Combined Administration of Pravastatin and Metformin Attenuates Acute Radiation-Induced Intestinal Injury in Mouse and Minipig Models
Abstract
:1. Introduction
2. Results
2.1. Effects of Combined PS and MF Treatment on Survival Rate and Radiation-Induced Intestinal Injury in the Mouse Model
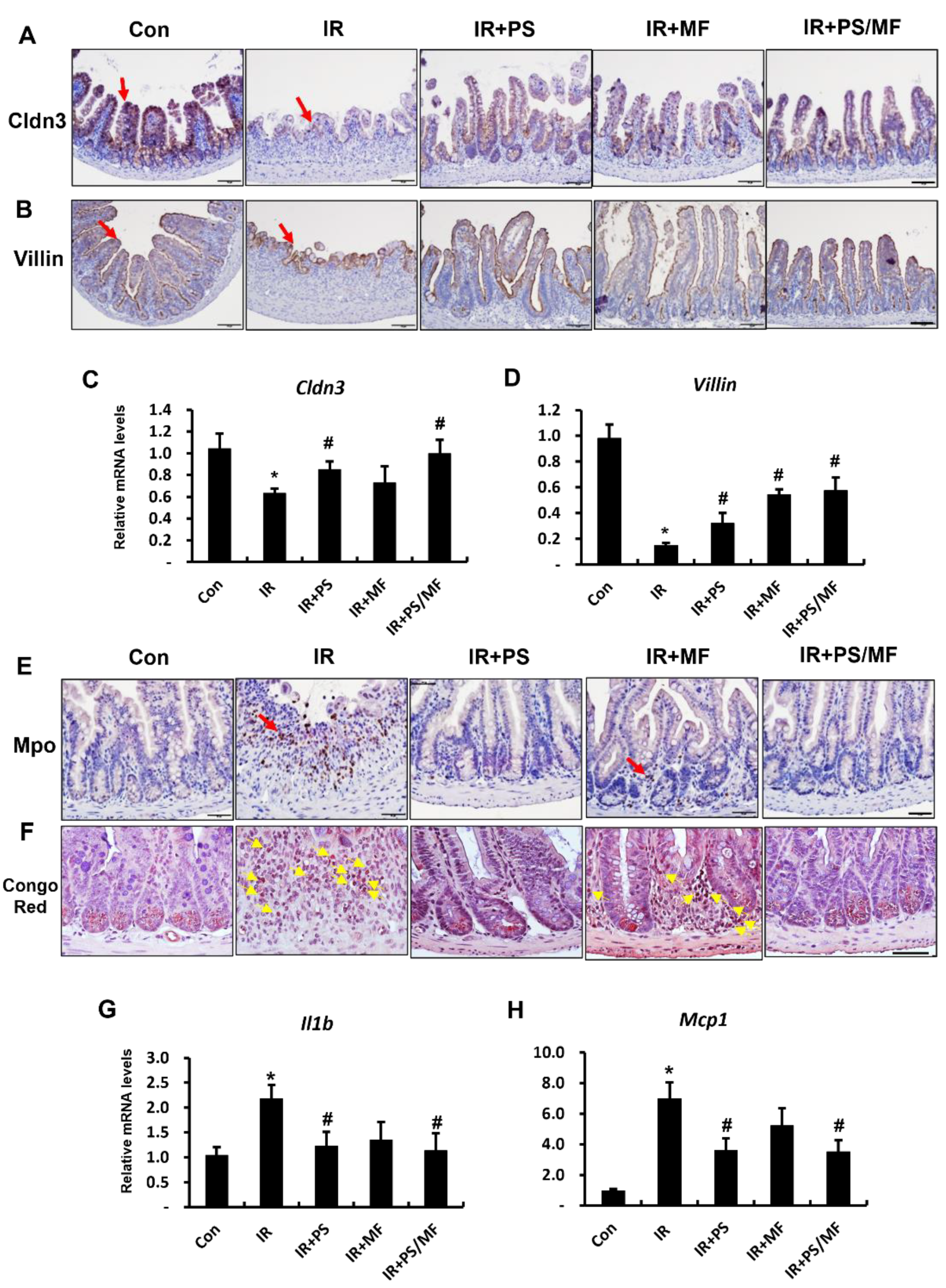
2.2. Effect of Combined PS and MF Treatment on Epithelial Barrier Damage and Inflammatory Response in Radiation-Induced Intestinal Injury
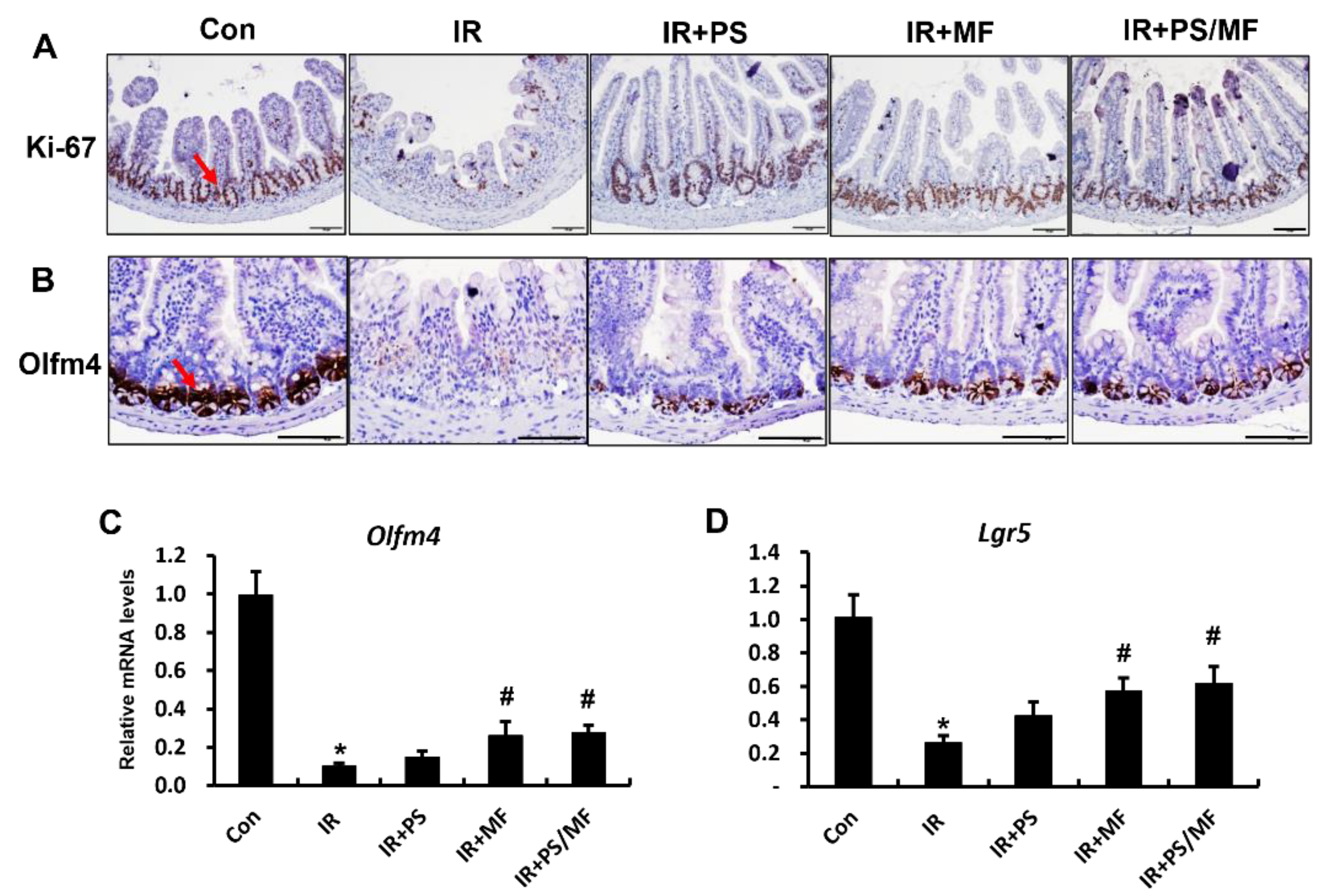
2.3. Effect of Combined PS and MF Treatment on Epithelial Cell Proliferation in Radiation-Induced Intestinal Injury
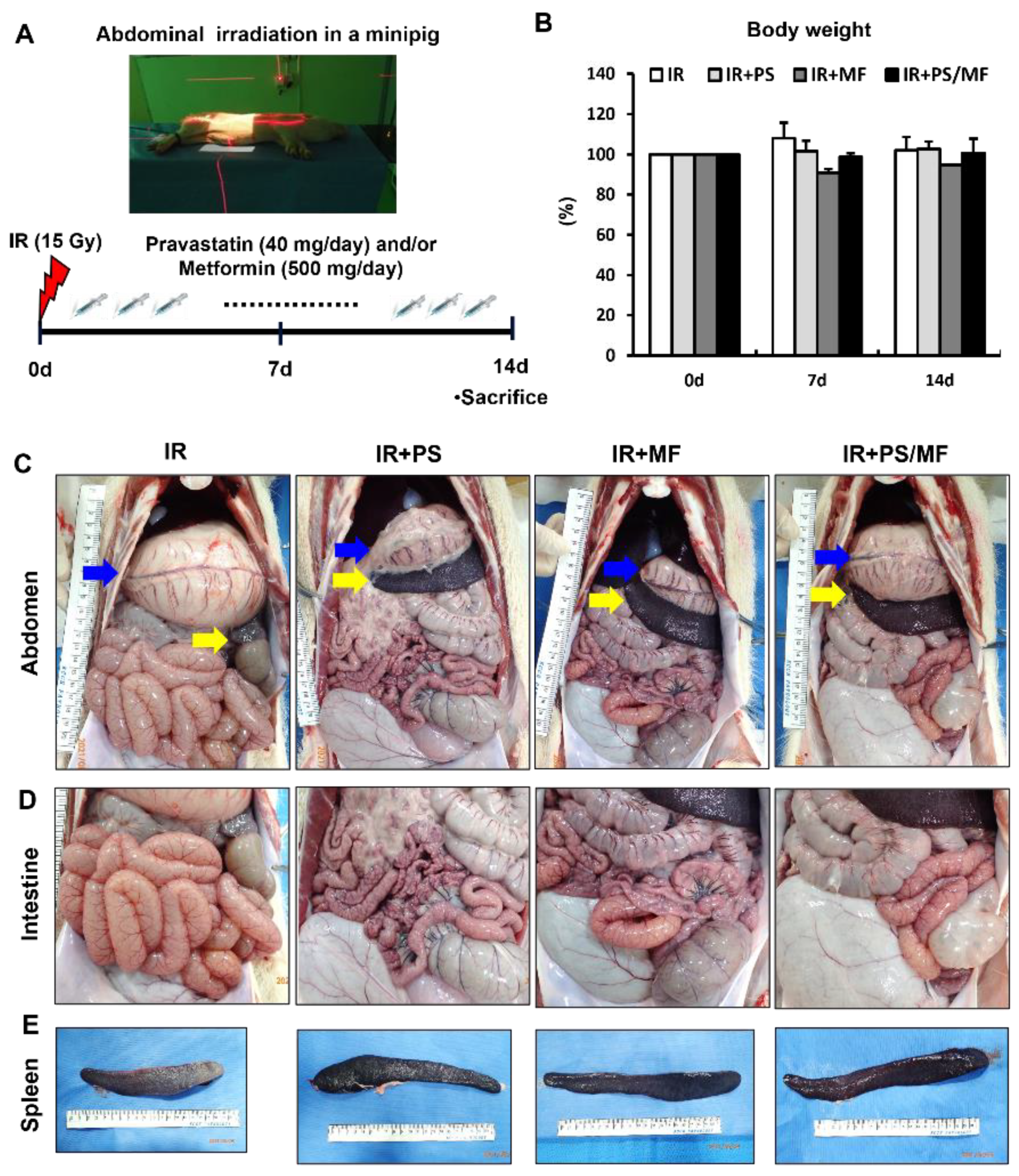
2.4. Effect of Combined PS and MF Treatment on Radiation-Induced Damage in a Minipig Model: Gross Morphology of Abdominal Organs
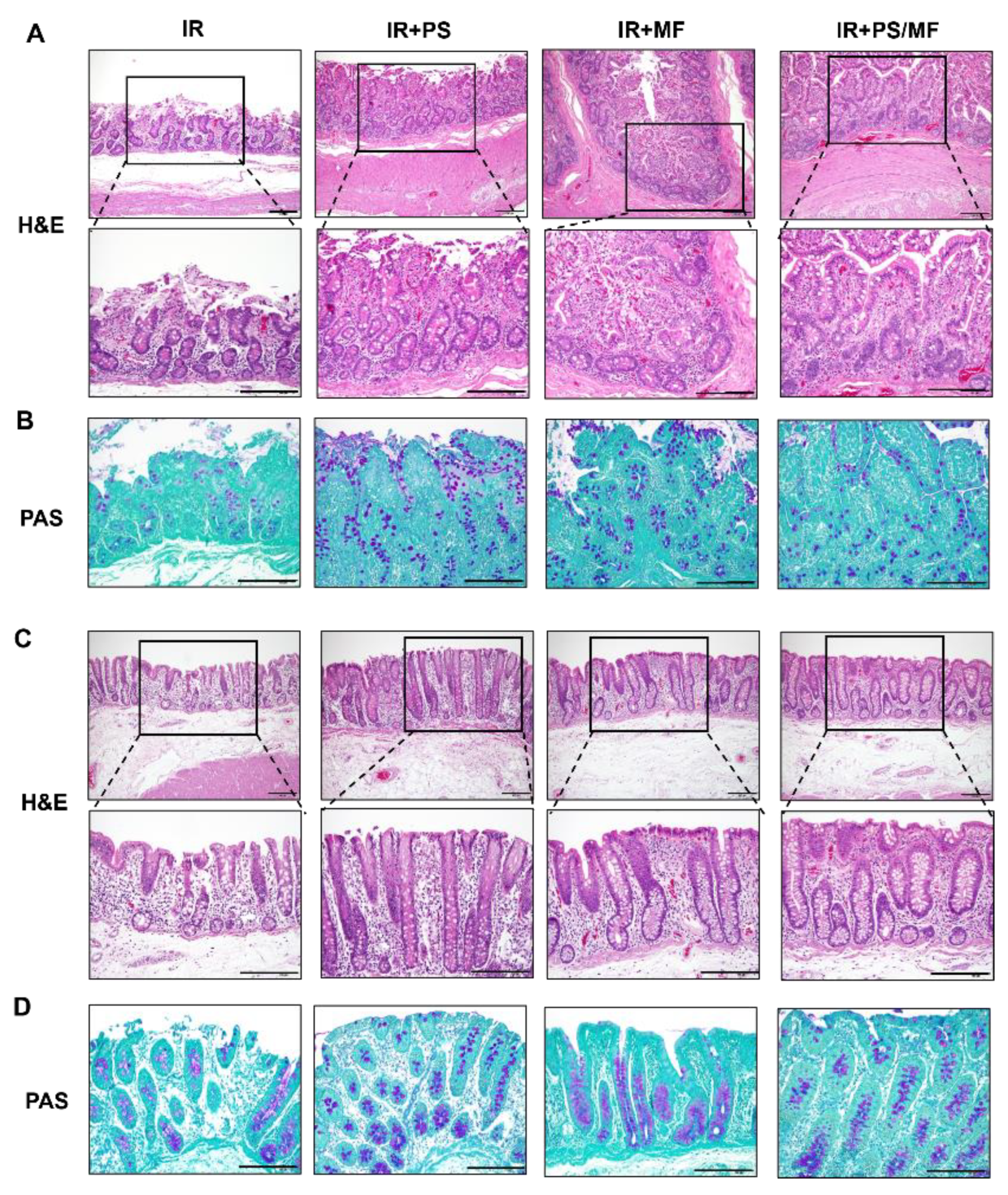
2.5. Effect of Combined PS and MF Treatment on Histological Damage of the Intestine in the Irradiated Minipig Model
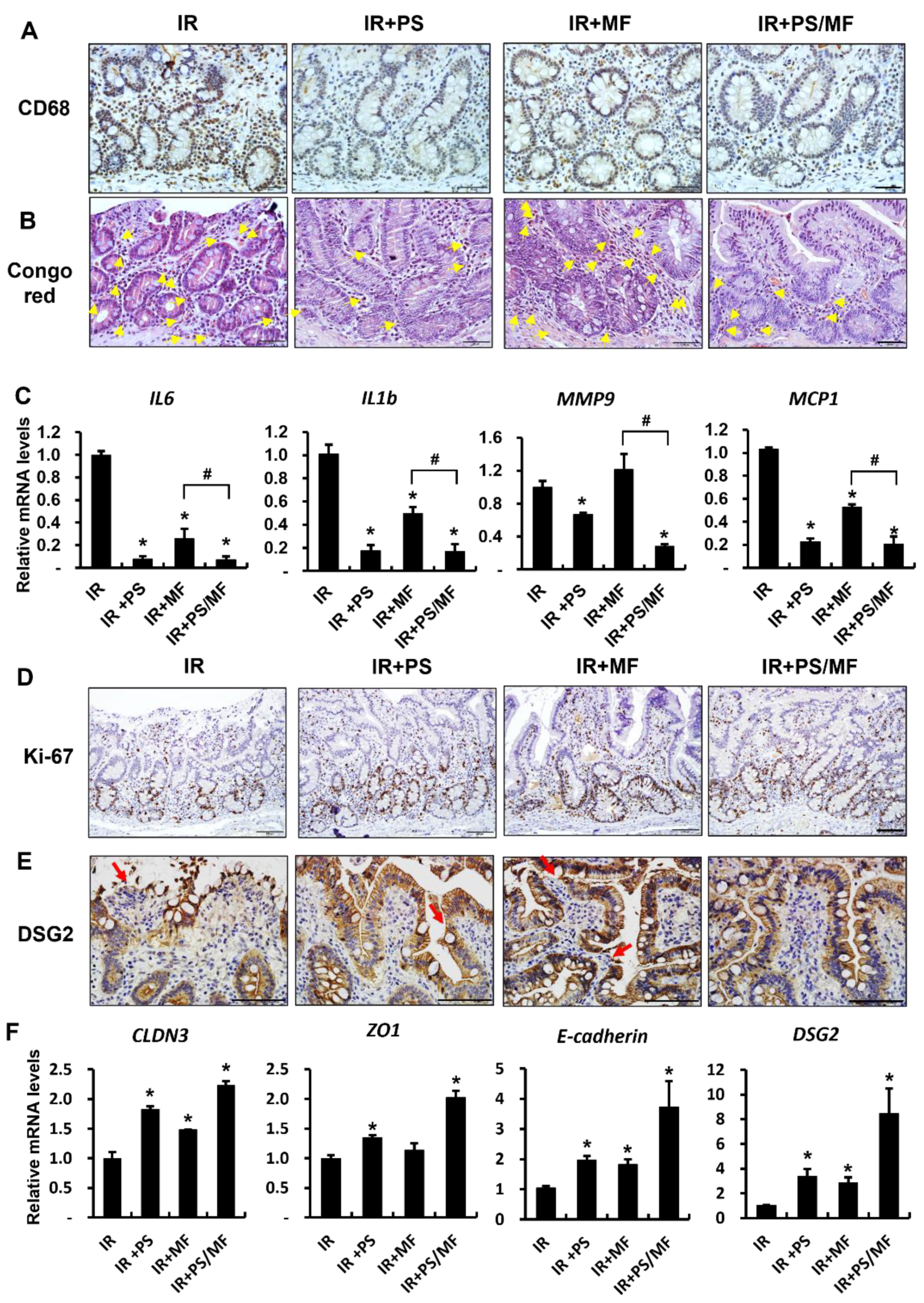
2.6. Effect of Combined PS and MF Treatment on Inflammatory Response and Epithelial Integrity in Irradiated Minipig Model
3. Discussion
4. Material and Methods
4.1. Animal
4.1.1. Mice
4.1.2. Minipigs
4.2. Irradiation and Treatment
4.2.1. Irradiation and Treatment in Mice
4.2.2. Irradiation and Treatment in Minipigs
4.3. Histological Analysis of the Intestinal Tissue
4.4. RNA Extraction, Reverse Transcription-Polymerase Chain Reaction (RT-PCR), and Real-Time PCR Quantification
4.5. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andreyev, J. Gastrointestinal complications of pelvic radiotherapy: Are they of any importance? Gut 2005, 54, 1051–1054. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, L.; Li, W.; Chen, L.; Su, Q.; Wang, Y.; Guo, Z.; Lu, Y.; Liu, B.; Qin, S. Radiation-induced intestinal damage: Latest molecular and clinical developments. Futur. Oncol. 2019, 15, 4105–4118. [Google Scholar] [CrossRef] [PubMed]
- Citrin, D.; Cotrim, A.P.; Hyodo, F.; Baum, B.J.; Krishna, M.C.; Mitchell, J.B. Radioprotectors and mitigators of radiation-induced normal tissue injury. Oncologist 2010, 15, 360–371. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Hu, W.; Wang, W.; Chen, P.; Ding, W.; Luo, W. Replanning during intensity modulated radiation therapy improved quality of life in patients with nasopharyngeal carcinoma. Int. J. Radiat. Oncol. 2013, 85, e47–e54. [Google Scholar] [CrossRef]
- Dubois, A.; Walker, R.I. Prospects for management of gastrointestinal injury associated with the acute radiation syndrome. Gastroenterology 1988, 95, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Damman, C.J.; Surawicz, C.M. The gut microbiota: A microbial arsenal protecting us from infectious and radiation-induced diarrhea. Gastroenterology 2009, 136, 722–724. [Google Scholar] [CrossRef] [PubMed]
- Rosenson, R.S. Non-lipid-lowering effects of statins on atherosclerosis. Curr. Cardiol. Rep. 1999, 1, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Meyer, N.; Brodowski, L.; Richter, K.; von Kaisenberg, C.S.; Schröder-Heurich, B.; von Versen-Höynck, F. Pravastatin promotes endothelial colony-forming cell function, angiogenic signaling and protein expression in vitro. J. Clin. Med. 2021, 10, 183. [Google Scholar] [CrossRef]
- Gaugler, M.-H.; Vereycken-Holler, V.; Squiban, C.; Vandamme, M.; Vozenin-Brotons, M.-C.; Benderitter, M. Pravastatin limits endothelial activation after irradiation and decreases the resulting inflammatory and thrombotic responses. Radiat. Res. 2005, 163, 479–487. [Google Scholar] [CrossRef]
- Haydont, V.; Bourgier, C.; Pocard, M.; Lusinchi, A.; Aigueperse, J.; Mathé, D.; Bourhis, J.; Vozenin-Brotons, M.-C. Pravastatin Inhibits the Rho/CCN2/extracellular matrix cascade in human fibrosis explants and improves radiation-induced intestinal fibrosis in rats. Clin. Cancer Res. 2007, 13, 5331–5340. [Google Scholar] [CrossRef]
- Holler, V.; Buard, V.; Gaugler, M.-H.; Guipaud, O.; Baudelin, C.; Sache, A.; Perez, M.d.R.; Squiban, C.; Tamarat, R.; Milliat, F. Pravastatin limits radiation-induced vascular dysfunction in the skin. J. Investig. Dermatol. 2009, 129, 1280–1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, H.; Lee, J.; Park, S.; Myung, H.; Kang, J.; Kim, K.; Kim, H.; Jang, W.-S.; Lee, S.-J.; Shim, S.; et al. Pravastatin attenuates acute radiation-induced enteropathy and improves epithelial cell function. Front. Pharmacol. 2018, 9, 1215. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Kwak, S.Y.; Park, S.; Kim, K.; Kim, Y.H.; Na, J.; Kim, H.; Jang, W.S.; Lee, S.J.; Kim, M.J.; et al. Pravastatin Alleviates Radiation Proctitis by Regulating Thrombomodulin in Irradiated Endothelial Cells. Int. J. Mol. Sci. 2020, 21, 1897. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwak, S.Y.; Jang, W.I.; Park, S.; Cho, S.S.; Lee, S.B.; Kim, M.-J.; Park, S.; Shim, S.; Jang, H. Metallothionein 2 activation by pravastatin reinforces epithelial integrity and ameliorates radiation-induced enteropathy. EBioMedicine 2021, 73, 103641. [Google Scholar] [CrossRef]
- Wedlake, L.J.; Silia, F.; Benton, B.; Lalji, A.; Thomas, K.; Dearnaley, D.P.; Blake, P.; Tait, D.; Khoo, V.S.; Andreyev, H.J.N. Evaluating the efficacy of statins and ACE-inhibitors in reducing gastrointestinal toxicity in patients receiving radiotherapy for pelvic malignancies. Eur. J. Cancer 2012, 48, 2117–2124. [Google Scholar] [CrossRef]
- Tao, L.; Li, D.; Liu, H.; Jiang, F.; Xu, Y.; Cao, Y.; Gao, R.; Chen, G. Neuroprotective effects of metformin on traumatic brain injury in rats associated with NF-κB and MAPK signaling pathway. Brain Res. Bull. 2018, 140, 154–161. [Google Scholar] [CrossRef]
- Mortezaee, K.; Shabeeb, D.; Musa, A.E.; Najafi, M.; Farhood, B. Metformin as a radiation modifier; implications to normal tissue protection and tumor sensitization. Curr. Clin. Pharmacol. 2019, 14, 41–53. [Google Scholar] [CrossRef]
- Pålsson-McDermott, E.M.; O’Neill, L.A. Targeting immunometabolism as an anti-inflammatory strategy. Cell Res. 2020, 30, 300–314. [Google Scholar] [CrossRef] [Green Version]
- Bagheri, H.; Rezapoor, S.; Najafi, M.; Safar, H.; Shabeeb, D.; Cheki, M.; Shekarchi, B.; Motevaseli, E. Metformin protects the rat small intestine against radiation enteritis. Jundishapur J. Nat. Pharm. Prod. 2019, 14, e67352. [Google Scholar] [CrossRef]
- Najafi, M.; Cheki, M.; Hassanzadeh, G.; Amini, P.; Shabeeb, D.; Musa, A.E. Protection from radiation-induced damage in rat’s ileum and colon by combined regimens of melatonin and metformin: A histopathological study. Anti-Inflamm. Anti-Allergy Agents Med. Chem. 2020, 19, 180–189. [Google Scholar] [CrossRef]
- Jang, H.; Kim, S.; Kim, H.; Oh, S.H.; Kwak, S.Y.; Joo, H.-W.; Lee, S.B.; Jang, W.I.; Park, S.; Shim, S. Metformin Protects the Intestinal Barrier by Activating Goblet Cell Maturation and Epithelial Proliferation in Radiation-Induced Enteropathy. Int. J. Mol. Sci. 2022, 23, 5929. [Google Scholar] [CrossRef] [PubMed]
- Vigneulle, R.M.; Rao, S.; Fasano, A.; MacVittie, T.J. Structural and functional alterations of the gastrointestinal tract following radiation-induced injury in the rhesus monkey. Am. J. Dig. Dis. 2002, 47, 1480–1491. [Google Scholar]
- Heining, P.; Ruysschaert, T. The use of minipig in drug discovery and development: Pros and cons of minipig selection and strategies to use as a preferred nonrodent species. Toxicol. Pathol. 2016, 44, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henze, L.J.; Koehl, N.J.; O’Shea, J.P.; Kostewicz, E.S.; Holm, R.; Griffin, B.T. The pig as a preclinical model for predicting oral bioavailability and in vivo performance of pharmaceutical oral dosage forms: A PEARRL review. J. Pharm. Pharmacol. 2019, 71, 581–602. [Google Scholar] [CrossRef] [Green Version]
- Augustine, A.D.; Gondré-Lewis, T.; McBride, W.; Miller, L.; Pellmar, T.C.; Rockwell, S. Animal models for radiation injury, protection and therapy. Radiat. Res. 2005, 164, 100–109. [Google Scholar] [CrossRef]
- Jones, S.; George, R.; West, J.; Verrelli, D. The relative effectiveness of fission neutrons for gastrointestinal death in miniature pigs. Radiat. Res. 1972, 50, 504–518. [Google Scholar] [CrossRef]
- Shim, S.; Jang, W.-S.; Lee, S.-J.; Jin, S.; Kim, J.; Lee, S.-S.; Bang, H.Y.; Jeon, B.S.; Park, S. Development of a new minipig model to study radiation-induced gastrointestinal syndrome and its application in clinical research. Radiat. Res. 2014, 181, 387–395. [Google Scholar] [CrossRef]
- Schulzke, J.D.; Ploeger, S.; Amasheh, M.; Fromm, A.; Zeissig, S.; Troeger, H.; Richter, J.; Bojarski, C.; Schumann, M.; Fromm, M. Epithelial tight junctions in intestinal inflammation. Ann. N. Y. Acad. Sci. 2009, 1165, 294–300. [Google Scholar] [CrossRef]
- Turner, J.R. Intestinal mucosal barrier function in health and disease. Nat. Rev. Immunol. 2009, 9, 799–809. [Google Scholar] [CrossRef]
- Shukla, P.K.; Gangwar, R.; Manda, B.; Meena, A.S.; Yadav, N.; Szabo, E.; Balogh, A.; Lee, S.C.; Tigyi, G.; Rao, R. Rapid disruption of intestinal epithelial tight junction and barrier dysfunction by ionizing radiation in mouse colon in vivo: Protection by N-acetyl-l-cysteine. Am. J. Physiol. Liver Physiol. 2016, 310, G705–G715. [Google Scholar] [CrossRef] [Green Version]
- Radnai, B.; Sturm, E.M.; Stančić, A.; Jandl, K.; Labocha, S.; Ferreirós, N.; Grill, M.; Hasenoehrl, C.; Gorkiewicz, G.; Marsche, G. Eosinophils contribute to intestinal inflammation via chemoattractant receptor-homologous molecule expressed on Th2 cells, CRTH2, in experimental Crohn’s disease. J. Crohn’s Colitis 2016, 10, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- Takemura, N.; Kurashima, Y.; Mori, Y.; Okada, K.; Ogino, T.; Osawa, H.; Matsuno, H.; Aayam, L.; Kaneto, S.; Park, E.J. Eosinophil depletion suppresses radiation-induced small intestinal fibrosis. Sci. Transl. Med. 2018, 10, eaan0333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eder, P.; Adler, M.; Dobrowolska, A.; Kamhieh-Milz, J.; Witowski, J. The role of adipose tissue in the pathogenesis and therapeutic outcomes of inflammatory bowel disease. Cells 2019, 8, 628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saha, S.; Bhanja, P.; Liu, L.; Alfieri, A.A.; Yu, D.; Kandimalla, E.R.; Agrawal, S.; Guha, C. TLR9 agonist protects mice from radiation-induced gastrointestinal syndrome. PLoS ONE 2012, 7, e29357. [Google Scholar] [CrossRef]
- Saha, S.; Aranda, E.; Hayakawa, Y.; Bhanja, P.; Atay, S.; Brodin, N.P.; Li, J.; Asfaha, S.; Liu, L.; Tailor, Y. Macrophage-derived extracellular vesicle-packaged WNTs rescue intestinal stem cells and enhance survival after radiation injury. Nat. Commun. 2016, 7, 13096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otsuka, K.; Suzuki, K. Differences in radiation dose response between small and large intestinal crypts. Radiat. Res. 2016, 186, 302–314. [Google Scholar] [CrossRef]
- Kim, C.-K.; Yang, V.W.; Bialkowska, A.B. The role of intestinal stem cells in epithelial regeneration following radiation-induced gut injury. Curr. Stem Cell Rep. 2017, 3, 320–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, V.K.; Newman, V.L.; Berg, A.N.; MacVittie, T.J. Animal models for acute radiation syndrome drug discovery. Expert Opin. Drug Discov. 2015, 10, 497–517. [Google Scholar] [CrossRef] [Green Version]
- Leibowitz, B.J.; Wei, L.; Zhang, L.; Ping, X.; Epperly, M.; Greenberger, J.; Cheng, T.; Yu, J. Ionizing irradiation induces acute haematopoietic syndrome and gastrointestinal syndrome independently in mice. Nat. Commun. 2014, 5, 3494. [Google Scholar] [CrossRef] [Green Version]
- Rios, C.I.; Cassatt, D.R.; Dicarlo, A.L.; Macchiarini, F.; Ramakrishnan, N.; Norman, M.K.; Maidment, B.W. Building the strategic national stockpile through the NIAID Radiation Nuclear Countermeasures Program. Drug Dev. Res. 2014, 75, 23–28. [Google Scholar] [CrossRef]
- Van der Laan, J.W.; Brightwell, J.; McAnulty, P.; Ratky, J.; Stark, C. Regulatory acceptability of the minipig in the development of pharmaceuticals, chemicals and other products. J. Pharmacol. Toxicol. Methods 2010, 62, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Kim, J.-s.; Shim, S.; Jang, W.-s.; Lee, S.-J.; Myung, J.K.; Lee, S.-S.; Park, S. Acute radiation syndrome in an irradiated minipig model for patients with radiation exposure. J. Radiat. Prot. Res. 2017, 42, 146–153. [Google Scholar] [CrossRef] [Green Version]
- Nejdfors, P.; Ekelund, M.; Weström, B.R.; Willén, R.; Jeppsson, B. Intestinal permeability in humans is increased after radiation therapy. Dis. Colon Rectum 2000, 43, 1582–1587. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Bhanja, P.; Kabarriti, R.; Liu, L.; Alfieri, A.A.; Guha, C. Bone marrow stromal cell transplantation mitigates radiation-induced gastrointestinal syndrome in mice. PLoS ONE 2011, 6, e24072. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, N.; Kishimoto, T. Interleukin 6: From bench to bedside. Nat. Clin. Pract. Rheumatol. 2006, 2, 619–626. [Google Scholar] [CrossRef]
- Liu, W.; Ding, I.; Chen, K.; Olschowka, J.; Xu, J.; Hu, D.; Morrow, G.R.; Okunieff, P. Interleukin 1beta (IL1B) signaling is a critical component of radiation-induced skin fibrosis. Radiat. Res. 2006, 165, 181–191. [Google Scholar] [CrossRef]
- Baugh, M.D.; Perry, M.J.; Hollander, A.P.; Davies, D.R.; Cross, S.S.; Lobo, A.J.; Taylor, C.J.; Evans, G.S. Matrix metalloproteinase levels are elevated in inflammatory bowel disease. Gastroenterology 1999, 117, 814–822. [Google Scholar] [CrossRef]
- Williams, M.R.; Azcutia, V.; Newton, G.; Alcaide, P.; Luscinskas, F.W. Emerging mechanisms of neutrophil recruitment across endothelium. Trends Immunol. 2011, 32, 461–469. [Google Scholar] [CrossRef] [Green Version]
- Al-Haddad, S.; Riddell, R.; Wanders, A.; Winqvist, O.; Carlson, M.; Lampinen, M. Eosinophil granulocytes are activated during the remission phase of ulcerative colitis. Commentary. Gut 2005, 54, 1674–1675. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Clevers, H. Coexistence of quiescent and active adult stem cells in mammals. Science 2010, 327, 542–545. [Google Scholar] [CrossRef] [Green Version]
- Barker, N. Adult intestinal stem cells: Critical drivers of epithelial homeostasis and regeneration. Nat. Rev. Mol. Cell Biol. 2014, 15, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Hua, G.; Thin, T.H.; Feldman, R.; Haimovitz–Friedman, A.; Clevers, H.; Fuks, Z.; Kolesnick, R. Crypt base columnar stem cells in small intestines of mice are radioresistant. Gastroenterology 2012, 143, 1266–1276. [Google Scholar] [CrossRef] [PubMed]

| Species | Primer | Forward (5′–3′) | Reverse (5′–3′) |
|---|---|---|---|
| Mouse | Cldn3 | AAGCCGAATGGACAAAGAA | CTGGCAAGTAGCTGCAGTG |
| Villin | CACCTTTGGAAGCTTCTTCG | CTCTCGTTGCCTTGAACCTC | |
| Il-1β | GCAACTGTTCCTGAACTCA | CTCGGAGCCTGTAGTGCAG | |
| Mcp-1 | GCAGTTAACGCCCCACTCA | CCCAGCCTACTCATTGGGATCA | |
| Olfm4 | GCTGGAAGTGAAGGAGATGC | ACAGAAGGAGCGCTGATGTT | |
| Lgr5 | TCAGTCAGCTGCTCCCGAAT | CGTTTCCCGCAAGACGTAAC | |
| Gapdh | AAGATGGTGATGGGCTTCCCG | TGGCAAAGTGGAGATTGTTGCC | |
| Minipig | IL-6 | TTCAGTCCAGTCGCCTTCT | GTGGCATCACCTTTGGCATCTTCTT |
| IL-1b | ACCTGGACCTTGGTTCTC | GGATTCTTCATCGGCTTC | |
| MMP-9 | AAGACGCAGAAGGTGGATTC | AACTCACACGCCAGAAGAAG | |
| MCP-1 | TCTCCAGTCACCTGCTGCTA | AGGCTTCGGAGTTTGGTTTT | |
| CLDN3 | GCCAAGATCCTCTACTCCGC | GAGAGCTGCCTAGCATCTGG | |
| ZO1 | GAGGATGGTCACACCGTGGT | GGAGGATGCTGTTGTCTCGG | |
| E-cadherin | AAATGCTAGCTGGTGGGGAC | GCCTCCCATTGCTAACACCT | |
| DSG2 | TCTTCCAGGCAGGGTCAAAC | CCAGGATCACAGTGCTTGGT | |
| GAPDH | GAAGGTCGGAGTGAACGGAT | CATGGGTAGAATCATACTGGAACA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.M.; Kim, H.; Oh, S.H.; Jang, W.I.; Lee, S.B.; Park, M.; Kim, S.; Park, S.; Shim, S.; Jang, H. Combined Administration of Pravastatin and Metformin Attenuates Acute Radiation-Induced Intestinal Injury in Mouse and Minipig Models. Int. J. Mol. Sci. 2022, 23, 14827. https://doi.org/10.3390/ijms232314827
Kim JM, Kim H, Oh SH, Jang WI, Lee SB, Park M, Kim S, Park S, Shim S, Jang H. Combined Administration of Pravastatin and Metformin Attenuates Acute Radiation-Induced Intestinal Injury in Mouse and Minipig Models. International Journal of Molecular Sciences. 2022; 23(23):14827. https://doi.org/10.3390/ijms232314827
Chicago/Turabian StyleKim, Jung Moon, Hyewon Kim, Su Hyun Oh, Won Il Jang, Seung Bum Lee, Mineon Park, Soyeon Kim, Sunhoo Park, Sehwan Shim, and Hyosun Jang. 2022. "Combined Administration of Pravastatin and Metformin Attenuates Acute Radiation-Induced Intestinal Injury in Mouse and Minipig Models" International Journal of Molecular Sciences 23, no. 23: 14827. https://doi.org/10.3390/ijms232314827
APA StyleKim, J. M., Kim, H., Oh, S. H., Jang, W. I., Lee, S. B., Park, M., Kim, S., Park, S., Shim, S., & Jang, H. (2022). Combined Administration of Pravastatin and Metformin Attenuates Acute Radiation-Induced Intestinal Injury in Mouse and Minipig Models. International Journal of Molecular Sciences, 23(23), 14827. https://doi.org/10.3390/ijms232314827





