Targeted Therapy and Immunotherapy in Early-Stage Non-Small Cell Lung Cancer: Current Evidence and Ongoing Trials
Abstract
:1. Introduction
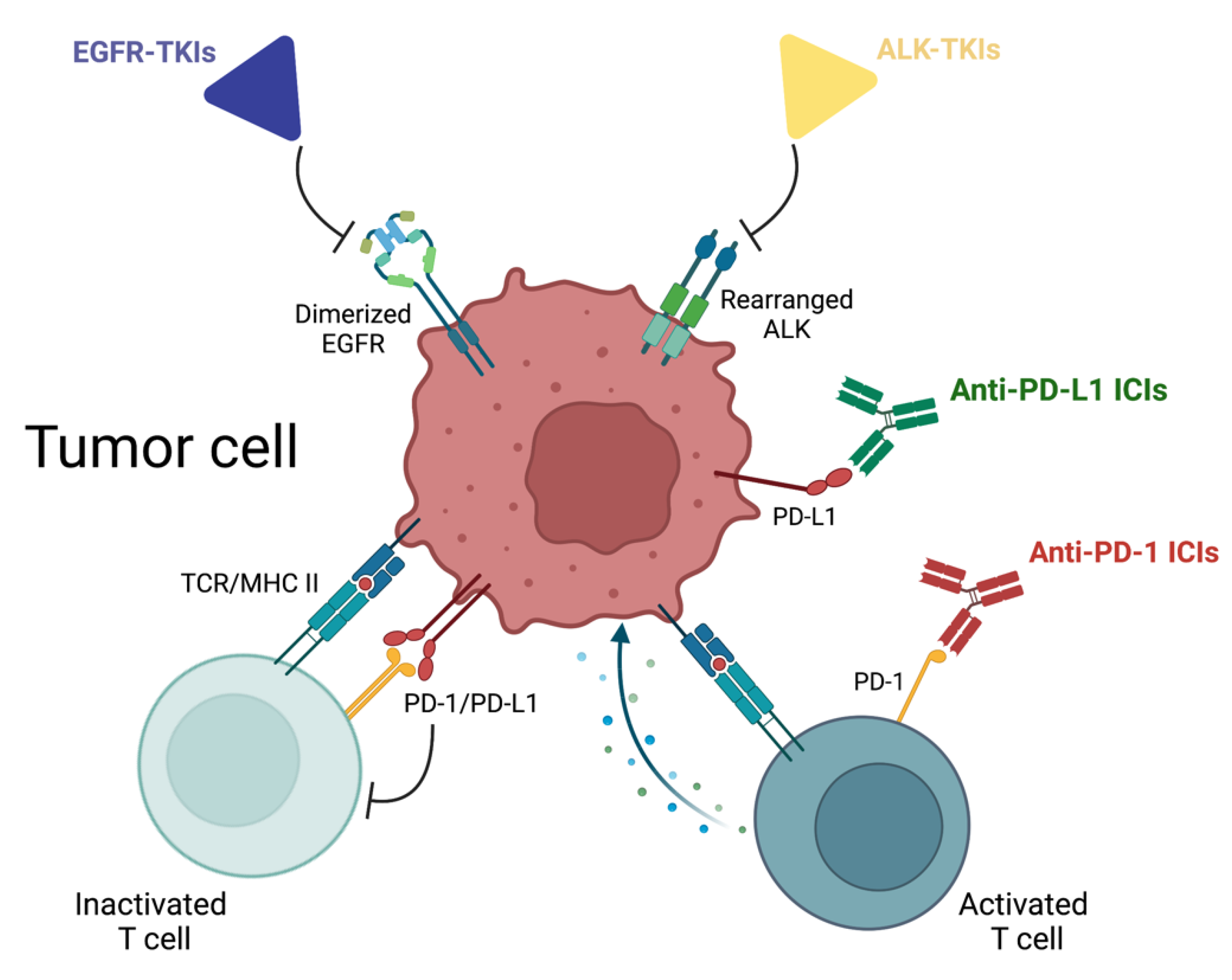
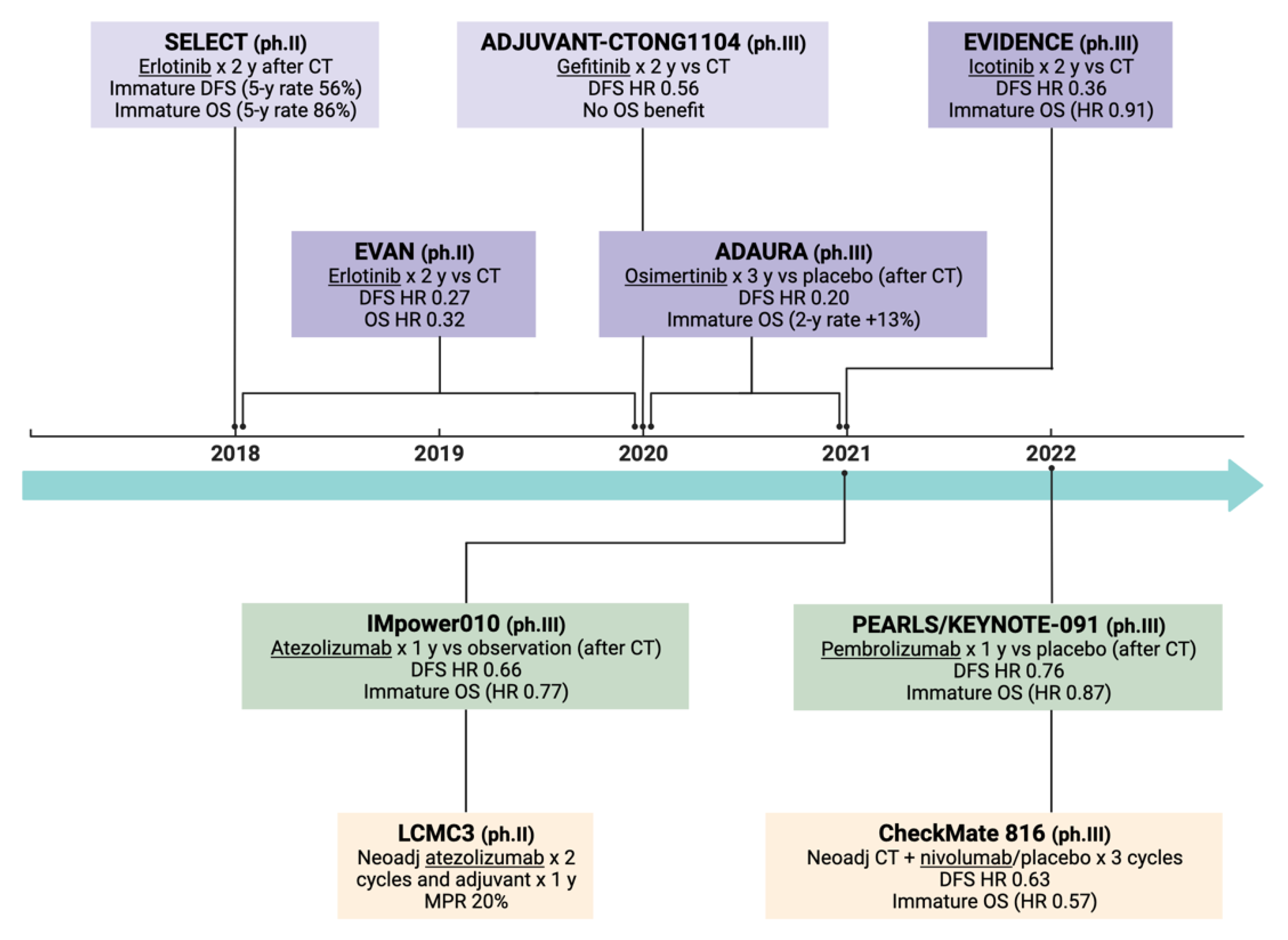
2. EGFR Tyrosine Kinase Inhibitors
2.1. Adjuvant Setting
2.2. Neoadjuvant Setting
3. ALK Tyrosine Kinase Inhibitors
4. Immune Checkpoint Inhibitors
4.1. Adjuvant Setting
4.2. Neodjuvant Setting
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pignon, J.-P.; Tribodet, H.; Scagliotti, G.V.; Douillard, J.-Y.; Shepherd, F.A.; Stephens, R.J.; Dunant, A.; Torri, V.; Rosell, R.; Seymour, L.; et al. Lung Adjuvant Cisplatin Evaluation: A Pooled Analysis by the LACE Collaborative Group. J. Clin. Oncol. 2008, 26, 3552–3559. [Google Scholar] [CrossRef]
- Burdett, S.; Pignon, J.P.; Tierney, J.; Tribodet, H.; Stewart, L.; Le Pechoux, C.; Aupérin, A.; Le Chevalier, T.; Stephens, R.J.; Arriagada, R.; et al. Adjuvant chemotherapy for resected early-stage non-small cell lung cancer. Cochrane Database Syst. Rev. 2015, 3, CD011430. [Google Scholar] [CrossRef]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.-L.; Yuan, J.-Q.; Wang, K.-F.; Fu, X.-H.; Han, X.-R.; Threapleton, D.; Yang, Z.-Y.; Mao, C.; Tang, J.-L. The prevalence of EGFR mutation in patients with non-small cell lung cancer: A systematic review and meta-analysis. Oncotarget 2016, 7, 78985–78993. [Google Scholar] [CrossRef] [Green Version]
- Rodig, S.J.; Mino-Kenudson, M.; Dacic, S.; Yeap, B.Y.; Shaw, A.; Barletta, J.A.; Stubbs, H.; Law, K.; Lindeman, N.; Mark, E.; et al. Unique Clinicopathologic Features Characterize ALK-Rearranged Lung Adenocarcinoma in the Western Population. Clin. Cancer Res. 2009, 15, 5216–5223. [Google Scholar] [CrossRef] [Green Version]
- Blackhall, F.H.; Peters, S.; Bubendorf, L.; Dafni, U.; Kerr, K.M.; Hager, H.; Soltermann, A.; O’Byrne, K.J.; Dooms, C.; Sejda, A.; et al. Prevalence and Clinical Outcomes for Patients With ALK-Positive Resected Stage I to III Adenocarcinoma: Results From the European Thoracic Oncology Platform Lungscape Project. J. Clin. Oncol. 2014, 32, 2780–2787. [Google Scholar] [CrossRef]
- Liang, H.; Huang, J.; Wang, B.; Liu, Z.; He, J.; Liang, W. The role of liquid biopsy in predicting post-operative recurrence of non-small cell lung cancer. J. Thorac. Dis. 2018, 10, S838–S845. [Google Scholar] [CrossRef] [Green Version]
- Abbosh, C.; Birkbak, N.J.; Swanton, C. Early stage NSCLC—challenges to implementing ctDNA-based screening and MRD detection. Nat. Rev. Clin. Oncol. 2018, 15, 577–586. [Google Scholar] [CrossRef]
- Takahashi, T.; Sakai, K.; Kenmotsu, H.; Yoh, K.; Daga, H.; Ohira, T.; Ueno, T.; Aoki, T.; Hayashi, H.; Yamazaki, K.; et al. Predictive value of EGFR mutation in non–small-cell lung cancer patients treated with platinum doublet postoperative chemotherapy. Cancer Sci. 2021, 113, 287–296. [Google Scholar] [CrossRef]
- Goss, G.D.; O’Callaghan, C.; Lorimer, I.; Tsao, M.-S.; Masters, G.A.; Jett, J.; Edelman, M.J.; Lilenbaum, R.; Choy, H.; Khuri, F.; et al. Gefitinib Versus Placebo in Completely Resected Non–Small-Cell Lung Cancer: Results of the NCIC CTG BR19 Study. J. Clin. Oncol. 2013, 31, 3320–3326. [Google Scholar] [CrossRef]
- Zhong, W.-Z.; Wang, Q.; Mao, W.-M.; Xu, S.-T.; Wu, L.; Wei, Y.-C.; Liu, Y.-Y.; Chen, C.; Cheng, Y.; Yin, R.; et al. Gefitinib Versus Vinorelbine Plus Cisplatin as Adjuvant Treatment for Stage II-IIIA (N1-N2) EGFR-Mutant NSCLC: Final Overall Survival Analysis of CTONG1104 Phase III Trial. J. Clin. Oncol. 2021, 39, 713–722. [Google Scholar] [CrossRef]
- Tada, H.; Mitsudomi, T.; Misumi, T.; Sugio, K.; Tsuboi, M.; Okamoto, I.; Iwamoto, Y.; Sakakura, N.; Sugawara, S.; Atagi, S.; et al. Randomized Phase III Study of Gefitinib Versus Cisplatin Plus Vinorelbine for Patients with Resected Stage II-IIIA Non–Small-Cell Lung Cancer with EGFR Mutation (IMPACT). J. Clin. Oncol. 2022, 40, 231–241. [Google Scholar] [CrossRef]
- Kelly, K.; Altorki, N.K.; Eberhardt, W.E.E.; O’Brien, M.E.R.; Spigel, D.R.; Crinò, L.; Tsai, C.-M.; Kim, J.-H.; Cho, E.K.; Hoffman, P.C.; et al. Adjuvant Erlotinib Versus Placebo in Patients with Stage IB-IIIA Non–Small-Cell Lung Cancer (RADIANT): A Randomized, Double-Blind, Phase III Trial. J. Clin. Oncol. 2015, 33, 4007–4014. [Google Scholar] [CrossRef]
- Pennell, N.A.; Neal, J.W.; Chaft, J.E.; Azzoli, C.G.; Jänne, P.A.; Govindan, R.; Evans, T.L.; Costa, D.B.; Wakelee, H.A.; Heist, R.S.; et al. SELECT: A Phase II Trial of Adjuvant Erlotinib in Patients with Resected Epidermal Growth Factor Receptor–Mutant Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2019, 37, 97–104. [Google Scholar] [CrossRef]
- Yue, D.; Xu, S.; Wang, Q.; Li, X.; Shen, Y.; Zhao, H.; Chen, C.; Mao, W.; Liu, W.; Liu, J.; et al. Erlotinib versus vinorelbine plus cisplatin as adjuvant therapy in Chinese patients with stage IIIA EGFR mutation-positive non-small-cell lung cancer (EVAN): A randomised, open-label, phase 2 trial. Lancet Respir. Med. 2018, 6, 863–873. [Google Scholar] [CrossRef]
- Yue, D.; Xu, S.-D.; Wang, Q.; Li, X.; Shen, Y.; Zhao, H.; Chen, C.; Mao, W.; Liu, W.; Liu, J.; et al. Updated overall survival (OS) and exploratory analysis from the randomized, phase II EVAN study of erlotinib (E) versus vinorelbine plus cisplatin (NP) as adjuvant therapy in Chinese patients with stage IIIA EGFR+ NSCLC. J. Clin. Oncol. 2021, 39, 8520. [Google Scholar] [CrossRef]
- He, J.; Su, C.; Liang, W.; Xu, S.; Wu, L.; Fu, X.; Zhang, X.; Ge, D.; Chen, Q.; Mao, W.; et al. Icotinib versus chemotherapy as adjuvant treatment for stage II–IIIA EGFR-mutant non-small-cell lung cancer (EVIDENCE): A randomised, open-label, phase 3 trial. Lancet Respir. Med. 2021, 9, 1021–1029. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Tsuboi, M.; He, J.; John, T.; Grohe, C.; Majem, M.; Goldman, J.W.; Laktionov, K.; Kim, S.-W.; Kato, T.; et al. Osimertinib in Resected EGFR-Mutated Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2020, 383, 1711–1723. [Google Scholar] [CrossRef]
- Wu, Y.-L.; John, T.; Grohe, C.; Majem, M.; Goldman, J.W.; Kim, S.-W.; Kato, T.; Laktionov, K.; Vu, H.V.; Wang, Z.; et al. Postoperative Chemotherapy Use and Outcomes From ADAURA: Osimertinib as Adjuvant Therapy for Resected EGFR-Mutated NSCLC. J. Thorac. Oncol. 2021, 17, 423–433. [Google Scholar] [CrossRef]
- Liu, Y.-T.; Hao, X.-Z.; Liu, D.-R.; Cheng, G.; Zhang, S.-C.; Xiao, W.-H.; Hu, Y.; Liu, J.-F.; He, M.; Ding, C.-M.; et al. Icotinib as Adjuvant Treatment for Stage II-IIIA Lung Adenocarcinoma Patients with EGFR Mutation (ICWIP Study): Study Protocol for a Randomised Controlled Trial. Cancer Manag. Res. 2020, 12, 4633–4643. [Google Scholar] [CrossRef]
- Yin, Q.; Xun, X.; Yang, G.; Cui, H.; Liu, H. Efficacy of Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in the Adjuvant Setting for Patients with Resected Epidermal Growth Factor Receptor Mutant Non-Small Cell Lung Cancer: A Meta-Analysis with 11 Trials. Oncol. Res. Treat. 2021, 44, 344–353. [Google Scholar] [CrossRef]
- Chen, R.-L.; Sun, L.-L.; Cao, Y.; Chen, H.-R.; Zhou, J.-X.; Gu, C.-Y.; Zhang, Y.; Wang, S.-Y.; Hou, W.; Lin, L.-Z. Adjuvant EGFR-TKIs for Patients with Resected EGFR-Mutant Non-Small Cell Lung Cancer: A Meta-Analysis of 1,283 Patients. Front. Oncol. 2021, 11, 629394. [Google Scholar] [CrossRef]
- Colclough, N.; Chen, K.; Johnström, P.; Strittmatter, N.; Yan, Y.; Wrigley, G.L.; Schou, M.; Goodwin, R.; Varnäs, K.; Adua, S.J.; et al. “Preclinical Comparison of the Blood–brain barrier Permeability of Osimertinib with Other EGFR TKIs. Clin. Cancer Res. 2020, 27, 189–201. [Google Scholar] [CrossRef]
- Lara-Guerra, H.; Waddell, T.K.; Salvarrey, M.A.; Joshua, A.M.; Chung, C.T.; Paul, N.; Boerner, S.; Sakurada, A.; Ludkovski, O.; Ma, C.; et al. Phase II Study of Preoperative Gefitinib in Clinical Stage I Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2009, 27, 6229–6236. [Google Scholar] [CrossRef]
- Zhong, W.; Yang, X.; Yan, H.; Zhang, X.; Su, J.; Chen, Z.; Liao, R.; Nie, Q.; Dong, S.; Zhou, Q.; et al. Phase II study of biomarker-guided neoadjuvant treatment strategy for IIIA-N2 non-small cell lung cancer based on epidermal growth factor receptor mutation status. J. Hematol. Oncol. 2015, 8, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Xiong, L.; Li, R.; Sun, J.; Lou, Y.; Zhang, W.; Bai, H.; Wang, H.; Shen, J.; Jing, B.; Shi, C.; et al. Erlotinib as Neoadjuvant Therapy in Stage IIIA (N2) EGFR Mutation-Positive Non-Small Cell Lung Cancer: A Prospective, Single-Arm, Phase II Study. Oncologist 2018, 24, 157-e64. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.-L.; Zhong, W.; Chen, K.-N.; Chen, C.; Yang, F.; Yang, X.-N.; Gu, C.; Mao, W.; Wang, Q.; Qiao, G.-B.; et al. CTONG1103: Final overall survival analysis of the randomized phase 2 trial of erlotinib versus gemcitabine plus cisplatin as neoadjuvant treatment of stage IIIA-N2 EGFR-mutant non–small cell lung cancer. J. Clin. Oncol. 2021, 39, 8502. [Google Scholar] [CrossRef]
- Tsuboi, M.; Weder, W.; Escriu, C.; Blakely, C.; He, J.; Dacic, S.; Yatabe, Y.; Zeng, L.; Walding, A.; Chaft, J.E. Neoadjuvant osimertinib with/without chemotherapy versus chemotherapy alone for EGFR-mutated resectable non-small-cell lung cancer: NeoADAURA. Futur. Oncol. 2021, 17, 4045–4055. [Google Scholar] [CrossRef]
- Yang, P.; Kulig, K.; Boland, J.M.; Erickson-Johnson, M.R.; Oliveira, A.M.; Wampfler, J.; Jatoi, A.; Deschamps, C.; Marks, R.; Fortner, C.; et al. Worse Disease-Free Survival in Never-Smokers with ALK+ Lung Adenocarcinoma. J. Thorac. Oncol. 2012, 7, 90–97. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.H.; Shim, H.S.; Kang, D.R.; Jung, J.Y.; Lee, C.Y.; Kim, D.J.; Lee, J.G.; Bae, M.K.; Kim, H.R.; Lim, S.M.; et al. Clinical and prognostic implications of ALK and ROS1 rearrangements in never-smokers with surgically resected lung adenocarcinoma. Lung Cancer 2014, 83, 389–395. [Google Scholar] [CrossRef]
- Seto, K.; Kuroda, H.; Yoshida, T.; Sakata, S.; Mizuno, T.; Sakakura, N.; Hida, T.; Yatabe, Y.; Sakao, Y. Higher frequency of occult lymph node metastasis in clinical N0 pulmonary adenocarcinoma with ALK rearrangement. Cancer Manag. Res. 2018, 10, 2117–2124. [Google Scholar] [CrossRef] [Green Version]
- Paik, J.H.; Choi, C.-M.; Kim, H.; Jang, S.J.; Choe, G.; Kim, D.K.; Kim, H.J.; Yoon, H.; Lee, C.-T.; Jheon, S.; et al. Clinicopathologic implication of ALK rearrangement in surgically resected lung cancer. Lung Cancer 2011, 76, 403–409. [Google Scholar] [CrossRef]
- Chaft, J.E.; Dagogo-Jack, I.; Santini, F.C.; Eng, J.; Yeap, B.Y.; Izar, B.; Chin, E.; Jones, D.R.; Kris, M.G.; Shaw, A.T.; et al. Clinical outcomes of patients with resected, early-stage ALK-positive lung cancer. Lung Cancer 2018, 122, 67–71. [Google Scholar] [CrossRef]
- Sands, J.; Mandrekar, S.J.; Oxnard, G.R.; Kozono, D.E.; Hillman, S.L.; Dahlberg, S.E.; Sun, Z.; Chaft, J.E.; Govindan, R.; Gerber, D.E.; et al. ALCHEMIST: Adjuvant targeted therapy or immunotherapy for high-risk resected NSCLC. J. Clin. Oncol. 2020, 38, TPS9077. [Google Scholar] [CrossRef]
- Solomon, B.J.; Ahn, J.S.; Barlesi, F.; Dziadziuszko, R.; Nishio, M.; Shaw, A.T.; Bordogna, W.; Meyenberg, C.; Wu, Y.-L. ALINA: A phase III study of alectinib versus chemotherapy as adjuvant therapy in patients with stage IB–IIIA anaplastic lymphoma kinase-positive (ALK+) non-small cell lung cancer (NSCLC). J. Clin. Oncol. 2019, 37, TPS8569. [Google Scholar] [CrossRef]
- Leonetti, A.; Minari, R.; Boni, L.; Gnetti, L.; Verzè, M.; Ventura, L.; Musini, L.; Tognetto, M.; Tiseo, M. Phase II, Open-label, Single-arm, Multicenter Study to Assess the Activity and Safety of Alectinib as Neoadjuvant Treatment in Surgically Resectable Stage III ALK-positive NSCLC: ALNEO Trial. Clin. Lung Cancer 2021, 22, 473–477. [Google Scholar] [CrossRef]
- Felip, E.; Altorki, N.; Zhou, C.; Csőszi, T.; Vynnychenko, I.; Goloborodko, O.; Luft, A.; Akopov, A.; Martinez-Marti, A.; Kenmotsu, H.; et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMpower010): A randomised, multicentre, open-label, phase 3 trial. Lancet 2021, 398, 1344–1357. [Google Scholar] [CrossRef]
- Paz-Ares, L.; O’Brien, M.E.R.; Mauer, M.; Dafni, U.; Oselin, K.; Havel, L.; Esteban Gonzalez, E.; Isla, D.; Martinez-Marti, A.; Faehling, M.; et al. VP3-2022: Pembrolizumab (pembro) versus placebo for early-stage non-small cell lung cancer (NSCLC) following complete resection and adjuvant chemotherapy (chemo) when indicated: Randomized, triple-blind, phase III EORTC-1416-LCG/ETOP 8-15–PEARLS/KEYNOTE-091 study. Ann. Oncol. 2022, 33, 451–453. [Google Scholar] [CrossRef]
- Lee, J.; Chaft, J.; Nicholas, A.; Patterson, A.; Waqar, S.; Toloza, E.; Haura, E.; Raz, D.; Reckamp, K.; Merritt, R.; et al. PS01.05 Surgical and Clinical Outcomes with Neoadjuvant Atezolizumab in Resectable Stage IB–IIIB NSCLC: LCMC3 Trial Primary Analysis. J. Thorac. Oncol. 2021, 16, S59–S61. [Google Scholar] [CrossRef]
- Forde, P.M.; Spicer, J.; Lu, S.; Provencio, M.; Mitsudomi, T.; Awad, M.M.; Felip, E.; Broderick, S.R.; Brahmer, J.R.; Swanson, S.J.; et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N. Engl. J. Med. 2022, 386, 1973–1985. [Google Scholar] [CrossRef]
- Sands, J.M.; Mandrekar, S.J.; Kozono, D.; Oxnard, G.R.; Hillman, S.L.; Wigle, D.A.; Govindan, R.; Carlisle, J.; Gray, J.; Salama, J.K.; et al. Integration of immunotherapy into adjuvant therapy for resected non-small-cell lung cancer: ALCHEMIST chemo-IO (ACCIO). Immunotherapy 2021, 13, 727–734. [Google Scholar] [CrossRef]
- Chaft, J.E.; Dahlberg, S.E.; Khullar, O.V.; Edelman, M.J.; Simone, C.B.; Heymach, J.; Rudin, C.M.; Ramalingam, S.S. EA5142 adjuvant nivolumab in resected lung cancers (ANVIL). J. Clin. Oncol. 2018, 36, TPS8581. [Google Scholar] [CrossRef]
- Calvo, V.; Domine, M.; Sullivan, I.; Gonzalez-Larriba, J.-L.; Ortega, A.L.; Bernabé, R.; Sala, M.A.; Campos, B.; De Castro, J.; Martín-Martorell, P.; et al. A phase III clinical trial of adjuvant chemotherapy versus chemoimmunotherapy for stage IB-IIIA completely resected non-small cell lung cancer (NSCLC) patients nadim-adjuvant: New adjuvant trial of chemotherapy versus chemoimmunotherapy. J. Clin. Oncol. 2021, 39, TPS8581. [Google Scholar] [CrossRef]
- Peters, S.; Spigel, D.; Ahn, M.; Tsuboi, M.; Chaft, J.; Harpole, D.; Goss, G.; Barlesi, F.; Abbosh, C.; Poole, L.; et al. P03.03 MERMAID-1: A Phase III Study of Adjuvant Durvalumab plus Chemotherapy in Resected NSCLC Patients with MRD+ Post-Surgery. J. Thorac. Oncol. 2021, 16, S258–S259. [Google Scholar] [CrossRef]
- Spigel, D.R.; Peters, S.; Ahn, M.-J.; Tsuboi, M.; Chaft, J.; Harpole, D.; Barlesi, F.; Abbosh, C.; Mann, H.; May, R.; et al. MERMAID-2: Phase 3 Study of Durvalumab in Patients with Resected, Stage II-III NSCLC Who Become MRD+ After Curative-Intent Therapy. J. Thorac. Oncol. 2021, 16 (Suppl. S4), S737–S747. [Google Scholar]
- Peters, S.; Kim, A.W.; Solomon, B.; Gandara, D.R.; Dziadziuszko, R.; Brunelli, A.; Garassino, M.C.; Reck, M.; Wang, L.; To, I.; et al. IMpower030: Phase III study evaluating neoadjuvant treatment of resectable stage II-IIIB non-small cell lung cancer (NSCLC) with atezolizumab (atezo) + chemotherapy. Ann. Oncol. 2019, 30, ii30. [Google Scholar] [CrossRef]
- Tsuboi, M.; Luft, A.; Ursol, G.; Kato, T.; Levchenko, E.; Eigendorff, E.; Berard, H.; Zurawski, B.; Demedts, I.; Garassino, M.C.; et al. 1235TiP Perioperative pembrolizumab + platinum-based chemotherapy for resectable locally advanced non-small cell lung cancer: The phase III KEYNOTE-671 study. Ann. Oncol. 2020, 31, S801–S802. [Google Scholar] [CrossRef]
- Cascone, T.; Provencio, M.; Sepesi, B.; Lu, S.; Aanur, N.; Li, S.; Spicer, J. Checkmate 77T: A phase III trial of neoadjuvant nivolumab (NIVO) plus chemotherapy (chemo) followed by adjuvant nivo in resectable early-stage NSCLC. J. Clin. Oncol. 2020, 38, TPS9076. [Google Scholar] [CrossRef]
- Heymach, J.; Taube, J.; Mitsudomi, T.; Harpole, D.; Aperghis, M.; Trani, L.; Powell, M.; Dennis, P.; Reck, M. P1.18-02 The AEGEAN Phase 3 Trial of Neoadjuvant/Adjuvant Durvalumab in Patients with Resectable Stage II/III NSCLC. J. Thorac. Oncol. 2019, 14, S625–S626. [Google Scholar] [CrossRef]
| Clinical Trial | Phase | N° pts a | Years | Stage | Treatment Arms | DFS | OS |
|---|---|---|---|---|---|---|---|
| BR19 [10] (NCT00049543) | III | 503 (EGFRm- unselected) | 2002–2005 | IB-IIIA | Gefitinib × 2 y vs. placebo (after adj CT) (1:1) | No difference (HR 1.22, 95% CI 0.93–1.61, p = 0.15) | No difference (HR 1.24, 95% CI 0.94–1.64, p = 0.14) |
| ADJUVANT-CTONG1104 [11] (NCT01405079) | III | 222 | 2011–2014 | II-IIIA | Gefitinib × 2 y vs. adj CT (1:1) | 30.8 vs. 19.8 m (HR 0.56, 95% CI 0.40–0.79, p = 0.001) | 75.5 vs. 62.8 m (HR 0.92, 95% CI 0.62–1.36, p = 0.674) |
| IMPACT [12] (UMIN000006252) | III | 234 | 2011–2015 | II-III | Gefitinib × 2 y vs. adj CT (1:1) | 35.9 vs. 25.1 m (HR 0.92, 95% CI 0.67–1.28, p = 0.63) | No difference (HR 1.03, 95% CI 0.65–1.65, p = 0.89) |
| RADIANT [13] (NCT00373425) | III | 973 (‘EGFR- positive’) | 2007–2010 | IB-IIIA | Erlotinib × 2 y vs. placebo (after adj CT) (2:1) | 50.5 vs. 48.2 m (HR 0.90, 95% CI 0.74–1.10, p = 0.324) | Not reached (HR 1.13, 95% CI 0.88–1.45, p = 0.335) |
| SELECT [14] (NCT00567359) | II | 100 | 2008–2012 | IA-IIIA | Erlotinib × 2 y (after adj CT) | Not reached (5-year DFS rate 56%) | Not reached (5-year OS rate 86%) |
| EVAN [15,16] (NCT01683175) | II | 102 | 2012–2015 | IIIA | Erlotinib × 2 y vs. adj CT (1:1) | 42.4 vs. 21.0 m (HR 0.27, 95% CI 0.14–0.53, p < 0.0001) | 84.2 vs. 61.1 m (HR 0.32, 95% CI 0.15–0.67) |
| EVIDENCE [17] (NCT02448797) | III | 322 | 2015–2019 | II-IIIA | Icotinib × 2 y vs. adj CT (1:1) | 47.0 vs. 22.1 m (HR 0.36, 95% CI 0.24–0.55, p < 0.0001) | Not reached (HR 0.91, 95% CI 0.42–1.94) |
| ADAURA [18,19] (NCT02511106) | III | 682 | 2015–2019 | IB-IIIA | Osimertinib × 3 y vs. placebo (after adj CT or not) (1:1) | Not reached vs. 27.5 m (HR 0.20, 99% CI 0.14–0.30, p < 0.001) b | Not reached (2-year OS rate 98% vs. 85%) b |
| Clinical Trial | Phase | N° pts | Estimated Primary Completion | Stage | Treatment Arms | Primary Endpoint |
|---|---|---|---|---|---|---|
| NCT02518802 | III | 220 | Jan 2018 | II-IIIA | Gefitinib × 2 y started during or after CT vs. adj CT | DFS |
| NCT03381430 | II | 50 | Mar 2023 | IIIA N2 | Gefitinib × 2 y + adj RT | DFS |
| NCT02193282 | III | 450 a | Oct 2026 | IB-IIIA | Erlotinib × 2 y vs. placebo (after adj CT) | OS |
| ICWIP [20] (NCT02125240) | III | 124 | Dec 2018 | II-IIIA | Icotinib × 3 y vs. placebo | DFS |
| ICTAN (NCT01996098) | III | 318 | Jan 2020 | II-IIIA | Icotinib × 6 m vs. icotinib × 12 m vs. observation (after adj CT) | DFS |
| NCT03983811 | III | 174 | Oct 2021 | IIB-IIIA | Icotinib/placebo on days 8–15 during adj q21 CT cycles, then × 2 y | DFS |
| CORIN (NCT02264210) | II | 128 | Dec 2025 | IB | Icotinib × 12 m vs. observation | DFS |
| NCT01746251 | II | 92 | Nov 2020 | I-III | Afatinib × 3 m vs. afatinib × 2 y | RFS |
| ADAURA2 (NCT05120349) | III | 380 | Aug 2027 | IA2-IA3 | Osimertinib × 3 y vs. placebo | DFS |
| FORWARD (NCT04853342) | III | 318 | Dec 2023 | II-IIIA | Furmonertinib vs. placebo (after adj CT) | DFS |
| ATHEM (NCT05165355) | II | 90 | Nov 2024 | IB-IIA b | Furmonertinib × 3 y | DFS |
| NCT04687241 | III | 192 | Jan 2026 | II-IIIB N2 | Almonertinib vs. placebo (after adj CT) | DFS |
| APEX (NCT04762459) | III | 606 | May 2026 | II-IIIA | Almonertinib × 3 y vs. almonertinib + adj CT vs. adj CT (3:2:1) | DFS |
| Clinical Trial | Phase | N° pts | Estimated Primary Completion | Stage | Treatment Arms | Primary Endpoint |
|---|---|---|---|---|---|---|
| NCT03656393 | III | 48 | Jul 2020 | II-IIIA | Gefitinib × 56 d vs. CT × 6 w (+ adj CT if not responding disease) | 2-year DFS rate |
| NCT03203590 | III | 590 | Jan 2026 | II-IIIA | Gefitinib × 8 w vs. CT × 2 cycles | 2-year DFS rate |
| NCT03749213 | II | 36 | Feb 2022 | IIIA N2 | Neoadj icotinib × 8 w, then × 2 y after surgery | ORR |
| Neoafa (NCT04470076) | II | 30 | Dec 2021 | II-IIIB | Neoadj CT + afatinib (48 h after and until 24 h before CT) × 3 cycles, then adj afatinib × 2 y after surgery | MPR, ORR |
| NCT03433469 | II | 27 | Dec 2022 | I-IIIA | Neoadj osimertinib × 1–2 cycles | MPR |
| NeoADAURA [28] (NCT04351555) | III | 328 | Mar 2024 | II-IIIB N2 | Neoadj osimertinib + CT × 3 cycles vs. placebo + CT vs. osimertinib alone (1:1:1) | MPR |
| Clinical Trial | Phase | N° pts | Estimated Primary Completion | Stage | Treatment Arms | Primary Endpoint |
|---|---|---|---|---|---|---|
| ALCHEMIST [34] (NCT02194738) | III | 8300 a | Sep 2026 | IB-IIIA | Crizotinib × 2 y vs. observation (after adj CT) | OS |
| ALINA [35] (NCT03456076) | III | 257 | Jun 2023 | IB-IIIA | Alectinib × 2 y vs. adj CT | DFS |
| NCT05341583 | III | 202 | Jun 2025 | II-IIIB | Ensartinib × 2 y vs. placebo | DFS |
| NCT05186506 | II | 152 | Dec 2025 | II-IIIA | Ensartinib × 2 y vs. adj CT | DFS |
| NCT05241028 | II | 80 | Feb 2027 | IB-IIIA | Ensartinib × 3 y (after adj CT) | 3-year DFS rate |
| ALNEO [36] (NCT05015010) | II | 33 | May 2023 | III | Neoadj alectinib × 8 w, then adj × 96 w after surgery | MPR |
| NAUTIKA1 (NCT04302025) | II | 80 a | Mar 2023 | IB-III | Neoadj alectinib × 8 w, then adj CT and alectinib × 2 y | MPR |
| Clinical Trial | Phase | N° pts | Years | Stage | Treatment Arms | DFS | OS |
|---|---|---|---|---|---|---|---|
| IMpower010 [37] (NCT02486718) | III | 1280 | 2015–2018 | IB-IIIA | Atezolizumab × 1 y vs. observation (after adj CT) (1:1) | Not reached vs. 35.3 m (HR 0.66, 95% CI 0.50–0.88, p = 0.0039) a | Immature data (HR 0.77, 95% CI 0.51–1.17) a |
| PEARLS/KEYNOTE-091 [38] (NCT02504372) | III | 1177 | 2015–2021 | IB-IIIA | Pembrolizumab × 1 y vs. placebo (after adj CT) (1:1) | 53.6 vs. 42.0 m (HR 0.76, 95% CI 0.63–0.91, p = 0.0014) | Immature data (HR 0.87, 95% CI 0.57–1.18, p = 0.14) |
| LCMC3 [39] (NCT02927301) | II | 181 | 2017–2020 | IB-IIIB N2 | Neoadj atezolizumab × 2 cycles, then adj atezolizumab × 1 y | Not available (primary endpoint MPR 20%) | Not available |
| CheckMate 816 [40] (NCT02998528) | III | 773 | 2017–2019 | Ib-IIIA | Neoadj CT + nivolumab/placebo × 3 cycles (1:1) | 31.6 vs. 20.8 m b (HR 0.63, 97% CI 0.43–0.91, p = 0.005) | Immature data (HR 0.57, 99% CI 0.30–1.07) |
| Clinical Trial | Phase | N° pts | Estimated Primary Completion | Stage | Treatment Arms | Primary Endpoint |
|---|---|---|---|---|---|---|
| NCT04367311 | II | 100 a (ctDNA+) | Jan 2023 | IB-IIIA | CT + atezo × 4 cycles, then atezo × 13 more cycles | % pts ctDNA- b |
| ACCIO [41] (NCT04267848) | III | 1210 | Dec 2024 | II-IIIB | CT + concomitant pembro × 4 cycles, then pembro × 13 cycles vs. CT + sequential pembro × 17 cycles vs. CT (1:1:1) | DFS |
| NCT04317534 | II | 368 | Apr 2025 | I | Pembro q42 × 9 cycles vs. observation (1:1) | DFS |
| ANVIL [42] (NCT02595944) | III | 903 | Jul 2024 | IB-IIIA | Nivolumab × 1 y vs observation (after adj CT) (1:1) | DFS, OS |
| NADIM- ADJUVANT [43] (NCT04564157) | III | 210 | Apr 2027 | IB-IIIA | CT + nivolumab q21 × 4 cycles, then nivolumab q28 × 6 cycles vs. CT × 4 cycles (1:1) | DFS |
| BR31 (NCT02273375) | III | 1415 | Jan 2023 | IB-IIIB N2 | Durvalumab × 1 y vs observation (after adj CT) (1:1) | DFS c |
| MERMAID-1 [44] (NCT04385368) | III | 332 | Dec 2024 | II-III | CT + durvalumab/placebo q21 × 4 cycles, then durvalumab/placebo q28 × 1 y (1:1) | DFS in ctDNA+ |
| MERMAID-2 [45] (NCT04642469) | III | 284 a (ctDNA+) | Nov 2025 | II-III | Durvalumab vs. placebo × 2 y (after (neo-)adj CT) (1:1) | DFS d |
| LungMate-008 (NCT04772287) | III | 341 | Dec 2026 | II-IIIB N2 | Toripalimab vs. placebo × 4 cycles (after adj CT) | DFS |
| IMpower-030 [46] (NCT03456063) | III | 451 | Nov 2024 | II-IIIB N2 | Neoadj CT + atezo × 4 cycles, then adj atezo × 16 cycles vs. neoadj CT + placebo and no adj treatment | EFS |
| NCT04832854 | II | 82 | Feb 2027 | II-IIIB N2 | Neoadj CT + atezo + tiragolumab × 4 cycles, then adj atezo + tiragolumab × 16 cycles | MPR |
| KEYNOTE-671 [47] (NCT03425643) | III | 786 | Jan 2024 | II-IIIB N2 | Neoadj CT + pembro/placebo × 4 cycles, then adj pembro/placebo × 13 cycles (1:1) | EFS, OS |
| INNWOP1 (NCT04875585) | II | 33 | Dec 2023 | I-IIIA | Neoadj pembro + lenvatinib × 6 w, then adj pembro × 15 cycles | MPR |
| CANOPY-N (NCT03968419) | II | 88 | Apr 2022 | IB-IIIA (no T4 or N2) | Neoadj pembrolizumab vs. canakinumab vs. pembrolizumab + canakinumab × 2 cycles | MPR |
| CheckMate 77T [48] (NCT04025879) | III | 452 | Dec 2023 | II-IIIB N2 | Neoadj CT + nivolumab/placebo, then adj nivolumab/placebo | EFS |
| GECP 16/03_NADIM (NCT03081689) | II | 46 | Jun 2022 | IIIA N2 | Neoadj CT + nivolumab × 3 cycles, then adj nivolumab × 1 y | 2-year PFS rate |
| NADIM II (NCT03838159) | II | 86 | Nov 2026 | IIIA-IIIB N2 | Neoadj CT + nivolumab/placebo, then adj nivolumab/observation | pCR |
| NeoCOAST 2 (NCT05061550) | II | 140 | Feb 2026 | II-IIIA | Neoadj CT + durvalumab + monalizumab/oleclumab q21 × 4 cycles, then adj monalizumab/oleclumab q28 (1:1) | pCR rate |
| AEGEAN [49] (NCT03800134) | III | 824 | Apr 2024 | II-IIIB N2 | Neoadj CT + durvalumab/placebo q21 × 4 cycles, then adj durvalumab/placebo q28 × 12 cycles (1:1) | pCR rate, EFS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Scordilli, M.; Michelotti, A.; Bertoli, E.; De Carlo, E.; Del Conte, A.; Bearz, A. Targeted Therapy and Immunotherapy in Early-Stage Non-Small Cell Lung Cancer: Current Evidence and Ongoing Trials. Int. J. Mol. Sci. 2022, 23, 7222. https://doi.org/10.3390/ijms23137222
de Scordilli M, Michelotti A, Bertoli E, De Carlo E, Del Conte A, Bearz A. Targeted Therapy and Immunotherapy in Early-Stage Non-Small Cell Lung Cancer: Current Evidence and Ongoing Trials. International Journal of Molecular Sciences. 2022; 23(13):7222. https://doi.org/10.3390/ijms23137222
Chicago/Turabian Stylede Scordilli, Marco, Anna Michelotti, Elisa Bertoli, Elisa De Carlo, Alessandro Del Conte, and Alessandra Bearz. 2022. "Targeted Therapy and Immunotherapy in Early-Stage Non-Small Cell Lung Cancer: Current Evidence and Ongoing Trials" International Journal of Molecular Sciences 23, no. 13: 7222. https://doi.org/10.3390/ijms23137222
APA Stylede Scordilli, M., Michelotti, A., Bertoli, E., De Carlo, E., Del Conte, A., & Bearz, A. (2022). Targeted Therapy and Immunotherapy in Early-Stage Non-Small Cell Lung Cancer: Current Evidence and Ongoing Trials. International Journal of Molecular Sciences, 23(13), 7222. https://doi.org/10.3390/ijms23137222







