Dimethyl Trisulfide Diminishes Traumatic Neuropathic Pain Acting on TRPA1 Receptors in Mice
Abstract
1. Introduction
2. Results
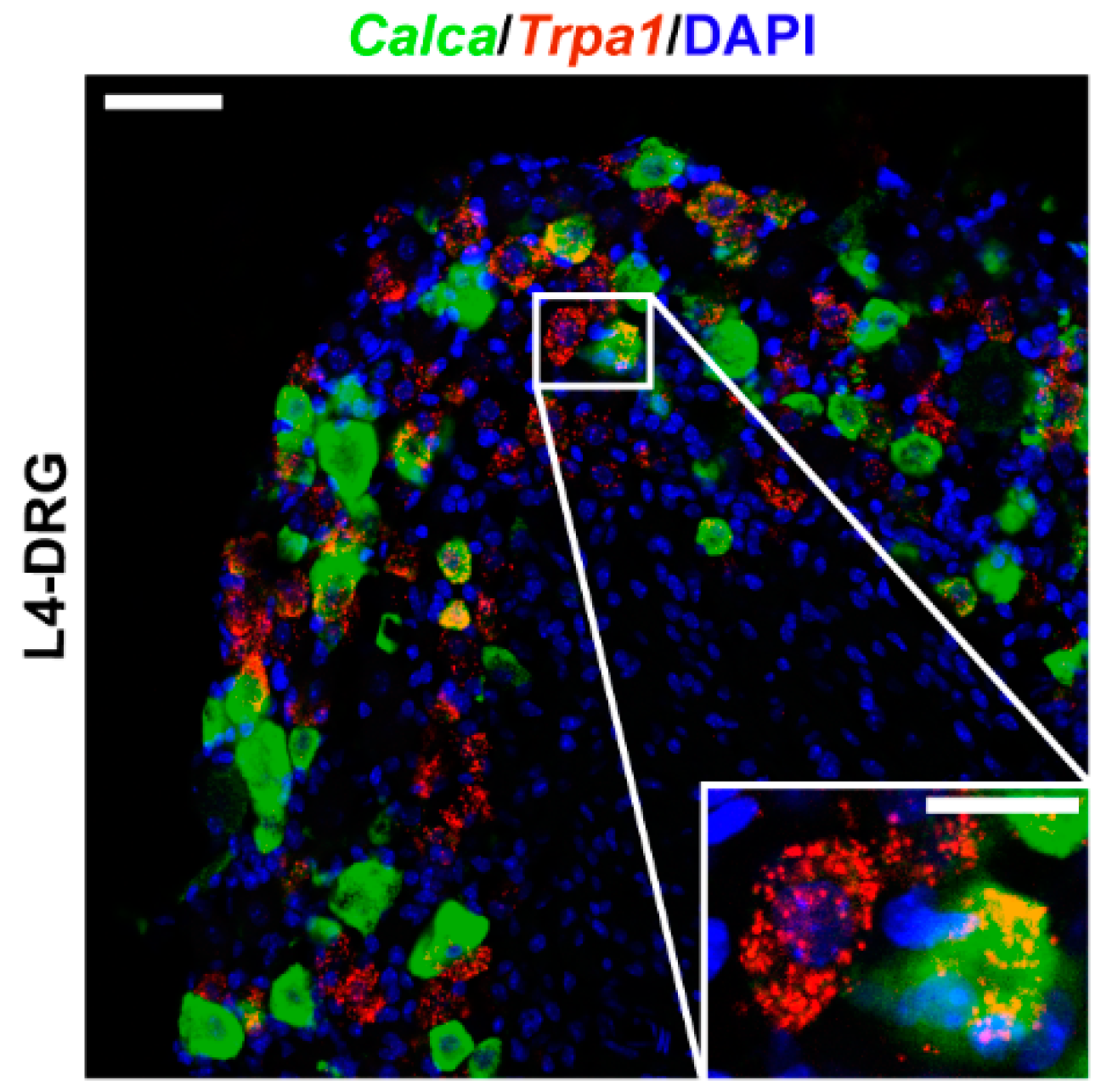
2.1. Trpa1 mRNA Is Expressed in Dorsal Root Ganglion Neurons
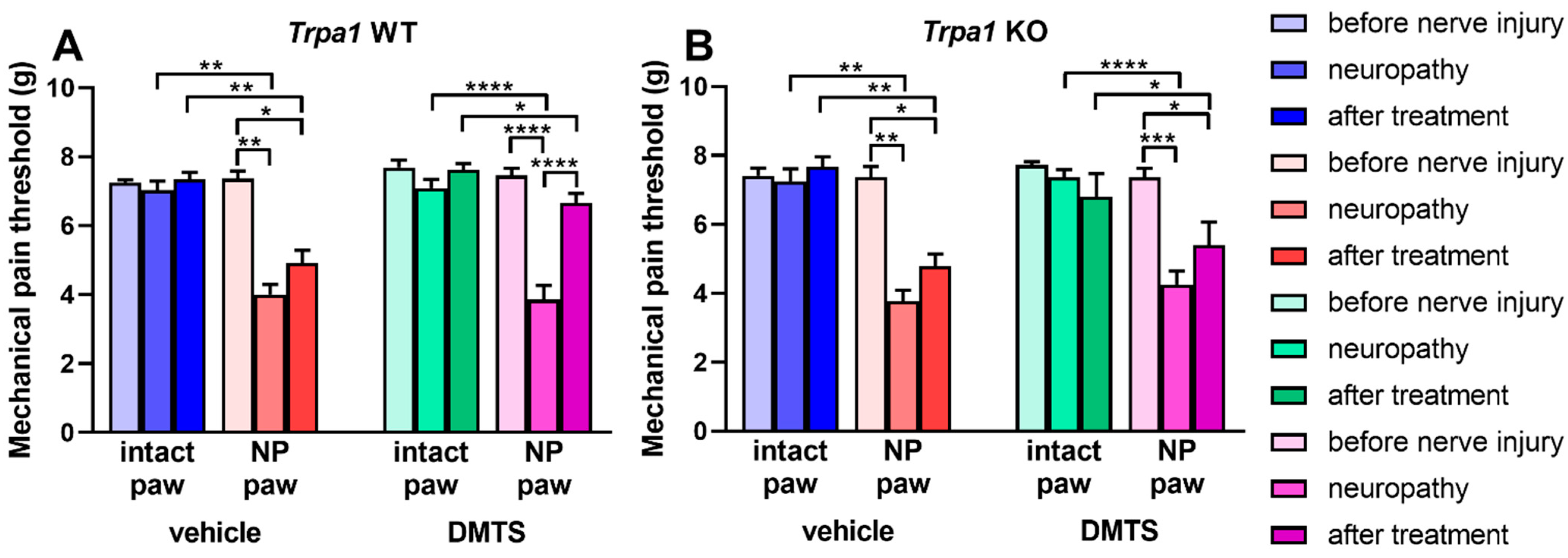
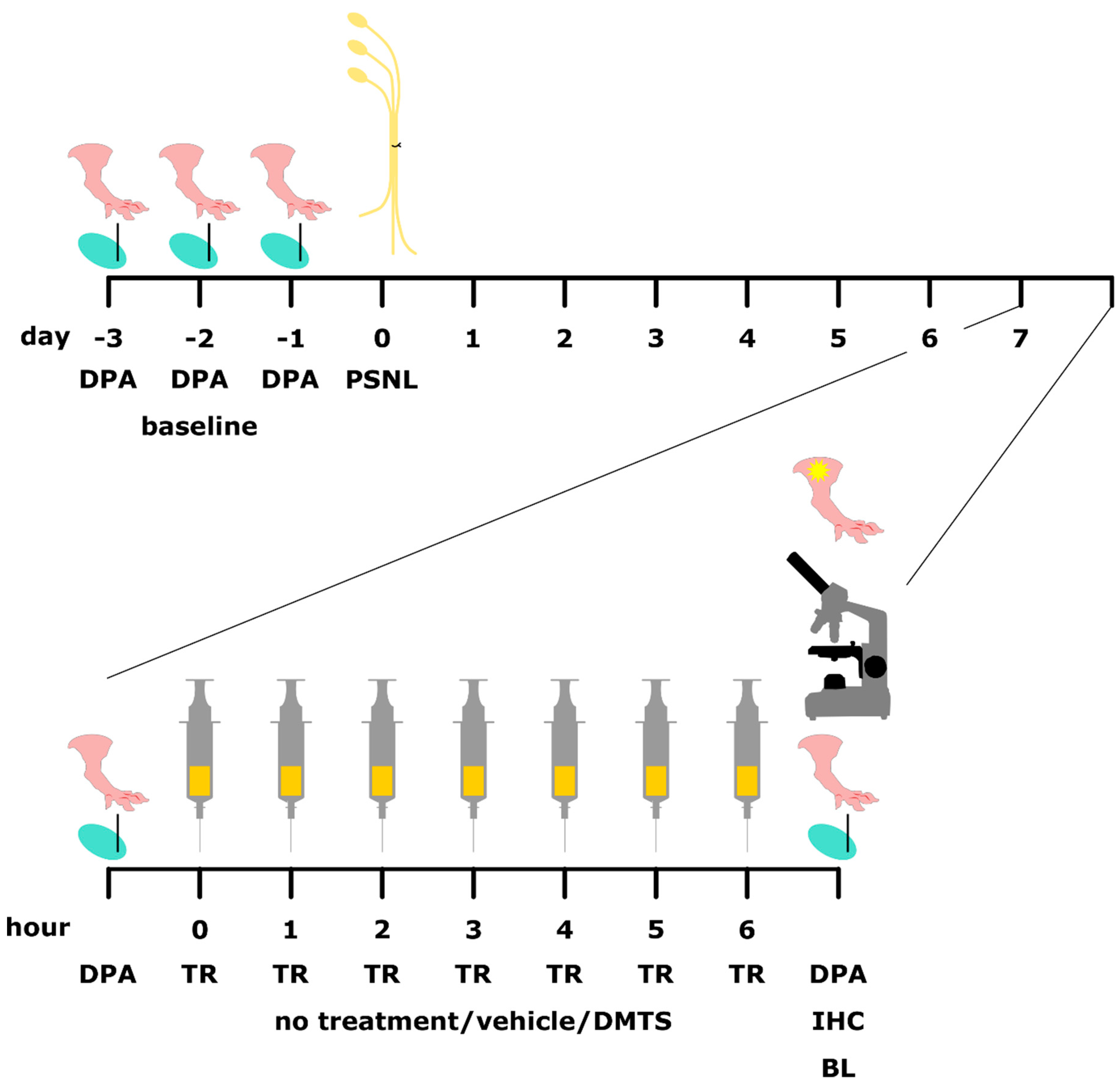
2.2. Dimethyl Trisulfide Alleviates Neuropathic Pain
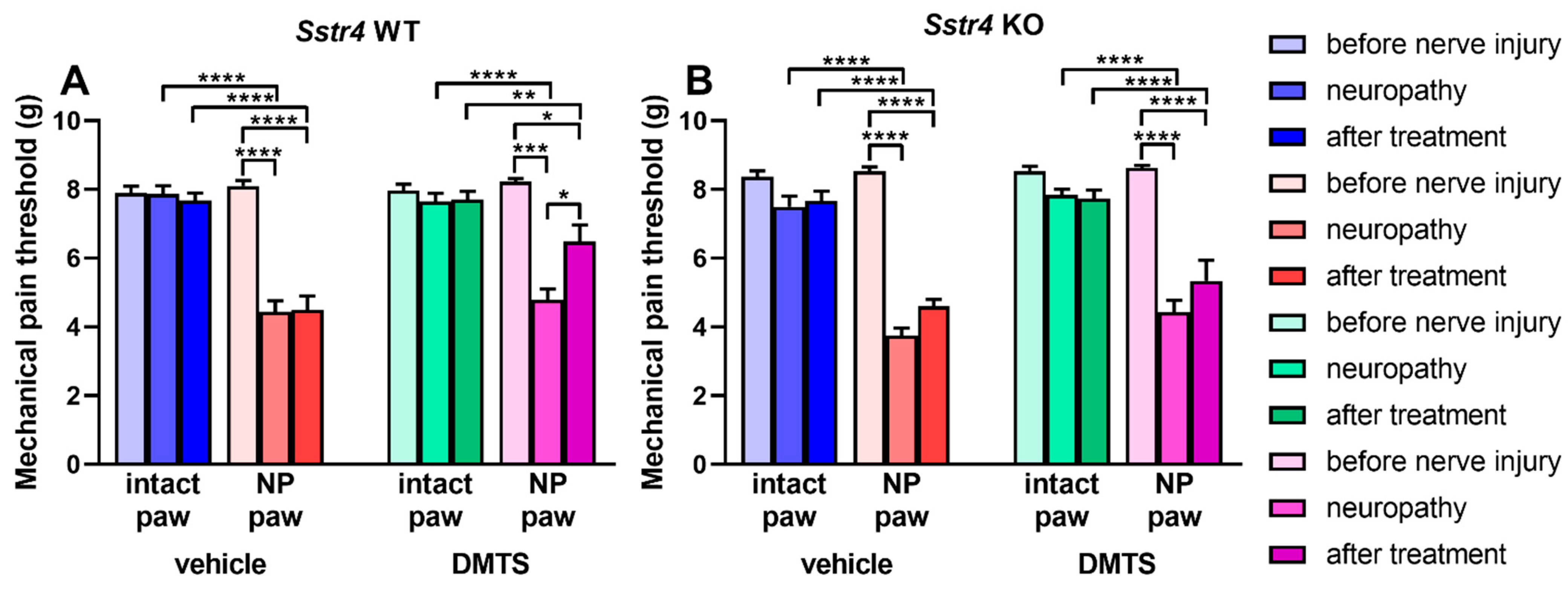
2.3. Beside TRPA1 Ion Channel, SST4 Somatostatin Receptor Mediates Antihyperalgesic Effect of DMTS
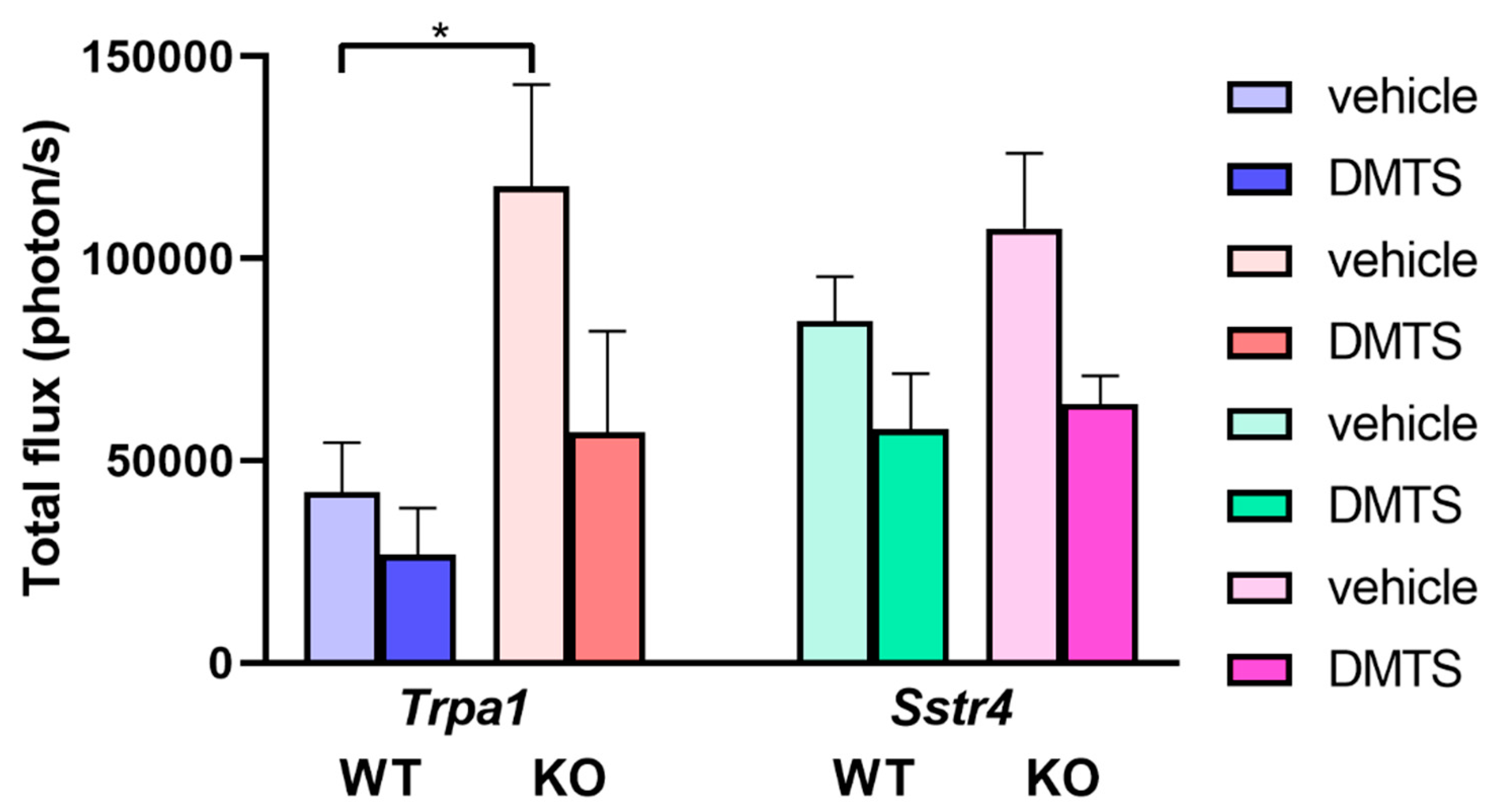
2.4. Dimethyl Trisulfide Does Not Alter Macrophage Activity Around the Damaged Sciatic Nerve
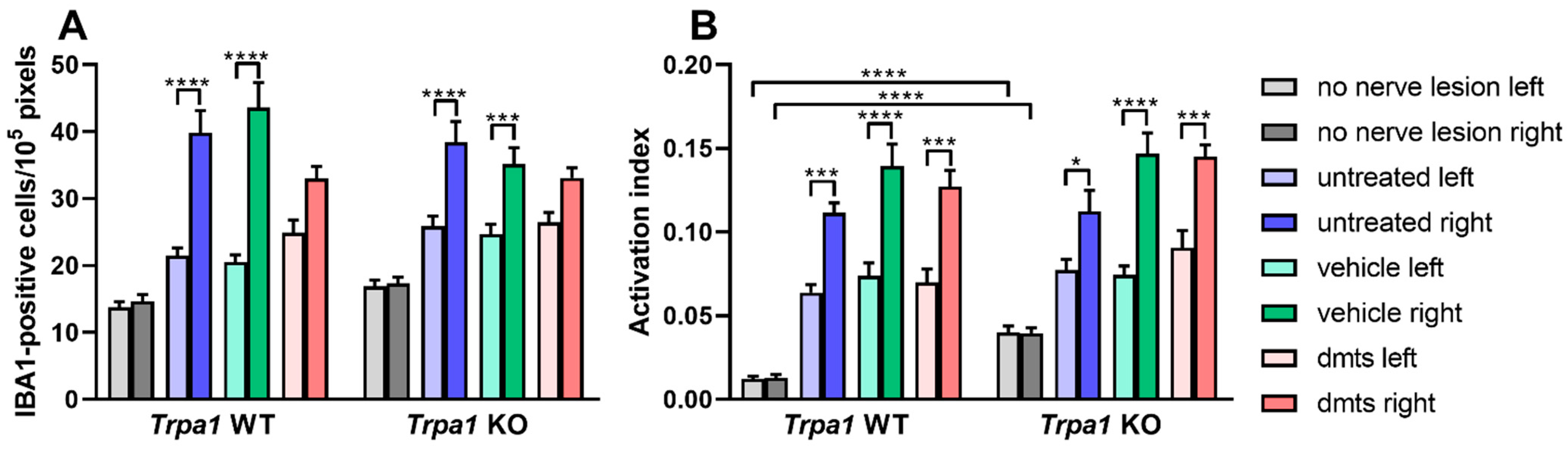
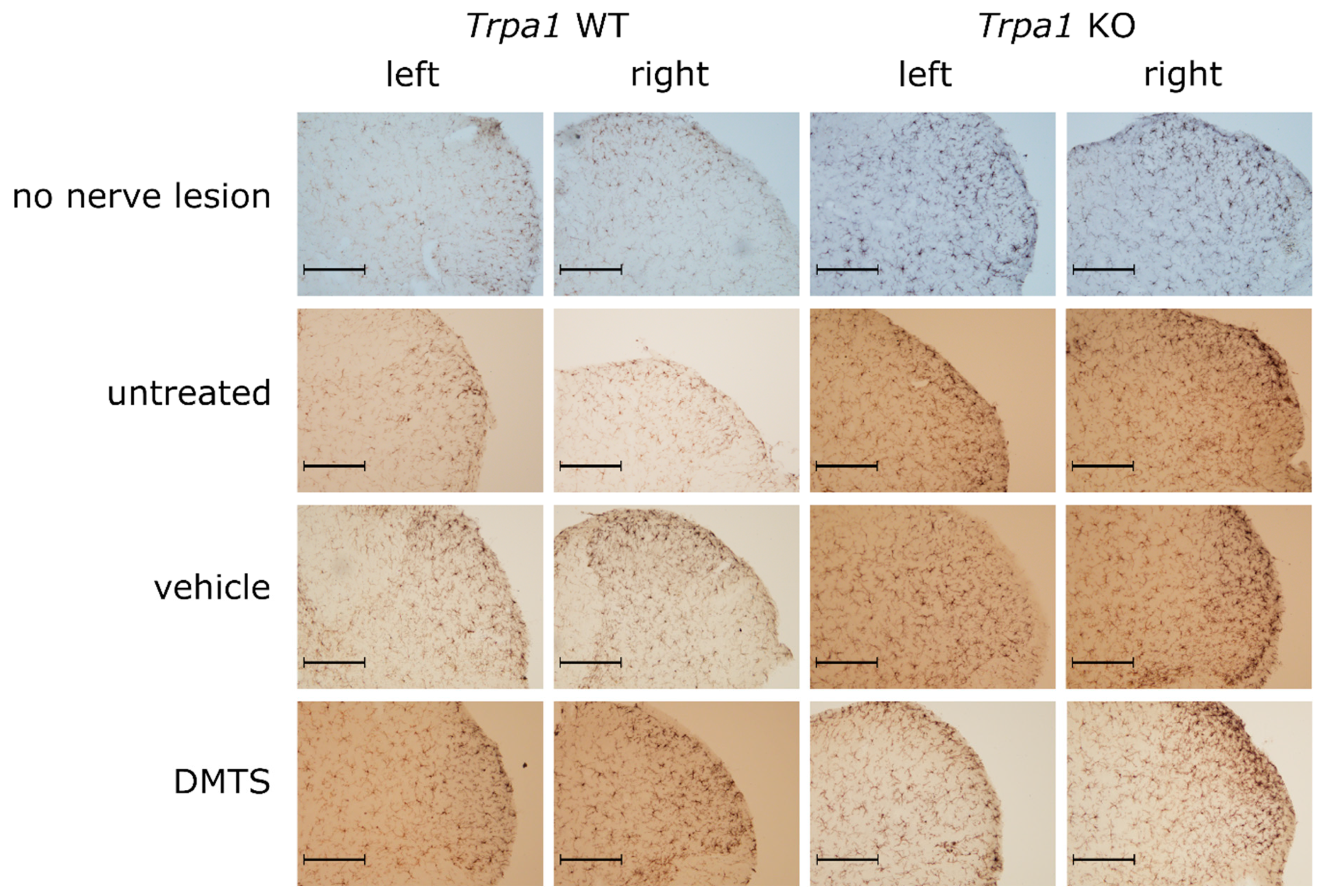
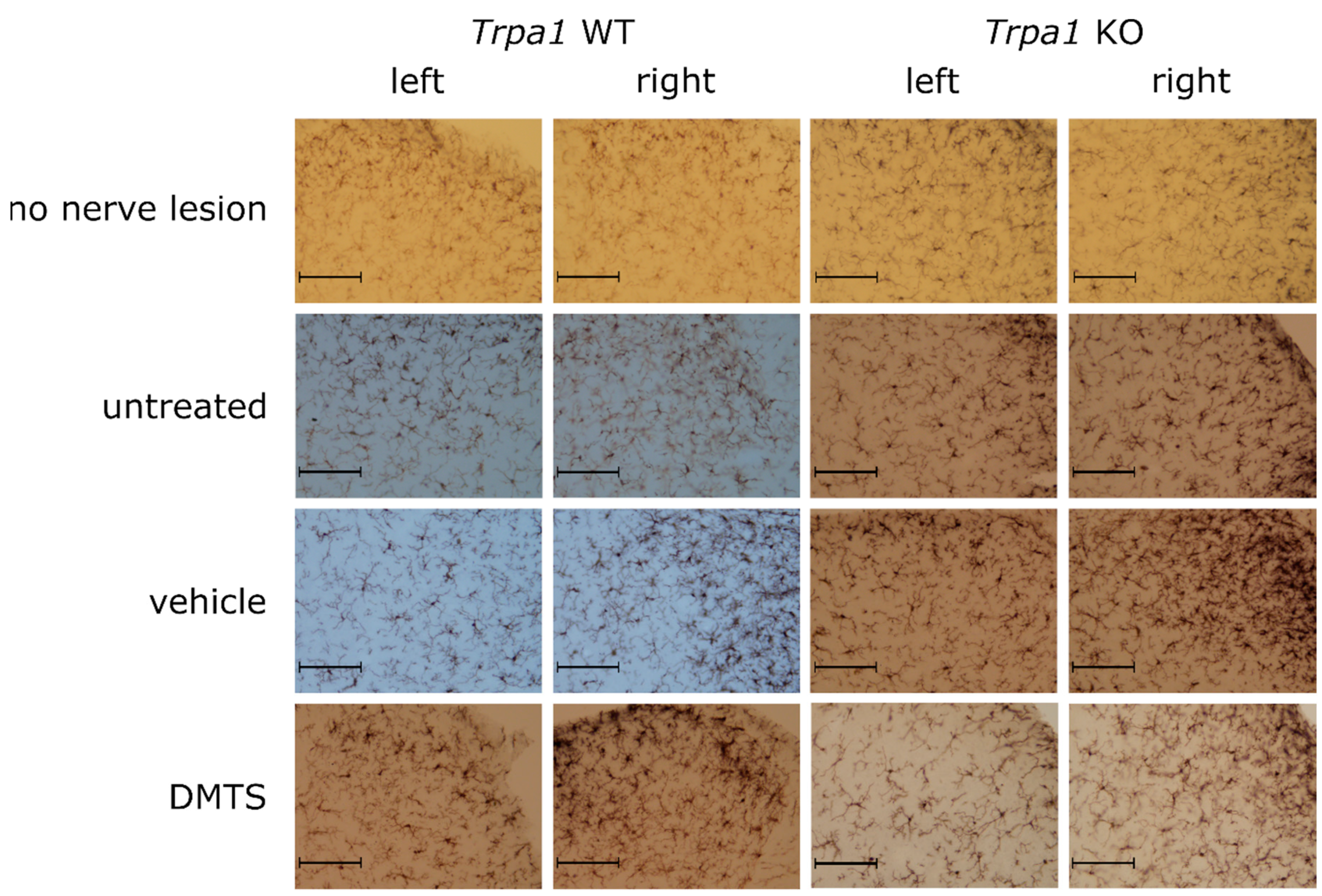
2.5. DMTS Mitigates Microglia Density in the Spinal Cord Dorsal Horn Independently from TRPA1
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. RNAscope In Situ Hybridization on Mouse Dorsal Root Ganglion
4.3. Partial Ligation of the Sciatic Nerve
4.4. Detection of Mechanical Allodynia
4.5. Dimethyl Trisulfide Treatment
4.6. Luminescent Imaging of Macrophages
4.7. Immunohistochemistry of IBA1
4.8. Histological Evaluation
4.9. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murnion, B.P. Neuropathic Pain: Current Definition and Review of Drug Treatment. Aust. Prescr. 2018, 41, 60–63. [Google Scholar] [CrossRef]
- Hicks, C.W.; Selvin, E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr. Diabetes Rep. 2019, 19, 86. [Google Scholar] [CrossRef]
- Andrew, R.; Derry, S.; Taylor, R.S.; Straube, S.; Phillips, C.J. The Costs and Consequences of Adequately Managed Chronic Non-Cancer Pain and Chronic Neuropathic Pain. Pain Pract. 2014, 14, 79–94. [Google Scholar] [CrossRef]
- Moisset, X.; Bouhassira, D.; Avez Couturier, J.; Alchaar, H.; Conradi, S.; Delmotte, M.H.; Lanteri-Minet, M.; Lefaucheur, J.P.; Mick, G.; Piano, V.; et al. Pharmacological and Non-Pharmacological Treatments for Neuropathic Pain: Systematic Review and French Recommendations. Rev. Neurol. 2020, 176, 325–352. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.A.; Straube, S.; Aldington, D. Pain Measures and Cut-Offs—‘No Worse than Mild Pain’ as a Simple, Universal Outcome. Anaesthesia 2013, 68, 400–412. [Google Scholar] [CrossRef] [PubMed]
- Evoy, K.E.; Covvey, J.R.; Peckham, A.M.; Ochs, L.; Hultgren, K.E. Reports of Gabapentin and Pregabalin Abuse, Misuse, Dependence, or Overdose: An Analysis of the Food and Drug Administration Adverse Events Reporting System (FAERS). Res. Soc. Adm. Pharm. 2019, 15, 953–958. [Google Scholar] [CrossRef]
- Vickers-Smith, R.; Sun, J.; Charnigo, R.J.; Lofwall, M.R.; Walsh, S.L.; Havens, J.R. Gabapentin Drug Misuse Signals: A Pharmacovigilance Assessment Using the FDA Adverse Event Reporting System. Drug Alcohol Depend. 2020, 206, 107709. [Google Scholar] [CrossRef]
- Giorgi, S.; Nikolaeva-Koleva, M.; Alarcón-Alarcón, D.; Butrón, L.; González-Rodríguez, S. Is TRPA1 Burning Down TRPV1 as Druggable Target for the Treatment of Chronic Pain? Int. J. Mol. Sci. 2019, 20, 2906. [Google Scholar] [CrossRef]
- Uchiyama, M.; Nakao, A.; Kurita, Y.; Fukushi, I.; Takeda, K.; Numata, T.; Tran, H.N.; Sawamura, S.; Ebert, M.; Kurokawa, T.; et al. O2-Dependent Protein Internalization Underlies Astrocytic Sensing of Acute Hypoxia by Restricting Multimodal TRPA1 Channel Responses. Curr. Biol. 2020, 30, 3378–3396.e7. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, S.S.; Majhi, R.K.; Tiwari, A.; Acharya, T.; Kumar, P.S.; Saha, S.; Kumar, A.; Goswami, C.; Chattopadhyay, S. Transient Receptor Potential Ankyrin1 Channel is Endogenously Expressed in T Cells and is Involved in Immune Functions. Biosci. Rep. 2019, 39. [Google Scholar] [CrossRef]
- Pozsgai, G.; Bátai, I.Z.; Pintér, E. Effects of Sulfide and Polysulfides Transmitted by Direct or Signal Transduction-mediated Activation of TRPA1 Channels. Br. J. Pharmacol. 2019, 176, 628–645. [Google Scholar] [CrossRef] [PubMed]
- Brandolini, L.; d’Angelo, M.; Antonosante, A.; Cimini, A.; Allegretti, M. Chemokine Signaling in Chemotherapy-Induced Neuropathic Pain. Int. J. Mol. Sci. 2019, 20, 2904. [Google Scholar] [CrossRef]
- De Araujo, D.S.M.; Nassini, R.; Geppetti, P.; Logu, F.D. TRPA1 as a Therapeutic Target for Nociceptive Pain. Expert Opin. Ther. Targets 2020, 24, 997–1008. [Google Scholar] [CrossRef]
- De Logu, F.; Nassini, R.; Materazzi, S.; Carvalho Gonçalves, M.; Nosi, D.; Rossi Degl’Innocenti, D.; Marone, I.M.; Ferreira, J.; Li Puma, S.; Benemei, S.; et al. Schwann Cell TRPA1 Mediates Neuroinflammation That Sustains Macrophage-Dependent Neuropathic Pain in Mice. Nat. Commun. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Nagahara, N.; Koike, S.; Nirasawa, T.; Kimura, H.; Ogasawara, Y. Alternative Pathway of H2S and Polysulfides Production from Sulfurated Catalytic-Cysteine of Reaction Intermediates of 3-Mercaptopyruvate Sulfurtransferase. Biochem. Biophys. Res. Commun. 2018, 496, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Bátai, I.Z.; Sár, C.P.; Horváth, Á.; Borbély, É.; Bölcskei, K.; Kemény, Á.; Sándor, Z.; Nemes, B.; Helyes, Z.; Perkecz, A.; et al. TRPA1 Ion Channel Determines Beneficial and Detrimental Effects of GYY4137 in Murine Serum-Transfer Arthritis. Front. Pharmacol. 2019, 10, 964. [Google Scholar] [CrossRef]
- Cortese-Krott, M.M.; Kuhnle, G.G.C.; Dyson, A.; Fernandez, B.O.; Grman, M.; DuMond, J.F.; Barrow, M.P.; McLeod, G.; Nakagawa, H.; Ondrias, K.; et al. Key Bioactive Reaction Products of the NO/H2S Interaction are S/N-Hybrid Species, Polysulfides, and Nitroxyl. Proc. Natl. Acad. Sci. USA 2015, 112, E4651–E4660. [Google Scholar] [CrossRef]
- Byers, J.A. Earwigs (Labidura Riparia) Mimic Rotting-Flesh Odor to Deceive Vertebrate Predators. Naturwissenschaften 2015, 102, 38. [Google Scholar] [CrossRef]
- Yamasaki, R.; Goshima, T.; Oba, K.; Isogai, A.; Ohdoi, R.; Hirata, D.; Akao, T. Characteristic Analysis of the Fermentation and Sporulation Properties of the Traditional Sake Yeast Strain Hiroshima No.6. Biosci. Biotechnol. Biochem. 2020, 84, 842–853. [Google Scholar] [CrossRef]
- Bátai, I.Z.; Horváth, Á.; Pintér, E.; Helyes, Z.; Pozsgai, G. Role of Transient Receptor Potential Ankyrin 1 Ion Channel and Somatostatin Sst4 Receptor in the Antinociceptive and Anti-Inflammatory Effects of Sodium Polysulfide and Dimethyl Trisulfide. Front. Endocrinol. 2018, 9, 55. [Google Scholar] [CrossRef]
- Hatakeyama, Y.; Takahashi, K.; Tominaga, M.; Kimura, H.; Ohta, T. Polysulfide Evokes Acute Pain through the Activation of Nociceptive TRPA1 in Mouse Sensory Neurons. Mol. Pain 2015, 11, 24. [Google Scholar] [CrossRef]
- Pozsgai, G.; Payrits, M.; Sághy, É.; Sebestyén-Bátai, R.; Steen, E.; Szőke, É.; Sándor, Z.; Solymár, M.; Garami, A.; Orvos, P.; et al. Analgesic Effect of Dimethyl Trisulfide in Mice is Mediated by TRPA1 and Sst4 Receptors. Nitric Oxide 2017, 65, 10–21. [Google Scholar] [CrossRef] [PubMed]
- De Silva, D.; Lee, S.; Duke, A.; Angalakurthi, S.; Chou, C.-E.; Ebrahimpour, A.; Thompson, D.E.; Petrikovics, I. Intravascular Residence Time Determination for the Cyanide Antidote Dimethyl Trisulfide in Rat by Using Liquid-Liquid Extraction Coupled with High Performance Liquid Chromatography. J. Anal. Methods Chem. 2016, 2016, 6546475. [Google Scholar] [CrossRef] [PubMed]
- Kántás, B.; Börzsei, R.; Szőke, É.; Bánhegyi, P.; Horváth, Á.; Hunyady, Á.; Borbély, É.; Hetényi, C.; Pintér, E.; Helyes, Z. Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain. Int. J. Mol. Sci. 2019, 20, 6245. [Google Scholar] [CrossRef]
- Kecskés, A.; Pohóczky, K.; Kecskés, M.; Varga, Z.V.; Kormos, V.; Szőke, É.; Henn-Mike, N.; Fehér, M.; Kun, J.; Gyenesei, A.; et al. Characterization of Neurons Expressing the Novel Analgesic Drug Target Somatostatin Receptor 4 in Mouse and Human Brains. Int. J. Mol. Sci. 2020, 21, 7788. [Google Scholar] [CrossRef]
- Billeter, A.T.; Galbraith, N.; Walker, S.; Lawson, C.; Gardner, S.A.; Sarojini, H.; Galandiuk, S.; Polk, H.C. TRPA1 Mediates the Effects of Hypothermia on the Monocyte Inflammatory Response. Surgery 2015, 158, 646–654. [Google Scholar] [CrossRef]
- Zhao, J.-F.; Shyue, S.-K.; Kou, Y.R.; Lu, T.-M.; Lee, T.-S. Transient Receptor Potential Ankyrin 1 Channel Involved in Atherosclerosis and Macrophage-Foam Cell Formation. Int. J. Biol. Sci. 2016, 12, 812–823. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Chen, K.; Zhang, F.; Peng, K.; Wang, Z.; Yang, D.; Yang, Y. TRPA1 Regulates Macrophages Phenotype Plasticity and Atherosclerosis Progression. Atherosclerosis 2020, 301, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Ueda, H.; Neyama, H.; Nagai, J.; Matsushita, Y.; Tsukahara, T.; Tsukahara, R. Involvement of Lysophosphatidic Acid-Induced Astrocyte Activation Underlying the Maintenance of Partial Sciatic Nerve Injury-Induced Neuropathic Pain. Pain 2018, 159, 2170–2178. [Google Scholar] [CrossRef]
- Yamagata, R.; Nemoto, W.; Nakagawasai, O.; Hung, W.-Y.; Shima, K.; Endo, Y.; Tan-No, K. Etidronate Attenuates Tactile Allodynia by Spinal ATP Release Inhibition in Mice with Partial Sciatic Nerve Ligation. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2019, 392, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Hunyady, Á.; Hajna, Z.; Gubányi, T.; Scheich, B.; Kemény, Á.; Gaszner, B.; Borbély, É.; Helyes, Z. Hemokinin-1 is an Important Mediator of Pain in Mouse Models of Neuropathic and Inflammatory Mechanisms. Brain Res. Bull. 2019, 147, 165–173. [Google Scholar] [CrossRef]
- Zhang, T.; Ono, K.; Tsutsuki, H.; Ihara, H.; Islam, W.; Akaike, T.; Sawa, T. Enhanced Cellular Polysulfides Negatively Regulate TLR4 Signaling and Mitigate Lethal Endotoxin Shock. Cell Chem. Biol. 2019. [Google Scholar] [CrossRef]
- Araki, S.; Takata, T.; Tsuchiya, Y.; Watanabe, Y. Reactive Sulfur Species Impair Ca2+/Calmodulin-Dependent Protein Kinase II via Polysulfidation. Biochem. Biophys. Res. Commun. 2019, 508, 550–555. [Google Scholar] [CrossRef]
- Dai, X.; Meng, J.; Deng, S.; Zhang, L.; Wan, C.; Lu, L.; Huang, J.; Hu, Y.; Zhang, Z.; Li, Y.; et al. Targeting CAMKII to Reprogram Tumor-Associated Macrophages and Inhibit Tumor Cells for Cancer Immunotherapy with an Injectable Hybrid Peptide Hydrogel. Theranostics 2020, 10, 3049–3063. [Google Scholar] [CrossRef] [PubMed]
- Doran, A.C.; Ozcan, L.; Cai, B.; Zheng, Z.; Fredman, G.; Rymond, C.C.; Dorweiler, B.; Sluimer, J.C.; Hsieh, J.; Kuriakose, G.; et al. CAMKIIγ Suppresses an Efferocytosis Pathway in Macrophages and Promotes Atherosclerotic Plaque Necrosis. J. Clin. Investig. 2017, 127, 4075–4089. [Google Scholar] [CrossRef]
- Lee, H.H.; Han, M.H.; Hwang, H.J.; Kim, G.-Y.; Moon, S.-K.; Hyun, J.-W.; Kim, W.-J.; Choi, Y.H. Diallyl Trisulfide Exerts Anti-Inflammatory Effects in Lipopolysaccharide-stimulated RAW 264.7 Macrophages by Suppressing the Toll-like Receptor 4/Nuclear Factor-ΚB Pathway. Int. J. Mol. Med. 2015, 35, 487–495. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, X.; He, N.; Wang, Y.; Kang, Q.; Shen, D.; Yu, F.; Chen, L. Imaging of Anti-Inflammatory Effects of HNO via a near-Infrared Fluorescent Probe in Cells and in Rat Gouty Arthritis Model. J. Mater. Chem. B 2019, 7, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Jeong, J.-W.; Hong, S.H.; Park, C.; Kim, B.W.; Choi, Y.H. Diallyl Trisulfide Suppresses the Production of Lipopolysaccharide-Induced Inflammatory Mediators in BV2 Microglia by Decreasing the NF-ΚB Pathway Activity Associated with Toll-like Receptor 4 and CXCL12/CXCR4 Pathway Blockade. J. Cancer Prev. 2018, 23, 134–140. [Google Scholar] [CrossRef]
- Braunstein, I.; Engelman, R.; Yitzhaki, O.; Ziv, T.; Galardon, E.; Benhar, M. Opposing Effects of Polysulfides and Thioredoxin on Apoptosis through Caspase Persulfidation. J. Biol. Chem. 2020, 295, 3590–3600. [Google Scholar] [CrossRef]
- Greiner, R.; Pálinkás, Z.; Bäsell, K.; Becher, D.; Antelmann, H.; Nagy, P.; Dick, T.P. Polysulfides Link H2S to Protein Thiol Oxidation. Antioxid. Redox Signal. 2013, 19, 1749–1765. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liu, H.; Chen, Z.; Zhao, R.; Wang, Q.; Ran, M.; Xia, Y.; Hu, X.; Liu, J.; Xian, M.; et al. Using Resonance Synchronous Spectroscopy to Characterize the Reactivity and Electrophilicity of Biologically Relevant Sulfane Sulfur. Redox Biol. 2019, 24. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.V.; Brabb, T.; Pekow, C.; Vasbinder, M.A. Administration of Substances to Laboratory Animals: Routes of Administration and Factors to Consider. J. Am. Assoc. Lab. Anim. Sci. 2011, 50, 600–613. [Google Scholar] [PubMed]
- Kiss, L.; Bocsik, A.; Walter, F.R.; Ross, J.; Brown, D.; Mendenhall, B.A.; Crews, S.R.; Lowry, J.; Coronado, V.; Thompson, D.E.; et al. From the Cover: In Vitro and In Vivo Blood-Brain Barrier Penetration Studies with the Novel Cyanide Antidote Candidate Dimethyl Trisulfide in Mice. Toxicol. Sci. 2017, 160, 398–407. [Google Scholar] [CrossRef] [PubMed]
- Story, G.M.; Peier, A.M.; Reeve, A.J.; Eid, S.R.; Mosbacher, J.; Hricik, T.R.; Earley, T.J.; Hergarden, A.C.; Andersson, D.A.; Hwang, S.W.; et al. ANKTM1, a TRP-like Channel Expressed in Nociceptive Neurons, is Activated by Cold Temperatures. Cell 2003, 112, 819–829. [Google Scholar] [CrossRef]
- Pethő, G.; Bölcskei, K.; Füredi, R.; Botz, B.; Bagoly, T.; Pintér, E.; Szolcsányi, J. Evidence for a Novel, Neurohumoral Antinociceptive Mechanism Mediated by Peripheral Capsaicin-Sensitive Nociceptors in Conscious Rats. Neuropeptides 2017, 62, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sándor, K.; Elekes, K.; Szabó, Á.; Pintér, E.; Engström, M.; Wurster, S.; Szolcsányi, J.; Helyes, Z. Analgesic Effects of the Somatostatin Sst4 Receptor Selective Agonist J-2156 in Acute and Chronic Pain Models. Eur. J. Pharmacol. 2006, 539, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Gorham, L.; Just, S.; Doods, H. Somatostatin 4 Receptor Activation Modulates TPRV1 Currents in Dorsal Root Ganglion Neurons. Neurosci. Lett. 2014, 573, 35–39. [Google Scholar] [CrossRef]
- Hamilton, N.B.; Kolodziejczyk, K.; Kougioumtzidou, E.; Attwell, D. Proton-Gated Ca2+-Permeable TRP Channels Damage Myelin in Conditions Mimicking Ischaemia. Nature 2016, 529, 523–527. [Google Scholar] [CrossRef]
- Jiang, L.; Ma, D.; Grubb, B.D.; Wang, M. ROS/TRPA1/CGRP Signaling Mediates Cortical Spreading Depression. J. Headache Pain 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.M.; Collins, M.A.; Chin, R.; Ge, T.; Rosenberg, M.D.; Holmes, A.J. Transcriptional and Imaging-Genetic Association of Cortical Interneurons, Brain Function, and Schizophrenia Risk. Nat. Commun. 2020, 11. [Google Scholar] [CrossRef]
- Thoss, V.S.; Ferez, J.; Duc, D.; Hoyer, D. Embryonic and Postnatal MRNA Distribution of Five Somatostatin Receptor Subtypes in the Rat Brain. Neuropharmacology 1995, 34, 1673–1688. [Google Scholar] [CrossRef]
- Selmer, I.-S.; Schindler, M.; Humphrey, P.P.A.; Emson, P.C. Immunohistochemical Localization of the Somatostatin Sst4 Receptor in Rat Brain. Neuroscience 2000, 98, 523–533. [Google Scholar] [CrossRef]
- Schreff, M.; Schulz, S.; Händel, M.; Keilhoff, G.; Braun, H.; Pereira, G.; Klutzny, M.; Schmidt, H.; Wolf, G.; Höllt, V. Distribution, Targeting, and Internalization of the Sst4 Somatostatin Receptor in Rat Brain. J. Neurosci. 2000, 20, 3785–3797. [Google Scholar] [CrossRef]
- Scheich, B.; Csekő, K.; Borbély, É.; Ábrahám, I.; Csernus, V.; Gaszner, B.; Helyes, Z. Higher Susceptibility of Somatostatin 4 Receptor Gene-Deleted Mice to Chronic Stress-Induced Behavioral and Neuroendocrine Alterations. Neuroscience 2017, 346, 320–336. [Google Scholar] [CrossRef]
- Scheich, B.; Gaszner, B.; Kormos, V.; László, K.; Ádori, C.; Borbély, É.; Hajna, Z.; Tékus, V.; Bölcskei, K.; Ábrahám, I.; et al. Somatostatin Receptor Subtype 4 Activation is Involved in Anxiety and Depression-like Behavior in Mouse Models. Neuropharmacology 2016, 101, 204–215. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Arora, P.; Sandhir, R. Hydrogen Sulfide Reverses LPS-Induced Behavioral Deficits by Suppressing Microglial Activation and Promoting M2 Polarization. J. Neuroimmune Pharmacol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Zhao, L.; Mao, J.; Huang, J.; Chen, J. Antioxidant Effects of Hydrogen Sulfide on Left Ventricular Remodeling in Smoking Rats are Mediated via PI3K/Akt-Dependent Activation of Nrf2. Toxicol. Sci. 2015, 144, 197–203. [Google Scholar] [CrossRef]
- Ma, S.; Zhang, Y.; He, K.; Wang, P.; Wang, D.H. Knockout of TRPA1 Exacerbates Angiotensin II-Induced Kidney Injury. Am. J. Physiol. Ren. Physiol. 2019, 317, F623–F631. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Wang, D.H. Knockout of Trpa1 Exacerbates Renal Ischemia-Reperfusion Injury with Classical Activation of Macrophages. Am. J. Hypertens. 2021, 34, 110–116. [Google Scholar] [CrossRef]
- Usui-Kusumoto, K.; Iwanishi, H.; Ichikawa, K.; Okada, Y.; Sumioka, T.; Miyajima, M.; Liu, C.-Y.; Reinach, P.S.; Saika, S. Suppression of Neovascularization in Corneal Stroma in a TRPA1-Null Mouse. Exp. Eye Res. 2019, 181, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Zeng, D.; Chen, C.; Zhou, W.; Ma, X.; Pu, X.; Zeng, Y.; Zhou, W.; Lv, F. TRPA1 Deficiency Alleviates Inflammation of Atopic Dermatitis by Reducing Macrophage Infiltration. Life Sci. 2021, 266, 118906. [Google Scholar] [CrossRef] [PubMed]
- Bautista, D.M.; Jordt, S.-E.; Nikai, T.; Tsuruda, P.R.; Read, A.J.; Poblete, J.; Yamoah, E.N.; Basbaum, A.I.; Julius, D. TRPA1 Mediates the Inflammatory Actions of Environmental Irritants and Proalgesic Agents. Cell 2006, 124, 1269–1282. [Google Scholar] [CrossRef]
- Helyes, Z.; Pintér, E.; Sándor, K.; Elekes, K.; Bánvölgyi, Á.; Keszthelyi, D.; Szőke, É.; Tóth, D.M.; Sándor, Z.; Kereskai, L.; et al. Impaired Defense Mechanism against Inflammation, Hyperalgesia, and Airway Hyperreactivity in Somatostatin 4 Receptor Gene-Deleted Mice. Proc. Natl. Acad. Sci. USA 2009, 106, 13088–13093. [Google Scholar] [CrossRef]
- Seltzer, Z.; Dubner, R.; Shir, Y. A Novel Behavioral Model of Neuropathic Pain Disorders Produced in Rats by Partial Sciatic Nerve Injury. Pain 1990, 43, 205–218. [Google Scholar] [CrossRef]
- Tseng, J.-C.; Kung, A.L. In Vivo Imaging of Inflammatory Phagocytes. Chem. Biol. 2012, 19, 1199–1209. [Google Scholar] [CrossRef]
- Botz, B.; Bölcskei, K.; Kereskai, L.; Kovács, M.; Németh, T.; Szigeti, K.; Horváth, I.; Máthé, D.; Kovács, N.; Hashimoto, H.; et al. Differential Regulatory Role of Pituitary Adenylate Cyclase–Activating Polypeptide in the Serum-Transfer Arthritis Model. Arthritis Rheumatol. 2014, 66, 2739–2750. [Google Scholar] [CrossRef] [PubMed]
- Gaszner, B.; Kormos, V.; Kozicz, T.; Hashimoto, H.; Reglodi, D.; Helyes, Z. The Behavioral Phenotype of Pituitary Adenylate-Cyclase Activating Polypeptide-Deficient Mice in Anxiety and Depression Tests is Accompanied by Blunted c-Fos Expression in the Bed Nucleus of the Stria Terminalis, Central Projecting Edinger-Westphal Nucleus, Ventral Lateral Septum, and Dorsal Raphe Nucleus. Neuroscience 2012, 202, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Helyes, Z.; Tékus, V.; Szentes, N.; Pohóczky, K.; Botz, B.; Kiss, T.; Kemény, Á.; Környei, Z.; Tóth, K.; Lénárt, N.; et al. Transfer of Complex Regional Pain Syndrome to Mice via Human Autoantibodies is Mediated by Interleukin-1–Induced Mechanisms. Proc. Natl. Acad. Sci. USA 2019, 116, 13067–13076. [Google Scholar] [CrossRef]
- Ducza, E.; Csányi, A.; Szőke, É.; Pohóczky, K.; Hajagos-Tóth, J.; Kothencz, A.; Tiszai, Z.; Gáspár, R. Significance of Transient Receptor Potential Vanilloid 4 and Aquaporin 5 Co-Expression in the Rat Uterus at Term. Heliyon 2019, 5. [Google Scholar] [CrossRef]
- Hovens, I.B.; Nyakas, C.; Schoemaker, R.G. A Novel Method for Evaluating Microglial Activation Using Ionized Calcium-Binding Adaptor Protein-1 Staining: Cell Body to Cell Size Ratio. Neuroimmunol. Neuroinflamm. 2014, 1, 82–88. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dombi, Á.; Sánta, C.; Bátai, I.Z.; Kormos, V.; Kecskés, A.; Tékus, V.; Pohóczky, K.; Bölcskei, K.; Pintér, E.; Pozsgai, G. Dimethyl Trisulfide Diminishes Traumatic Neuropathic Pain Acting on TRPA1 Receptors in Mice. Int. J. Mol. Sci. 2021, 22, 3363. https://doi.org/10.3390/ijms22073363
Dombi Á, Sánta C, Bátai IZ, Kormos V, Kecskés A, Tékus V, Pohóczky K, Bölcskei K, Pintér E, Pozsgai G. Dimethyl Trisulfide Diminishes Traumatic Neuropathic Pain Acting on TRPA1 Receptors in Mice. International Journal of Molecular Sciences. 2021; 22(7):3363. https://doi.org/10.3390/ijms22073363
Chicago/Turabian StyleDombi, Ágnes, Csenge Sánta, István Z. Bátai, Viktória Kormos, Angéla Kecskés, Valéria Tékus, Krisztina Pohóczky, Kata Bölcskei, Erika Pintér, and Gábor Pozsgai. 2021. "Dimethyl Trisulfide Diminishes Traumatic Neuropathic Pain Acting on TRPA1 Receptors in Mice" International Journal of Molecular Sciences 22, no. 7: 3363. https://doi.org/10.3390/ijms22073363
APA StyleDombi, Á., Sánta, C., Bátai, I. Z., Kormos, V., Kecskés, A., Tékus, V., Pohóczky, K., Bölcskei, K., Pintér, E., & Pozsgai, G. (2021). Dimethyl Trisulfide Diminishes Traumatic Neuropathic Pain Acting on TRPA1 Receptors in Mice. International Journal of Molecular Sciences, 22(7), 3363. https://doi.org/10.3390/ijms22073363






