1. Introduction
Polyester (PET) vascular prostheses, usually named Dacron
R grafts, are nowadays widely used in reconstructive vascular surgery. Over the period of 60 years, since their first implantations in humans, in 50th ties of the last century [
1], the polyester grafts have undergone multiple biochemical modifications to make them more and more safe and effective for applications in vascular patients. One of the most crucial modifications was related to blood sealing properties of PET tubes, which resulted in albumin- or collagen-sealed PET grafts [
2,
3]. This specific modification is now present in the majority of PET vascular grafts available on the market, with prevalence of the collagen coating, which has been found to be optimal. Impregnation with collagen makes the PET prosthesis non-permeable for blood and thus ready for implantation without any previous preparation procedures as so-called pre-clotting of unsealed PET prostheses. Collagen is not only compatible with synthetic polymers but also non-toxic, hemostatic, biodegradable and highly susceptible to various modifications. This last feature allows one to control the collagen degradation rate (via cross-linking with formaldehyde, glutaraldehyde, carbodiimide, acylazide, examethylenediisocyanate etc.) and offers a platform to synthesize a variety of collagen-based systems for drug delivery (including vancomycin, trimethoprim, amphotericin-B, gentamycin, polymyxin-B sulfate and tobramycin) [
4,
5,
6]. This made collagen coating a milestone in reconstructive vascular surgery.
However, the problem of early or late infection of vascular prostheses still remains the Achilles’ heel of modern vascular surgery. Vascular graft infection occurs in 0.6 to 5% of patients after reconstructions in aorto-iliac level. Mortality in this group is estimated to be between 25–88% [
7]. Moreover, 40–70% of the patients will undergo major amputation [
8]. To reduce this problem, silver- and rifampicin-bounded grafts were produced and they became the most frequently used collagen-coated grafts. However, they are definitely not the final solution for this serious and possibly lethal outcome complication [
9]. The rate of re-infections of silver coated grafts in the femoral-popliteal segment is reported to be 19% [
10]. Continuity of infection and bacterial resistance was found in 31% of patients after replacement of infected vascular graft with rifampicin coated prostheses [
11]. Therefore, there is still a strong clinical need for further attempts at biochemical modification of PET vascular prostheses in order to create a product which could be maximally resistant to early or late vascular graft infection.
In the quest for the solution to this problem, one should remember that collagen must be treated with care to retain its natural properties. Its native triple helix conformation is maintained at low temperatures (30–40 °C) [
12], and strong alkaline pH may cause its disturbance in restoration of thick fibril-bundle structures [
13] while acidic pH may cause collagen dissolution. Therefore, mild collagen modification conditions must be selected to bind antibacterial factors. In 2007, a new method to deposit a multifunctional polydopamine polymer on various substrates through simple dip-coating in aqueous dopamine (compound of catecholamine family) solution was reported [
14]. Since then, the described method has attracted growing attention, not only due to the feasibility of coating deposition but also to its multifunctionality [
15]. Among others, polydopamine (PDA) can be a platform (due to the presence of catechol moieties) for attachment of antibacterial or antifouling agents containing free amino and thiol groups. Moreover, it allows for the attachment and encapsulation of living cells, serves as “primer” for in situ silver nanoparticle deposition, increases the surface hydrophilicity and decreases the toxicity of coated substrates [
16]. Polydopamine coating also increases the attachment and spreading of human endothelial cells on polycaprolactone fibers and stainless steel [
17,
18]. Interestingly, not only dopamine but also its biochemical precursor levodopa (L-DOPA) can form coatings on different substrates. L-DOPA was already reported as more beneficial (in terms of modification of polyester fibers with antibiotics) than dopamine [
19]. We have recently reported the deposition of polymerized L-DOPA (PLD) on natural curdlan (β-1,3-glucan) and synthetic polyester fibers (of complex 3D structure), followed by gentamicin immobilization on the coatings. Both curdlan and polyester fibers, coated with PLD, exhibited higher antibiotic binding yield and antimicrobial activity in comparison with the same fibers coated with PDA [
19,
20,
21]. It was also shown that human endothelial cells proliferated better on PLD-coated polyester fibers than on the pristine ones and that this modification reduced the toxicity against Danio rerio embryos [
19].
To our knowledge, a strategy for polycatecholamine-based functionalization of collagen-sealed vascular prostheses has never been proposed before. Therefore, in this study we tested the possibility of polycatecholamine grafting on collagen-sealed polyester vascular prostheses. In a pilot experiment, we tested both PDA (polydopamine) and PLD (polymerized L-DOPA) as coatings and then we selected the most promising one. First, we wanted to prove that coating of collagen-sealed vascular grafts using polycatecholamines is possible and that the procedure is effective without the loss of the collagen-sealing layer and important properties of the grafts (their hydrophilicity, elasticity, favored attachment and proliferation of endothelial cells and biological safety). Second, we hypothesized that the grafted polycatecholamine layer can serve as a platform for further immobilization of antibiotics to protect the collagen-sealed grafts against bacterial adhesion and growth.
2. Results and Discussion
In our previous work, the coating with polycatecholamine layers was performed on polyester knitted vascular grafts [
19]. Despite their complex shape, the coating was relatively uniform and it enabled the immobilization of significant amounts of gentamicin via catechol moieties of polycatecholamines (PDA produced from dopamine and PLD produced from L-DOPA as monomers, respectively) [
19]. Thus, we decided to test similar coating conditions for modification of collagen-sealed prostheses, although relative sensitivity of collagen fibers to chemical environment was a challenging factor. According to the manufacturer, the graft selected for our study was sealed with bovine dehydrothermal crosslinked collagen type I mixed with glycerol before the graft coating.
Overall, optimization of the process of collagen-sealed graft coating with polycatecholamines, as demonstrated in
Supporting Information, showed that the most promising results were obtained when the following conditions were used: 10 mM Tris buffer pH 8.5, addition of Cu
2+, Na
+ and Mg
2+ ions, coating temperature 37 °C and L-DOPA as a monomer (which polymerized into PLD coating). This set of conditions allowed us to produce the grafts with a uniform (according to visual observations) PLD layer which enabled binding maximum gentamicin amount with the highest antibacterial activity. Therefore, this set of conditions was used for prostheses coating in all further experiments. However, during the pilot experiments we observed that the coating procedure caused the decrease of dry prosthesis weight (by approximately 50%) and significant increase of stiffness and brittleness. This second phenomenon is particularly undesirable for vascular grafts because it hinders the procedure of graft implantation and suturing with the blood vessel wall. We found that glycerol removal during the coating process is responsible for this phenomenon. Thus, we performed a series of tests aiming to restore the grafts’ flexibility by reintroduction of glycerol into their structure (data not shown). We found that simple soaking of PLD-coated grafts in 30% aqueous glycerol solution at 25 °C for 10 min, followed by drying at 37 °C, restored the flexibility and initial weight of the prostheses. Thus, PLD-coated glycerol-regenerated grafts were also subjected to further tests.
Table 1 describes the samples used in these experiments.
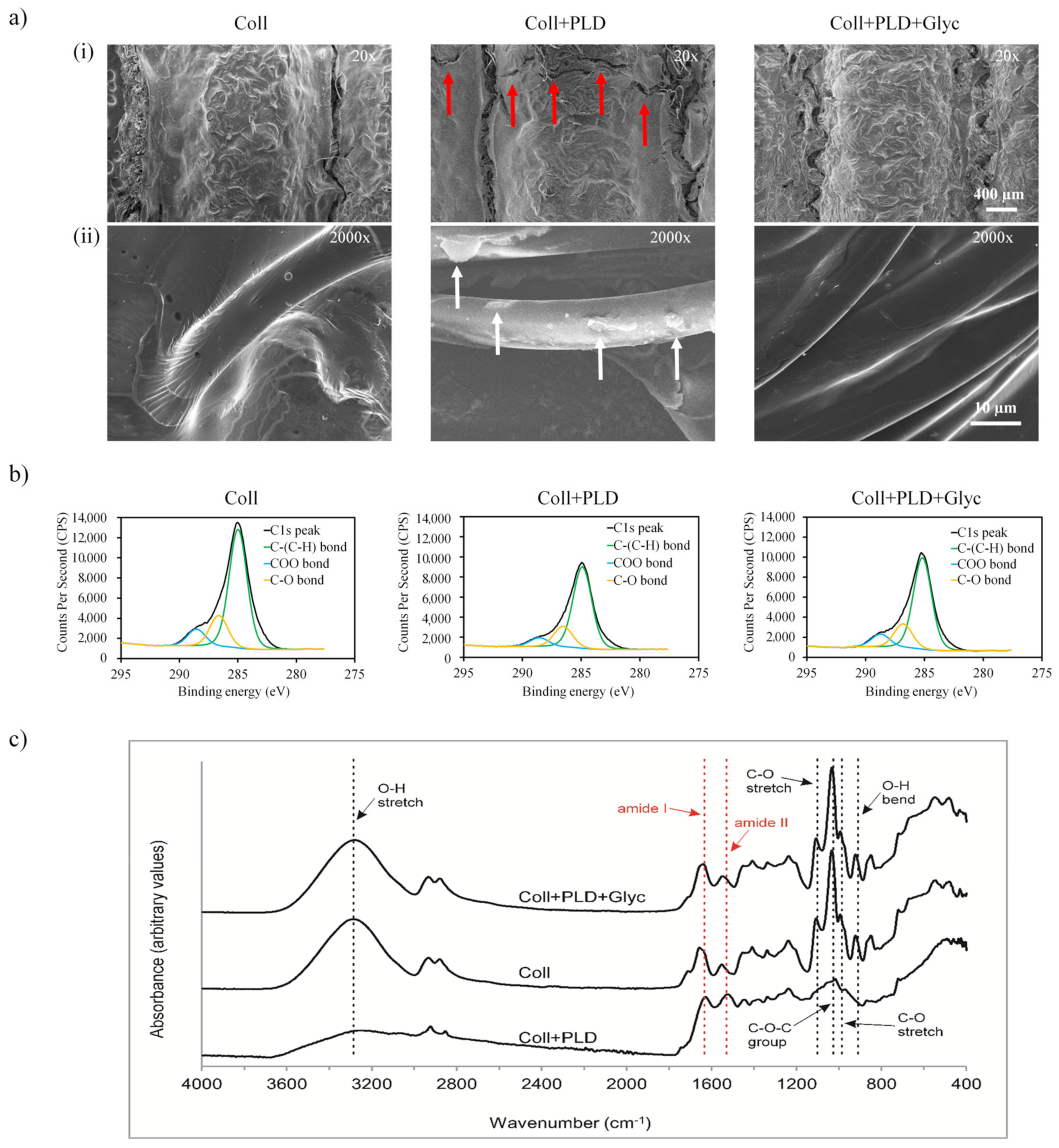
The first hypothesis put forward in our study was that our optimized coating procedure did not disrupt the collagen-sealing layer and left intact the most important properties of the grafts, such as surface topography and chemical composition, hydrophilicity, elasticity, favored attachment and proliferation of endothelial cells and biological safety. Therefore, PLD-coated grafts (both glycerol-regenerated and non-regenerated) were subjected to series of experiments and compared with pristine grafts. In the first place, we evaluated the surface topography of Coll, Coll+PLD and Coll+PLD+Glyc samples by SEM (
Figure 1a). All the tubular knitted samples showed similar macrostructure showing a thick layer of coating over the polyester multifilaments. However, some microcracks were observed in the Coll+PLD vascular grafts (indicated by red arrows in
Figure 1(ai)) which were not present in the Coll and Coll+PLD+Glyc samples. At higher magnification (2000×), the surface of the fibers of Coll and Coll+PLD+Glyc samples were similar, both showing a smooth topography (
Figure 1(aii)), with a polymeric coating bonding the fibers. In contrast, the surface of Coll+PLD vascular grafts displayed the individual fibers without the continuous coating, which was only observed as rough irregular deposits on the surface of the fibers (indicated by white arrows).
In order to further characterize the studied samples, the chemical nature of the different surfaces was evaluated by XPS and ATR-FTIR analysis. The chemical composition of the first nanometers of the surface revealed the presence of C1s, O1s and N1s, in agreement with the structure of collagen (
Table 2). Following PLD coating, the O/C ratio and N/C decreased in Coll+PLD samples reflecting a higher C amount in the PLD molecules than in collagen and, thus, the presence of the molecule on the surface—from 0.2039 (Coll) to 0.1201 (Coll+PLD) in O/C and from 0.0670 (Coll) to 0.0458 (Coll+PLD) in N/C. After the glycerol soaking process, Coll+PLD+Glyc vascular grafts displayed similar values to the Coll sample, which might indicate that glycerol is not retained on the surface but rather mainly absorbed by the graft structure. To determine the percentage of the different C bonds present in the surface of the studied vascular grafts, the C1s peak deconvolution reflected the presence of C-(C/H), C-O or C-N and COO bonds (
Figure 1b). In all the samples, C-(C/H) bond was the most predominant C bond, followed by C-O and COO. Comparing Coll and Coll+PLD samples, the PLD coating caused an increase of C-(C/H) from 71.43% to 73.48%, while C-O bonds remained similar (18.54% for Coll and 18.67 for Coll+PLD) and COO bonds decreased from 10.04% to 7.86%. Then, after the glycerol soaking process, Coll+PLD+Glyc vascular grafts showed similar values to the Coll samples, with 71.55% for C-(C/H), 18.18% C-O and 10.26% for COO. This phenomenon may be a consequence of glycerol contamination with fatty acids which contain carboxyl groups in their chain (glycerol is frequently produced by transesterification of fatty acids) [
22].
The ATR-FTIR spectral analysis of Coll, Coll+PLD and Coll+PLD+Glyc samples (
Figure 1c) confirmed the presence of amide I (1640 cm
−1) and amide II (1548 cm
−1) bands, characteristic for proteins. However, for Coll and Coll+PLD+Glyc samples, the bands were slightly shifted to higher wavenumbers which correlated with the higher N1s atomic concentration percentage found in the XPS analysis compared to Coll+PLD values. The change of amide I band position to 1645 cm
−1 could be ascribed to the presence of hydroxyl groups of adsorbed water within glycerol-modified grafts [
23,
24]. The shift of amide II band position to 1580 cm
−1 could be speculated to be related to impurities in glycerol (containing COO
− groups) which were absent in pure glycerol [
25,
26] and which match with the XPS results. Thus, the collagen layer was demonstrated to remain on fibrous prostheses after the process of PLD coating which is important in view of the principal feature of the grafts—lack of permeability to blood. Presence of PLD was impossible to detect because primary amine groups which are characteristic for catecholamine compounds are likely to be overlapped by amide bands of collagen. The bands attributed to glycerol were observed at 921 cm
−1 (O-H bending vibrations), 993 cm
−1 (C-O stretching vibrations in CH
2OH), 1034 cm
−1 (C-O-C group), 1107 cm
−1 (C-O stretching vibrations in CHOH) and in the region 3600–3000 cm
−1 (O-H stretching vibrations) [
23,
25,
27]. These bands, suggesting glycerol presence, were shown for Coll and Coll+PLD+Glyc samples. In the spectrum of the Coll+PLD sample, most of these bands disappeared, suggesting that at least a major amount of glycerol was eluted from the prostheses during PLD coating procedure (
Figure 1c).
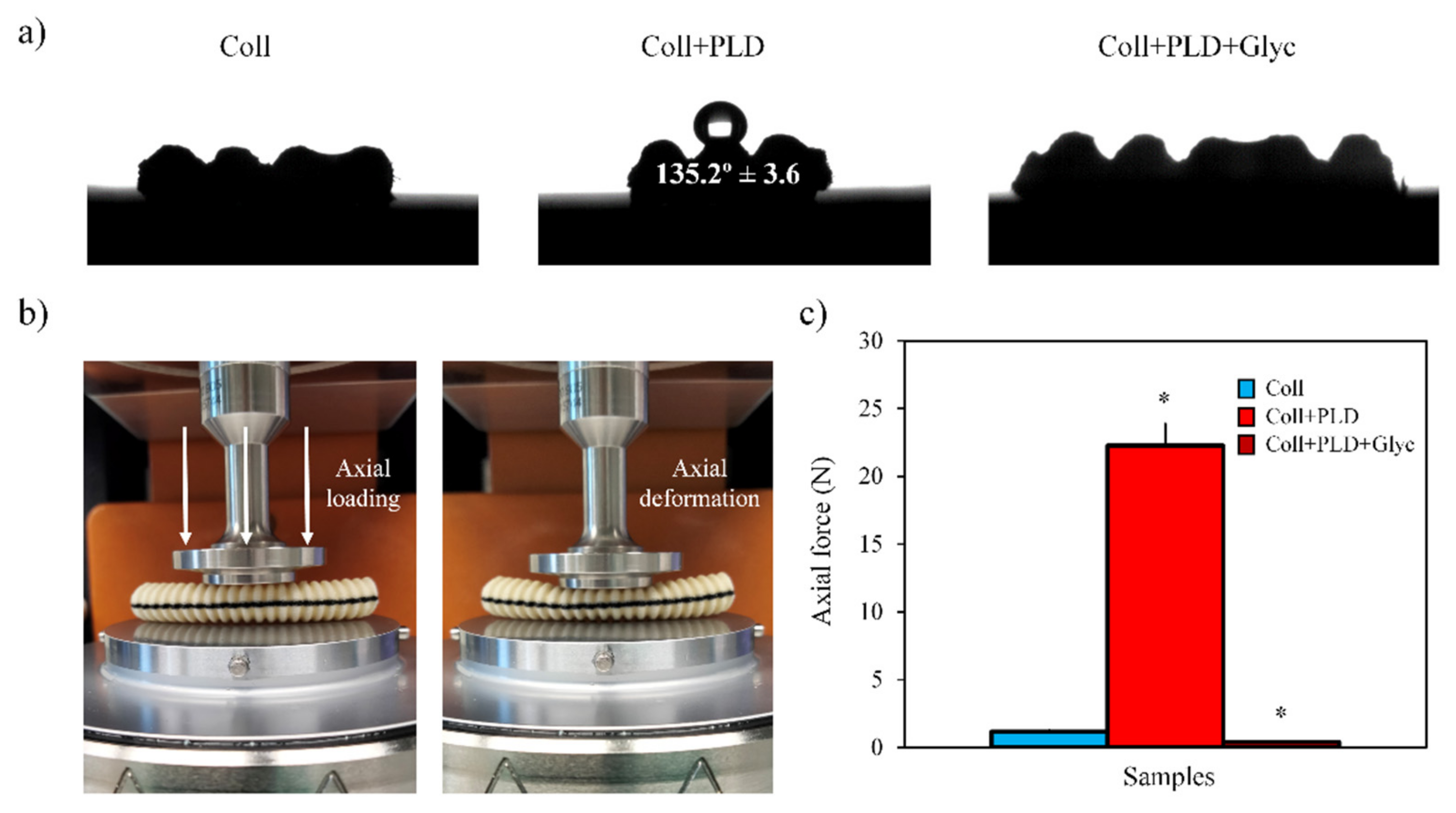
From another point of view, the influence of the PLD coating and glycerol soaking process on the physical properties of the studied samples was evaluated focusing on their hydrophilicity and elastic behavior. Regarding the hydrophilicity of the vascular grafts, the contact angle of 10 µL water droplets was measured on the surface of Coll, Coll+PLD and Coll+PLD+Glyc samples (
Figure 2a). Coll and Coll+PLD+Glyc vascular grafts displayed similar hydrophilic behavior since, after deposition, the water droplet was quickly absorbed within <1 s. This could be attributed to the presence of glycerol, which has low surface tension, favoring the wettability of the material. In contrast, in Coll+PLD samples, the water droplet was not absorbed and remained on the surface of the sample, showing a contact angle of 135.2° ± 3.6, typical of hydrophobic surfaces.
Regarding the elastic behavior, the force required to cause an axial deformation of 50% in all the studied vascular grafts was determined using a highly sensitive load cell in the rheometer (
Figure 2b). In this experiment we confirmed the increase of the stiffness caused by the PLD coating, since the force required to deform the Coll+PLD samples (≈22 N) was around 19 times higher than Coll samples (≈1.17 N) (
Figure 2c). In addition, during the compression, Coll+PLD samples denoted brittleness as they suffered visible cracks and, after applying the axial force, the samples were not able to recover the initial shape. In contrast, the Coll samples, in addition to lower stiffness, also displayed an elastic behavior since Coll samples were not cracked and were able to recover the initial state. Then, thanks to the reintroduction of glycerol into the vascular grafts structure in Coll+PLD+Glyc, the samples restored the stiffness and flexibility achieving similar axial force values to Coll (≈0.4 N for Coll+PLD+Glyc). Overall, analyzing the data obtained from the material characterization, we determined that the glycerol soaking process was able to restore the chemical and physical properties in Coll+PLD+Glyc vascular grafts, obtaining characteristics very close to the pristine Coll samples.
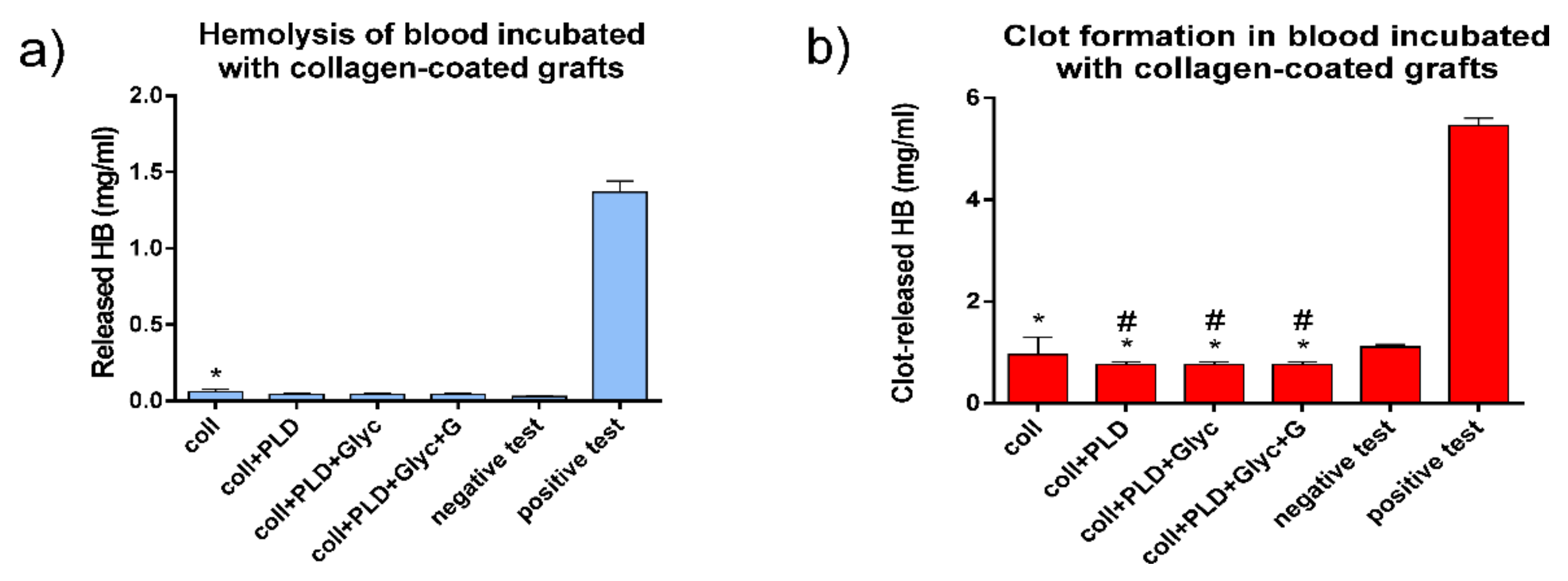
After performing the physicochemical characterization of all samples, we evaluated the biological safety of the studied vascular grafts. Biological safety of implantable materials concerns many aspects of biomaterial–human body interactions. In this sense, vascular prostheses are designed for continuous contact with circulating human blood. Therefore, blood reaction to the contact with modified and control prostheses was evaluated in terms of blood hemolysis and clot formation. All tested prosthesis samples, Coll, Coll+PLD and Coll+PLD+Glyc, were found relatively safe for evaluated blood parameters. With respect to hemolysis, all PLD-coated prostheses were comparable to negative test, whereas the Coll graft induced slight but significantly different blood hemolysis (
Figure 3a). With respect to clot-forming dynamics, the lower the amount of hemoglobin released from erythrocytes not entrapped within a clot, the higher the blood clotting capacity. As shown in
Figure 3b, all the grafts caused significantly different but slight increases of clot-forming rate in comparison with negative test. Moreover, all three PLD-coated samples slightly induced clot formation (this induction was also significantly different) when compared to Coll grafts (
Figure 3b), which is promising in relation to reduction of wound bleeding directly after the implantation. Overall, neither PLD-coating nor glycerol addition was found to be harmful for interactions between the grafts and human blood.
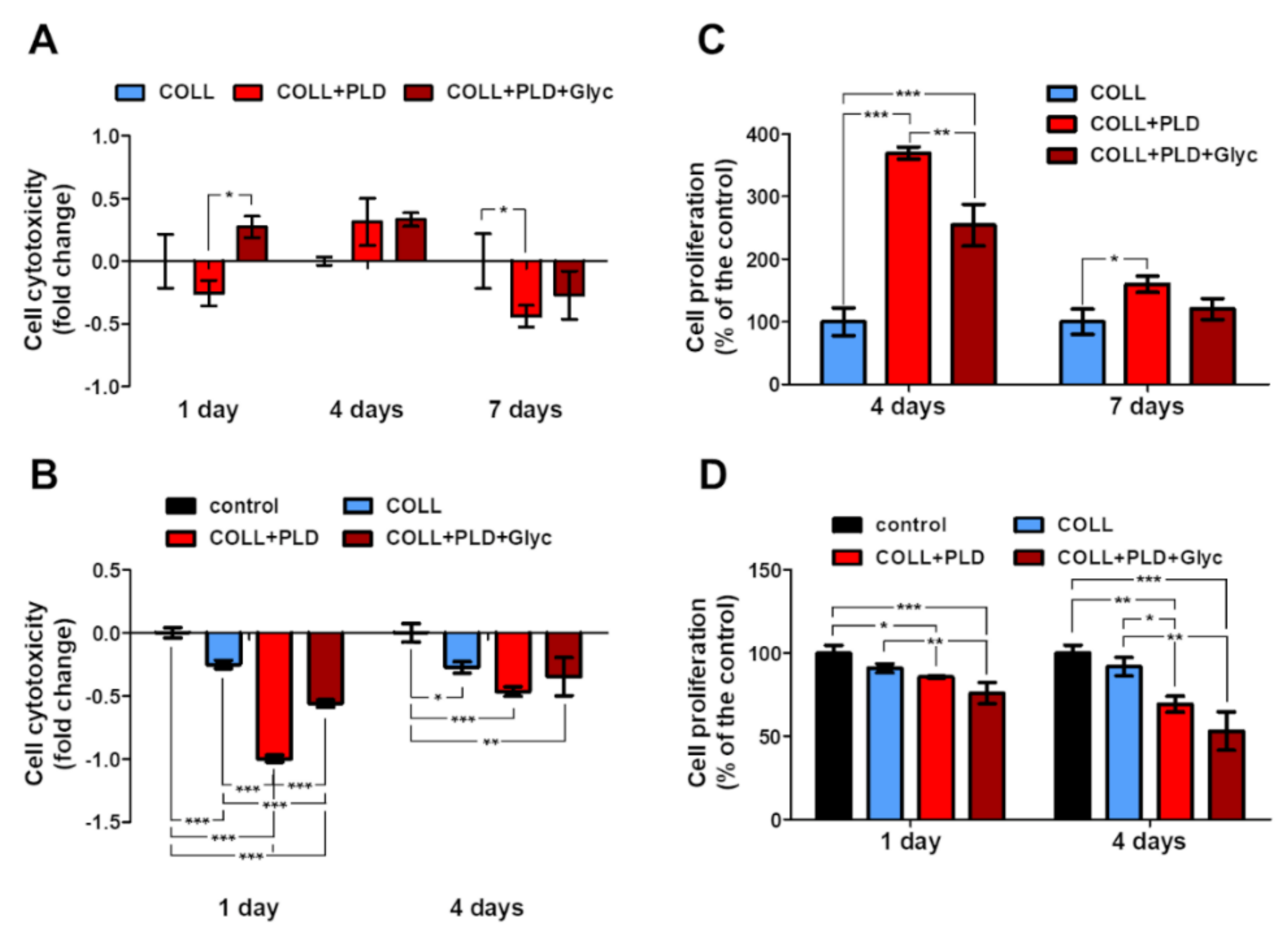
Another important aspect of human–body–implant interactions concerns the cytotoxicity against a target cell line. For vascular prostheses, human endothelial cells (HUVECs) are the most appreciated model. Therefore, viability and proliferation of HUVECs was evaluated for Coll, Coll+PLD and Coll+PLD+Glyc graft samples. The HUVEC cells grew on all prostheses without harmful effects on them—no significant cytotoxicity was observed in almost all cases (excluding Coll+PLD+Glyc at 1 day incubation) (
Figure 4A,B). On the 4th day a slight rise in cytotoxicity was noted, but no value was statistically significant (cytotoxicity higher by 8.6% and 2.7% than in the control, exerted by Coll+PLD and Coll+PLD+Glyc prostheses, respectively). By the 7th day, cytotoxicity of the Coll+PLD and Coll+PLD+Glyc prostheses was lower than Coll. Furthermore, a significant decrease in cytotoxicity was noted on the 7th day of growth on Coll+PLD prosthesis (cytotoxicity lower by 22.2% compared to the control (Coll) prosthesis,
p = 0.0418) (
Figure 4A). Such an event (higher cytotoxicity at 4th and lower at 7th day) may have occurred due to adaptation of the cells, previously grown as 2D culture, to the new conditions of 3D culture. Besides the growth of the cells on the prostheses (direct tests), the effect of the prosthesis extracts was evaluated (indirect tests). Cells were incubated with medium previously incubated with prostheses or without them (used in the indirect analyses as control). Significant decrease in LDH level was observed, along with slight decrease in proliferation. No prosthesis extract exerted a cytotoxic effect towards HUVEC cells. Furthermore, the cytotoxicity of Coll+PLD and Coll+PLD+Glyc extracts was lower than in the case of Coll extract. After 1-day incubation, Coll+PLD and Coll+PLD+Glyc graft extracts caused a significant decrease in cell cytotoxicity (by 99.9% and 56.0% of the control, respectively, with
p < 0.0001), compared to both control and Coll prosthesis’ (cytotoxicity decrease of Coll by 25.1% compared to the control) extracts. After 4-day incubation, observed cytotoxicity decrease was lower (decreased by 46.6 and 34.7% compared to the control) than after 1-day; however, it was still lower than in control and Coll prosthesis (decrease by 27.4% in reference to the control) variants (with
p = 0.0013) (
Figure 4B).
The proliferation of the cells on the Coll+PLD prostheses was induced compared to the Coll. Initially, the cell divisions were boosted, which was noted as a statically significant rise in proliferation at the 4th day (to the 396.6 ± 9.4% and 254.5 ± 33.5% of the control, in case of Coll+PLD and Coll+PLD+Glyc prostheses, respectively;
p < 0.0001). With time, the proliferation acceleration was slowed down, leading to the proliferation rate at 7th day of 160.1 ± 13.2% and 120.4 ± 16.8% compared to the control, of the cells grown on Coll+PLD and Coll+PLD+Glyc prostheses, respectively (with statistically significant results in the case of Coll+PLD prosthesis with
p = 0.0130) (
Figure 4C). However, the rate of proliferation of the HUVEC on Coll+PLD and Coll+PLD+Glyc prostheses was still higher than on Coll. The proliferation of the HUVEC cells incubated with prosthesis extracts was lower than cells incubated with control extract. A slight but statistically significant decrease in cell proliferation was noted: to the 85.7 ± 0.7% and 75.9 ± 6.4% of the control (
p = 0.0007), exerted by Coll+PLD and Coll+PLD+Glyc extracts, respectively, after 1-day incubation, and to the 69.3 ± 4.8% and 53.2 ± 11.5% of the control (
p = 0.0009), respectively, after 4-day incubation. The Coll prosthesis extract exerted a decrease in proliferation (to the 90.9 ± 2.7% and 91.9 ± 5.6% of the control, after 1 and 4 days, respectively); however, the values were not statistically significant (
Figure 4D).
The modified prostheses exerted no cytotoxic effect and induced proliferation of the HUVEC cells. It has been demonstrated that modification of commercially available collagen-sealed prostheses with polymers or proteins may be beneficial for the cells, i.a. through improvement of the cell adhesion or proliferation [
28,
29,
30]. The lowest LDH level and highest proliferation ratio were observed in the case of the Coll+PLD prosthesis. As mentioned before, glycerol was washed off from the biomaterial during the modification step. The compound is, however, present on Coll and Coll+PLD+Glyc prostheses. This may indicate the negative effect of the glycerol on HUVEC cells. The harmful effect of the glycerol on cells is carried mainly through alteration in osmotic forces and has been demonstrated before on various cellular models [
31,
32]. However, it seems that modification of the commercially available prosthesis with PLD reversed the harmful effect of the glycerin, resulting in lower cytotoxicity and higher proliferation (Coll+PLD+Glyc vs. Coll). Slightly different results were obtained in MTT indirect test. In general, the differences between direct and indirect tests are a consequence of differences between 3D and 2D cultures. Furthermore, culture for MTT indirect test was continued for 4 days without medium exchange, which may have resulted in depletion of the medium of nutrients and accumulation of products of metabolism.
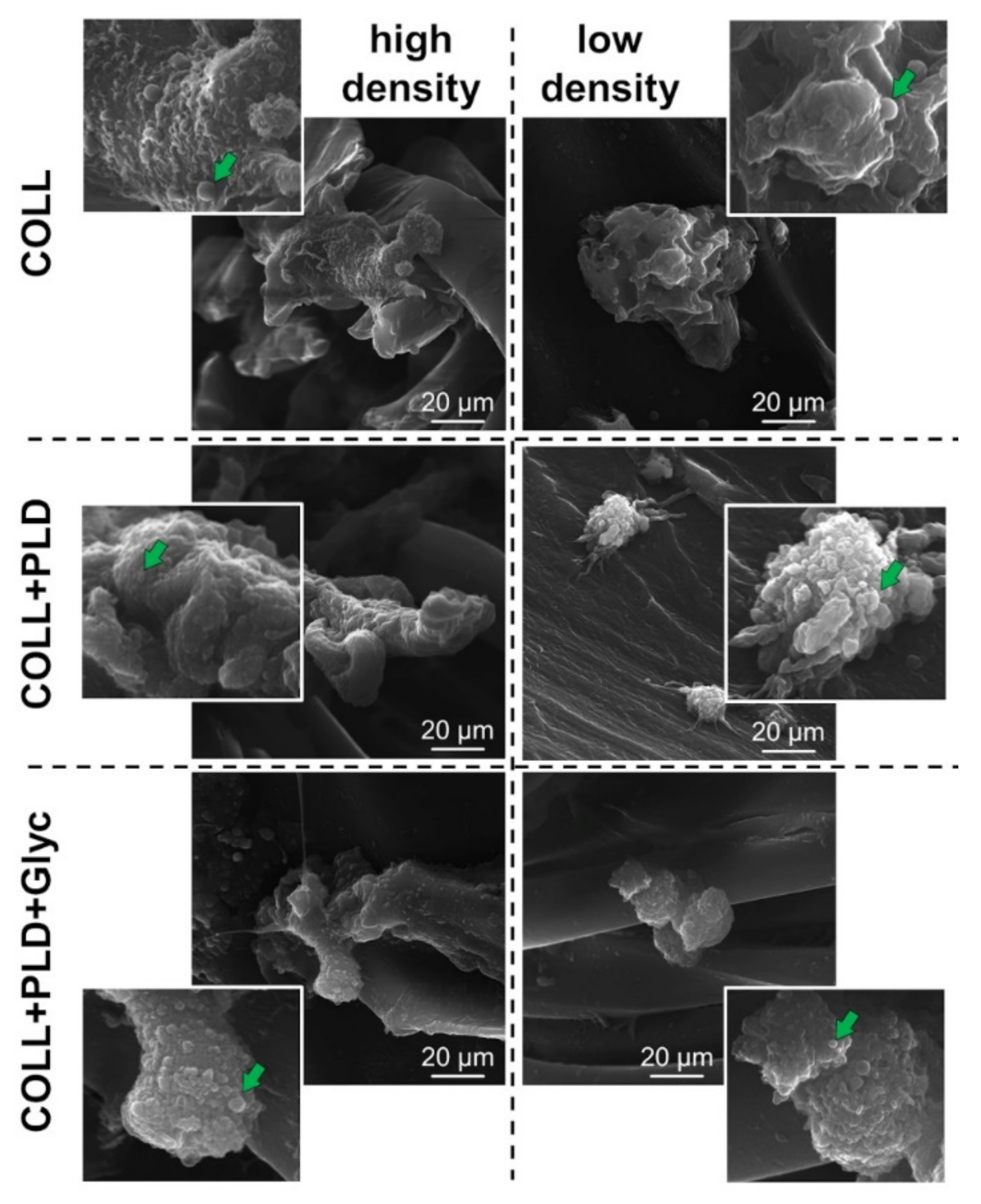
Morphology of the HUVEC cells grown on the prostheses for 4 days was evaluated. Pictures of high and low density of the cells were taken using SEM technique (complete set of SEM images is available in
Supporting Information file). No significant changes were observed in comparing cells grown on Coll+PLD and Coll+PLD+Glyc prostheses with ones cultured on Coll prostheses. However, cells present at sites with lower cellular density grown on Coll+PLD and Coll+PLD+Glyc prostheses appeared to possess rounder structures, presumably extracellular vesicles, compared to the cells grown on Coll prostheses (for the reference images, see: [
33,
34,
35] (
Figure 5, right column). It has been demonstrated that production of the EVs and microvesicles by endothelial cells and their progenitors may be beneficial for activation, growth and survival of the endothelial cells and vascularization process [
36,
37]. Coll+PLD and Coll+PLD+Glyc prostheses, which turned out to be more suitable for HUVEC cell growth compared to the control Coll prosthesis, induced production of the vesicles (
Figure 5, right column). Nevertheless, no harmful effect was noted in the case of each prosthesis.
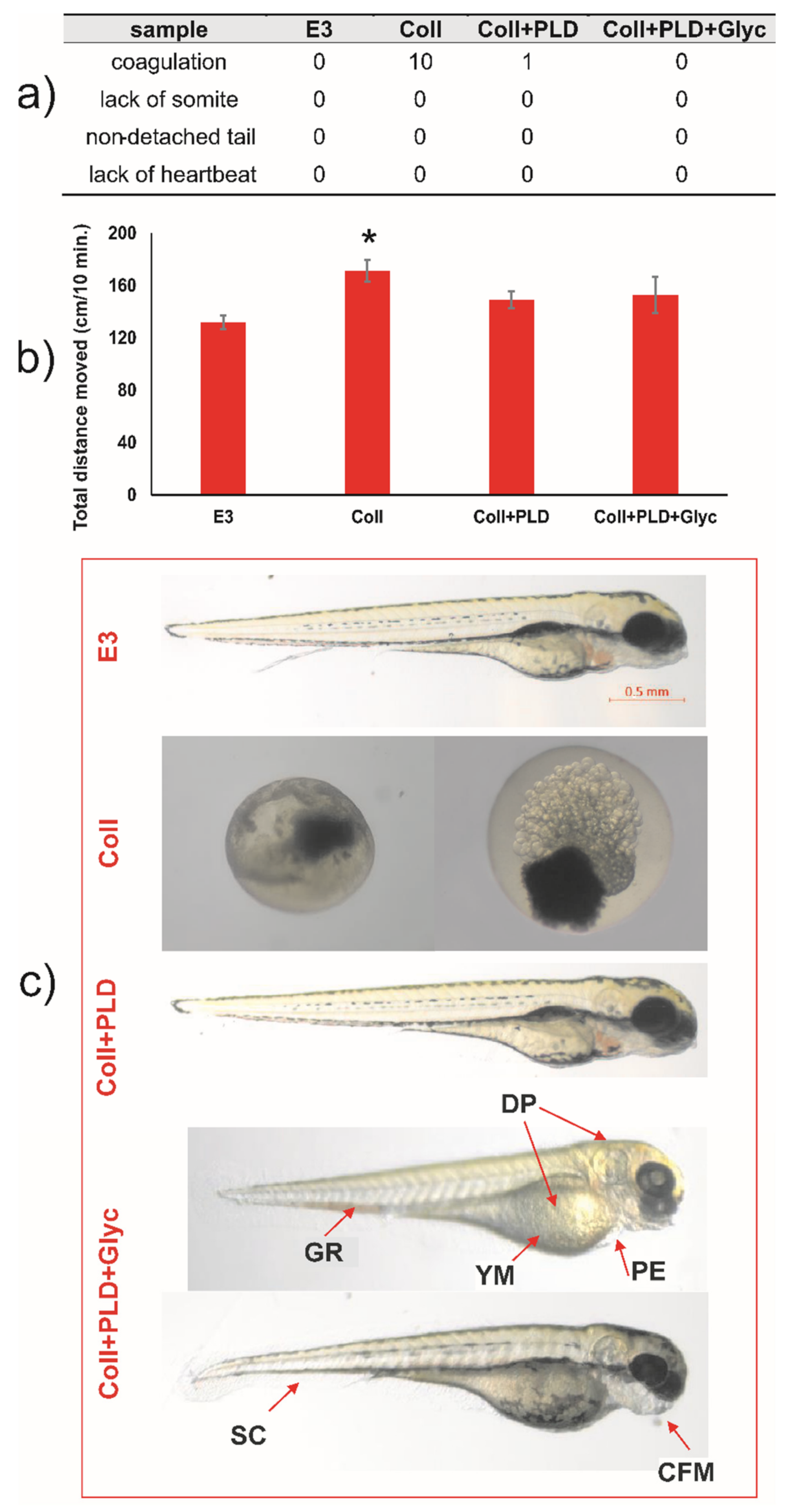
Results of experiments on the Danio rerio model gave interesting results concerning the toxicity of the modified vascular prostheses. During 96 h post-fertilization, the lack of coagulation, tail detachment, development of somites, and heartbeat was observed for negative E3 control. For extracts of prostheses samples, the coagulation was noticed: 10 per 10 embryos treated with extract of Coll, 1 per 10 embryos in extract of Coll+PLD and 0 per 10 in extract of Coll+PLD+Glyc (
Figure 6a). Thus, extract of Coll (pristine graft) was shown to be highly embryotoxic while for that of Coll+PLD and Coll+PLD+Glyc it was shown to be highly safe.
For embryos incubated in extracts of Coll+PLD and Coll+PLD+Glyc grafts, the appearance of morphological and physiological abnormalities was controlled as a marker of cytotoxic effect. There was no incidence of morphological and physiological abnormalities of zebrafish during 4 days of incubation and also in extract of Coll+PLD, suggesting the safety of poly(L-DOPA) modification. Extract of Coll+PLD+Glyc grafts induced craniofacial malformation, (3/10), pericardial oedema (7/10), spinal curvature (1/10), yolk sac malformation (7/10), depigmentation (7/10) and growth retardation (4/10) (
Figure 6a,c). In LLA, extract of pristine prostheses (Coll) influenced the locomotor activity of 5 dpf zebrafish in a statistically significant way one-way ANOVA: F (4,88) = 3.626;
p = 0.0123). Thus, we cannot exclude the neurotoxic effects of extract of Coll graft (
Figure 6b). The other studied extracts did not exert this effect. Overall, the results observed for Danio rerio model confirmed our observations for HUVECs cultures suggesting that PLD-coating generally reduced the toxicity of Coll grafts and that glycerol-regeneration of Coll+PLD grafts is less harmful for both models than pristine grafts (Coll).
On the basis of these experiments, it is quite clear that pristine collagen-sealed vascular grafts are not entirely safe in zebrafish model. Despite their approval for commercial use in medicine, the Coll graft showed strong pro-coagulation activity against fish embryos under stringent cytotoxicity assessment conditions of the performed tests (concentrated extract possessed by prosthesis incubation with E3 medium in proportion 0.1 g/1 mL). Comparison of the results obtained for Coll and Coll+PLD grafts suggested that glycerol may exert cytotoxic effect against Danio rerio embryos. As glycerol constituted approximately 50% weight of Coll and Coll+PLD+Glyc grafts, the extracts prepared for Danio rerio tests contained approx. 5% of glycerol. It was reported that 0.5% glycerol is the highest concentration safe for Danio rerio 1 hpf (hour post-fertilization) embryos [
38]. Moreover, 5% glycerol reduced the survival of the embryos with the rate related to their age—from 0% of survival for 1 hpf embryos to 60% of survival for 36–48 hpf embryos [
38]. Similarly, Maes et al. [
39] showed the increasing tolerance of Danio rerio embryos to glycerol depending on their age: 4 hpf embryos tolerated 1.5% glycerol while 5–7 dpf tolerated above 2.5% glycerol. They also demonstrated that 1 hpf embryos treated with 2.5% glycerol displayed anterior-posterior axis truncation with no extended tail,
cardia bifida and u-shaped somites [
39]. However, both Coll and Coll+PLD+Glyc contained similar amounts of glycerol but the Coll graft was much more harmful for zebrafish embryos than Coll+PLD+Glyc ones (
Figure 6). It is therefore possible that some post-production impurities in the pristine graft were responsible for its higher toxicity in comparison with the Coll+PLD+Glyc graft. Nevertheless, one should remember that pristine vascular prostheses were designed for the implantation into blood vessels in mature human organism and harmful agents are likely to be eluted/diluted by blood circulating around the implant, thus reducing their negative effect.
The second of the goals of this work was to verify whether PLD coating on collagen-sealed vascular grafts can serve as a platform for further immobilization of antibiotics to protect the grafts against bacterial adhesion and growth. Pilot experiment confirmed this hypothesis.
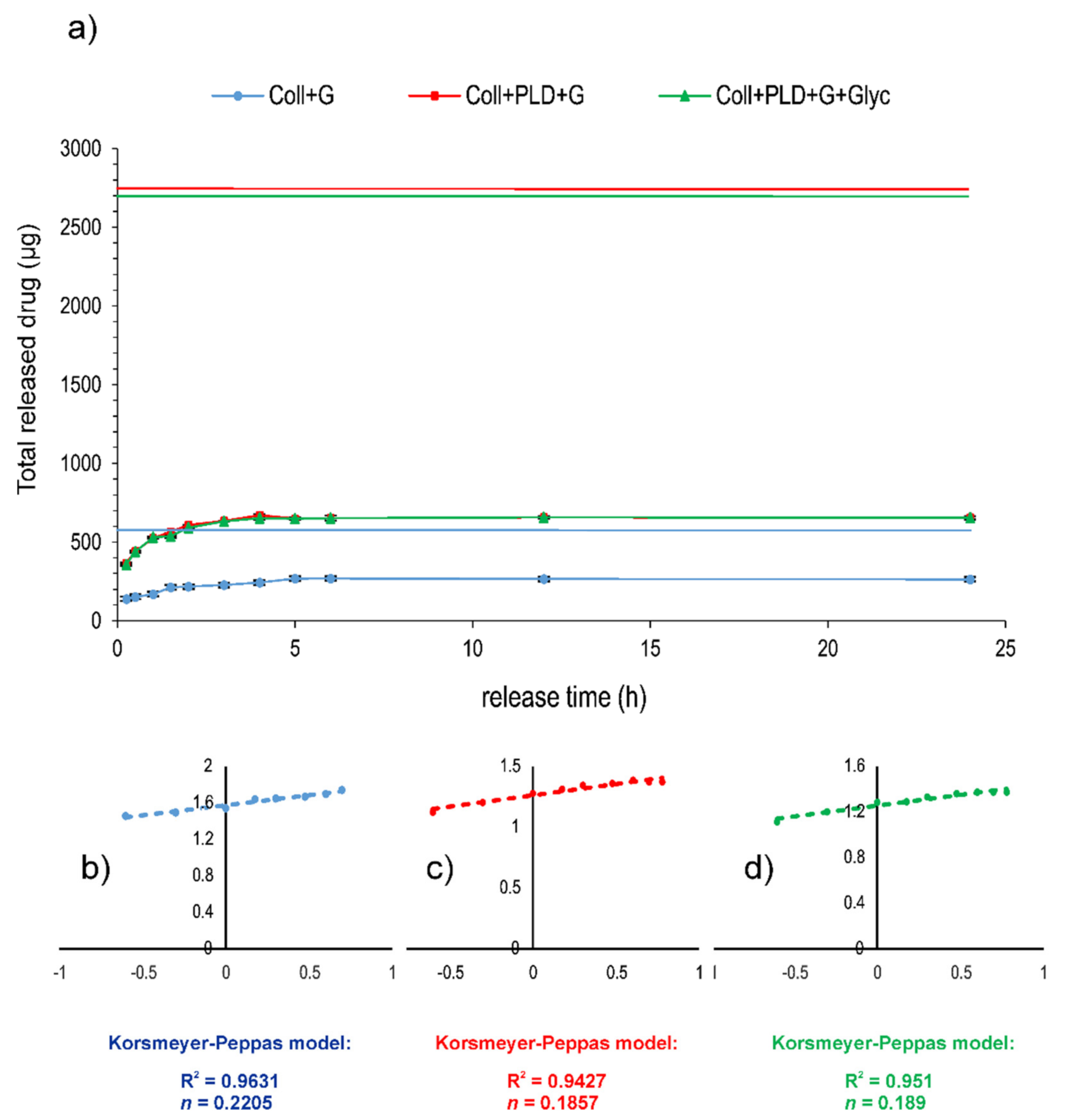
To evaluate the effect of PLD graft coating on antibiotic binding more extensively, gentamicin release from prostheses before and after PLD coating (Coll and Coll+PLD, respectively) was coupled with the drug by simple soaking in antibiotic solutions and subjected to the release test in a close-loop system. Moreover, Coll+PLD+G was additionally soaked in glycerol solution (producing Coll+PLD+G+Glyc sample). Coll+G, Coll+PLD+G and Coll+PLD+G+Glyc samples were loaded into the release units in similar quantities (approx. 0.5 g of dry prosthesis weight). However, the amount of immobilized antibiotic significantly differed: 822 and 5067 µg/g of prosthesis for Coll+G and Coll+PLD+G or Coll+PLD+G+Glyc, respectively. Thus, the amounts of gentamicin loaded into the cells also differed: 485, 2758 and 2728 µg for Coll+G and Coll+PLD+G or Coll+PLD+G+Glyc, respectively (
Table 3). The profiles of drug release are presented in
Figure 7a. They all suggest a quick and pore-dependent [
40] mechanism of drug release. Drug release exponents (
n) calculated for all samples on the basis of the Korsmeyer–Peppas model were 0.2205, 0.1857 and 0.189 for Coll+G, Coll+PLD+G and Coll+PLD+G+Glyc, respectively (
Figure 7b–d). According to Rither and Peppas [
41],
n values lower than 0.5 indicate Fickian diffusion dissolution mode. The drug was released from the prostheses during the first 5 h of the process: in 55.17% of initial content for Coll+G but only in 23.6–23.9% of initial content from Coll+PLD+G and Coll+PLD+G+Glyc grafts (
Table 3). Profiles of gentamicin release from Coll+PLD+G and Coll+PLD+G+Glyc samples were similar. Therefore, it seems that glycerol soaking did not affect the profile of gentamicin release from PLD-coated samples. The amount of antibiotic remaining on prostheses for Coll+G was equal to 397 µg/g of prosthesis but for Coll+PLD+G and Coll+PLD+G+Glyc it was 3855–3871 µg/g of prosthesis, therefore 10-fold more (
Table 3). The fact that PLD-coated grafts contain high amounts of non-eluted antibiotic attached to the fibers may suggest the higher probability of Coll+PLD+G (and Coll+PLD+G+Glyc) graft protection against bacterial adhesion.
To summarize, significantly more gentamicin was bound and more drug remained stably attached to the prosthesis after the release test in the case of PLD-coated grafts compared to pristine prostheses. A similar observation was made for PLD-coated curdlan hydrogels coupled with antibiotic—approximately 5 times more drug was bound to PLD-coated hydrogel than to a pristine one [
20]. Glycerol soaking, used to restore initial elasticity of the grafts, did not play a significant role in this phenomenon.
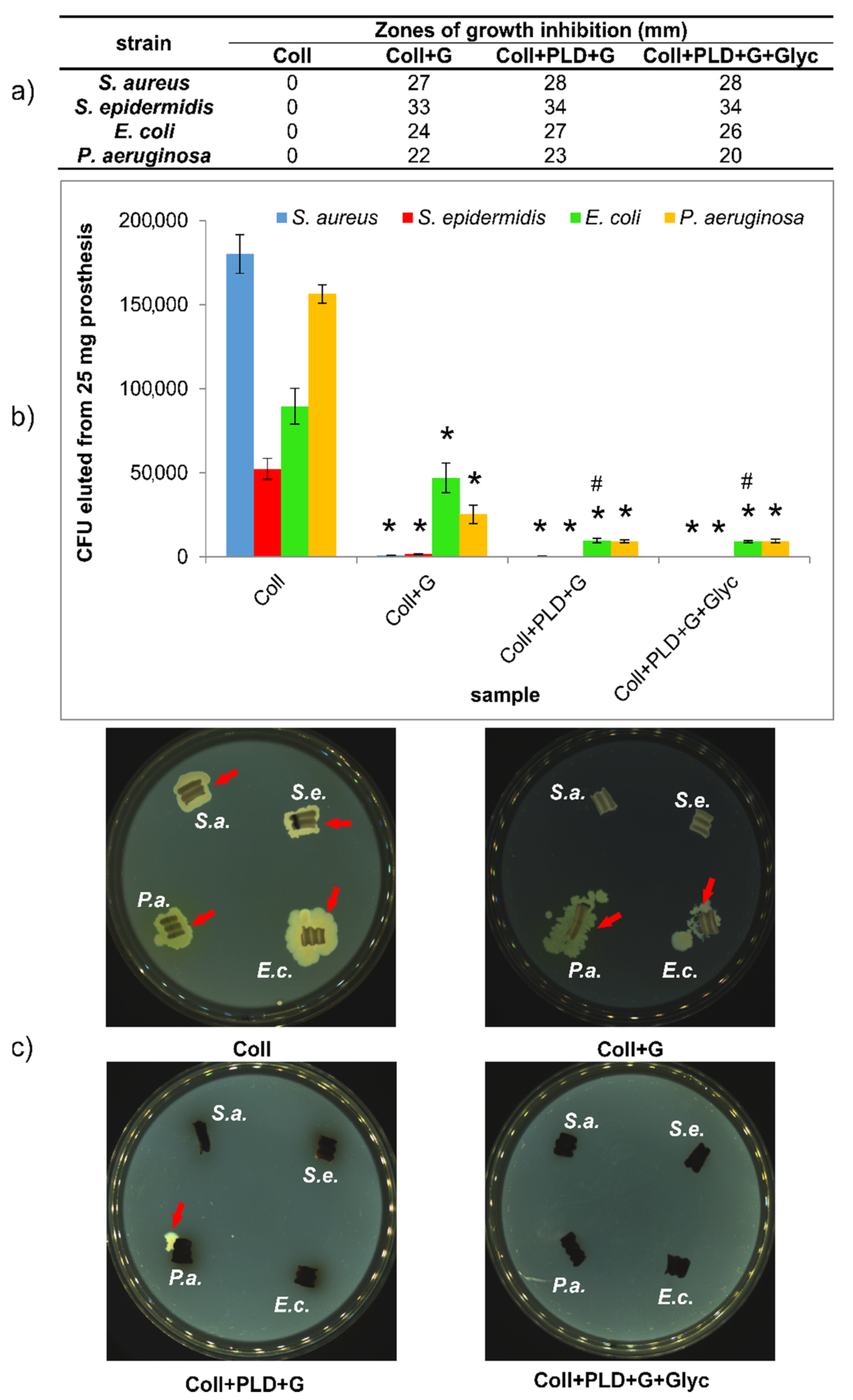
Careful evaluation of antibacterial properties of PLD-modified grafts is extremely important because collagen-sealed biomaterials are endangered per se (the collagen layer may serve both as an attachment surface and a nutrient for bacteria). Therefore, pristine Coll prosthesis was used as a reference in all experiments. Antibacterial activity of gentamicin-coupled pristine and PLD-coated prostheses was subjected to various tests. First, gentamicin diffusion test in agar medium was made, to evaluate how the prostheses were able to protect their close surroundings. The results showed, as expected, that Coll grafts did not show any growth inhibition zones for 4 Gram-positive and Gram-negative strains:
S. aureus, S. epidermidis, E. coli and
P. aeruginosa. Coll+G, Coll+PLD+G and Coll+PLD+G+Glyc samples caused the appearance of bacterial growth inhibition zones in the range 22–33 mm for non-modified graft and 20–34 mm for both PLD-modified samples (
Figure 8a). Therefore, there is some positive effect of PLD-coating on bacterial safety of collagen-sealed prostheses. Glycerol did not cause any change in the size of growth inhibition zone around the samples for Gram-positive bacteria. However, the zones of
E. coli and
P. aeruginosa growth inhibition were slightly reduced for glycerol-soaked sample in comparison with Coll+PLD+G. This may result from the presence of glycerol as a nutrient for Gram-negative bacteria. The differences between PLD-treated and untreated grafts are small. However, it should be noted that only removable drugs act antibacterially in this growth inhibition test.
Another aspect of antibacterial properties of biomaterials is their ability to reduce the bacterial adhesion to their surfaces. This aspect was verified by incubation of the samples in bacterial suspension for 2 h and evaluation of their adhesion in two ways. First, graft-adhered bacteria were enzymatically detached using trypsin followed by their counting (by plating on agar medium method). Second, the grafts with adhered bacteria were placed directly on agar medium to verify whether the bacteria can divide, migrate into the surrounding medium and spread. The results showed that bacteria freely adhere to pristine Coll grafts (in amount 50,000–180,000 CFU/25 mg graft) and they can divide and spread when exposed to agar medium (
Figure 8b,c). In the case of Coll+G graft, both Gram-positive strains adhered only to a small extent (933–1533 CFU), whereas
E. coli and
P. aeruginosa adhered to Coll+G graft in an amount reduced by approx. 50% and 80%, respectively, in comparison with Coll prostheses (
Figure 8b). Interestingly, for both Gram-negative strains, PLD-coating caused additional reduction of graft-adhered bacterial cells in comparison with Coll+G (for
E. coli, the reduction was significantly different) (
Figure 8b).
A similar tendency was observed for bacterial migration from the grafts and spreading on agar medium. In the case of both PLD-modified grafts with gentamicin (without and with glycerin), no bacteria were attached to the samples with the exception of single
P. aeruginosa colony. In contrast to Gram-negative strains, migration of Gram-positive bacteria to agar medium was not observed in the case of Coll+G samples (
Figure 8c). In conclusion, all obtained results confirmed the beneficial effect of PLD-coating on antibacterial activity of collagen-sealed grafts. Thus, these results are in agreement with our previous data concerning PLD-treatment of polyester fibrous prostheses and their resistance to bacterial adhesion [
19].
Although short-term resistance of biomaterials to bacterial attack is important, long-term response is also extremely essential. One must remember that implanted vascular grafts are permanently surrounded by circulating blood which cause constant elution of graft-bound antibacterial agent. Thus, gentamicin-bound pristine and PLD-coated grafts were subjected to drug elution for 10 days in subsequent buffer exchanges and antibacterial activity in collected extracts was evaluated against four reference strains (
Figure 9). It was found that the antibacterial effect of collected extracts is: (i) strain-dependent and (ii) titer-dependent (in some cases). For
S. aureus, PLD-modification of the prostheses only slightly reduced the rate of bacterial growth (the difference was significant for higher initial bacterial titer). However, this effect against
S. epidermidis was much more distinct—in the lower initial titer of bacteria, their growth was completely inhibited while for the higher initial titer, their growth was significantly diminished (significantly different results). Similarly for the strain
E. coli, PLD-coating caused partial reduction of bacterial growth in collected extracts (significantly different results). For
P. aeruginosa this effect was much smaller and significantly indifferent (
Figure 9). However, one must remember that both tested initial titers (1.5 × 10
5 CFU/mL or 1.5 × 10
6 CFU/mL) are very high and rarely appear in circulating blood. As reported elsewhere, in microbial infections, the typical target concentration in human blood is as low as 10
3 CFU/mL [
42]. Thus, the obtained results of bacterial growth reduction by the extracts collected during the experiment should be considered as highly promising in relation to the prevention of vascular graft infection [
43].