Mild Therapeutic Hypothermia Protects from Acute and Chronic Renal Ischemia-Reperfusion Injury in Mice by Mitigated Mitochondrial Dysfunction and Modulation of Local and Systemic Inflammation
Abstract
1. Introduction
2. Results
2.1. Mortality
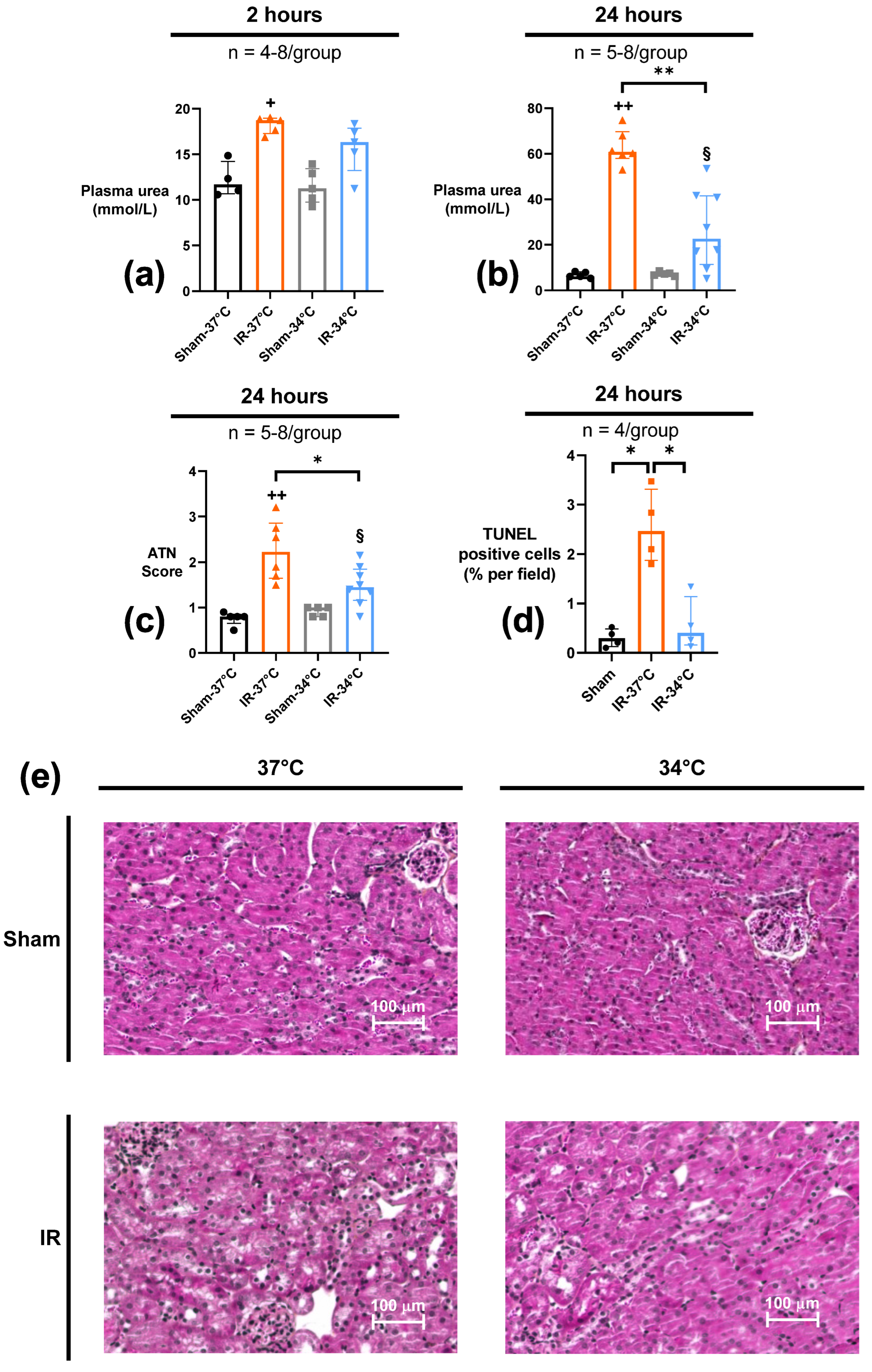
2.2. Renal Parameters
2.2.1. Acute Kidney Injury (AKI), Tubular Necrosis (ATN) and Apoptosis
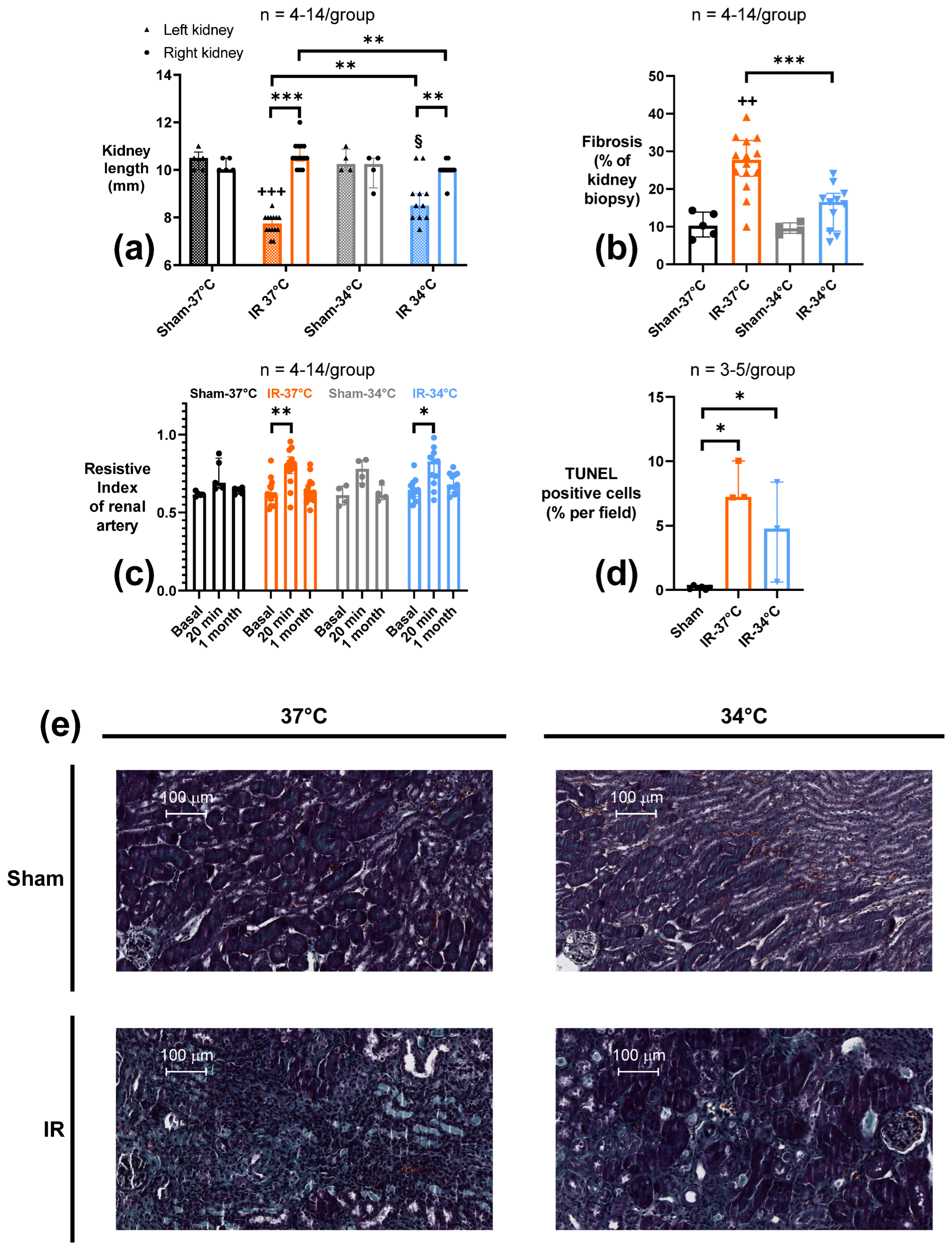
2.2.2. Chronic Kidney Atrophy, Fibrosis and Apoptosis
2.2.3. Renal Vascular Resistance (RVR)
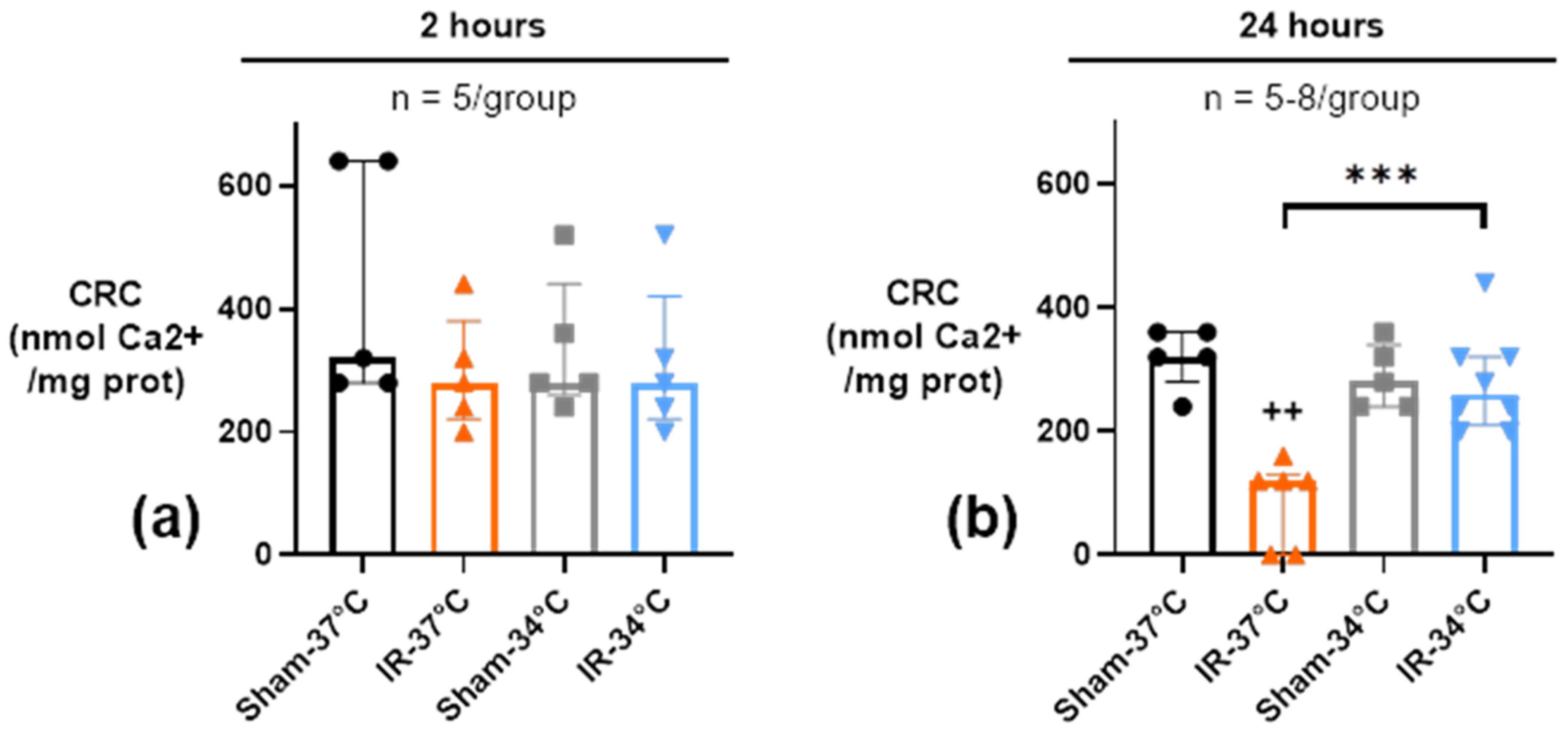
2.3. Renal Mitochondria Function
2.3.1. Mitochondrial Calcium Retention Capacity (CRC)
2.3.2. Oxidative Phosphorylation (OX-PHOS)
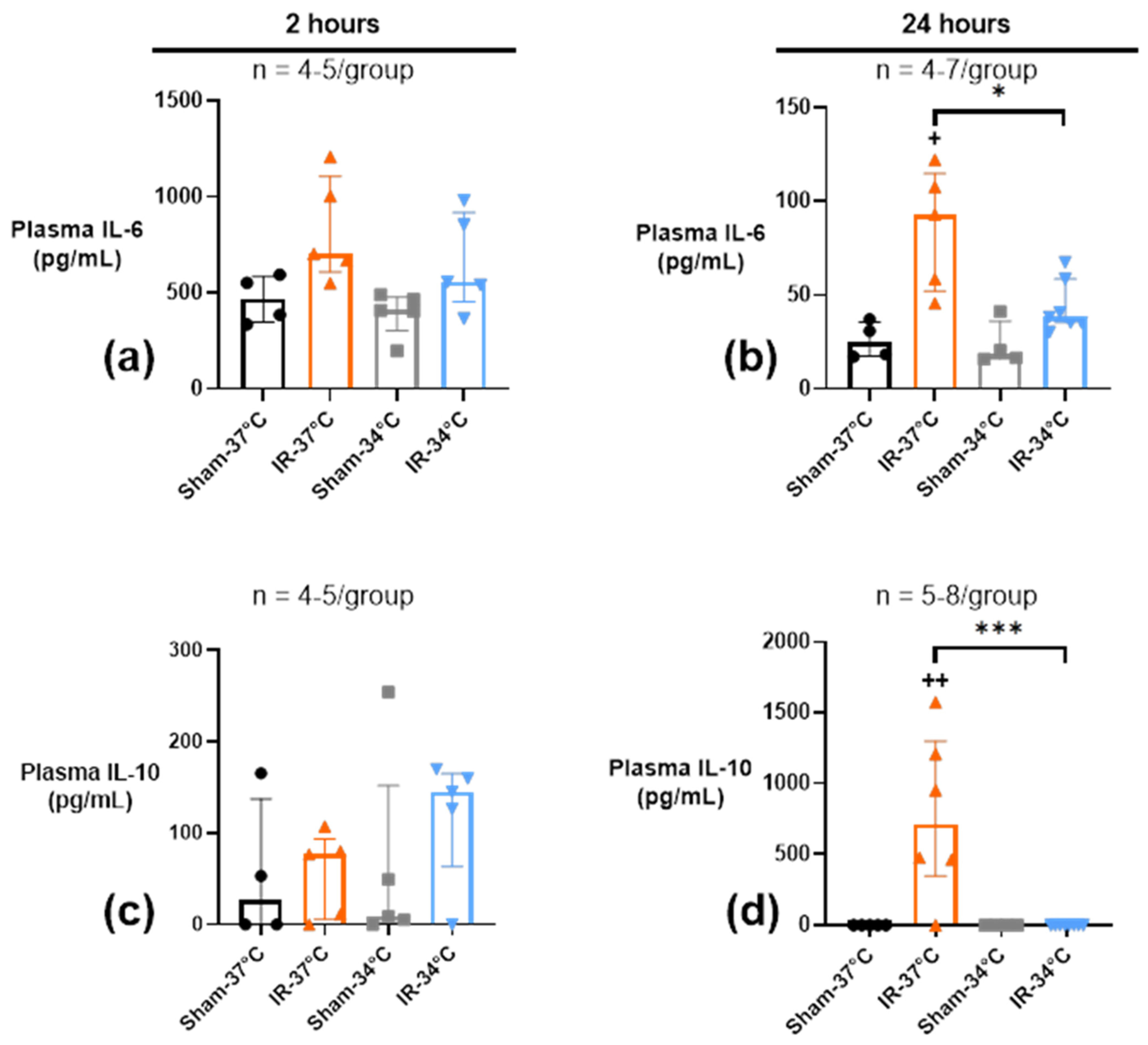
2.4. Inflammatory Response
2.4.1. Acute Systemic Plasmatic Inflammation
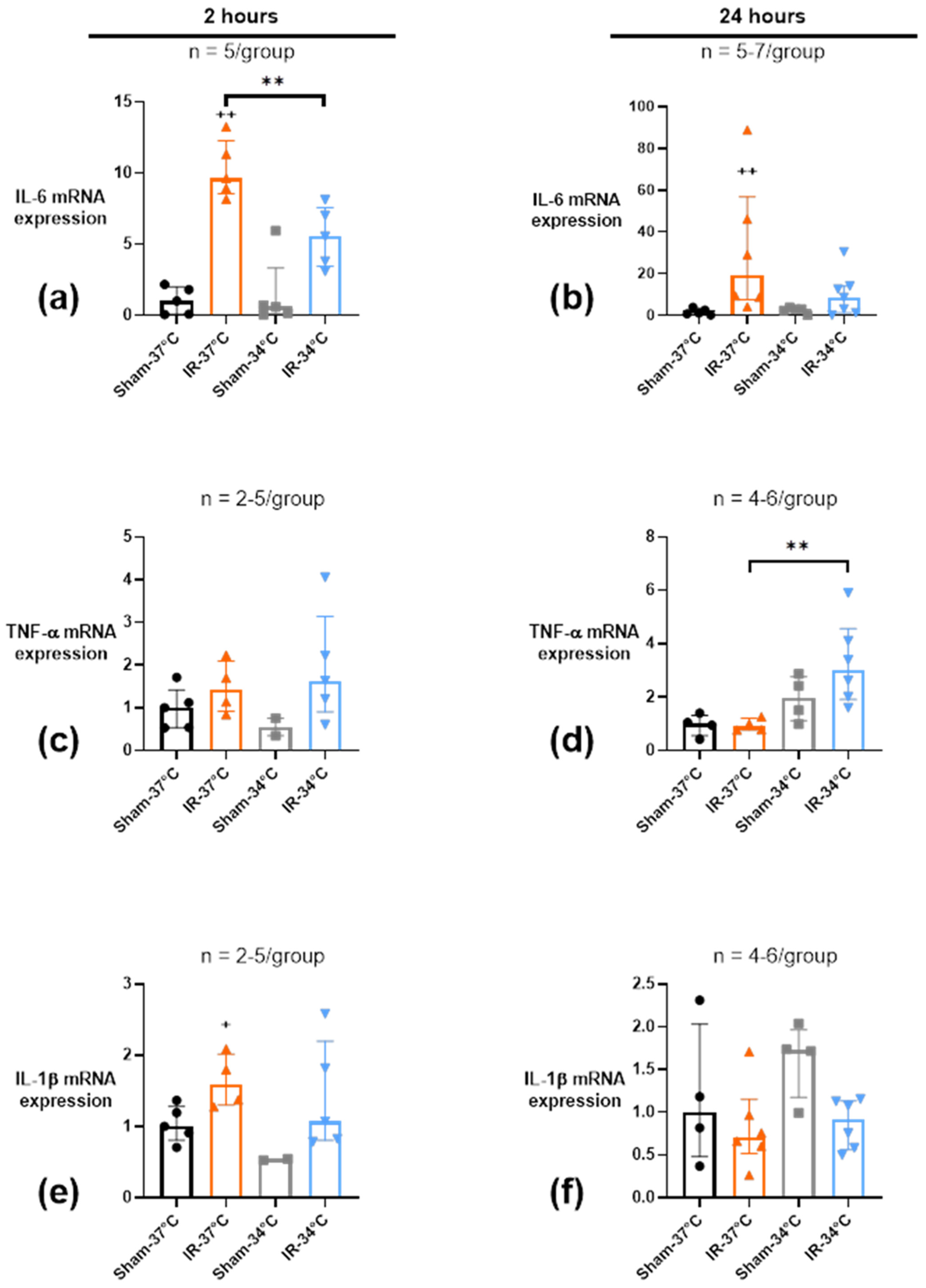
2.4.2. Acute Renal Inflammation
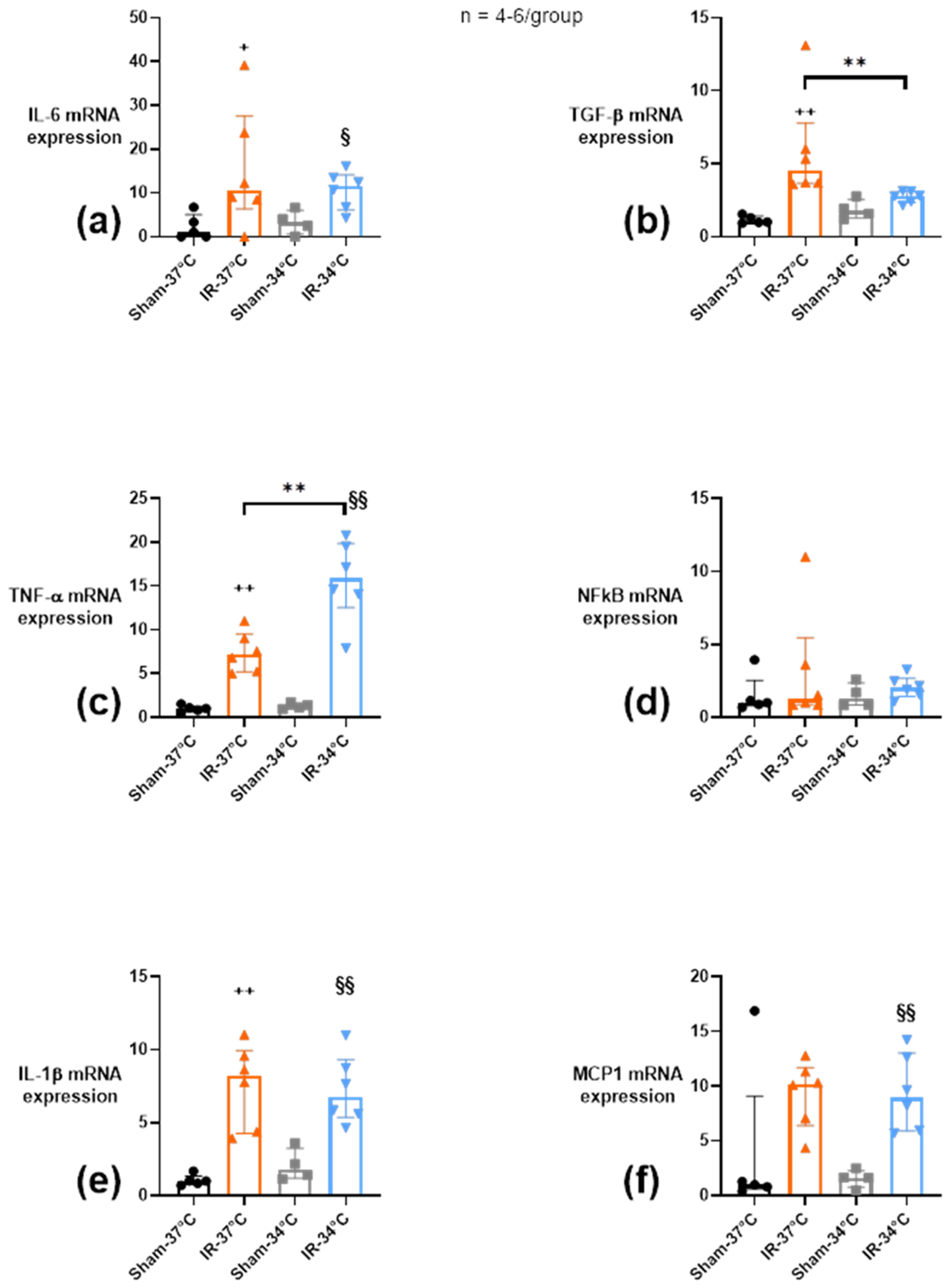
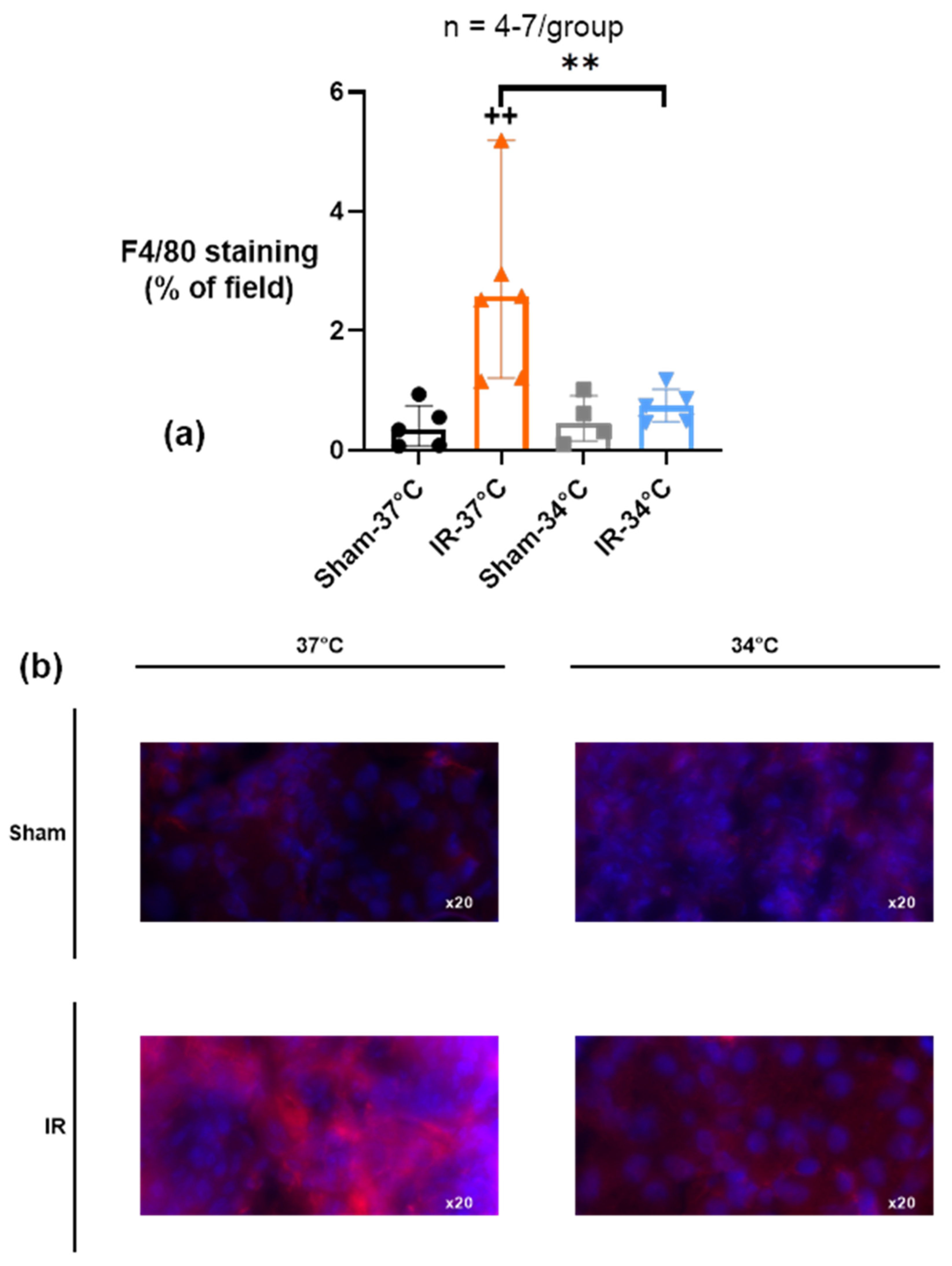
2.4.3. Chronic Renal Inflammation
3. Discussion
4. Materials and Methods
4.1. Animals and Surgical Procedures
4.2. Experimental Design
4.3. Renal Investigations
4.3.1. Urea Titration
4.3.2. Renal Histological Analysis
4.4. Mitochondrial Investigations
4.4.1. Preparation of Isolated Mitochondria
4.4.2. Calcium Retention Capacity
4.4.3. Mitochondrial Oxidative Phosphorylation (OX-PHOS)
4.5. Renal Ultrasound Imaging
4.6. Inflammation Quantification
4.6.1. Enzyme Linked Immunosorbent Assay (ELISA)
4.6.2. Quantitative Real-Time PCR (qRT-PCR)
4.6.3. Immunofluorescence
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eltzschig, H.K.; Eckle, T. Ischemia and reperfusion—From mechanism to translation. Nat. Med. 2011, 17, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Coca, S.; Yusuf, B.; Shlipak, M.G.; Garg, A.X.; Parikh, C.R. Long-term Risk of Mortality and Other Adverse Outcomes After Acute Kidney Injury: A Systematic Review and Meta-analysis. Am. J. Kidney Dis. 2009, 53, 961–973. [Google Scholar] [CrossRef] [PubMed]
- Yellon, D.M.; Hausenloy, D.J. Myocardial reperfusion injury. N. Engl. J. Med. 2007, 357, 1121–1135. [Google Scholar] [CrossRef] [PubMed]
- Cariou, A.; Payen, J.-F.; Asehnoune, K.; Audibert, G.; Botte, A.; Brissaud, O.; Debaty, G.; Deltour, S.; Deye, N.; Engrand, N.; et al. Targeted temperature management in the ICU: Guidelines from a French expert panel. Anaesth. Crit. Care Pain Med. 2017, 37, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.; Servillo, G.; Sutherasan, Y.; Rodríguez-González, R.; Brunetti, I.; Pelosi, P. Effects of in-hospital low targeted temperature after out of hospital cardiac arrest: A systematic review with meta-analysis of randomized clinical trials. Resuscitation 2015, 91, 8–18. [Google Scholar] [CrossRef]
- Lascarrou, J.-B.; Merdji, H.; Le Gouge, A.; Colin, G.; Grillet, G.; Girardie, P.; Coupez, E.; Dequin, P.-F.; Cariou, A.; Boulain, T.; et al. Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm. N. Engl. J. Med. 2019, 381, 2327–2337. [Google Scholar] [CrossRef]
- Edwards, A.D.; Brocklehurst, P.; Gunn, A.; Halliday, H.; Juszczak, E.; Levene, M.; Strohm, B.; Thoresen, M.; Whitelaw, A.; Azzopardi, D. Neurological outcomes at 18 months of age after moderate hypothermia for perinatal hypoxic ischaemic encephalopathy: Synthesis and meta-analysis of trial data. BMJ 2010, 340, c363. [Google Scholar] [CrossRef]
- Jacobs, S.E.; Berg, M.; Hunt, R.; Tarnow-Mordi, W.O.; Inder, T.E.; Davis, P.G. Cooling for newborns with hypoxic ischaemic encepha-lopathy. Cochrane Database Syst. Rev. 2013, 2013, CD003311. [Google Scholar] [CrossRef]
- Niemann, C.U.; Feiner, J.; Swain, S.; Bunting, S.; Friedman, M.; Crutchfield, M.; Broglio, K.; Hirose, R.; Roberts, J.P.; Malinoski, D. Therapeutic Hypothermia in Deceased Organ Donors and Kidney-Graft Function. N. Engl. J. Med. 2015, 373, 405–414. [Google Scholar] [CrossRef]
- Baines, C.P.; Kaiser, R.A.; Purcell, N.H.; Blair, N.S.; Osinska, H.; Hambleton, M.A.; Brunskill, E.W.; Sayen, M.R.; Gottlieb, R.A.; Dorn, G.W., II.; et al. Loss of cyclophilin D reveals a critical role for mitochondrial permeability transition in cell death. Nature 2005, 434, 658–662. [Google Scholar] [CrossRef]
- Yang, C.W.; Ahn, H.J.; Han, H.J.; Kim, W.Y.; Li, C.; Shin, M.J.; Kim, S.K.; Park, J.H.; Kim, Y.S.; Moon, I.S.; et al. Pharmacological preconditioning with low-dose cyclosporine or FK506 reduces subsequent ischemia/reperfusion injury in rat kidney. Transplantation 2001, 72, 1753–1759. [Google Scholar] [CrossRef]
- Lemoine, S.; Pillot, B.; Rognant, N.; Augeul, L.; Rayberin, M.; Varennes, A.; Laville, M.; Ovize, M.; Juillard, L. Postconditioning With Cyclosporine A Reduces Early Renal Dysfunction by Inhibiting Mitochondrial Permeability Transition. Transplantation 2015, 99, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, S.; Pillot, B.; Augeul, L.; Rabeyrin, M.; Varennes, A.; Normand, G.; Baetz, D.; Ovize, M.; Juillard, L. Dose and timing of injections for effective cyclo-sporine A pretreatment before renal ischemia reperfusion in mice. PLoS ONE 2017, 12, e0182358. [Google Scholar] [CrossRef] [PubMed]
- Thurman, J.M. Triggers of inflammation after renal ischemia/reperfusion. Clin. Immunol. 2007, 123, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Chawla, L.S.; Kimmel, P.L. Acute kidney injury and chronic kidney disease: An integrated clinical syndrome. Kidney Int. 2012, 82, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Mulay, S.R.; Linkermann, A.; Anders, H.J. Necroinflammation in Kidney Disease. J. Am. Soc. Nephrol. JASN 2016, 27, 27–39. [Google Scholar] [CrossRef]
- Duffield, J.S. Cellular and molecular mechanisms in kidney fibrosis. J. Clin. Investig. 2014, 124, 2299–2306. [Google Scholar] [CrossRef]
- Kurts, C.; Panzer, U.; Anders, H.-J.; Rees, A.J. The immune system and kidney disease: Basic concepts and clinical implications. Nat. Rev. Immunol. 2013, 13, 738–753. [Google Scholar] [CrossRef]
- Tissier, R.; Cohen, M.V.; Downey, J.M. Does mild hypothermia protect against reperfusion injury? The debate continues. Basic Res. Cardiol. 2011, 106, 691–695. [Google Scholar] [CrossRef][Green Version]
- Dankiewicz, J.; Cronberg, T.; Lilja, G.; Jakobsen, J.C.; Levin, H.; Ullén, S.; Rylander, C.; Wise, M.P.; Oddo, M.; Cariou, A.; et al. Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2021, 384, 2283–2294. [Google Scholar] [CrossRef]
- Jahandiez, V.; Cour, M.; Bochaton, T.; Abrial, M.; Loufouat, J.; Gharib, A.; Varennes, A.; Ovize, M.; Argaud, L. Fast therapeutic hypothermia prevents post-cardiac arrest syndrome through cyclophilin D-mediated mitochondrial permeability transition inhibition. Basic Res. Cardiol. 2017, 112, 35. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.B.; Myers, B.D.; Derby, G.; Blouch, K.L.; Yan, J.; Ho, B.; Tan, J.C. Adaptive hyperfiltration in the aging kidney after contralateral nephrectomy. Am. J. Physiol. Physiol. 2006, 291, F629–F634. [Google Scholar] [CrossRef] [PubMed]
- Xia, Z.; Wang, W.; Xiao, Q.; Ye, Q.; Zhang, X.; Wang, Y. Mild Hypothermia Protects Renal Function in Ischemia-reperfusion Kidney: An Experimental Study in Mice. Transplant. Proc. 2018, 50, 3816–3821. [Google Scholar] [CrossRef] [PubMed]
- Cour, M.; Jahandiez, V.; Loufouat, J.; Ovize, M.; Argaud, L. Minor Changes in Core Temperature Prior to Cardiac Arrest Influence Outcomes: An Experimental Study. J. Cardiovasc. Pharmacol. Ther. 2015, 20, 407–413. [Google Scholar] [CrossRef]
- Yamamoto, S.; Yamamoto, M.; Nakamura, J.; Mii, A.; Yamamoto, S.; Takahashi, M.; Kaneko, K.; Uchino, E.; Sato, Y.; Fukuma, S.; et al. Spatiotemporal ATP Dynamics during AKI Predict Renal Prognosis. J. Am. Soc. Nephrol. 2020, 31, 2855–2869. [Google Scholar] [CrossRef]
- Le Dorze, M.; Bouglé, A.; Deruddre, S.; Duranteau, J. Renal Doppler ultrasound: A new tool to assess renal perfusion in critical illness. Shock 2012, 37, 360–365. [Google Scholar] [CrossRef]
- Broman, M.; Källskog, O. The effects of hypothermia on renal function and haemodynamics in the rat. Acta Physiol. Scand. 1995, 153, 179–184. [Google Scholar] [CrossRef]
- Cao, W.; Cui, S.; Yang, L.; Wu, C.; Liu, J.; Yang, F.; Liu, Y.; Bin, J.; Hou, F.F. Contrast-Enhanced Ultrasound for Assessing Renal Perfusion Impairment and Predicting Acute Kidney Injury to Chronic Kidney Disease Progression. Antioxid. Redox Signal. 2017, 27, 1397–1411. [Google Scholar] [CrossRef]
- Okumura, K.; Matsumoto, J.; Iwata, Y.; Yoshida, K.; Yoneda, N.; Ogi, T.; Kitao, A.; Kozaka, K.; Koda, W.; Kobayashi, S.; et al. Evaluation of renal oxygen saturation using photoa-coustic imaging for the early prediction of chronic renal function in a model of ischemia-induced acute kidney injury. PLoS ONE 2018, 13, e0206461. [Google Scholar] [CrossRef]
- Tissier, R.; Chenoune, M.; Pons, S.; Zini, R.; Darbera, L.; Lidouren, F.; Ghaleh, B.; Berdeaux, A.; Morin, D. Mild hypothermia reduces per-ischemic reactive oxygen species production and preserves mitochondrial respiratory complexes. Resuscitation 2013, 84, 249–255. [Google Scholar] [CrossRef]
- Gomez, L.; Paillard, M.; Thibault, H.; Derumeaux, G.; Ovize, M. Inhibition of GSK3beta by postconditioning is required to prevent opening of the mitochondrial permeability transition pore during reperfusion. Circulation 2008, 117, 2761–2768. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, T.; Rotaru, D.; Saba, H.; Smith, R.A.J.; Murphy, M.P.; MacMillan-Crow, L.A. The mitochondria-targeted antioxidant mi-toquinone protects against cold storage injury of renal tubular cells and rat kidneys. J. Pharmacol. Exp. Ther. 2011, 336, 682–692. [Google Scholar] [CrossRef] [PubMed]
- Parajuli, N.; Shrum, S.; Tobacyk, J.; Harb, A.; Arthur, J.; MacMillan-Crow, L.A. Renal cold storage followed by transplantation impairs expression of key mitochondrial fission and fusion proteins. PLoS ONE 2017, 12, e0185542. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.; MacMillan-Crow, L.A.; Parajuli, N. Renal cold storage followed by transplantation impairs proteasome function and mi-tochondrial protein homeostasis. Am. J. Physiol. Renal. Physiol. 2019, 316, F42–F53. [Google Scholar] [CrossRef] [PubMed]
- Maekawa, H.; Inoue, T.; Ouchi, H.; Jao, T.M.; Inoue, R.; Nishi, H.; Fujii, R.; Ishidate, F.; Tanaka, T.; Tanaka, Y.; et al. Mitochondrial Damage Causes Inflammation via cGAS-STING Signaling in Acute Kidney Injury. Cell Rep. 2019, 29, 1261–1273.e6. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Song, J.; Liu, Y.; Li, Y.; Liu, Z. Mild Hypothermia Protects Pigs’ Gastric Mucosa After Cardiopulmonary Resuscitation via Inhibiting Interleukin 6 (IL-6) Production. Med. Sci. Monit. 2016, 22, 3523–3528. [Google Scholar] [CrossRef]
- Xia, J.; Li, R.; Yang, R.; Zhang, L.; Sun, B.; Feng, Y.; Jin, J.; Huang, L.; Zhan, Q. Mild hypothermia attenuate kidney injury in canines with oleic acid-induced acute respiratory distress syndrome. Injury 2016, 47, 1445–1451. [Google Scholar] [CrossRef]
- Stewart, C.R.; Landseadel, J.P.; Gurka, M.J.; Fairchild, K.D. Hypothermia increases interleukin-6 and interleukin-10 in juvenile en-dotoxemic mice. Pediatr. Crit. Care Med. J. Soc. Crit. Care Med. World Fed. Pediatr. Intensive Crit. Care Soc. 2010, 11, 109–116. [Google Scholar]
- Cao, Q.; Harris, D.C.H.; Wang, Y. Macrophages in Kidney Injury, Inflammation, and Fibrosis. Physiology 2015, 30, 183–194. [Google Scholar] [CrossRef]
- Meng, X.-M.; Nikolic-Paterson, D.J.; Lan, H.Y. TGF-β: The master regulator of fibrosis. Nat. Rev. Nephrol. 2016, 12, 325–338. [Google Scholar] [CrossRef]
- Tang, P.M.K.; Nikolic-Paterson, D.J.; Lan, H.-Y. Macrophages: Versatile players in renal inflammation and fibrosis. Nat. Rev. Nephrol. 2019, 15, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Wowro, S.J.; Tong, G.; Krech, J.; Rolfs, N.; Berger, F.; Schmitt, K.R.L. Combined Cyclosporin A and Hypothermia Treatment Inhibits Activation of BV-2 Microglia but Induces an Inflammatory Response in an Ischemia/Reperfusion Hippocampal Slice Culture Model. Front. Cell. Neurosci. 2019, 13, 273. [Google Scholar] [CrossRef] [PubMed]
- Lv, W.; Booz, G.W.; Wang, Y.; Fan, F.; Roman, R.J. Inflammation and renal fibrosis: Recent developments on key signaling molecules as potential therapeutic targets. Eur. J. Pharmacol. 2018, 820, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, H.M.; White, D.M.; Domowicz, M.S.; Kraig, R.P. Cold pre-conditioning neuroprotection depends on TNF-α and is enhanced by blockade of interleukin-11. J. Neurochem. 2011, 117, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Ichas, F.; Jouaville, L.S.; Sidash, S.S.; Mazat, J.-P.; Holmuhamedov, E.L. Mitochondrial calcium spiking: A transduction mechanism based on calcium-induced permeability transition involved in cell calcium signalling. FEBS Lett. 1994, 348, 211–215. [Google Scholar] [CrossRef]
- Pfaffl, M.W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001, 29, e45. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schleef, M.; Gonnot, F.; Pillot, B.; Leon, C.; Chanon, S.; Vieille-Marchiset, A.; Rabeyrin, M.; Bidaux, G.; Guebre-Egziabher, F.; Juillard, L.; et al. Mild Therapeutic Hypothermia Protects from Acute and Chronic Renal Ischemia-Reperfusion Injury in Mice by Mitigated Mitochondrial Dysfunction and Modulation of Local and Systemic Inflammation. Int. J. Mol. Sci. 2022, 23, 9229. https://doi.org/10.3390/ijms23169229
Schleef M, Gonnot F, Pillot B, Leon C, Chanon S, Vieille-Marchiset A, Rabeyrin M, Bidaux G, Guebre-Egziabher F, Juillard L, et al. Mild Therapeutic Hypothermia Protects from Acute and Chronic Renal Ischemia-Reperfusion Injury in Mice by Mitigated Mitochondrial Dysfunction and Modulation of Local and Systemic Inflammation. International Journal of Molecular Sciences. 2022; 23(16):9229. https://doi.org/10.3390/ijms23169229
Chicago/Turabian StyleSchleef, Maxime, Fabrice Gonnot, Bruno Pillot, Christelle Leon, Stéphanie Chanon, Aurélie Vieille-Marchiset, Maud Rabeyrin, Gabriel Bidaux, Fitsum Guebre-Egziabher, Laurent Juillard, and et al. 2022. "Mild Therapeutic Hypothermia Protects from Acute and Chronic Renal Ischemia-Reperfusion Injury in Mice by Mitigated Mitochondrial Dysfunction and Modulation of Local and Systemic Inflammation" International Journal of Molecular Sciences 23, no. 16: 9229. https://doi.org/10.3390/ijms23169229
APA StyleSchleef, M., Gonnot, F., Pillot, B., Leon, C., Chanon, S., Vieille-Marchiset, A., Rabeyrin, M., Bidaux, G., Guebre-Egziabher, F., Juillard, L., Baetz, D., & Lemoine, S. (2022). Mild Therapeutic Hypothermia Protects from Acute and Chronic Renal Ischemia-Reperfusion Injury in Mice by Mitigated Mitochondrial Dysfunction and Modulation of Local and Systemic Inflammation. International Journal of Molecular Sciences, 23(16), 9229. https://doi.org/10.3390/ijms23169229







