The Potential of Using an Autogenous Tendon Graft by Injecting Bone Marrow Aspirate in a Rabbit Meniscectomy Model
Abstract
1. Introduction
2. Results
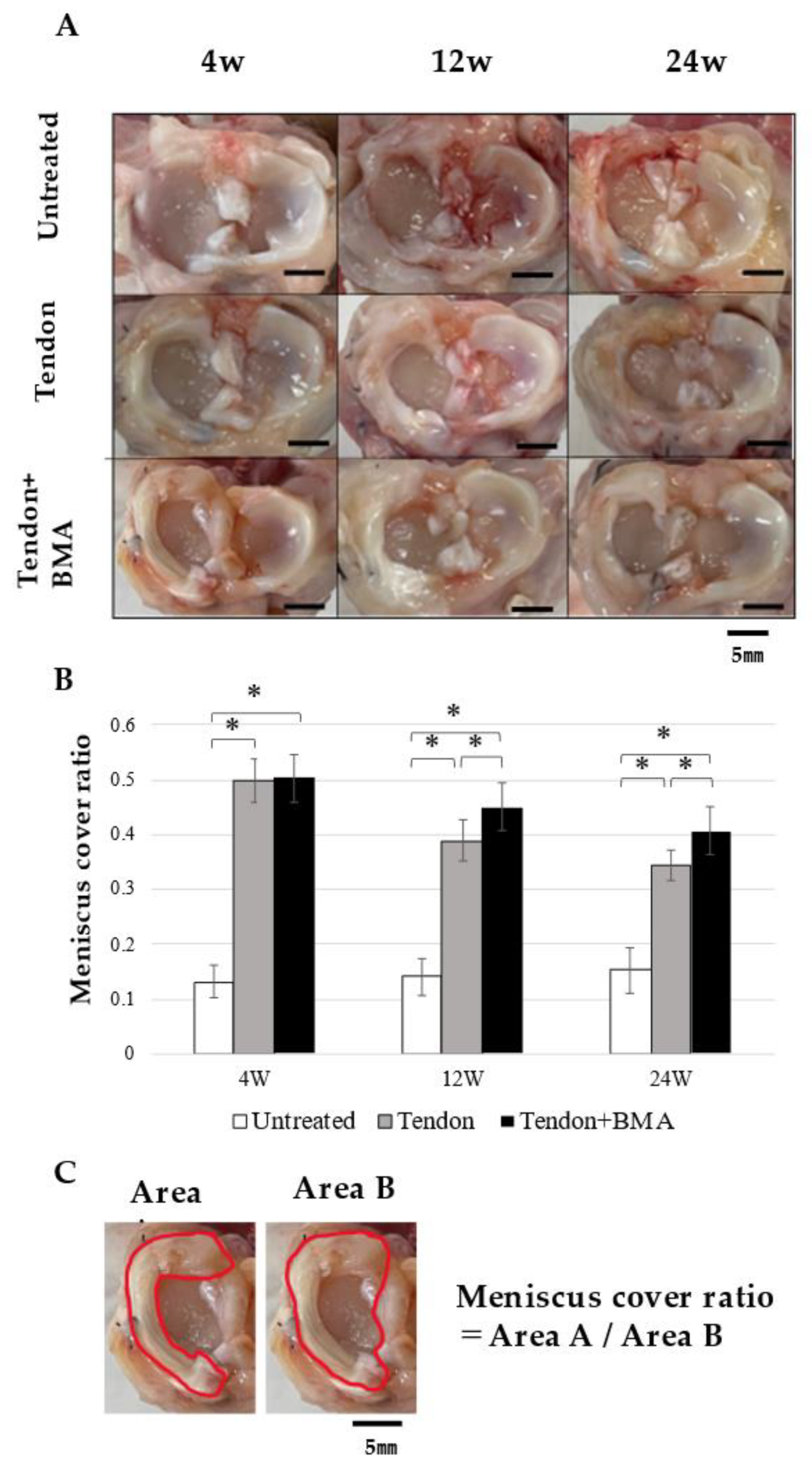
2.1. Macroscopic Observation
2.2. Radiology of the Tendon Grafts
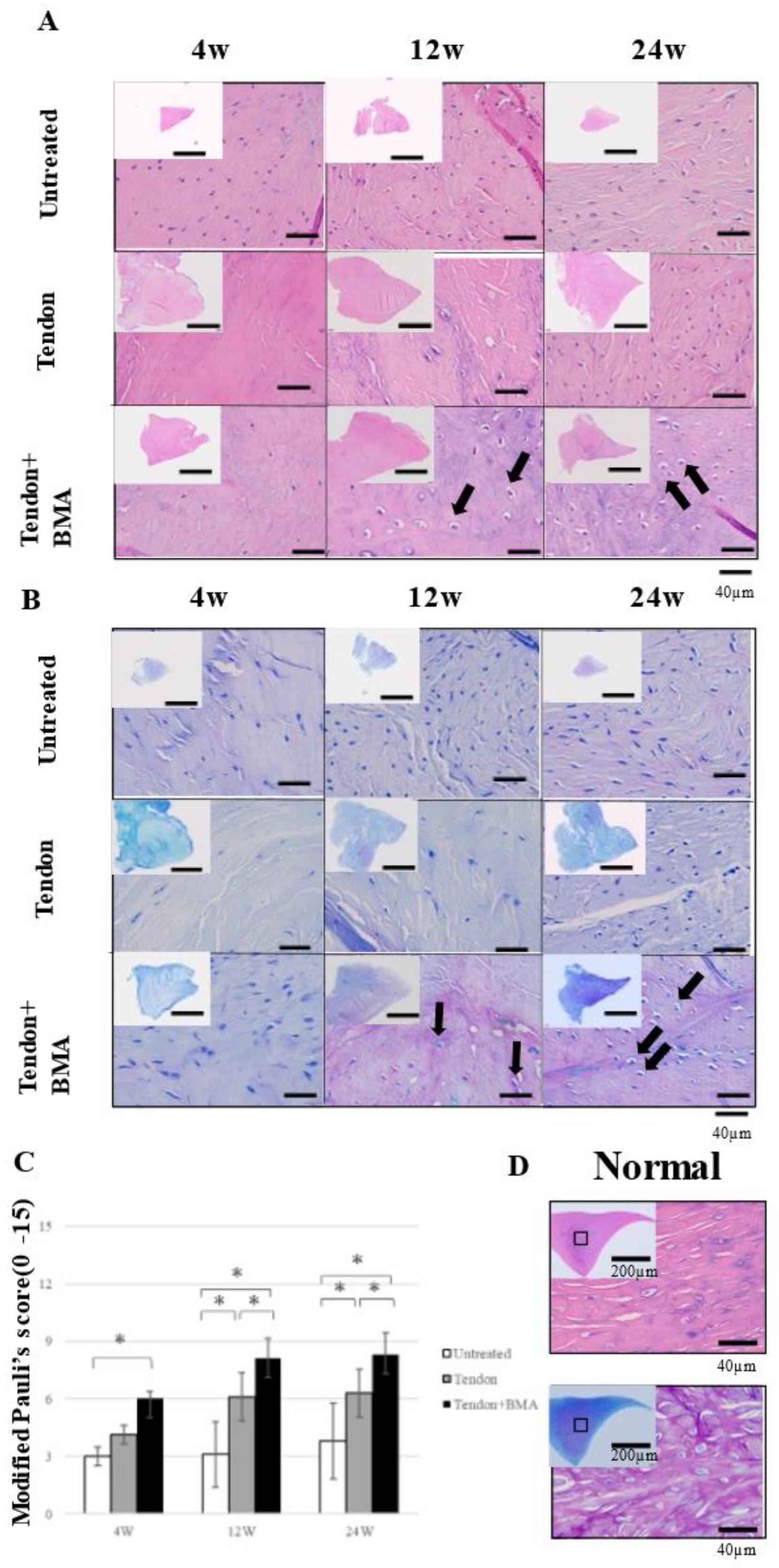
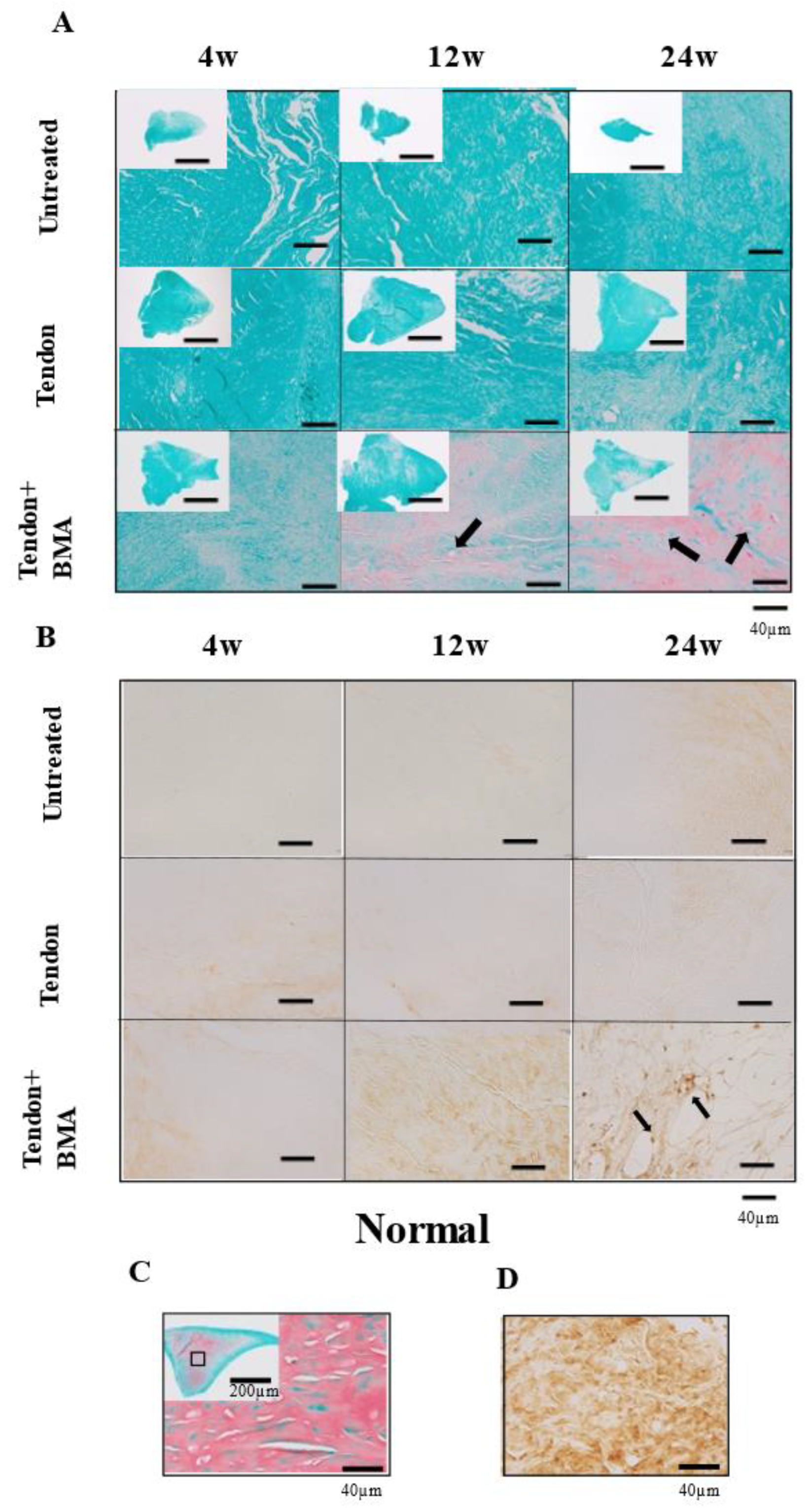
2.3. Histology and Immunohistochemical Analyses of the Tendon Grafts
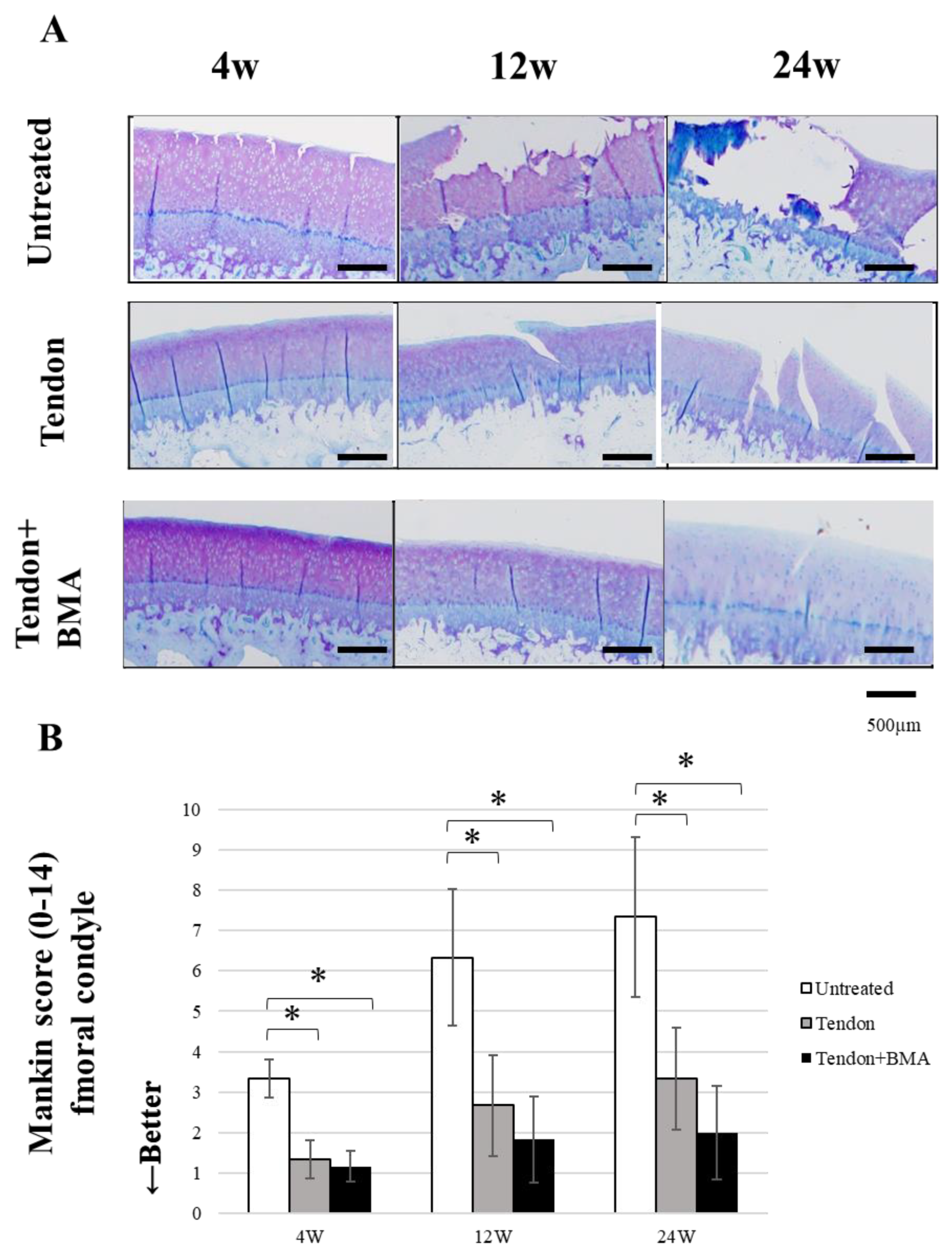
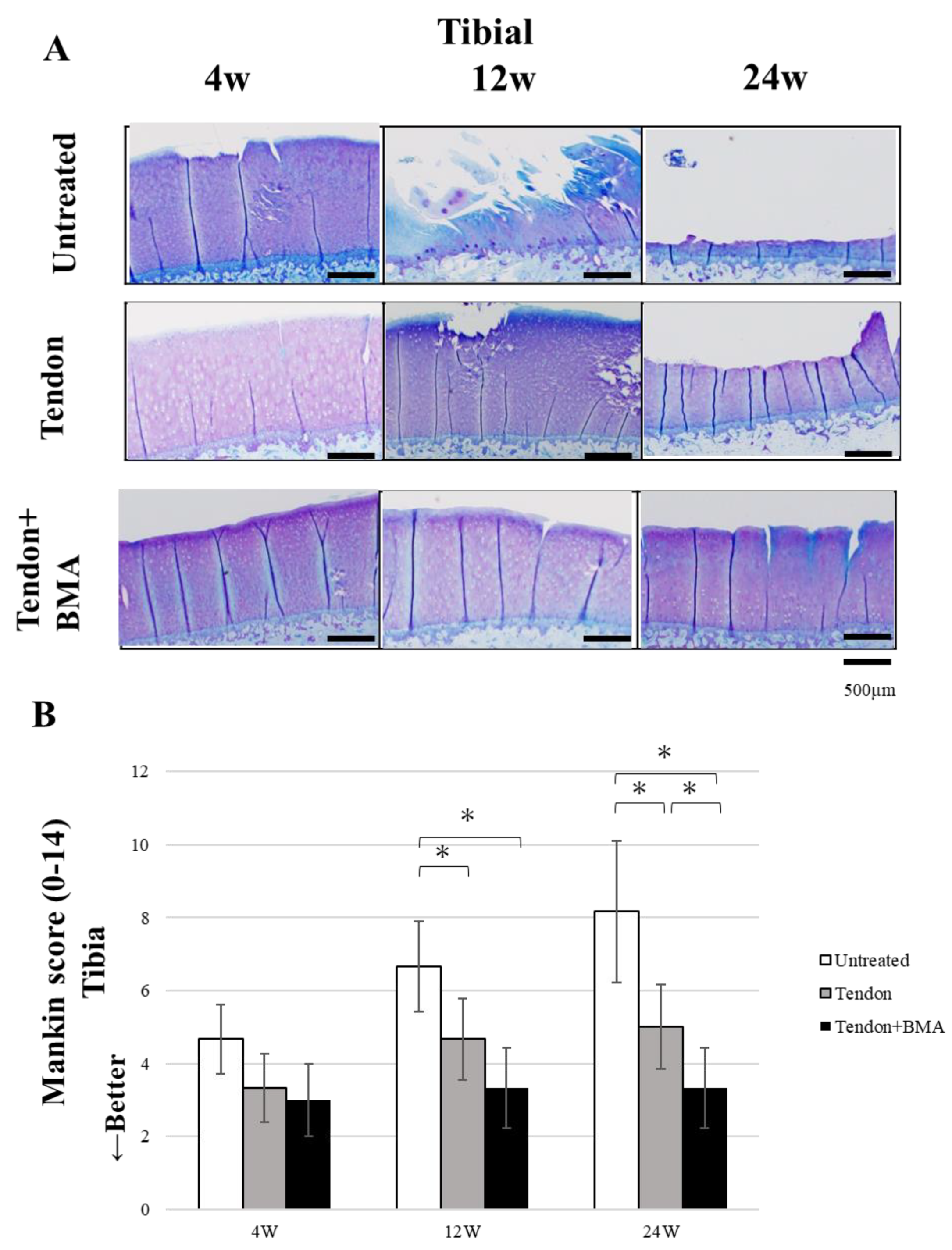
2.4. Evaluation of the Chondroprotective Effect of Meniscus Reconstruction
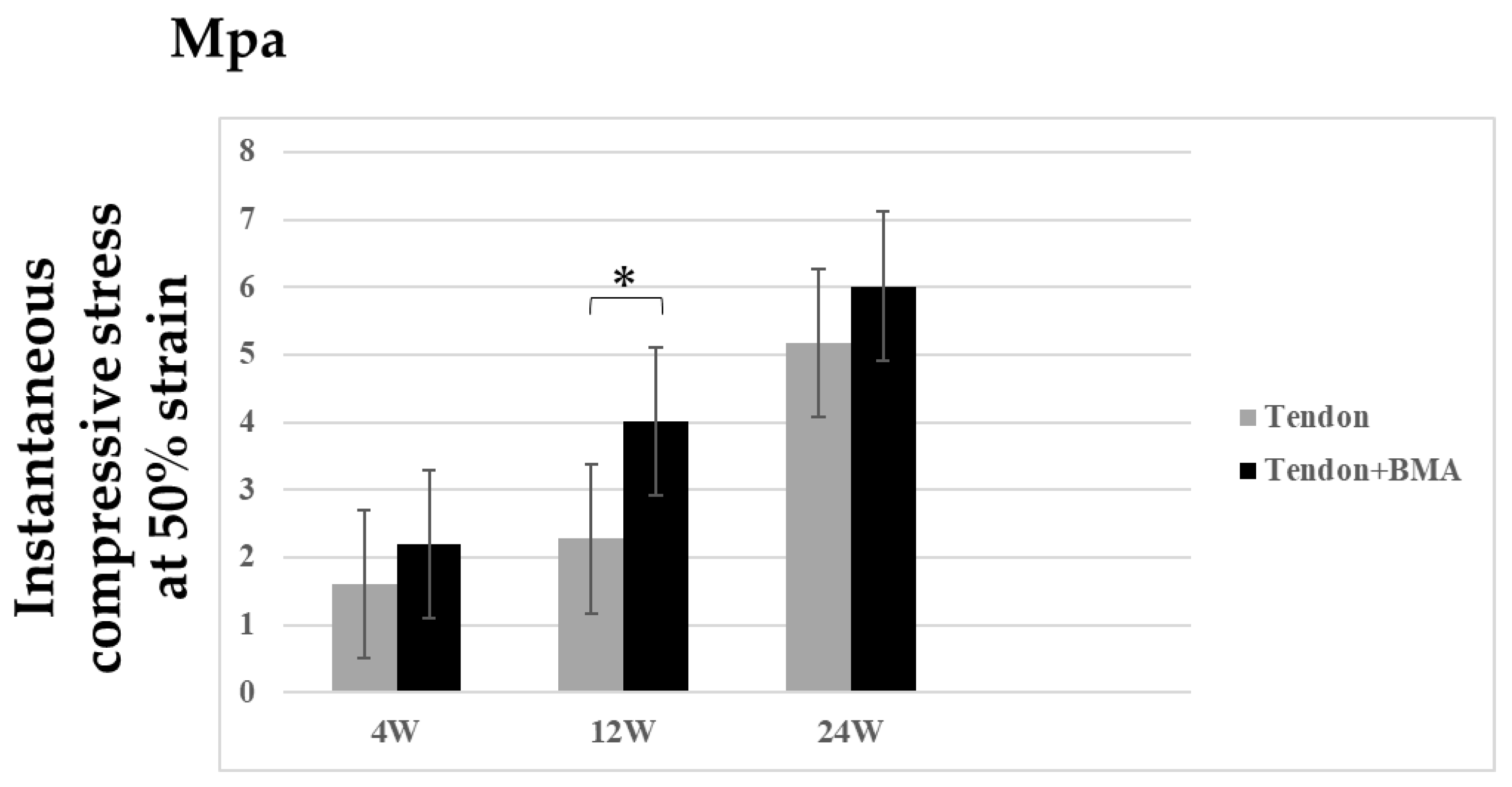
2.5. Biomechanical Testing
3. Discussion
Limitations
4. Materials and Methods
4.1. Animals
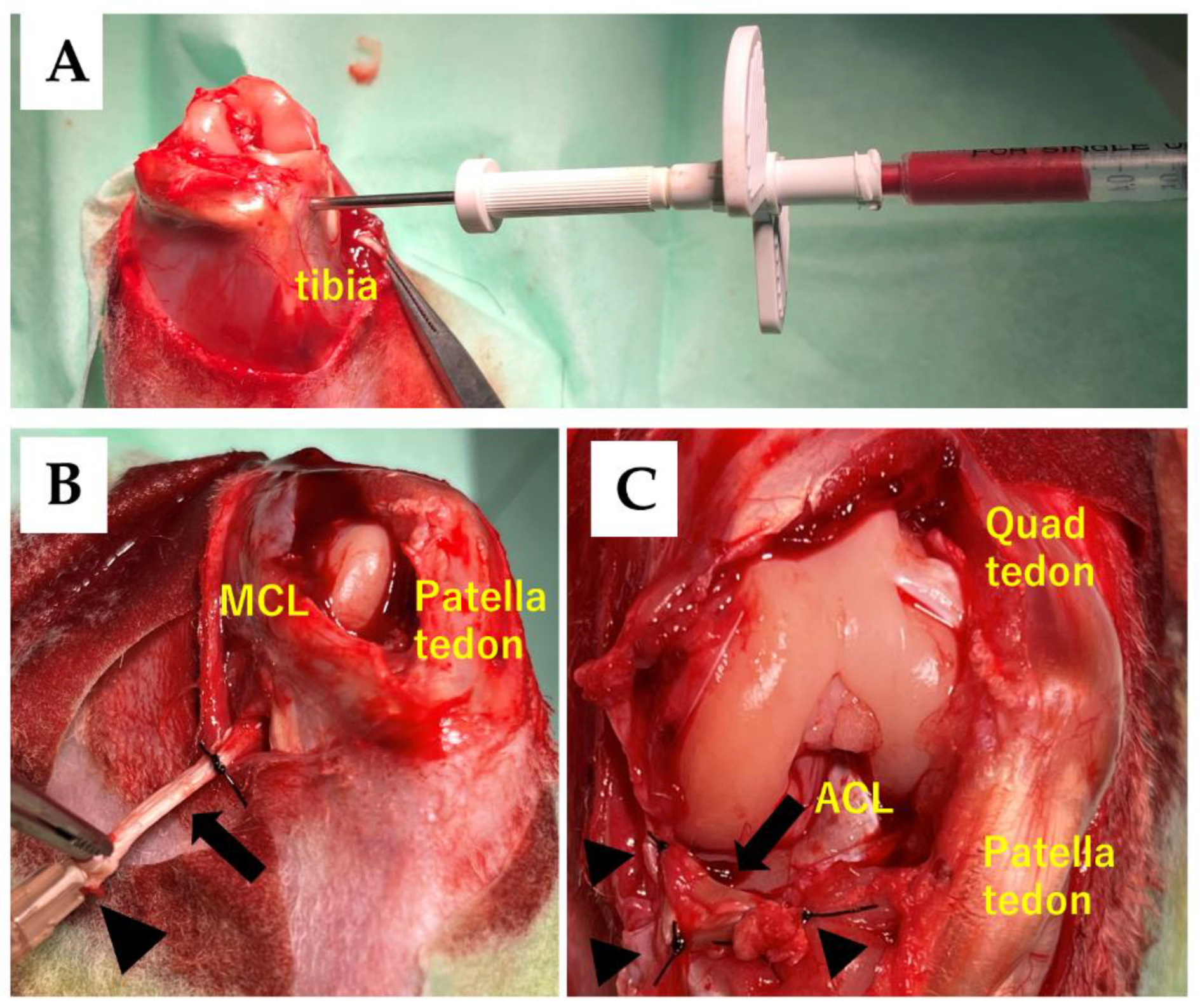
4.2. Surgical Procedure of the Meniscus Reconstruction with an Autogenous Tendon Graft
4.3. Study Design
4.4. Macroscopic Observation
4.5. Radiological Examination
4.6. Histological Evaluation
4.7. Immunohistochemical Examination
4.8. Biomechanical Analyses
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Greis, P.E.; Bardana, D.D.; Holmstrom, M.C.; Burks, R.T. Meniscal injury: I. Basic science and evaluation. J. Am. Acad. Orthop. Surg. 2002, 10, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Englund, M. The role of biomechanics in the initiation and progression of OA of the knee. Best Pract. Res. Clin. Rheumatol. 2010, 24, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Garrett, W.E., Jr.; Swiontkowski, M.F.; Weinstein, J.N. American Board of Orthopaedic Surgery Practice of theOrthopaedic Surgeon: Part-II, certification examination case mix. J. Bone Jt. Surg. 2006, 88, 660–667. [Google Scholar] [CrossRef]
- Andersson-Molina, H.; Karlsson, H.; Rockborn, P. Arthroscopic partial and total meniscectomy: A long-term follow-up study with matched controls. Arthroscopy 2002, 18, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, I.D.; Moran, C.J.; Potter, H.G.; Warren, R.F.; Rodeo, S.A. Restoration of the meniscus: Form and function. Am. J. Sport. Med. 2014, 42, 987–998. [Google Scholar] [CrossRef]
- Cook, J.L.; Fox, D.B.; Malaviya, P.; Tomlinson, J.; Farr, J.; Kuroki, K.; Cook, C. Evaluation of small intestinal submucosa grafts for meniscal regeneration in a clinically relevant posterior meniscectomy model in dogs. J. Knee Surg. 2006, 19, 159–167. [Google Scholar] [CrossRef]
- Gastel, J.A.; Muirhead, W.R.; Lifrak, J.T.; Fadale, P.D.; Hulstyn, M.J.; Labrador, D.P. Meniscal tissue regeneration using a collagenous biomaterial derived from porcine small intestine submucosa. Arthroscopy 2001, 17, 151–159. [Google Scholar] [CrossRef]
- Lubowitz, J.H.; Verdonk, P.C.M.; Reid, J.B.; Verdonk, R. Meniscus allograft transplantation: A current concepts review. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 476–492. [Google Scholar] [CrossRef]
- Kohn, D. Autograft meniscus replacement: Experimental and clinical results. Knee Surg. Sports Traumatol. Arthrosc. 1993, 1, 123–125. [Google Scholar] [CrossRef]
- Ozeki, N.; Muneta, T.; Matsuta, S.; Koga, H.; Nakagawa, Y.; Mizuno, M.; Tsuji, K.; Mabuchi, Y.; Akazawa, C.; Kobayashi, E.; et al. Synovial mesenchymal stem cells promote meniscus regeneration augmented by an autologous achilles tendon graft in a rat partial meniscus defect model. Stem Cells 2015, 33, 1927–1938. [Google Scholar] [CrossRef]
- Johnson, L.L.; Feagin, J.A. Autogenous tendon graft substitution for absent knee joint meniscus: A pilot study. Arthroscopy 2000, 16, 191–196. [Google Scholar] [CrossRef]
- Veronesi, F.; Salamanna, F.; Tschon, M.; Maglio, M.; Nicoli Aldini, N.; Fini, M. Mesenchymal stem cells for tendon healing: What is on the horizon. J. Tissue Eng. Regen. Med. 2017, 11, 3202–3219. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Idrees, E.; Andrews, S.H.J.; Labib, K.; Szojka, A.; Kunze, M.; Burbank, A.D.; Mulet-Sierra, A.; Jomha, N.M.; Adesida, A.B. Plasticity of Human Meniscus Fibrochondrocytes: A Study on Effects of Mitotic Divisions and Oxygen Tension. Sci. Rep. 2017, 7, 12148. [Google Scholar] [CrossRef]
- Hashimoto, Y.; Nishino, K.; Orita, K.; Yamasaki, S.; Nishida, Y.; Kinoshita, T.; Nakamura, H. Biochemical Characteristics and Clinical Result of Bone Marrow–Derived Fibrin Clot for Repair of Isolated Meniscal Injury in the Avascular Zone. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 38, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Brittberg, M.; Winalski, C.S. Evaluation of cartilage injuries and repair. J. Bone Jt. Surg. 2003, 85 (Suppl. S1), 58–69. [Google Scholar] [CrossRef] [PubMed]
- Hatsushika, D.; Muneta, T.; Horie, M.; Koga, H.; Tsuji, K.; Sekiya, I. Intraarticular injection of synovial stem cells promotes meniscal regeneration in a rabbit massive meniscal defect model. J. Orthop. Res. 2013, 31, 1354–1359. [Google Scholar] [CrossRef]
- Moriguchi, Y.; Tateishi, K.; Ando, W.; Shimomura, K.; Yonetani, Y.; Tanaka, Y.; Kita, K.; Hart, D.A.; Gobbi, A.; Shino, K.; et al. Repair of meniscal lesions using a scaffold-free tissue-engineered construct derived from allogenic synovial MSCs in a miniature swine model. Biomaterials 2013, 34, 2185–2193. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.; Chen, J.; Zhu, T.; Chen, L.; Zhang, W.; Fang, Z.; Heng, B.C.; Yin, Z.; Chen, X.; Ji, J.; et al. Intra-Articular Injection of Human Meniscus Stem/Progenitor Cells Promotes Meniscus Regeneration and Ameliorates Osteoarthritis Through Stromal Cell-Derived Factor-1/CXCR4-Mediated Homing. Stem Cells Transl. Med. 2014, 3, 387–394. [Google Scholar] [CrossRef]
- Fortier, L.A.; Potter, H.G.; Rickey, E.J.; Schnabel, L.V.; Foo, L.F.; Chong, L.R.; Stokol, T.; Cheetham, J.; Nixon, A.J. Concentrated bone marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. J. Bone Jt. Surg. 2010, 92, 1927–1937. [Google Scholar] [CrossRef]
- Connolly, J.F. Injectable bone marrow preparations to stimulate osteogenic repair. Clin. Orthop. Relat. Res. 1995, 313, 8–18. [Google Scholar]
- Patel, J.M.; Ghodbane, S.A.; Brzezinski, A.; Gatt, C.J.; Dunn, M.G. Tissue-Engineered Total Meniscus Replacement with a Fiber-Reinforced Scaffold in a 2-Year Ovine Model. Am. J. Sports Med. 2018, 46, 1844–1856. [Google Scholar] [CrossRef]
- Otsuki, S.; Nakagawa, K.; Murakami, T.; Sezaki, S.; Sato, H.; Suzuki, M.; Okuno, N.; Wakama, H.; Kaihatsu, K.; Neo, M. Evaluation of Meniscal Regeneration in a Mini Pig Model Treated with a Novel Polyglycolic Acid Meniscal Scaffold. Am. J. Sports Med. 2019, 47, 1804–1815. [Google Scholar] [CrossRef] [PubMed]
- Hannink, G.; van Tienen, T.G.; Schouten, A.J.; Buma, P. Changes in articular cartilage after meniscectomy and meniscus replacement using a biodegradable porous polymer implant. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Chevrier, A.; Nelea, M.; Hurtig, M.B.; Hoemann, C.D.; Buschmann, M.D. Meniscus Structure in Human, Sheep, and Rabbit for Animal Models of Meniscus Repair. J. Orthop. Res. 2009, 27, 1197–1203. [Google Scholar] [CrossRef]
- Naka, Y.; Hashimoto, Y.; Nakamura, H.; Takaoka, K. Repair of a meniscus defect through cartilaginous metaplasia of the autogenous tendon graft by injecting recombinant human bone morphogenetic protein-2. J. Musculoskelet. Res. 2011, 14, 1–4. [Google Scholar] [CrossRef]
- Nishida, Y.; Hashimoto, Y.; Orita, K.; Nishino, K.; Kinoshita, T.; Nakamura, H. Intra-articular injection of stromal cell-derived factor 1α promotes meniscal healing via macrophage and mesenchymal stem cell accumulation in a rat meniscal defect model. Int. J. Mol. Sci. 2020, 21, 5454. [Google Scholar] [CrossRef]
- Pauli, C.; Grogan, S.; Patil, S.; Akihiko, S.; Koziol, J.; Lotz, M.; D’Lima, D. 438 Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthr. Cartil. 2011, 19, S202. [Google Scholar] [CrossRef][Green Version]
- Mankin, H.J.; Dorfman, H.; Lippiello, L.; Zarins, A. From the Departments of Orthopaedics. J. Bone Jt. Surg. 1971, 53-A, 523–537. [Google Scholar] [CrossRef]
- Baek, J.; Sovani, S.; Glembotski, N.E.; Du, J.; Jin, S.; Grogan, S.P.; D’Lima, D.D. Repair of Avascular Meniscus Tears with Electrospun Collagen Scaffolds Seeded with Human Cells. Tissue Eng.-Part A 2016, 22, 436–448. [Google Scholar] [CrossRef]


| 4 Weeks | 12 Weeks | 24 Weeks | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Scores | p Value | Scores | p Value | Scores | p Value | ||||
| Untreated group | 0.83 ± 0.37 | 0.54 0.69 | 0.16 | 1.83 ± 0.37 | 0.04 0.21 | 0.11 | 2.0 ± 0.57 | 0.03 0.04 | 0.01 |
| Tendon group | 0.5 ± 0.5 | 1.0 ± 0.58 | 1.16 ± 0.37 | ||||||
| Tendon + BMA group | 0.33 ± 0.47 | 0.33 ± 0.47 | 0.5 ± 0.5 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iida, K.; Hashimoto, Y.; Orita, K.; Nishino, K.; Kinoshita, T.; Nakamura, H. The Potential of Using an Autogenous Tendon Graft by Injecting Bone Marrow Aspirate in a Rabbit Meniscectomy Model. Int. J. Mol. Sci. 2022, 23, 12458. https://doi.org/10.3390/ijms232012458
Iida K, Hashimoto Y, Orita K, Nishino K, Kinoshita T, Nakamura H. The Potential of Using an Autogenous Tendon Graft by Injecting Bone Marrow Aspirate in a Rabbit Meniscectomy Model. International Journal of Molecular Sciences. 2022; 23(20):12458. https://doi.org/10.3390/ijms232012458
Chicago/Turabian StyleIida, Ken, Yusuke Hashimoto, Kumi Orita, Kazuya Nishino, Takuya Kinoshita, and Hiroaki Nakamura. 2022. "The Potential of Using an Autogenous Tendon Graft by Injecting Bone Marrow Aspirate in a Rabbit Meniscectomy Model" International Journal of Molecular Sciences 23, no. 20: 12458. https://doi.org/10.3390/ijms232012458
APA StyleIida, K., Hashimoto, Y., Orita, K., Nishino, K., Kinoshita, T., & Nakamura, H. (2022). The Potential of Using an Autogenous Tendon Graft by Injecting Bone Marrow Aspirate in a Rabbit Meniscectomy Model. International Journal of Molecular Sciences, 23(20), 12458. https://doi.org/10.3390/ijms232012458





