Abstract
One of the most serious complications following the implantation of orthopedic biomaterials is the development of infection. Orthopedic implant-related infections do not only entail clinical problems and patient suffering, but also cause a burden on healthcare care systems. Additionally, the ageing of the world population, in particular in developed countries, has led to an increase in the population above 60 years. This is a significantly vulnerable population segment insofar as biomaterials use is concerned. Implanted materials are highly susceptible to bacterial and fungal colonization and the consequent infection. These microorganisms are often opportunistic, taking advantage of the weakening of the body defenses at the implant surface–tissue interface to attach to tissues or implant surfaces, instigating biofilm formation and subsequent development of infection. The establishment of biofilm leads to tissue destruction, systemic dissemination of the pathogen, and dysfunction of the implant/bone joint, leading to implant failure. Moreover, the contaminated implant can be a reservoir for infection of the surrounding tissue where microorganisms are protected. Therefore, the biofilm increases the pathogenesis of infection since that structure offers protection against host defenses and antimicrobial therapies. Additionally, the rapid emergence of bacterial strains resistant to antibiotics prompted the development of new alternative approaches to prevent and control implant-related infections. Several concepts and approaches have been developed to obtain biomaterials endowed with anti-infective properties. In this review, several anti-infective strategies based on biomaterial engineering are described and discussed in terms of design and fabrication, mechanisms of action, benefits, and drawbacks for preventing and treating orthopaedic biomaterials-related infections.
1. Introduction
In orthopedic surgery and traumatology, bone grafting is one of the most frequently performed surgical procedures used for bone-loss repair and bone augmentation [1]. However, prosthetic joints and other orthopedic implant devices (such as pins, screws, plates, and external fixators), required in situations such as osteomyelitis post-debridement, are extremely sensitive to contamination by microorganisms and the subsequent development of infection [2,3].
Orthopedic implant-related infections are among the main reasons for joint arthroplasty and osteosynthesis failure, with severe and devastating outcomes for patients and health systems. Their treatment requires in most cases, the infected implant removal, implant replacement, revision surgeries, or/and amputation, which translates to high rates of morbidity, and increased risk of mortality [4]. In addition to causing significant physical and emotional suffering, implant infections are a massive economic burden to the health systems, estimated to cost more than $8.6 billion annually in the United States and €2 billion in Europe [4,5]. The implant-related infection rate varies according to the type of bone involved (e.g., hip, knee, ankle, or tibia), grade/type of fracture (i.e., closed or open), or type of surgery (i.e., primary or revision) [6,7,8]. For instance, the likelihood of infection following the implantation of a prosthetic hip is 0.3–2.4%, while a total knee replacement is 1–3% [8]. In closed fractures, the incidence of infection after internal fixation is generally low (0.5–2%) when compared to open fractures, wherein the infection rate may exceed 30% [6,7,8]. In revision surgeries concerning implant removal, amputation, or tissue debridement, the risk of infection is higher when compared to primary ones. For instance, the infection rate following total hip arthroplasties is 14.8%, while for total knee revision it is 25.2% [9].
The Centers for Disease Control (CDC) classified biofilms as one of the most pressing clinical obstacles of the century, since they contribute to more than 80% of human bacterial infections [10,11,12]. Biofilms act as communities of microbial cells attached to an inert or living surface that are functionally organized and enclosed in a self-produced polymeric matrix (EPSs), thus contributing to the increasing infection pathogenicity [13].
Over the past 20 years, a wide range of different bioengineering approaches for the treatment of orthopedic implant-related infections has been investigated both in vitro and in vivo with promising results [14,15,16,17,18,19]. However, their implementation in orthopedics is still at an early stage. The present review has as its major goal to revisit the main anti-infective strategies based on biomaterial engineering to overcome orthopedic implant-related infections.
2. Implant-Infecting Microorganisms
Implanted materials are highly susceptible to bacterial and fungal colonization and consequent infection [20]. These microorganisms are frequently opportunistic, taking advantage of the weakening of the body defenses at the implant surface–tissue interface, thereby attaching to tissues or implant surfaces, instigating biofilm formation and subsequent development of infection [13,21]. The development of biofilm causes tissue destruction, systemic dissemination of the pathogen and dysfunction of the implant/bone interface, resulting in the failure of implanted material [13,21]. Additionally, the contaminated implant may serve as a reservoir for an infection of the surrounding tissue, where microorganisms may reside intracellularly [13,21].
In Europe and U.S, the most prevalent microorganisms in implant-related infections are Gram-positive bacteria, mainly Staphylococcus aureus (33–43%) and Staphylococcus epidermidis (17–21%) [13,22], as reflected in Table 1. Other Gram-positive bacteria, such as Streptococcus viridans and Enterococcus spp. (mainly Enterococcus faecalis), are encountered in 1–10% and 3–7% of infections, respectively [13,22,23]. Gram-negative organisms, including Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumonia, Proteus mirabilis and Proteus vulgaris are less frequent than Gram-positive, causing around 6% of cases [24]. Anaerobic bacteria (including Propionibacterium acnes) and fungi (mainly Candida albicans) are also involved on implant-related infections (2–3%) [13,24]. Polymicrobial infections are reported in about 10–11% of the cases; the majority are caused by two bacterial species such as methicillin-resistant S. aureus (MRSA) and Klebsiella spp. [24,25]. It should be noted that bacteria isolation and identification always depend on the quality of the diagnostic procedure and preceding antimicrobial therapy [24].

Table 1.
Prevalence of implant-infecting bacteria in Europe and the U.S. according to the implant type and site.
In the literature, three types of biomaterials-associated infections are reported: (i) exogenous infection that occurs during or immediately after surgery through direct inoculation into the surgical site; (ii) contiguous infections acquired from spread from an adjacent infectious focus, and (iii) hematogenous infections provided from the distant focus of infection, such as blood or lymph. Concerning the time since surgery and the onset of the infection, these infections can be classified into: (i) early infections (less than three months after the surgery); (ii) delayed infections (between three to 24 months after surgery), and (iii) late infections (more than 24 months after surgery) [29]. Early and delayed infections are commonly caused by trauma or contamination during surgery. S. aureus, Enterococcus spp., and Gram-negative bacilli, intrinsically virulent microorganisms, are usually the pathogenic agents related to early infections [13,29]. Coagulase-negative Staphylococci and P. acnes, low-virulent microorganisms, are usually pathogenic agents of delayed infections. Late infections are usually acquired by hematogenous spread, having a considerable range of pathogenic agents originating from the skin, respiratory, dental, or urinary tract infections [13,29,30,31,32].
Methicillin-resistant S. aureus (MRSA), Vancomycin-resistant S. aureus (VRSA), Methicillin-resistant S. epidermidis (MRSE), Vancomycin-resistant Enterococcus (VRE) and extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBLs) are examples of antibiotic-resistant bacteria that have been commonly linked to implant-related infections, which are a huge threat to human health since they limit therapeutic options to adopt [33,34,35]. In addition, these bacteria are producers of virulence factors (e.g., catalase, hyaluronidase, collagenase, toxins) that play an important role in the degree of severity of the infection, once they promote bacterial adherence to the bone and implant and severe tissue damage [13,21].
3. Pathogenesis of Implant-Related Infections
Biofilm formation consists in the irreversible attachment and growth of microorganisms onto surfaces with the concomitant production of the extracellular polymer matrix (EPSs), which alters the microorganism’s phenotypic, growth rate and gene transcription. Biofilms are three-dimensional complex structures that confer significant survival advantages to microorganism communities, which can lead to the recurrence of biofilm-related implant infection. This is a huge concern in the orthopedic field, especially since these communities are highly resilient to host immunity and to conventional anti-microbial therapies [24,36,37,38,39,40,41,42].
Independent-of-the-infection mechanism biofilm formation has four steps (Figure 1): (1) initial adhesion; (2) irreversible adhesion and cell–cell adhesion; (3) proliferation; (4) growth and maturation, and (5) detachment [20,40].
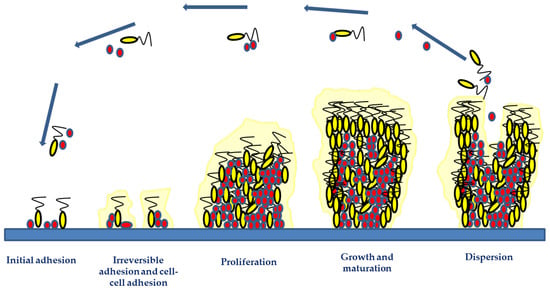
Figure 1.
Biofilm development phases include initial adhesion, irreversible adhesion and cell–cell adhesion, proliferation, growth and maturation, and detachment. The two initial phases involve the attachment of microorganisms via hydrophobic or electrostatic interactions to implant surfaces and their involvement in cell-to-cell bindings. The microorganism growth and accumulation during the proliferation and maturation phases result in the development of a mature biofilm structure. Adhesive and disruptive processes occur during the biofilm maturation phase. The final stage of biofilm formation is the detachment phase, involving microbial dispersal and dissemination, which may lead to new infection foci.
The initial microbial attachment consists of the adhesion of planktonic cells to the implant surfaces or the host through hydrophobic or electrostatic interactions between bacteria and surfaces, mediated by: physical shear forces (e.g., van der Waal, steric interactions, and electrostatic forces); microbial appendages (e.g., pili, flagella, or fimbriae), and adhesion surface proteins (e.g., fibronectin, fibrinogen, vitronectin, thrombospondin, laminin, collagen, von Willebrand factor, and polysaccharides) [20,36,40,43]. Twenty surface-associated adhesins are involved in Staphylococcal biofilm formation. These adhesins mediate initial biofilm attachment and intercellular adhesion during maturation-enhancing cohesion. Autolysins (like At1E) mediated the adhesion of S. epidermidis to polymeric surfaces, whereas fibronectin-binding proteins, e.g., FnBPA and FnBPB, induce S. aureus invasion into epithelial cells, endothelial cells, and keratinocytes [20,36,40,42,43].
Biofilm maturation consists of microbial proliferation and aggregation, macro- and microcolonies formation, intercellular signaling and quorum sensing (QS). These are mechanisms that induce the expression of specific genes and proteins involved in biofilm structure, virulence and regulation processes [44]. During biofilm maturation, the microbial cells start the secretion of the EPSs and eDNA, that besides stabilizing the biofilm network into the implant surface, are responsible for linkage between clusters, cell-to-cell cohesion, and cellular communication [44]. The main polysaccharide of S. epidermidis biofilm matrix is polysaccharide intercellular adhesin (PIA), which aids staphylococci in colonizing biomaterial surfaces and protects the proliferating bacteria from polymorphonuclear leukocytes [45]. The microbial microcolonies encased within the EPS communicate between neighboring cells through the QS phenomenon, which controls several physiological processes such as bioluminescence, secretion of virulence factors, biofilm formation and antibiotic resistance [44]. For instance, N-acylated homoserine lactone QS systems of P. aeruginosa are responsible for eDNA release and for biofilm structure [46]. The S. aureus small peptide named AIP QS activates the agrA gene, which regulates the transcription of genes that code for proteases involved in biofilm dispersal [47].
As the biofilm matures, there is an increase in stress-inducing conditions, toxic product accumulation, and limited nutrient availability. These phenomena take the microbial cells to disperse them to other regions of the host’s body or other regions of the medical implant [13,44]. This constitutes the biofilm dispersal phase, where microbial cells (either single cells or clumps of cells) are sloughed off the biofilm. Biofilm dispersal can lead to the dissemination of the detaching microorganisms, which can cause chronic infections, or even reach the bloodstream and cause systemic infections [13,44]. Inhibition of matrix production, enzymatic degradation of EPSs, and surfactant molecules are the mechanisms that contribute to biofilm dispersal. In staphylococci, extracellular enzymes (e.g., staphopain cysteine proteases, the V8 glutamyl endopeptidase SspA and staphylococcal nuclease) and Phenol Soluble Modulins (PSMs) have an essential role in the dispersive phase, particularly in implant-associated biofilm infections. This is because these enzymes are able to degrade the biofilm matrix, contributing to the bacterial dispersal and dissemination of biofilm clusters to distal sites [13,44].
Therefore, developing biomaterials that can prevent bacterial adhesion and/or biofilm formation at the implantation site could be an important breakthrough in bone disease treatments.
4. Bioengineering Materials as Therapeutic Approaches
The design and fabrication of new antimicrobial approaches based on bioengineering materials remains an important research line in the orthopedic field, given the impact of implanted-related infections on the quality of life of patients and health systems [48].
Various concepts and approaches have been developed to obtain bioengineered materials with anti-infective properties (Figure 2), i.e., capable of preventing microbial adhesion and colonization of bone tissue and implant surfaces, as well as creating a bacteria-free environment around the implant [49,50]. Biomaterials endowed with anti-infective properties need to be tailored according to the specific application. According to their strategy, anti-infective biomaterials can be classified into two main groups: passive surfaces and active surfaces [49,50].
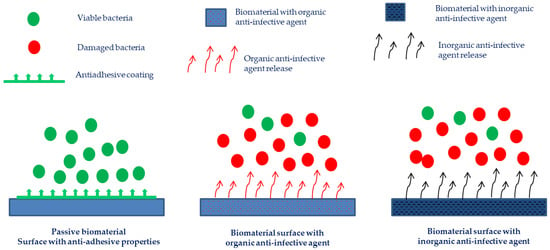
Figure 2.
Different strategies have been developed to trigger anti-infective activity in biomaterials.
Passive (anti-adhesive) surfaces are those presenting chemistry and/or structure modifications that aim at preventing or reducing bacterial adhesion, without releasing bactericidal agents into the surrounding tissues. Active surfaces have in their composition pre-coated antimicrobial agents such as organic substances (antibiotics and anti-infective peptides, bacteriophages), metals or metal ions (silver, zinc, copper, among others), and/or their combinations, that may inhibit microbial colonization and biofilm formation. The coatings may simply act by delivering high local concentrations of one or more pre-loaded antimicrobials, or they may have a direct or synergistic antimicrobial activity [49,50,51,52,53].
The following sections describe several developed strategies based on biomaterial engineering to fight orthopedic implant-related infections.
4.1. Anti-Adhesive Biomaterials
The physicochemical characteristics of the materials integrating the implant surface have a significant impact on microbial adherence. Therefore, material surface chemical composition, surface charge density, surface energy, wettability (hydrophobicity and hydrophilicity), and surface topography may substantially change the implant susceptibility to microbial adhesion and colonization [49,50].
The principle of an anti-adhesive surface development is based on five physical-chemical mechanisms: steric repulsion, electrostatic repulsion, low surface energy, superhydrophobic and hydrophobic interactions, and substrate–microorganism physical interaction [47,53,54,55,56].
Regarding chemical modification, a variety of polymers can be used to create antifouling surfaces, such as poly(ethylene glycol) (PEG), poly-zwitterionic polymers (e.g., poly(2-methacryloyloxyethyl phosphorylcholine), low-energy polymers (e.g., fluoropolymers) and polymers-based hydrogels (e.g., chitosan), as detailed below [54,56,57,58].
PEG is the most employed antifouling polymer for coating implant materials, due to its ability, in an aqueous environment, to form a layer of tightly bound water molecules that act as a physical barrier (steric repulsion) against the attachment of proteins and microorganisms [54,56,57,58]. Francolini et al. produced polyethylene glycol (PEG)-grafted segmented polyurethanes capable of preventing the adhesion of S. epidermidis onto their surfaces. Their anti-adhesive property results from the exposure of PEG chains at the material/water interface, enhancing the material bulk and surface hydrophilicity, and consequently the repulsion interactions [58,59].
Due to their higher in vivo stability, poly-zwitterionic materials (highly hydrophilic antifouling polymers) have been used as substitutes for PEG-based antifouling biomaterials [56]. The antifouling properties of poly-zwitterion materials are due to the positive and negative groups incorporated into their structure, as well as the formation of a hydration layer that acts as a physical barrier to avoid protein and bacterial adhesion [56,60,61].
Hydrogels are three-dimensional (3D) porous, highly water-absorbent polymeric networks that can be crosslinked physically or chemically. Hydrogels can be obtained from natural (e.g., chitosan and gelatin) or synthetic polymers (e.g., poly(vinyl alcohol) and poly(sulphobetaine)) [56,58,59,62]. This biomaterial is frequently used in tissue engineering, drug administration, contact lenses, wound dressings, and implantable devices, due to its “soft and wet” characteristics. However, the hydrogels’ poor mechanical qualities generally prevent them from being used in orthopedic implants [56,58,59,62]. Alternatively, coating a thin hydrogel layer onto the device surface is an effective way to combine the advantages of the bulk property of biomedical devices and the biological merit of hydrogels. The attachment and anchoring of hydrogels to implant surface can be performed through several reactions such as surface-initiated radical polymerization, direct photografting, click chemistry, free radical polymerization, photochemical coupling, dopamine-functionalized polymer, self-condensation of silane, and layer-by-layer coating [56,62]. Chitosan (CS) is the most frequently used natural polymer for preparing implant coatings due to its inherent tissue adhesion, antibacterial, and hemostatic properties [58,59,63]. D’Almeida et al. covalently grafted titanium alloy with chitosan through TriEthoxySilylPropylSuccinic Anhydride process to prevent post-surgical infection [63]. That study revealed that CS positively charged quaternary ammonium moieties exerted strong electrostatic interactions on the negatively charged bacterial cell surface, leading to microbial membrane disruption and bacterial death [56,63,64].
Low-surface-energy polymeric coatings (surface energy less than 36 mJ/m2 and hydrophobic performance) are considered effective non-sticking surfaces due to their chemical inertness and non-wetting properties [65,66,67]. For instance, Song et al. have shown that the fluorine components, introduced into poly(butyl methacrylate-co-ethylene dimethacrylate) films, caused low surface energy and hydrophobicity, thus preventing E. coli and S. aureus adhesion [67].
Several studies have focused on obtaining material surfaces with extreme wettability, super-hydrophobic (Ɵ > 150°) or super-hydrophilic (Ɵ < 5°), as potential anti-infective surfaces [68,69,70,71,72]. Super-hydrophobic surfaces can present bacterial repellency properties through their high surface roughness and low surface energy that create a stable or metastable air layer at the material surface (called the “lotus effect”), where debris and pathogens are removed as water contacts and subsequently rolls off the surface [68,69,70,71,72]. For instance, Naderizadeh et al. showed that the adhesion of E. coli, S. aureus, and P. aeruginosa was significantly reduced on the superhydrophobic coatings based on biomass-derived bioresin polyfurfuryl alcohol (PFA) [71]. Stallard et al. reported that superhydrophobic surfaces based on siloxane and fluorinated siloxane elastomeric coatings exhibit antimicrobial properties and significantly reduce bovine serum albumin and bovine fibrinogen adsorption [68]. On the other hand, extremely water-attractive surfaces can also exhibit anti-infective performance via their super-hydrophilicity, which is able to form a dense layer of water molecules, weakening the interaction between bacteria and substratum [68,69,70,71,72]. Choi et al. produced super-hydrophilic interfaces by layer-by-layer (LbL) assembly of the biotic materials chitosan (CHI) and rice husk ash (RHA) nanosilica with anti-adhesive properties, reducing the attachment of proteins, as well as of S. aureus and P. aeruginosa [73].
Another method to reduce bacterial adhesion to biomaterials consists of coating of the surfaces with serum, plasma, or protein solutions [74,75]. These solutions cause changes in the physicochemical properties of the biomaterial’s surfaces, interfering with bacterial adherence and host adhesins adsorption [49,66,67,74,75,76,77,78,79]. An et al., using a rabbit model, showed that albumin-coated implants presented a lower infection rate than non-coated implants [64,74,80,81,82]. This inhibition can be explained through binding to the bacterial receptors or by changing the substratum surface to a more hydrophilic behavior [74,75].
The ability of a microbial cell to remain attached to a surface reflects the nature of non-covalent interactions between the substrate and cell wall functional groups during the initial attachment phases [81]. According to attachment point theory, the biomaterial structure and morphology can be modified to produce anti-adhesive surfaces. Several patterning techniques (e.g., lithography, reactive ion etching, femtosecond laser writing, electro-chemical oxidation, electron beam evaporation, micro-contact printing, hot embossing and microfluidics) can be employed to fabricate antifouling structured surfaces [81]. These strategies can be applied whether at the micro- and/or nano-metric levels or nanometer-size combined with the micro-patterns. The antifouling phenomenon from physical modifications of material surfaces could be due to the: (i) surface roughness size (below 0.2 μm) that induces low susceptibility to bacterial attachment; (ii) micrometric and nanometric pillars, peaks and valleys of the implant surface that affect the organization of bacterial cells and their intracellular transduction signaling pathways, and (iii) changing of surface properties such as wettability [80,81,83,84]. It should be noted that the nanostructures are important parameters in the production of antifouling surfaces since effective air entrapment in the three-dimensional nanomorphology renders these surfaces superhydrophobic and slippery. For instance, Pucket et al. showed that on nano-rough titanium surfaces produced by electron beam evaporation, the amount of adhered S. aureus, S. epidermidis and P. aeruginosa was lower when compared to conventional titanium surfaces [83]. Moreover, they observed that the hydrophilicity of nano-tubular and nano-textured titanium surfaces, produced through anodizing processes, also contributed to increasing the antifouling surfaces [83].
4.2. Active Biomaterials
Active biomaterials are based on pre-coated surfaces with antimicrobial agents that can be: (i) organic compounds (e.g., antibiotics, antimicrobial peptides, QS inhibitors or bacteriophages), and (ii) inorganic compounds (mainly metal ions, e.g., silver, gold, zinc, copper, magnesium), as detailed in the sections below. These surfaces are interesting in bone implant-related infections due to their capability to kill pathogens upon contact. According to their functional principle, surfaces can be categorized as either active-releasing surfaces or contact-active surfaces. Active-releasing surfaces result from the entrapment or coating of an antimicrobial agent in the bulk or in the coating of a biomaterial, which will be released upon interaction with its surrounding environment and/or stimuli, killing the planktonic and sessile microorganisms. Conversely, contact-active surfaces result from the covalent immobilization of an active agent on the implant’s surface, killing microorganisms that attempt to adhere [49,50,51,52,53]. Some research data illustrating the efficiency of active biomaterials in battling infections associated with bone-related biomaterials are included in Table 2.

Table 2.
Some examples of active biomaterials in fighting bone-related biomaterial infections.
In general, the antimicrobial substances (organic or inorganic) can be incorporated by mixing them with materials during production, absorbing them after production in the case of permeable or porous biomaterials, covalently binding them to functionalized coatings, and incorporating them into self-assembled mono/multilayer organic coatings [49,50,51,52,53]. Drug release occurs mainly by the means of the following: diffusion to the aqueous phase; erosion/degradation of resorbable loaded matrices, and hydrolysis of covalent bonds. The active principle release kinetics depends on the molecular bonds and the biodegradation/bioerosion rate, therefore it is possible to obtain several delivery kinetics profiles [49,50,51,52,53].
4.2.1. Biomaterials with Anti-Infective Organic Agents
Antibiotics (e.g., vancomycin, daptomycin, rifampicin, amoxicillin, levofloxacin, gentamicin or linezolid) are widely employed for the prevention and treatment of peri-prosthetic infections [123]. Up to now, despite wide research on several antibacterial surfaces, antibiotic-loaded implant materials are the only approach that has reached the market [85,87,89,90]. However, this approach has some drawbacks: (a) dose-dependent antibiotic activity; (b) delivery of sub-therapeutic antibiotic levels, favoring bacterial resistance development (c) limited antibiotic diffusion into peri-implant tissues, and (d) systemic and local cytotoxicity, impairing bone growth and implant osseointegration [86,88,124].
Therefore, it is essential to have alternative antimicrobial solutions to solve the aforementioned issues as well as to effectively prevent and manage implant-related infections.
Antimicrobial peptides (AMPs) are an interesting group of anti-infective agents currently viewed as alternatives to mitigate the problem of antibiotic-resistant microorganisms. Such peptides combine the antimicrobial activity against a wide range of pathogens (Gram-positive and Gram-negative bacteria, fungi, parasites and enveloped viruses) with acceptable biocompatibility [125,126,127,128]. AMPs are positively charged and present amphipathic behavior which enables interactions with bacterial membranes (lipopolysaccharides in Gram-negative and teichoic acids in Gram-positive bacteria), disrupting bacterial membrane integrity and leading to bacterial lysis [77,79,94,95,129,130,131]. It should be noted that AMPs hardly lead to resistance development [128]. Therefore, AMPs can represent excellent coating agents with broad-spectrum antimicrobial activity for preventing implant-associated infections [132,133,134]. AMPs coating onto implant surfaces is based on three strategies: (i) direct coating of peptide sequences onto biomaterials [93]; (ii) covalent linkage of peptides onto biomaterials using functional groups [91] and (iii) integration of peptides into a matrix layer or scaffold to be released over time [92]. In the latter method, peptides are initially encapsulated in a hydrogel or matrix, after which this hydrogel or matrix is applied to the biomaterial’s surface as a layer [128]. Independently of the chosen method, AMPs coating density on biomaterials is always a large challenge. In addition, crucial factors such as the peptides’ length, flexibility, and orientation, as well as spacer molecules that bind the peptides to the surface, must be taken into account for a coating to be successful and effective [128]. Besides, although several biophysical techniques exist that prove the existence of an AMP layer on the material, it is still difficult to pinpoint exactly how many molecules are attached. Moreover, AMPs are expensive to produce and are vulnerable to pH fluctuations and proteases in the environment [77,95,128].
As previously mentioned, the bacterial behavior within biofilms, bacterial biofilm resistance to external conditions and the virulence pathway of bacteria are regulated by the QS phenomenon [104,135]. Several studies have shown that QS inhibitors can effectively reduce the growth of planktonic bacteria and effectively inhibit/disintegrate bacterial biofilms, so as to achieve the effect of treating bacterial infection [102,103,104,135,136]. Therefore, these inhibitors interfere with bacterial communication, blocking the QS-mediated pathogenic infection by shutting down the expression of the pathogenic gene and diminishing the expression of virulence factors [96,98,137,138]. Staphylococcal infections are the primary cause of orthopedic implant failure, and the accessory gene regulator (agr) QS system is a crucial regulator of their pathogenic phenotype. For instance, Agr antagonist TrAIP-II or the AI agonist AIP-I interferes with QS communication or biofilm dispersal, respectively [99,101,135]. Several anti-Agr compounds have been studied as alternative agents for anti-infective biomaterials formulation [100,135]. Several studies have shown that dihydropyrrolones (DHPs), derivatives of the fimbrolide class of QS inhibitors, covalently immobilized on biomaterial surfaces, can diminish a microorganism’s colonization and avoid biofilm formation [99,101,135]. Nevertheless, there are still some drawbacks related to this approach, such as a narrow target spectrum; bacteria employing unique QS systems; the lack of large-scale clinical QS inhibitors testing, and the possibility to develop bacterial resistance toward QS inhibitors [135].
Bacteriophage (phage) therapy has emerged as a potential alternative therapy to conventional antibiotics to manage and treat biofilm-related infections [139,140,141,142,143,144]. Lytic phages, natural antimicrobial agents, are viruses harmless to humans that infect and kill target bacteria. They are specific to a bacterial host, replicating exponentially inside the bacterial cell. At the end of their life cycle, newly formed phages are released to infect new bacterial targets [142,145]. Additionally, phages encode in their genome some important hydrolytic enzymes (hydrolases and lyases) that degrade extracellular polymeric substances (EPSs) present in biofilms, making them a powerful weapon against biofilm-related infections [140,142]. Several pre-clinical animal studies support the use of phage therapy in the clinical treatment of infections, such as implant-related, diabetic cutaneous wounds, peri-prosthetic joint osteomyelitis and soft tissue infections [144,146,147]. These studies showed that the administration of phage solutions to the site of infections resulted in biofilm burden reduction and improvement of treatment outcomes [144,146,147]. Biomaterial-based local phage delivery systems have emerged as a therapeutic option in managing bone and joint infections because, besides conferring phage protection and stability, they allow for attaining phage delivery at or close to the infection site, phage bioavailability and prolonged residence at the infected site [17,34,105,106,107,148]. In general, three strategies can be used to produce phage-loaded biomaterials: (1) embedding; (2) encapsulation, and (3) surface functionalization through phage adsorption or covalent binding. The strategy choice is dictated by biomaterial type and its processability [149]. For instance, ceramics such as hydroxyapatite (HAP) or other calcium phosphates (CAP) require high sintering temperatures during processing, which dictates that phage adsorption after sintering is the only viable method [97]. One of the most commonly used strategies is the encapsulation of phages into hydrogels, liposomes or fibers. Barros et al. encapsulated phages into the alginate-nanohydroxyapatite hydrogel, showing that this delivery system can be a successful strategy in the management of bone implant-related infections by providing phage release within a broad range of pH (5 to 9). This strategy leads to promising features for phage delivery in the bone environment, with adequate tissue response and biosafety profiles, strong osteogenic and mineralization response, and excellent antimicrobial activity by inhibiting the attachment and colonization of multidrug-resistant bacteria surrounding and inside the femoral tissues [17]. In 2019, the Food and Drug Administration (FDA) approved the first United States (US) clinical trial for intravenous phage therapy [108]; however, there are still limitations, such as the production of robust and standardized phage preparations, the limited number of in vivo pharmacokinetic and pharmacodynamic studies, and so more testing is required to allow phage therapy to become a standardized and well-accepted strategy in clinical practice.
Figure 3 represents the main biomaterials strategies based on coating organic agents to avoid contamination and subsequent orthopedic implant-related infection.
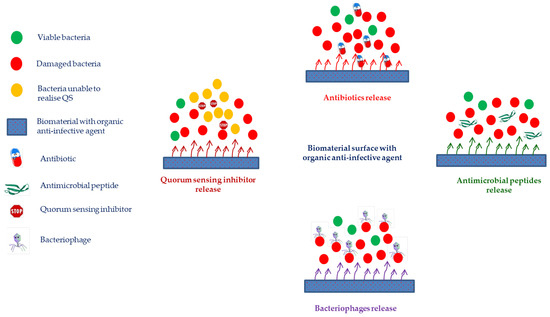
Figure 3.
Several strategies developed to trigger antibacterial action in biomaterials involving anti-infective organic agents.
4.2.2. Biomaterials with Anti-Infective Inorganic Agents
Silver, gold, zinc oxide, titanium dioxide, magnesium oxide, or copper oxide are inorganic metallic nanoparticles (NPs) that have been deemed to be effective antimicrobial agents to fight against biofilm-related infections [119]. The antimicrobial effectiveness of NPs are typically correlated with their capacity to: penetrate and disrupt the membrane of the microbial cells via membrane-damaging abrasiveness; reduce the cell’s permeability, and induce antimicrobial effects within the cells (e.g., producing reactive oxygen species (ROS), nucleic acids and protein interactions, enzyme inactivation and efflux pump overexpression) [119,150]. Besides, NPs can also cross the reticuloendothelial barrier, improving the antimicrobial agent’s internalization and the distribution of both hydrophilic and lipophilic molecules [119,150]. The physicochemical characteristics of NPs, including their chemistry, particle size and shape, surface charge and zeta potential, solubility, stability, and surface-to-volume ratio, have a direct impact on the antimicrobial capability of these materials [117,119,151]. For instance, NPs’ surface charge can affect cellular biodistribution and uptake once the NPs’ charges regulate interactions with tissues and tissue constituents. Although hydrophilic NPs have longer blood circulation due to reduced interactions with opsonins, hydrophobic NPs can modulate the interactions with the phospholipid layer within the microbial membrane [119]. There are three major ways to incorporate inorganic metallic nanoparticles into biomaterials: (1) integration into biomaterial matrix; (2) production of a film coated with inorganic NPs, and (3) grafting/immobilization onto the biomaterial surface [119]. As described by Spirescu et al., the sorts of matrices employed for NPs-loaded biomaterials development include a variety of materials, from natural or manufactured polymers to carbonaceous materials, such as graphene [119].
Silver (Ag) NPs are used for coatings of biomaterials due to their antimicrobial effectiveness against a wide assemblage of microorganisms, such as fungi, viruses, Gram-negative and Gram-positive bacteria including drug-resistant bacteria [110,111,152,153,154,155]. Although the exact mechanism of action of Ag+ ions is still not known, there are various hypothesized mechanisms, including direct damage to microorganism membrane, ROS formation, and disruption of ATP synthesis and DNA replication [109,156,157]. Additionally, to Ag+ ions, the morphology, size and shape of nanoparticles themselves, which determine their physicochemical properties and Ag+ release kinetics, also contribute to Ag NPs antimicrobial efficiency [158,159]. For instance, NPs with smaller diameters and greater surface areas contribute to increased antimicrobial bioactivity because they lead to the production of more ROS, necrotic factors, and apoptotic agents [119]. Ag NPs generally bind to the microbial cell membrane, and inside microorganisms interact with phosphorous- and sulfur-containing compounds (e.g., DNA), causing microbial death. The respiratory chain and cell division are first affected by the Ag NPs [110]. However, high Ag+ ions concentrations may have harmful effects on human cells. Therefore, the use of Ag NPs should be carefully regulated [119,160].
Gold (Au) NPs are stable metallic particles with intrinsic antibacterial and antifungal activity [109,112,113,114,119,160]. It should be noted that Au NPs exhibit in general higher antibacterial activity against Gram-negative bacteria probably due to their thinner cell walls and more stable electrostatic contacts [119,160]. The antimicrobial effects of Au NPs mechanisms include: (i) interactions between NPs and the microbial cell wall guided by electrostatic forces and carbohydrate, lipid, and protein binding; (ii) damages in the microbial cell membrane and wall with subsequent ribosome and mitochondrion impairment; (iii) inhibition of thiol groups present within microbial cells; (iv) intracellular ROS concentration increase and (v) microbial cell lysis [119,160,161,162]. The size and functionalization of Au NPs have a direct impact on their antimicrobial activity; as a result, NPs with smaller average sizes have enhanced antimicrobial performance. Moreover, the Physicochemical characteristics of the capping materials also influence their activity, once they regulate NPs’ surface characteristics [119,163]. However, cytotoxicity and biocompatibility problems have been linked to the use of Au NPs, making it necessary to strike a balance between toxic effects and antimicrobial activity when designing Au NPs [119,163].
The biocompatibility of zinc oxide (ZnO) NPs makes them attractive for many biomedical applications, such as tissue engineering, drug delivery systems, antimicrobial coatings, bioimaging, and antioxidant agents [116,117,118,119]. ZnO NPs have been explored as antimicrobial agents against bacteria, fungi and viruses by several authors due to their attractive properties such as large surface area, reduced size, high surface reactivity, and ability to absorb UV radiation [116,117,118,119]. In general, ZnO NPs’ antimicrobial action mechanisms include: (i) cell membrane structure deformation and consequent loss in cell integrity; (ii) disruption of metabolic and enzymatic processes and/or (iii) ROS production [119,153,164,165]. However, the release of Zn2+ ions depends on the NPs physicochemical and morphological properties. Furthermore, antimicrobial features are also influenced by the microbial strain, NPs concentration, and time of interaction [119].
Titanium dioxide (TiO2) NPs, due to their photocatalytic antimicrobial activity, are the most studied NPs as an alternative antimicrobial agent [121]. TiO2 NPs generate ROS, such as hydrogen peroxide and hydroxyl radicals, that upon exposure to ultraviolet (UV) radiation, lead to damage to microbial cell membranes, compromising membrane semipermeability, interfering with oxidative phosphorylation, and causing microbial cell death [120,153]. Similarly to ZnO NPs, TiO2 NPs main characteristics that affect their antibacterial activities are the shape, size, crystal structure, surface charge, chemistry, concentration, and exposure time [119].
Like to TiO NPs, MgO NPs have been approved by the FDA as safe materials, which has sparked curiosity among scientists about their potential use in biomedical fields. MgO NPs present antibacterial activity against Gram-positive and Gram-negative bacteria (e.g., S. aureus, P. aeruginosa, and E. coli) and fungi (e.g., Candida albicans), as well as anti-biofilm characteristics [122]. The antimicrobial mechanisms underlying MgO NPs are based on (1) the dissociation of Mg2+ ions, which generate the superoxide anion through the reaction with oxygen present on the microbial cell surface, and (2) ROS production, which induces disruption of the membrane and causes cell death. MgO NPs physicochemical properties such as surface area, chemistry, roughness, and wettability, could also interfere with the bacterial QS, thus inhibiting biofilm formation [119].
Copper oxide (CuO) NPs have been used as competitor antimicrobial agents to Au NPs and Ag NPs, due to their low production costs involved. In general, the antimicrobial bioactivity of Cu NP results from the formation of the Cu+ ions complexes and the production of ROS, processes that lead to the inactivation of microbial enzymes and disturbances of amino acid and nucleic acid biosynthesis, respectively. However, some cytotoxicity and genotoxic effects of Cu NPs have been reported, namely when used at high concentrations, thereby more studies should be performed to ensure their safety [119,166].
5. Conclusions and Final Remarks
Any surgical intervention, particularly ones including the implantation of biomaterials, has a high risk of associated infections. These infections can be devastating for the patients and overload healthcare systems.
Currently, prophylactic systemic antibiotic therapy is administered as a preventive and therapeutic measure to patients to whom an implant is applied. However, this therapy entails many disadvantages, including the low drug concentration reaching the target site and the corresponding limited antimicrobial activity at the target site. Moreover, the wide variety of pathogenic bacteria causing infections related to orthopedic implants, the emergence of bacteria resistant to antibiotics and the cytotoxicity associated with them lead to the need to search for new alternative approaches to prevent and control implant-related infections. The use of local strategies such as anti-adhesive surfaces or active surfaces has emerged as an effective approach to preventing and treating orthopedic biomaterial-related infections. Various concepts and approaches have been applied in the development of bioengineered materials with anti-infective properties, preventing microbial adhesion and colonization into bone tissue, and implant surfaces, and/or creating a free-bacteria environment around the implant. Biomaterials endowed with anti-infective properties need to be tailored according to the specific application and can be classified into two main groups: passive surfaces presenting chemistry and/or structure modifications which prevent or reduce microbial adhesion; and active surfaces with pre-entrapped or coated antimicrobial agents (antibiotics, peptides, bacteriophages, metals or metal ions), which will be released upon interaction with its surrounding environment and/or stimuli, killing the planktonic and sessile microorganisms.
A variety of polymers (e.g., PEG or polymer-based hydrogels), solutions (serum, plasma, or protein) and physical modifications (structure or morphology) can be used to create passive surfaces. Their anti-fouling mechanism is based on physicochemical mechanisms (e.g., steric repulsion, electrostatic repulsion, low surface energy, superhydrophobic and hydrophobic interactions, and substrate-microorganism physical interaction), which act as a physical barrier to avoid protein and bacterial adhesion.
Active biomaterials are based on the incorporation of organic (e.g., antibiotics, antimicrobial peptides, QS inhibitors, or bacteriophages) and inorganic (mainly metal ions, e.g., silver, gold, zinc, copper, magnesium) antimicrobial agents into the biomaterial surface. The antimicrobial agents can be covalently bound to functionalized coatings, or incorporated into self-assembled mono/multilayer coatings during or after biomaterial production.
Antibiotics (e.g., vancomycin, daptomycin, rifampicin, amoxicillin, levofloxacin, gentamicin, or linezolid) are widely employed for the prevention and treatment of peri-prosthetic infections. Up to now, antibiotic-loaded implant materials are the only approach that has reached the market. However, this approach has some drawbacks namely: dose-dependent activity; sub-therapeutic delivery, limited diffusion into peri-implant tissues, and systemic and local cytotoxicity.
Antimicrobial peptides (AMPs) are an interesting group of anti-infective agents currently viewed as alternatives to mitigate the problem of antibiotic-resistant microorganisms. However, AMPs are expensive to produce and are vulnerable to pH fluctuations and proteases in the environment.
QS inhibitors show interesting antimicrobial properties, namely in the inhibition and disintegration of biofilms. Nevertheless, some drawbacks are reported, such as a narrow target spectrum, specific QS for target bacteria, the lack of large-scale clinical QS inhibitors testing, and QS-resistant bacteria development.
Phage therapy has emerged as a potential alternative therapy to conventional antibiotics to manage and treat biofilm-related infections. However, more tests such as standardized and robust phage production, in vivo pharmacokinetic and pharmacodynamics studies, are required in order to allow phage therapy to become a standardized and well-accepted strategy in clinical practice.
Silver, gold, zinc oxide, titanium dioxide, magnesium oxide, or copper oxide are in-organic metallic nanoparticles (NPs), that have been deemed to be effective antimicrobial agents to fight against biofilm-related infections; however, there are still several side effects to be controlled concerning its use in clinical applications.
In sum, a variety of concepts and approaches are applied to create anti-infective bioengineered materials to combat infections associated with orthopedic biomaterials. However, there is still a long way to go before they are used in clinical settings, requiring a search for new approaches or the improve of the available ones in order to overcome safety and efficacy issues related to their implementation.
Author Contributions
Conceptualization, J.B. and M.P.F.; methodology, writing—original draft preparation, writing—review and editing, J.B., F.J.M. and M.P.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wang, W.; Yeung, K.W.K. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef] [PubMed]
- Trampuz, A.; Zimmerli, W. Diagnosis and treatment of infections associated with fracture-fixation devices. Injury 2006, 37, S59–S66. [Google Scholar] [CrossRef] [PubMed]
- Nisyrios, T.; Karygianni, L.; Fretwurst, T.; Nelson, K.; Hellwig, E.; Schmelzeisen, R.; Al-Ahmad, A. High Potential of Bacterial Adhesion on Block Bone Graft Materials. Materials 2020, 13, 2102. [Google Scholar] [CrossRef] [PubMed]
- Xi, W.; Hegde, V.; Zoller, S.D.; Park, H.Y.; Hart, C.M.; Kondo, T.; Hamad, C.D.; Hu, Y.; Loftin, A.H.; Johansen, D.O.; et al. Point-of-care antimicrobial coating protects orthopaedic implants from bacterial challenge. Nat. Commun. 2021, 12, 5473. [Google Scholar] [CrossRef] [PubMed]
- Puhto, T.; Puhto, A.P.; Vielma, M.; Syrjala, H. Infection triples the cost of a primary joint arthroplasty. Infect. Dis. 2019, 51, 348–355. [Google Scholar] [CrossRef]
- Metsemakers, W.J.; Onsea, J.; Neutjens, E.; Steffens, E.; Schuermans, A.; McNally, M.; Nijs, S. Prevention of fracture-related infection: A multidisciplinary care package. Int. Orthop. 2017, 41, 2457–2469. [Google Scholar] [CrossRef]
- Seebach, E.; Kubatzky, K.F. Chronic Implant-Related Bone Infections-Can Immune Modulation be a Therapeutic Strategy? Front. Immunol. 2019, 10, 1724. [Google Scholar] [CrossRef]
- Cerioli, M.; Batailler, C.; Conrad, A.; Roux, S.; Perpoint, T.; Becker, A.; Triffault-Fillit, C.; Lustig, S.; Fessy, M.H.; Laurent, F.; et al. Pseudomonas aeruginosa Implant-Associated Bone and Joint Infections: Experience in a Regional Reference Center in France. Front. Med. 2020, 7, 513242. [Google Scholar] [CrossRef]
- Chang, C.H.; Hu, C.C.; Chang, Y.; Hsieh, P.H.; Shih, H.N.; Ueng, S.W. Two-stage revision arthroplasty for Mycobacterium Tuberculosis periprosthetic joint infection: An outcome analysis. PLoS ONE 2018, 13, e0203585. [Google Scholar] [CrossRef]
- Rhoads, D.D.; Wolcott, R.D.; Percival, S.L. Biofilms in wounds: Management strategies. J. Wound Care 2008, 17, 502–508. [Google Scholar] [CrossRef]
- Zilberman, M.; Elsner, J.J. Antibiotic-eluting medical devices for various applications. J. Control. Release 2008, 130, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Blackledge, M.S.; Worthington, R.J.; Melander, C. Biologically inspired strategies for combating bacterial biofilms. Curr. Opin. Pharmacol. 2013, 13, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Arciola, C.R.; Campoccia, D.; Montanaro, L. Implant infections: Adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 2018, 16, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Qin, H.; Cao, H.; Zhao, Y.; Zhu, C.; Cheng, T.; Wang, Q.; Peng, X.; Cheng, M.; Wang, J.; Jin, G.; et al. In vitro and in vivo anti-biofilm effects of silver nanoparticles immobilized on titanium. Biomaterials 2014, 35, 9114–9125. [Google Scholar] [CrossRef] [PubMed]
- Barros, J.; Grenho, L.; Fontenente, S.; Manuel, C.M.; Nunes, O.C.; Melo, L.F.; Monteiro, F.J.; Ferraz, M.P. Staphylococcus aureus and Escherichia coli dual-species biofilms on nanohydroxyapatite loaded with CHX or ZnO nanoparticles. J. Biomed. Mater. Res. A 2017, 105, 491–497. [Google Scholar] [CrossRef]
- Riool, M.; de Breij, A.; Drijfhout, J.W.; Nibbering, P.H.; Zaat, S.A.J. Antimicrobial Peptides in Biomedical Device Manufacturing. Front. Chem. 2017, 5, 63. [Google Scholar] [CrossRef]
- Barros, J.A.R.; Melo, L.D.R.; Silva, R.; Ferraz, M.P.; Azeredo, J.; Pinheiro, V.M.C.; Colaco, B.J.A.; Fernandes, M.H.R.; Gomes, P.S.; Monteiro, F.J. Encapsulated bacteriophages in alginate-nanohydroxyapatite hydrogel as a novel delivery system to prevent orthopedic implant-associated infections. Nanomedicine 2020, 24, 102145. [Google Scholar] [CrossRef]
- Marques, D.M.; Oliveira, V.C.; Souza, M.T.; Zanotto, E.D.; Issa, J.P.M.; Watanabe, E. Biomaterials for orthopedics: Anti-biofilm activity of a new bioactive glass coating on titanium implants. Biofouling 2020, 36, 234–244. [Google Scholar] [CrossRef]
- Coppola, G.A.; Onsea, J.; Moriarty, T.F.; Nehrbass, D.; Constant, C.; Zeiter, S.; Aktan, M.K.; Braem, A.; Van der Eycken, E.V.; Steenackers, H.P.; et al. An Improved 2-Aminoimidazole Based Anti-Biofilm Coating for Orthopedic Implants: Activity, Stability, and in vivo Biocompatibility. Front. Microbiol. 2021, 12, 658521. [Google Scholar] [CrossRef]
- Otto, M. Staphylococcal infections: Mechanisms of biofilm maturation and detachment as critical determinants of pathogenicity. Annu. Rev. Med. 2013, 64, 175–188. [Google Scholar] [CrossRef]
- Shrestha, L.; Fan, H.M.; Tao, H.R.; Huang, J.D. Recent Strategies to Combat Biofilms Using Antimicrobial Agents and Therapeutic Approaches. Pathogens 2022, 11, 292. [Google Scholar] [CrossRef] [PubMed]
- Arts, J.J.C.; Geurts, J. ScienceDirect. Management of Periprosthetic Joint Infections (PJIs); Woodhead Publishing: Duxford, UK, 2016. [Google Scholar]
- Moriarty, T.F.; Kuehl, R.; Coenye, T.; Metsemakers, W.J.; Morgenstern, M.; Schwarz, E.M.; Riool, M.; Zaat, S.A.J.; Khana, N.; Kates, S.L.; et al. Orthopaedic device-related infection: Current and future interventions for improved prevention and treatment. EFORT Open Rev. 2016, 1, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, W.; Moser, C. Pathogenesis and treatment concepts of orthopaedic biofilm infections. FEMS Immunol. Med. Microbiol. 2012, 65, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.; Dias, M. The Microbiological Profiles of Infected Prosthetic Implants with an Emphasis on the Organisms which Form Biofilms. J. Clin. Diagn. Res. 2013, 7, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Arciola, C.R.; An, Y.H.; Campoccia, D.; Donati, M.E.; Montanaro, L. Etiology of implant orthopedic infections: A survey on 1027 clinical isolates. Int. J. Artif. Organs 2005, 28, 1091–1100. [Google Scholar] [CrossRef] [PubMed]
- Montanaro, L.; Speziale, P.; Campoccia, D.; Ravaioli, S.; Cangini, I.; Pietrocola, G.; Giannini, S.; Arciola, C.R. Scenery of Staphylococcus implant infections in orthopedics. Future Microbiol. 2011, 6, 1329–1349. [Google Scholar] [CrossRef]
- Aggarwal, V.K.; Bakhshi, H.; Ecker, N.U.; Parvizi, J.; Gehrke, T.; Kendoff, D. Organism profile in periprosthetic joint infection: Pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J. Knee Surg. 2014, 27, 399–406. [Google Scholar] [CrossRef]
- Metsemakers, W.J.; Kuehl, R.; Moriarty, T.F.; Richards, R.G.; Verhofstad, M.H.J.; Borens, O.; Kates, S.; Morgenstern, M. Infection after fracture fixation: Current surgical and microbiological concepts. Injury 2018, 49, 511–522. [Google Scholar] [CrossRef]
- Esposito, S.; Leone, S. Prosthetic joint infections: Microbiology, diagnosis, management and prevention. Int. J. Antimicrob. Agents 2008, 32, 287–293. [Google Scholar] [CrossRef]
- Trampuz, A.; Zimmerli, W. Diagnosis and treatment of implant-associated septic arthritis and osteomyelitis. Curr. Infect. Dis. Rep. 2008, 10, 394–403. [Google Scholar] [CrossRef]
- Trampuz, A.; Widmer, A.F. Infections associated with orthopedic implants. Curr. Opin. Infect. Dis. 2006, 19, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Webster, T.J. Bacteria antibiotic resistance: New challenges and opportunities for implant-associated orthopedic infections. J. Orthop. Res. 2018, 36, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Barros, J.; Melo, L.D.R.; Poeta, P.; Igrejas, G.; Ferraz, M.P.; Azeredo, J.; Monteiro, F.J. Lytic bacteriophages against multidrug-resistant Staphylococcus aureus, Enterococcus faecalis and Escherichia coli isolates from orthopaedic implant-associated infections. Int. J. Antimicrob. Agents 2019, 54, 329–337. [Google Scholar] [CrossRef] [PubMed]
- You, D.Z.; Schneider, P.S. Surgical timing for open fractures: Middle of the night or the light of day, which fractures, what time? OTA Int. 2020, 3, e067. [Google Scholar] [CrossRef]
- Otto, M. Staphylococcal biofilms. Curr. Top. Microbiol. Immunol. 2008, 322, 207–228. [Google Scholar] [CrossRef]
- Zimmerli, W.; Sendi, P. Pathogenesis of implant-associated infection: The role of the host. Semin. Immunopathol. 2011, 33, 295–306. [Google Scholar] [CrossRef]
- Arciola, C.R.; Campoccia, D.; Speziale, P.; Montanaro, L.; Costerton, J.W. Biofilm formation in Staphylococcus implant infections. A review of molecular mechanisms and implications for biofilm-resistant materials. Biomaterials 2012, 33, 5967–5982. [Google Scholar] [CrossRef]
- Glinel, K.; Thebault, P.; Humblot, V.; Pradier, C.M.; Jouenne, T. Antibacterial surfaces developed from bio-inspired approaches. Acta Biomater. 2012, 8, 1670–1684. [Google Scholar] [CrossRef]
- Joo, H.S.; Otto, M. Molecular basis of in vivo biofilm formation by bacterial pathogens. Chem. Biol. 2012, 19, 1503–1513. [Google Scholar] [CrossRef]
- Schaer, T.P.; Stewart, S.; Hsu, B.B.; Klibanov, A.M. Hydrophobic polycationic coatings that inhibit biofilms and support bone healing during infection. Biomaterials 2012, 33, 1245–1254. [Google Scholar] [CrossRef]
- Rodriguez-Merchan, E.C.; Davidson, D.J.; Liddle, A.D. Recent Strategies to Combat Infections from Biofilm-Forming Bacteria on Orthopaedic Implants. Int. J. Mol. Sci. 2021, 22, 10243. [Google Scholar] [CrossRef] [PubMed]
- Bryers, J.D. Medical biofilms. Biotechnol. Bioeng. 2008, 100, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Khatoon, Z.; McTiernan, C.D.; Suuronen, E.J.; Mah, T.F.; Alarcon, E.I. Bacterial biofilm formation on implantable devices and approaches to its treatment and prevention. Heliyon 2018, 4, e01067. [Google Scholar] [CrossRef] [PubMed]
- Vuong, C.; Voyich, J.M.; Fischer, E.R.; Braughton, K.R.; Whitney, A.R.; DeLeo, F.R.; Otto, M. Polysaccharide intercellular adhesin (PIA) protects Staphylococcus epidermidis against major components of the human innate immune system. Cell Microbiol. 2004, 6, 269–275. [Google Scholar] [CrossRef]
- Gupta, R.; Schuster, M. Quorum sensing modulates colony morphology through alkyl quinolones in Pseudomonas aeruginosa. BMC Microbiol. 2012, 12, 30. [Google Scholar] [CrossRef]
- Wang, B.; Muir, T.W. Regulation of Virulence in Staphylococcus aureus: Molecular Mechanisms and Remaining Puzzles. Cell Chem. Biol. 2016, 23, 214–224. [Google Scholar] [CrossRef]
- Hasan, J.; Crawford, R.J.; Ivanova, E.P. Antibacterial surfaces: The quest for a new generation of biomaterials. Trends Biotechnol. 2013, 31, 295–304. [Google Scholar] [CrossRef]
- Gallo, J.; Holinka, M.; Moucha, C.S. Antibacterial surface treatment for orthopaedic implants. Int. J. Mol. Sci. 2014, 15, 13849–13880. [Google Scholar] [CrossRef]
- Romano, C.L.; Scarponi, S.; Gallazzi, E.; Romano, D.; Drago, L. Antibacterial coating of implants in orthopaedics and trauma: A classification proposal in an evolving panorama. J. Orthop. Surg. Res. 2015, 10, 157. [Google Scholar] [CrossRef]
- Hetrick, E.M.; Schoenfisch, M.H. Reducing implant-related infections: Active release strategies. Chem. Soc. Rev. 2006, 35, 780–789. [Google Scholar] [CrossRef]
- Charville, G.W.; Hetrick, E.M.; Geer, C.B.; Schoenfisch, M.H. Reduced bacterial adhesion to fibrinogen-coated substrates via nitric oxide release. Biomaterials 2008, 29, 4039–4044. [Google Scholar] [CrossRef] [PubMed]
- Sileika, T.S.; Kim, H.D.; Maniak, P.; Messersmith, P.B. Antibacterial performance of polydopamine-modified polymer surfaces containing passive and active components. ACS Appl. Mater. Interfaces 2011, 3, 4602–4610. [Google Scholar] [CrossRef] [PubMed]
- Harris, L.G.; Tosatti, S.; Wieland, M.; Textor, M.; Richards, R.G. Staphylococcus aureus adhesion to titanium oxide surfaces coated with non-functionalized and peptide-functionalized poly(L-lysine)-grafted-poly(ethylene glycol) copolymers. Biomaterials 2004, 25, 4135–4148. [Google Scholar] [CrossRef] [PubMed]
- Beloin, C.; Renard, S.; Ghigo, J.M.; Lebeaux, D. Novel approaches to combat bacterial biofilms. Curr. Opin. Pharmacol. 2014, 18, 61–68. [Google Scholar] [CrossRef]
- Uneputty, A.; Davila-Lezama, A.; Garibo, D.; Oknianska, A.; Bogdanchikova, N.; Hernandez-Sanchez, J.F.; Susarrey-Arce, A. Strategies applied to modify structured and smooth surfaces: A step closer to reduce bacterial adhesion and biofilm formation. Colloid Interfac. Sci. 2022, 46, 100560. [Google Scholar] [CrossRef]
- Yu, Q.; Zhang, Y.; Wang, H.; Brash, J.; Chen, H. Anti-fouling bioactive surfaces. Acta Biomater. 2011, 7, 1550–1557. [Google Scholar] [CrossRef]
- Francolini, I.; Silvestro, I.; Di Lisio, V.; Martinelli, A.; Piozzi, A. Synthesis, Characterization, and Bacterial Fouling-Resistance Properties of Polyethylene Glycol-Grafted Polyurethane Elastomers. Int. J. Mol. Sci. 2019, 20, 1001. [Google Scholar] [CrossRef]
- Peng, L.; Chang, L.; Si, M.; Lin, J.; Wei, Y.; Wang, S.; Liu, H.; Han, B.; Jiang, L. Hydrogel-Coated Dental Device with Adhesion-Inhibiting and Colony-Suppressing Properties. ACS Appl. Mater. Interfaces 2020, 12, 9718–9725. [Google Scholar] [CrossRef]
- Estephan, Z.G.; Schlenoff, P.S.; Schlenoff, J.B. Zwitteration As an Alternative to PEGylation. Langmuir 2011, 27, 6794–6800. [Google Scholar] [CrossRef]
- Hu, G.; Emrick, T. Functional Choline Phosphate Polymers. J. Am. Chem. Soc. 2016, 138, 1828–1831. [Google Scholar] [CrossRef]
- Zhao, C.; Zhou, L.; Chiao, M.; Yang, W. Antibacterial hydrogel coating: Strategies in surface chemistry. Adv. Colloid Interface Sci. 2020, 285, 102280. [Google Scholar] [CrossRef]
- D’Almeida, M.; Attik, N.; Amalric, J.; Brunon, C.; Renaud, F.; Abouelleil, H.; Toury, B.; Grosgogeat, B. Chitosan coating as an antibacterial surface for biomedical applications. PLoS ONE 2017, 12, e0189537. [Google Scholar] [CrossRef] [PubMed]
- Francone, A.; Merino, S.; Retolaza, A.; Ramiro, J.; Alves, S.A.; de Castro, J.V.; Neves, N.M.; Arana, A.; Marimon, J.M.; Torres, C.M.S.; et al. Impact of surface topography on the bacterial attachment to micro- and nano-patterned polymer films. Surf. Interfaces 2021, 27, 101494. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.C.; Wang, Z.P.; Guo, S.; Zhang, J.Y.; Song, Y.; Dong, X.M.; Wang, X.N.; Yu, J.H. Antibacterial and anti-adhesive zeolite coatings on titanium alloy surface. Micropor. Mesopor. Mat. 2011, 146, 216–222. [Google Scholar] [CrossRef]
- Huang, S.; Wan, Y.; Ming, X.; Zhou, J.; Zhou, M.; Chen, H.; Zhang, Q.; Zhu, S. Adhering Low Surface Energy Materials without Surface Pretreatment via Ion-Dipole Interactions. ACS Appl. Mater. Interfaces 2021, 13, 41112–41119. [Google Scholar] [CrossRef]
- Song, F.; Zhang, L.; Chen, R.; Liu, Q.; Liu, J.; Yu, J.; Liu, P.; Duan, J.; Wang, J. Bioinspired Durable Antibacterial and Antifouling Coatings Based on Borneol Fluorinated Polymers: Demonstrating Direct Evidence of Antiadhesion. ACS Appl. Mater. Interfaces 2021, 13, 33417–33426. [Google Scholar] [CrossRef]
- Stallard, C.P.; McDonnell, K.A.; Onayemi, O.D.; O’Gara, J.P.; Dowling, D.P. Evaluation of protein adsorption on atmospheric plasma deposited coatings exhibiting superhydrophilic to superhydrophobic properties. Biointerphases 2012, 7, 31. [Google Scholar] [CrossRef]
- Zhang, X.X.; Wang, L.; Levanen, E. Superhydrophobic surfaces for the reduction of bacterial adhesion. Rsc. Adv. 2013, 3, 12003–12020. [Google Scholar] [CrossRef]
- Falde, E.J.; Yohe, S.T.; Colson, Y.L.; Grinstaff, M.W. Superhydrophobic materials for biomedical applications. Biomaterials 2016, 104, 87–103. [Google Scholar] [CrossRef]
- Naderizadeh, S.; Dante, S.; Picone, P.; Di Carlo, M.; Carzino, R.; Athanassiou, A.; Bayer, I.S. Bioresin-based superhydrophobic coatings with reduced bacterial adhesion. J. Colloid Interface Sci. 2020, 574, 20–32. [Google Scholar] [CrossRef]
- Emelyanenko, A.M.; Domantovsky, A.G.; Kaminsky, V.V.; Pytskii, I.S.; Emelyanenko, K.A.; Boinovich, L.B. The Mechanisms of Antibacterial Activity of Magnesium Alloys with Extreme Wettability. Materials 2021, 14, 5454. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Xiangde, L.; Park, J.; Choi, D.; Heo, J.; Chang, M.; Lee, C.; Hong, J. Superhydrophilic coatings with intricate nanostructure based on biotic materials for antifogging and antibiofouling applications. Chem. Eng. J. 2017, 309, 463–470. [Google Scholar] [CrossRef]
- An, Y.H.; Bradley, J.; Powers, D.L.; Friedman, R.J. The prevention of prosthetic infection using a cross-linked albumin coating in a rabbit model. J. Bone Joint Surg. Br. 1997, 79, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Katsikogianni, M.; Missirlis, Y.F. Concise review of mechanisms of bacterial adhesion to biomaterials and of techniques used in estimating bacteria-material interactions. Eur. Cell Mater. 2004, 8, 37–57. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.; Aytac, S.; Hansch, G.M. Biofilm growth on implants: Bacteria prefer plasma coats. Int. J. Artif. Organs 2011, 34, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.D.; Won, H.S.; Kim, J.H.; Mishig-Ochir, T.; Lee, B.J. Antimicrobial Peptides for Therapeutic Applications: A Review. Molecules 2012, 17, 12276–12286. [Google Scholar] [CrossRef]
- Vadillo-Rodriguez, V.; Pacha-Olivenza, M.A.; Gonzalez-Martin, M.L.; Bruque, J.M.; Gallardo-Moreno, A.M. Adsorption behavior of human plasma fibronectin on hydrophobic and hydrophilic Ti6Al4V substrata and its influence on bacterial adhesion and detachment. J. Biomed. Mater. Res. A 2013, 101, 1397–1404. [Google Scholar] [CrossRef]
- Muszanska, A.K.; Rochford, E.T.J.; Gruszka, A.; Bastian, A.A.; Busscher, H.J.; Norde, W.; van der Mei, H.C.; Herrmann, A. Antiadhesive Polymer Brush Coating Functionalized with Antimicrobial and RGD Peptides to Reduce Biofilm Formation and Enhance Tissue Integration. Biomacromolecules 2014, 15, 2019–2026. [Google Scholar] [CrossRef]
- Arango-Santander, S.; Pelaez-Vargas, A.; Freitas, S.C.; Garcia, C. A novel approach to create an antibacterial surface using titanium dioxide and a combination of dip-pen nanolithography and soft lithography. Sci. Rep. 2018, 8, 15818. [Google Scholar] [CrossRef]
- Lutey, A.H.A.; Gemini, L.; Romoli, L.; Lazzini, G.; Fuso, F.; Faucon, M.; Kling, R. Towards Laser-Textured Antibacterial Surfaces. Sci. Rep. 2018, 8, 10112. [Google Scholar] [CrossRef]
- Rigo, S.; Cai, C.; Gunkel-Grabole, G.; Maurizi, L.; Zhang, X.; Xu, J.; Palivan, C.G. Nanoscience-Based Strategies to Engineer Antimicrobial Surfaces. Adv. Sci. 2018, 5, 1700892. [Google Scholar] [CrossRef] [PubMed]
- Puckett, S.D.; Taylor, E.; Raimondo, T.; Webster, T.J. The relationship between the nanostructure of titanium surfaces and bacterial attachment. Biomaterials 2010, 31, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Damiati, L.; Eales, M.G.; Nobbs, A.H.; Su, B.; Tsimbouri, P.M.; Salmeron-Sanchez, M.; Dalby, M.J. Impact of surface topography and coating on osteogenesis and bacterial attachment on titanium implants. J. Tissue Eng. 2018, 9, 2041731418790694. [Google Scholar] [CrossRef] [PubMed]
- Antoci, V., Jr.; King, S.B.; Jose, B.; Parvizi, J.; Zeiger, A.R.; Wickstrom, E.; Freeman, T.A.; Composto, R.J.; Ducheyne, P.; Shapiro, I.M.; et al. Vancomycin covalently bonded to titanium alloy prevents bacterial colonization. J. Orthop. Res. 2007, 25, 858–866. [Google Scholar] [CrossRef]
- Hickok, N.J.; Shapiro, I.M. Immobilized antibiotics to prevent orthopaedic implant infections. Adv. Drug Deliv. Rev. 2012, 64, 1165–1176. [Google Scholar] [CrossRef]
- Neut, D.; Dijkstra, R.J.; Thompson, J.I.; van der Mei, H.C.; Busscher, H.J. A gentamicin-releasing coating for cementless hip prostheses-Longitudinal evaluation of efficacy using in vitro bio-optical imaging and its wide-spectrum antibacterial efficacy. J. Biomed. Mater. Res. A 2012, 100, 3220–3226. [Google Scholar] [CrossRef]
- Zegre, M.; Barros, J.; Ribeiro, I.A.C.; Santos, C.; Caetano, L.A.; Goncalves, L.; Monteiro, F.J.; Ferraz, M.P.; Bettencourt, A. Poly(DL-lactic acid) scaffolds as a bone targeting platform for the co-delivery of antimicrobial agents against S. aureus-C. albicans mixed biofilms. Int. J. Pharm. 2022, 622, 121832. [Google Scholar] [CrossRef]
- Alt, V.; Bitschnau, A.; Osterling, J.; Sewing, A.; Meyer, C.; Kraus, R.; Meissner, S.A.; Wenisch, S.; Domann, E.; Schnettler, R. The effects of combined gentamicin-hydroxyapatite coating for cementless joint prostheses on the reduction of infection rates in a rabbit infection prophylaxis model. Biomaterials 2006, 27, 4627–4634. [Google Scholar] [CrossRef]
- Van Vugt, T.A.G.; Arts, J.J.; Geurts, J.A.P. Antibiotic-Loaded Polymethylmethacrylate Beads and Spacers in Treatment of Orthopedic Infections and the Role of Biofilm Formation. Front. Microbiol. 2019, 10, 1626. [Google Scholar] [CrossRef]
- Monteiro, C.; Costa, F.; Pirttila, A.M.; Tejesvi, M.V.; Martins, M.C.L. Prevention of urinary catheter-associated infections by coating antimicrobial peptides from crowberry endophytes. Sci. Rep. 2019, 9, 10753. [Google Scholar] [CrossRef]
- Chen, J.; Shi, X.; Zhu, Y.; Chen, Y.; Gao, M.; Gao, H.; Liu, L.; Wang, L.; Mao, C.; Wang, Y. On-demand storage and release of antimicrobial peptides using Pandora’s box-like nanotubes gated with a bacterial infection-responsive polymer. Theranostics 2020, 10, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Wisdom, E.C.; Zhou, Y.; Chen, C.; Tamerler, C.; Snead, M.L. Mitigation of peri-implantitis by rational design of bifunctional peptides with antimicrobial properties. ACS Biomater. Sci. Eng. 2020, 6, 2682–2695. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, A.; Pirri, G.; Nicoletto, S.F. Antimicrobial peptides: An overview of a promising class of therapeutics. Cent. Eur. J. Biol. 2007, 2, 1–33. [Google Scholar] [CrossRef]
- Gordon, Y.J.; Romanowski, E.G.; McDermott, A.M. A review of antimicrobial peptides and their therapeutic potential as anti-infective drugs. Curr. Eye Res. 2005, 30, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Maeda, T.; Garcia-Contreras, R.; Pu, M.; Sheng, L.; Garcia, L.R.; Tomas, M.; Wood, T.K. Quorum quenching quandary: Resistance to antivirulence compounds. ISME J. 2012, 6, 493–501. [Google Scholar] [CrossRef]
- Meurice, E.; Rguiti, E.; Brutel, A.; Hornez, J.C.; Leriche, A.; Descamps, M.; Bouchart, F. New antibacterial microporous CaP materials loaded with phages for prophylactic treatment in bone surgery. J. Mater. Sci. Mater. Med. 2012, 23, 2445–2452. [Google Scholar] [CrossRef]
- Kalia, V.C. Quorum sensing inhibitors: An overview. Biotechnol. Adv. 2013, 31, 224–245. [Google Scholar] [CrossRef]
- Ho, K.K.; Chen, R.; Willcox, M.D.; Rice, S.A.; Cole, N.; Iskander, G.; Kumar, N. Quorum sensing inhibitory activities of surface immobilized antibacterial dihydropyrrolones via click chemistry. Biomaterials 2014, 35, 2336–2345. [Google Scholar] [CrossRef]
- Kim, M.K.; Zhao, A.; Wang, A.; Brown, Z.Z.; Muir, T.W.; Stone, H.A.; Bassler, B.L. Surface-attached molecules control Staphylococcus aureus quorum sensing and biofilm development. Nat. Microbiol. 2017, 2, 17080. [Google Scholar] [CrossRef]
- Ozcelik, B.; Ho, K.K.K.; Glattauer, V.; Willcox, M.; Kumar, N.; Thissen, H. Poly(ethylene glycol)-Based Coatings Combining Low-Biofouling and Quorum-Sensing Inhibiting Properties to Reduce Bacterial Colonization. ACS Biomater. Sci. Eng. 2017, 3, 78–87. [Google Scholar] [CrossRef]
- Wang, D.; Shi, J.; Xiong, Y.; Hu, J.; Lin, Z.; Qiu, Y.; Cheng, J. A QSAR-based mechanistic study on the combined toxicity of antibiotics and quorum sensing inhibitors against Escherichia coli. J. Hazard. Mater. 2018, 341, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.K.; Murgia, X.; De Rossi, C.; Christmann, R.; Hufner de Mello Martins, A.G.; Koch, M.; Andreas, A.; Herrmann, J.; Muller, R.; Empting, M.; et al. Squalenyl Hydrogen Sulfate Nanoparticles for Simultaneous Delivery of Tobramycin and an Alkylquinolone Quorum Sensing Inhibitor Enable the Eradication of P. aeruginosa Biofilm Infections. Angew. Chem. Int. Ed. Engl. 2020, 59, 10292–10296. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Ding, Y.; Tao, B.; Yuan, Z.; Yang, Y.; Xu, K.; Li, X.; Liu, P.; Cai, K. Surface modification of titanium substrate via combining photothermal therapy and quorum-sensing-inhibition strategy for improving osseointegration and treating biofilm-associated bacterial infection. Bioact. Mater. 2022, 18, 228–241. [Google Scholar] [CrossRef]
- Barros, J.; Ferraz, M.P.; Azeredo, J.; Fernandes, M.H.; Gomes, P.S.; Monteiro, F.J. Alginate-nanohydroxyapatite hydrogel system: Optimizing the formulation for enhanced bone regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 105, 109985. [Google Scholar] [CrossRef] [PubMed]
- Pouget, C.; Dunyach-Remy, C.; Pantel, A.; Boutet-Dubois, A.; Schuldiner, S.; Sotto, A.; Lavigne, J.P.; Loubet, P. Alternative Approaches for the Management of Diabetic Foot Ulcers. Front. Microbiol 2021, 12, 747618. [Google Scholar] [CrossRef]
- Wassif, R.K.; Elkayal, M.; Shamma, R.N.; Elkheshen, S.A. Recent advances in the local antibiotics delivery systems for management of osteomyelitis. Drug Deliv. 2021, 28, 2392–2414. [Google Scholar] [CrossRef]
- Aswani, V.H.; Shukla, S.K. An Early History of Phage Therapy in the United States: Is it Time to Reconsider? Clin. Med. Res. 2021, 19, 82–89. [Google Scholar] [CrossRef]
- Ribeiro, M.; Ferraz, M.P.; Monteiro, F.J.; Fernandes, M.H.; Beppu, M.M.; Mantione, D.; Sardon, H. Antibacterial silk fibroin/nanohydroxyapatite hydrogels with silver and gold nanoparticles for bone regeneration. Nanomedicine 2017, 13, 231–239. [Google Scholar] [CrossRef]
- Rai, M.; Yadav, A.; Gade, A. Silver nanoparticles as a new generation of antimicrobials. Biotechnol. Adv. 2009, 27, 76–83. [Google Scholar] [CrossRef]
- Chaloupka, K.; Malam, Y.; Seifalian, A.M. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010, 28, 580–588. [Google Scholar] [CrossRef]
- Zhang, Y.; Peng, H.; Huang, W.; Zhou, Y.; Yan, D. Facile preparation and characterization of highly antimicrobial colloid Ag or Au nanoparticles. J. Colloid Interface Sci. 2008, 325, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Badwaik, V.D.; Vangala, L.M.; Pender, D.S.; Willis, C.B.; Aguilar, Z.P.; Gonzalez, M.S.; Paripelly, R.; Dakshinamurthy, R. Size-dependent antimicrobial properties of sugar-encapsulated gold nanoparticles synthesized by a green method. Nanoscale Res. Lett. 2012, 7, 623. [Google Scholar] [CrossRef] [PubMed]
- Li, X.N.; Robinson, S.M.; Gupta, A.; Saha, K.; Jiang, Z.W.; Moyano, D.F.; Sahar, A.; Riley, M.A.; Rotello, V.M. Functional Gold Nanoparticles as Potent Antimicrobial Agents against Multi-Drug-Resistant Bacteria. ACS Nano 2014, 8, 10682–10686. [Google Scholar] [CrossRef] [PubMed]
- Rabiee, N.; Ahmadi, S.; Akhavan, O.; Luque, R. Silver and Gold Nanoparticles for Antimicrobial Purposes against Multi-Drug Resistance Bacteria. Materials 2022, 15, 1799. [Google Scholar] [CrossRef]
- Reddy, K.M.; Feris, K.; Bell, J.; Wingett, D.G.; Hanley, C.; Punnoose, A. Selective toxicity of zinc oxide nanoparticles to prokaryotic and eukaryotic systems. Appl. Phys. Lett. 2007, 90, 213902. [Google Scholar] [CrossRef]
- Azam, A.; Ahmed, A.S.; Oves, M.; Khan, M.S.; Habib, S.S.; Memic, A. Antimicrobial activity of metal oxide nanoparticles against Gram-positive and Gram-negative bacteria: A comparative study. Int. J. Nanomed. 2012, 7, 6003–6009. [Google Scholar] [CrossRef]
- Grenho, L.; Salgado, C.L.; Fernandes, M.H.; Monteiro, F.J.; Ferraz, M.P. Antibacterial activity and biocompatibility of three-dimensional nanostructured porous granules of hydroxyapatite and zinc oxide nanoparticles—An in vitro and in vivo study. Nanotechnology 2015, 26, 315101. [Google Scholar] [CrossRef]
- Spirescu, V.A.; Chircov, C.; Grumezescu, A.M.; Vasile, B.S.; Andronescu, E. Inorganic Nanoparticles and Composite Films for Antimicrobial Therapies. Int. J. Mol. Sci. 2021, 22, 4595. [Google Scholar] [CrossRef]
- Carre, G.; Hamon, E.; Ennahar, S.; Estner, M.; Lett, M.C.; Horvatovich, P.; Gies, J.P.; Keller, V.; Keller, N.; Andre, P. TiO2 Photocatalysis Damages Lipids and Proteins in Escherichia coli. Appl. Environ. Microb. 2014, 80, 2573–2581. [Google Scholar] [CrossRef]
- Kumaravel, V.; Nair, K.M.; Mathew, S.; Bartlett, J.; Kennedy, J.E.; Manning, H.G.; Whelan, B.J.; Leyland, N.S.; Pillai, S.C. Antimicrobial TiO2 nanocomposite coatings for surfaces, dental and orthopaedic implants. Chem. Eng. J. 2021, 416, 129071. [Google Scholar] [CrossRef]
- Abid, S.; Uzair, B.; Niazi, M.B.K.; Fasim, F.; Bano, S.A.; Jamil, N.; Batool, R.; Sajjad, S. Bursting the Virulence Traits of MDR Strain of Candida albicans Using Sodium Alginate-based Microspheres Containing Nystatin-loaded MgO/CuO Nanocomposites. Int. J. Nanomed. 2021, 16, 1157–1174. [Google Scholar] [CrossRef]
- Le Vavasseur, B.; Zeller, V. Antibiotic Therapy for Prosthetic Joint Infections: An Overview. Antibiotics 2022, 11, 486. [Google Scholar] [CrossRef] [PubMed]
- Palumbi, S.R. Humans as the world’s greatest evolutionary force. Science 2001, 293, 1786–1790. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.W.; DeGrado, W.F.; Tew, G.N. De novo designed synthetic mimics of antimicrobial peptides. Curr. Opin. Biotechnol. 2008, 19, 620–627. [Google Scholar] [CrossRef]
- Yount, N.Y.; Yeaman, M.R. Emerging themes and therapeutic prospects for anti-infective peptides. Annu. Rev. Pharmacol. Toxicol. 2012, 52, 337–360. [Google Scholar] [CrossRef] [PubMed]
- Salwiczek, M.; Qu, Y.; Gardiner, J.; Strugnell, R.A.; Lithgow, T.; McLean, K.M.; Thissen, H. Emerging rules for effective antimicrobial coatings. Trends Biotechnol. 2014, 32, 82–90. [Google Scholar] [CrossRef]
- Drexelius, M.G.; Neundorf, I. Application of Antimicrobial Peptides on Biomedical Implants: Three Ways to Pursue Peptide Coatings. Int. J. Mol. Sci. 2021, 22, 13212. [Google Scholar] [CrossRef]
- Auvynet, C.; Rosenstein, Y. Multifunctional host defense peptides: Antimicrobial peptides, the small yet big players in innate and adaptive immunity. FEBS J. 2009, 276, 6497–6508. [Google Scholar] [CrossRef]
- Matsuzaki, K. Control of cell selectivity of antimicrobial peptides. Biochim. Biophys. Acta 2009, 1788, 1687–1692. [Google Scholar] [CrossRef]
- Guani-Guerra, E.; Santos-Mendoza, T.; Lugo-Reyes, S.O.; Teran, L.M. Antimicrobial peptides: General overview and clinical implications in human health and disease. Clin. Immunol. 2010, 135, 1–11. [Google Scholar] [CrossRef]
- Chen, R.; Cole, N.; Willcox, M.D.; Park, J.; Rasul, R.; Carter, E.; Kumar, N. Synthesis, characterization and in vitro activity of a surface-attached antimicrobial cationic peptide. Biofouling 2009, 25, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Kazemzadeh-Narbat, M.; Kindrachuk, J.; Duan, K.; Jenssen, H.; Hancock, R.E.; Wang, R. Antimicrobial peptides on calcium phosphate-coated titanium for the prevention of implant-associated infections. Biomaterials 2010, 31, 9519–9526. [Google Scholar] [CrossRef] [PubMed]
- Kazemzadeh-Narbat, M.; Lai, B.F.; Ding, C.; Kizhakkedathu, J.N.; Hancock, R.E.; Wang, R. Multilayered coating on titanium for controlled release of antimicrobial peptides for the prevention of implant-associated infections. Biomaterials 2013, 34, 5969–5977. [Google Scholar] [CrossRef] [PubMed]
- Amin Yavari, S.; Castenmiller, S.M.; van Strijp, J.A.G.; Croes, M. Combating Implant Infections: Shifting Focus from Bacteria to Host. Adv Mater 2020, 32, e2002962. [Google Scholar] [CrossRef] [PubMed]
- Kalia, V.C.; Patel, S.K.S.; Kang, Y.C.; Lee, J.K. Quorum sensing inhibitors as antipathogens: Biotechnological applications. Biotechnol. Adv. 2019, 37, 68–90. [Google Scholar] [CrossRef]
- Rasmussen, T.B.; Givskov, M. Quorum-sensing inhibitors as anti-pathogenic drugs. Int. J. Med. Microbiol. 2006, 296, 149–161. [Google Scholar] [CrossRef]
- Chen, F.; Gao, Y.; Chen, X.; Yu, Z.; Li, X. Quorum quenching enzymes and their application in degrading signal molecules to block quorum sensing-dependent infection. Int. J. Mol. Sci. 2013, 14, 17477–17500. [Google Scholar] [CrossRef]
- Kaur, S.; Harjai, K.; Chhibber, S. Bacteriophage mediated killing of Staphylococcus aureus in vitro on orthopaedic K wires in presence of linezolid prevents implant colonization. PLoS ONE 2014, 9, e90411. [Google Scholar] [CrossRef]
- Pires, D.P.; Oliveira, H.; Melo, L.D.; Sillankorva, S.; Azeredo, J. Bacteriophage-encoded depolymerases: Their diversity and biotechnological applications. Appl. Microbiol. Biotechnol. 2016, 100, 2141–2151. [Google Scholar] [CrossRef]
- Chan, C.W.; Carson, L.; Smith, G.C.; Morelli, A.; Lee, S. Enhancing the antibacterial performance of orthopaedic implant materials by fibre laser surface engineering. Appl. Surf. Sci. 2017, 404, 67–81. [Google Scholar] [CrossRef]
- Pires, D.P.; Melo, L.; Vilas Boas, D.; Sillankorva, S.; Azeredo, J. Phage therapy as an alternative or complementary strategy to prevent and control biofilm-related infections. Curr. Opin. Microbiol. 2017, 39, 48–56. [Google Scholar] [CrossRef]
- Fish, R.; Kutter, E.; Bryan, D.; Wheat, G.; Kuhl, S. Resolving Digital Staphylococcal Osteomyelitis Using Bacteriophage-A Case Report. Antibiotics 2018, 7, 87. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.; Kelly, N.; Elliott, L.; Grant, A.; Wilkinson, M.; Hazratwala, K.; McEwen, P. Evaluation of Bacteriophage Anti-Biofilm Activity for Potential Control of Orthopedic Implant-Related Infections Caused by Staphylococcus aureus. Surg. Infect. 2019, 20, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Milho, C.; Andrade, M.; Vilas Boas, D.; Alves, D.; Sillankorva, S. Antimicrobial assessment of phage therapy using a porcine model of biofilm infection. Int. J. Pharm. 2019, 557, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Mendes, J.J.; Leandro, C.; Corte-Real, S.; Barbosa, R.; Cavaco-Silva, P.; Melo-Cristino, J.; Gorski, A.; Garcia, M. Wound healing potential of topical bacteriophage therapy on diabetic cutaneous wounds. Wound Repair Regen. 2013, 21, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Cobb, L.H.; Park, J.; Swanson, E.A.; Beard, M.C.; McCabe, E.M.; Rourke, A.S.; Seo, K.S.; Olivier, A.K.; Priddy, L.B. CRISPR-Cas9 modified bacteriophage for treatment of Staphylococcus aureus induced osteomyelitis and soft tissue infection. PLoS ONE 2019, 14, e0220421. [Google Scholar] [CrossRef]
- Gibb, B.P.; Hadjiargyrou, M. Bacteriophage therapy for bone and joint infections. Bone Joint J. 2021, 103-B, 234–244. [Google Scholar] [CrossRef]
- Rotman, S.G.; Sumrall, E.; Ziadlou, R.; Grijpma, D.W.; Richards, R.G.; Eglin, D.; Moriarty, T.F. Local Bacteriophage Delivery for Treatment and Prevention of Bacterial Infections. Front. Microbiol. 2020, 11, 538060. [Google Scholar] [CrossRef]
- Besinis, A.; De Peralta, T.; Handy, R.D. The antibacterial effects of silver, titanium dioxide and silica dioxide nanoparticles compared to the dental disinfectant chlorhexidine on Streptococcus mutans using a suite of bioassays. Nanotoxicology 2014, 8, 1–16. [Google Scholar] [CrossRef]
- Seil, J.T.; Webster, T.J. Antimicrobial applications of nanotechnology: Methods and literature. Int. J. Nanomed. 2012, 7, 2767–2781. [Google Scholar] [CrossRef]
- Hindi, K.M.; Ditto, A.J.; Panzner, M.J.; Medvetz, D.A.; Han, D.S.; Hovis, C.E.; Hilliard, J.K.; Taylor, J.B.; Yun, Y.H.; Cannon, C.L.; et al. The antimicrobial efficacy of sustained release silver-carbene complex-loaded L-tyrosine polyphosphate nanoparticles: Characterization, in vitro and in vivo studies. Biomaterials 2009, 30, 3771–3779. [Google Scholar] [CrossRef] [PubMed]
- Blecher, K.; Nasir, A.; Friedman, A. The growing role of nanotechnology in combating infectious disease. Virulence 2011, 2, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Knetsch, M.L.W.; Koole, L.H. New Strategies in the Development of Antimicrobial Coatings: The Example of Increasing Usage of Silver and Silver Nanoparticles. Polymers 2011, 3, 340–366. [Google Scholar] [CrossRef]
- Higuchi, J.; Klimek, K.; Wojnarowicz, J.; Opalinska, A.; Chodara, A.; Szalaj, U.; Dabrowska, S.; Fudala, D.; Ginalska, G. Electrospun Membrane Surface Modification by Sonocoating with HA and ZnO:Ag Nanoparticles-Characterization and Evaluation of Osteoblasts and Bacterial Cell Behavior In Vitro. Cells 2022, 11, 1582. [Google Scholar] [CrossRef]
- Xiu, Z.M.; Zhang, Q.B.; Puppala, H.L.; Colvin, V.L.; Alvarez, P.J.J. Negligible Particle-Specific Antibacterial Activity of Silver Nanoparticles. Nano Lett. 2012, 12, 4271–4275. [Google Scholar] [CrossRef]
- Rizzello, L.; Pompa, P.P. Nanosilver-based antibacterial drugs and devices: Mechanisms, methodological drawbacks, and guidelines. Chem. Soc. Rev. 2014, 43, 1501–1518. [Google Scholar] [CrossRef]
- Lubick, N. Nanosilver toxicity: Ions, nanoparticles-or both? Environ. Sci. Technol. 2008, 42, 8617. [Google Scholar] [CrossRef]
- Fabrega, J.; Fawcett, S.R.; Renshaw, J.C.; Lead, J.R. Silver Nanoparticle Impact on Bacterial Growth: Effect of pH, Concentration, and Organic Matter. Environ. Sci. Technol. 2009, 43, 7285–7290. [Google Scholar] [CrossRef]
- Liao, C.; Li, Y.; Tjong, S.C. Bactericidal and Cytotoxic Properties of Silver Nanoparticles. Int. J. Mol. Sci. 2019, 20, 449. [Google Scholar] [CrossRef]
- Wani, I.A.; Ahmad, T.; Manzoor, N. Size and shape dependant antifungal activity of gold nanoparticles: A case study of Candida (vol 101, pg 162, 2012). Colloid Surface B 2013, 103, 666. [Google Scholar] [CrossRef]
- Regiel-Futyra, A.; Kus-Liskiewicz, M.; Sebastian, V.; Irusta, S.; Arruebo, M.; Stochel, G.; Kyziol, A. Development of Noncytotoxic Chitosan-Gold Nanocomposites as Efficient Antibacterial Materials. ACS Appl. Mater. Inter. 2015, 7, 1087–1099. [Google Scholar] [CrossRef]
- Yeh, Y.C.; Creran, B.; Rotello, V.M. Gold nanoparticles: Preparation, properties, and applications in bionanotechnology. Nanoscale 2012, 4, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.B.; Zheng, X.; Yan, D.H.; Yin, G.F.; Liao, X.M.; Kang, Y.Q.; Yao, Y.D.; Huang, D.; Hao, B.Q. Toxicological effect of ZnO nanoparticles based on bacteria. Langmuir 2008, 24, 4140–4144. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.L.; Ding, Y.L.; Povey, M.; York, D. ZnO nanofluids—A potential antibacterial agent. Prog. Nat. Sci. Mater. 2008, 18, 939–944. [Google Scholar] [CrossRef]
- Di Bucchianico, S.; Fabbrizi, M.R.; Misra, S.K.; Valsami-Jones, E.; Berhanu, D.; Reip, P.; Bergamaschi, E.; Migliore, L. Multiple cytotoxic and genotoxic effects induced in vitro by differently shaped copper oxide nanomaterials. Mutagenesis 2013, 28, 287–299. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).