1. Introduction
The knee is the largest hinge joint associated with weight-bearing and movement in the human body. The meniscus is at type of fibrocartilage, has properties similar to those of bone, and serves many important biomechanical functions such as stabilizing joints and absorbing damage. The knee contains medial and lateral menisci; the medial meniscus tends to experience more frequent damage than the lateral meniscus due to its anatomical structure and articular mechanism [
1]. Such damage includes a tear, which occurs when placing excessive pressure on or twisting the knee joint. Meniscal degeneration and surgically removed meniscus are risk factors for osteoarthritis [
2], while aging of the meniscus results in molecular and cellular changes. Thus, an understanding of the proteomic changes in the medial and lateral meniscal tissues will contribute to uncovering the cause of knee-related degenerative disease.
The extracellular matrix (ECM) plays an essential role in many processes, including cell-cell adhesion, signaling, and tissue repair. The meniscal ECM consists of water, fibrillar protein, proteoglycans, and adhesive glycoproteins, the activities of which are not fully understood.
To date, meniscus proteomics studies are rare, although information on hyaline cartilage protein has been reported [
3,
4,
5]. Recently, global proteomic investigations have been performed on medial meniscal tissues to analyze the global protein expression profiles in radial zones using mass spectrometric technologies. Pairwise comparisons of the medial/lateral meniscus is a potentially unique model for the study of cartilage proteomics in osteoarthritis genesis and progression, because the anatomical structure and biomechanical configuration of the knee is typically associated with much more severe cartilage loss on the predominantly weight-bearing medial compartment. Also, pairwise comparisons of the lateral/medial meniscus have advantages independent of heterogeneous factors such as age, sex, osteoarthritis severity, underlying disease, and individual variability.
Deep proteomics might be a powerful tool in characterization of meniscal tissues [
6,
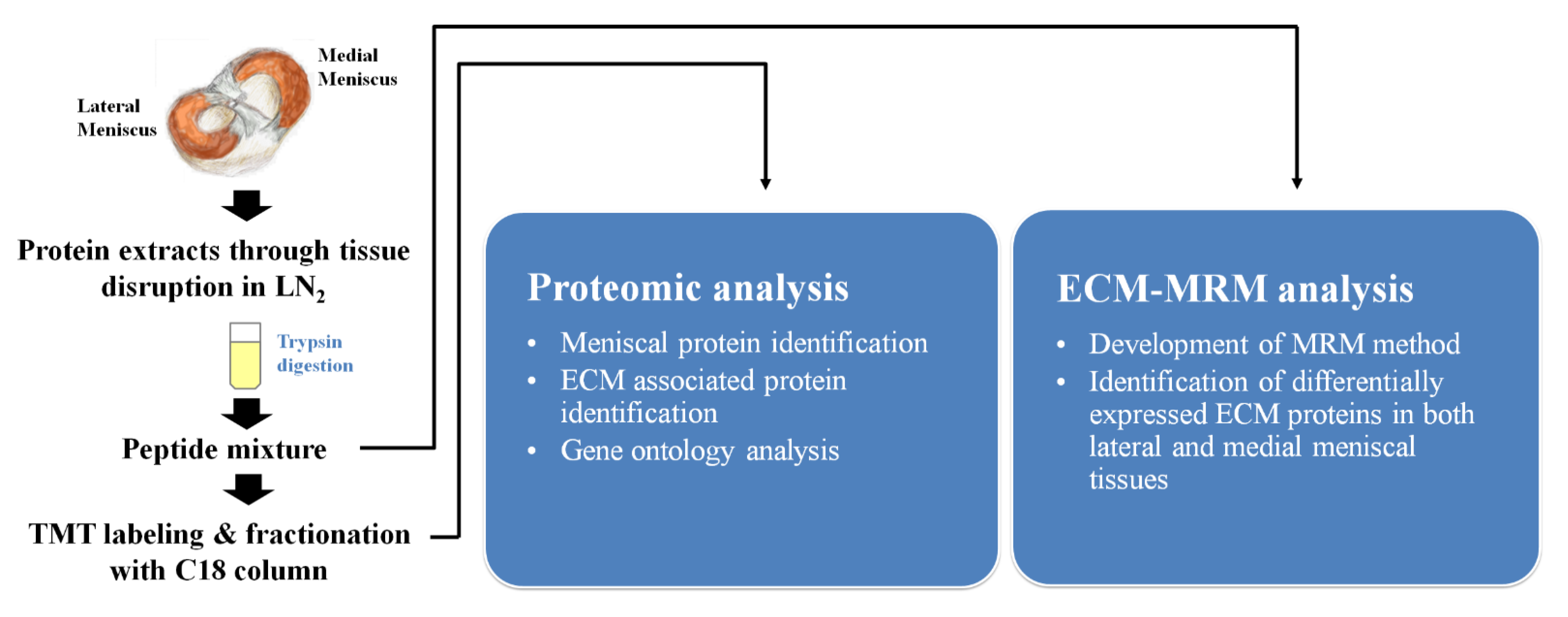
7]. Therefore, we investigated the proteome profile of meniscal tissue of lateral and medial lesions and characterized the extracellular matrix proteins. Herein, we provide extracellular matrix data and use multiple reaction monitoring (ECM-MRM) assays to compare expression levels in two lesion types.
3. Discussion
To investigate the type and distribution of ECM proteins in meniscal tissue is very important in cartilage tissue engineering as well as in identifying related disease etiologies, including osteoarthritis. Several studies have profiled the proteome of articular cartilage and medial meniscus tissue, but the ECM profile in these tissues is not sufficiently covered and quantified [
8,
9]. Thus, in this study, we characterized the proteomic profile of meniscal tissues consisting of medial and lateral lesions from osteoarthritis patients, which are still uncovered their protein composition but also quantified. We focused on meniscal ECM proteins, which contribute to repair and regenerate tissues and reported that ECM composition and expression levels in both lesions using both TMT analysis and MRM-MS. Herein we first provided the characterization of osteoarthritic meniscus using quantitative-based proteomic analysis, although there was few concentration change for major cartilage proteins such as COMP, CILP, CAN and collagens in the protein expression profile between lateral and medial meniscus.
Recently only a few pairwise comparisons of the lateral and medial osteoarthritis knee have been conducted (
Supplementary Table S5). Moreover, only one study was performed for the proteomic comparison between osteoarthritis menisci. Our study was conducted as a preliminary study to help us understand the mechanisms of osteoarthritis by comparing protein composition within lateral and medial from an expanded number of osteoarthritis subjects. We think it is important to analyze ECM proteins and to discover biomarkers that are definitely lacking in this field.
Osteoarthritis is caused by failure of chondrocytes to maintain homeostasis between synthesis and degradation of ECM components, such as polypeptide, growth factors and cytokines. Recent studies reported that the Wnt/β-catenin pathway plays an important role in the pathophysiology of osteoarthritis [
10]. We found that these differentially expressed ECM proteins were increased in regulation of peptidase activity, biological extracellular matrix processes, and ECM modulation. Among these ECM proteins, FRZB showed lower expression in the medial meniscus than lateral meniscus, whereas SMOC2, CSTB, CTSD, and CTSZ showed higher expression in the medial than lateral meniscus. FRZB acts as the WNT inhibitor, and loss of function of FRZB results from excessive WNT activation and increases susceptibility to osteoarthritis [
10]. SMOC2 is a member of the secreted protein acidic and rich in cysteine (SPARC) family and is associated with adult wound healing and age-dependent bone loss. Lu et al. recently demonstrated that SMOC2 directly interacted with WNT receptors and activated the WNT/β-catenin pathway in endometrial carcinoma [
11]. Furthermore, inflammation modulators (such as CSTB, CTSD, and CTSZ), which have been reported to contribute to osteoarthritis, were more highly expressed in the medial than lateral meniscus [
12]. These proteins might play an important role in regulation of chondrocyte growth and proliferation compared to cartilage proteins, which have a slow turnover rate. Therefore, alteration of these proteins can affect ECM regeneration, leading to promotion of osteoarthritis.
Our study has some limitations. First, we could not perform comparisons between osteoarthritis patients and healthy controls, because it is difficult to obtain intact meniscus samples from healthy subjects. Also, it is unclear whether the differences in protein expression levels of ECM in lateral and medial menisci from osteoarthritis patients directly correlate with tissue damage. Further study should be conducted to elucidate the relationship between the patterns of protein expression in meniscus and tissue damage in osteoarthritis.
Despite these limitations, the results of this study would be expected to provide important information in the treatment and diagnosis of various joint diseases as well as osteoarthritis in the future.
4. Methods
4.1. Clinical Samples
This study enrolled 12 osteoarthritis patients who received knee arthroscopy surgery at Samsung Medical Center. All 12 patients were female and had a mean age of 72.9 years (range 65–82 year). Tissue from lateral/medial menisci pairs was obtained during surgery, and the mean weight of the tissues was 2260 mg (range 950–4100 mg). Written informed consent was obtained from all enrolled patients. This study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (Seoul, Korea) (IRB file No. 2015-12-166).
4.2. Preparation of Tissues
About 200–300 mg of cartilage tissue was cut from each sample and pulverized in liquid nitrogen using a ball grinder. RIPA buffer (150 mM sodium chloride, 1% Triton X-100, 1% sodium deoxycholate, 0.1% SDS, 50 mM Tris-HCl pH 7.5, 2 mM EDTA, sterile solution, protease inhibitor) was added to the pulverized tissue and sonicated four times for 15 s each. A total of 500 µg of protein extract was subjected to FASP [
13]. Trypsin digestion was performed in a microwave at 450 W and 55 °C for one hour using a Rapid Enzyme Digestion system (Asta, Seoul, Korea). Desalting and concentration of the samples were performed using a StrataTM-X 33 um (Phenomenex Inc., Torrance, CA, USA) according to manufacturer instructions. These protein extracts were subjected to further mass spectrometry-based comparative proteomic analysis and an MRM assay (
Figure 2).
4.3. LC-MS/MS Analysis
In-solution digestion with trypsin, followed by 6-plex TMT treatment were performed according to the manufacturer’s instructions (Thermo Fisher Scientific, Waltham, MA, USA). After pooling each disease group, labeled peptide mixtures were separated via reverse phase HPLC into 12 fractions and were analyzed using an Orbitrap Elite mass spectrometer (Thermo Finnigan, San Jose, CA, USA) equipped with a nano-electrospray ion source.
The TMT-labeled peptide mixtures were analyzed using an Orbitrap Elite mass spectrometer equipped with a nano-electrospray ion source. The mobile phase consisted of buffer A (0.1% formic acid in water) and buffer B (0.1% formic acid in ACN). After injecting a sample onto the analytical column (75 um × 50 cm packed C18, 2 um particles, 100 Å pores) (Thermo Finnigan, CA, USA), a 90-min gradient method was used to separate the peptide mixture. Sample loading onto the analytical column was conducted at 3% buffer B, the mobile phase was held at 4% buffer B for 1 min, followed by a linear gradient to 32% buffer B over 91 min, followed by a linear gradient to 80% buffer B over 8 min at a flow rate of 300 nL/min.
4.4. MRM Assay for ECM Protein Determination
To develop the MRM assay, ECM MatrisomeDB 2.0 depository (
http://www.matrisomedb.org/) (accessed on 20 September 2018) was used to extract ECM-related proteins from the identified meniscal tissue profile. Those peptides and MRM transitions were generated using Skyline 4.1.011796 (MacCoss Lab Software, Seattle, WA, USA) and employed for further refinement of the selected peptides. At least three transitions from one proteotypic peptide were generated; 2 or 3 peptide charge states containing 8–30 amino acids, no post-translational modification (PTM), and non-specific cleavage were not allowed. Therefore, a total of 3024 MRM transitions was generated against 131 ECM proteins and 474 peptides. These MRM transitions were refined experimentally in protein extracts obtained from pooled meniscal tissues. A minimum of 3 MRM transitions per peptide should match the same retention times with S/N > 10. MRM was performed in positive mode using a QTRAP 5500 hybrid triple quadrupole/linear ion trap mass spectrometer (Sciex, Framingham, MA, USA) interfaced with a nano-electrospray ion source.
4.5. Data Annotation
All MS/MS spectra were searched against the UniProt Human protein database (8 August 2016, Reviewed 20197proteins) using the Integrated Proteomics Pipeline v.3 (IP2) search algorithm for peptide identification. The search parameters were as follows: specific to trypsin with two missed cleavages, variable modification of methionine oxidation, fixed modification of carbamidomethyl cysteine, ±10 ppm precursor-ion tolerance, ±600 ppm fragment-ion tolerance, and ±10 reporter ion tolerance.
Peak area ratio (PAR) was calculated to compare expression profiles among meniscal tissues. The peak area of each peptide transition was divided by the peak area of the corresponding transition from the isotope-labeled peptide. The concentration of these proteins was calculated as the product of PAR.
Gene Ontology (GO) analysis was performed using Funrich software (Version 3.1.3) and the web-based browser STRING (
https://string-db.org) (accessed on 19 November 2019) to classify the cellular components, biological process, and molecular function.
4.6. Statistics
Data acquired from MRM experiments were analyzed using the SPSS statistical package (IBM Corporation, Somers, NY, USA) ver 21.0 and MedCalc software ver 19.0.7 (Mariakerke, Belgium). Non-parametric tests were used for all proteomic markers. The proteomic differences in expression of markers between lateral and medial menisci groups were assessed with the Wilcoxon test. A p-value ≤ 0.05 was considered statistically significant.