A | 157 (137–183) | 1.3 (1.1–1.6) | 1.1 |
| hα6/α3β4R70C | 126 (111–141) | 1.2 (1.1–1.5) | 0.9 |
| hα6/α3β4I84V | 135 (119–157) | 1.1 (1.0–1.4) | 0.9 |
| hα6/α3β4L107V | 65 (55–75) | 1.9 (1.1–3.1) | 0.4 |
| hα6/α3β4V115I | 112 (97–149) | 1.4 (1.0–2.2) | 0.8 |
| hα6/α3β4L116Q | 161 (140–184) | 1.4 (1.2–1.7) | 1.1 |
| hα6/α3β4Y133H | 195 (160–237) | 1.2 (0.9–1.4) | 1.4 |
| hα6/α3β4M160K | 96 (69–131) | 0.9 (0.7–1.3) | 0.7 |
| hα6/α3β4T161S | 163 (139–192) | 1.1 (0.9–1.4) | 1.2 |
| hα6/α3β4S165I | 51 (41–58) | 2.9 (1.8–4.9) | 0.4 |
| nAChRs | IC50 (95% CI) a (nM) | Hill Slope | Ratio b |
|---|---|---|---|
| hα6/α3β4 | 537 (492–588) | 0.8 (0.8–0.9) | 1 |
| hα6/α3β4K31R | 1173 (994–1394) | 0.8 (0.7–0.9) | 2.2 |
| hα6/α3β4Q33E | 446 (359–553) | 0.9 (0.7–1.0) | 0.8 |
| hα6/α3β4A37S | 559 (507–616) | 0.9 (0.8–1.0) | 1.1 |
| hα6/α3β4V53I | 589 (531–655) | 0.8 (0.7–0.9) | 1.1 |
| hα6/α3β4T65A | 551 (491–619) | 0.9 (0.8–1.0) | 1 |
| hα6/α3β4R70C | 503 (430–590) | 0.8 (0.7–1.0) | 0.9 |
| hα6/α3β4I84V | 767 (631–946) | 0.8 (0.8–0.9) | 1.4 |
| hα6/α3β4L107V | 1760 (620–1914) | 0.8 (0.7–0.9) | 3.3 |
| hα6/α3β4V115I | 1525 (1388–1742) | 0.8 (0.7–0.9) | 2.8 |
| hα6/α3β4L116Q | 910 (794–1048) | 0.8 (0.7–0.9) | 1.7 |
| hα6/α3β4Y133H | 681 (542–864) | 0.8 (0.7–1.0) | 1.3 |
| hα6/α3β4M160K | 825 (680–1017) | 0.9 (0.7–1.1) | 1.5 |
| hα6/α3β4T161S | 977 (775–1243) | 0.8 (0.6–0.9) | 1.8 |
| hα6/α3β4S165I | 547 (464–645) | 0.7 (0.6–0.9) | 1 |
| nAChRs | EC50 (95% CI) a (μM) | Hill Slope | Ratio b |
|---|---|---|---|
| hα6/α3β4 | 138 (121–158) | 1.4 (1.2–1.7) | 1 |
| h[α6R3Q/α3]β4 | 137 (117–159) | 1.4 (1.2–1.8) | 1 |
| h[α6K7T/α3]β4 | 154 (127–18) | 1.5 (1.1–1.9) | 1.1 |
| h[α6S10A/α3]β4 | 175 (142–217) | 1.6 (1.2–2.3) | 1.3 |
| h[α6Q14R/α3]β4 | 216 (191–243) | 1.4 (1.2–1.6) | 1.6 |
| h[α6V32L/α3]β4 | 167 (146–192) | 1.5 (1.3–1.9) | 1.2 |
| h[α6I56V/α3]β4 | 153 (136–173) | 1.3 (1.1–1.5) | 1.1 |
| h[α6N58K/α3]β4 | 176 (156–199) | 1.4 (1.2–1.7) | 1.3 |
| h[α6K61R/α3]β4 | 202 (178–229) | 1.4 (1.2–1.7) | 1.5 |
| h[α6R63C/α3]β4 | 150 (131–173) | 1.5 (1.2–1.8) | 1.1 |
| h[α6M67T/α3]β4 | 122 (91–166) | 1.4 (0.9–2.2) | 0.9 |
| h[α6K81N/α3]β4 | 171 (154–190) | 1.4 (1.3–1.7) | 1.2 |
| h[α6N110D/α3]β4 | 182 (146–227) | 1.2 (0.9–1.6) | 1.3 |
| h[α6M112V/α3]β4 | 109 (94–128) | 1.4 (1.1–1.8) | 0.8 |
| h[α6I176V/α3]β4 | 125 (130–139) | 1.7 (1.4–2.1) | 0.9 |
| nAChRs | IC50 (95% CI) a (nM) | Hill Slope | Ratio b |
|---|---|---|---|
| hα6/α3β4 | 537 (492–588) | 0.8 (0.8–0.9) | 1 |
| h[α6R3Q/α3]β4 | 486 (434–545) | 0.9 (0.8–1.1) | 0.9 |
| h[α6K7T/α3]β4 | 732 (615–876) | 0.8 (0.6–0.9) | 1.4 |
| h[α6S10A/α3]β4 | 624 (529–737) | 0.8 (0.7–0.9) | 1.2 |
| h[α6Q14R/α3]β4 | 514 (421–629) | 0.9 (0.7–1.2) | 1 |
| h[α6V32L/α3]β4 | 2283 (1985–2631) | 0.7 (0.7–0.8) | 4.2 |
| h[α6I56V/α3]β4 | 489 (427–559) | 1.0 (0.9–1.2) | 0.9 |
| h[α6N58K/α3]β4 | 471 (409–541) | 0.9 (0.8–1.1) | 0.9 |
| h[α6K61R/α3]β4 | 1833 (1609–2097) | 0.8 (0.7–0.9) | 3.4 |
| h[α6R63C/α3]β4 | 512 (439–599) | 0.9 (0. 8–1.1) | 0.9 |
| h[α6M67T/α3]β4 | 567 (483–668) | 0.9 (0.7–1.0) | 1.1 |
| h[α6K81N/α3]β4 | 634 (561–718) | 0.8 (0.7–0.9) | 1.2 |
| h[α6N110D/α3]β4 | 884 (808–970) | 0.9 (0.8–1.0) | 1.6 |
| h[α6M112V/α3]β4 | 337 (293–388) | 0.8 (0.7–0.9) | 0.6 |
| h[α6I176V/α3]β4 | 451 (388–523) | 0.8 (0.7–0.9) | 0.8 |
| nAChRs | EC50 (95% CI) a (μM) | Hill Slope | Ratio b | n |
|---|---|---|---|---|
| hα6/α3β4 | 138 (121–158) | 1.4 (1.2–1.7) | 1 | 9 |
| hα6/α3β4L107V, V115I | 94 (79–112) | 1.5 (1.1–2.1) | 0.7 | 10 |
| h[α6V32L, K61R/α3]β4 | 246 (227–267) | 1.2 (1.1–1.3) | 1.8 | 7 |
| h[α6V32L, K61R/α3]β4L107V,V115I | 133 (115–154) | 1.2 (1.0–1.5) | 0.9 | 7 |
| nAChRs | IC50 (95% CI) a (nM) | Hill Slope | Ratio b |
|---|---|---|---|
| hα6/α3β4 | 537 (492–588) | 0.9 (0.8–0.9) | 1 |
| hα6/α3β4L107V, V115I | 2608 (2386–2854) | 0.8 (0.8–0.9) | 4.9 |
| h[α6V32L, K61R/α3]β4 | 4342 (3633–5217) | 0.8 (0.7–1) | 8.1 |
| h[α6V32L, K61R/α3]β4L107V,V115I | 22,550 (17,860–29,170) | 0.8 (0.6–0.9) | 42 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, T.; Qin, Y.; Zhao, J.; Dong, J.; Qi, P.; Zhang, P.; Zhangsun, D.; Zhu, X.; Yu, J.; Luo, S. Molecular Determinants of Species Specificity of α-Conotoxin TxIB towards Rat and Human α6/α3β4 Nicotinic Acetylcholine Receptors. Int. J. Mol. Sci. 2023, 24, 8618. https://doi.org/10.3390/ijms24108618
Xie T, Qin Y, Zhao J, Dong J, Qi P, Zhang P, Zhangsun D, Zhu X, Yu J, Luo S. Molecular Determinants of Species Specificity of α-Conotoxin TxIB towards Rat and Human α6/α3β4 Nicotinic Acetylcholine Receptors. International Journal of Molecular Sciences. 2023; 24(10):8618. https://doi.org/10.3390/ijms24108618
Chicago/Turabian StyleXie, Ting, Yuan Qin, Jinyuan Zhao, Jianying Dong, Panpan Qi, Panpan Zhang, Dongting Zhangsun, Xiaopeng Zhu, Jinpeng Yu, and Sulan Luo. 2023. "Molecular Determinants of Species Specificity of α-Conotoxin TxIB towards Rat and Human α6/α3β4 Nicotinic Acetylcholine Receptors" International Journal of Molecular Sciences 24, no. 10: 8618. https://doi.org/10.3390/ijms24108618
APA StyleXie, T., Qin, Y., Zhao, J., Dong, J., Qi, P., Zhang, P., Zhangsun, D., Zhu, X., Yu, J., & Luo, S. (2023). Molecular Determinants of Species Specificity of α-Conotoxin TxIB towards Rat and Human α6/α3β4 Nicotinic Acetylcholine Receptors. International Journal of Molecular Sciences, 24(10), 8618. https://doi.org/10.3390/ijms24108618






