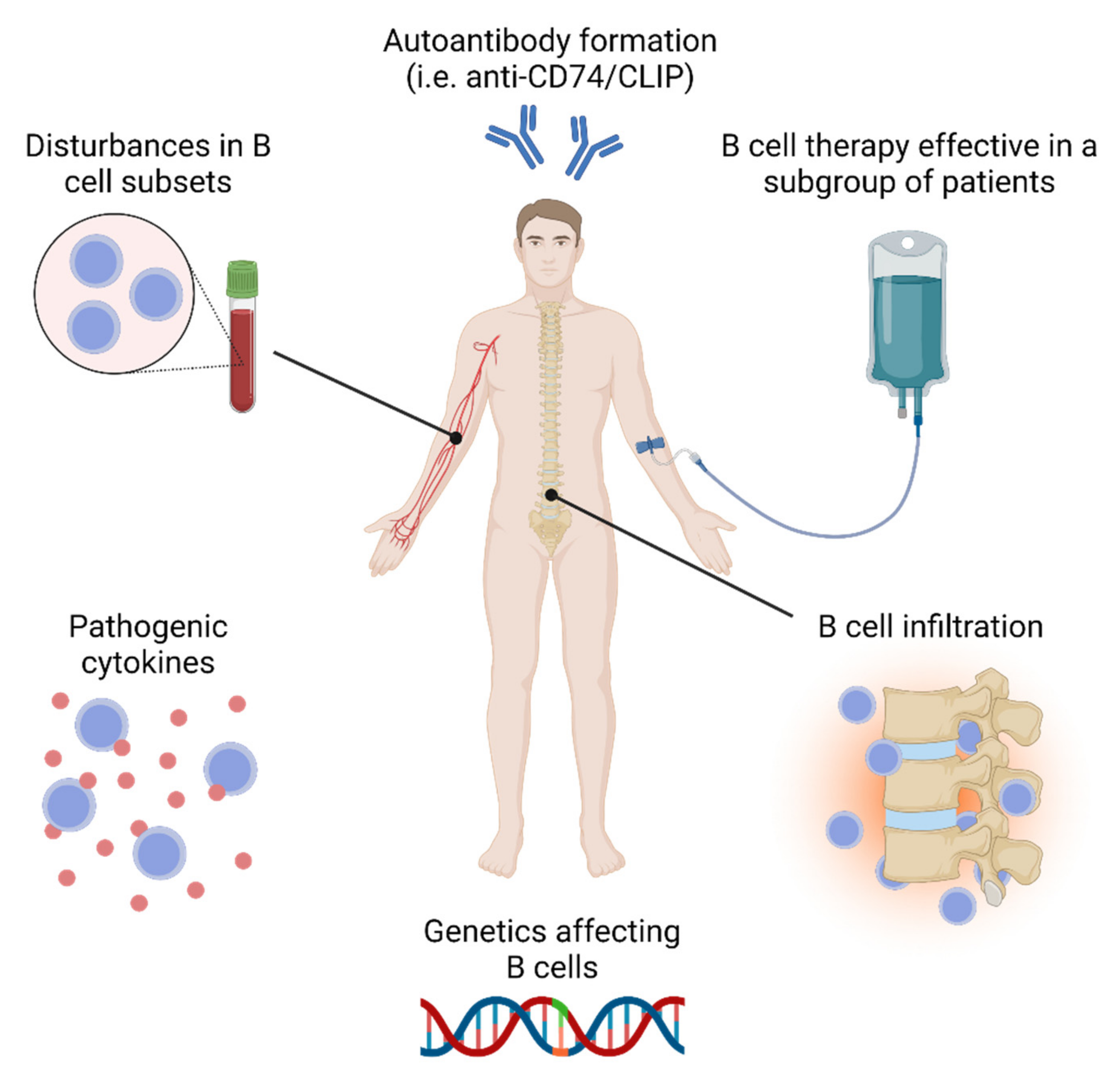
B Cell Involvement in the Pathogenesis of Ankylosing Spondylitis
Abstract
1. Introduction
2. Gene Variants in AS Modulating B Cell Function
3. Disturbances of the Peripheral B Cell Compartment in AS
3.1. Disturbances in the Total B Cells and Major B Cells in Subpopulations
| Reference | Total B | Transitional | Naïve | Memory | Plasmablast/Cell |
|---|---|---|---|---|---|
| CD19+ | CD24+CD38+ | IgD+CD27− | IgD−CD27+ | CD27hi/CD38hi | |
| Brand et al. [41] | Normal | N/A | N/A | N/A | N/A |
| Chen et al. [42] | Normal | N/A | N/A | N/A | N/A |
| Szanto et al. [43] | Normal | N/A | N/A | N/A | N/A |
| Bautista-Caro et al. [48] | N/A | N/A | N/A | N/A | ↓ $ |
| Lin et al. [46] | ↑ * | Normal | Normal | Normal | ↑ ** |
| Long et al. [44] | Normal | N/A | ↑ * | ↓ * | ↑ |
| Yang et al. [47] | ↑ | ↓ | N/A | ↑/↓ % | ↓ |
| Bautista-Caro et al. [45] | Normal | ↑ | N/A | N/A | N/A |
| Chen et al. [38] | Normal | Normal | ↓ | ↑ | ↑ |
| Niu et al. [49] | N/A | N/A | Normal | ↓ | N/A |
| Wilbrink et al. [20] | Normal | Normal | Normal | Normal | ↑ |
3.2. IL-10 Producing B Cells in AS
3.3. Activated B Cells in AS
3.4. The CD21low B Cell Population in AS
4. Auto-Reactive and Non-Autoreactive Antibodies in AS
| Reactivity Against | Category | Reference |
|---|---|---|
| Intracellular components | ||
| Nuclear antibodies (ANAs) | Nuclear antigens | [69,70] |
| Antineutrophil cytoplasmic antibodies(ANCA) | Cytoplasmic molecules | [71,72] |
| Prefoldin subunit 5 | Chaperone proteins | [73] |
| Beta-2 microglobulin and CD74 | MHC class I and II related molecules | [74,75,76,77,78,79,80,81,82] |
| Microbial components | ||
| Klebsiella pneumonia, and mycobacterium | Microbial epitopes and molecules | [83,84,85,86,87,88,89] |
| Bone metabolism and connective components | ||
| Sclerostin, bone metabolism, and signaling molecules (NAD-dependent protein deacytelase sirtuin-1 and osteoprotegerin) | Bone tissue | [90,91,92,93,94,95,96] |
| Extracellular matrix proteins, collagen and ATP synthase subunit-α | Connective and skeletal muscle tissue | [92,97,98] |
| Post-translational modifications | ||
| Citrullinated cyclic peptides and carbamylated proteins | Modified molecules | [99,100,101] |
| Other components | ||
| UH-axSpA peptides | Unidentified proteins and peptides | [102] |
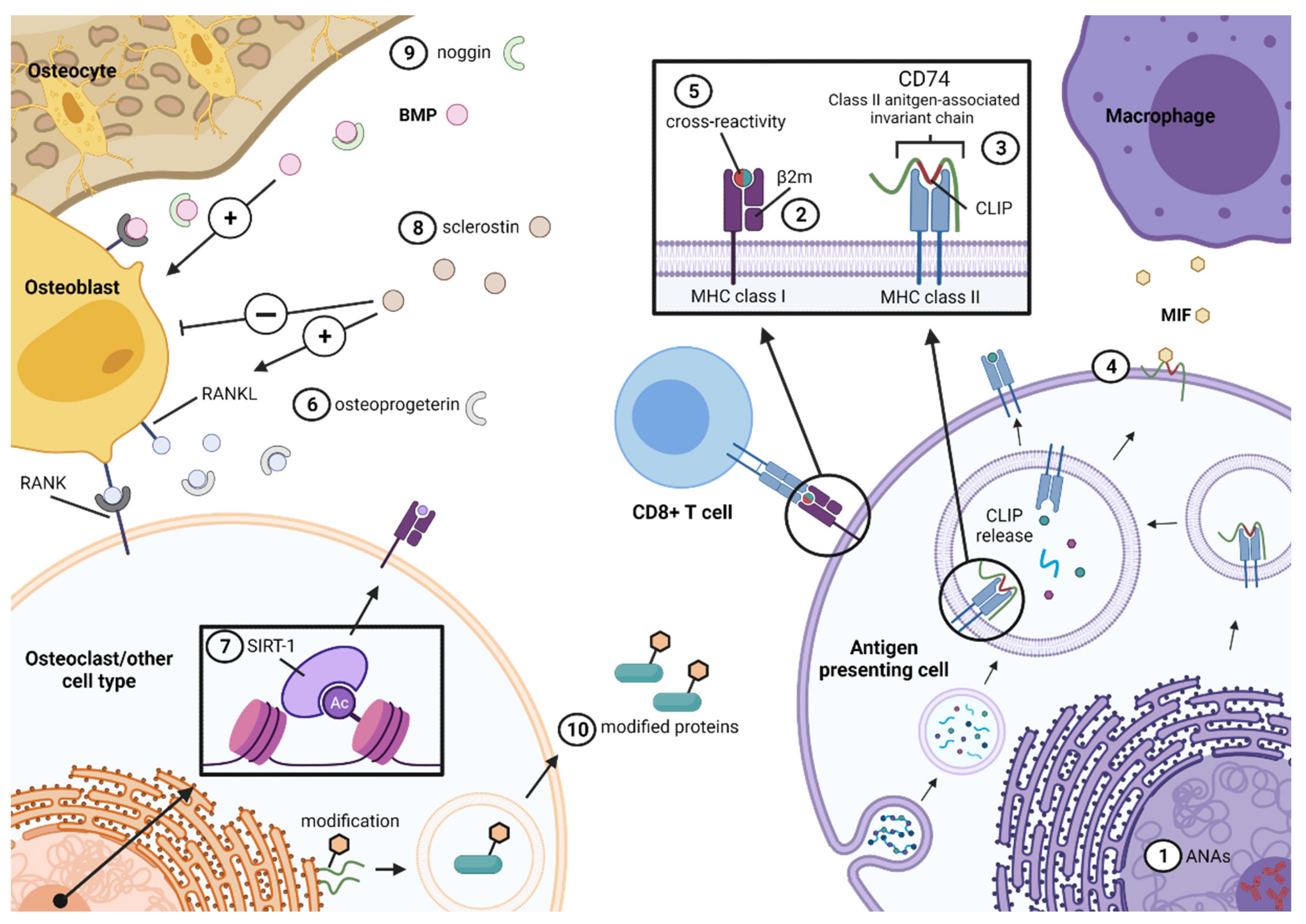
4.1. Autoantibodies Reactive to Intracellular Antigens
4.2. Antibodies Directed against Intracellular Molecules Involved in Antigen Presentation
4.3. Antibodies Affecting Bone Metabolism
4.4. Antibodies to Cross-Reactive Microbial Antigens
4.5. Antibodies Directed against Modified Self-Proteins and Self-Peptides
5. B-Cell-Associated Cytokines in AS
6. B Cell Infiltration of AS Target Tissues
7. Targeting B Cells in AS
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dougados, M.; Baeten, D. Spondyloarthritis. Lancet 2011, 377, 2127–2137. [Google Scholar] [CrossRef]
- Sieper, J.; Poddubnyy, D. Axial Spondyloarthritis. Lancet 2017, 390, 73–84. [Google Scholar] [CrossRef]
- Stolwijk, C.; van Tubergen, A.; Castillo-Ortiz, J.D.; Boonen, A. Prevalence of Extra-Articular Manifestations in Patients with Ankylosing Spondylitis: A Systematic Review and Meta-Analysis. Ann. Rheum. Dis. 2015, 74, 65–73. [Google Scholar] [CrossRef]
- Zhu, W.; He, X.; Cheng, K.; Zhang, L.; Chen, D.; Wang, X.; Qiu, G.; Cao, X.; Weng, X. Ankylosing Spondylitis: Etiology, Pathogenesis, and Treatments. Bone Res. 2019, 7, 22. [Google Scholar] [CrossRef]
- Mauro, D.; Thomas, R.; Guggino, G.; Lories, R.; Brown, M.A.; Ciccia, F. Ankylosing Spondylitis: An Autoimmune or Autoinflammatory Disease? Nat. Rev. Rheumatol. 2021, 17, 387–404. [Google Scholar] [CrossRef]
- Sieper, J.; Poddubnyy, D.; Miossec, P. The IL-23–IL-17 Pathway as a Therapeutic Target in Axial Spondyloarthritis. Nat. Rev. Rheumatol. 2019, 15, 747–757. [Google Scholar] [CrossRef]
- Watad, A.; Bridgewood, C.; Russell, T.; Marzo-Ortega, H.; Cuthbert, R.; McGonagle, D. The Early Phases of Ankylosing Spondylitis: Emerging Insights From Clinical and Basic Science. Front. Immunol. 2018, 9, 2668. [Google Scholar] [CrossRef] [PubMed]
- Debusschere, K.; Cambré, I.; Gracey, E.; Elewaut, D. Born to Run: The Paradox of Biomechanical Force in Spondyloarthritis from an Evolutionary Perspective. Best Pract. Res. Clin. Rheumatol. 2017, 31, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.P.; Brown, M.A. Genetics and Genomics of Ankylosing Spondylitis. Immunol. Rev. 2010, 233, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Wielińska, J.; Świerkot, J.; Kolossa, K.; Bugaj, B.; Chaszczewska-Markowska, M.; Jeka, S.; Bogunia-Kubik, K. Polymorphisms within Genes Coding for IL-17A and F and Their Receptor as Clinical Hallmarks in Ankylosing Spondylitis. Mediat. Inflamm. 2021, 2021, 3125922. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, G.; Guan, Y.; Zhao, X.; Wang, Q.; Li, H.; Qi, J. Association of IFN-γ Polymorphisms with Ankylosing Spondylitis Risk. J. Cell. Mol. Med. 2020, 24, 10615. [Google Scholar] [CrossRef] [PubMed]
- Cortes, A.; Hadler, J.; Pointon, J.P.; Robinson, P.C.; Karaderi, T.; Leo, P.; Cremin, K.; Pryce, K.; Harris, J.; Lee, S.; et al. Identification of Multiple Risk Variants for Ankylosing Spondylitis through High-Density Genotyping of Immune-Related Loci. Nat. Genet. 2013, 45, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A. Regulation of Cytokine Production by the Unfolded Protein Response; Implications for Infection and Autoimmunity. Front. Immunol. 2018, 9, 422. [Google Scholar] [CrossRef]
- Ramos, M.; Alvarez, I.; Sesma, L.; Logean, A.; Rognan, D.; de López Castro, J.A. Molecular Mimicry of an HLA-B27-Derived Ligand of Arthritis-Linked Subtypes with Chlamydial Proteins. J. Biol. Chem. 2002, 277, 37573–37581. [Google Scholar] [CrossRef] [PubMed]
- Ciccia, F.; Guggino, G.; Rizzo, A.; Allesandro, R.; Luchetti, M.M.; Milling, S.; Saieva, L.; Cypers, H.; Stampone, T.; Di Benedetto, P.; et al. Dysbiosis and Zonulin Upregulation Alter Gut Epithelial and Vascular Barriers in Patients with Ankylosing Spondylitis. Ann. Rheum. Dis. 2017, 76, 1123–1132. [Google Scholar] [CrossRef]
- Simone, D.; Mossawi, M.H.L.; Bowness, P. Progress in Our Understanding of the Pathogenesis of Ankylosing Spondylitis. Rheumatology 2018, 57, vi4. [Google Scholar] [CrossRef] [PubMed]
- Gravallese, E.M.; Schett, G. Effects of the IL-23–IL-17 Pathway on Bone in Spondyloarthritis. Nat. Rev. Rheumatol. 2018, 14, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Gong, Y.; Zhang, Y.; Wang, D.; Xiao, Z. Immunohistological Analysis of Active Sacroiliitis in Patients with Axial Spondyloarthritis. Medicine 2017, 96, e6605. [Google Scholar] [CrossRef]
- Appel, H.; Kuhne, M.; Spiekermann, S.; Ebhardt, H.; Grozdanovic, Z.; Köhler, D.; Dreimann, M.; Hempfing, A.; Rudwaleit, M.; Stein, H.; et al. Immunohistologic Analysis of Zygapophyseal Joints in Patients with Ankylosing Spondylitis. Arthritis Rheum. 2006, 54, 2845–2851. [Google Scholar] [CrossRef]
- Wilbrink, R.; Spoorenberg, A.; Arends, S.; van der Geest, K.S.M.; Brouwer, E.; Bootsma, H.; Kroese, F.G.M.; Verstappen, G.M. CD27-CD38lowCD21low B-Cells Are Increased in Axial Spondyloarthritis. Front. Immunol. 2021, 12, 2148. [Google Scholar] [CrossRef]
- Quaden, D.H.F.; de Winter, L.M.; Somers, V. Detection of Novel Diagnostic Antibodies in Ankylosing Spondylitis: An Overview; Elsevier B.V.: Amsterdam, The Netherlands, 2016; Volume 15, pp. 820–832. [Google Scholar]
- Song, I.-H.; Heldmann, F.; Rudwaleit, M.; Listing, J.; Appel, H.; Braun, J.; Sieper, J. Different Response to Rituximab in Tumor Necrosis Factor Blocker-Naive Patients with Active Ankylosing Spondylitis and in Patients in Whom Tumor Necrosis Factor Blockers Have Failed: A Twenty-Four-Week Clinical Trial. Arthritis Rheum. 2010, 62, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Reveille, J.D.; Zhou, X.; Lee, M.; Weisman, M.H.; Yi, L.; Gensler, L.S.; Zou, H.; Ward, M.M.; Ishimori, M.; Learch, T.J.; et al. HLA Class I and II Alleles in Susceptibility to Ankylosing Spondylitis. Ann. Rheum. Dis. 2019, 78, 66. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wu, H.; Zhao, M.; Chang, C.; Lu, Q. The Bach Family of Transcription Factors: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2016, 50, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Muto, A.; Ochiai, K.; Kimura, Y.; Itoh-Nakadai, A.; Calame, K.L.; Ikebe, D.; Tashiro, S.; Igarashi, K. Bach2 Represses Plasma Cell Gene Regulatory Network in B Cells to Promote Antibody Class Switch. EMBO J. 2010, 29, 4048. [Google Scholar] [CrossRef] [PubMed]
- Lahmann, A.; Kuhrau, J.; Fuhrmann, F.; Heinrich, F.; Bauer, L.; Durek, P.; Mashreghi, M.-F.; Hutloff, A. Bach2 Controls T Follicular Helper Cells by Direct Repression of Bcl-6. J. Immunol. 2019, 202, 2229–2239. [Google Scholar] [CrossRef]
- Geng, J.; Wei, H.; Shi, B.; Wang, Y.-H.; Greer, B.D.; Pittman, M.; Smith, E.; Thomas, P.G.; Kutsch, O.; Hu, H. Bach2 Negatively Regulates Tfh Cell Differentiation and Is Critical for CD4+ T Cell Memory. J. Immunol. 2019, 202, 2991. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Haynes, K.; Pennisi, D.J.; Anderson, L.K.; Song, X.; Thomas, G.P.; Kenna, T.; Leo, P.; Brown, M.A. Epigenetic and Gene Expression Analysis of Ankylosing Spondylitis-Associated Loci Implicate Immune Cells and the Gut in the Disease Pathogenesis. Genes Immun. 2017, 18, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Lazarevic, V.; Glimcher, L.H.; Lord, G.M. T-Bet: A Bridge between Innate and Adaptive Immunity. Nat. Rev. Immunol. 2013, 13, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Szabo, S.J.; Kim, S.T.; Costa, G.L.; Zhang, X.; Fathman, C.G.; Glimcher, L.H. A Novel Transcription Factor, T-Bet, Directs Th1 Lineage Commitment. Cell 2000, 100, 655–669. [Google Scholar] [CrossRef]
- Koch, M.A.; Tucker-Heard, G.; Perdue, N.R.; Killebrew, J.R.; Urdahl, K.B.; Campbell, D.J. The Transcription Factor T-Bet Controls Regulatory T Cell Homeostasis and Function during Type 1 Inflammation. Nat. Immunol. 2009, 10, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.L.; Szabo, S.J.; Glimcher, L.H. T-Bet Regulates IgG Class Switching and Pathogenic Production. Proc. Natl. Acad. Sci. USA 2002, 99, 5545. [Google Scholar] [CrossRef] [PubMed]
- Knox, J.J.; Myles, A.; Cancro, M.P. T-Bet+ Memory B Cells: Generation, Function, and Fate. Immunol. Rev. 2019, 288, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Ly, A.; Liao, Y.; Pietrzak, H.; Ioannidis, L.J.; Sidwell, T.; Gloury, R.; Doerflinger, M.; Triglia, T.; Qin, R.Z.; Groom, J.R.; et al. Transcription Factor T-Bet in B Cells Modulates Germinal Center Polarization and Antibody Affinity Maturation in Response to Malaria. Cell Rep. 2019, 29, 2257–2269.e6. [Google Scholar] [CrossRef] [PubMed]
- Braga, M.; Lara-Armi, F.F.; Neves, J.S.F.; Rocha-Loures, M.A.; Terron-Monich, M.d.S.; Bahls-Pinto, L.D.; de Lima Neto, Q.A.; Zacarias, J.M.V.; Sell, A.M.; Visentainer, J.E.L. Influence of IL10 (Rs1800896) Polymorphism and TNF-α, IL-10, IL-17A, and IL-17F Serum Levels in Ankylosing Spondylitis. Front. Immunol. 2021, 12, 653611. [Google Scholar] [CrossRef] [PubMed]
- Saraiva, M.; O’Garra, A. The Regulation of IL-10 Production by Immune Cells. Nat. Rev. Immunol. 2010, 10, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Blair, P.A.; Noreña, L.Y.; Flores-Borja, F.; Rawlings, D.J.; Isenberg, D.A.; Ehrenstein, M.R.; Mauri, C. CD19+CD24hiCD38hi B Cells Exhibit Regulatory Capacity in Healthy Individuals but Are Functionally Impaired in Systemic Lupus Erythematosus Patients. Immunity 2010, 32, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Zhang, L.; Ren, Y.; Zhang, K.; Yang, Y.; Fang, Y.; Yan, X.; Peng, D.; Gao, C.; Li, S. Defective Function of CD24+CD38+ Regulatory B Cells in Ankylosing Spondylitis. DNA Cell Biol. 2016, 35, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Cyster, J.G.; Allen, C.D.C. B Cell Responses: Cell Interaction Dynamics and Decisions. Cell 2019, 177, 524–540. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.; Luo, Z.; Yang, H. Peripheral B Cell Subsets in Autoimmune Diseases: Clinical Implications and Effects of B Cell-Targeted Therapies. J. Immunol. Res. 2020, 2020, 9518137. [Google Scholar] [CrossRef] [PubMed]
- Brand, J.-M.; Neustock, P.; Kruse, A.; Alvarez-Ossorio, L.; Schnabel, A.; Kirchner, H. Stimulation of Whole Blood Cultures in Patients with Ankylosing Spondylitis by a Mitogen Derived FromMycoplasma Arthritidis (MAS) and Other Mitogens. Rheumatol. Int. 1997, 16, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-H.; Chen, W.-S.; Lee, H.-T.; Tsai, C.-Y.; Chou, C.-T. Inverse Correlation of Programmed Death 1 (PD-1) Expression in T Cells to the Spinal Radiologic Changes in Taiwanese Patients with Ankylosing Spondylitis. Clin. Rheumatol. 2011, 30, 1181–1187. [Google Scholar] [CrossRef]
- Szántó, S.; Alesza, M.; Mihály, E.; Lakos, G.; Szabó, Z.; Vegvari, A.; Sipka, S.; Szekanecz, Z. Intracytoplasmic Cytokine Expression and T Cell Subset Distribution in the Peripheral Blood of Patients with Ankylosing Spondylitis. J. Rheumatol. 2008, 35, 2372–2375. [Google Scholar] [CrossRef]
- Long, S.; Ma, L.; Wang, D.; Shang, X. High Frequency of Circulating Follicular Helper T Cells Is Correlated with B Cell Subtypes in Patients with Ankylosing Spondylitis. Exp. Ther. Med. 2018, 15, 4578. [Google Scholar] [CrossRef] [PubMed]
- Bautista-Caro, M.B.; de Miguel, E.; Peiteado, D.; Plasencia-Rodríguez, C.; Villalba, A.; Monjo-Henry, I.; Puig-Kröger, A.; Sánchez-Mateos, P.; Martín-Mola, E.; Miranda-Carús, M.E. Increased Frequency of Circulating CD19 +CD24hiCD38hi B Cells with Regulatory Capacity in Patients with Ankylosing Spondylitis (AS) Naïve for Biological Agents. PLoS ONE 2017, 12, e0180726. [Google Scholar] [CrossRef]
- Lin, Q.; Gu, J.R.; Li, T.W.; Zhang, F.C.; Lin, Z.M.; Liao, Z.T.; Wei, Q.J.; Cao, S.Y.; Li, L. Value of the Peripheral Blood B-Cells Subsets in Patients with Ankylosing Spondylitis. Chin. Med. J. 2009, 122, 1784–1789. [Google Scholar] [CrossRef]
- Yang, M.; Lv, Q.; Wei, Q.; Jiang, Y.; Qi, J.; Xiao, M.; Fang, L.; Xie, Y.; Cao, S.; Lin, Z.; et al. TNF-α Inhibitor Therapy Can Improve the Immune Imbalance of CD4+ T Cells and Negative Regulatory Cells but Not CD8+ T Cells in Ankylosing Spondylitis. Arthritis Res. Ther. 2020, 22, 149. [Google Scholar] [CrossRef] [PubMed]
- Bautista-Caro, M.B.; Arroyo-Villa, I.; Castillo-Gallego, C.; de Miguel, E.; Peiteado, D.; Plasencia-Rodríguez, C.; Villalba, A.; Sanchez-Mateos, P.; Puig-Kröger, A.; Martín-Mola, E.; et al. Decreased Frequencies of Circulating Follicular Helper T Cell Counterparts and Plasmablasts in Ankylosing Spondylitis Patients Naïve for TNF Blockers. PLoS ONE 2014, 9, e107086. [Google Scholar] [CrossRef][Green Version]
- Niu, X.-Y.; Zhang, H.-Y.; Liu, Y.-J.; Zhao, D.; Shan, Y.-X.; Jiang, Y.-F. Peripheral B-Cell Activation and Exhaustion Markers in Patients with Ankylosing Spondylitis. Life Sci. 2013, 93, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Sanz, I.; Wei, C.; Jenks, S.A.; Cashman, K.S.; Tipton, C.; Woodruff, M.C.; Hom, J.; Lee, F.E.-H. Challenges and Opportunities for Consistent Classification of Human B Cell and Plasma Cell Populations. Front. Immunol. 2019, 10, 2458. [Google Scholar] [CrossRef]
- Sindhava, V.J.; Bondada, S. Multiple Regulatory Mechanisms Control B-1 B Cell Activation. Front. Immunol. 2012, 3, 372. [Google Scholar] [CrossRef]
- Cantaert, T.; Doorenspleet, M.E.; Francosalinas, G.; Paramarta, J.E.; Klarenbeek, P.L.; Tiersma, Y.; van der Loos, C.M.; de Vries, N.; Tak, P.P.; Baeten, D.L. Increased Numbers of CD5+ B Lymphocytes with a Regulatory Phenotype in Spondylarthritis. Arthritis Rheum. 2012, 64, 1859–1868. [Google Scholar] [CrossRef] [PubMed]
- Ge, L.; Wang, J.; Zhu, B.Q.; Zhang, Z.S. Effect of Abnormal Activated B Cells in Patients with Ankylosing Spondylitis and Its Molecular Mechanism. Eur. Rev. Med Pharmacol. Sci. 2018, 22, 2527–2533. [Google Scholar] [CrossRef]
- Madej, M.; Nowak, B.; Świerkot, J.; Sokolik, R.; Chlebicki, A.; Korman, L.; Woytala, P.; Lubiński, Ł.; Wiland, P. Cytokine Profiles in Axial Spondyloarthritis. Reumatologia 2015, 53, 9. [Google Scholar] [CrossRef] [PubMed]
- Funaro, A.; Morra, M.; Calosso, L.; Zini, M.G.; Ausiello, C.M.; Malavasi, F. Role of the Human CD38 Molecule in B Cell Activation and Proliferation. Tissue Antigens 1997, 49, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Suvas, S.; Singh, V.; Sahdev, S.; Vohra, H.; Agrewala, J.N. Distinct Role of CD80 and CD86 in the Regulation of the Activation of B Cell and B Cell Lymphoma. J. Biol. Chem. 2002, 277, 7766–7775. [Google Scholar] [CrossRef] [PubMed]
- Hahne, M.; Renno, T.; Schroeter, M.; Irmler, M.; French, L.; Bornand, T.; MacDonald, H.R.; Tschopp, J. Activated B Cells Express Functional Fas Ligand. Eur. J. Immunol. 1996, 26, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Koncz, G.; Hueber, A.O. The Fas/CD95 Receptor Regulates the Death of Autoreactive B Cells and the Selection of Antigen-Specific B Cells. Front. Immunol. 2012, 3, 207. [Google Scholar] [CrossRef] [PubMed]
- Fink, K. Origin and Function of Circulating Plasmablasts during Acute Viral Infections. Front. Immunol. 2012, 3, 78. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Yang, T.; Pan, F.; Xia, G.; Hu, Y.; Liu, L.; Fan, D.; Duan, Z.; Ding, N.; Xu, S.; et al. Increased Frequency of Circulating Follicular Helper T Cells in Patients with Ankylosing Spondylitis. Mod. Rheumatol. 2015, 25, 110–115. [Google Scholar] [CrossRef]
- Thorarinsdottir, K.; Camponeschi, A.; Gjertsson, I.; Mårtensson, I.-L. CD21 −/Low B Cells: A Snapshot of a Unique B Cell Subset in Health and Disease. Scand. J. Immunol. 2015, 82, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Wehr, C.; Eibel, H.; Masilamani, M.; Illges, H.; Schlesier, M.; Peter, H.-H.; Warnatz, K. A New CD21low B Cell Population in the Peripheral Blood of Patients with SLE. Clin. Immunol. 2004, 113, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, D.; Terrier, B.; Bannock, J.; Vazquez, T.; Massad, C.; Kang, I.; Joly, F.; Rosenzwajg, M.; Sene, D.; Benech, P.; et al. Expansion of Autoreactive Unresponsive CD21-/Low B Cells in Sjögren’s Syndrome-Associated Lymphoproliferation. Arthritis Rheum. 2013, 65, 1085–1096. [Google Scholar] [CrossRef] [PubMed]
- Isnardi, I.; Ng, Y.-S.; Menard, L.; Meyers, G.; Saadoun, D.; Srdanovic, I.; Samuels, J.; Berman, J.; Buckner, J.H.; Cunningham-Rundles, C.; et al. Complement Receptor 2/CD21- Human Naive B Cells Contain Mostly Autoreactive Unresponsive Clones. Blood 2010, 115, 5026–5036. [Google Scholar] [CrossRef]
- Thorarinsdottir, K.; Camponeschi, A.; Cavallini, N.; Grimsholm, O.; Jacobsson, L.; Gjertsson, I.; Mårtensson, I.L. CD21–/Low B Cells in Human Blood Are Memory Cells. Clin. Exp. Immunol. 2016, 185, 252–262. [Google Scholar] [CrossRef]
- Wang, S.; Wang, J.; Kumar, V.; Karnell, J.L.; Naiman, B.; Gross, P.S.; Rahman, S.; Zerrouki, K.; Hanna, R.; Morehouse, C.; et al. IL-21 Drives Expansion and Plasma Cell Differentiation of Autoreactive CD11chiT-Bet+ B Cells in SLE. Nat. Commun. 2018, 9, 1758. [Google Scholar] [CrossRef]
- Stone, S.L.; Peel, J.; Scharer, C.D.; Risley, C.A.; Chisolm, D.A.; Schultz, M.D.; Yu, B.; Ballesteros-Tato, A.; Wojciechowski, W.; Mousseau, B.; et al. T-Bet Transcription Factor Promotes Antibody Secreting Cell Differentiation by Limiting the Inflammatory Effects of IFNγ on B Cells HHS Public Access. Immunity 2019, 50, 1172–1187. [Google Scholar] [CrossRef] [PubMed]
- Golinski, M.-L.; Demeules, M.; Derambure, C.; Riou, G.; Maho-Vaillant, M.; Boyer, O.; Joly, P.; Calbo, S. CD11c+ B Cells Are Mainly Memory Cells, Precursors of Antibody Secreting Cells in Healthy Donors. Front. Immunol. 2020, 11, 32. [Google Scholar] [CrossRef]
- Vasey, F.B.; Kinsella, T.D. Increased Frequency of Leukocyte-Reactive Antinuclear Antibody in Patients with Ankylosing Spondylitis. J. Rheumatol. 1977, 4, 158–164. [Google Scholar] [PubMed]
- Rosenberg, J.N.; Johnson, G.D.; Holborow, E.J. Antinuclear Antibodies in Ankylosing Spondylitis, Psoriatic Arthritis, and Psoriasis. Ann. Rheum. Dis. 1979, 38, 526–528. [Google Scholar] [CrossRef] [PubMed]
- Locht, H.; Skogh, T.; Kihlström, E. Anti-Lactoferrin Antibodies and Other Types of Anti-Neutrophil Cytoplasmic Antibodies (ANCA) in Reactive Arthritis and Ankylosing Spondylitis. Clin. Exp. Immunol. 1999, 117, 568–573. [Google Scholar] [CrossRef] [PubMed]
- De Vries, M.; van der Horst-Bruinsma, I.; van Hoogstraten, I.; van Bodegraven, A.; von Blomberg, M.; Ratnawati, H.; Dijkmans, B. PANCA, ASCA, and OmpC Antibodies in Patients with Ankylosing Spondylitis without Inflammatory Bowel Disease. J. Rheumatol. 2010, 37, 2340–2344. [Google Scholar] [CrossRef]
- Kwon, O.C.; Lee, E.J.; Lee, J.Y.; Youn, J.; Kim, T.H.; Hong, S.; Lee, C.K.; Yoo, B.; Robinson, W.H.; Kim, Y.G. Prefoldin 5 and Anti-Prefoldin 5 Antibodies as Biomarkers for Uveitis in Ankylosing Spondylitis. Front. Immunol. 2019, 10, 384. [Google Scholar] [CrossRef] [PubMed]
- Curry, R.; Thoen, J.; Shelborne, C.; Gaudernack, G.; Messner, R. Antibodies to and Elevations of Beta 2 Microglobulin in the Serum of Ankylosing Spondylitis Patients. Arthritis Rheum. 1982, 25, 375–380. [Google Scholar] [CrossRef]
- Baerlecken, N.T.; Nothdorft, S.; Stummvoll, G.H.; Sieper, J.; Rudwaleit, M.; Reuter, S.; Matthias, T.; Schmidt, R.E.; Witte, T. Autoantibodies against CD74 in Spondyloarthritis. Ann. Rheum. Dis. 2014, 73, 1211–1214. [Google Scholar] [CrossRef] [PubMed]
- Witte, T.; Köhler, M.; Georgi, J.; Schweikhard, E.; Matthias, T.; Baerlecken, N.; Hermann, K.G.; Sieper, J.; Rudwaleit, M.; Poddubnyy, D. IgA Antibodies against CD74 Are Associated with Structural Damage in the Axial Skeleton in Patients with Axial Spondyloarthritis. Clin. Exp. Rheumatol. 2020, 38, 1127–1131. [Google Scholar] [PubMed]
- Ziade, N.R.; Mallak, I.; Merheb, G.; Ghorra, P.; Baerlecken, N.; Witte, T.; Baraliakos, X. Added Value of Anti-CD74 Autoantibodies in Axial SpondyloArthritis in a Population With Low HLA-B27 Prevalence. Front. Immunol. 2019, 10, 574. [Google Scholar] [CrossRef] [PubMed]
- De Winter, J.J.; van de Sande, M.G.; Baerlecken, N.; Berg, I.; Ramonda, R.; van der Heijde, D.; van Gaalen, F.A.; Witte, T.; Baeten, D.L. Anti-CD74 Antibodies Have No Diagnostic Value in Early Axial Spondyloarthritis: Data from the Spondyloarthritis Caught Early (SPACE) Cohort. Arthritis Res. Ther. 2018, 20, 38. [Google Scholar] [CrossRef] [PubMed]
- Baraliakos, X.; Baerlecken, N.; Witte, T.; Heldmann, F.; Braun, J. High Prevalence of Anti-CD74 Antibodies Specific for the HLA Class II-Associated Invariant Chain Peptide (CLIP) in Patients with Axial Spondyloarthritis. Ann. Rheum. Dis. 2014, 73, 1079–1082. [Google Scholar] [CrossRef] [PubMed]
- Riechers, E.; Baerlecken, N.; Baraliakos, X.; Achilles-Mehr Bakhsh, K.; Aries, P.; Bannert, B.; Becker, K.; Brandt-Jürgens, J.; Braun, J.; Ehrenstein, B.; et al. Sensitivity and Specificity of Autoantibodies Against CD74 in Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019, 71, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.-J.; Li, M.-T.; Li, X.; Peng, L.-Y.; Zhang, S.-Z.; Leng, X.-M.; Su, J.-M.; Zeng, X.-F. CD74 Auto-Antibodies Display Little Clinical Value in Chinese Han Population with Axial Spondyloarthritis. Medicine 2020, 99, e23433. [Google Scholar] [CrossRef]
- Do, L.; Granåsen, G.; Hellman, U.; Lejon, K.; Geijer, M.; Baraliakos, X.; Witte, T.; Forsblad-d’Elia, H. Anti-CD74 IgA Autoantibodies in Radiographic Axial Spondyloarthritis: A Longitudinal Swedish Study. Rheumatology 2021, 60, 4085. [Google Scholar] [CrossRef] [PubMed]
- Mäki-Ikola, O.; Nissilä, M.; Lehtinen, K.; Leirisalo-Repo, M.; Granfors, K. IgAl and IgA2 Subclass Antibodies against Klebsiella Pneumoniae in the Sera of Patients with Peripheral and Axial Types of Ankylosing Spondylitis. Ann. Rheum. Dis. 1995, 54, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, I.E.A.; Demetter, P.; Peeters, M.; de Vos, M.; Mielants, H.; Veys, E.M.; de Keyser, F. Anti-Saccharomyces Cerevisiae IgA Antibodies Are Raised in Ankylosing Spondylitis and Undifferentiated Spondyloarthropathy. Ann. Rheum. Dis. 2003, 62, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Wallis, D.; Asaduzzaman, A.; Weisman, M.; Haroon, N.; Anton, A.; McGovern, D.; Targan, S.; Inman, R. Elevated Serum Anti-Flagellin Antibodies Implicate Subclinical Bowel Inflammation in Ankylosing Spondylitis: An Observational Study. Arthritis Res. Ther. 2013, 15, R166. [Google Scholar] [CrossRef] [PubMed]
- Puccetti, A.; Dolcino, M.; Tinazzi, E.; Moretta, F.; D’Angelo, S.; Olivieri, I.; Lunardi, C. Antibodies Directed against a Peptide Epitope of a Klebsiella Pneumoniae-Derived Protein Are Present in Ankylosing Spondylitis. PLoS ONE 2017, 12, e0171073. [Google Scholar] [CrossRef] [PubMed]
- Ulusoy, H.; Akgol, G.; Gulkesen, A.; Kaya, A.; Kal, G.A.; Kaman, D.; Tuncer, T. Serum Heat-Shock Protein-65 Antibody Levels Are Elevated but Not Associated with Disease Activity in Patients with Rheumatoid Arthritis and Ankylosing Spondylitis. Open Access Rheumatol. Res. Rev. 2018, 10, 55–60. [Google Scholar] [CrossRef]
- Trull, A.K.; Ebringer, R.; Panayi, G.S.; Colthorpe, D.; James, D.C.O.; Ebringer, A. Iga Antibodies to Klebsiella Pneumoniae in Ankylosing Spondylitis. Scand. J. Rheumatol. 2009, 12, 249–253. [Google Scholar] [CrossRef]
- Blankenberg-Sprenkels, S.H.; Fielder, M.; Feltkamp, T.E.; Tiwana, H.; Wilson, C.; Ebringer, A. Antibodies to Klebsiella Pneumoniae in Dutch Patients with Ankylosing Spondylitis and Acute Anterior Uveitis and to Proteus Mirabilis in Rheumatoid Arthritis. J. Rheumatol. 1998, 25, 743–747. [Google Scholar]
- Luchetti, M.M.; Ciccia, F.; Avellini, C.; Benfaremo, D.; Guggino, G.; Farinelli, A.; Ciferri, M.; Rossini, M.; Svegliati, S.; Spadoni, T.; et al. Sclerostin and Antisclerostin Antibody Serum Levels Predict the Presence of Axial Spondyloarthritis in Patients with Inflammatory Bowel Disease. J. Rheumatol. 2018, 45, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Tsui, F.W.L.; Tsui, H.W.; Heras, F.L.; Pritzker, K.P.H.; Inman, R.D. Serum Levels of Novel Noggin and Sclerostin-Immune Complexes Are Elevated in Ankylosing Spondylitis. Ann. Rheum. Dis. 2014, 73, 1873–1879. [Google Scholar] [CrossRef]
- Wright, C.; Sibani, S.; Trudgian, D.; Fischer, R.; Kessler, B.; LaBaer, J.; Bowness, P. Detection of Multiple Autoantibodies in Patients with Ankylosing Spondylitis Using Nucleic Acid Programmable Protein Arrays. Mol. Cell. Proteom. 2012, 11, M9.00384. [Google Scholar] [CrossRef]
- Hu, Q.; Sun, Y.; Li, Y.; Shi, H.; Teng, J.; Liu, H.; Cheng, X.; Ye, J.; Su, Y.; Yin, Y.; et al. Anti-SIRT1 Autoantibody Is Elevated in Ankylosing Spondylitis: A Potential Disease Biomarker. BMC Immunol. 2018, 19, 38. [Google Scholar] [CrossRef]
- Kim, Y.G.; Sohn, D.H.; Zhao, X.; Sokolove, J.; Lindstrom, T.M.; Yoo, B.; Lee, C.K.; Reveille, J.D.; Taurog, J.D.; Robinson, W.H. Role of Protein Phosphatase Magnesium-Dependent 1a and Anti-Protein Phosphatase Magnesium-Dependent 1A Autoantibodies in Ankylosing Spondylitis. Arthritis Rheumatol. 2014, 66, 2793–2803. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-S.; Lee, E.-J.; Lee, J.-H.; Hong, S.-C.; Lee, C.-K.; Yoo, B.; Oh, J.-S.; Lee, S.-H.; Kim, T.-J.; Lee, S.-H.; et al. Autoantibodies against Protein Phosphatase Magnesium-Dependent 1A as a Biomarker for Predicting Radiographic Progression in Ankylosing Spondylitis Treated with Anti-Tumor Necrosis Factor Agents. J. Clin. Med. 2020, 9, 3968. [Google Scholar] [CrossRef]
- Hauser, B.; Zhao, S.; Visconti, M.R.; Riches, P.L.; Fraser, W.D.; Piec, I.; Goodson, N.J.; Ralston, S.H. Autoantibodies to Osteoprotegerin Are Associated with Low Hip Bone Mineral Density and History of Fractures in Axial Spondyloarthritis: A Cross-Sectional Observational Study. Calcif. Tissue Int. 2017, 101, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Guglielmi, V.; Vattemi, G.; Cecconi, D.; Fracasso, G.; Marini, M.; Tomelleri, G. Acute Sarcomeric M-Line Disease Associated with ATP Synthase Subunit a Autoantibodies in Ankylosing Spondylitis. J. Neuropathol. Exp. Neurol. 2018, 77, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Tani, Y.; Sato, H.; Tanaka, N.; Mori, K.; Doida, Y.; Hukuda, S. Serum IgA1 and IgA2 Subclass Antibodies against Collagens in Patients with Ankylosing Spondylitis. Scand. J. Rheumatol. 1997, 26, 380–382. [Google Scholar] [CrossRef]
- Singh Sangha, M.; Wright, M.L.; Ciurtin, C. Strongly Positive Anti-CCP Antibodies in Patients with Sacroiliitis or Reactive Arthritis Post-E. Coli Infection: A Mini Case-Series Based Review. Int. J. Rheum. Dis. 2018, 21, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Lamacchia, C.; Courvoisier, D.S.; Jarlborg, M.; Bas, S.; Roux-Lombard, P.; Möller, B.; Ciurea, A.; Finckh, A.; Bentow, C.; Martinez-Prat, L.; et al. Predictive Value of Anti-CarP and Anti-PAD3 Antibodies Alone or in Combination with RF and ACPA for the Severity of Rheumatoid Arthritis. Rheumatology 2021, 60, 4598–4608. [Google Scholar] [CrossRef]
- Sidiras, P.; Spruyt, D.; Gangji, V.; Imbault, V.; Sokolova, T.; Durez, P.; Communi, D.; Rasschaert, J.; Badot, V. Antibodies against Carbamylated Proteins: Prevalence and Associated Disease Characteristics in Belgian Patients with Rheumatoid Arthritis or Other Rheumatic Diseases. Scand. J. Rheumatol. 2021, 50, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Quaden, D.; Vandormael, P.; Ruytinx, P.; Geusens, P.; Corten, K.; Vanhoof, J.; Liesenborgs, J.; van Reeth, F.; Agten, A.; Vandenabeele, F.; et al. Antibodies Against Three Novel Peptides in Early Axial Spondyloarthritis Patients From Two Independent Cohorts. Arthritis Rheumatol. 2020, 72, 2094–2105. [Google Scholar] [CrossRef] [PubMed]
- Gonnet-Gracia, C.; Barnetche, T.; Richez, C.; Blanco, P.; Dehais, J.; Schaeverbecke, T. Anti-Nuclear Antibodies, Acti-DNA and C4 Complement Evolution in Rheumatiod Arthritis and Ankylosing Spondylitis Treated with TNF-α Blockers. Clin. Exp. Rheumatol. 2008, 26, 401–407. [Google Scholar] [PubMed]
- Arends, S.; Lebbink, H.R.; Spoorenberg, A.; Bungener, L.B.; Roozendaal, C.; van der Veer, E.; Houtman, P.M.; Griep, E.N.; Limburg, P.C.; Kallenberg, C.G.M.; et al. The Formation of Autoantibodies and Antibodies to TNF-α Blocking Agents in Relation to Clinical Response in Patients with Ankylosing Spondylitis. Clin. Exp. Rheumatol. 2010, 28, 661–668. [Google Scholar]
- García-De LaTorre, I.; García-Valladares, I. Antinuclear Antibody (ANA) Testing in Patients Treated with Biological DMARDs: Is It Useful? Curr. Rheumatol. Rep. 2015, 17, 23. [Google Scholar] [CrossRef]
- Abe, A.; Takashi-Niki, K.; Takekoshi, Y.; Shimizu, T.; Kitaura, H.; Maita, H.; Iguchi-Ariga, S.M.; Ariga, H. Prefoldin Plays a Role as a Clearance Factor in Preventing Proteasome Inhibitor-Induced Protein Aggregation. J. Biol. Chem. 2013, 288, 27764–27776. [Google Scholar] [CrossRef] [PubMed]
- Townsend, A.; Öhlén, C.; Bastin, J.; Ljunggren, H.-G.; Foster, L.; Kärre, K. Association of Class I Major Histocompatibility Heavy and Light Chains Induced by Viral Peptides. Nature 1989, 340, 443–448. [Google Scholar] [CrossRef]
- Lotteau, V.; Teyton, L.; Peleraux, A.; Nilsson, T.; Karlsson, L.; Schmid, S.L.; Quaranta, V.; Peterson, P.A. Intracellular Transport of Class II MHC Molecules Directed by Invariant Chain. Nature 1990, 348, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Farr, L.; Ghosh, S.; Moonah, S. Role of MIF Cytokine/CD74 Receptor Pathway in Protecting Against Injury and Promoting Repair. Front. Immunol. 2020, 11, 1273. [Google Scholar] [CrossRef]
- Calandra, T.; Roger, T. Macrophage Migration Inhibitory Factor: A Regulator of Innate Immunity. Nat. Rev. Immunol. 2003, 3, 791–800. [Google Scholar] [CrossRef]
- Gu, R.; Santos, L.L.; Ngo, D.; Fan, H.P.; Singh, P.P.; Fingerle-Rowson, G.; Bucala, R.; Xu, J.; Quinn, J.M.W.; Morand, E.F. Macrophage Migration Inhibitory Factor Is Essential for Osteoclastogenic Mechanisms in Vitro and in Vivo Mouse Model of Arthritis. Cytokine 2015, 72, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Jacquin, C.; Koczon-Jaremko, B.; Aguila, H.L.; Leng, L.; Bucala, R.; Kuchel, G.A.; Lee, S.K. Macrophage Migration Inhibitory Factor Inhibits Osteoclastogenesis. Bone 2009, 45, 640–649. [Google Scholar] [CrossRef]
- Onodera, S.; Sasaki, S.; Ohshima, S.; Amizuka, N.; Li, M.; Udagawa, N.; Irie, K.; Nishihira, J.; Koyama, Y.; Shiraishi, A.; et al. Transgenic Mice Overexpressing Macrophage Migration Inhibitory Factor (MIF) Exhibit High-Turnover Osteoporosis. J. Bone Miner. Res. 2006, 21, 876–885. [Google Scholar] [CrossRef]
- Ranganathan, V.; Ciccia, F.; Zeng, F.; Sari, I.; Guggiino, G.; Muralitharan, J.; Gracey, E.; Haroon, N. Macrophage Migration Inhibitory Factor Induces Inflammation and Predicts Spinal Progression in Ankylosing Spondylitis. Arthritis Rheumatol. 2017, 69, 1796–1806. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; Zeng, F.; Nakamura, S.; Reid, K.T.; Gracey, E.; Lim, M.; Leng, L.; Jo, S.; Park, Y.-S.; Kusuda, M.; et al. Macrophage Migration Inhibitory Factor Drives Pathology in a Mouse Model of Spondyloarthritis and Is Associated with Human Disease. Sci. Transl. Med. 2021, 13, eabg1210. [Google Scholar] [CrossRef]
- Matza, D.; Wolstein, O.; Dikstein, R.; Shachar, I. Invariant Chain Induces B Cell Maturation by Activating a TAFII105-NF-ΚB-Dependent Transcription Program. J. Biol. Chem. 2001, 276, 27203–27206. [Google Scholar] [CrossRef] [PubMed]
- Starlets, D.; Gore, Y.; Binsky, I.; Haran, M.; Harpaz, N.; Shvidel, L.; Becker-Herman, S.; Berrebi, A.; Shachar, I. Cell-Surface CD74 Initiates a Signaling Cascade Leading to Cell Proliferation and Survival. Blood 2006, 107, 4807–4816. [Google Scholar] [CrossRef] [PubMed]
- Leng, L.; Metz, C.N.; Fang, Y.; Xu, J.; Donnelly, S.; Baugh, J.; Delohery, T.; Chen, Y.; Mitchell, R.A.; Bucala, R. MIF Signal Transduction Initiated by Binding to CD74. J. Exp. Med. 2003, 197, 1467–1476. [Google Scholar] [CrossRef] [PubMed]
- Kozaci, L.D.; Sari, I.; Alacacioglu, A.; Akar, S.; Akkoc, N. Evaluation of Inflammation and Oxidative Stress in Ankylosing Spondylitis: A Role for Macrophage Migration Inhibitory Factor. Mod. Rheumatol. 2014, 20, 34–39. [Google Scholar] [CrossRef]
- Abdelaziz, M.M.; Gamal, R.M.; Ismail, N.M.; Lafy, R.A.; Hetta, H.F. Diagnostic Value of Anti-CD74 Antibodies in Early and Late Axial Spondyloarthritis and Its Relationship to Disease Activity. Rheumatology 2021, 60, 263–268. [Google Scholar] [CrossRef]
- Van Kempen, T.S.; Leijten, E.F.A.; Lindenbergh, M.F.S.; Nordkamp, M.O.; Driessen, C.; Lebbink, R.J.; Baerlecken, N.; Witte, T.; Radstake, T.R.D.J.; Boes, M. Impaired Proteolysis by SPPL2a Causes CD74 Fragment Accumulation That Can Be Recognized by Anti-CD74 Autoantibodies in Human Ankylosing Spondylitis. Eur. J. Immunol. 2020, 50, 1209–1219. [Google Scholar] [CrossRef]
- Real, A.; Gilbert, N.; Hauser, B.; Kennedy, N.; Shand, A.; Gillet, H.; Gillett, P.; Goddard, C.; Cebolla, Á.; Sousa, C.; et al. Characterisation of Osteoprotegerin Autoantibodies in Coeliac Disease. Calcif. Tissue Int. 2015, 97, 125–133. [Google Scholar] [CrossRef]
- Boyce, B.F.; Xing, L. Biology of RANK, RANKL, and Osteoprotegerin. Arthritis Res. Ther. 2007, 9, S1. [Google Scholar] [CrossRef] [PubMed]
- Takayanagi, H. Osteoimmunology: Shared Mechanisms and Crosstalk between the Immune and Bone Systems. Nat. Rev. Immunol. 2007, 7, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Meednu, N.; Zhang, H.; Owen, T.; Sun, W.; Wang, V.; Cistrone, C.; Rangel-Moreno, J.; Xing, L.; Anolik, J.H. Production of RANKL by Memory B Cells: A Link Between B Cells and Bone Erosion in Rheumatoid Arthritis. Arthritis Rheumatol. 2016, 68, 805–816. [Google Scholar] [CrossRef]
- Ghozlani, I.; Ghazi, M.; Nouijai, A.; Mounach, A.; Rezqi, A.; Achemlal, L.; Bezza, A.; el Maghraoui, A. Prevalence and Risk Factors of Osteoporosis and Vertebral Fractures in Patients with Ankylosing Spondylitis. Bone 2009, 44, 772–776. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, F.; Liu, H.; Li, J.; Che, H.; Shen, J.; Luo, E. SIRT1, a Promising Regulator of Bone Homeostasis. Life Sci. 2021, 269, 119041. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Kfir, E.; Artsi, H.; Levin, A.; Abramowitz, E.; Bajayo, A.; Gurt, I.; Zhong, L.; D’Urso, A.; Toiber, D.; Mostoslavsky, R.; et al. Sirt1 Is a Regulator of Bone Mass and a Repressor of Sost Encoding for Sclerostin, a Bone Formation Inhibitor. Endocrinology 2011, 152, 4514–4524. [Google Scholar] [CrossRef]
- Delgado-Calle, J.; Sato, A.Y.; Bellido, T. Role and Mechanism of Action of Sclerostin in Bone. Bone 2017, 96, 29. [Google Scholar] [CrossRef]
- Krause, C.; Guzman, A.; Knaus, P. Noggin. Int. J. Biochem. Cell Biol. 2011, 43, 478–481. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Xu, S.; Chen, M.; Yuan, Y.; Zhang, X.; Ma, Y.; Wu, M.; Han, R.; Hu, X.; Liu, R.; et al. Serum Sclerostin and Bone Morphogenetic Protein-2 Levels in Patients with Ankylosing Spondylitis: A Meta-Analysis. Calcif. Tissue Int. 2019, 105, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Appel, H.; Ruiz-Heiland, G.; Listing, J.; Zwerina, J.; Herrmann, M.; Mueller, R.; Haibel, H.; Baraliakos, X.; Hempfing, A.; Rudwaleit, M.; et al. Altered Skeletal Expression of Sclerostin and Its Link to Radiographic Progression in Ankylosing Spondylitis. Arthritis Rheumatol. 2009, 60, 3257–3262. [Google Scholar] [CrossRef] [PubMed]
- Lories, R.J.U.; Derese, I.; Luyten, F.P. Modulation of Bone Morphogenetic Protein Signaling Inhibits the Onset and Progression of Ankylosing Enthesitis. J. Clin. Investig. 2005, 115, 1571–1579. [Google Scholar] [CrossRef] [PubMed]
- Cain, C.J.; Rueda, R.; McLelland, B.; Collette, N.M.; Loots, G.G.; Manilay, J.O. Absence of Sclerostin Adversely Affects B-Cell Survival. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2012, 27, 1451–1461. [Google Scholar] [CrossRef]
- Donham, C.; Manilay, J.O. The Effects of Sclerostin on the Immune System. Curr. Osteoporos. Rep. 2020, 18, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, O.; Cantero-Hinojosa, J.; Paule-Sastre, P.; Gómez-Magán, J.C.; Salvatierra-Ríos, D. Intestinal Permeability in Patients with Ankylosing Spondylitis and Their Healthy Relatives. Br. J. Rheumatol. 1994, 33, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Van Praet, L.; van den Bosch, F.E.; Jacques, P.; Carron, P.; Jans, L.; Colman, R.; Glorieus, E.; Peeters, H.; Mielants, H.; de Vos, M.; et al. Microscopic Gut Inflammation in Axial Spondyloarthritis: A Multiparametric Predictive Model. Ann. Rheum. Dis. 2013, 72, 414–417. [Google Scholar] [CrossRef]
- Mielants, H.; Veys, E.M.; Cuvelier, C.; de Vos, M. Ileocolonoscopic Findings in Seronegative Spondylarthropathies. Br. J. Rheumatol. 1988, 27 (Suppl. S2), 95–105. [Google Scholar] [CrossRef] [PubMed]
- Hocini, H.; Iscaki, S.; Benlahrache, C.; Vitalis, L.; Chevalier, X.; Larget-Piet, B.; Bouvet, J.P. Increased Levels of Serum IgA as IgA1 Monomers in Ankylosing Spondylitis. Ann. Rheum. Dis. 1992, 51, 790–792. [Google Scholar] [CrossRef] [PubMed]
- Franssen, M.J.A.M.; van de Putte, L.B.A.; Gribnau, F.W.J. IgA Serum Levels and Disease Activity in Ankylosing Spondylitis: A Prospective Study. Ann. Rheum. Dis. 1985, 44, 766–771. [Google Scholar] [CrossRef]
- Yang, L.; Wang, L.; Wang, X.; Xian, C.J.; Lu, H. A Possible Role of Intestinal Microbiota in the Pathogenesis of Ankylosing Spondylitis. Int. J. Mol. Sci. 2016, 17, 2126. [Google Scholar] [CrossRef] [PubMed]
- Shovman, O.; Sherer, Y.; Gilbourd, B.; Gerli, R.; Bocci, E.B.; Monache, F.D.; Luccioli, F.; Shoenfeld, Y. Low Levels of Heat Shock Proteins-60 and -65 Autoantibodies in Sjögren’s Syndrome. Isr. Med. Assoc. J. IMAJ 2005, 7, 778–780. [Google Scholar]
- Pruijn, G.J.M. Citrullination and Carbamylation in the Pathophysiology of Rheumatoid Arthritis. Front. Immunol. 2015, 6, 192. [Google Scholar] [CrossRef]
- Kim, J.O.; Lee, J.S.; Choi, J.Y.; Lee, K.H.; Kim, Y.B.; Yoo, D.H.; Kim, T.H. The Relationship between Peripheral Arthritis and Anti-Cyclic Citrullinated Peptide Antibodies in Ankylosing Spondylitis. Jt. Bone Spine 2013, 80, 399–401. [Google Scholar] [CrossRef] [PubMed]
- Tsukazaki, H.; Kaito, T. The Role of the IL-23/IL-17 Pathway in the Pathogenesis of Spondyloarthritis. Int. J. Mol. Sci. 2020, 21, 6401. [Google Scholar] [CrossRef]
- Chen, W.S.; Chang, Y.S.; Lin, K.C.; Lai, C.C.; Wang, S.H.; Hsiao, K.H.; Lee, H.T.; Chen, M.H.; Tsai, C.Y.; Chou, C.T. Association of Serum Interleukin-17 and Interleukin-23 Levels with Disease Activity in Chinese Patients with Ankylosing Spondylitis. J. Chin. Med. Assoc. 2012, 75, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Mei, Y.; Pan, F.; Gao, J.; Ge, R.; Duan, Z.; Zeng, Z.; Liao, F.; Xia, G.; Wang, S.; Xu, S.; et al. Increased Serum IL-17 and IL-23 in the Patient with Ankylosing Spondylitis. Clin. Rheumatol. 2010, 30, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lin, Z.; Wei, Q.; Jiang, Y.; Gu, J. Expression of IL-23 and IL-17 and Effect of IL-23 on IL-17 Production in Ankylosing Spondylitis. Rheumatol. Int. 2009, 29, 1343–1347. [Google Scholar] [CrossRef] [PubMed]
- Baeten, D.; Østergaard, M.; Wei, J.C.-C.; Sieper, J.; Järvinen, P.; Tam, L.-S.; Salvarani, C.; Kim, T.-H.; Solinger, A.; Datsenko, Y.; et al. Risankizumab, an IL-23 Inhibitor, for Ankylosing Spondylitis: Results of a Randomised, Double-Blind, Placebo-Controlled, Proof-of-Concept, Dose-Finding Phase 2 Study. Ann. Rheum. Dis. 2018, 77, 1295. [Google Scholar] [CrossRef] [PubMed]
- Deodhar, A.; Gensler, L.S.; Sieper, J.; Clark, M.; Calderon, C.; Wang, Y.; Zhou, Y.; Leu, J.H.; Campbell, K.; Sweet, K.; et al. Three Multicenter, Randomized, Double-Blind, Placebo-Controlled Studies Evaluating the Efficacy and Safety of Ustekinumab in Axial Spondyloarthritis. Arthritis Rheumatol. 2019, 71, 258–270. [Google Scholar] [CrossRef]
- Wang, R.; Maksymowych, W.P. Targeting the Interleukin-23/Interleukin-17 Inflammatory Pathway: Successes and Failures in the Treatment of Axial Spondyloarthritis. Front. Immunol. 2021, 12, 3472. [Google Scholar] [CrossRef]
- Baeten, D.L.; Adamopoulos, I.E. IL-23 Inhibition in Ankylosing Spondylitis: Where Did It Go Wrong? Front. Immunol. 2021, 11, 3825. [Google Scholar] [CrossRef] [PubMed]
- Gaffen, S.L.; Jain, R.; Garg, A.V.; Cua, D.J. The IL-23-IL-17 Immune Axis: From Mechanisms to Therapeutic Testing. Nat. Rev. Immunol. 2014, 14, 585–600. [Google Scholar] [CrossRef]
- Cuthbert, R.J.; Watad, A.; Fragkakis, E.M.; Dunsmuir, R.; Loughenbury, P.; Khan, A.; Millner, P.A.; Davison, A.; Marzo-Ortega, H.; Newton, D.; et al. Evidence That Tissue Resident Human Enthesis ΓδT-Cells Can Produce IL-17A Independently of IL-23R Transcript Expression. Ann. Rheum. Dis. 2019, 78, 1559–1565. [Google Scholar] [CrossRef]
- Sherlock, J.P.; Joyce-Shaikh, B.; Turner, S.P.; Chao, C.-C.; Sathe, M.; Grein, J.; Gorman, D.M.; Bowman, E.P.; McClanahan, T.K.; Yearley, J.H.; et al. IL-23 Induces Spondyloarthropathy by Acting on ROR-Γt + CD3 + CD4 − CD8 − Entheseal Resident T Cells. Nat. Med. 2012, 18, 1069–1076. [Google Scholar] [CrossRef]
- Gracey, E.; Qaiyum, Z.; Almaghlouth, I.; Lawson, D.; Karki, S.; Avvaru, N.; Zhang, Z.; Yao, Y.; Ranganathan, V.; Baglaenko, Y.; et al. IL-7 Primes IL-17 in Mucosal-Associated Invariant T (MAIT) Cells, Which Contribute to the Th17-Axis in Ankylosing Spondylitis. Ann. Rheum. Dis. 2016, 75, 2124–2132. [Google Scholar] [CrossRef]
- Lee, J.S.; Tato, C.M.; Joyce-Shaikh, B.; Gulen, M.F.; Cayatte, C.; Chen, Y.; Blumenschein, W.M.; Judo, M.; Ayanoglu, G.; McClanahan, T.K.; et al. Interleukin-23-Independent IL-17 Production Regulates Intestinal Epithelial Permeability. Immunity 2015, 43, 727–738. [Google Scholar] [CrossRef]
- Shen, H.; Goodall, J.C.; Hill-Gaston, J. S Frequency and Phenotype of Peripheral Blood Th17 Cells in Ankylosing Spondylitis and Rheumatoid Arthritis. Arthritis Rheum. 2009, 60, 1647–1656. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Tello, A.; Halwani, R.; Li, R.; Nadigel, J.; Bar-Or, A.; Mazer, B.D.; Eidelman, D.H.; Al-Muhsen, S.; Hamid, Q. IL-17A and IL-17F Expression in B Lymphocytes. Int. Arch. Allergy Immunol. 2012, 157, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Schlegel, P.M.; Steiert, I.; Kötter, I.; Müller, C.A. B Cells Contribute to Heterogeneity of IL-17 Producing Cells in Rheumatoid Arthritis and Healthy Controls. PLoS ONE 2013, 8, 82580. [Google Scholar] [CrossRef]
- Hsu, H.-C.; Yang, P.; Wang, J.; Wu, Q.; Myers, R.; Chen, J.; Yi, J.; Guentert, T.; Tousson, A.; Stanus, A.L.; et al. Interleukin 17–Producing T Helper Cells and Interleukin 17 Orchestrate Autoreactive Germinal Center Development in Autoimmune BXD2 Mice. Nat. Immunol. 2007, 9, 166–175. [Google Scholar] [CrossRef]
- Halwani, R.; Al-Kufaidy, R.; Vazquez-Tello, A.; Pureza, M.A.; BaHammam, A.S.; Al-Jahdali, H.; Alnassar, S.A.; Hamid, Q.; Al-Muhsen, S. IL-17 Enhances Chemotaxis of Primary Human B Cells during Asthma. PLoS ONE 2014, 9, e114604. [Google Scholar] [CrossRef]
- Subbarayal, B.; Chauhan, S.K.; di Zazzo, A.; Dana, R. IL-17 Augments B Cell Activation in Ocular Surface Autoimmunity. J. Immunol. 2016, 197, 3464–3470. [Google Scholar] [CrossRef]
- Pitzalis, C.; Jones, G.W.; Bombardieri, M.; Jones, S.A. Ectopic Lymphoid-like Structures in Infection, Cancer and Autoimmunity. Nat. Rev. Immunol. 2014, 14, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Spolski, R.; Leonard, W.J. Interleukin-21: A Double-Edged Sword with Therapeutic Potential. Nat. Rev. Drug Discov. 2014, 13, 379–395. [Google Scholar] [CrossRef]
- Andersen, T.; Rasmussen, T.K.; Hvid, M.; Holm, C.K.; Madsen, K.J.-N.B.; Jurik, A.G.; Hokland, M.; Stengaard-Pedersen, K.; Schiøttz-Christensen, B.; Deleuran, B. Increased Plasma Levels of IL-21 and IL-23 in Spondyloarthritis Are Not Associated with Clinical and MRI Findings. Rheumatol. Int. 2010, 32, 387–393. [Google Scholar] [CrossRef]
- Xiao, F.; Zhang, H.-Y.; Liu, Y.-J.; Zhao, D.; Shan, Y.-X.; Jiang, Y.-F. Higher Frequency of Peripheral Blood Interleukin 21 Positive Follicular Helper T Cells in Patients with Ankylosing Spondylitis. J. Rheumatol. 2013, 40, 2029–2037. [Google Scholar] [CrossRef] [PubMed]
- Levack, R.C.; Newell, K.L.; Popescu, M.; Cabrera-Martinez, B.; Winslow, G.M. CD11c + T-Bet + B Cells Require IL-21 and IFN-γ from Type 1 T Follicular Helper Cells and Intrinsic Bcl-6 Expression but Develop Normally in the Absence of T-Bet. J. Immunol. 2020, 205, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Kaaij, M.H.; Tok, M.N.V.; Blijdorp, I.C.; Ambarus, C.A.; Stock, M.; Pots, D.; Knaup, V.L.; Armaka, M.; Christodoulou-Vafeiadou, E.; Melsen, T.K.V.; et al. Transmembrane TNF Drives Osteoproliferative Joint Inflammation Reminiscent of Human Spondyloarthritis. J. Exp. Med. 2020, 217, e20200288. [Google Scholar] [CrossRef] [PubMed]
- Bollow, M.; Fischer, T.; ReiBhauer, H.; Backhaus, M.; Sieper, J.; Hamm, B.; Braun, J. Quantitative Analyses of Sacroiliac Biopsies in Spondyloarthropathies: T Cells and Macrophages Predominate in Early and Active Sacroiliitis—Cellularity Correlates with the Degree of Enhancement Detected by Magnetic Resonance Imaging. Ann. Rheum. Dis. 2000, 59, 135. [Google Scholar] [CrossRef]
- Vander Cruyssen, B.; Muñoz-Gomariz, E.; Font, P.; Mulero, J.; de Vlam, K.; Boonen, A.; Vazquez-Mellado, J.; Flores, D.; Vastesaeger, N.; Collantes, E.; et al. Hip Involvement in Ankylosing Spondylitis: Epidemiology and Risk Factors Associated with Hip Replacement Surgery. Rheumatology 2010, 49, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Xu, X.; Wang, Y.; Zheng, Z.; Lin, G. Ectopic Germinal Centers and IgG4-Producing Plasmacytes Observed in Synovia of HLA-B27+ Ankylosing Spondylitis Patients with Advanced Hip Involvement. Int. J. Rheumatol. 2015, 2015, 316421. [Google Scholar] [CrossRef]
- Voswinkel, J.; Weisgerber, K.; Pfreundschuh, M.; Gause, A. B Lymphocyte Involvement in Ankylosing Spondylitis: The Heavy Chain Variable Segment Gene Repertoire of B Lymphocytes from Germinal Center-like Foci in the Synovial Membrane Indicates Antigen Selection. Arthritis Res. 2001, 3, 189–195. [Google Scholar] [CrossRef] [PubMed]
- VOSWINKEL, J.; TRÜMPER, L.; CARBON, G.; HOPF, T.; PFREUNDSCHUH, M.; GAUSE, A. Evidence for a Selected Humoral Immune Response Encoded by VH4 Family Genes in the Synovial Membrane of a Patient with Rheumatoid Arthritis (RA). Clin. Exp. Immunol. 1996, 106, 5. [Google Scholar] [CrossRef] [PubMed]
- Laloux, L.; Voisin, M.C.; Allain, J.; Martin, N.; Kerboull, L.; Chevalier, X.; Claudepierre, P. Immunohistological Study of Entheses in Spondyloarthropathies: Comparison in Rheumatoid Arthritis and Osteoarthritis. Ann. Rheum. Dis. 2001, 60, 316. [Google Scholar] [CrossRef]
- Revell, P.A.; Mayston, V. Histopathology of the Synovial Membrane of Peripheral Joints in Ankylosing Spondylitis. Ann. Rheum. Dis. 1982, 41, 579–586. [Google Scholar] [CrossRef]
- Cunnane, G.; Bresnihan, B.; FitzGerald, O. Immunohistologic Analysis of Peripheral Joint Disease in Ankylosing Spondylitis. Arthritis Rheumatol. 1998, 41, 180–182. [Google Scholar] [CrossRef]
- Kruithof, E.; Baeten, D.; van den Bosch, F.; Mielants, H.; Veys, E.M.; de Keyser, F. Histological Evidence That Infliximab Treatment Leads to Downregulation of Inflammation and Tissue Remodelling of the Synovial Membrane in Spondyloarthropathy. Ann. Rheum. Dis. 2005, 64, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.S.W.; Rojas, O.L.; Gommerman, J.L. B Cell Depletion Therapies in Autoimmune Disease: Advances and Mechanistic Insights. Nat. Rev. Drug Discov. 2020, 20, 179–199. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Escalera, C.; Fernández-Nebro, A. The Use of Rituximab to Treat a Patient with Ankylosing Spondylitis and Hepatitis, B. Rheumatology 2008, 47, 1732–1733. [Google Scholar] [CrossRef] [PubMed]
- Nocturne, G.; Dougados, M.; Constantin, A.; Richez, C.; Sellam, J.; Simon, A.; Wendling, D.; Mariette, X.; Gottenberg, J.-E. Rituximab in the Spondyloarthropathies: Data of Eight Patients Followed up in the French Autoimmunity and Rituximab (AIR) Registry. Ann. Rheum. Dis. 2010, 69, 471–472. [Google Scholar] [CrossRef] [PubMed]
- AlDhaheri, F.; Almteri, T.; Dwid, N.; Majdali, A.; Janoudi, N.; Almoallim, H. Rituximab Can Induce Remission in a Patient with Ankylosing Spondylitis Who Failed Anti-TNF-α Agent. Am. J. Case Rep. 2017, 18, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Kobak, S.; Karaarslan, A.; Oksel, F. The Efficacy and Safety of Rituximab in a Patient with Rheumatoid Spondylitis. Case Rep. Rheumatol. 2013, 2013, 792526. [Google Scholar] [CrossRef] [PubMed]
- Omair, M.A.; Alnaqbi, K.A.; Lee, P. Rituximab in a Patient with Ankylosing Spondylitis with Demyelinating Disease: A Case Report and Review of the Literature. Clin. Rheumatol. 2012, 31, 1259–1261. [Google Scholar] [CrossRef] [PubMed]
- Wendling, D.; Augé, B.; Streit, G.; Toussirot, E.; Mathieu, S. Lack of Short-Term Efficacy of Rituximab upon Symptoms of Ankylosing Spondylitis Treated for an Associated Vasculitis. Jt. Bone Spine 2008, 75, 510–511. [Google Scholar] [CrossRef] [PubMed]
- Baeten, D.; Kruithof, E.; Breban, M.; Tak, P.P. Spondylarthritis in the Absence of B Lymphocytes. Arthritis Rheum. 2008, 58, 730–733. [Google Scholar] [CrossRef] [PubMed]
- Song, I.-H.; Heldmann, F.; Rudwaleit, M.; Listing, J.; Appel, H.; Haug-Rost, I.; Braun, J.; Sieper, J. One-Year Follow-up of Ankylosing Spondylitis Patients Responding to Rituximab Treatment and Re-Treated in Case of a Flare. Ann. Rheum. Dis. 2013, 72, 305–306. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, L.J.; Zochling, J.; Boonen, A.; Singh, J.A.; Veras, M.M.S.; Tanjong Ghogomu, E.; Benkhalti Jandu, M.; Tugwell, P.; Wells, G.A. TNF-Alpha Inhibitors for Ankylosing Spondylitis. Cochrane Database Syst. Rev. 2015, 4, CD005468. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilbrink, R.; Spoorenberg, A.; Verstappen, G.M.P.J.; Kroese, F.G.M. B Cell Involvement in the Pathogenesis of Ankylosing Spondylitis. Int. J. Mol. Sci. 2021, 22, 13325. https://doi.org/10.3390/ijms222413325
Wilbrink R, Spoorenberg A, Verstappen GMPJ, Kroese FGM. B Cell Involvement in the Pathogenesis of Ankylosing Spondylitis. International Journal of Molecular Sciences. 2021; 22(24):13325. https://doi.org/10.3390/ijms222413325
Chicago/Turabian StyleWilbrink, Rick, Anneke Spoorenberg, Gwenny M. P. J. Verstappen, and Frans G. M. Kroese. 2021. "B Cell Involvement in the Pathogenesis of Ankylosing Spondylitis" International Journal of Molecular Sciences 22, no. 24: 13325. https://doi.org/10.3390/ijms222413325
APA StyleWilbrink, R., Spoorenberg, A., Verstappen, G. M. P. J., & Kroese, F. G. M. (2021). B Cell Involvement in the Pathogenesis of Ankylosing Spondylitis. International Journal of Molecular Sciences, 22(24), 13325. https://doi.org/10.3390/ijms222413325






