What Genetics Can Do for Oncological Imaging: A Systematic Review of the Genetic Validation Data Used in Radiomics Studies
Abstract
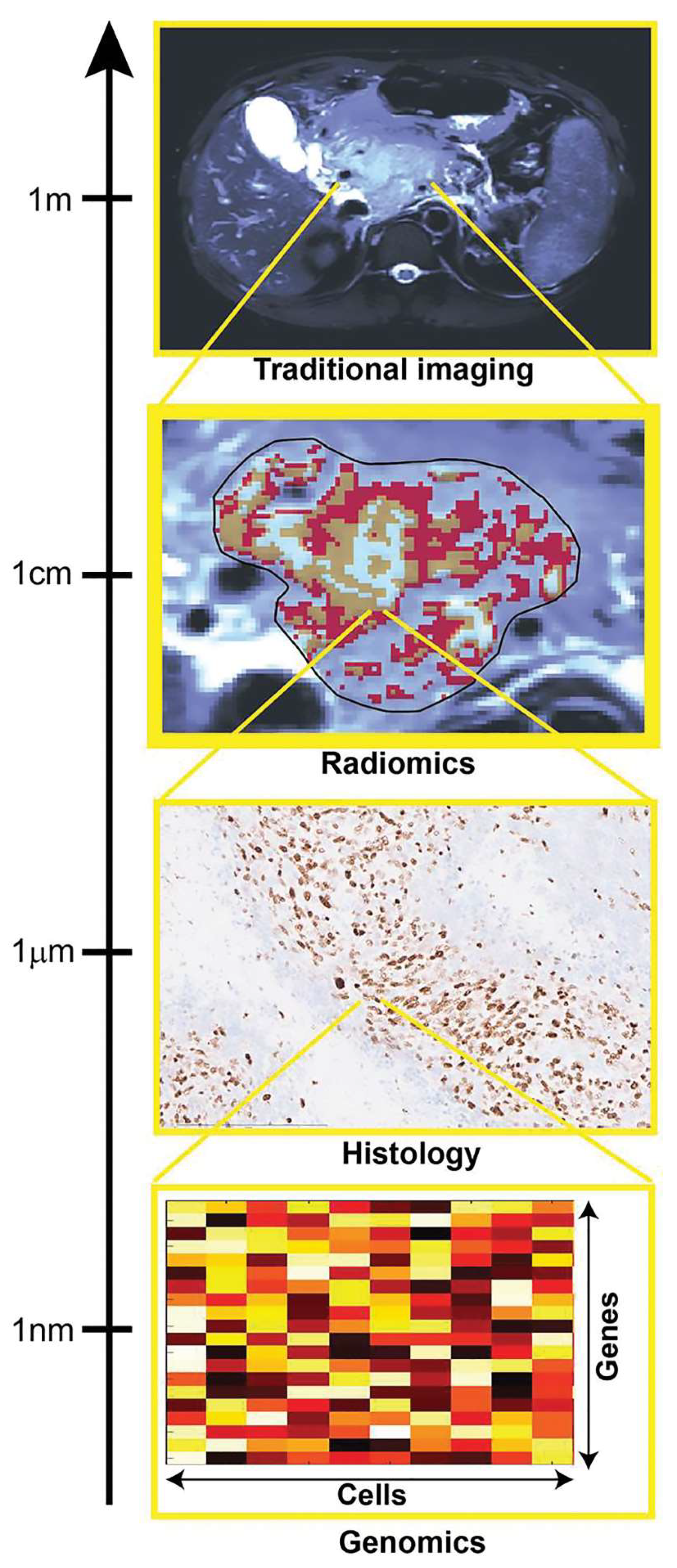
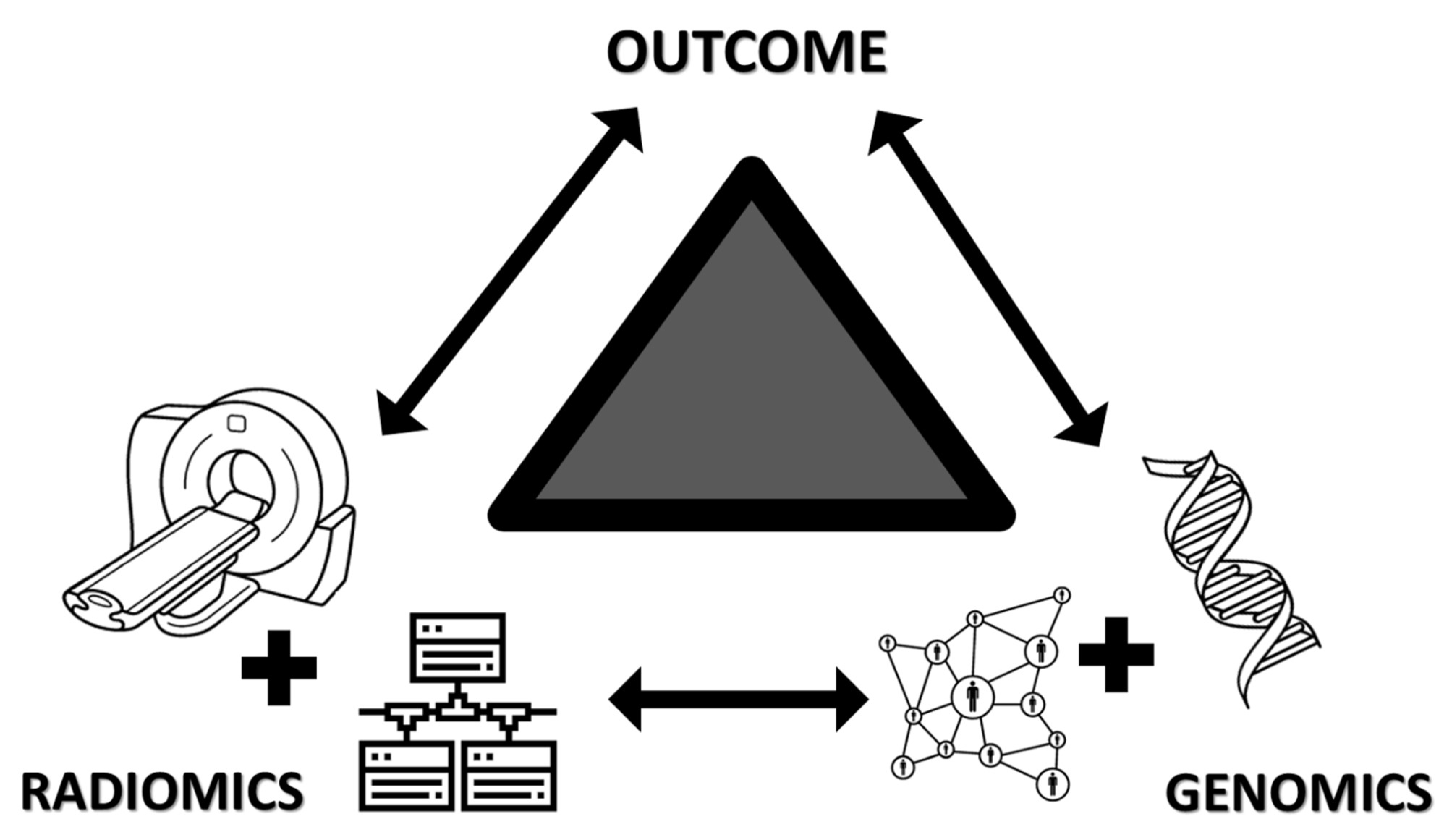
:1. Introduction
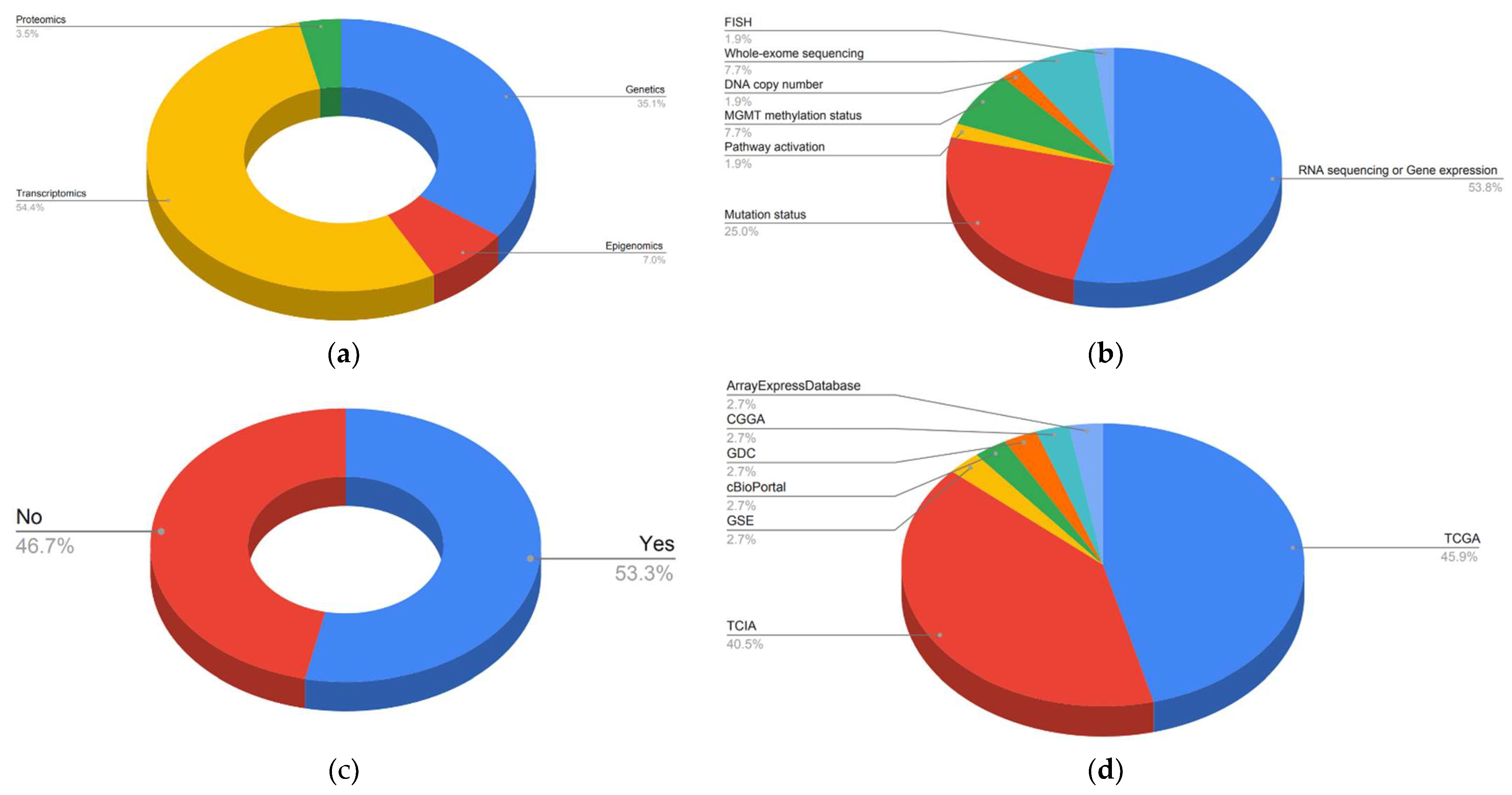
2. Results
2.1. Study Characteristics
2.2. Brain Tumors (Gliomas/Astrocytomas)
2.3. Lung and Head and Neck Cancers
2.4. Breast, Ovarian, and Endometrial Cancer
2.5. Urogenital Cancers (Kidney, Bladder, and Prostate)
2.6. Gastrointestinal Tumors (Esophagus, Gastric, Colon Cancer, and Hepatocellular Carcinoma)
2.7. Others (Melanoma, Solid Tumors)
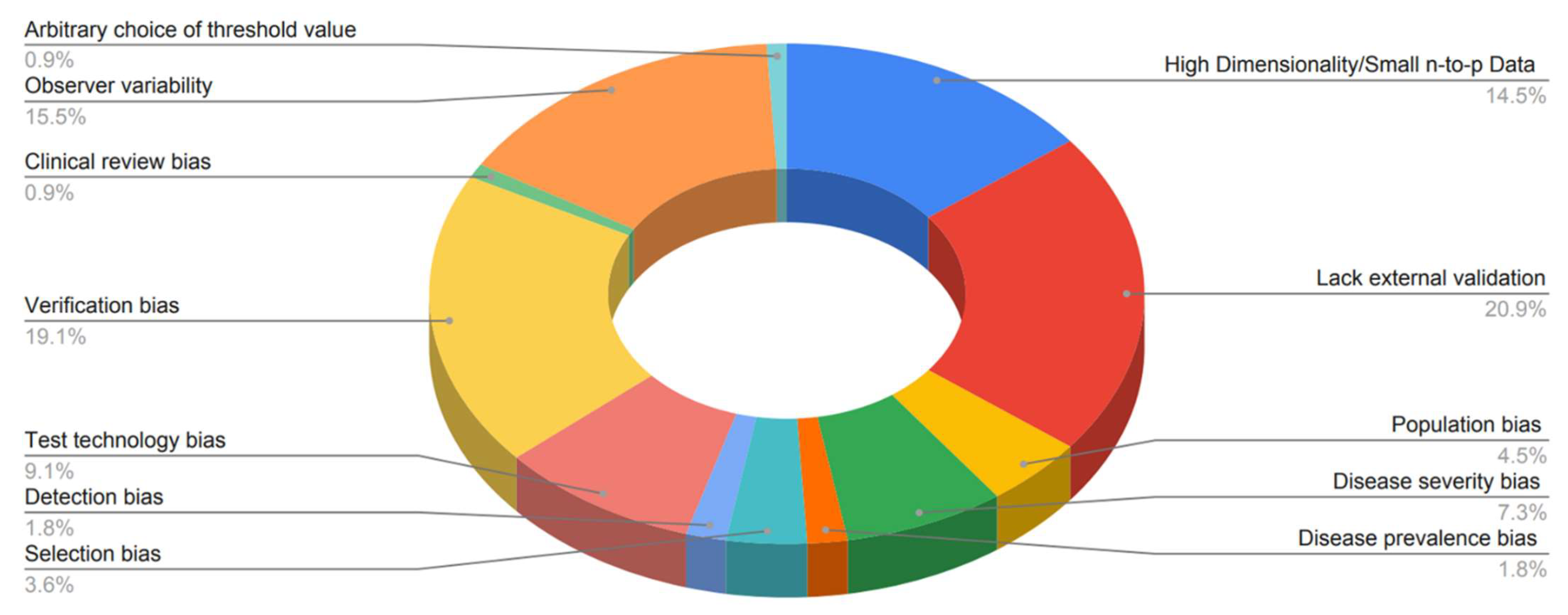
3. Discussion
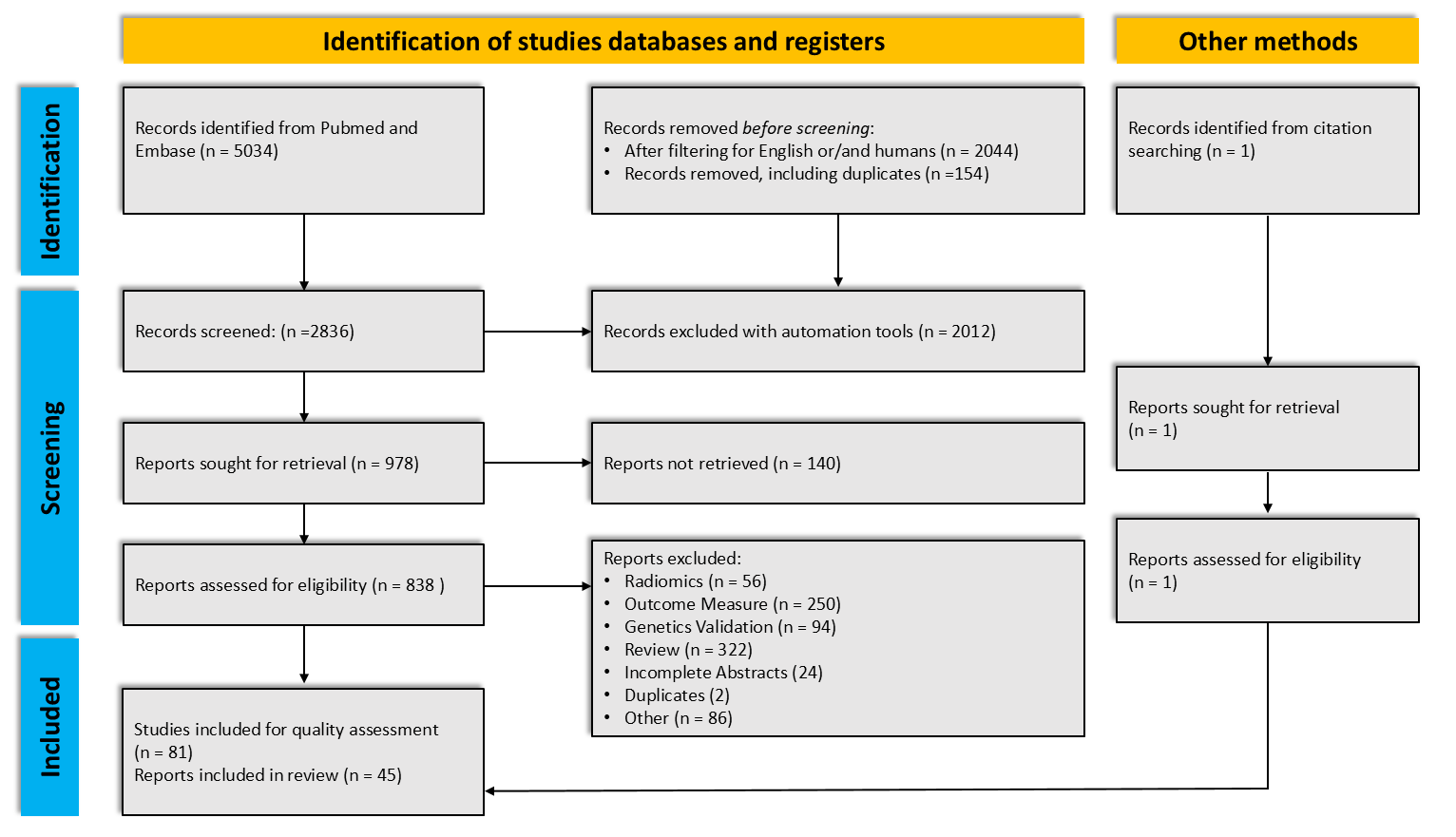
4. Materials and Methods
4.1. Search Strategy
4.2. Inclusion and Exclusion Criteria
4.3. Selection Process
4.4. Data Extraction and Quality Assessment
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADC | Apparent diffusion coefficient |
| AUC | area under the curve |
| ATRX mutation | X-linked helicase II |
| BMP4 | Bone morphogenetic protein 4 |
| BRAF mutation | proto-oncogene B-Raf |
| BRCA mutation | breast cancer gene |
| ccRCC | clear cell renal cell carcinoma |
| CE | Contrast-enhanced |
| CGGA | Chinese Glioma Genome Atlas |
| CI | confidence interval |
| C-index | Concordance index |
| COX | Cox proportional hazards model |
| CT | computerized tomography |
| CTLA4 | cytotoxic T lymphocyte antigen 4 |
| DCB | Durable clinical benefit |
| DFS | Disease-free survival |
| DSS | Disease-specific survival |
| EGFR | epidermal growth factor receptor |
| FDG | fluorodeoxyglucose |
| FISH | Fluorescence In Situ Hybridization |
| GBM | glioblastoma multiforme |
| GDC | Genomic Data Commons |
| GSE | Gene Expression Omnibus |
| GSEA | Gene Set Enrichment Analysis |
| HER2 | Human epidermal growth factor receptor 2 |
| HR | hazard ratio |
| HU | Hounsfield units |
| IDH mutation | isocitrate dehydrogenase |
| IHC | Inmunohistochemestry |
| HES | hypoxia enrichment score |
| KMA | Kaplan–Meier analysis |
| KEGG | pathway enrichment analysis |
| MFS | Metastasis-free survival |
| MGMT methylation status | O(6)-methylguanine-DNA methyltransferase promoter methylation status |
| MAPK | Mitogen-activated protein kinase |
| MRI | Magnetic resonance imaging |
| NFkB | NF-kappaB, nuclear factor kappa-light-chain-enhancer of activated B cells |
| LASSO | Least absolute shrinkage and selection operator |
| OR | odds ratio |
| OS | overall survival |
| PCA | principal component analysis |
| pCR | pathologic complete response |
| PD-1 | programmed cell death protein 1 |
| PD-L1 | Programmed death-ligand 1 |
| PET | positron emission tomography |
| PFI | progression-free interval |
| PFS | progression-free survival |
| ROC | receiver operator characteristic curve |
| RF | random forest selection |
| RFS | Recurrence-free survival |
| RR | radiomic and radiographic features |
| SE | standard error |
| TCGA | The Cancer Genome Atlas program |
| TCIA | The Cancer Imaging Atlas |
| TERT | Telomerase reverse transcriptase |
| TMZ | Temozolomide |
| TTF | time-to-treatment failure |
| VHL mutation | Von Hippel-Lindau |
| WGCNA | Weighted gene coexpression network analysis |
Appendix A
| Category | Number | Name | Definition |
|---|---|---|---|
| Highly related to big-data sciences | 1 | High Dimensionality and Small n-to-p Data | Radiomics yields “large-predictors (p) and small number of patients (n)” or “small n-to-p” data, in which the number of measurements is far greater than the number of independent samples g a radiomics approach; however, the number of extracted features can range from hundreds to thousands while the number of patients remains small. The multiplicity of data can result in a high probability of a false-positive rate. |
| 2 | Lack external validation or generalizability | External validation is necessary to determine a prediction model’s reproducibility and generalizability to new and different patients. Various methodological considerations are important when assessing or designing an external validation study. | |
| Population | 3 | Population bias or demographics features variation | Tests may perform differently in various samples. Therefore, demographic features may lead to variations in estimates of test performance. |
| 4 | Spectrum bias | Occurs when a diagnostic test is studied in a different range of individuals to the intended population for the test The ideal diagnostic test would have both high sensitivity (the proportion of people testing positive who actually have the disease) and high specificity (the proportion of people testing negative who do not have the disease). However, the sensitivity and specificity of diagnostic tests vary in different settings. Spectrum bias can have varying effects on sensitivity and specificity. For example, there is consistent evidence that when using a case–control design in diagnostic accuracy studies, both sensitivity and specificity are increased. | |
| 5 | Disease severity bias or variation | Differences in disease severity among studies may lead to differences in estimates of test performance. | |
| 6 | Disease prevalence bias or variation | The prevalence of the target condition varies according to setting and may affect estimates of test performance. Context bias, the tendency of interpreters to consider test results to be positive more frequently in settings with higher disease prevalence, may also affect estimates of test performance. | |
| 7 | Selection bias or distorted selection of participants | Occurs when individuals or groups in a study differ systematically from the population of interest leading to a systematic error in an association or outcome. The selection process determines the composition of the study sample. If the selection process does not aim to include a patient spectrum similar to the population in which the test will be used in practice, the results of the study may have limited applicability. | |
| 8 | Detection bias | A test or treatment for a disease may perform differently according to some characteristic of the study participant, which itself may influence the likelihood of disease detection or the effectiveness of the treatment. Detection bias can occur in trials when groups differ in the way outcome information is collected or the way outcomes are verified. | |
| Test protocol: materials and methods | 9 | Test execution variation | A sufficient description of the execution of index and reference standards is important because variation in measures of diagnostic accuracy can be the result of differences in test execution. |
| 10 | Test technology bias or variation | When the characteristics of a diagnostic test change over time as a result of technological improvement or the experience of the operator of the test, estimates of test performance may be affected. | |
| 11 | Treatment paradox and disease progression bias | Disease progression bias occurs when the index test is performed an unusually long time before the reference standard, so the disease is at a more advanced stage when the reference standard is performed. Treatment paradox occurs when treatment is started on the basis of the knowledge of the results of the index test, and the reference standard is applied after treatment has started. | |
| Reference standard and verification procedure | 12 | Verification bias | This occurs when only a proportion of the study group receives confirmation of the diagnosis by the reference standard, or if some patients receive a different reference standard at the time of diagnosis. Verification bias (sometimes referred to as “work-up bias”) occurs during investigations of diagnostic test accuracy when there is a difference in testing strategy between groups of individuals, leading to differing ways of verifying the disease of interest. Many reference tests are invasive, expensive, or carry a procedural risk (e.g., angiography, biopsy, surgery), and therefore, patients and clinicians may be less likely to pursue further tests if a preliminary test is negative. This may be either partial verification, where only those with a positive test receive the reference standard, or differential verification, where a different reference test is used depending on whether the index test was positive or negative. |
| 13 | Inappropriate reference standard bias | Errors of imperfect reference standard or standards bias the measurement of diagnostic accuracy of the index test | |
| Interpretation, reading process | 14 | Review bias | “Interpretation of the index test or reference standard is influenced by knowledge of the results of the other test. Diagnostic review bias occurs when the results of the index test are known when the reference standard is interpreted. Test review bias occurs when results of the reference standard are known while the index test is interpreted.” |
| 15 | Clinical review bias | “The availability of information on clinical data, such as age, sex, and symptoms, during interpretation of test results may affect estimates of test performance.” | |
| 16 | Incorporation bias | The result of the index test is used to establish the final diagnosis. In a diagnostic accuracy study, ideally, the index test and the reference test should be independent of each other. Incorporation bias is a type of verification bias that occurs when results of the index test form part of the reference test. This occurs most frequently when the reference test is a composite of the results of several tests. | |
| 17 | Observer variability | The reproducibility of test results is one of the determinants of the diagnostic accuracy of an index test. Because of variation in laboratory procedures or observers, a test may not consistently yield the same result when repeated. In 2 or more observations of the same diagnostic study, intraobserver variability occurs when the same person obtains different results, and interobserver variability occurs when 2 or more people disagree. | |
| Analysis | 18 | Handling of indeterminate results | A diagnostic test can produce an uninterpretable result with varying frequency depending on the test. These problems are often not reported in test efficacy studies; the uninterpretable results are simply removed from the analysis. This may lead to a biased assessment of the test characteristics. |
| 19 | Arbitrary choice of a threshold value | The selection of the threshold value for the index test that maximizes the sensitivity and specificity of the test may lead to over-optimistic measures of test performance. The performance of this cutoff in an independent set of patients may not be the same as in the original study. | |
| Other | 20 | Hot stuff bias | When a topic is fashionable (‘hot’), investigators may be less critical in their approach to their research, and investigators and editors may not be able to resist the temptation to publish the results. |
References
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Shui, L.; Ren, H.; Yang, X.; Li, J.; Chen, Z.; Yi, C.; Zhu, H.; Shui, P. The Era of Radiogenomics in Precision Medicine: An Emerging Approach to Support Diagnosis, Treatment Decisions, and Prognostication in Oncology. Front. Oncol. 2020, 10, 570465. [Google Scholar] [CrossRef] [PubMed]
- Yip, S.S.; Aerts, H.J. Applications and limitations of radiomics. Phys. Med. Biol. 2016, 61, R150–R166. [Google Scholar] [CrossRef] [Green Version]
- Gatta, R.; Depeursinge, A.; Ratib, O.; Michielin, O.; Leimgruber, A. Integrating radiomics into holomics for personalised oncology: From algorithms to bedside. Eur. Radiol. Exp. 2020, 4, 11. [Google Scholar] [CrossRef]
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur. J. Cancer 2012, 48, 441–446. [Google Scholar] [CrossRef] [Green Version]
- Tomaszewski, M.R.; Gillies, R.J. The Biological Meaning of Radiomic Features. Radiology 2021, 298, 505–516. [Google Scholar] [CrossRef]
- Incoronato, M.; Aiello, M.; Infante, T.; Cavaliere, C.; Grimaldi, A.M.; Mirabelli, P.; Monti, S.; Salvatore, M. Radiogenomic Analysis of Oncological Data: A Technical Survey. Int. J. Mol. Sci. 2017, 18, 805. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Wu, K.; Wu, B.; Tang, X.; Yuan, H.; Pang, H.; Huang, Y.; Zhu, X.; Luo, H.; Qi, Y. Imaging genomics for accurate diagnosis and treatment of tumors: A cutting edge overview. Biomed. Pharmacother. 2021, 135, 111173. [Google Scholar] [CrossRef]
- Zanfardino, M.; Pane, K.; Mirabelli, P.; Salvatore, M.; Franzese, M. TCGA-TCIA Impact on Radiogenomics Cancer Research: A Systematic Review. Int. J. Mol. Sci. 2019, 20, 6033. [Google Scholar] [CrossRef] [Green Version]
- Napel, S.; Mu, W.; Jardim-Perassi, B.V.; Aerts, H.; Gillies, R.J. Quantitative imaging of cancer in the postgenomic era: Radio(geno)mics, deep learning, and habitats. Cancer 2018, 124, 4633–4649. [Google Scholar] [CrossRef]
- Trivizakis, E.; Papadakis, G.Z.; Souglakos, I.; Papanikolaou, N.; Koumakis, L.; Spandidos, D.A.; Tsatsakis, A.; Karantanas, A.H.; Marias, K. Artificial intelligence radiogenomics for advancing precision and effectiveness in oncologic care (Review). Int. J. Oncol. 2020, 57, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, P.; Gutman, D.A.; Dunn, W.D., Jr.; Holder, C.A.; Aerts, H.J. Imaging-genomics reveals driving pathways of MRI derived volumetric tumor phenotype features in Glioblastoma. BMC Cancer 2016, 16, 611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dextraze, K.; Saha, A.; Kim, D.; Lehrer, M.; Narang, S.; Rao, D.; Ahmed, S.; Madhugiri, V.; Fuller, C.D.; Kim, M.M.; et al. Spatial habitats from multiparametric MR imaging are associated with signaling pathway activities and survival in glioblastoma. Oncotarget 2017, 8, 112992–113001. [Google Scholar] [CrossRef] [Green Version]
- Liao, X.; Cai, B.; Tian, B.; Luo, Y.; Song, W.; Li, Y. Machine-learning based radiogenomics analysis of MRI features and metagenes in glioblastoma multiforme patients with different survival time. J. Cell. Mol. Med. 2019, 23, 4375–4385. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Yang, G.; Hao, X.; Gu, D.; Tan, Y.; Wang, X.; Dong, D.; Zhang, S.; Wang, L.; Zhang, H.; et al. A multi-sequence and habitat-based MRI radiomics signature for preoperative prediction of MGMT promoter methylation in astrocytomas with prognostic implication. Eur. Radiol. 2019, 29, 877–888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qian, Z.; Li, Y.; Sun, Z.; Fan, X.; Xu, K.; Wang, K.; Li, S.; Zhang, Z.; Jiang, T.; Liu, X.; et al. Radiogenomics of lower-grade gliomas: A radiomic signature as a biological surrogate for survival prediction. Aging (Albany NY) 2018, 10, 2884–2899. [Google Scholar] [CrossRef] [PubMed]
- Beig, N.; Patel, J.; Prasanna, P.; Hill, V.; Gupta, A.; Correa, R.; Bera, K.; Singh, S.; Partovi, S.; Varadan, V.; et al. Radiogenomic analysis of hypoxia pathway is predictive of overall survival in Glioblastoma. Sci. Rep. 2018, 8, 7. [Google Scholar] [CrossRef] [Green Version]
- Kong, Z.; Lin, Y.; Jiang, C.; Li, L.; Liu, Z.; Wang, Y.; Dai, C.; Liu, D.; Qin, X.; Wang, Y.; et al. (18)F-FDG-PET-based Radiomics signature predicts MGMT promoter methylation status in primary diffuse glioma. Cancer Imaging 2019, 19, 58. [Google Scholar] [CrossRef] [Green Version]
- Sasaki, T.; Kinoshita, M.; Fujita, K.; Fukai, J.; Hayashi, N.; Uematsu, Y.; Okita, Y.; Nonaka, M.; Moriuchi, S.; Uda, T.; et al. Radiomics and MGMT promoter methylation for prognostication of newly diagnosed glioblastoma. Sci. Rep. 2019, 9, 14435. [Google Scholar] [CrossRef]
- Tan, Y.; Mu, W.; Wang, X.C.; Yang, G.Q.; Gillies, R.J.; Zhang, H. Improving survival prediction of high-grade glioma via machine learning techniques based on MRI radiomic, genetic and clinical risk factors. Eur. J. Radiol. 2019, 120, 108609. [Google Scholar] [CrossRef]
- Choi, S.W.; Cho, H.H.; Koo, H.; Cho, K.R.; Nenning, K.H.; Langs, G.; Furtner, J.; Baumann, B.; Woehrer, A.; Cho, H.J.; et al. Multi-habitat radiomics unravels distinct phenotypic subtypes of glioblastoma with clinical and genomic significance. Cancers 2020, 12, 1707. [Google Scholar] [CrossRef]
- Lin, P.; Peng, Y.T.; Gao, R.Z.; Wei, Y.; Li, X.J.; Huang, S.N.; Fang, Y.Y.; Wei, Z.X.; Huang, Z.G.; Yang, H.; et al. Radiomic profiles in diffuse glioma reveal distinct subtypes with prognostic value. J. Cancer Res. Clin. Oncol. 2020, 146, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.S.; Ahn, S.S.; Chang, J.H.; Kang, S.G.; Kim, E.H.; Kim, S.H.; Jain, R.; Lee, S.K. Machine learning and radiomic phenotyping of lower grade gliomas: Improving survival prediction. Eur. Radiol. 2020, 30, 3834–3842. [Google Scholar] [CrossRef] [PubMed]
- Beig, N.; Bera, K.; Prasanna, P.; Antunes, J.; Correa, R.; Singh, S.; Bamashmos, A.S.; Ismail, M.; Braman, N.; Verma, R.; et al. Radiogenomic-based survival risk stratification of tumor habitat on Gd-T1w MRI is associated with biological processes in glioblastoma. Clin. Cancer Res. 2020, 26, 1866–1876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, Q.; Chen, Y.; Liang, C.; Zhao, Y.; Lv, X.; Zou, Y.; Yan, K.; Zheng, H.; Liang, D.; Li, Z.C. Biologic Pathways Underlying Prognostic Radiomics Phenotypes from Paired MRI and RNA Sequencing in Glioblastoma. Radiology 2021, 301, 654–663. [Google Scholar] [CrossRef]
- Wan, Y.; Zhou, S.; Zhang, Y.; Deng, X.; Xu, L. Radiomic Analysis of Contrast-Enhanced MRI Predicts DNA Copy-Number Subtype and Outcome in Lower-Grade Gliomas. Acad. Radiol. 2021, S1076-6332(21)00488-8. [Google Scholar] [CrossRef]
- Aerts, H.J.; Velazquez, E.R.; Leijenaar, R.T.; Parmar, C.; Grossmann, P.; Carvalho, S.; Bussink, J.; Monshouwer, R.; Haibe-Kains, B.; Rietveld, D.; et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat. Commun. 2014, 5, 4006. [Google Scholar] [CrossRef] [PubMed]
- Aerts, H.J.; Grossmann, P.; Tan, Y.; Oxnard, G.R.; Rizvi, N.; Schwartz, L.H.; Zhao, B. Defining a Radiomic Response Phenotype: A Pilot Study using targeted therapy in NSCLC. Sci. Rep. 2016, 6, 33860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bak, S.H.; Park, H.; Lee, H.Y.; Kim, Y.; Kim, H.L.; Jung, S.H.; Kim, H.; Kim, J.; Park, K. Imaging genotyping of functional signaling pathways in lung squamous cell carcinoma using a radiomics approach. Sci. Rep. 2018, 8, 3284. [Google Scholar] [CrossRef]
- Xie, D.; Wang, T.T.; Huang, S.J.; Deng, J.J.; Ren, Y.J.; Yang, Y.; Wu, J.Q.; Zhang, L.; Fei, K.; Sun, X.W.; et al. Radiomics nomogram for prediction disease-free survival and adjuvant chemotherapy benefits in patients with resected stage I lung adenocarcinoma. Transl. Lung Cancer Res. 2020, 9, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Lafata, K.J.; Corradetti, M.N.; Gao, J.; Jacobs, C.D.; Weng, J.; Chang, Y.; Wang, C.; Hatch, A.; Xanthopoulos, E.; Jones, G.; et al. Radiogenomic Analysis of Locally Advanced Lung Cancer Based on CT Imaging and Intratreatment Changes in Cell-Free DNA. Radiol. Imaging Cancer 2021, 3, e200157. [Google Scholar] [CrossRef] [PubMed]
- Mu, W.; Jiang, L.; Zhang, J.; Shi, Y.; Gray, J.E.; Tunali, I.; Gao, C.; Sun, Y.; Tian, J.; Zhao, X.; et al. Non-invasive decision support for NSCLC treatment using PET/CT radiomics. Nat. Commun. 2020, 11, 5228. [Google Scholar] [CrossRef]
- Perez-Morales, J.; Tunali, I.; Stringfield, O.; Eschrich, S.A.; Balagurunathan, Y.; Gillies, R.J.; Schabath, M.B. Peritumoral and intratumoral radiomic features predict survival outcomes among patients diagnosed in lung cancer screening. Sci. Rep. 2020, 10, 10528. [Google Scholar] [CrossRef]
- Kirienko, M.; Sollini, M.; Corbetta, M.; Voulaz, E.; Gozzi, N.; Interlenghi, M.; Gallivanone, F.; Castiglioni, I.; Asselta, R.; Duga, S.; et al. Radiomics and gene expression profile to characterise the disease and predict outcome in patients with lung cancer. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3643–3655. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhu, Y.; Burnside, E.S.; Drukker, K.; Hoadley, K.A.; Fan, C.; Conzen, S.D.; Whitman, G.J.; Sutton, E.J.; Net, J.M.; et al. MR Imaging Radiomics Signatures for Predicting the Risk of Breast Cancer Recurrence as Given by Research Versions of MammaPrint, Oncotype DX, and PAM50 Gene Assays. Radiology 2016, 281, 382–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.; Li, B.; Sun, X.; Cao, G.; Rubin, D.L.; Napel, S.; Ikeda, D.M.; Kurian, A.W.; Li, R. Heterogeneous Enhancement Patterns of Tumor-adjacent Parenchyma at MR Imaging Are Associated with Dysregulated Signaling Pathways and Poor Survival in Breast Cancer. Radiology 2017, 285, 401–413. [Google Scholar] [CrossRef] [Green Version]
- Bitencourt, A.G.V.; Gibbs, P.; Rossi Saccarelli, C.; Daimiel, I.; Lo Gullo, R.; Fox, M.J.; Thakur, S.; Pinker, K.; Morris, E.A.; Morrow, M.; et al. MRI-based machine learning radiomics can predict HER2 expression level and pathologic response after neoadjuvant therapy in HER2 overexpressing breast cancer. EBioMedicine 2020, 61, 103042. [Google Scholar] [CrossRef] [PubMed]
- Vargas, H.A.; Veeraraghavan, H.; Micco, M.; Nougaret, S.; Lakhman, Y.; Meier, A.A.; Sosa, R.; Soslow, R.A.; Levine, D.A.; Weigelt, B.; et al. A novel representation of inter-site tumour heterogeneity from pre-treatment computed tomography textures classifies ovarian cancers by clinical outcome. Eur. Radiol. 2017, 27, 3991–4001. [Google Scholar] [CrossRef]
- Meier, A.; Veeraraghavan, H.; Nougaret, S.; Lakhman, Y.; Sosa, R.; Soslow, R.A.; Sutton, E.J.; Hricak, H.; Sala, E.; Vargas, H.A. Association between CT-texture-derived tumor heterogeneity, outcomes, and BRCA mutation status in patients with high-grade serous ovarian cancer. Abdom. Radiol. 2019, 44, 2040–2047. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Arshad, M.; Thornton, A.; Avesani, G.; Cunnea, P.; Curry, E.; Kanavati, F.; Liang, J.; Nixon, K.; Williams, S.T.; et al. A mathematical-descriptor of tumor-mesoscopic-structure from computed-tomography images annotates prognostic- and molecular-phenotypes of epithelial ovarian cancer. Nat. Commun. 2019, 10, 764. [Google Scholar] [CrossRef] [PubMed]
- Hoivik, E.A.; Hodnel, E.; Dybvik, J.A.; Wagner-Larsen, K.S.; Fasmer, K.E.; Berg, H.F.; Halle, M.K.; Haldorsen, I.S.; Krakstad, C. A radiogenomics application for prognostic profiling of endometrial cancer. Commun. Biol. 2021, 4, 1363. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Cho, H.H.; Joung, J.G.; Jeon, H.G.; Jeong, B.C.; Jeon, S.S.; Lee, H.M.; Nam, D.H.; Park, W.Y.; Kim, C.K.; et al. Integrative radiogenomics approach for risk assessment of post-operative metastasis in pathological T1 renal cell carcinoma: A pilot retrospective cohort study. Cancers 2020, 12, 866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, J.; Ye, F.; Han, F.; Wang, X.; Jiang, H.; Zhang, J. A Novel Radiogenomics Biomarker Based on Hypoxic-Gene Subset: Accurate Survival and Prognostic Prediction of Renal Clear Cell Carcinoma. Front. Oncol. 2021, 11, 739815. [Google Scholar] [CrossRef] [PubMed]
- Ruizhi, G.; Hui, Q.; Peng, L.; Chenjun, M.; Chengyang, L.; Rong, W.; Jing, H.; Da, W.; Dongyue, W.; Yiqiong, L.; et al. Development and Validation of a Radiomic Nomogram for Predicting the Prognosis of Kidney Renal Clear Cell Carcinoma. Front. Oncol. 2021, 11, 613668. [Google Scholar]
- Lin, P.; Lin, Y.Q.; Gao, R.Z.; Wen, R.; Qin, H.; He, Y.; Yang, H. Radiomic profiling of clear cell renal cell carcinoma reveals subtypes with distinct prognoses and molecular pathways. Transl. Oncol. 2021, 14, 101078. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Wu, P.; Yang, K.; Li, Z.; Kong, S.; Yu, L.; Zhang, E.; Liu, H.; Guo, Q.; Wu, S. A comprehensive texture feature analysis framework of renal cell carcinoma: Pathological, prognostic, and genomic evaluation based on CT images. Eur. Radiol. 2021, 32, 2255–2265. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Chen, L.; Wang, M.; Luo, Y.; Huang, Y.; Ma, X. Integrative radiogenomics analysis for predicting molecular features and survival in clear cell renal cell carcinoma. Aging (Albany NY) 2021, 13, 9960–9975. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.; Wen, D.Y.; Chen, L.; Li, X.; Li, S.H.; Yan, H.B.; He, R.Q.; Chen, G.; He, Y.; Yang, H. A radiogenomics signature for predicting the clinical outcome of bladder urothelial carcinoma. Eur. Radiol. 2019, 30, 547–557. [Google Scholar] [CrossRef]
- Hectors, S.J.; Cherny, M.; Yadav, K.K.; Beksaç, A.T.; Thulasidass, H.; Lewis, S.; Davicioni, E.; Wang, P.; Tewari, A.K.; Taouli, B. Radiomics Features Measured with Multiparametric Magnetic Resonance Imaging Predict Prostate Cancer Aggressiveness. J. Urol. 2019, 202, 498–505. [Google Scholar] [CrossRef]
- Hu, Y.; Xie, C.; Yang, H.; Ho, J.W.K.; Wen, J.; Han, L.; Chiu, K.W.H.; Fu, J.; Vardhanabhuti, V. Assessment of Intratumoral and Peritumoral Computed Tomography Radiomics for Predicting Pathological Complete Response to Neoadjuvant Chemoradiation in Patients with Esophageal Squamous Cell Carcinoma. JAMA Netw. Open 2020, 3, e2015927. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.Y.; Hu, Y.H.; Ho, J.W.K.; Han, L.J.; Yang, H.; Wen, J.; Lam, K.O.; Wong, I.Y.H.; Law, S.Y.K.; Chiu, K.W.H.; et al. Using genomics feature selection method in radiomics pipeline improves prognostication performance in locally advanced esophageal squamous cell carcinoma-a pilot study. Cancers 2021, 13, 2145. [Google Scholar] [CrossRef]
- Jin, Y.; Xu, Y.; Li, Y.; Chen, R.; Cai, W. Integrative Radiogenomics Approach for Risk Assessment of Postoperative and Adjuvant Chemotherapy Benefits for Gastric Cancer Patients. Front. Oncol. 2021, 11, 755271. [Google Scholar] [CrossRef]
- Negreros-Osuna, A.A.; Parakh, A.; Corcoran, R.B.; Pourvaziri, A.; Kambadakone, A.; Ryan, D.P.; Sahani, D.V. Radiomics Texture Features in Advanced Colorectal Cancer: Correlation with BRAF Mutation and 5-year Overall Survival. Radiol. Imaging Cancer 2020, 2, e190084. [Google Scholar] [CrossRef]
- Hectors, S.J.; Lewis, S.; Besa, C.; King, M.J.; Said, D.; Putra, J.; Ward, S.; Higashi, T.; Thung, S.; Yao, S.; et al. MRI radiomics features predict immuno-oncological characteristics of hepatocellular carcinoma. Eur. Radiol. 2020, 30, 3759–3769. [Google Scholar] [CrossRef]
- Aoude, L.G.; Wong, B.Z.Y.; Bonazzi, V.F.; Brosda, S.; Walters, S.B.; Koufariotis, L.T.; Naeini, M.M.; Pearson, J.V.; Oey, H.; Patel, K.; et al. Radiomics Biomarkers Correlate with CD8 Expression and Predict Immune Signatures in Melanoma Patients. Mol. Cancer Res. 2021, 19, 950–956. [Google Scholar] [CrossRef]
- Sun, R.; Limkin, E.J.; Vakalopoulou, M.; Dercle, L.; Champiat, S.; Han, S.R.; Verlingue, L.; Brandao, D.; Lancia, A.; Ammari, S.; et al. A radiomics approach to assess tumour-infiltrating CD8 cells and response to anti-PD-1 or anti-PD-L1 immunotherapy: An imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018, 19, 1180–1191. [Google Scholar] [CrossRef]
- Li, Y.; Eresen, A.; Shangguan, J.; Yang, J.; Benson, A.B., 3rd; Yaghmai, V.; Zhang, Z. Preoperative prediction of perineural invasion and KRAS mutation in colon cancer using machine learning. J. Cancer Res. Clin. Oncol. 2020, 146, 3165–3174. [Google Scholar] [CrossRef]
- Lionello, I.; Mangia, P.; Gattinoni, L.; Pende, D.; Cippone, A.; Sensi, M.; Rigatti, P.; Traversari, C. CD8(+) T lymphocytes isolated from renal cancer patients recognize tumour cells through an HLA- and TCR/CD3-independent pathway. Cancer Immunol. Immunother. 2007, 56, 1065–1076. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [Green Version]
- Sonpavde, G.; Bellmunt, J. Bladder cancer: Angiogenesis as a therapeutic target in urothelial carcinoma. Nat. Rev. Urol. 2016, 13, 306–307. [Google Scholar] [CrossRef]
- Ye, F.; Hu, Y.; Gao, J.; Liang, Y.; Liu, Y.; Ou, Y.; Cheng, Z.; Jiang, H. Radiogenomics Map Reveals the Landscape of m6A Methylation Modification Pattern in Bladder Cancer. Front. Immunol. 2021, 12, 722642. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.G.; Chang, S.L.; Spratt, D.E.; Erho, N.; Yu, M.; Ashab, H.A.; Alshalalfa, M.; Speers, C.; Tomlins, S.A.; Davicioni, E.; et al. Development and validation of a 24-gene predictor of response to postoperative radiotherapy in prostate cancer: A matched, retrospective analysis. Lancet Oncol. 2016, 17, 1612–1620. [Google Scholar] [CrossRef]
- Stoyanova, R.; Pollack, A.; Takhar, M.; Lynne, C.; Parra, N.; Lam, L.L.; Alshalalfa, M.; Buerki, C.; Castillo, R.; Jorda, M.; et al. Association of multiparametric MRI quantitative imaging features with prostate cancer gene expression in MRI-targeted prostate biopsies. Oncotarget 2016, 7, 53362–53376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goh, V.; Ganeshan, B.; Nathan, P.; Juttla, J.K.; Vinayan, A.; Miles, K.A. Assessment of response to tyrosine kinase inhibitors in metastatic renal cell cancer: CT texture as a predictive biomarker. Radiology 2011, 261, 165–171. [Google Scholar] [CrossRef]
- Rao, S.X.; Lambregts, D.M.; Schnerr, R.S.; Beckers, R.C.; Maas, M.; Albarello, F.; Riedl, R.G.; Dejong, C.H.; Martens, M.H.; Heijnen, L.A.; et al. CT texture analysis in colorectal liver metastases: A better way than size and volume measurements to assess response to chemotherapy? United Eur. Gastroenterol. J. 2016, 4, 257–263. [Google Scholar] [CrossRef]
- Zhao, B. Understanding Sources of Variation to Improve the Reproducibility of Radiomics. Front. Oncol. 2021, 11, 633176. [Google Scholar] [CrossRef]
- Park, J.E.; Park, S.Y.; Kim, H.J.; Kim, H.S. Reproducibility and Generalizability in Radiomics Modeling: Possible Strategies in Radiologic and Statistical Perspectives. Kr. J. Radiol. 2019, 20, 1124–1137. [Google Scholar] [CrossRef]
- Oikonomou, E.K.; Williams, M.C.; Kotanidis, C.P.; Desai, M.Y.; Marwan, M.; Antonopoulos, A.S.; Thomas, K.E.; Thomas, S.; Akoumianakis, I.; Fan, L.M.; et al. A novel machine learning-derived radiotranscriptomic signature of perivascular fat improves cardiac risk prediction using coronary CT angiography. Eur. Heart J. 2019, 40, 3529–3543. [Google Scholar] [CrossRef]
- Infante, T.; Cavaliere, C.; Punzo, B.; Grimaldi, V.; Salvatore, M.; Napoli, C. Radiogenomics and Artificial Intelligence Approaches Applied to Cardiac Computed Tomography Angiography and Cardiac Magnetic Resonance for Precision Medicine in Coronary Heart Disease: A Systematic Review. Circ. Cardiovasc. Imaging 2021, 14, 1133–1146. [Google Scholar] [CrossRef]
- Mirón Mombiela, R.; Borrás, C. The Usefulness of Radiomics Methodology for Developing Descriptive and Prognostic Image-Based Phenotyping in the Aging Population: Results From a Small Feasibility Study. Front. Aging 2022, 3, 853671. [Google Scholar] [CrossRef]
- Tsimberidou, A.M.; Hong, D.S.; Ye, Y.; Cartwright, C.; Wheler, J.J.; Falchook, G.S.; Naing, A.; Fu, S.; Piha-Paul, S.; Janku, F.; et al. Initiative for Molecular Profiling and Advanced Cancer Therapy (IMPACT): An MD Anderson Precision Medicine Study. JCO Precis. Oncol. 2017, 2017, 1–18. [Google Scholar]
- Tsimberidou, A.M.; Eggermont, A.M.; Schilsky, R.L. Precision cancer medicine: The future is now, only better. Am. Soc. Clin. Oncol. Educ. Book 2014, 34, 61–69. [Google Scholar] [CrossRef] [PubMed]



| Utility/ Outcome Measured | Imaging Modality | RQS | Genetic Data | Genetics Database Used/ Name | Patients: Genetic Validation/ Total | Limitations ** | Year/ [Ref.] |
|---|---|---|---|---|---|---|---|
| Brain tumors: Gliomas/Astrocytomas | |||||||
| Prognosis/OS | MRI | 8 | GBM gene expression (mRNA)/Transcriptomics | Yes/TCGA and TCIA | 91/141 | 12 | 2016 [12] |
| Prognosis/OS | MRI | 6 | Pathway activation/Transcriptomics and Proteomics | Yes/TCGA, TCIA, and cBioPortal | 85/85 | 1, 2 | 2017 [13] |
| Prognosis/OS | MRI | 13 | Gene expression/Transcriptomics | Yes/TCIA and GDC | 46/137 | 1, 12 | 2018 [14] |
| Prognosis/OS | MRI | 13 | MGMT methylation/Epigenomics | No | 105/105 | 2, 6 | 2018 [15] |
| Prognosis/OS | MRI | 11 | Gene expression/Transcriptomics | Yes/TCGA and CGGA | 85/85 | 1 | 2018 [16] |
| Prognosis/OS | MRI | 18 | RNA sequencing/Transcriptomics | Yes/TCIA | 115/115 | 2 | 2018 [17] |
| Prognosis/OS | FDG PET-CT | 16 | MGMT methylation/Epigenetics | No | 107/107 | 2, 7 | 2019 [18] |
| Prognosis/OS | MRI | 13 | MGMT methylation/Epigenetics | No | 201/201 | 2 | 2019 [19] |
| Prognosis/ OS | MRI | 13 | IDH1 (2 mutations)/Genetics | No | 105/105 | 2 | 2019 [20] |
| Prognosis/ OS | MRI | 15 | RNA sequencing/Transcriptomics | No | 144/144 | 1, 2 | 2020 [21] |
| Prognosis/ OS | MRI | 11 | MGMT methylation, RNA sequencing/Epigenetics and Transcriptomics | Yes/TCGA and TCIA | 85/166 | 1, 2, 10, 12 | 2020 [22] |
| Prognosis/ OS | MRI | 19 | IDH mutation status/Genetics | Yes/TCGA and TCIA | 296/296 | 10, 15 | 2020 [23] |
| Prognosis/ PFS | MRI | 17 | IDH mutation, RNA sequencing/Genetics and Transcriptomics | Yes/TCIA | 125/203 | 1, 12 | 2020 [24] |
| Prognosis/ OS | MRI | 18 | RNA sequencing/Transcriptomics | Yes/TCGA and TCIA | 173/435 | 12 | 2021 [25] |
| Prognosis/ PFS and OS | MRI | 5 | DNA copy-number subtypes (CN1, CN2 or CN3)/Genetics | Yes/TCGA | 153/153 | 1, 2, 6, 10 | 2021 [26] |
| Lung and Head and Neck Cancers | |||||||
| Prognosis/OS | CT | 16 | Gene expression/Transcriptomics | No | 89/1019 | 1, 3, 12 | 2014 [27] |
| Treatment Response | CT | 13 | EGFR sensitizing mutations/Genetics | No | 49/49 | 1 | 2016 [28] |
| Prognosis/ DFS and OS | CT | 8 | Whole exome sequencing/Genetics and Transcriptomics | No | 57/57 | 2, 3, 5, 10 | 2018 [29] |
| Prognosis/DFS | CT | 13 | RNA sequencing/Transcriptomics | Yes/TCIA | 79/554 | 2, 12 | 2020 [30] |
| Prognosis/OS | CT | 14 | ctDNA TP53 mutations/Genetics | No | 24/24 | 1, 2 | 2020 [31] |
| Prognosis + Treatment Response/ PFS, TTF, and DCB | FDG PET-CT | 17 | EGFR mutation/Genetics | No | 681/837 | 5, 12 | 2020 [32] |
| Prognosis/ PFS and OS | CT | 11 | Gene expression/Transcriptomics | No | 103/399 | 12 | 2020 [33] |
| Prognosis/Relapse + Histotype | FDG PET-CT | 5 | RNA sequencing/Transcriptomics | No | 74/151 | 2, 12 | 2021 [34] |
| Breast Cancer | |||||||
| Risk Assessment/ Risk of recurrence | MRI | 16 | RNA sequencing/Transcriptomics | Yes/TCGA | 84/84 | 2, 10 | 2016 [35] |
| Prognosis/ PFS and OS | CE MRI | 15 | RNA-sequencing of tumor and adjacent tumor parenchyma/Transcriptomics | Yes/TCGA and GSE 1456 | 423/1362 | 8, 12 | 2017 [36] |
| Response to Treatment/ pCR | MRI | 10 | FISH and IHC/Genetics | No | 311/311 | 2 | 2020 [37] |
| Ovarian Cancer | |||||||
| Prognosis/OS | CT | 9 | CCNE1 cyclin E1 gene + CLOVAR transcriptomic profiles/Genetics and Transcriptomics | No | 38/38 | 2 | 2017 [38] |
| Prognosis/ PFS and OS | CT | 5 | BRCA mutation/Genetics | No | 88/88 | 2 | 2018 [39] |
| Prognosis/ PFS and OS | CT | 20 | DNA sequencing of tumors/Genetics | Yes/TCGA | 364/364 | 5 | 2019 [40] |
| Endometrial Cancer | |||||||
| Prognosis/RFS and DSS | MRI | 12 | RNA sequencing/Transcriptomics | Yes/TCGA | 51/487 | 2, 7, 10, 12 | 2021 [41] |
| Renal Cell Carcinoma | |||||||
| Prognosis/MFS and OS | CT | 12 | Gene expression/Genetics and Transcriptomics | Yes/TCGA + TCIA | 509/520 | 10, 12 | 2020 [42] |
| Prognosis/OS | CT | 11 | Hypoxia-related genes/Genetics | Yes/TCGA + TCIA | 419/419 | 3, 5, 17, | 2021 [43] |
| Prognosis/PFI | CT | 15 | Gene mutations and gene expression/Genetics and Transcriptomics | Yes/TCGA + TCIA | 78/214 | 1, 5, 10, 12 | 2021 [44] |
| Prognosis/ PFI and OS | CT | 6 | Differentially expressed genes and enriched pathways/Transcriptomics | Yes/TCGA + Array-Express database | 261/261 | 5 | 2021 [45] |
| Prognosis/ OS | CT | 14 | mRNA subtype, miRNA subtype, VHL mutation/Genetics and Transcriptomics | Yes/TCIA | 267/443 | 2, 12 | 2021 [46] |
| Prognosis/ OS | CT | 14 | Mutated genes (VHL, BAP1, PBRM1, SETD2), four mRNA patterns/Genetics and Transcriptomics | Yes/TCGA + TCIA | 279/382 | 12,19 | 2021 [47] |
| Bladder Cancer | |||||||
| Prognosis/ PFI | 21 | 8 | RNA sequencing/Transcriptomics | Yes/TCGA + TCIA | 62/62 | 1, 2 | 2019 [48] |
| Prostate Cancer | |||||||
| Risk Assessment/Risk of metastasis | MRI | 10 | RNA expression/Transcriptomics | No | 64/64 | 1, 2, 5 | 2019 [49] |
| Esophagus Cancer | |||||||
| Treatment Response/pCR | CT | 17 | RNA sequencing/Transcriptomics | No | 40/231 | 1, 12 | 2020 [50] |
| Prognosis + Treatment Response/DFS, OS and pCR | CT | 17 | Gene expression/Transcriptomics | No | 28/106 | 1, 7, 12 | 2021 [51] |
| Gastric Cancer | |||||||
| Prognosis + Treatment Response/ PFS and OS | CT | 11 | RNA sequencing/Transcriptomics | Yes/ TCIA | 47/475 | 12 | 2021 [52] |
| Colorectal Cancer | |||||||
| Prognosis/ OS | CT | 8 | BRAF mutation/Genetics | No | 145/145 | 10 | 2020 [53] |
| Hepatocellular Carcinoma | |||||||
| Risk Assessment/Early recurrence | MRI | 7 | Gene expression/Transcriptomics | No | 48/48 | 1, 2, 10 | 2020 [54] |
| Melanoma | |||||||
| Prognosis/ OS | FDG PET-CT | 7 | RNA sequencing. Whole-exon sequencing for common oncogenes. BRAF mutation/Genomics and Transcriptomics | No | 33/52 | 2, 3, 7, 12 | 2021 [55] |
| Solid tumors * | |||||||
| Prognosis + Treatment Response/ PFI and OS | CT | 9 | Gene expression (CD8 cells)/Transcriptomics | Yes/TCGA | 254/491 | 3, 4, 8, 12 | 2018 [56] |
| Database | Syntax |
|---|---|
| PubMed | (“radiomic *” [All Fields] AND (“genetic *” [All Fields] OR “genomic *” [All Fields])) OR “imaging genomic” [All Fields] filters: human and English language 1 |
| EMBASE | (radiomics.mp AND exp genetics/) OR imaging genomics.mp filters: human and English language 2,3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirón Mombiela, R.; Arildskov, A.R.; Bruun, F.J.; Hasselbalch, L.H.; Holst, K.B.; Rasmussen, S.H.; Borrás, C. What Genetics Can Do for Oncological Imaging: A Systematic Review of the Genetic Validation Data Used in Radiomics Studies. Int. J. Mol. Sci. 2022, 23, 6504. https://doi.org/10.3390/ijms23126504
Mirón Mombiela R, Arildskov AR, Bruun FJ, Hasselbalch LH, Holst KB, Rasmussen SH, Borrás C. What Genetics Can Do for Oncological Imaging: A Systematic Review of the Genetic Validation Data Used in Radiomics Studies. International Journal of Molecular Sciences. 2022; 23(12):6504. https://doi.org/10.3390/ijms23126504
Chicago/Turabian StyleMirón Mombiela, Rebeca, Anne Rix Arildskov, Frederik Jager Bruun, Lotte Harries Hasselbalch, Kristine Bærentz Holst, Sine Hvid Rasmussen, and Consuelo Borrás. 2022. "What Genetics Can Do for Oncological Imaging: A Systematic Review of the Genetic Validation Data Used in Radiomics Studies" International Journal of Molecular Sciences 23, no. 12: 6504. https://doi.org/10.3390/ijms23126504
APA StyleMirón Mombiela, R., Arildskov, A. R., Bruun, F. J., Hasselbalch, L. H., Holst, K. B., Rasmussen, S. H., & Borrás, C. (2022). What Genetics Can Do for Oncological Imaging: A Systematic Review of the Genetic Validation Data Used in Radiomics Studies. International Journal of Molecular Sciences, 23(12), 6504. https://doi.org/10.3390/ijms23126504







