Circadian Regulation of Retinal Pigment Epithelium Function
Abstract
1. Introduction
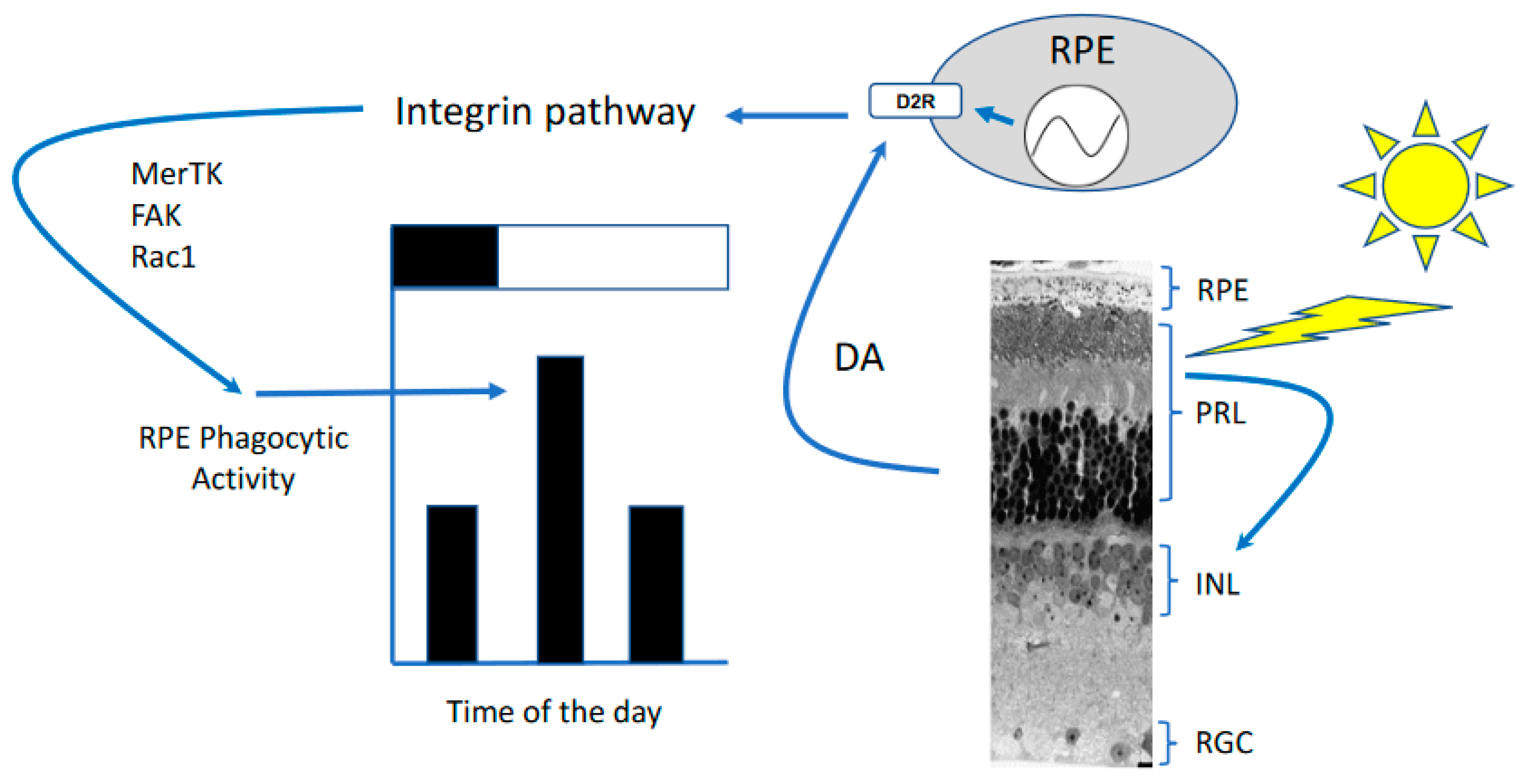
2. Regulation of RPE Function In Vivo
| Function in RPE | Animal Model | Human Retinal Disease | |
|---|---|---|---|
| MerTK receptor | Outer segment binding & internalization | RCS rat [43,44] Merkd mouse [45] | Retinitis pigmentosa, rod-cone dystrophy [46,47,48,49,50] |
| Gas6, Protein S | MerTK ligands | Gas6 double KO and ProS1 [51] | Diabetic Retinopathy and macular edema [52] |
| ανβ5 integrin receptor | Outer segment binding, Control the diurnal rhythm in peak of phagocytosis | β5−/− mouse [29] | unknown |
| MFG-E8 | ανβ5 integrin ligand Control the diurnal rhythm in peak of phagocytosis | MFG-E8−/− mouse [30] | unknown |
| Dopamine receptor 2 | Controls the rhythm in RPE circadian clocks, light adaptation, peak of phagocytosis after light onset | D2R KO mouse [31] | unkown |
| Melatonin receptor 1 and 2 | Control the timing of the peak of phagocytosis | MT1 & MT2 KO mouse [34] | |
| RPE specific Bmal1 KO | Control the diurnal rhythm in peak of phagocytosis | RPEcre; Bmal1fl/fl [42] | unknown |
| Per1/Per2 global KO | Controls the amplitude of the peak of phagocytosis | Per1−/−Per2Brdm1 [41] | unknown |
3. Regulation of RPE Function In Vitro
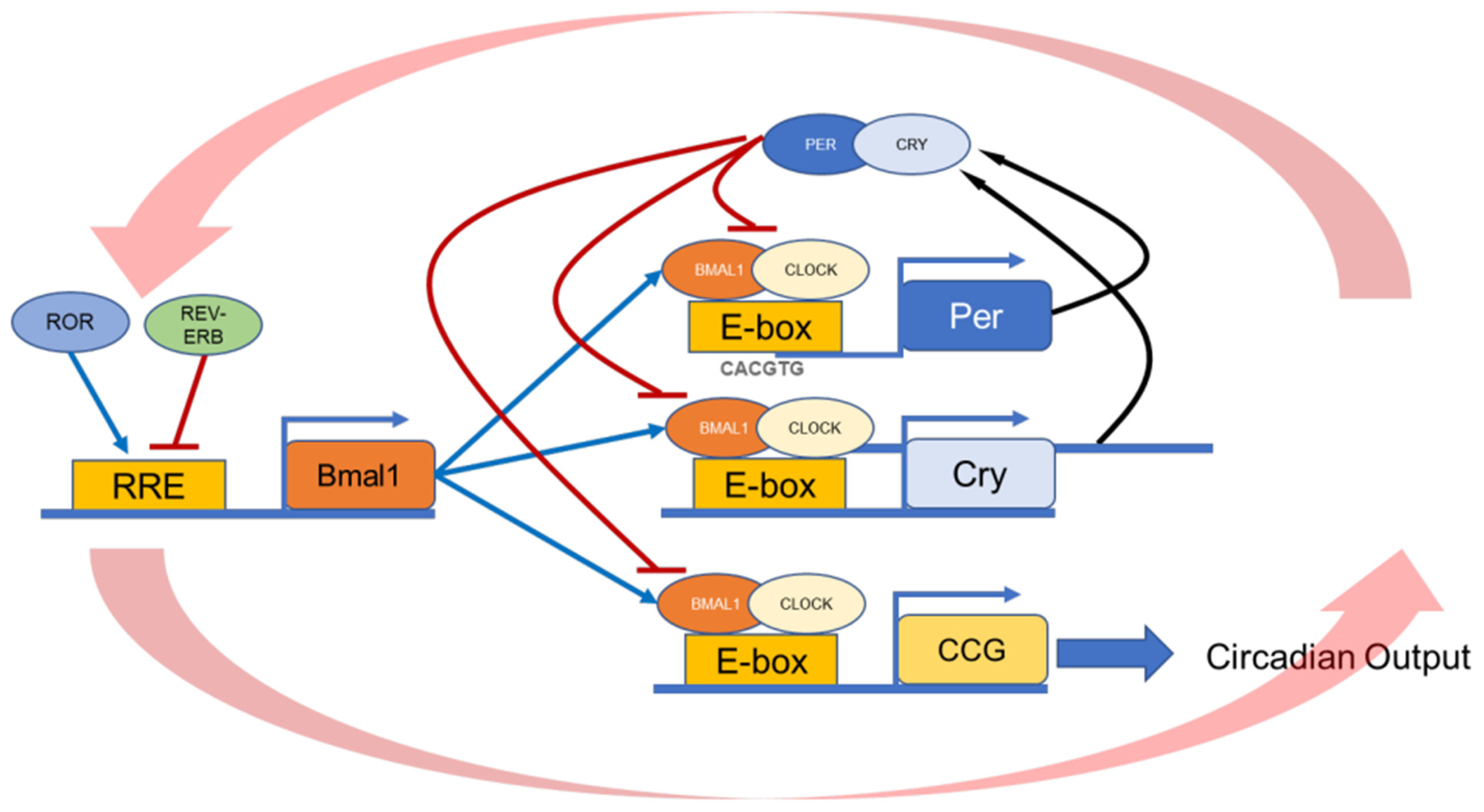
4. Entrainment of the RPE Circadian Clock
5. Is the Daily Burst in Phagocytic Activity Important for Photoreceptor and RPE Health?
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Felder, M.-P.; Buhr, E.D.; Dkhissi-Benyahya, O.; Hicks, D.; Peirson, S.N.; Ribelayga, C.P.; Sandu, C.; Spessert, R.; Tosini, G. Ocular Clocks: Adapting Mechanisms for Eye Functions and Health. Investig. Opthalmology Vis. Sci. 2018, 59, 4856–4870. [Google Scholar] [CrossRef] [PubMed]
- Kondratov, R.V.; Kondratova, A.A.; Gorbacheva, V.Y.; Vykhovanets, O.V.; Antoch, M.P. Early aging and age-related pathologies in mice deficient in BMAL1, the core componentof the circadian clock. Genes Dev. 2006, 20, 1868–1873. [Google Scholar] [CrossRef] [PubMed]
- Storch, K.-F.; Paz, C.; Signorovitch, J.; Raviola, E.; Pawlyk, B.; Li, T.; Weitz, C.J. Intrinsic Circadian Clock of the Mammalian Retina: Importance for Retinal Processing of Visual Information. Cell 2007, 130, 730–741. [Google Scholar] [CrossRef] [PubMed]
- Sawant, O.B.; Horton, A.M.; Zucaro, O.F.; Chan, R.; Bonilha, V.L.; Samuels, I.S.; Rao, S. The Circadian Clock Gene Bmal1 Controls Thyroid Hormone-Mediated Spectral Identity and Cone Photoreceptor Function. Cell Rep. 2017, 21, 692–706. [Google Scholar] [CrossRef]
- Baba, K.; Pozdeyev, N.; Mazzoni, F.; Contreras-Alcantara, S.; Liu, C.; Kasamatsu, M.; Martinez-Merlos, T.; Strettoi, E.; Iuvone, P.M.; Tosini, G. Melatonin modulates visual function and cell viability in the mouse retina via the MT1 melatonin receptor. Proc. Natl. Acad. Sci. USA 2009, 106, 15043–15048. [Google Scholar] [CrossRef]
- Baba, K.; Piano, I.; Lyuboslavsky, P.; Chrenek, M.A.; Sellers, J.T.; Zhang, S.; Gargini, C.; He, L.; Tosini, G.; Iuvone, P.M. Removal of clock gene Bmal1 from the retina affects retinal development and accelerates cone photoreceptor degeneration during aging. Proc. Natl. Acad. Sci. USA 2018, 115, 13099–13104. [Google Scholar] [CrossRef]
- Baba, K.; Tosini, G. Aging Alters Circadian Rhythms in the Mouse Eye. J. Biol. Rhythm. 2018, 33, 441–445. [Google Scholar] [CrossRef]
- Gianesini, C.; Hiragaki, S.; Laurent, V.; Hicks, D.; Tosini, G. Cone Viability Is Affected by Disruption of Melatonin Receptors Signaling. Investig. Opthalmology Vis. Sci. 2016, 57, 94–104. [Google Scholar] [CrossRef]
- Ait-Hmyed, O.; Felder-Schmittbuhl, M.-P.; Garcia-Garrido, M.; Beck, S.C.; Seide, C.; Sothilingam, V.; Tanimoto, N.; Seeliger, W.M.; Bennis, M.; Hicks, D. Mice lacking Period 1 and Period 2 circadian clock genes exhibit blue cone photoreceptor defects. Eur. J. Neurosci. 2013, 37, 1048–1060. [Google Scholar] [CrossRef]
- Hakkari, O.A.; Acar, N.; Savier, E.; Spinnhirny, P.; Bennis, M.; Felder-Schmittbuhl, M.; Mendoza, J.; Hicks, D. Rev-Erbα modulates retinal visual processing and behavioral responses to light. FASEB J. 2016, 30, 3690–3701. [Google Scholar] [CrossRef]
- Kevany, B.M.; Palczewski, K. Phagocytosis of Retinal Rod and Cone Photoreceptors. Physiology 2010, 25, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Bok, D. The retinal pigment epithelium: A versatile partner in vision. J. Cell Sci. 1993, 1993, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Nguyen-Legros, J.; Hicks, D. Renewal of photoreceptor outer segments and their phagocytosis by theretinal pigment epithelium. Adv. Virus Res. 2000, 196, 245–313. [Google Scholar] [CrossRef]
- LaVail, M.M. Chapter 44 Legacy of the RCS rat: Impact of a seminal study on retinal cell biology and retinal degenerative diseases. Prog. Brain Res. 2001, 131, 617–627. [Google Scholar] [CrossRef]
- Lavail, M.M. Interaction of environmental light and eye pigmentation with inherited retinal degenerations. Vis. Res. 1980, 20, 1173–1177. [Google Scholar] [CrossRef]
- LaVail, M.M. Rod Outer Segment Disk Shedding in Rat Retina: Relationship to Cyclic Lighting. Science 1976, 194, 1071–1074. [Google Scholar] [CrossRef]
- Grace, M.S.; Chiba, A.; Menaker, M. Circadian control of photoreceptor outer segment membrane turnover in mice genetically incapable of melatonin synthesis. Vis. Neurosci. 1999, 16, 909–918. [Google Scholar] [CrossRef]
- Besharse, J.C.; Hollyfield, J.G. Turnover of mouse photoreceptor outer segments in constant light and darkness. Investig. Ophthalmol. Vis. Sci. 1979, 18, 1019–1024. [Google Scholar]
- Teirstein, P.S.; Goldman, A.I.; O’Brien, P.J. Evidence for both local and central regulation of rat rod outer segment disc shedding. Investig. Ophthalmol. Vis. Sci. 1980, 19, 1268–1273. [Google Scholar]
- Terman, J.S.; Reme, C.E.; Terman, M. Rod outer segment disk shedding in rats with lesions of the suprachiasmatic nucleus. Brain Res. 1993, 605, 256–264. [Google Scholar] [CrossRef]
- Tosini, G.; Menaker, M. Circadian Rhythms in Cultured Mammalian Retina. Science 1996, 272, 419–421. [Google Scholar] [CrossRef] [PubMed]
- Ruan, G.-X.; Allen, G.C.; Yamazaki, S.; McMahon, D.G. An Autonomous Circadian Clock in the Inner Mouse Retina Regulated by Dopamine and GABA. PLoS Biol. 2008, 6, e249-18. [Google Scholar] [CrossRef] [PubMed]
- Tosini, G.; Davidson, A.J.; Fukuhara, C.; Kasamatsu, M.; Castanon-Cervantes, O. Localization of a circadian clock in mammalian photoreceptors. FASEB J. 2007, 21, 3866–3871. [Google Scholar] [CrossRef] [PubMed]
- Jaeger, C.; Sandu, C.; Malan, A.; Mellac, K.; Hicks, D.; Felder-Schmittbuhl, M. Circadian organization of the rodent retina involves strongly coupled, layer-specific oscillators. FASEB J. 2015, 29, 1493–1504. [Google Scholar] [CrossRef]
- Baba, K.; Sengupta, A.; Tosini, M.; Contreras-Alcantara, S.; Tosini, G. Circadian regulation of the PERIOD 2::LUCIFERASE bioluminescence rhythm in the mouse retinal pigment epithelium-choroid. Mol. Vis. 2010, 16, 2605. [Google Scholar]
- Baba, K.; DeBruyne, J.P.; Tosini, G. Dopamine 2 Receptor Activation Entrains Circadian Clocks in Mouse Retinal Pigment Epithelium. Sci. Rep. 2017, 7, 1–9. [Google Scholar]
- Bobu, C.; Craft, C.M.; Masson-Pevet, M.; Hicks, D. Photoreceptor Organization and Rhythmic Phagocytosis in the Nile RatArvicanthis Ansorgei: A Novel Diurnal Rodent Model for the Study of Cone Pathophysiology. Investig. Opthalmology Vis. Sci. 2006, 47, 3109–3118. [Google Scholar] [CrossRef][Green Version]
- Krigel, A.; Felder-Schmittbuhl, M.-P.; Hicks, D. Circadian-clock driven cone-like photoreceptor phagocytosis in the neural retina leucine zipper gene knockout mouse. Mol. Vis. 2010, 16, 2873–2881. [Google Scholar] [PubMed]
- Nandrot, E.F.; Kim, Y.; Brodie, S.; Huang, X.; Sheppard, D.; Finnemann, S.C. Loss of Synchronized Retinal Phagocytosis and Age-related Blindness in Mice Lacking αvβ5 Integrin. J. Exp. Med. 2004, 200, 1539–1545. [Google Scholar] [CrossRef]
- Nandrot, E.; Anand, M.; Almeida, D.; Atabai, K.; Sheppard, D.; Finnemann, S.C. Essential role for MFG-E8 as ligand for vbeta5 integrin in diurnal retinal phagocytosis. Proc. Natl. Acad. Sci. USA 2007, 104, 12005–12010. [Google Scholar] [CrossRef]
- Goyal, V.; DeVera, C.; Laurent, V.; Sellers, J.; Chrenek, M.A.; Hicks, D.; Baba, K.; Iuvone, P.M.; Tosini, G. Dopamine 2 Receptor Signaling Controls the Daily Burst in Phagocytic Activity in the Mouse Retinal Pigment Epithelium. Investig. Opthalmology Vis. Sci. 2020, 61, 10. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Finnemann, S.C. Analysis of Photoreceptor Outer Segment Phagocytosis by RPE Cells in Culture. Program. Necrosis 2012, 935, 285–295. [Google Scholar] [CrossRef]
- Ruggiero, L.; Connor, M.P.; Chen, J.; Langen, R.; Finnemann, S.C. Diurnal, localized exposure of phosphatidylserine by rod outer segment tips in wild-type but not Itgb5-/- or Mfge8-/- mouse retina. Proc. Natl. Acad. Sci. USA 2012, 109, 8145–8148. [Google Scholar] [CrossRef] [PubMed]
- Laurent, V.; Sengupta, A.; Sanchez, A.S.-B.; Hicks, D.; Tosini, G. Melatonin signaling affects the timing in the daily rhythm of phagocytic activity by the retinal pigment epithelium. Exp. Eye Res. 2017, 165, 90–95. [Google Scholar] [CrossRef]
- Gibbs, D.; Kitamoto, J.; Williams, D.S. Abnormal phagocytosis by retinal pigmented epithelium that lacks myosin VIIa, the Usher syndrome 1B protein. Proc. Natl. Acad. Sci. USA 2003, 100, 6481–6486. [Google Scholar] [CrossRef]
- Law, A.-L.; Ling, Q.; Hajjar, K.A.; Futter, C.E.; Greenwood, J.; Adamson, P.; Wavre-Shapton, S.T.; Moss, S.E.; Hayes, M.J. Annexin A2 Regulates Phagocytosis of Photoreceptor Outer Segments in the Mouse Retina. Mol. Biol. Cell 2009, 20, 3896–3904. [Google Scholar] [CrossRef]
- Mustafi, D.; Kevany, B.M.; Genoud, C.; Bai, X.; Palczewski, K. Photoreceptor phagocytosis is mediated by phosphoinositide signaling. FASEB J. 2013, 27, 4585–4595. [Google Scholar] [CrossRef]
- DeVera, C.; Tosini, G. Circadian analysis of the mouse retinal pigment epithelium transcriptome. Exp. Eye Res. 2020, 193, 107988. [Google Scholar] [CrossRef]
- Louer, E.M.; Günzel, D.; Rosenthal, R.; Carmone, C.; Yi, G.; Stunnenberg, H.G.; Hollander, A.I.D.; Deen, P.M. Differential day-night expression of tight junction components in murine retinal pigment epithelium. Exp. Eye Res. 2020, 193, 107985. [Google Scholar] [CrossRef]
- Chao, J.R.; Knight, K.; Engel, A.L.; Jankowski, C.; Wang, Y.; Manson, M.A.; Gu, H.; Djukovic, D.; Raftery, D.; Hurley, J.B.; et al. Human retinal pigment epithelial cells prefer proline as a nutrient and transport metabolic intermediates to the retinal side. J. Biol. Chem. 2017, 292, 12895–12905. [Google Scholar] [CrossRef]
- Milićević, N.; Hakkari, O.A.; Bagchi, U.; Sandu, C.; Jongejan, A.; Moerland, P.D.; Brink, J.B.T.; Hicks, D.; Bergen, A.A.; Felder-Schmittbuhl, M. Core circadian clock genes Per1 and Per2 regulate the rhythm in photoreceptor outer segment phagocytosis. FASEB J. 2021, 35, e21722. [Google Scholar] [CrossRef] [PubMed]
- DeVera, C.; Dixon, J.; Chrenek, M.A.; Baba, K.; Iuvone, P.M.; Tosini, G. The circadian clock in the retinal pigment epithelium controls the diurnal rhythm of phagocytic activity. bioRxiv 2020. [Google Scholar] [CrossRef]
- Nandrot, E.; Dufour, E.M.; Provost, A.C.; Péquignot, M.O.; Bonnel, S.; Gogat, K.; Marchant, D.; Rouillac, C.; de Condé, B.S.; Bihoreau, M.-T.; et al. Homozygous Deletion in the Coding Sequence of the c-mer Gene in RCS Rats Unravels General Mechanisms of Physiological Cell Adhesion and Apoptosis. Neurobiol. Dis. 2000, 7, 586–599. [Google Scholar] [CrossRef] [PubMed]
- D’Cruz, P.M.; Yasumura, D.; Weir, J.; Matthes, M.T.; Abderrahim, H.; Lavail, M.M.; Vollrath, D. Mutation of the receptor tyrosine kinase gene Mertk in the retinal dystrophic RCS rat. Hum. Mol. Genet. 2000, 9, 645–651. [Google Scholar] [CrossRef]
- Lu, Q.; Gore, M.; Zhang, Q.; Camenisch, T.; Boast, S.; Casagranda, F.; Lai, C.; Skinner, M.K.; Klein, R.; Matsushima, G.K.; et al. Tyro-3 family receptors are essential regulators of mammalian spermatogenesis. Nature 1999, 398, 723–728. [Google Scholar] [CrossRef]
- Brea-Fernandez, A.J.; Pomares, E.; Brion, M.J.; Marfany, G.; Blanco, M.J.; Sanchez-Salorio, M.; Gonzalez-Duarte, R.; Carracedo, A. Novel splice donor site mutation in MERTK gene associated with retinitis pigmentosa. Br. J. Ophthalmol. 2008, 92, 1419–1423. [Google Scholar] [CrossRef]
- Ksantini, M.; Lafont, E.; Bocquet, B.; Meunier, I.; Hamel, C.P. Homozygous Mutation in MERTK Causes Severe Autosomal Recessive Retinitis Pigmentosa. Eur. J. Ophthalmol. 2011, 22, 647–653. [Google Scholar] [CrossRef]
- Mackay, D.S.; Henderson, R.H.; Sergouniotis, P.I.; Li, Z.; Moradi, P.; Holder, G.E.; Waseem, N.; Bhattacharya, S.S.; Aldahmesh, M.A.; Alkuraya, F.S.; et al. Novel mutations in MERTK associated with childhood onset rod-cone dystrophy. Mol. Vis. 2010, 16, 369–377. [Google Scholar]
- McHenry, C.L.; Liu, Y.; Feng, W.; Nair, A.R.; Feathers, K.L.; Ding, X.; Gal, A.; Vollrath, U.; Sieving, P.A.; Thompson, D. MERTK arginine-844-cysteine in a patient with severe rod-cone dystrophy: Loss of mutant protein function in transfected cells. Investig. Opthalmology Vis. Sci. 2004, 45, 1456–1463. [Google Scholar] [CrossRef]
- Tschernutter, M.; Jenkins, S.A.; Waseem, N.H.; Saihan, Z.; E Holder, G.; Bird, A.C.; Bhattacharya, S.S.; Ali, R.R.; Webster, A.R. Clinical characterisation of a family with retinal dystrophy caused by mutation in the Mertk gene. Br. J. Ophthalmol. 2006, 90, 718–723. [Google Scholar] [CrossRef]
- Prasad, D.; Rothlin, C.V.; Burrola, P.; Burstyn-Cohen, T.; Lu, Q.; de Frutos, P.G.; Lemke, G. TAM receptor function in the retinal pigment epithelium. Mol. Cell. Neurosci. 2006, 33, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Kondo, M.; Yasuma, T.; D’Alessandro-Gabazza, C.N.; Toda, M.; Imai, H.; Nakamura, M.; Gabazza, E.C. Increased expression of Protein S in eyes with diabetic retinopathy and diabetic macular edema. Sci. Rep. 2021, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Adijanto, J.; Philp, N.J. Cultured primary human fetal retinal pigment epithelium (hfRPE) as a model for evaluating RPE metabolism. Exp. Eye Res. 2014, 126, 77–84. [Google Scholar] [CrossRef]
- Hu, J.; Bok, D. The use of cultured human fetal retinal pigment epithelium in studies of the classical retinoid visual cycle and retinoid-based disease processes. Exp. Eye Res. 2013, 126, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Mayerson, P.L.; Hall, M.O.; Clark, V.; Abrams, T. An improved method for isolation and culture of rat retinal pigment epithelial cells. Investig. Ophthalmol. Vis. Sci. 1985, 26, 1599–1609. [Google Scholar]
- Sonoda, S.; Spee, C.; Barron, E.; Ryan, S.J.; Kannan, R.; Hinton, D.R. A protocol for the culture and differentiation of highly polarized human retinal pigment epithelial cells. Nat. Protoc. 2009, 4, 662–673. [Google Scholar] [CrossRef]
- Godino, R.F.; Garland, D.L.; Pierce, E. Isolation, culture and characterization of primary mouse RPE cells. Nat. Protoc. 2016, 11, 1206–1218. [Google Scholar] [CrossRef]
- Dunn, K.C.; Aotaki-Keen, A.E.; Putkey, F.R.; Hjelmeland, L.M. ARPE-19, A Human Retinal Pigment Epithelial Cell Line with Differentiated Properties. Exp. Eye Res. 1996, 62, 155–170. [Google Scholar] [CrossRef]
- Nabi, I.; Mathews, A.; Cohen-Gould, L.; Gundersen, D.; Rodriguez-Boulan, E. Immortalization of polarized rat retinal pigment epithelium. J. Cell Sci. 1993, 104, 37–49. [Google Scholar] [CrossRef]
- Kuznetsova, A.V.; Kurinov, A.M.; Aleksandrova, M.A. Cell Models to Study Regulation of Cell Transformation in Pathologies of Retinal Pigment Epithelium. J. Ophthalmol. 2014, 2014, 1–18. [Google Scholar] [CrossRef]
- Fronk, A.H.; Vargis, E. Methods for culturing retinal pigment epithelial cells: A review of current protocols and future recommendations. J. Tissue Eng. 2016, 7, 27493715. [Google Scholar] [CrossRef]
- Lakkaraju, A.; Umapathy, A.; Tan, L.X.; Daniele, L.; Philp, N.J.; Boesze-Battaglia, K.; Williams, D.S. The cell biology of the retinal pigment epithelium. Prog. Retin. Eye Res. 2020, 78, 100846. [Google Scholar] [CrossRef] [PubMed]
- Pavan, B.; Frigato, E.; Pozzati, S.; Prasad, P.D.; Bertolucci, C.; Biondi, C. Circadian clocks regulate adenylyl cyclase activity rhythms in human RPE cells. Biochem. Biophys. Res. Commun. 2006, 350, 169–173. [Google Scholar] [CrossRef]
- Yoshikawa, A.; Shimada, H.; Numazawa, K.; Sasaki, T.; Ikeda, M.; Kawashima, M.; Kato, N.; Tokunaga, K.; Ebisawa, T. Establishment of human cell lines showing circadian rhythms of bioluminescence. Neurosci. Lett. 2008, 446, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Milićević, N.; Mazzaro, N.; De Bruin, I.; Wils, E.; Brink, J.T.; Asbroek, A.T.; Mendoza, J.; Bergen, A.; Felder-Schmittbuhl, M.-P. Rev-Erbα and Photoreceptor Outer Segments modulate the Circadian Clock in Retinal Pigment Epithelial Cells. Sci. Rep. 2019, 9, 1–13. [Google Scholar] [CrossRef]
- Yoo, S.H.; Yamazaki, S.; Lowrey, P.L.; Shimomura, K.; Ko, C.H.; Buhr, E.D.; Siepka, S.M.; Hong, H.K.; Oh, W.J.; Yoo, O.J.; et al. PERIOD2::LUCIFERASE real-time reporting of circadian dynamics reveals persistent circadian oscillations in mouse peripheral tissues. Proc. Natl. Acad. Sci. USA 2004, 101, 5339–5346. [Google Scholar] [CrossRef] [PubMed]
- Baba, K.; Davidson, A.J.; Tosini, G. Melatonin Entrains PER2::LUC Bioluminescence Circadian Rhythm in the Mouse Cornea. Invest. Ophthalmol. Vis. Sci. 2015, 56, 4753–4758. [Google Scholar] [CrossRef]
- Dunmire, J.; Dalvin, L.; Bouhenni, R.; Edward, D. Expression of Circadian Rhythm Genes in the Mouse Iris-Ciliary Body Complex. Investig. Ophthalmol. Vis. Sci. 2013, 54, 1994. [Google Scholar]
- Tsuchiya, S.; Buhr, E.D.; Higashide, T.; Sugiyama, K.; Van Gelder, R.N. Light entrainment of the murine intraocular pressure circadian rhythm utilizes non-local mechanisms. PLoS ONE 2017, 12, e0184790. [Google Scholar] [CrossRef]
- Evans, J.A.; Suen, T.-C.; Callif, B.L.; Mitchell, A.S.; Castanon-Cervantes, O.; Baker, K.M.; Kloehn, I.; Baba, K.; Teubner, B.J.W.; Ehlen, J.C.; et al. Shell neurons of the master circadian clock coordinate the phase of tissue clocks throughout the brain and body. BMC Biol. 2015, 13, 1–15. [Google Scholar] [CrossRef]
- Buhr, E.D.; Yue, W.W.S.; Ren, X.; Jiang, Z.; Liao, H.-W.R.; Mei, X.; Vemaraju, S.; Nguyen, M.-T.; Reed, R.R.; Lang, R.; et al. Neuropsin (OPN5)-mediated photoentrainment of local circadian oscillators in mammalian retina and cornea. Proc. Natl. Acad. Sci. USA 2015, 112, 13093–13098. [Google Scholar] [CrossRef]
- Ikarashi, R.; Akechi, H.; Kanda, Y.; Ahmad, A.; Takeuchi, K.; Morioka, E.; Sugiyama, T.; Ebisawa, T.; Ikeda, M.; Ikeda, M. Regulation of molecular clock oscillations and phagocytic activity via muscarinic Ca2+ signaling in human retinal pigment epithelial cells. Sci. Rep. 2017, 7, 44175. [Google Scholar] [CrossRef] [PubMed]
- Besharse, J.C.; Dunis, D.A. Methoxyindoles and Photoreceptor Metabolism: Activation of Rod Shedding. Science 1983, 219, 1341–1343. [Google Scholar] [CrossRef] [PubMed]
- Reme, C.; Wirz-Justice, A.; Rhyner, A.; Hofmann, S. Circadian rhythm in the light response of rat retinal disk-shedding and autophagy. Brain Res. 1986, 369, 356–360. [Google Scholar] [CrossRef]
- Mariani, A.P.; Neff, N.H.; Hadjiconstantinou, M. 1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) treatment decreases dopamine and increases lipofuscin in mouse retina. Neurosci. Lett. 1986, 72, 221–226. [Google Scholar] [CrossRef]
- Ginty, D.D.; Kornhauser, J.M.; Thompson, M.A.; Bading, H.; Mayo, K.E.; Takahashi, J.S.; Greenberg, M.E. Regulation of CREB Phosphorylation in the Suprachiasmatic Nucleus by Light and a Circadian Clock. Science 1993, 260, 238–241. [Google Scholar] [CrossRef]
- Ding, J.M.; Faiman, L.E.; Hurst, W.J.; Kuriashkina, L.R.; Gillette, M.U. Resetting the Biological Clock: Mediation of Nocturnal CREB Phosphorylation via Light, Glutamate, and Nitric Oxide. J. Neurosci. 1997, 17, 667–675. [Google Scholar] [CrossRef]
- Yagita, K.; Okamura, H. Forskolin induces circadian gene expression of rPer1, rPer2 and dbp in mammalian rat-1 fibroblasts. FEBS Lett. 1999, 465, 79–82. [Google Scholar] [CrossRef]
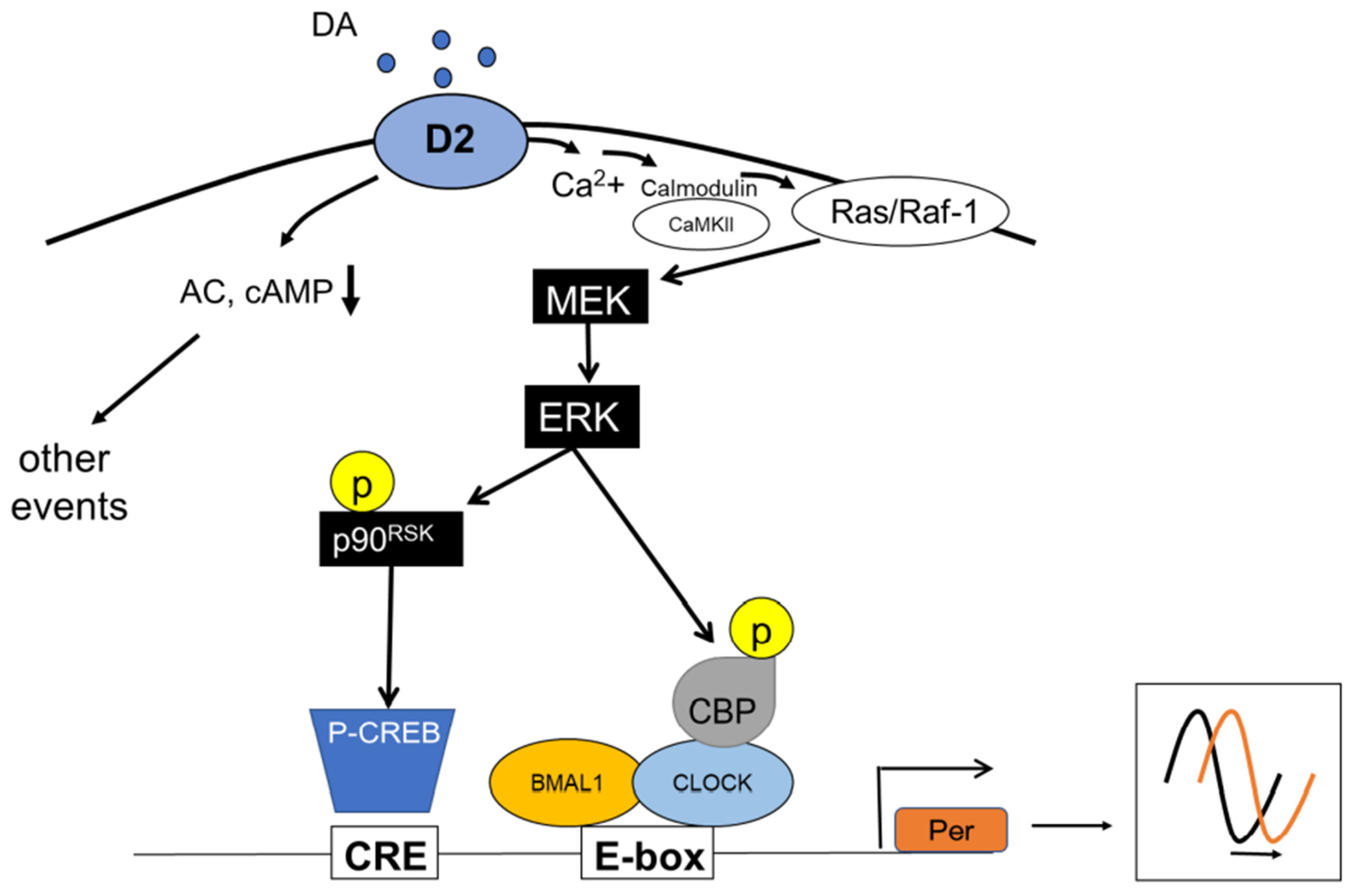
- Yan, Z.; Feng, J.; Fienberg, A.A.; Greengard, P. D2 dopamine receptors induce mitogen-activated protein kinase and cAMP response element-binding protein phosphorylation in neurons. Proc. Natl. Acad. Sci. USA 1999, 96, 11607–11612. [Google Scholar] [CrossRef]
- Choe, E.S.; Wang, J.Q. CaMKII regulates amphetamine-induced ERK1/2 phosphorylation in striatal neurons. Neuroreport 2002, 13, 1013–1016. [Google Scholar] [CrossRef]
- Illario, M.; Cavallo, A.L.; Bayer, K.U.; Di Matola, T.; Fenzi, G.; Rossi, G.; Vitale, M. Calcium/Calmodulin-dependent Protein Kinase II Binds to Raf-1 and Modulates Integrin-stimulated ERK Activation. J. Biol. Chem. 2003, 278, 45101–45108. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, J.M.; Wayman, G.A.; Nozaki, N.; Soderling, T.R. Calcium Activation of ERK Mediated by Calmodulin Kinase I. J. Biol. Chem. 2004, 279, 24064–24072. [Google Scholar] [CrossRef] [PubMed]
- Obrietan, K.; Impey, S.; Storm, D.R. Light and circadian rhythmicity regulate MAP kinase activation in the suprachiasmatic nuclei. Nat. Neurosci. 1998, 1, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Butcher, G.Q.; Lee, B.; Obrietan, K. Temporal Regulation of Light-Induced Extracellular Signal-Regulated Kinase Activation in the Suprachiasmatic Nucleus. J. Neurophysiol. 2003, 90, 3854–3863. [Google Scholar] [CrossRef] [PubMed]
- Coogan, A.N.; Piggins, H.D. Circadian and photic regulation of phosphorylation of ERK1/2 and Elk-1 in the suprachiasmatic nuclei of the Syrian hamster. J. Neurosci. 2003, 23, 3085–3093. [Google Scholar] [CrossRef]
- Nakaya, M.; Sanada, K.; Fukada, Y. Spatial and temporal regulation of mitogen-activated protein kinase phosphorylation in the mouse suprachiasmatic nucleus. Biochem. Biophys. Res. Commun. 2003, 305, 494–501. [Google Scholar] [CrossRef]
- Baler, R.; Covington, S.; Klein, D.C. The Rat Arylalkylamine N-Acetyltransferase Gene Promoter: cAMP activation via A cAMP-responsive element-CCAAT complex. J. Biol. Chem. 1997, 272, 6979–6985. [Google Scholar] [CrossRef]
- Butcher, G.Q.; Lee, B.; Hsieh, F.; Obrietan, K. Light- and clock-dependent regulation of ribosomal S6 kinase activity in the suprachiasmatic nucleus. Eur. J. Neurosci. 2004, 19, 907–915. [Google Scholar] [CrossRef]
- Morioka, E.; Kanda, Y.; Koizumi, H.; Miyamoto, T.; Ikeda, M. Histamine Regulates Molecular Clock Oscillations in Human Retinal Pigment Epithelial Cells via H1 Receptors. Front. Endocrinol. 2018, 9, 108. [Google Scholar] [CrossRef]
- Yujnovsky, I.; Hirayama, J.; Doi, M.; Borrelli, E.; Sassone-Corsi, P. Signaling mediated by the dopamine D2 receptor potentiates circadian regulation by CLOCK:BMAL1. Proc. Natl. Acad. Sci. USA 2006, 103, 6386–6391. [Google Scholar] [CrossRef]
- Iuvone, P.M.; Galli, C.L.; Garrison-Gund, C.K.; Neff, N.H. Light Stimulates Tyrosine Hydroxylase Activity and Dopamine Synthesis in Retinal Amacrine Neurons. Science 1978, 202, 901–902. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baba, K.; Goyal, V.; Tosini, G. Circadian Regulation of Retinal Pigment Epithelium Function. Int. J. Mol. Sci. 2022, 23, 2699. https://doi.org/10.3390/ijms23052699
Baba K, Goyal V, Tosini G. Circadian Regulation of Retinal Pigment Epithelium Function. International Journal of Molecular Sciences. 2022; 23(5):2699. https://doi.org/10.3390/ijms23052699
Chicago/Turabian StyleBaba, Kenkichi, Varunika Goyal, and Gianluca Tosini. 2022. "Circadian Regulation of Retinal Pigment Epithelium Function" International Journal of Molecular Sciences 23, no. 5: 2699. https://doi.org/10.3390/ijms23052699
APA StyleBaba, K., Goyal, V., & Tosini, G. (2022). Circadian Regulation of Retinal Pigment Epithelium Function. International Journal of Molecular Sciences, 23(5), 2699. https://doi.org/10.3390/ijms23052699






