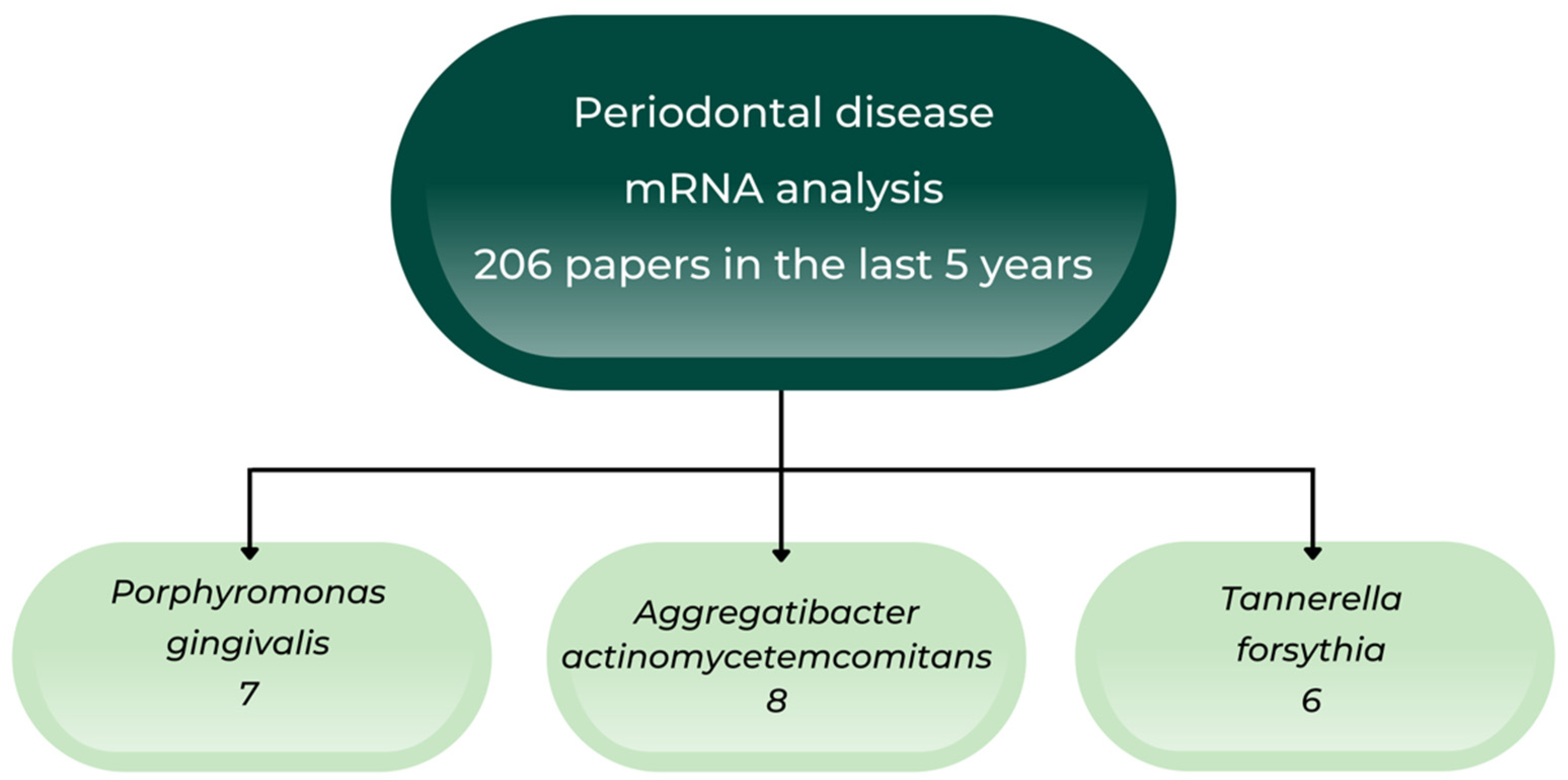
Host mRNA Analysis of Periodontal Disease Patients Positive for Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia
Abstract
:1. Introduction
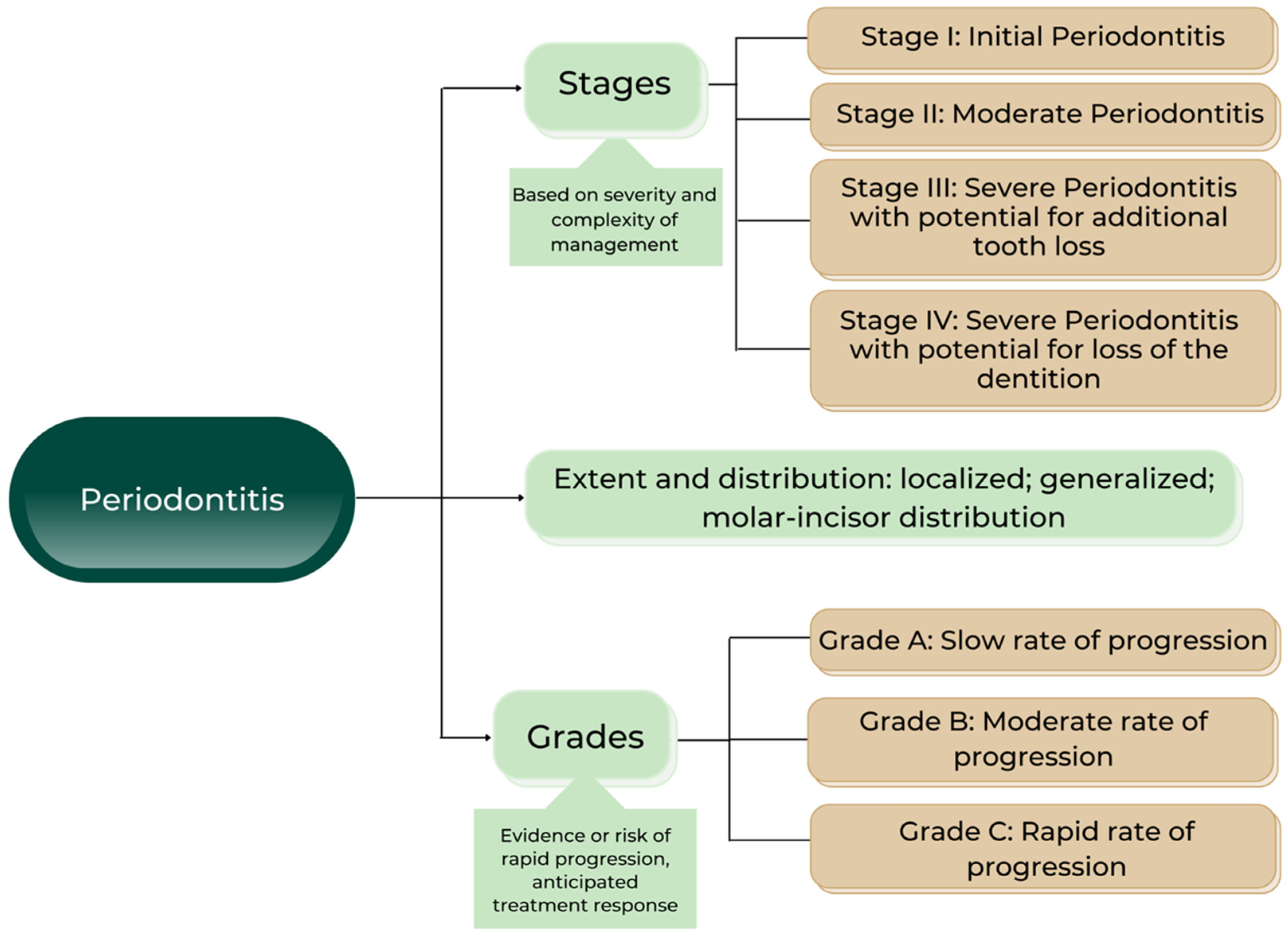
2. Updates in Periodontal Disease Classification
3. Biomarkers Early Detection by mRNA Assays
4. Oral Anaerobic Bacteria and Cancer
5. Circular RNAs Assessing in Periodontal Disease
6. RNA-seq and Periodontal Diseases
7. The Optimal Therapy of Periodontal Diseases
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Luchian, I.; Moscalu, M.; Goriuc, A.; Nucci, L.; Tatarciuc, M.; Martu, I.; Covasa, M. Using Salivary MMP-9 to Successfully Quantify Periodontal Inflammation during Orthodontic Treatment. J. Clin. Med. 2021, 10, 379. [Google Scholar] [CrossRef]
- Luchian, I.; Goriuc, A.; Sandu, D.; Covasa, M. The Role of Matrix Metalloproteinases (MMP-8, MMP-9, MMP-13) in Periodontal and Peri-Implant Pathological Processes. Int. J. Mol. Sci. 2022, 23, 1806. [Google Scholar] [CrossRef]
- Preshaw, P.M.; Seymour, R.A.; Heasman, P.A. Current Concepts in Periodontal Pathogenesis. Dent. Update 2004, 31, 570–572, 574–578. [Google Scholar] [CrossRef]
- Kwon, T.; Lamster, I.B.; Levin, L. Current Concepts in the Management of Periodontitis. Int. Dent. J. 2021, 71, 462–476. [Google Scholar] [CrossRef]
- Bringuier, A.; Khelaifia, S.; Richet, H.; Aboudharam, G.; Drancourt, M. Real-Time PCR Quantification of Methanobrevibacter Oralis in Periodontitis. J. Clin. Microbiol. 2013, 51, 993–994. [Google Scholar] [CrossRef]
- Belkacemi, S.; Mazel, A.; Tardivo, D.; Tavitian, P.; Stephan, G.; Bianca, G.; Terrer, E.; Drancourt, M.; Aboudharam, G. Peri-Implantitis-Associated Methanogens: A Preliminary Report. Sci. Rep. 2018, 8, 9447. [Google Scholar] [CrossRef]
- Ptasiewicz, M.; Grywalska, E.; Mertowska, P.; Korona-Głowniak, I.; Poniewierska-Baran, A.; Niedźwiedzka-Rystwej, P.; Chałas, R. Armed to the Teeth—The Oral Mucosa Immunity System and Microbiota. Int. J. Mol. Sci. 2022, 23, 882. [Google Scholar] [CrossRef]
- Holtfreter, B.; Albandar, J.M.; Dietrich, T.; Dye, B.A.; Eaton, K.A.; Eke, P.I.; Papapanou, P.N.; Kocher, T. Joint EU/USA Periodontal Epidemiology Working Group Standards for Reporting Chronic Periodontitis Prevalence and Severity in Epidemiologic Studies: Proposed Standards from the Joint EU/USA Periodontal Epidemiology Working Group. J. Clin. Periodontol. 2015, 42, 407–412. [Google Scholar] [CrossRef]
- Adel-Khattab, D.; Montero, E.; Herrera, D.; Zhao, D.; Jin, L.; Al-Shaikh, Z.; Renvert, S.; Meyle, J. Evaluation of the FDI Chairside Guide for Assessment of Periodontal Conditions: A Multicentre Observational Study. Int. Dent. J. 2021, 71, 390–398. [Google Scholar] [CrossRef]
- von Bültzingslöwen, I.; Östholm, H.; Gahnberg, L.; Ericson, D.; Wennström, J.L.; Paulander, J. Swedish Quality Registry for Caries and Periodontal Diseases—A Framework for Quality Development in Dentistry. Int. Dent. J. 2019, 69, 361–368. [Google Scholar] [CrossRef] [Green Version]
- Edman, K.; Norderyd, O.; Holmlund, A. Periodontal Health and Disease in an Older Population: A 10-Year Longitudinal Study. Community Dent. Oral Epidemiol. 2022, 50, 225–232. [Google Scholar] [CrossRef]
- Renvert, S.; Berglund, J.S.; Persson, G.R.; Söderlin, M.K. The Association between Rheumatoid Arthritis and Periodontal Disease in a Population-Based Cross-Sectional Case-Control Study. BMC Rheumatol. 2020, 4, 31. [Google Scholar] [CrossRef]
- Jönsson, D.; Orho-Melander, M.; Demmer, R.T.; Engström, G.; Melander, O.; Klinge, B.; Nilsson, P.M. Periodontal Disease Is Associated with Carotid Plaque Area: The Malmö Offspring Dental Study (MODS). J. Intern. Med. 2020, 287, 301–309. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A New Classification Scheme for Periodontal and Peri-Implant Diseases and Conditions—Introduction and Key Changes from the 1999 Classification. J. Periodontol. 2018, 89 (Suppl. 1), S1–S8. [Google Scholar] [CrossRef]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K.; de Sanctis, M.; Ercoli, C.; Fan, J.; et al. Periodontal Manifestations of Systemic Diseases and Developmental and Acquired Conditions: Consensus Report of Workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S219–S229. [Google Scholar] [CrossRef]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Beglundh, T.; Sculean, A.; Tonetti, M.S. EFP Workshop Participants and Methodological Consultants Treatment of Stage I–III Periodontitis-The EFP S3 Level Clinical Practice Guideline. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 4–60. [Google Scholar] [CrossRef]
- Herrera, D.; Sanz, M.; Kebschull, M.; Jepsen, S.; Sculean, A.; Berglundh, T.; Papapanou, P.N.; Chapple, I.; Tonetti, M.S. EFP Workshop Participants and Methodological Consultant Treatment of Stage IV Periodontitis: The EFP S3 Level Clinical Practice Guideline. J. Clin. Periodontol. 2022, 49 (Suppl. 24), 4–71. [Google Scholar] [CrossRef]
- Catalanotto, C.; Cogoni, C.; Zardo, G. MicroRNA in Control of Gene Expression: An Overview of Nuclear Functions. Int. J. Mol. Sci. 2016, 17, 1712. [Google Scholar] [CrossRef]
- Matta, A.; Nader, V.; Lebrin, M.; Gross, F.; Prats, A.-C.; Cussac, D.; Galinier, M.; Roncalli, J. Pre-Conditioning Methods and Novel Approaches with Mesenchymal Stem Cells Therapy in Cardiovascular Disease. Cells 2022, 11, 1620. [Google Scholar] [CrossRef]
- Bonnet-Magnaval, F.; Diallo, L.H.; Brunchault, V.; Laugero, N.; Morfoisse, F.; David, F.; Roussel, E.; Nougue, M.; Zamora, A.; Marchaud, E.; et al. High Level of Staufen1 Expression Confers Longer Recurrence Free Survival to Non-Small Cell Lung Cancer Patients by Promoting THBS1 MRNA Degradation. Int. J. Mol. Sci. 2021, 23, 215. [Google Scholar] [CrossRef]
- Mi, Z.; Zhongqiang, C.; Caiyun, J.; Yanan, L.; Jianhua, W.; Liang, L. Circular RNA Detection Methods: A Minireview. Talanta 2022, 238, 123066. [Google Scholar] [CrossRef]
- Wei, B.; Goyon, A.; Zhang, K. Analysis of Therapeutic Nucleic Acids by Capillary Electrophoresis. J. Pharm. Biomed. Anal. 2022, 219, 114928. [Google Scholar] [CrossRef]
- Kantrong, N.; Buranaphatthana, W.; Hormdee, D.; Suwannarong, W.; Chaichit, R.; Pattanaporn, K.; Klanrit, P.; Krisanaprakornkit, S. Expression of Human Caspase-4 in the Gingival Epithelium Affected with Periodontitis: Its Involvement in Porphyromonas gingivalis-Challenged Gingival Epithelial Cells. Arch. Oral Biol. 2022, 140, 105466. [Google Scholar] [CrossRef]
- Firatli, Y.; Firatli, E.; Loimaranta, V.; Elmanfi, S.; Gürsoy, U.K. Regulation of Gingival Keratinocyte Monocyte Chemoattractant Protein-1-Induced Protein (MCPIP)-1 and Mucosa-Associated Lymphoid Tissue Lymphoma Translocation Protein (MALT)-1 Expressions by Periodontal Bacteria, Lipopolysaccharide and Interleukin-1β. J. Periodontol. 2022. ahead of print. [Google Scholar] [CrossRef]
- Li, D.; Zhu, Y.; Zhang, L.; Shi, L.; Deng, L.; Ding, Z.; Ai, R.; Zhang, X.; He, Y. MZB1 Targeted by MiR-185-5p Inhibits the Migration of Human Periodontal Ligament Cells through NF-κB Signaling and Promotes Alveolar Bone Loss. J. Periodontal. Res. 2022, 57, 811–823. [Google Scholar] [CrossRef]
- Wang, H.; Peng, W.; Zhang, G.; Jiang, M.; Zhao, J.; Zhao, X.; Pan, Y.; Lin, L. Role of PG0192 and PG0193 in the Modulation of Pro-Inflammatory Cytokines in Macrophages in Response to Porphyromonas gingivalis. Eur. J. Oral Sci. 2022, 130, e12851. [Google Scholar] [CrossRef]
- Bekić, M.; Radanović, M.; Đokić, J.; Tomić, S.; Eraković, M.; Radojević, D.; Duka, M.; Marković, D.; Marković, M.; Ismaili, B.; et al. Mesenchymal Stromal Cells from Healthy and Inflamed Human Gingiva Respond Differently to Porphyromonas gingivalis. Int. J. Mol. Sci. 2022, 23, 3510. [Google Scholar] [CrossRef]
- Huang, X.-Y.; Guan, W.-Q. CTHRC1 Expressed in Periodontitis and Human Periodontal Fibroblasts Exposed to Inflammatory Stimuli. Oral Dis. 2022. ahead of print. [Google Scholar] [CrossRef]
- Braun, M.L.; Tomek, M.B.; Grünwald-Gruber, C.; Nguyen, P.Q.; Bloch, S.; Potempa, J.S.; Andrukhov, O.; Schäffer, C. Shut-Down of Type IX Protein Secretion Alters the Host Immune Response to Tannerella Forsythia and Porphyromonas gingivalis. Front. Cell. Infect. Microbiol. 2022, 12, 835509. [Google Scholar] [CrossRef]
- Jia, R.; Shi, R.; Guan, D.; Wu, Y.; Qian, W. Lactobacillus Helveticus Prevents Periodontitis Induced by Aggregatibacter actinomycetemcomitans in Rats by Regulating β-Defensins. Comput. Math. Methods Med. 2022, 2022, 4968016. [Google Scholar] [CrossRef]
- Wang, B.; Bai, S.; Wang, J.; Ren, N.; Xie, R.; Cheng, G.; Yu, Y. TPCA-1 Negatively Regulates Inflammation Mediated by NF-κB Pathway in Mouse Chronic Periodontitis Model. Mol. Oral Microbiol. 2021, 36, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Shiba, F.; Miyauchi, M.; Chea, C.; Furusho, H.; Iwasaki, S.; Shimizu, R.; Ohta, K.; Nishihara, T.; Takata, T. Anti-Inflammatory Effect of Glycyrrhizin with Equisetum Arvense Extract. Odontology 2021, 109, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Pourhajibagher, M.; Bahador, A. Attenuation of Aggregatibacter actinomycetemcomitans Virulence Using Curcumin-Decorated Nanophytosomes-Mediated Photo-Sonoantimicrobial Chemotherapy. Sci. Rep. 2021, 11, 6012. [Google Scholar] [CrossRef]
- Kim, M.-J.; You, Y.-O.; Kang, J.-Y.; Kim, H.-J.; Kang, M.-S. Weissella Cibaria CMU Exerts an Anti-inflammatory Effect by Inhibiting Aggregatibacter actinomycetemcomitans-induced NF-κB Activation in Macrophages. Mol. Med. Rep. 2020, 22, 4143–4150. [Google Scholar] [CrossRef]
- Díaz-Zúñiga, J.; Muñoz, Y.; Melgar-Rodríguez, S.; More, J.; Bruna, B.; Lobos, P.; Monasterio, G.; Vernal, R.; Paula-Lima, A. Serotype b of Aggregatibacter actinomycetemcomitans Triggers Pro-Inflammatory Responses and Amyloid Beta Secretion in Hippocampal Cells: A Novel Link between Periodontitis and Alzheimer´s Disease? J. Oral Microbiol. 2019, 11, 1586423. [Google Scholar] [CrossRef] [PubMed]
- Monasterio, G.; Guevara, J.; Ibarra, J.P.; Castillo, F.; Díaz-Zúñiga, J.; Alvarez, C.; Cafferata, E.A.; Vernal, R. Immunostimulatory Activity of Low-Molecular-Weight Hyaluronan on Dendritic Cells Stimulated with Aggregatibacter actinomycetemcomitans or Porphyromonas gingivalis. Clin. Oral Investig. 2019, 23, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- Engström, M.; Eriksson, K.; Lee, L.; Hermansson, M.; Johansson, A.; Nicholas, A.P.; Gerasimcik, N.; Lundberg, K.; Klareskog, L.; Catrina, A.I.; et al. Increased Citrullination and Expression of Peptidylarginine Deiminases Independently of P. gingivalis and A. actinomycetemcomitans in Gingival Tissue of Patients with Periodontitis. J. Transl. Med. 2018, 16, 214. [Google Scholar] [CrossRef]
- Yun, I.-G.; Ahn, S.-H.; Yoon, W.-J.; Kim, C.S.; Lim, Y.K.; Kook, J.-K.; Jung, S.; Choi, C.-H.; Lee, T.-H. Litsea Japonica Leaf Extract Suppresses Proinflammatory Cytokine Production in Periodontal Ligament Fibroblasts Stimulated with Oral Pathogenic Bacteria or Interleukin-1β. Int. J. Mol. Sci. 2018, 19, 2494. [Google Scholar] [CrossRef]
- Eckert, M.; Mizgalska, D.; Sculean, A.; Potempa, J.; Stavropoulos, A.; Eick, S. In Vivo Expression of Proteases and Protease Inhibitor, a Serpin, by Periodontal Pathogens at Teeth and Implants. Mol. Oral Microbiol. 2018, 33, 240–248. [Google Scholar] [CrossRef]
- Lee, S.-J.; Choi, B.-K. Involvement of NLRP10 in IL-1α Induction of Oral Epithelial Cells by Periodontal Pathogens. Innate Immun. 2017, 23, 569–577. [Google Scholar] [CrossRef]
- Ran, S.; Liu, B.; Gu, S.; Sun, Z.; Liang, J. Analysis of the Expression of NLRP3 and AIM2 in Periapical Lesions with Apical Periodontitis and Microbial Analysis Outside the Apical Segment of Teeth. Arch. Oral Biol. 2017, 78, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Willi, M.; Belibasakis, G.N.; Bostanci, N. Expression and Regulation of Triggering Receptor Expressed on Myeloid Cells 1 in Periodontal Diseases. Clin. Exp. Immunol. 2014, 178, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Ursu, R.G.; Luchian, I.; Ghetu, N.; Costan, V.V.; Stamatin, O.; Palade, O.D.; Damian, C.; Iancu, L.S.; Porumb-Andrese, E. Emerging Oncogenic Viruses in Head and Neck Cancers from Romanian Patients. Appl. Sci. 2021, 11, 9356. [Google Scholar] [CrossRef]
- Han, Y.W. Fusobacterium nucleatum: A Commensal-Turned Pathogen. Curr. Opin. Microbiol. 2015, 23, 141–147. [Google Scholar] [CrossRef]
- Castellarin, M.; Warren, R.L.; Freeman, J.D.; Dreolini, L.; Krzywinski, M.; Strauss, J.; Barnes, R.; Watson, P.; Allen-Vercoe, E.; Moore, R.A.; et al. Fusobacterium nucleatum Infection Is Prevalent in Human Colorectal Carcinoma. Genome Res. 2012, 22, 299–306. [Google Scholar] [CrossRef]
- Kostic, A.D.; Gevers, D.; Pedamallu, C.S.; Michaud, M.; Duke, F.; Earl, A.M.; Ojesina, A.I.; Jung, J.; Bass, A.J.; Tabernero, J.; et al. Genomic Analysis Identifies Association of Fusobacterium with Colorectal Carcinoma. Genome Res. 2012, 22, 292–298. [Google Scholar] [CrossRef]
- Zhang, X.; Zhu, X.; Cao, Y.; Fang, J.-Y.; Hong, J.; Chen, H. Fecal Fusobacterium nucleatum for the Diagnosis of Colorectal Tumor: A Systematic Review and Meta-Analysis. Cancer Med. 2019, 8, 480–491. [Google Scholar] [CrossRef]
- Guo, S.; Li, L.; Xu, B.; Li, M.; Zeng, Q.; Xiao, H.; Xue, Y.; Wu, Y.; Wang, Y.; Liu, W.; et al. A Simple and Novel Fecal Biomarker for Colorectal Cancer: Ratio of Fusobacterium nucleatum to Probiotics Populations, Based on Their Antagonistic Effect. Clin. Chem. 2018, 64, 1327–1337. [Google Scholar] [CrossRef]
- Osman, M.A.; Neoh, H.-M.; Mutalib, N.-S.A.; Chin, S.-F.; Mazlan, L.; Raja Ali, R.A.; Zakaria, A.D.; Ngiu, C.S.; Ang, M.Y.; Jamal, R. Parvimonas micra, Peptostreptococcus stomatis, Fusobacterium nucleatum and Akkermansia muciniphila as a Four-Bacteria Biomarker Panel of Colorectal Cancer. Sci. Rep. 2021, 11, 2925. [Google Scholar] [CrossRef]
- Ghosh, S.K.; Weinberg, A. When Mr. Fap Meets the Gals. Cell Host Microbe 2016, 20, 125–126. [Google Scholar] [CrossRef] [Green Version]
- Coppenhagen-Glazer, S.; Sol, A.; Abed, J.; Naor, R.; Zhang, X.; Han, Y.W.; Bachrach, G. Fap2 of Fusobacterium nucleatum Is a Galactose-Inhibitable Adhesin Involved in Coaggregation, Cell Adhesion, and Preterm Birth. Infect. Immun. 2015, 83, 1104–1113. [Google Scholar] [CrossRef] [PubMed]
- Parhi, L.; Abed, J.; Shhadeh, A.; Alon-Maimon, T.; Udi, S.; Ben-Arye, S.L.; Tam, J.; Parnas, O.; Padler-Karavani, V.; Goldman-Wohl, D.; et al. Placental Colonization by Fusobacterium nucleatum Is Mediated by Binding of the Fap2 Lectin to Placentally Displayed Gal-GalNAc. Cell Rep. 2022, 38, 110537. [Google Scholar] [CrossRef] [PubMed]
- Parhi, L.; Alon-Maimon, T.; Sol, A.; Nejman, D.; Shhadeh, A.; Fainsod-Levi, T.; Yajuk, O.; Isaacson, B.; Abed, J.; Maalouf, N.; et al. Breast Cancer Colonization by Fusobacterium nucleatum Accelerates Tumor Growth and Metastatic Progression. Nat. Commun. 2020, 11, 3259. [Google Scholar] [CrossRef] [PubMed]
- Kunzmann, A.T.; Proença, M.A.; Jordao, H.W.; Jiraskova, K.; Schneiderova, M.; Levy, M.; Liska, V.; Buchler, T.; Vodickova, L.; Vymetalkova, V.; et al. Fusobacterium nucleatum Tumor DNA Levels Are Associated with Survival in Colorectal Cancer Patients. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1891–1899. [Google Scholar] [CrossRef]
- Yamamura, K.; Izumi, D.; Kandimalla, R.; Sonohara, F.; Baba, Y.; Yoshida, N.; Kodera, Y.; Baba, H.; Goel, A. Intratumoral Fusobacterium nucleatum Levels Predict Therapeutic Response to Neoadjuvant Chemotherapy in Esophageal Squamous Cell Carcinoma. Clin. Cancer Res. 2019, 25, 6170–6179. [Google Scholar] [CrossRef]
- Luchian, I.; Goriuc, A.; Martu, M.A.; Covasa, M. Clindamycin as an Alternative Option in Optimizing Periodontal Therapy. Antibiotics 2021, 10, 814. [Google Scholar] [CrossRef]
- Zheng, D.-W.; Dong, X.; Pan, P.; Chen, K.-W.; Fan, J.-X.; Cheng, S.-X.; Zhang, X.-Z. Phage-Guided Modulation of the Gut Microbiota of Mouse Models of Colorectal Cancer Augments Their Responses to Chemotherapy. Nat. Biomed. Eng. 2019, 3, 717–728. [Google Scholar] [CrossRef]
- Deng, W.; Wang, X.; Zhang, J.; Zhao, S. Circ_0138959/MiR-495-3p/TRAF6 Axis Regulates Proliferation, Wound Healing and Osteoblastic Differentiation of Periodontal Ligament Cells in Periodontitis. J. Dent. Sci. 2022, 17, 1125–1134. [Google Scholar] [CrossRef]
- Wang, L.; Li, Y.; Hong, F.; Ning, H. Circ_0062491 Alleviates LPS-Induced Apoptosis and Inflammation in Periodontitis by Regulating MiR-498/SOCS6 Axis. Innate Immun. 2022, 28, 174–184. [Google Scholar] [CrossRef]
- Li, Q.; Hu, Z.; Yang, F.; Peng, Y. Circ_0066881 Targets MiR-144-5p/RORA Axis to Alleviate LPS-Induced Apoptotic and Inflammatory Damages in Human Periodontal Ligament Cells. Innate Immun. 2022, 28, 164–173. [Google Scholar] [CrossRef]
- Yu, W.; Gu, Q.; Wu, D.; Zhang, W.; Li, G.; Lin, L.; Lowe, J.M.; Hu, S.; Li, T.W.; Zhou, Z.; et al. Identification of Potentially Functional CircRNAs and Prediction of CircRNA-MiRNA-MRNA Regulatory Network in Periodontitis: Bridging the Gap between Bioinformatics and Clinical Needs. J. Periodontal. Res. 2022, 57, 594–614. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, C.; Zhu, C.; Ye, W.; Gu, Q.; Shu, C.; Feng, X.; Chen, X.; Zhang, W.; Shan, T. Redondoviridae Infection Regulates CircRNAome in Periodontitis. J. Med. Virol. 2022, 94, 2537–2547. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhang, Z.; Li, Y.; Wang, Z. Abnormal Hsa_circ_0003948 Expression Affects Chronic Periodontitis Development by Regulating MiR-144-3p/NR2F2/PTEN Signaling. J. Periodontal. Res. 2022, 57, 316–323. [Google Scholar] [CrossRef]
- Du, W.; Wang, L.; Liao, Z.; Wang, J. Circ_0085289 Alleviates the Progression of Periodontitis by Regulating Let-7f-5p/SOCS6 Pathway. Inflammation 2021, 44, 1607–1619. [Google Scholar] [CrossRef] [PubMed]
- Jiao, K.; Walsh, L.J.; Ivanovski, S.; Han, P. The Emerging Regulatory Role of Circular RNAs in Periodontal Tissues and Cells. Int. J. Mol. Sci. 2021, 22, 4636. [Google Scholar] [CrossRef]
- Teles, F.; Wang, Y.; Hajishengallis, G.; Hasturk, H.; Marchesan, J.T. Impact of Systemic Factors in Shaping the Periodontal Microbiome. Periodontology 2000 2021, 85, 126–160. [Google Scholar] [CrossRef]
- Chen, X.; Sun, B.; Li, L.; Sun, Z.; Zhu, X.; Zhong, X.; Xu, Y. The Oral Microbiome Analysis Reveals the Similarities and Differences between Periodontitis and Crohn’s Disease-Associated Periodontitis. FEMS Microbiol. Lett. 2022, 369, fnac054. [Google Scholar] [CrossRef]
- Ge, D.; Wang, F.; Hu, Y.; Wang, B.; Gao, X.; Chen, Z. Fast, Simple, and Highly Specific Molecular Detection of Porphyromonas gingivalis Using Isothermal Amplification and Lateral Flow Strip Methods. Front. Cell. Infect. Microbiol. 2022, 12, 895261. [Google Scholar] [CrossRef]
- Jiang, Y.; Song, B.; Brandt, B.W.; Cheng, L.; Zhou, X.; Exterkate, R.A.M.; Crielaard, W.; Deng, D.M. Comparison of Red-Complex Bacteria between Saliva and Subgingival Plaque of Periodontitis Patients: A Systematic Review and Meta-Analysis. Front. Cell. Infect. Microbiol. 2021, 11, 727732. [Google Scholar] [CrossRef]
- Chang, C.; Geng, F.; Shi, X.; Li, Y.; Zhang, X.; Zhao, X.; Pan, Y. The Prevalence Rate of Periodontal Pathogens and Its Association with Oral Squamous Cell Carcinoma. Appl. Microbiol. Biotechnol. 2019, 103, 1393–1404. [Google Scholar] [CrossRef]
- Ursu, R.G.; Danciu, M.; Spiridon, I.A.; Ridder, R.; Rehm, S.; Maffini, F.; McKay-Chopin, S.; Carreira, C.; Lucas, E.; Costan, V.-V.; et al. Role of Mucosal High-Risk Human Papillomavirus Types in Head and Neck Cancers in Romania. PLoS ONE 2018, 13, e0199663. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Wu, T.; Xu, X.; Chen, D.; Mo, A.; Lei, Y.; Cheng, L.; Man, Y.; Zhou, X.; Wang, Y.; et al. Smoking May Lead to Marginal Bone Loss Around Non-Submerged Implants during Bone Healing by Altering Salivary Microbiome: A Prospective Study. J. Periodontol. 2017, 88, 1297–1308. [Google Scholar] [CrossRef] [PubMed]
- Lundmark, A.; Hu, Y.O.O.; Huss, M.; Johannsen, G.; Andersson, A.F.; Yucel-Lindberg, T. Identification of Salivary Microbiota and Its Association with Host Inflammatory Mediators in Periodontitis. Front. Cell. Infect. Microbiol. 2019, 9, 216. [Google Scholar] [CrossRef]
- Moreno, C.; Bybee, E.; Tellez Freitas, C.M.; Pickett, B.E.; Weber, K.S. Meta-Analysis of Two Human RNA-Seq Datasets to Determine Periodontitis Diagnostic Biomarkers and Drug Target Candidates. Int. J. Mol. Sci. 2022, 23, 5580. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C.; Pico, A.; Dopico, J.; Gándara, P.; Blanco, J.; Liñares, A. Adjunctive Benefits of Systemic Metronidazole on Non-Surgical Treatment of Peri-Implantitis. A Randomized Placebo-Controlled Clinical Trial. J. Clin. Periodontol. 2022, 49, 15–27. [Google Scholar] [CrossRef]
- Teles, F.R.F.; Lynch, M.C.; Patel, M.; Torresyap, G.; Martin, L. Bacterial Resistance to Minocycline after Adjunctive Minocycline Microspheres during Periodontal Maintenance: A Randomized Clinical Trial. J. Periodontol. 2021, 92, 1222–1231. [Google Scholar] [CrossRef]
- Cosgarea, R.; Eick, S.; Jepsen, S.; Arweiler, N.B.; Juncar, R.; Tristiu, R.; Salvi, G.E.; Heumann, C.; Sculean, A. Microbiological and Host-Derived Biomarker Evaluation Following Non-Surgical Periodontal Therapy with Short-Term Administration of Systemic Antimicrobials: Secondary Outcomes of an RCT. Sci. Rep. 2020, 10, 16322. [Google Scholar] [CrossRef]
- Cha, J.K.; Lee, J.S.; Kim, C.S. Surgical Therapy of Peri-Implantitis with Local Minocycline: A 6-Month Randomized Controlled Clinical Trial. J. Dent. Res. 2019, 98, 288–295. [Google Scholar] [CrossRef]
- Lockhart, P.B.; Tampi, M.P.; Abt, E.; Aminoshariae, A.; Durkin, M.J.; Fouad, A.F.; Gopal, P.; Hatten, B.W.; Kennedy, E.; Lang, M.S.; et al. Evidence-Based Clinical Practice Guideline on Antibiotic Use for the Urgent Management of Pulpal- and Periapical-Related Dental Pain and Intraoral Swelling: A Report from the American Dental Association. J. Am. Dent. Assoc. 2019, 150, 906–921.e12. [Google Scholar] [CrossRef] [Green Version]

| Authors Year, Country | Sample Type | mRNA Analysis Assay | Results | Novelty |
|---|---|---|---|---|
| Kantrong N et al., 2022, Khon Kaen, Thailand [23] | Gingival biopsies, healthy participants with periodontitis or clinically healthy gingiva | mRNA expressions/RT-qPCR of human β-defensin-2 (hBD-2), interleukin (IL-) 8, and IL-18 in stimulated GECs in the presence or absence of a caspase-4 inhibitor | mRNA upregulations of hBD-2, IL-8, and IL-18 upon P. gingivalis stimulation were significantly reduced by caspase-4 inhibition (p < 0.05), while, for F. nucleatum, the inhibitor did not exhibit the same suppressor activity | Caspase-4 activation in P. gingivalis-infected GECs showed an upregulation of immune effector molecules, suggesting a possible detection mechanism of caspase-4 in GECs in periodontal disease pathogenesis |
| Firatli Y et al., 2022, Turku, Finland [24] | Human gingival keratinocyte (HMK) monolayers were incubated with P. gingivalis, F. nucleatum, P. gingivalis LPS and IL-1β. | Immunoblots and mRNA levels by qPCR for protein levels of MCPIP-1 and MALT-1 | MCPIP-1 mRNA levels were increased by P. gingivalis, F. nucleatum, and IL-1β, but no change was detected in MALT-1 mRNA levels | - Infection and inflammatory mediators regulate the gingival keratinocyte MCPIP-1 and MALT-1 mRNA and protein expression responses. - Periodontitis-associated bacteria-induced modifications in MCPIP-1 and MALT-1 responses can be a part of periodontal disease pathogenesis |
| Li D et al., 2022, Chongqing, China [25] | human gingival tissues | Dual-luciferase reporter assay, which assessed the binding of miR-185-5p to MZB1 (ER-localized protein) | MZB1 was markedly increased in the gingival tissues of periodontitis patients, in mouse models, and in the hPDLCs treated with lipopolysaccharide of P. gingivalis (LPS-PG) | MZB1 (a target gene of miR-185-5p) plays an important role in inhibiting the migration of hPDLCs through NF-κB signaling pathway and deteriorating alveolar bone loss |
| Wang H wr al., 2022, Shenyang, Liaoning Province, China [26] | the effects of the P. gingivalis outer membrane protein OmpH (encoded by PG0192 and PG0193) on IL-6 and tumor necrosis factor-α (TNF-α) expression in macrophages to assess the pro-inflammatory cytokine responses | Macrophages treated with mutant strains (PG0192-PG0193 deletion) showed a downregulation in the expression of IL-6 and TNF-α at mRNA and protein levels | IL-6 and TNF-α mRNA levels were up-regulated following treatment of macrophages with P. gingivalis W83 co-incubated with rOmpH-1 or rOmpH-2 | - The roles of PG0192 and PG0193 in promoting IL-6 and TNF-α expression in macrophages exposed to P. gingivalis - Involvement of C5aR in the pro-inflammatory response |
| Bekić M et al., 2022, Belgrade, Serbia [27] | 10 H-GMSC and 12 P-GMSC lines | P. gingivalis up-regulated the mRNA expression of IL-6, IL-8, MCP-1, GRO-α, RANTES, TLR-2, HIF-1α, OPG, MMP-3, SDF-1, HGF and IP-10 in P-GMSCs, while only IL-6, MCP-1 and GRO-α were up-regulated in H-GMSCs. | P-GMSCs had a significantly higher expression of MCP-1, RANTES, IP-10 and HGF compared to H-GMSCs, but IDO1 was lower | Cultures of P-GMSCs retain their pro-inflammatory properties, while exhibiting lower immunosuppressive potential than their healthy counterparts, and reduced regeneration-associated gene induction in culture. All these functions are positively influenced by P. gingivalis treatment |
| Huang XY et al., 2022, Fuzhou, China [28] | gingival tissue samples from clinically healthy subjects (15 cases) and patients with periodontitis (30 cases) | mRNA levels of the intracellular collagen triple helix repeat containing-1 (CTHRC1) and protein expression of the extracellular CTHRC1 | In the periodontitis group, protein expression of CTHRC1 was higher than that of the clinically healthy group | - CTHRC1 might play a role in the development of periodontitis - Expression level might be significantly correlated with the stimulation produced by P. gingivalis LPS on fibroblasts |
| Braun ML et al., 2022, Vienna, Austria [29] | wild-type T. forsythia and P. gingivalis and T9SS signal peptidase-deficient mutants defective in protein secretion were used to stimulate human macrophages and gingival fibroblasts | mRNA expression levels of the pro-inflammatory mediators IL-6, IL-8, MCP-1 and TNF-α by qPCR | - 16 h post-stimulation, the T. forsythia T9SS mutant induced a significantly lower production of cytokines and the chemokine in cells compared to the corresponding wild-type strain - The opposite was noted for the P. gingivalis T9SS mutant | - T9SS shut-down translates into an altered inflammatory response towards periodontal pathogens - T9SS needs further evaluation as a potential novel target for periodontal therapy |
| Authors Year, Country | Sample Type | mRNA Analysis Assay | Results | Novelty |
|---|---|---|---|---|
| Jia R et al., 2022 Shanghai, China [30] | Gingival tissues of eighteen 8-week-old female rats were randomly distributed into three groups: Sham group, Trehalose group and Lactobacillus helveticus SBT2171 (LH2171) group | Expression of β-defensins, TNF-α IL-1β and IL-6 and the number of A. actinomycetemcomitans in rat gingival tissues by qRT PCR | mRNA level expression and release of inflammatory factors in the tissue samples in the LH2171 group were notably lower than those in the Trehalose group | L. helveticus improves alveolar bone resorption, increases the expression of β-defensins, inhibits the number of A. actinomycetemcomitans and prevents periodontitis |
| Wang B et al., 2021, Shaanxi, China [31] | - Mouse chronic periodontitis was induced by an in vivo ligature-induced periodontitis model - TPCA-1 (2-[(aminocarbonyl)amino]-5-(4-fluorophenyl)-3-thiophenecarboxamide (TPCA-1) is a IκB kinases (IKK) inhibitor) was intravenously injected into mice after chronic periodontitis induction | mRNA levels by qRT-PCR | - A. actinomycetemcomitans -induced expression of pro-inflammatory cytokines was inhibited in vitro by TPCA-1 treatment - NF-κB signal activation in osteoclasts | Treatment with TPCA-1 downregulates inflammation response and inhibits the osteoclastogenesis through - The inactivation of NF-κB pathway in chronic periodontitis mice model |
| Shiba F et al., 2021, Hyogo, Japan [32] | Effects of extracts from six different plants on Glycyrrhizin (GL)-suppressed TNF-α expression in A. actinomycetemcomitans -LPS-stimulated human oral keratinocytes (RT7) | At both mRNA and protein levels, Equisetum arvense (EA) extract had the strongest additive effect on the suppression of TNF-α by GL | LPS-induced periodontitis rat model showed that GL with EA supplementation significantly decreased TNF-α mRNA levels in the gingival tissue | GL and EA combination may improve the development of new oral hygiene products with the purpose of enhancing periodontal health |
| Pourhajibagher M et al., 2021, Tehran, Iran [33] | Curcumin-decorated nanophytosomes (Cur-NPhs) as a novel photo-sonosensitizer | Cur-NPhs-PSACT (photo-sonodynamic antimicrobial chemotherapy), the antimicrobial activities of Cur-NPhs against A. actinomycetemcomitans were investigated by analyzing cell viability, biofilm killing/degradation capacity, metabolic activity, expression of quorum-sensing-associated qseB and qseC genes, and biofilm-associated rcpA gene | The antimicrobial effect of Cur-NPhs-PSACT was dose-dependent | - Cur-NPhs-PSACT had antimicrobial activity against A. actinomycetemcomitans by decreasing the expression of virulence genes - Cur-NPhs attenuate this bacterium, potentially decreasing periodontal disease severity in patients |
| Kim MJ et al., 2020, Jellabukdo, Republic of Korea [34] | Anti-inflammatory effects of live oraCMU (Weissella cibaria CMU) against stimulation with the formalin-inactivated periodontal pathogen Aggregatibacter actinomycetemcomitans in RAW 264.7 macrophages | mRNA expression of proinflammatory cytokines such as IL1β and IL6 was assessed by qRT PCR | In A. actinomycetemcomitans-stimulated RAW 264.7 macrophages (Cell culture, The RAW 264.7 macrophage line (TIB-71, ATCC)), oraCMU reduced nitric oxide production by suppressing iNOS expression and downregulating the proinflammatory cytokines mRNA expression of in a dose-dependent manner. | Probiotic oraCMU showed anti-inflammatory activity associated with the inhibition of NF-κB signal activation in response to periodontal pathogens |
| Díaz-Zúñiga J et al., 2019, Santiago, Chile [35] | Effects of purified LPS, from serotypes a, b or c of A. actinomycetemcomitans, on primary cultures of microglia or mixed hippocampal cells | Cultures treated with serotype a-LPS displayed increased mRNA levels of the IL-4 and IL-10 modulatory cytokines | LPS from different A. actinomycetemcomitans serotypes triggers discriminatory immune responses, which differentially affect primary hippocampal cells | Serotype b-LPS treatment triggers the secretion of proinflammatory cytokines by microglia, induces neurite shrinking, and increases the extracellular Aβ1-42 levels, all features strongly associated with the etiology of Alzheimer’s disease. |
| Monasterio G et al., 2019, Santiago, Chile. [36] | Dendritic cells (DCs) play a central role in the host’s immune response during periodontitis; thus, this study aimed to analyze whether low-molecular-weight hyalurona (LMW-HA) has an immunostimulatory activity on DCs when stimulated with bacteria involved in periodontitis. | LMW-HA-treated and non-treated DCs were stimulated with A. actinomycetemcomitans or P. gingivalis and the mRNA expression for cytokines TNF- α, IL-1B, IL-6, and IL-23A was quantified by RT-qPCR | Higher expression levels of TNF-α, IL-1B, IL-6, and IL-23A were detected in DCs treated with LMW-HA after bacterial infection, as compared with non-treated DCs | LMW-HA plays an immunostimulatory role on the immune response triggered by DCs during infection with A. actinomycetemcomitans or P. gingivalis |
| Engström M et al., 2018, Stockholm, Sweden [37] Karolinska Institutet | Gingival tissue biopsy samples were obtained from 15 patients with periodontitis and 15 individuals with no periodontal disease. The presence of citrullinated proteins and expression of endogenous peptidylarginine deiminases (PAD2 and PAD4), in periodontal tissue of individuals with periodontitis and healthy controls, in relation to the periodontal pathogens P. gingivalis and A. actinomycetemcomitans | There was an increased staining of the citrullinating enzymes PAD2 and PAD4 in gingival connective tissue of patients with periodontitis, while similar levels of PAD2 and PAD4 were observed in the gingival epithelium of the two groups. Similarly, the mRNA expression of PADI2 and PADI4 were also increased in the gingival tissue samples of patients with periodontitis compared to the healthy group. | P. gingivalis and leukotoxins was comparable in both epithelium and connective tissue of the two groups | - Chronic gingival inflammation is associated with an increased local citrullination and PAD2 and PAD4 expression in periodontitis - The presence of P. gingivalis and A. actinomycetemcomitans leukotoxin were not connected, however, to the increased citrullination and PAD2 and PAD4 expression in periodontitis These two periodontitis pathogens have been suggested to be linked to anti-citrullinated protein antibodies in patients with rheumatoid arthritis |
| Authors Year, Country | Sample Type | mRNA Analysis Assay | Results | Novelty |
|---|---|---|---|---|
| Braun ML et al., 2022, Vienna, Austria [29] | Wild-type T. forsythia and P. gingivalis and T9SS signal peptidase-deficient mutants defective in protein secretion were used to stimulate human macrophages and gingival fibroblasts | mRNA expression levels of the pro-inflammatory mediators IL-6, IL-8, MCP-1 and TNF-α by qPCR | T9SS shutdown translates into an altered inflammatory response in periodontal pathogens | T9SS as a potential novel target for periodontal therapy needs further evaluation |
| Yun IG et al., 2018, Gwangju, Korea [38] | The ability of Litsea japonica leaf extract (LJLE) to inhibit pro-inflammatory cytokine production in PDLFs in response to various stimulants | mRNA and protein expression | Anti-inflammatory effect of LJLE in PDLFs after infection with various oral bacteria, including F. nucleatum, P. gingivalis, Treponema denticola, and T. forsythia | LJLE has anti-inflammatory activity that could be exploited to control inflammation in human periodontitis |
| Eckert M et al., 2018, Bern, Switzerland [39] | Biofilm and gingival crevicular fluid (GCF)/ peri-implant sulcular fluid (PISF) samples were taken from 10 healthy tooth and implant sites, 12 gingivitis and mucositis sites, and 10 periodontitis and peri-implantitis sites | mRNA expression of individual genes | Gingipains’ expression level was associated with the levels of miropin and certain T. forsythia proteases around teeth but not implants | KLIKK-proteases, especially miropin, might be involved in the pathogenesis of both periodontal and peri-implant diseases |
| Lee SJ et al., 2017, Seoul, Korea [40] | The human oral epithelial cell line HOK-16B was infected T. forsythia and F. nucleatum, at various MOIs | RT-PCR and immunoblotting assays for mRNA and protein expression | Infection increased mRNA and protein expression of NLRP10, respectively NLRP10 is involved in activating the ERK signaling pathway in HOK-16B cells infected with T. forsythia and F. nucleatum | Pro-inflammatory cytokine IL-1α levels are augmented by the activation of the ERK pathway, which may play a critical role in periodontitis |
| Ran S et al., 2017, Shanghai, China [41] | Periapical lesions | mRNA levels of apoptosis-associated speck-like protein (ASC), caspase-1IL-1β, NLRP3 and AIM2 in THP-1-derived macrophages treated with Porphyromonas LPS were quantified by real-time PCR | Up-regulation of NLRP3 mRNA was correlated with a simultaneous up-regulation of caspase-1 mRNA in most samples | NLRP3 and AIM2 proteins are involved in the pathogenesis of periapical periodontitis. Anaerobes, such as P. endodontalis, P. gingivalis, F. nucleatum and T. forsythia, were the most important microbial stimuli that might activate inflammasomes in periapical tissues |
| Willi M et al., 2014, Zürich, Switzerland [42] | Gingival tissue | TREM-1 mRNA expression | TREM-1 expression was found to be increased in both aggressive and chronic periodontitis, compared to healthy tissues, and correlated with the levels of the ‘red complex’ species in the tissue | TREM-1 tissue expression is up-regulated in periodontal disease and correlates with the level of periodontal pathogens |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ursu, R.G.; Iancu, L.S.; Porumb-Andrese, E.; Damian, C.; Cobzaru, R.G.; Nichitean, G.; Ripa, C.; Sandu, D.; Luchian, I. Host mRNA Analysis of Periodontal Disease Patients Positive for Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia. Int. J. Mol. Sci. 2022, 23, 9915. https://doi.org/10.3390/ijms23179915
Ursu RG, Iancu LS, Porumb-Andrese E, Damian C, Cobzaru RG, Nichitean G, Ripa C, Sandu D, Luchian I. Host mRNA Analysis of Periodontal Disease Patients Positive for Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia. International Journal of Molecular Sciences. 2022; 23(17):9915. https://doi.org/10.3390/ijms23179915
Chicago/Turabian StyleUrsu, Ramona Gabriela, Luminita Smaranda Iancu, Elena Porumb-Andrese, Costin Damian, Roxana Gabriela Cobzaru, Giorgio Nichitean, Carmen Ripa, Darius Sandu, and Ionut Luchian. 2022. "Host mRNA Analysis of Periodontal Disease Patients Positive for Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia" International Journal of Molecular Sciences 23, no. 17: 9915. https://doi.org/10.3390/ijms23179915
APA StyleUrsu, R. G., Iancu, L. S., Porumb-Andrese, E., Damian, C., Cobzaru, R. G., Nichitean, G., Ripa, C., Sandu, D., & Luchian, I. (2022). Host mRNA Analysis of Periodontal Disease Patients Positive for Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia. International Journal of Molecular Sciences, 23(17), 9915. https://doi.org/10.3390/ijms23179915








