Pharmacotherapy Based on ACE2 Targeting and COVID-19 Infection
Abstract
:1. COVID-19
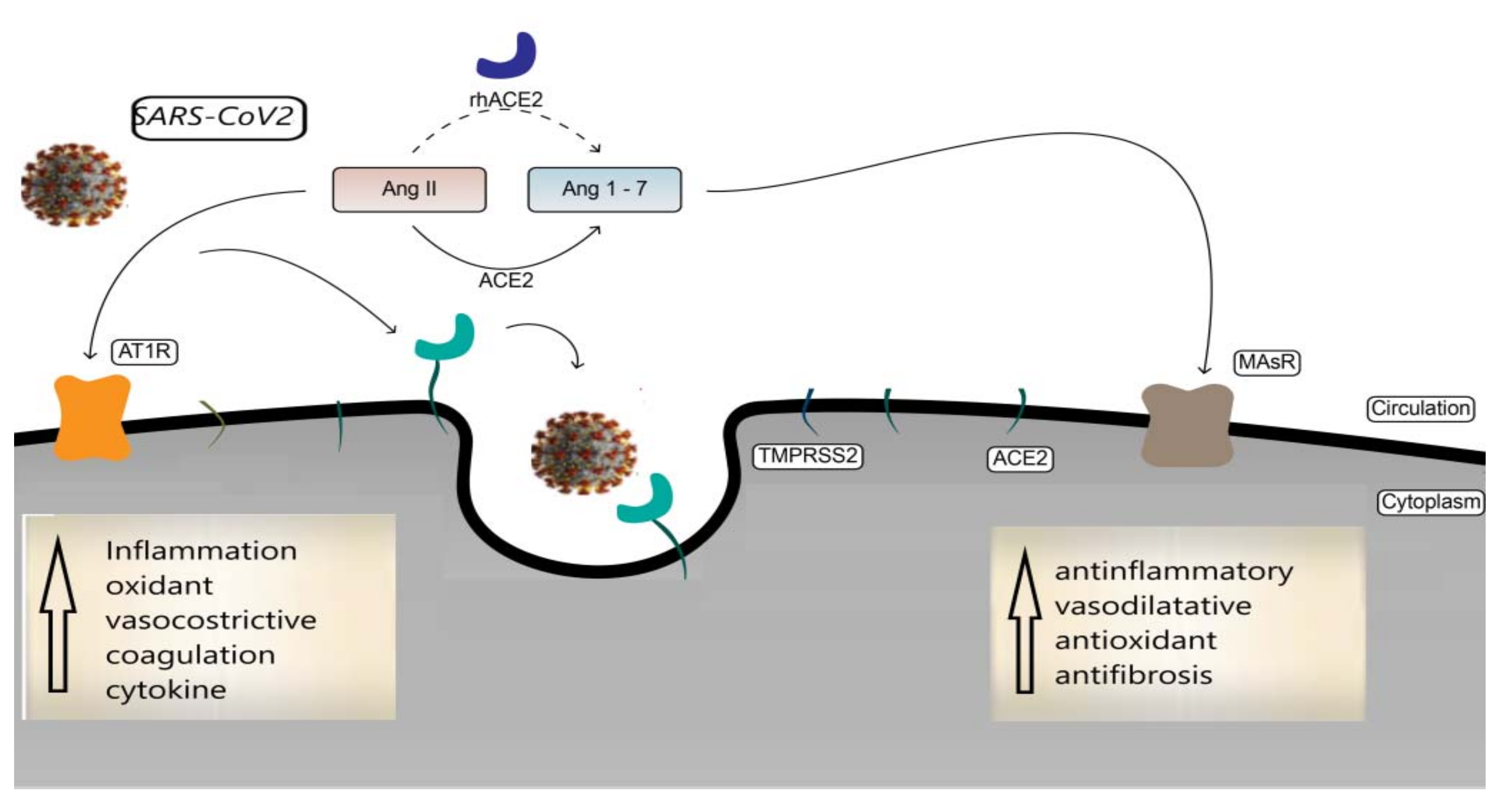
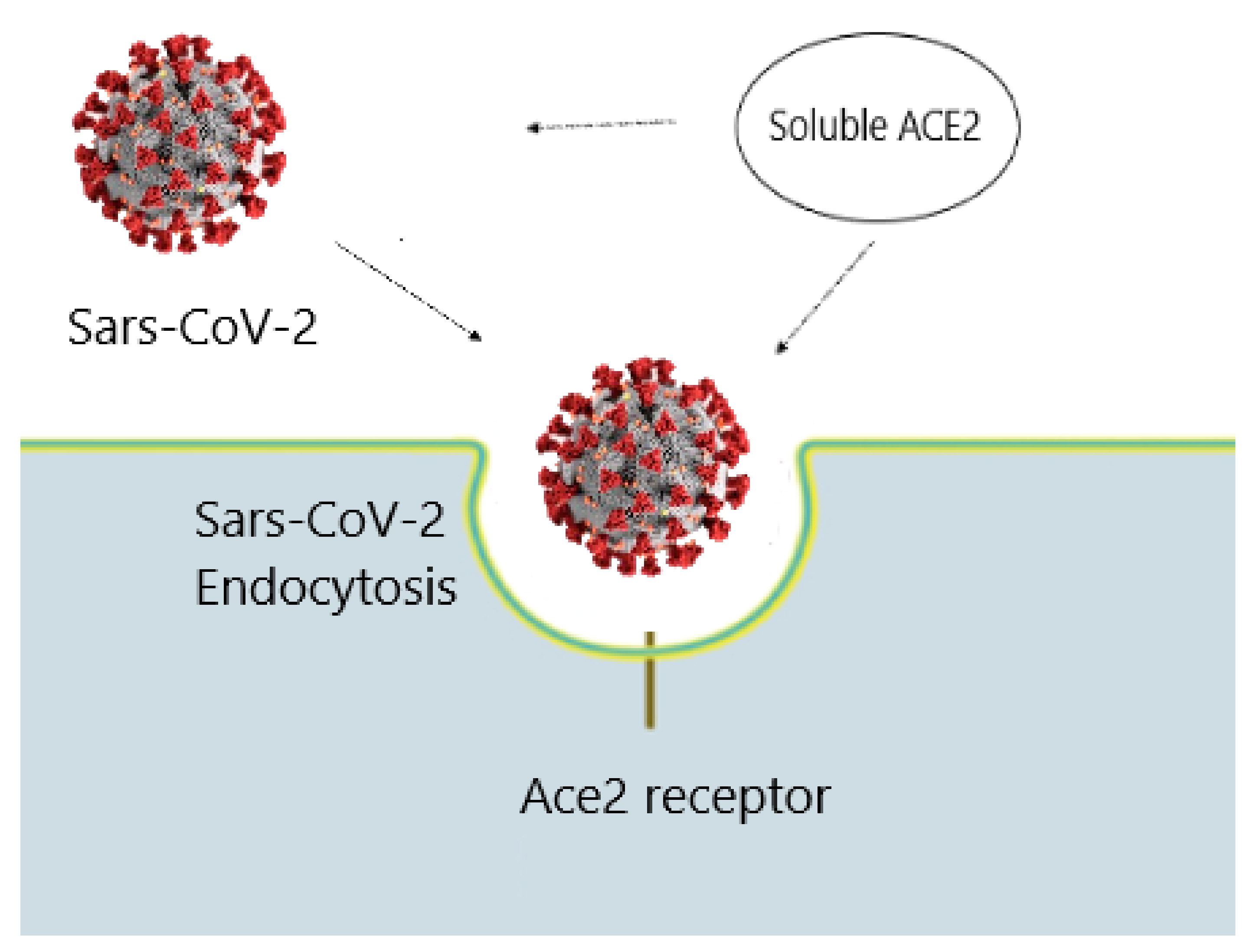
2. The Role of ACE2
3. Pharmacological Approach on ACE2
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| renin-angiotensin system | (RAS) |
| acute respiratory distress syndrome | (ARDS) |
| angiotensin-converting enzyme 2 | (ACE2) |
References
- World Health Organization (WHO). Situation Reports May 2022. Available online: https://www.who.int/emergencies/diseases/novelcoronavirus2019/situation-reports (accessed on 1 May 2022).
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Huang, C. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Li, Q. Early transmission dynamics in Wuhan, China, of novel coronavirus- infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Gorbalenya, A.E. Severe acute respiratory syndrome-related coronavirus: The species and its viruses—A statement of the Coronavirus Study Group. Microbiology 2020, 5, 536–544. [Google Scholar] [CrossRef] [Green Version]
- Guarner, J. Three emerging coronaviruses in two decades. Am. J. Clin. Pathol. 2020, 153, 420–421. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F. Colchicine and SARS-CoV-2: Management of the hyperinflammatory state. Respir. Med. 2021, 178, 106322. [Google Scholar] [CrossRef]
- Vitiello, A.; La Porta, R.; D’Aiuto, V.; Ferrara, F. Pharmacological approach for the reduction of inflammatory and prothrombotic hyperactive state in COVID-19 positive patients by acting on complement cascade. Hum. Immunol. 2021, 82, 264–269. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F.; Pelliccia, C.; Granata, G.; La Porta, R. Cytokine storm and colchicine potential role in fighting SARS-CoV-2 pneumonia. Ital. J. Med. 2020, 14, 88–94. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F. Remdesivir versus ritonavir/lopinavir in COVID-19 patients. Ir. J. Med Sci. 2020, 18, 1249–1250. [Google Scholar] [CrossRef]
- Vitiello, A.; La Porta, R.; Ferrara, F. Sacubitril, valsartan and SARS-CoV-2. BMJ Evid. Based Med. 2020, 27, 205. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, F.; Vitiello, A. Efficacy of synthetic glucocorticoids in COVID-19 endothelites. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2021, 394, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, S.C.J.; Kebriaei, R.; Dresser, L.D. Remdesivir: Review of Pharmacology, Pre-clinical Data, and Emerging Clinical Experience for COVID-19. Pharmacotherapy 2020, 40, 659–671. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, F.; Granata, G.; Pelliccia, C.; La Porta, R.; Vitiello, A. The added value of pirfenidone to fight inflammation and fibrotic state induced by SARS-CoV-2: Anti-inflammatory and anti-fibrotic therapy could solve the lung complications of the infection? Eur. J. Clin. Pharmacol. 2020, 76, 1615–1618. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, A.; Pelliccia, C.; Ferrara, F. Drugs acting on the renin–angiotensin system and SARS-CoV-2. Drug Discov. Today 2021, 26, 870–874. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F. Therapeutic Strategies for SARS-CoV-2 acting on ACE-2. Eur. J. Pharm. Sci. 2021, 156, 105579. [Google Scholar] [CrossRef]
- Camargo-Martínez, W.; Lozada-Martínez, I.; Escobar-Collazos, A.; Navarro-Coronado, A.; Moscote-Salazar, L.; Pacheco-Hernández, A.; Janjua, T.; Bosque-Varela, P. Post-COVID 19 neurological syndrome: Implications for sequelae’s treatment. J. Clin. Neurosci. 2021, 88, 219–225. [Google Scholar] [CrossRef]
- Ma, L.; Song, K.; Huang, Y. Coronavirus Disease-2019 (COVID-19) and Cardiovascular Complications. Cardiothorac. Vasc. Anesth. 2021, 35, 1860–1865. [Google Scholar] [CrossRef]
- Madjunkov, M.; Dviri, M.; Librach, C. A comprehensive review of the impact of COVID-19 on human reproductive biology, assisted reproduction care and pregnancy: A Canadian perspective. J. Ovarian Res. 2020, 13, 140. [Google Scholar] [CrossRef]
- Gurwitz, D. Angiotensin receptor blockers as tentative SARSCoV-2 therapeutics. Drug Dev. Res. 2020, 81, 537–540. [Google Scholar] [CrossRef] [Green Version]
- Hamming, I.; Timens, W.; Bulthuis, M.; Lely, A.; Navis, G.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. A J. Pathol. Soc. Great Br. Irel. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Penninger, J.M.; Li, Y.; Zhong, N.; Slutsky, A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020, 46, 586–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashimoto, T.; Perlot, T.; Rehman, A.; Trichereau, J.; Ishiguro, H.; Paolino, M.; Penninger, J.M. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature 2012, 487, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, A.; La Porta, R.; Ferrara, F. Scientific hypothesis and rational pharmacological for the use of sacubitril/valsartan in cardiac damage caused by COVID-19. Med. Hypotheses 2021, 147, 110486. [Google Scholar] [CrossRef] [PubMed]
- Maza, M.D.C.; Úbeda, M.; Delgado, P. ACE2 Serum Levels as Predictor of Infectability and Outcome in COVID-19. Front. Immunol. 2022, 13, 836516. [Google Scholar] [CrossRef]
- Mortaz, E.; Jamaati, H.; Roofchayee, N.D.; Sheikhzade, H.; Mirenayat, M.; Sadeghi, M.; Lookzadeh, S.; Dezfuli, N.K.; Folkerts, G.; Mumby, S.; et al. Decreased serum levels of angiotensin converting enzyme (ACE)2 and enhanced cytokine levels with severity of COVID-19: Normalisation upon disease recovery. Heliyon 2022, 8, e08957. [Google Scholar] [CrossRef]
- Paz Ocaranza, M.; Riquelme, J.A.; García, L.; Jalil, J.E.; Chiong, M.; Santos, R.A.S.; Lavandero, S. Counter-regulatory renin-angiotensin system in cardiovascular disease. Nat. Rev. Cardiol. 2020, 17, 116–129. [Google Scholar] [CrossRef] [Green Version]
- Vaduganathan, M.; Vardeny, O.; Michel, T.; McMurray, J.J.V.; Pfeffer, M.A.; Solomon, S.D. Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. N. Engl. J. Med. 2020, 382, 1653–1659. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F. Correlation between renin-angiotensin system and Severe Acute Respiratory Syndrome Coronavirus 2 infection: What do we know? Eur. J. Pharmacol. 2020, 883, 173373. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F. Pharmacological agents to therapeutic treatment of cardiac injury caused by Covid-19. Life Sci. 2020, 262, 118510. [Google Scholar] [CrossRef]
- Imai, Y.; Kuba, K.; Penninger, J.M. Angiotensin-converting enzyme 2 in acute respiratory distress syndrome. Cell. Mol. Life Sci. 2007, 64, 2006–2012. [Google Scholar] [CrossRef] [PubMed]
- Muslim, S.; Nasrin, N.; Alotaibi, F.O.; Prasad, G.; Singh, S.K.; Alam, I.; Mustafa, G. Treatment Options Available for COVID-19 and an Analysis on Possible Role of Combination of rhACE2, Angiotensin (1-7) and Angiotensin (1-9) as Effective Therapeutic Measure. SN Compr. Clin. Med. 2020, 2, 1761–1766. [Google Scholar] [CrossRef] [PubMed]
- Tabassum, A.; Iqbal, M.S.; Sultan, S.; Alhuthali, R.A.; Alshubaili, D.I.; Sayyam, R.S.; Abyad, L.M.; Qasem, A.H.; Arbaeen, A.F. Dysregulated Bradykinin: Mystery in the Pathogenesis of COVID-19. Mediat. Inflamm. 2022, 2022, 7423537. [Google Scholar] [CrossRef] [PubMed]
- Monteil, V.; Kwon, H.; Prado, P.; Hagelkrüys, A.; Wimmer, R.A.; Stahl, M.; Leopoldi, A.; Garreta, E.; Hurtado Del Pozo, C.; Prosper, F.; et al. Inhibition of SARS-CoV-2 Infections in Engineered Human Tissues Using Clinical-Grade Soluble Human ACE2. Cell 2020, 181, 905–913e7. [Google Scholar] [CrossRef]
- Monteil, V.; Dyczynski, M.; Lauschke, V.M.; Kwon, H.; Wirnsberger, G.; Youhanna, S.; Zhang, H.; Slutsky, A.S.; Hurtado Del Pozo, C.; Horn, M.; et al. Human soluble ACE2 improves the effect of remdesivir in SARS-CoV-2 infection. EMBO Mol. Med. 2021, 13, e13426. [Google Scholar] [CrossRef]
- Vitiello, A.; Ferrara, F.; La Porta, R. Remdesivir and COVID-19 infection, therapeutic benefitsor unnecessary risks? Ir. J. Med. Sci. 2021, 190, 1637–1638. [Google Scholar] [CrossRef]
- Bilezikian, J.P.; Bikle, D.; Hewison, M.; Lazaretti-Castro, M.; Formenti, A.M.; Gupta, A.; Madhavan, M.V.; Nair, N.; Babalyan, V.; Hutchings, N.; et al. MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19. Eur. J. Endocrinol. 2020, 183, R133–R147. [Google Scholar] [CrossRef]
- Marquez, A.; Wysocki, J.; Pandit, J.; Batlle, D. An update on ACE2 amplification and its therapeutic potential. Acta Physiol. 2020, 231, e13513. [Google Scholar] [CrossRef]
- Chan, K.K.; Dorosky, D.; Sharma, P.; Abbasi, S.A.; Dye, J.M.; Kranz, D.M.; Herbert, A.S.; Procko, E. Engineering human ACE2 to optimize binding to the spike protein of SARS coronavirus 2. Science 2020, 369, 1261–1265. [Google Scholar] [CrossRef]
- Nussinov, R.; Tsai, C.J. The different ways through which specificity works in orthosteric and allosteric drugs. Curr. Pharm. Des. 2012, 18, 1311–1316. [Google Scholar] [CrossRef]
- Wang, D.S.; Hayatshahi, H.S.; Jayasinghe-Arachchige, V.M.; Liu, J. Allosteric Modulation of Small Molecule Drugs on ACE2 Conformational Change upon Binding to SARS-CoV-2 Spike Protein. In Proceedings of the 2021 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Houston, TX, USA, 9–12 December 2021; pp. 2587–2594. [Google Scholar] [CrossRef]
- Higuchi, Y.; Suzuki, T.; Arimori, T.; Ikemura, N.; Mihara, E.; Kirita, Y.; Ohgitani, E.; Mazda, O.; Motooka, D.; Nakamura, S. Engineered ACE2 receptor therapy overcomes mutational escape of SARS-CoV-2. Nat. Commun. 2021, 12, 3802. [Google Scholar] [CrossRef] [PubMed]
- Dutta, K. Allosteric Site of ACE-2 as a Drug Target for COVID-19. ACS Pharmacol. Transl Sci. 2022, 5, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Chen, Z.; Ni, L.; Chen, L.; Zhou, C.; Gao, C.; Wu, X.; Hua, L.; Huang, X.; Cui, X.; et al. Impact of Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers on the Inflammatory Response and Viral Clearance in COVID-19 Patients. Front. Cardiovasc. Med. 2021, 8, 710946. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, A.; Ferrara, F. Association and pharmacological synergism of the triple drug therapy baricitinib/remdesivir/rhACE2 for the management of COVID-19 infection. Naunyn Schmiedebergs Arch Pharmacol. 2022, 395, 99–104. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vitiello, A.; Ferrara, F. Pharmacotherapy Based on ACE2 Targeting and COVID-19 Infection. Int. J. Mol. Sci. 2022, 23, 6644. https://doi.org/10.3390/ijms23126644
Vitiello A, Ferrara F. Pharmacotherapy Based on ACE2 Targeting and COVID-19 Infection. International Journal of Molecular Sciences. 2022; 23(12):6644. https://doi.org/10.3390/ijms23126644
Chicago/Turabian StyleVitiello, Antonio, and Francesco Ferrara. 2022. "Pharmacotherapy Based on ACE2 Targeting and COVID-19 Infection" International Journal of Molecular Sciences 23, no. 12: 6644. https://doi.org/10.3390/ijms23126644
APA StyleVitiello, A., & Ferrara, F. (2022). Pharmacotherapy Based on ACE2 Targeting and COVID-19 Infection. International Journal of Molecular Sciences, 23(12), 6644. https://doi.org/10.3390/ijms23126644






