0.1% RGN-259 (Thymosin ß4) Ophthalmic Solution Promotes Healing and Improves Comfort in Neurotrophic Keratopathy Patients in a Randomized, Placebo-Controlled, Double-Masked Phase III Clinical Trial
Abstract
1. Introduction
2. Results
2.1. RGN-259-Treated Subjects Showed Faster Healing at 4 Weeks
2.2. RGN-259-Treated Subjects Had a Lower Mackie Classification by 4 Weeks
2.3. RGN-259-Treated Subjects Had Improved Ocular Discomfort by 2 Weeks
2.4. RGN-259 Was Very Safe for the NK Subjects
3. Discussion
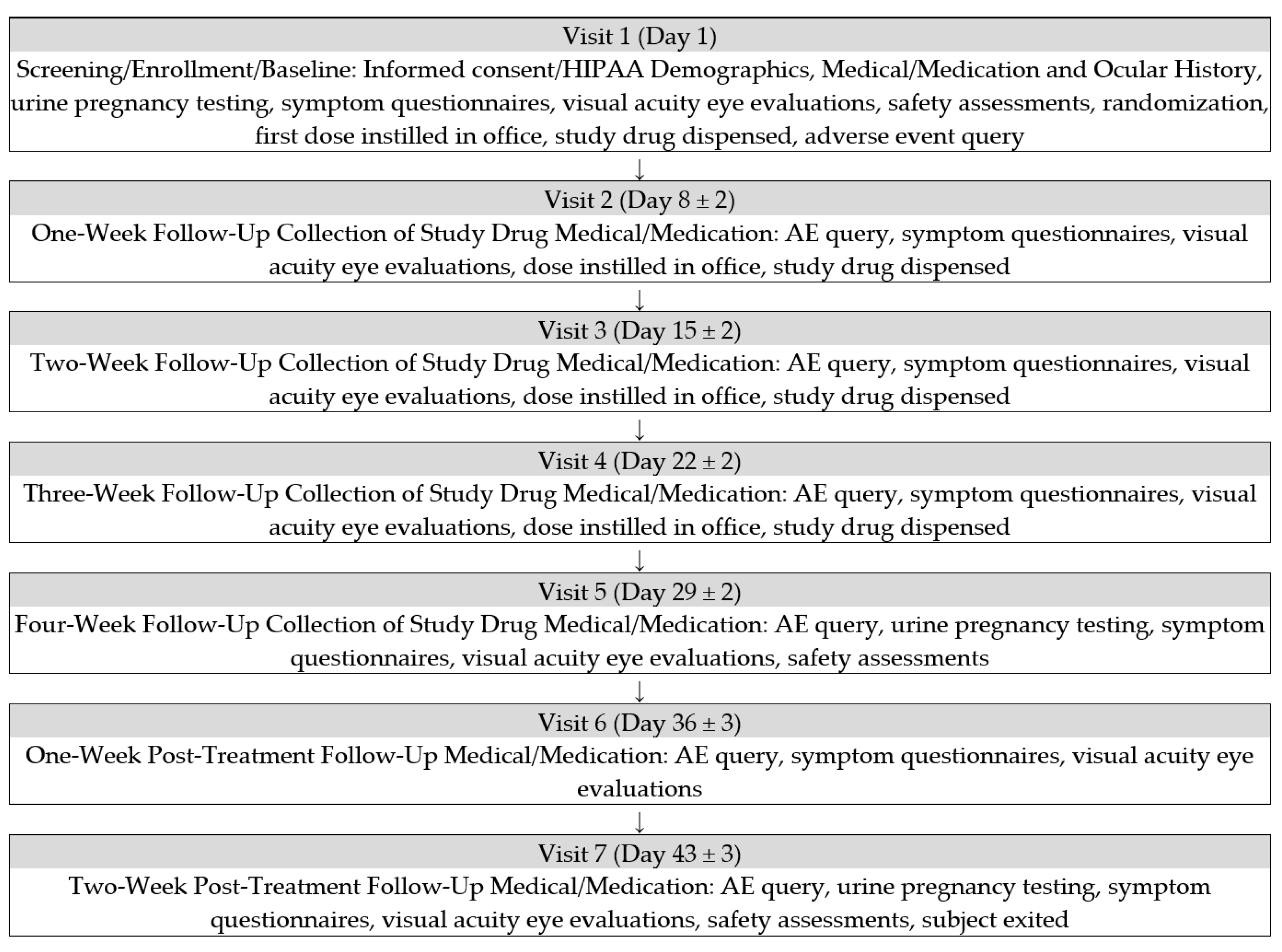
4. Materials and Methods
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bonini, S.; Rama, R.; Olzi, D.; Lambiase, A. Neurotrophic keratitis. Eye 2003, 17, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Lozano, R.E.; Hernandez-Camarena, J.C.; Loya-Garcia, D.; Merayo-Lloves, J.; Rodriguez-Garcia, A. The molecular basis of neurotrophic keratopathy: Diagnostic and therapeutic implications. A review. Ocul. Surf. 2021, 19, 224–240. [Google Scholar] [CrossRef] [PubMed]
- Sacchetti, M.; Lambiase, A. Diagnosis and management of neurotrophic keratitis. Clin. Ophthalmol. 2014, 8, 571–579. [Google Scholar] [PubMed]
- Bian, Y.; Ma, K.K.; Hall, N.E.; Elze, T.; Lorch, A.; Miller, J.W.; Dana, R.; Yin, J. Neurotrophic Keratopathy in the United States: An Intelligent Research in Sight Registry Analysis. Ophthalmology 2022, 129, 1255–1262. [Google Scholar] [CrossRef]
- NaPier, E.; Camancho, M.; McDevitt, T.F.; Sweener, A.R. Neurotrophic keratopathy: Current challenges and future prospects. Ann. Med. 2022, 54, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Pflugfelder, S.C.; Massaro-Giordano, M.; Perez, V.L.; Hamrah, P.; Deng, S.X.; Espandar, L.; Stephen Foster, C.; Affeldt, J.; Seedor, J.A.; Afshari, N.A.; et al. Topical recombinant human nerve growth factor (cenegermin) for neurotrophic keratopathy: A multicenter randomized vehicle-controlled pivotal trial. Ophthalmology 2020, 127, 14–26. [Google Scholar] [CrossRef]
- Bonzano, C.; Olivari, S.; Cutolo, C.A.; Macri, A.; Sindaco, D.; Borrono, D.; Bonzano, E.; Traverso, C.E. Recombinant human nerve growth factor (cenegermin)-driven corneal wound healing process: An evidence-based analysis. Front. Pharmacol. 2022, 12, 760507. [Google Scholar] [CrossRef]
- Goldstein, A.l.; Kleinman, H.K. Advances in the basic and clinical applications of thymosin beta 4. Exp. Opin. Biol. Ther. 2015, 15 (Suppl. 1), s139–s145. [Google Scholar] [CrossRef]
- Sosne, G.; Kleinman, H.K. Primary mechanisms of thymosin beta 4 repair activity in dry eye and other tissue disorders. Investig. Ophthalmol. Vis. Sci. 2015, 56, 5110–5117. [Google Scholar] [CrossRef]
- Sosne, G.; Szliter, E.A.; Barrett, R.; Kernacki, K.A.; Kleinman, H.; Hazlett, L.D. Thymosin beta 4 promotes corneal wound healing and decreases inflammation in vivo following alkali injury. Exp. Eye Res. 2002, 74, 293–299. [Google Scholar] [CrossRef]
- Sosne, G.; Christopherson, P.L.; Barrett, R.P.; Fridman, R. Thymosin beta 4 modulates corneal matrix-metalloproteinase levels and polymophonuclear cell infiltration after alkali injury. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2388–2395. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.U.; Kleinman, H.K.; Sosne, G.; Ousler, G.W.; Kim, K.; Kang, S.; Yang, J. RGN-259 (thymosin beta 4) improves clinically important dry eye efficacies in comparison with prescription drugs in a dry eye model. Sci. Rep. 2018, 8, 1–14. [Google Scholar]
- Zhang, J.; Zhang, Z.G.; Morris, D.; Li, Y.; Roberts, S.; Elias, S.G.; Chopp, M. Neurological functional recovery after thymosin beta 4 treatment in mice with experimental auto encephalomyelitis. Neuroscience 2009, 164, 1887–1893. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Chopp, M.; Szalad, A.; Liu, Z.; Lu, M.; Zhang, L.; Zhang, J.; Zhang, R.L.; Morris, D.; Zhang, Z.G. Thymosin beta 4 promotes the recovery of peripheral neuropathy in type II diabetic mice. Neurobiol. Dis. 2012, 48, 546–555. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morris, D.C.; Zhang, Z.G.; Zhang, J.; Xiong, X.; Zhang, L.; Chopp, M. Treatment of neurological injury with thymosin beta 4. Ann. N. Y. Acad. Sci. 2012, 1269, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Kuang, F.; Zhang, H.; Ju, G.; Wang, J. Beneficial effects of thymosin beta 4 on spinal cord injury in the rat. Neuropharmacology 2014, 85, 408–416. [Google Scholar] [CrossRef]
- Dunn, S.P.; Heidemann, D.G.; Chow, C.Y.; Crockford, D.; Turjman, N.; Angel, J.; Allan, C.B.; Sosne, G. Treatment of chronic nonhealing neurotrophic corneal epithelial defects with thymosin beta4. Ann. N. Y. Acad. Sci. 2010, 1194, 199–206. [Google Scholar] [CrossRef]
- Sosne, G.; Ousler, G.W. Thymosin beta 4 ophthalmic solution for dry eye: A randomized, placebo-controlled, Phase II clinical trial conducted using the controlled adverse environment (CAE™) model. Clin. Ophthal. 2015, 9, 877–884. [Google Scholar]
- Sosne, G.; Rimmer, D.; Kleinman, H.K.; Ousler, G. Thymosin beta 4: A potential novel therapy for Neurotrophic Keratopathy, dry eye, and ocular surface diseases. Vitam. Horm. 2016, 102, 277–306. [Google Scholar]
- Badamchian, M.; Deamavandy, A.A.; Darmavandy, H.; Washwa, S.D.; Katz, B.; Goldstein, A.L. Identification and quantification of thymosin beta 4 in human saliva and tears. Ann. N. Y. Acad. Sci. 2007, 1112, 458–465. [Google Scholar] [CrossRef]
- Magharious, M.; D’Onofrio, D.; Hollander, A.; Zhu, P.; Chen, J.; Koeberle, P.D. Quantitative iTRAQ analysis of retinal ganglion cell degeneration after optic nerve crush. J. Proteome. Res. 2011, 10, 3344–3362. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, Q.; Zhang, X.; Zheng, X.; Zhang, Q. Thymosin beta 4 suppresses CCL4-induced murine hepatic fibrosis by down-regulating transforming growth factor beta receptor-II. J. Gene. Med. 2018, 20, e3043. [Google Scholar] [CrossRef] [PubMed]
- Conte, E.; Genovese, T.; Gili, E.; Esposito, E.; Iemmolo, M.; Fruciano, M.; Fagone, E.; Pistorio, M.P.; Crimi, N.; Cuzzocrea, S.; et al. Thymosin beta 4 protects C57BL/6 mice from bleomycin-induced damage in the lung. Eur. J. Clin. Investig. 2013, 43, 309–315. [Google Scholar] [CrossRef]
- Hong, Y.; Yao, Q.; Zheng, L. Thymosin beta 4 attenuates liver fibrosis vis suppressing Notch signaling. Biochem. Biophys. Res. Commun. 2017, 493, 1396–1401. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Yao, N.; Wang, F.; Ruan, L. Thymosin beta 4 suppressed LPS-induced lung fibrosis by attenuating oxidative injury and alleviating inflammation. Inflammation 2022, 45, 59–73. [Google Scholar] [CrossRef]
- Wang, F.; He, Y.; Yao, N.; Ruan, L.; Tian, Z. Thymosin beta 4 protects against cardiac damage and subsequent cardiac fibrosis in mice with myocardial infarction. Cardiovasc. Ther. 2022, 2022, 1308651. [Google Scholar] [CrossRef]
- Conte, E.; Iemmolo, M.; Fruciano, M.; Fagone, E.; Gili, E.; Genovese, T.; Esposito, E.; Cuzzocrea, S.; Vacheri, C. Effects of thymosin beta 4 and its N-terminal fragment Ac-SDKP on TGF-beta treated human lung fibroblasts and in the mouse model of bleomycin-induced lung fibrosis. Exp. Opin. Biol. Ther. 2018, 15 (Suppl. 1), 211–221. [Google Scholar] [CrossRef] [PubMed]
- Hrenak, J.; Paulis, L.; Simko, F. N-acetyl-seryl-aspartyl-lysyl-proline (Ac-SDKP): Potential target molecule in research of heart, kidney, and brain. Curr. Parm. Des. 2015, 21, 5135–5143. [Google Scholar] [CrossRef]
- Peng, H.; Carreter, O.A.; Brigstock, D.R.; Oja-Tebbe, N.; Rhaleb, N.E. Ac-SDKP reverses cardiac fibrosis in rats with renovascular hypertension. Hypertension 2003, 42, 1164–1170. [Google Scholar] [CrossRef]
- Qui, Y.; Wang, W.; Zhang, X.; Huang, P.; Zhang, W.; Zhang, K.; Wang, S.; He, L.; Guo, Y.; Xiang, A.; et al. A long-acting isomer of Ac-SDKP attenuates pulmonary fibrosis through SRPK1-mediated P13/AKT and Smad2 pathway inhibition. IUBMB Life 2020, 72, 2611–2626. [Google Scholar]
- Yang, F.; Yang, X.P.; Liu, Y.H.; Xu, J.; Cingolani, O.; Rhaleb, N.E.; Carretero, O.A. Ac-SDKP reverses inflammation and fibrosis in rats with heart failure after myocardial infarction. Hypertension 2004, 43, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xu, L.M.; Chen, Y.W.; Ni, Q.W.; Zhou, M.; Qu, C.Y.; Zhang, Y. Antifibrotic effect of N-acetyl-seryl-aspartyl-lysyl-proline on bile duct ligation induced liver fibrosis in rats. World J. Gastroenterol. 2012, 18, 5283–5288. [Google Scholar] [PubMed]
- Zuo, Y.; Chun, B.; Potthoff, S.A.; Kazi, N.; Brolin, T.J.; Orhan, D.; Yang, H.-C.; Ma, L.-J.; Kon, V.; Myöhänen, T.; et al. Thymosin beta 4 and its degradation product, ac-SDKP, are novel reparative factors in renal fibrosis. Kidney Int. 2013, 84, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Kanasaki, K. N-acetyl-seryl-aspartyl-proline is a valuable endogenous antifibrotic peptide for kidney fibrosis in diabetes: An update and translational aspects. J. Diabetes Investig. 2020, 11, 516–526. [Google Scholar] [CrossRef]
| Variable | Treated with 0.1% RGN-259 (n = 10) | Placebo (n = 8) |
|---|---|---|
| Gender (n) | ||
| Male | 2 | 4 |
| Female | 8 | 4 |
| Average Age (SD) | 63.7 (15.58) | 72.5 (7.87) |
| Race | ||
| Hispanic Latino | 0 | 1 |
| White | 10 | 7 |
| Mackie Classification | ||
| Stage 1 | 0 | 0 |
| Stage 2 | 9 | 7 |
| Stage 3 | 1 | 1 |
| Frequent Eye Disorders | ||
| Cataract | 7 | 8 |
| Corneal opacity | 0 | 3 |
| Corneal scar | 1 | 2 |
| Dry eye | 9 | 6 |
| Glaucoma | 2 | 2 |
| Open angle glaucoma | 2 | 1 |
| Retinal detachment | 1 | 3 |
| Surgical Procedures | ||
| Cataract | 7 | 4 |
| Eye surgery | 1 | 2 |
| Lens implant | 4 | 4 |
| Keratoplasty | 2 | 3 |
| Post lens Capsulotomy | 2 | 2 |
| Retinal laser coagulation. | 2 | 2 |
| Retinopexy | 1 | 2 |
| Area of Epithelial Defect (mm2) | ||
| Mean (SD) | 6.815 (3.848) | 9.871 (7.134) |
| Median | 6.570 | 7.375 |
| Duration of NK (Days) | ||
| Mean (SD) | 213 (229.2) | 973 (1557.3) |
| Median | 107.5 | 206.0 |
| Ocular Discomfort * | ||
| Mean (SD) | 3.3 (1.16) | 1.6 (1.60) |
| Median | 3.0 | 1.5 |
| Visual acuity (log MAR) | ||
| Mean (SD) | 1.386 (1.1566) | 1.196 (0.9098) |
| Visit Measurement | 0.1% RGN-259 (n = 10) | Placebo (n = 8) |
|---|---|---|
| Visit 2 (Day 8 ± 2) | ||
| Complete Healing: n (%) | 0 | 0 |
| Two-sided 95% CI | (0.000, 0.000) | (0.000, 0.000) |
| Difference in Proportions, RGN-259—Placebo | 0.000 | - |
| Two-sided 95% CI | (NC, NC) | - |
| p-value, Fisher’s Exact Test (Primary) | NC | - |
| p-value, Chi-square Test (Ad Hoc) | NC | |
| Visit 3 (Day 15 ± 2) | ||
| Complete Healing: n (%) | 3 (30.0%) | 1 (12.5%) |
| Two-sided 95% CI | (0.016, 0.584) | (0.000, 0.354) |
| Difference in Proportions, RGN-259—Placebo | 0.175 | - |
| Two-sided 95% CI | (−0.190, 0.540) | - |
| p-value, Fisher’s Exact Test (Primary) | 0.5882 | - |
| p-value, Chi-square Test (Ad Hoc) | 0.3749 | |
| Visit 4 (Day 22 ± 2) | ||
| Complete Healing: n (%) | 4 (40.0%) | 2 (25.0%) |
| Two-sided 95% CI | (0.096, 0.704) | (0.000, 0.550) |
| Difference in Proportions, RGN-259—Placebo | 0.150 | - |
| Two-sided 95% CI | (−0.277, 0.577) | - |
| p-value, Fisher’s Exact Test (Primary) | 0.6380 | - |
| p-value, Chi-square Test (Ad Hoc) | 0.5023 | |
| Visit 5 (Day 29 ± 2) | ||
| Complete Healing: n (%) | 6 (60.0%) | 1 (12.5%) |
| Two-sided 95% CI | (0.296, 0.904) | (0.000, 0.354) |
| Difference in Proportions, RGN-259—Placebo | 0.475 | - |
| Two-sided 95% CI | (0.095, 0.855) | - |
| p-value, Fisher’s Exact Test (Primary) | 0.0656 | - |
| p-value, Chi-square Test (Ad Hoc) | 0.0400 | |
| Visit 6 (Day 36 ± 3) | ||
| Complete Healing: n (%) | 4 (40.0%) | 1 (12.5%) |
| Two-sided 95% CI | (0.096, 0.704) | (0.000, 0.354) |
| Difference in Proportions, RGN-259—Placebo | 0.275 | - |
| Two-sided 95% CI | (−0.105, 0.655) | - |
| p-value, Fisher’s Exact Test (Primary) | 0.3137 | - |
| p-value, Chi-square Test (Ad Hoc) | 0.1955 | |
| Visit 7 (Day 43 ± 3) | ||
| Complete Healing: n (%) | 5 (50.0%) | 0 |
| Two-sided 95% CI | (0.190, 0.810) | (0.000, 0.000) |
| Difference in Proportions, RGN-259—Placebo | 0.500 | - |
| Two-sided 95% CI | (0.190, 0.810) | - |
| p-value, Fisher’s Exact Test (Primary) | 0.0359 | - |
| p-value, Chi-square Test (Ad Hoc) | 0.0186 | |
| Day 1 | Day 29 | Day 36 | Day 43 | |||||
|---|---|---|---|---|---|---|---|---|
| 0.1% RGN-259 | Placebo | 0.1% RGN-259 | Placebo | 0.1% RGN-259 * | Placebo | 0.1% RGN-259 * | Placebo | |
| Stage 1 | 0 | 0 | 6 | 2 | 5 | 1 | 4 | 1 |
| Stage 2 | 9 | 7 | 2 | 6 | 3 | 6 | 3 | 7 |
| Stage 3 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 |
| p value | 0.0818 | 0.0625 | 0.0467 | |||||
| Visit | Statistical Measurement | 0.1% RGN-259 (n = 10) | Placebo (n = 8) |
|---|---|---|---|
| Ocular Discomfort | |||
| Visit 2 (Day 8 ± 2) | Mean (SD) | −1.5 (0.97) | −0.6 (1.19) |
| p-value, Two-Sample t-test | 0.1045 | - | |
| p-value, ANCOVA model | 0.6676 | - | |
| Visit 3 (Day 15 ± 2) | Mean (SD) | −1.8 (0.79) | −0.3 (1.04) |
| p-value, Two-Sample t-test | 0.0023 | - | |
| p-value, ANCOVA model | 0.0193 | - | |
| Visit 4 (Day 22 ± 2) | Mean (SD) | −1.7 (1.06) | −0.4 (0.92) |
| p-value, Two-Sample t-test | 0.0130 | - | |
| p-value, ANCOVA model | 0.0541 | - | |
| Visit 5 (Day 29 ± 2) | Mean (SD) | −2.0 (1.05) | −0.3 (1.04) |
| p-value, Two-Sample t-test | 0.0028 | - | |
| p-value, ANCOVA model | 0.0365 | - | |
| Visit 6 (Day 36 ± 3) | Mean (SD) | −1.4 (1.43) | −0.1 (0.99) |
| p-value, Two-Sample t-test | 0.0482 | - | |
| p-value, ANCOVA model | 0.1909 | ||
| Visit 7 (Day 43 ± 3) | Mean (SD) | −1.4 (1.26) | −0.3 (1.28) |
| p-value, Two-Sample t-test | 0.0748 | - | |
| p-value, ANCOVA model | 0.2154 | - | |
| Foreign Body Sensation | |||
| Visit 2 (Day 8 ± 2) | Mean (SD) | −1.9 (2.02) | −0.1 (0.99) |
| p-value, Two-Sample t-test | 0.0201 | - | |
| p-value, ANCOVA model | 0.5107 | - | |
| Visit 3 (Day 15 ± 2) | Mean (SD) | −1.6 (1.35) | −0.1 (0.99) |
| p-value, Two-Sample t-test | 0.0202 | - | |
| p-value, ANCOVA model | 0.3993 | - | |
| Visit 4 (Day 22 ± 2) | Mean (SD) | −2.3 (0.95) | −0.1 (0.83) |
| p-value, Two-Sample t-test | 0.0001 | - | |
| p-value, ANCOVA model | 0.0107 | - | |
| Visit 5 (Day 29 ± 2) | Mean (SD) | −2.3 (1.34) | 0.1 (1.13) |
| p-value, Two-Sample t-test | 0.0009 | - | |
| p-value, ANCOVA model | 0.0176 | - | |
| Visit 6 (Day 36 ± 3) | Mean (SD) | −2.1 (1.37) | 0.1 (1.13) |
| p-value, Two-Sample t-test | 0.0020 | - | |
| p-value, ANCOVA model | 0.0409 | - | |
| Visit 7 (Day 43 ± 3) | Mean (SD) | −2.2 (1.62) | 0.5 (0.93) |
| p-value, Two-Sample t-test | 0.0007 | - | |
| p-value, ANCOVA model | 0.0213 | - | |
| Dryness | |||
| Visit 2 (Day 8 ± 2) | Mean (SD) | −1.1 (1.10) | 0.4 (1.30) |
| p-value, Two-Sample t-test | 0.0191 | - | |
| p-value, ANCOVA model | 0.0443 | - | |
| Visit 3 (Day 15 ± 2) | Mean (SD) | −0.9 (1.37) | 0.3 (1.58) |
| p-value, Two-Sample t-test | 0.1177 | - | |
| p-value, ANCOVA model | 0.2546 | - | |
| Visit 4 (Day 22 ± 2) | Mean (SD) | −1.3 (1.06) | −0.3 (1.83) |
| p-value, Two-Sample t-test | 0.1462 | - | |
| p-value, ANCOVA model | 0.3445 | - | |
| Visit 5 (Day 29 ± 2) | Mean (SD) | −0.8 (1.69) | −0.3 (2.55) |
| p-value, Two-Sample t-test | 0.5899 | - | |
| p-value, ANCOVA model | 0.8980 | - | |
| Visit 6 (Day 36 ± 3) | Mean (SD) | −0.7 (1.16) | 0.3 (1.67) |
| p-value, Two-Sample t-test | 0.1733 | - | |
| p-value, ANCOVA model | 0.3943 | - | |
| Visit 7 (Day 43 ± 3) | Mean (SD) | −0.6 (1.07) | 0.0 (2.45) |
| p-value, Two-Sample t-test | 0.4946 | - | |
| p-value, ANCOVA model | 0.8554 | - | |
| 0.1% RGN-259 (n = 10) n (%) | Placebo (n = 8) n (%) | |
|---|---|---|
| Adverse Events (Ocular and Non-Ocular) | ||
| Number of AEs | 11 | 5 |
| Number of Subjects with at Least One AE | 4 (40.0%) | 3 (37.5%) |
| Number of Treatment-Related AEs | 1 | 0 |
| Number of Subjects with at Least One Treatment-Related AE | 1 (10.0%) | 0 |
| Number of SAEs | 1 | 0 |
| Number of Subjects with at Least One SAE | 1 (10.0%) | 0 |
| Number of Treatment-Related SAEs | 0 | 0 |
| Ocular AEs | ||
| Number of AEs | 7 | 4 |
| Number of Subjects with at Least One AE | 3 (30.0%) | 2 (25.0%) |
| Number of AEs in Treated Eyes | 5 | 0 |
| Number of Subjects with at Least One AE in a Treated Eye | 2 (20.0%) | 0 |
| Number of AEs in Study Eyes | 5 | 0 |
| Number of Subjects with at Least One AE in a Study Eye | 2 (20.0%) | 0 |
| Ocular AEs | ||
| Number of AEs in Treated Fellow Eyes | 0 | 0 |
| Number of AEs in Untreated Fellow Eyes | 2 | 4 |
| Number of Subjects with at Least One AE in an Untreated Fellow Eye | 2 (20.0%) | 2 (25.0%) |
| Number of Treatment-Related AEs | 1 | 0 |
| Number of SAEs | 0 | 0 |
| Non-Ocular AEs | ||
| Number of AEs | 4 | 1 |
| Number of Subjects with at Least One AE | 2 (20.0%) | 1 (12.5%) |
| Number of Treatment-Related AEs | 0 | 0 |
| Number of SAEs | 1 | 0 |
| Number of Subjects with at Least One SAE | 1 (10.0%) | 0 |
| 0.1% RGN-259 (n = 10) | Placebo (n = 8) | |||
|---|---|---|---|---|
| System Organ Class (SOC) Preferred Term (PT) | Events | Subjects n (%) | Events | Subjects n (%) |
| Total—Ocular AEs | 7 | 3 (30.0%) | 4 | 2 (25.0%) |
| Eye disorders | 7 | 3 (30.0%) | 4 | 2 (25.0%) |
| Corneal epithelium defect | 2 | 2 (20.0%) | 0 | 0 |
| Corneal opacity | 2 | 1 (10.0%) | 0 | 0 |
| Keratic precipitates | 1 | 1 (10.0%) | 0 | 0 |
| Visual impairment | 1 | 1 (10.0%) | 1 | 1 (12.5%) |
| Vitreous detachment | 1 | 1 (10.0%) | 0 | 0 |
| Visual acuity reduced | 0 | 0 | 3 | 1 (12.5%) |
| Total—Non-Ocular AEs | 4 | 2 (20.0%) | 1 | 1 (12.5%) |
| Infections and infestations | 1 | 1 (12.5%) | ||
| Upper respiratory tract infection1 | 1 | 1 (12.5%) | ||
| General disorders and administration site conditions | 1 | 1 (10.0%) | ||
| Inflammation | 1 | 1 (10.0%) | ||
| Investigations | 1 | 1 (10.0%) | ||
| Blood glucose decreased | 1 | 1 (10.0%) | ||
| Nervous system disorders | 1 | 1 (10.0%) | ||
| Unresponsive to stimuli | 1 | 1 (10.0%) | ||
| Psychiatric disorders | 1 | 1 (10.0%) | ||
| Depression | 1 | 1 (10.0%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sosne, G.; Kleinman, H.K.; Springs, C.; Gross, R.H.; Sung, J.; Kang, S. 0.1% RGN-259 (Thymosin ß4) Ophthalmic Solution Promotes Healing and Improves Comfort in Neurotrophic Keratopathy Patients in a Randomized, Placebo-Controlled, Double-Masked Phase III Clinical Trial. Int. J. Mol. Sci. 2023, 24, 554. https://doi.org/10.3390/ijms24010554
Sosne G, Kleinman HK, Springs C, Gross RH, Sung J, Kang S. 0.1% RGN-259 (Thymosin ß4) Ophthalmic Solution Promotes Healing and Improves Comfort in Neurotrophic Keratopathy Patients in a Randomized, Placebo-Controlled, Double-Masked Phase III Clinical Trial. International Journal of Molecular Sciences. 2023; 24(1):554. https://doi.org/10.3390/ijms24010554
Chicago/Turabian StyleSosne, Gabriel, Hynda K. Kleinman, Clark Springs, Robert Hollis Gross, Jihye Sung, and Shinwook Kang. 2023. "0.1% RGN-259 (Thymosin ß4) Ophthalmic Solution Promotes Healing and Improves Comfort in Neurotrophic Keratopathy Patients in a Randomized, Placebo-Controlled, Double-Masked Phase III Clinical Trial" International Journal of Molecular Sciences 24, no. 1: 554. https://doi.org/10.3390/ijms24010554
APA StyleSosne, G., Kleinman, H. K., Springs, C., Gross, R. H., Sung, J., & Kang, S. (2023). 0.1% RGN-259 (Thymosin ß4) Ophthalmic Solution Promotes Healing and Improves Comfort in Neurotrophic Keratopathy Patients in a Randomized, Placebo-Controlled, Double-Masked Phase III Clinical Trial. International Journal of Molecular Sciences, 24(1), 554. https://doi.org/10.3390/ijms24010554






