Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels
Abstract
1. Introduction
2. Short Overview of Genetic Factors That Influence TSH and Thyroid Hormone Levels
3. Environmental Factors That Influence TSH and Thyroid Hormone Levels
3.1. Lifestyle Factors
3.1.1. Smoking
3.1.2. Alcohol Consumption
3.1.3. Body Mass Index
3.1.4. Diet
Soy
Brassica Vegetables
Olive Oil
Food Associated with the Development of Endemic Goiter
Other Food
Beverages
Micronutrients (Vitamins, Trace Minerals, Macrominerals)
3.1.5. Exercise
| Factor | Effect on Hormone Levels | Number of Participants | Reference | ||
|---|---|---|---|---|---|
| Smoking | ↓TSH, ↑fT4, ↑fT3 | 5766 | [16] | ||
↓TSH,  fT4, fT4,  fT3 fT3 | 4585 | [146] | |||
| ↓TSH, ↑fT4 | 895 | [21] | |||
↓TSH,  fT4 fT4 | 4357 | [28] | |||
| ↓TSH | 15,181 | [27] | |||
↓TSH,  fT4 fT4 | 3404 | [251] | |||
| ↓TSH | 5639 | [252] | |||
| ↓TSH | 4427 | [253] | |||
| ↓TSH, ↓tT4, ↑Tg | 1409 | [208] | |||
↓TSH, ↓tT4,  fT4, fT4,  tT3, ↑fT3, ↑Tg tT3, ↑fT3, ↑Tg | 1540 | [254] | |||
| ↓TSH | 1581 | [255] | |||
 TSH, TSH,  fT4, ↑fT3 fT4, ↑fT3 | 931 | [256] | |||
↓TSH,  fT4 fT4 | 3399 | [26] | |||
| ↓TSH, ↓tT4, ↓tT3 | 237 | [257] | |||
↓TSH,  fT4 fT4 | 1853 | [64] | |||
| ↓TSH, ↑fT4, ↑fT3 | 7799 | [22] | |||
| ↓TSH | 30,834 | [25] | |||
| ↓TSH, ↑fT4, ↑fT3 | 6085 | [258] | |||
↓TSH,  T4 T4 | 15,592 | [24] | |||
| ↓TSH, ↑T4 | 4462 | [259] | |||
↓TSH,  T4, T4,  fT4, fT4,  T3, T3,  fT3 fT3 | 1154 | [260] | |||
↓TSH,  T3 T3 | 4100 | [261] | |||
 TSH, TSH,  T4, ↑T3 T4, ↑T3 | 50 | [262] | |||
↓TSH,  T4, T4,  T3, ↑Tg T3, ↑Tg | 219 | [263] | |||
↓TSH, ↑T4,  T3 T3 | 181 | [264] | |||
 TSH, ↓T4, ↓T3 TSH, ↓T4, ↓T3 | 200 | [265] | |||
↓TSH,  T4, ↑T3, ↓rT3, ↑Tg T4, ↑T3, ↓rT3, ↑Tg | 441 | [266] | |||
| Alcohol consumption | ↑TSH, ↓fT3 | 5766 | [16] | ||
 TSH, ↓fT4 TSH, ↓fT4 | 549 (men) | [40] | |||
 TSH, ↓fT4, ↓fT3 TSH, ↓fT4, ↓fT3 | 67 | [39] | |||
 TSH, TSH,  T4, T4,  T3 T3 | 100 | [38] | |||
 TSH, TSH,  T4, ↑T3 T4, ↑T3 | 30 | ||||
 TSH, TSH,  fT4, ↓T4, fT4, ↓T4,  fT3, fT3,  T3 T3 | 55 | [37] | |||
| ↑fT4 | 21 | [43] | |||
 TSH, TSH,  T4, T4,  fT4, ↓T3, ↓fT3 fT4, ↓T3, ↓fT3 | 70 | [36] | |||
↑TSH,  T4, T4,  fT4, ↓fT3, ↓T3 fT4, ↓fT3, ↓T3 | 80 | [41] | |||
 TSH, TSH,  T4, T4,  T3, ↑Tg T3, ↑Tg | 111 | [44] | |||
 TSH, TSH,  fT4, ↓tT4, ↓tT3 fT4, ↓tT4, ↓tT3 | 38 | [42] | |||
| Increased body mass index |  TSH, ↓fT4 TSH, ↓fT4 | 90 | [267] | ||
| ↑TSH (BMI higher than 25.3 kg/m2) | 11,224 | [268] | |||
| ↓TSH (BMI lower than 25.3 kg/m2) | |||||
| ↑TSH | 75 | [269] | |||
| ↑TSH | 2789 | [15] | |||
 TSH, TSH,  fT4, fT4,  fT3 fT3 | 34 | [270] | |||
| ↑TSH, ↓fT4, ↑fT3 | 77,991 | [9] | |||
 TSH TSH | 88 | [271] | |||
| ↓fT4, ↑fT3, ↑fT3/ fT4 | 16,975 | [65] | |||
 TSH, TSH,  fT4, ↓fT3 fT4, ↓fT3 | 36,655 (all subjects) | [272] | |||
| ↓fT4 | 18,746 (men) | ||||
| ↑TSH | 80 | [273] | |||
 TSH, ↓fT4 TSH, ↓fT4 | 7693 | [274] | |||
 TSH, ↓fT4 TSH, ↓fT4 | 1100 | [275] | |||
| ↑TSH | 140 | [276] | |||
 TSH, TSH,  fT4, ↑fT3 fT4, ↑fT3 | 940 | [277] | |||
↑TSH, ↓fT4,  fT3 fT3 | 26,719 | [56] | |||
 TSH, TSH,  fT4, fT4,  fT3 fT3 | 1275 | [278] | |||
 TSH TSH | 162 | [279] | |||
| ↑TSH, ↓fT4 | 9402 | [8] | |||
| ↑TSH | 800 | [280] | |||
 TSH TSH | 1097 | [281] | |||
↑TSH,  fT4, fT4,  tT4, tT4,  fT3, ↑tT3, ↑Tg fT3, ↑tT3, ↑Tg | 746 (men) | [208] | |||
| ↑TSH | 1044 (men) | [282] | |||
 TSH, ↓fT4, ↑fT3, ↑tT3, ↑fT3/ fT4 TSH, ↓fT4, ↑fT3, ↑tT3, ↑fT3/ fT4 | 2315 | [60] | |||
 TSH, ↓fT4 TSH, ↓fT4 | 6241 (all subjects) | [283] | |||
| ↓TSH | 2837 (women) | ||||
 TSH, TSH,  fT4, ↑tT4, fT4, ↑tT4,  fT3, ↑tT3 fT3, ↑tT3 | 736 | [67] | |||
| ↑TSH | 417 | [284] | |||
| ↑TSH | 5918 | [285] | |||
↑TSH,  fT4, fT4,  fT3 fT3 | 60 | [286] | |||
 fT4, ↑fT3 fT4, ↑fT3 | 865 | [287] | |||
↑TSH,  fT4, ↑fT3 fT4, ↑fT3 | 3114 | [288] | |||
↑TSH,  fT4 fT4 | 778 | [289] | |||
| ↑TSH | 1084 | [290] | |||
| ↑TSH | 15,020 | [291] | |||
↑TSH,  fT4 fT4 | 581 | [292] | |||
↑TSH,  fT4, ↑fT3 fT4, ↑fT3 | 520 | [59] | |||
 TSH, TSH,  fT4, ↑T3, ↑T3/fT4 fT4, ↑T3, ↑T3/fT4 | 275 | [293] | |||
↑TSH,  fT4, fT4,  tT3 tT3 | 27,097 | [53] | |||
 TSH, ↓fT4 TSH, ↓fT4 | 44,196 | [294] | |||
 TSH, ↓fT4 TSH, ↓fT4 | 1853 | [64] | |||
↑TSH,  fT4, ↑fT3 fT4, ↑fT3 | 152 | [242] | |||
 TSH, ↓fT4 TSH, ↓fT4 | 1572 | [295] | |||
↑TSH,  fT4, fT4,  fT3 fT3 | 265 | [296] | |||
↑TSH,  fT4 fT4 | 86 | [297] | |||
 TSH, TSH,  fT4, ↑fT3, ↑fT3/ fT4 fT4, ↑fT3, ↑fT3/ fT4 | 201 | [57] | |||
| ↑TSH | 1725 | [23] | |||
↑TSH,  fT4, fT4,  fT3 fT3 | 87 | [298] | |||
↑TSH, ↓fT4,  fT3 fT3 | 4082 | [55] | |||
| Diet | Soy food or soy isoflavones | ↑TSH,  fT4, fT4,  fT3 fT3 | Meta-analysis | [14] | |
↑TSH, ↓fT4,  fT3, ↑rT3 fT3, ↑rT3 | 400 | [96] | |||
↑TSH, ↓fT4,  fT3 fT3 | 200 | [95] | |||
 TSH, TSH,  fT4, fT4,  fT3 fT3 | 47 | [93] | |||
 TSH, TSH,  fT4 fT4 | 505 | [299] | |||
 TSH, TSH,  fT4, ↓fT3 fT4, ↓fT3 | 43 | [100] | |||
 TSH, TSH,  fT4 fT4 | 403 | [94] | |||
 TSH, TSH,  fT4, fT4,  fT3 fT3 | 93 | [300] | |||
 TSH, TSH,  fT4 fT4 | 63 | [301] | |||
 TSH, TSH,  fT4, fT4,  fT3 fT3 | 389 | [92] | |||
 TSH, TSH,  T4 T4 | Meta-analysis | [302] | |||
 TSH TSH | 77 | [303] | |||
 TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 147 | [91] | |||
 TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3 tT3 | 35 | [90] | |||
 TSH, TSH,  T4, T4,  T3, T3,  fT4 fT4 | 25 | [143] | |||
 TSH TSH | 89 | [304] | |||
 TSH, TSH,  T4, T4,  T3 T3 | 38 | [89] | |||
 TSH, ↓fT4, TSH, ↓fT4,  fT3 fT3 | 32 | [98] | |||
| ↑TSH, ↑T4, ↑T3 | 73 | [97] | |||
 TSH TSH | 76 | [305] | |||
 TSH, TSH,  fT4, ↓fT3, fT4, ↓fT3,  T4, T4,  T3 T3 | 14 | [306] | |||
 TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3 tT3 | 18 | [99] | |||
| Brassica vegetables | Sulforaphane (natural product present in cruciferous vegetables like broccoli) |  TSH, TSH,  T4, T4,  Tg Tg | 45 | [109] | |
| Roots of cruciferous plant Lepidium peruvianum Chacon |  TSH, TSH,  T4, T4,  T3 T3 | 20 | [108] | ||
| Brussels sprouts |  TSH, TSH,  tT4, tT4,  fT4, fT4,  tT3 tT3 | 10 | [107] | ||
| Other food | Seaweed | ↑TSH,  fT3, fT3,  fT4 fT4 | 19 | [144] | |
| Seaweed | ↑TSH (returned to normal after several days),  fT4 fT4 | 9 | [145] | ||
| Seaweed | ↑TSH (returned to normal after several days), ↓fT4, ↓fT3 (returned to normal after several days) | 13 | [141] | ||
| Seaweed | ↑TSH,  T4, T4,  T3, T3,  fT4 fT4 | 25 | [143] | ||
| Kelp | ↑TSH,  fT4, ↓fT3 fT4, ↓fT3 | 36 | [142] | ||
| Kelp, vegans vs. omnivores | ↑TSH | 101 | [307] | ||
| Full-fat cheese, cottage cheese, hard cheese | ↓fT4 | 4585 | [146] | ||
| Pasta and rice | ↑fT4 | ||||
| Whole-grain bread | ↓fT4 | ||||
| White bread | ↑fT4 | ||||
| White fish, blue fish, dried fish, seafood, squid | ↑fT4, ↑fT3 | ||||
| Fruit juices, cedevita, nonalcoholic drinks | ↓TSH, ↑fT4 | ||||
| Pork, beef, eggs | ↓fT4 | ||||
| Bacon, sausages | ↑fT4, ↑fT3 | ||||
| Butter, animal fat | ↓fT4 | ||||
| Canned vegetables, mushrooms | ↓fT4, ↓fT3 | ||||
| Powder soups, vegetable juices | ↑fT4 | ||||
| Venison, fish derivates | ↓TSH | ||||
| Non-home-made meal | ↑T4 | 100 | [147] | ||
| Whole grains, green tea | ↓T3 | ||||
| Pasta | ↑fT4 | ||||
| Olive oil | Mediterranean diet |  TSH, ↓fT4, ↓fT3 TSH, ↓fT4, ↓fT3 | 324 | [120] | |
| Olive oil |  TSH, ↓fT4, ↓fT3 TSH, ↓fT4, ↓fT3 | ||||
| Vegetables cooked with olive oil | ↑T3 | 100 | [147] | ||
| Food associated with the development of endemic goiter | Cassava | ↓T4, ↓T3 | 20 | [308] | |
| Beverages | Coffee |  TSH, ↑fT4 TSH, ↑fT4 | 9408 | [164] | |
| Coffee |  TSH, TSH,  T3 T3 | Not reported | [163] | ||
| Micronutrients | ↑ Vitamin D |  TSH, ↑fT4, TSH, ↑fT4,  fT3 fT3 | 123 | [309] | |
| ↑ Vitamin D |  TSH, ↓T4, ↓T3 TSH, ↓T4, ↓T3 | 300 | [184] | ||
| ↓ Vitamin D |  TSH, TSH,  fT4 fT4 | 2006 | [310] | ||
| ↓ Vitamin D | ↑TSH | 294 | [182] | ||
| ↑ Vitamin D | ↓TSH | 1424 | [183] | ||
| ↑ Vitamin D | ↓TSH | 2582 | [175] | ||
| ↑Selenium |  TSH, ↓fT4, TSH, ↓fT4,  fT3 fT3 | 69 | [207] | ||
 TSH, ↑fT4 TSH, ↑fT4 | 184 (women) | [229] | |||
 TSH, TSH,  T4, T4,  fT4, fT4,  T3, T3,  rT3 rT3 | 387 | [311] | |||
↓TSH, ↓fT4,  fT3 fT3 | 361 | [206] | |||
 TSH, TSH,  fT4, fT4,  fT3, fT3,  Tg Tg | 1383 | [208] | |||
 TSH, ↓fT4, ↓fT3 TSH, ↓fT4, ↓fT3 | 1144 | [205] | |||
 TSH, ↑fT4 TSH, ↑fT4 | 140 | [312] | |||
 TSH, TSH,  tT4, ↑T3, tT4, ↑T3, | 28 | [313] | |||
 TSH, TSH,  fT4, fT4,  fT3, fT3,  Tg Tg | 88 | [314] | |||
 TSH, TSH,  T4, T4,  T3 T3 | 42 | [315] | |||
 TSH, ↓fT4, TSH, ↓fT4,  fT3 fT3 | 52 | [316] | |||
 TSH, ↓fT4, TSH, ↓fT4,  tT4, tT4,  fT3, fT3,  tT3, ↑fT3/fT4 tT3, ↑fT3/fT4 | 368 | [204] | |||
| ↑TSH, ↓T3 | 12 | [317] | |||
 TSH, TSH,  fT4, fT4,  fT3, fT3,  fT3/fT4 fT3/fT4 | 44 | [219] | |||
↓T4,  Tg Tg | 52 | [203] | |||
 TSH, ↓T4, TSH, ↓T4,  T3, ↑T3/T4 T3, ↑T3/T4 | 109 | [202] | |||
 TSH, ↓T4, ↓fT4, TSH, ↓T4, ↓fT4,  T3, ↓rT3 T3, ↓rT3 | 52 | [201] | |||
| ↑Zinc |  TSH, TSH,  fT4, fT4,  fT3 fT3 | 98 | [217] | ||
 TSH, ↓tT4, ↓fT4, TSH, ↓tT4, ↓fT4,  tT3, tT3,  fT3 fT3 | 746 (men) | [208] | |||
 TSH, TSH,  fT4, ↑fT3 fT4, ↑fT3 | 64 | [220] | |||
 TSH TSH | 219 | [318] | |||
↓tT4,  tT3 tT3 | 178 | [218] | |||
 TSH, TSH,  fT4, ↑fT3, ↑fT3/fT4 fT4, ↑fT3, ↑fT3/fT4 | 44 | [219] | |||
 TSH, TSH,  tT4, tT4,  fT4, fT4,  tT3 tT3 | 109 | [202] | |||
| Iron deficiency |  TSH, ↓fT4, ↓fT3 TSH, ↓fT4, ↓fT3 | 3846 | [228] | ||
| Iron deficiency anemia |  TSH, ↓tT4, TSH, ↓tT4,  fT4, ↓tT3, fT4, ↓tT3,  fT3 fT3 | 128 | [227] | ||
| Anemia |  TSH, TSH,  fT4, fT4,  tT4, ↑fT3 tT4, ↑fT3 | 50 | [226] | ||
| Iron supplements |  TSH, TSH,  fT4, ↑tT4, ↑tT3, ↓rT3 fT4, ↑tT4, ↑tT3, ↓rT3 | 94 | [319] | ||
| Anemia | ↓fT4, ↓fT3 | 20 | [320] | ||
| ↑Copper |  TSH, ↑fT4 TSH, ↑fT4 | 417 | [229] | ||
 TSH, ↑fT4, ↑tT4, TSH, ↑fT4, ↑tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 746 (men) | [208] | |||
 TSH, TSH,  fT4, ↑tT4, fT4, ↑tT4,  fT3, ↑tT3, fT3, ↑tT3,  Tg Tg | 663 (women) | ||||
| Iodine excess | ↑TSH | Meta-analysis | [240] | ||
| ↑TSH | 78,470 | [241] | |||
↑TSH,  fT4, ↓fT3 fT4, ↓fT3 | 854 | [239] | |||
| ↑TSH, ↓fT4, ↓fT3 | 236 | [321] | |||
| ↑TSH, ↓fT4, ↓fT3 | 256 | [238] | |||
| ↑TSH, ↓fT4, ↑Tg | 10 | [237] | |||
↓T4,  T3 T3 | 30 | [235] | |||
| ↑TSH, ↓T4, ↓T3 | 32 | [236] | |||
| Exercise |  TSH, TSH,  fT4 fT4 | 2470 | [250] | ||
| ↓TSH, ↑T4, ↑T3 | 36 | [248] | |||
 TSH, ↑fT4, ↑fT3 TSH, ↑fT4, ↑fT3 | 9 | [247] | |||
| ↑TSH, ↑fT4, ↑T4, ↓fT3, ↓T3 | 60 | [249] | |||
 TSH, TSH,  fT4, fT4,  T4, T4,  fT3, fT3,  T3 T3 | 26 | [246] | |||
| ↑fT4, ↓fT3, ↓T3, ↑rT3 | 27 | [322] | |||
 TSH TSH | 6 | [323] | |||
 fT4, fT4,  T4, T4,  fT3, fT3,  T3, T3,  rT3 rT3 | 46 | [324] | |||
| ↑TSH, ↑fT4 | 14 | [325] | |||
 T4, ↑T3, ↑rT3 T4, ↑T3, ↑rT3 | 12 | [326] | |||
| ↑T4, ↓T3, ↑rT3 | 4 | [327] | |||
| ↑TSH | 8 | [328] | |||
3.2. Pollutants
3.2.1. Chemicals
Polychlorinated Biphenyls and Polybrominated Biphenyls
Polybrominated Diphenyl Ethers
Bisphenol A
Phthalates
Perchlorate
Perfluoroalkyl Substances
Pesticides
Nitrate
3.2.2. Heavy Metals
| Factor | Compounds Used in the Study | Effect on Hormone Levels | Number of Participants | Reference | ||
|---|---|---|---|---|---|---|
| Chemicals | Polychlorinated biphenyls and polybrominated biphenyls | PBB |  TSH, ↓fT4, ↑fT3, ↑tT3, ↑fT3/fT4 TSH, ↓fT4, ↑fT3, ↑tT3, ↑fT3/fT4 | 715 | [349] | |
| PCB |  TSH, ↑fT4, TSH, ↑fT4,  fT3, ↑fT3/fT4 fT3, ↑fT3/fT4 | |||||
| PCBs and hydroxylated PCBs |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3 tT3 | 79 | [348] | |||
| PCB |  TSH, ↑fT4, ↑tT4, ↑fT3, ↑tT3 TSH, ↑fT4, ↑tT4, ↑fT3, ↑tT3 | 551 | [347] | |||
| PCB |  TSH, ↓fT4, ↓fT3 TSH, ↓fT4, ↓fT3 | 122 | [346] | |||
| PCB |  TSH, ↓fT4, ↑tT4, TSH, ↓fT4, ↑tT4,  tT3 tT3 | 87 | [345] | |||
| PCB | ↓TSH, ↑fT4, ↑tT4, ↑fT3, ↑tT3 | 67 | [353] | |||
| PCB | ↓tT3 | 114 | [435] | |||
| PCB x BDE | ↑tT3 | |||||
| PCB |  TSH, TSH,  fT4, ↓tT3 fT4, ↓tT3 | 623 | [344] | |||
| PCB | ↑TSH, ↓T4, ↓T3 | 211 | [351] | |||
| PCB | ↑TSH, ↓fT4,  tT4, tT4,  tT3 tT3 | 232 | [423] | |||
| PCB |  TSH, ↑fT4, ↑tT3 TSH, ↑fT4, ↑tT3 | 2042 | [484] | |||
| PCB |  TSH, TSH,  fT4, ↓tT3 fT4, ↓tT3 | 341 | [343] | |||
| PCB |  TSH, ↑fT4 TSH, ↑fT4 | 2045 | [422] | |||
| PCB | ↓tT4 | 2445 | [356] | |||
| Dioxin-like toxic equivalents | ↑TSH, ↓tT4 | |||||
| PCB | ↓TSH | 454 | [418] | |||
| PCB |  TSH, TSH,  fT4 fT4 | 196 | [341] | |||
| PCB | ↓TSH, ↓tT4, ↓tT3 | 66 | [352] | |||
| Dioxin-like toxic equivalents | ↓TSH | |||||
| PCB |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3 tT3 | 110 | [354] | |||
| PCB |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, ↓tT3 fT3, ↓tT3 | 182 | [339] | |||
| PCB | ↓T4 | 229 | [355] | |||
| PCB |  TSH, TSH,  fT4, fT4,  tT4 tT4 | 192 | [421] | |||
| PCB |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3 fT3 | 173 | [340] | |||
| PCB |  tT4 tT4 | 111 | [350] | |||
| Polybrominated diphenyl ethers | PBDE | ↑TSH,  fT4, fT4,  tT4, ↑fT3, ↓tT3 tT4, ↑fT3, ↓tT3 | 85 | [362] | ||
| PBDE |  TSH, TSH,  fT4, ↑tT4, fT4, ↑tT4,  fT3, ↑tT3 fT3, ↑tT3 | 79 | [348] | |||
| PBDE |  TSH, TSH,  fT4, ↓tT4, fT4, ↓tT4,  tT3 tT3 | 52 | [361] | |||
| PBDE |  TSH, TSH,  fT4, ↑tT3 fT4, ↑tT3 | 623 | [344] | |||
| PBDE | ↑TSH | 49 | [363] | |||
| PBDE |  TSH, TSH,  fT4, fT4,  tT4, tT4,  tT3 tT3 | 36 | [360] | |||
| PBDE | ↓TSH, ↑tT4, ↓tT3, ↑rT3 | 308 | [364] | |||
| PBDE (BDE-47) | ↓TSH,  tT4, tT4,  fT4, fT4,  tT3, tT3,  fT3 fT3 | 110 | [354] | |||
| Bisphenol A | BPA |  TSH, TSH,  tT4, ↑tT3 tT4, ↑tT3 | 90 | [368] | ||
| BPA | ↓TSH,  tT4, tT4,  tT3 tT3 | 6003 | [372] | |||
| BPA | ↑TSH,  fT4 fT4 | 194 | [370] | |||
| BPA |  TSH, ↓fT4 TSH, ↓fT4 | 2340 | [367] | |||
| BPA | ↓TSH,  fT4, ↑fT3 fT4, ↑fT3 | 3394 | [371] | |||
| BPA |  TSH, TSH,  fT4, fT4,  tT4, tT4,  tT3, tT3,  Tg Tg | 1346 | [369] | |||
| BPA | ↓TSH,  fT4, fT4,  tT3 tT3 | 167 | [373] | |||
| Phthalates | DEHP metabolites and MEHHP | ↓tT4 | Meta-analysis (included studies on pregnant women and children) | [382] | ||
| MEOHP | ↓fT4 | |||||
| MEHHP, DEHP metabolite |  TSH, TSH,  fT4, ↓T4, fT4, ↓T4,  T3 T3 | 279 | [379] | |||
| MEHP, MEOHP |  TSH, ↓fT4, TSH, ↓fT4,  T4, T4,  T3 T3 | |||||
| Monoethyl phthalate |  TSH, ↑fT4, TSH, ↑fT4,  T4, T4,  T3 T3 | |||||
| MEOHP | ↑TSH,  tT4, tT4,  tT3 tT3 | 6003 | [372] | |||
| DEHP metabolites |  TSH, ↓tT4, TSH, ↓tT4,  tT3 tT3 | |||||
| MnBP |  TSH, TSH,  tT4, ↓tT3 tT4, ↓tT3 | |||||
| MnBP | ↑TSH,  fT4 fT4 | 43 (all subjects) | [380] | |||
| MnBP, 5Cx-MEP, 5Oxo-MEHP, MBzP | ↑TSH,  fT4 fT4 | 30 (women) | ||||
| MEHHP | ↓tT4 | 1877 (all subjects) | [381] | |||
| MEOHP | ↑tT4 | 907 (women) | ||||
| DEHP | ↑TSH, ↓fT4, ↓tT4, ↓tT3, ↓Tg | 1346 | [369] | |||
| MEHP |  TSH, ↓fT4, ↓tT3 TSH, ↓fT4, ↓tT3 | 408 | [378] | |||
| Perchlorate | Perchlorate |  TSH, ↓fT4 TSH, ↓fT4 | 2702 | [388] | ||
| ↓fT4 | 564 | [387] | ||||
 TSH, ↓fT4, ↓tT4 TSH, ↓fT4, ↓tT4 | 4023 | [386] | ||||
↓fT4, ↓tT4, ↓fT3,  tT3 tT3 | 1877 | [381] | ||||
| ↑TSH, ↓tT4 | 1111 | [385] | ||||
| Perfluoroalkyl substances | PFAS |  TSH, TSH,  fT4, fT4,  fT3 fT3 | 3297 | [399] | ||
| PFOS, PFNA, PFAS, PFHxS |  TSH, ↑fT4, TSH, ↑fT4,  tT4, tT4,  fT3, fT3,  tT3 tT3 | 1325 | [400] | |||
| PFOA |  TSH, ↓tT4, ↓fT4, TSH, ↓tT4, ↓fT4,  tT3 tT3 | 3070 | [398] | |||
| PFOS |  TSH, ↓tT4, TSH, ↓tT4,  fT4, fT4,  tT3 tT3 | |||||
| PFNA, PFDeA | ↓TSH,  tT4, tT4,  fT4, fT4,  tT3 tT3 | |||||
| PFOA, PFNA | ↑TSH,  tT4, tT4,  fT4, fT4,  tT3, tT3,  fT3 fT3 | 85 | [406] | |||
| PFNA | ↑tT3, ↑fT3 | 47 (women) | ||||
| PFNA | ↓tT3, ↓fT3 | 38 (men) | ||||
| PFOS | ↑fT3 | 47 (women) | ||||
| PFOS | ↓fT3 | 38 (men) | ||||
| PFOS | ↑TSH, ↓tT4, ↑fT4, ↓tT3 | Meta-analysis (including pregnant women) | [401] | |||
| PFOA |  TSH, ↓tT4, TSH, ↓tT4,  tT3 tT3 | |||||
| PFNA |  TSH, TSH,  T4, ↑fT4, ↑T3 T4, ↑fT4, ↑T3 | 99 | [397] | |||
| PFOA |  TSH, TSH,  T4, T4,  fT4, ↑T3 fT4, ↑T3 | |||||
| PFOA |  TSH, TSH,  fT4, fT4,  tT4, tT4,  tT3, ↑fT3 tT3, ↑fT3 | 1012 | [396] | |||
| PFOS |  TSH, ↑fT4, ↑tT4, TSH, ↑fT4, ↑tT4,  tT3 tT3 | 87 | [345] | |||
| PFOS, PFNA | ↓TSH,  tT4, tT4,  fT4, fT4,  tT3, tT3,  fT3 fT3 | 158 (male adolescents) | [402] | |||
| PFOA | ↓TSH,  tT4, tT4,  fT4, fT4,  tT3, tT3,  fT3 fT3 | 145 (female adolescents) | ||||
| PFOA, PFOS, PFNA |  TSH, TSH,  tT4, ↑fT4, tT4, ↑fT4,  tT3, tT3,  fT3 fT3 | 257 (women 20-40 years old) | ||||
| PFOA |  TSH, TSH,  tT4, tT4,  fT4, ↑tT3, ↑fT3 fT4, ↑tT3, ↑fT3 | 199 (women 60-80 years old) | ||||
| PFNA |  TSH, ↑fT4 TSH, ↑fT4 | 567 | [403] | |||
| PFOA | ↑TSH,  tT4, tT4,  fT4, ↑tT3, fT4, ↑tT3,  fT3, fT3,  Tg Tg | 1540 | [254] | |||
| PFHxS |  TSH, ↑tT4, TSH, ↑tT4,  fT4, fT4,  tT3, tT3,  fT3, fT3,  Tg Tg | |||||
| PFOA |  TSH, TSH,  tT4, tT4,  fT4, ↑tT3, fT4, ↑tT3,  fT3 fT3 | 509 (women) | [395] | |||
| PFHxS |  TSH, ↑tT4, TSH, ↑tT4,  fT4, ↑tT3, fT4, ↑tT3,  fT3 fT3 | 509 (women) | ||||
 TSH, TSH,  tT4, ↓fT4, tT4, ↓fT4,  tT3, tT3,  fT3 fT3 | 672 (men) | |||||
| PFTrDA | ↑TSH, ↓tT4 | 633 | [405] | |||
| PFOS, PFOA |  TSH, ↑tT4 TSH, ↑tT4 | 50,113 | [394] | |||
| PFC |  TSH, TSH,  fT4 fT4 | 31 | [393] | |||
| PFOS | ↓TSH, ↑fT4, ↓tT3 | 623 | [344] | |||
| PFOA |  TSH, ↓fT4, TSH, ↓fT4,  T4, ↑T3 T4, ↑T3 | 506 | [392] | |||
| PFOA |  TSH TSH | 371 | [391] | |||
| PFOS |  TSH, TSH,  fT4, fT4,  T4, ↑T3 T4, ↑T3 | 255 | [404] | |||
| Pesticides | Conventional farmers that use insecticides, herbicides and fungicides in comparison to organic farmers | ↑TSH, ↓fT4, ↑T4, ↑fT3, ↑T3 | 438 | [410] | ||
| Organophosphate insecticides |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3 tT3 | 41 | [432] | |||
| Rural workers exposed to pesticides in comparison to controls | ↓TSH, ↑fT4, ↑tT3 | 73 | [420] | |||
| 3-PBA (metabolite of pyrethroid insecticide) |  TSH, ↓tT4, ↓tT3 TSH, ↓tT4, ↓tT3 | 6208 | [429] | |||
| Insecticides and pyrethroids for >20 years | ↓fT4, ↓tT3 | 106 | [436] | |||
| TCPY (a metabolite of chlorpyrifos) |  TSH, ↓tT4, TSH, ↓tT4,  fT4, fT4,  tT3, tT3,  fT3, ↓Tg fT3, ↓Tg | 2015 | [427] | |||
| Mancozeb (fungicide) |  TSH, TSH,  fT4, ↓T4, ↑fT3, fT4, ↓T4, ↑fT3,  T3, ↓Tg T3, ↓Tg | 63 | [428] | |||
| 3-PBA |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 2015 | [430] | |||
| p,p′-DDE (a stable metabolite of DDT) |  TSH, ↑tT4, ↑tT3 TSH, ↑tT4, ↑tT3 | 136 | [434] | |||
| Pesticide sprayers exposed to organophosphate and organochlorine pesticides | ↑TSH,  T4, ↓T3 T4, ↓T3 | 60 | [417] | |||
| DDT+DDE | ↑tT4, ↑tT3 | 48 (women) | [435] | |||
| DDT+DDE + PCB | ↑tT4 | |||||
| DDT+DDE + PCB | ↓tT3 | 66 (men) | ||||
| Exposure to organophosphate and carbamate pesticides |  TSH, TSH,  fT4 fT4 | 99 | [425] | |||
| High exposure pesticide season |  TSH, ↓fT4, TSH, ↓fT4,  tT3 tT3 | 91 | [426] | |||
| HCH | ↑TSH, ↓fT4 | 303 (men) | [416] | |||
| HCB, heptachlor, o,p′-DDT and p,p′-DDT | ↑fT4 | 305 (women) | ||||
| Endosulphan 2 | ↓tT3 | 303 (men) | ||||
| Alpha-chlordane, p,p′- DDT, endosulphan 2 and methoxychlor | ↑tT3 | 305 (women) | ||||
| TCPY (a metabolite of chlorpyrifos) | ↓TSH, ↑tT4 | 1589 (men) | [415] | |||
| ↑TSH | 218 (women) | |||||
| Insecticide fipronil sulfone metabolite | ↓TSH,  fT4, fT4,  tT4 tT4 | 155 | [419] | |||
| DAP | ↑TSH, ↑tT4 | 215 | [414] | |||
| DMP | ↑TSH, ↑tT4, ↓tT3 | |||||
| Organochlorine pesticides | ↓tT3 | 623 | [344] | |||
| Hexachlorobenzene | ↓fT4 | |||||
| cis-DCCA (pyrethroid metabolite) |  TSH, TSH,  fT4, fT4,  tT3 tT3 | 161 | [424] | |||
| 3-PBA and trans-DCCA (pyrethroid metabolites) |  TSH, TSH,  fT4, fT4,  tT3 tT3 | |||||
| HCB |  TSH, TSH,  fT4, ↓tT4, fT4, ↓tT4,  tT3 tT3 | 232 | [423] | |||
| DDE |  TSH, ↓fT4, ↑tT3 TSH, ↓fT4, ↑tT3 | 2045 | [422] | |||
| HCB | ↑TSH, ↓fT4,  tT3 tT3 | |||||
| p,p′-DDE | ↓TSH, ↑fT4, ↑tT3 | 341 | [343] | |||
| HCB | ↓tT3 | |||||
| p,p′-DDE |  TSH, TSH,  tT4 tT4 | 2445 | [356] | |||
| PCB + DDE + HCB | ↓TSH | 454 | [418] | |||
| DDE |  TSH, TSH,  tT4, tT4,  tT3 tT3 | 66 | [352] | |||
| p,p′-DDE | ↑TSH,  fT4 fT4 | 196 | [341] | |||
| High exposure pesticide season |  TSH, ↓fT4, TSH, ↓fT4,  fT3, fT3,  tT3 tT3 | 122 | [433] | |||
| In the fall in comparison to the spring season (people are exposed to higher levels of pesticides in fall) | ↓TSH, ↑fT4, ↑fT3, ↑tT3 | |||||
| TCPY (a metabolite of chlorpyrifos) | ↑TSH,  fT4, fT4,  tT3 tT3 | 322 | [413] | |||
| 1N (a metabolite of carbaryl and naphthalene) |  TSH, TSH,  fT4, fT4,  tT3 tT3 | |||||
| EBDC fungicides |  TSH TSH | 131 | [431] | |||
| HCB |  T4 T4 | 66 | [485] | |||
| High exposure pesticide season | ↑TSH, ↑fT4, ↑tT4 | 193 | [412] | |||
| DDT, HCB | ↓T3 | 16 | [438] | |||
| DDE |  TSH, TSH,  T4, T4,  T3 T3 | 51 | [355] | |||
| HCB |  TSH, TSH,  fT4, ↓tT4 fT4, ↓tT4 | 192 | [421] | |||
| Exposure to organophosphates and organochlorine pesticides |  TSH, TSH,  T4, ↓T3 T4, ↓T3 | 50 | [437] | |||
| EBDC fungicides | ↑TSH,  T4 T4 | 94 | [411] | |||
| Nitrate | Nitrate |  T4, T4,  T3 T3 | 30 | [445] | ||
↑TSH,  fT4 fT4 | 41 | [443] | ||||
| ↓fT4 | 307 | [387] | ||||
 TSH, ↓tT4 TSH, ↓tT4 | 1111 | [385] | ||||
 TSH, TSH,  T4, T4,  T3 T3 | 20 | [444] | ||||
| ↓TSH, ↑T4 | 60 | [442] | ||||
| Heavy metals | Studies determining multiple metals | Pb, Cd, As |  TSH TSH | 102 | [454] | |
| Pb | ↑TSH,  fT4, fT4,  fT3 fT3 | 100 | [460] | |||
| Cd |  TSH, TSH,  fT4, fT4,  fT3 fT3 | |||||
| Pb | ↑TSH,  tT4, tT4,  tT3 tT3 | 5628 | [461] | |||
| Cd |  TSH, TSH,  tT4, tT4,  tT3 tT3 | |||||
| Cd |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 1391 | [459] | |||
| Pb |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | |||||
| Cd |  TSH, ↑fT4, TSH, ↑fT4,  tT4, tT4,  fT3, fT3,  tT3, ↑Tg tT3, ↑Tg | 6231 (all subjects) | [458] | |||
 TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, ↑tT3, ↑Tg fT3, ↑tT3, ↑Tg | 3231 (men) | |||||
| Pb |  TSH, TSH,  fT4, fT4,  tT4, ↑fT3, tT4, ↑fT3,  tT3, tT3,  Tg Tg | 6231 (all subjects) | ||||
 TSH, TSH,  fT4, ↓tT4, fT4, ↓tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 3231 (men) | |||||
 TSH, ↑fT4, TSH, ↑fT4,  tT4, tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 3000 (women) | |||||
| Hg |  TSH, TSH,  fT4, ↓tT4, ↓fT3, ↓tT3, fT4, ↓tT4, ↓fT3, ↓tT3,  Tg Tg | 4409 | [457] | |||
| Cd |  TSH, TSH,  fT4, ↑tT4, ↑fT3, ↑tT3, ↑Tg fT4, ↑tT4, ↑fT3, ↑tT3, ↑Tg | |||||
| Pb |  TSH, TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | |||||
| Hg |  TSH, TSH,  fT4, ↓T4, ↓fT3, ↓T3 fT4, ↓T4, ↓fT3, ↓T3 | 1587 | [456] | |||
| Cd | ↓TSH, ↑fT4, ↑T4, ↑fT3, ↑T3 | |||||
| Pb | ↓TSH | 219 | [318] | |||
| As | ↑TSH | |||||
| Hg, Cd |  TSH TSH | |||||
| Pb | ↓TSH,  T4, ↑T3 T4, ↑T3 | 211 | [351] | |||
| Hg | ↑TSH,  T4, T4,  T3 T3 | |||||
| Pb |  TSH, TSH,  fT4, fT4,  tT4, ↑T3 tT4, ↑T3 | 232 | [423] | |||
| Hg |  TSH, TSH,  fT4, fT4,  tT4, tT4,  T3 T3 | |||||
| Studies determining single metal | Arsenic | UDMA | ↑TSH, ↓fT4, ↓tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | 4126 | [453] | |
| UAAS |  TSH, TSH,  fT4, ↓tT4, fT4, ↓tT4,  fT3, fT3,  tT3, tT3,  Tg Tg | |||||
| UAS, UAB | ↓TSH,  fT4, fT4,  tT4, tT4,  fT3, fT3,  tT3, ↓Tg tT3, ↓Tg | |||||
↑TSH,  fT4, fT4,  fT3 fT3 | 38 | [452] | ||||
| ↑TSH, ↓fT4, ↓fT3, ↑Tg | 185 | [451] | ||||
| Cadmium |  TSH, ↓fT4 TSH, ↓fT4 | 1972 | [463] | |||
 TSH, ↑fT4, ↑fT3 TSH, ↑fT4, ↑fT3 | 1724 | [462] | ||||
| ↑TSH, ↓fT4, ↓fT3 | 277 | [455] | ||||
| ↓fT4, ↑tT3 | 105 | [464] | ||||
| Mercury | ↑TSH, ↑fT4, ↓T4,  fT3, fT3,  T3 T3 | Meta-analysis | [480] | |||
↑TSH,  fT4, fT4,  fT3, fT3,  tT3 tT3 | 110 | [479] | ||||
 TSH, ↓T4, ↓T3 TSH, ↓T4, ↓T3 | 137 | [482] | ||||
 TSH, ↑fT4, ↓fT3, ↑fT4/fT3 TSH, ↑fT4, ↓fT3, ↑fT4/fT3 | 82 | [481] | ||||
| ↑rT3, ↑fT4/fT3 | 94 | [483] | ||||
| Lead | ↓TSH, ↑fT4, ↑fT3 | 87 | [468] | |||
 TSH, TSH,  fT4, fT4,  T4, T4,  fT3, fT3,  T3 T3 | Meta-analysis | [475] | ||||
 TSH, TSH,  T4, T4,  T3 T3 | 195 | [474] | ||||
 T4, ↓fT4 T4, ↓fT4 | 220 | [478] | ||||
| ↑T3, ↑T4 | 76 | [477] | ||||
| ↑TSH | 125 | [467] | ||||
 TSH, ↓fT4, TSH, ↓fT4,  fT3 fT3 | 97 | [473] | ||||
 TSH, TSH,  fT4, fT4,  T4, ↓fT3, ↓T3 T4, ↓fT3, ↓T3 | 157 | [472] | ||||
 TSH, TSH,  fT4, fT4,  fT3 fT3 | 103 | [471] | ||||
↑TSH,  fT4, ↓T4, ↓T3 fT4, ↓T4, ↓T3 | 75 | [465] | ||||
↑TSH,  fT4, fT4,  fT3 fT3 | 93 | [466] | ||||
 TSH, ↑fT4, ↑tT4, ↑fT3, TSH, ↑fT4, ↑tT4, ↑fT3,  tT3 tT3 | 57 | [476] | ||||
 TSH, TSH,  T4 T4 | 151 | [469] | ||||
 TSH, ↓fT4, ↓tT4, TSH, ↓fT4, ↓tT4,  tT3 tT3 | 176 | [470] | ||||
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 1N | 1-naphthol |
| 3-PBA | phenoxybenzoic acid |
| 5Cx-MEP | mono-ethyl phthalate |
| 5Oxo-MEHP | mono-(2-ethylhexyl) phthalate |
| As | arsenic |
| BMI | body mass index |
| BPA | bisphenol A |
| Cd | cadmium |
| DAP | dialkyl phosphate |
| cis and trans-DCCA | cis and trans-3-2,2-dichlorovinyl-2,2-dimethylcyclopropane carboxylic acid |
| DDE | p,p′-diphenyldichloroethene |
| DDT | p,p′-dichlorodiphenyltrichloroethane |
| DEHP | di-(2-ethylhexyl) phthalate |
| Dio1 | type 1 iodothyronine deiodinase |
| Dio2 | type 2 iodothyronine deiodinase |
| DMP | dimethyl metabolite |
| EBDC | ethylene bisdithiocarbamate |
| EDC | endocrine-disrupting compound |
| ESS | euthyroid sick syndrome |
| fT3 | free triiodothyronine |
| fT4 | free thyroxine |
| GWAS | genome-wide association studies |
| HCB | hexachlorobenzene |
| HCH | beta-hexachlorocyclohexane |
| Hg | mercury |
| HPT axis | hypothalamus–pituitary–thyroid axis |
| MBzP | mono-benzyl phthalate |
| MEHP | mono(2-ethylhexyl) phthalate |
| MEHHP | mono (2-ethyl-5-hydroxyhexyl) phthalate |
| MEOHP | mono-(2-ethyl-5-oxohexyl) phthalate |
| MnBP | mono-n-butyl phthalate |
| NIS | sodium/iodide symporter |
| PBB | polybrominated biphenyl |
| PBDE | polybrominated diphenyl ether |
| PCB | polychlorinated biphenyl |
| PFAS | perfluoroalkyl substance |
| PFC | perfluorinated compound |
| PFDeA | perfluorodecanoate |
| PFHxS | perfluorohexane sulfonate |
| PFNA | perfluorononanoic acid |
| PFOA | perfluorooctanoic acid |
| PFOS | perfluorooctane sulfonic acid |
| PFTrDA | perfluorotridecanoic acid |
| POP | persistent organic pollutant |
| rT3 | reverse triiodothyronine |
| T3 | triiodothyronine |
| T4 | thyroxine |
| tT3 | total T3 |
| tT4 | total T4 |
| TCPY | trichloro-2-pyridinol |
| Tg | thyroglobulin |
| TPO | thyroid peroxidase |
| TRH | thyrotropin-releasing hormone |
| TSH | thyroid-stimulating hormone |
| UAAS | arsenic adjusted for arsenobetaine |
| UAB | arsenobetaine |
| UAS | total arsenic |
| UDMA | dimethylarsinic acid |
| VDR | vitamin D receptor |
References
- Fekete, C.; Lechan, R.M. Central regulation of hypothalamic-pituitary-thyroid axis under physiological and pathophysiological conditions. Endocr. Rev. 2014, 35, 159–194. [Google Scholar] [CrossRef]
- Dayan, C.; Panicker, V. Management of hypothyroidism with combination thyroxine (T4) and triiodothyronine (T3) hormone replacement in clinical practice: A review of suggested guidance. Thyroid Res. 2018, 11, 1. [Google Scholar] [CrossRef]
- Bianco, A.; Kim, B. Deiodinases: Implications of the local control of thyroid hormone action. J. Clin. Investig. 2006, 116, 2571–2579. [Google Scholar] [CrossRef]
- Hoermann, R.; Midgley, J.E.M.; Larisch, R.; Dietrich, J.W. Relational stability in the expression of normality, variation, and control of thyroid function. Front. Endocrinol. 2016, 7, 142. [Google Scholar] [CrossRef]
- American Thyroid Association. Available online: https://www.thyroid.org/media-main/press-room/ (accessed on 30 March 2021).
- Hansen, P.S.; Brix, T.H.; Sørensen, T.I.A.; Kyvik, K.O.; Hegedüs, L. Major genetic influence on the regulation of the pituitary-thyroid axis: A study of healthy danish twins. J. Clin. Endocrinol. Metab. 2004, 89, 1181–1187. [Google Scholar] [CrossRef]
- Panicker, V.; Wilson, S.G.; Spector, T.D.; Brown, S.J.; Falchi, M.; Richards, J.B.; Surdulescu, G.L.; Lim, E.M.; Fletcher, S.J.; Walsh, J.P. Heritability of serum TSH, free T4 and free T3 concentrations: A study of a large UK twin cohort. Clin. Endocrinol. 2008, 68, 652–659. [Google Scholar] [CrossRef]
- Chaker, L.; Korevaar, T.I.M.; Medici, M.; Uitterlinden, A.G.; Hofman, A.; Dehghan, A.; Franco, O.H.; Peeters, R.P. Thyroid function characteristics and determinants: The Rotterdam study. Thyroid 2016, 26, 1195–1204. [Google Scholar] [CrossRef]
- Song, Q.; Chen, X.; Su, Y.; Xie, Z.; Wang, S.; Cui, B. Age and gender specific thyroid hormones and their relationships with body mass index in a large chinese population. Int. J. Endocrinol. Metab. 2019, 17, e66450. [Google Scholar] [CrossRef] [PubMed]
- Knezevic, J.; Starchl, C.; Berisha, A.T.; Amrein, K. Thyroid-gut-axis: How does the microbiota influence thyroid function? Nutrients 2020, 12, 1769. [Google Scholar] [CrossRef] [PubMed]
- Helmreich, D.L.; Parfitt, D.B.; Lu, X.Y.; Akil, H.; Watson, S.J. Relation between the Hypothalamic-Pituitary-Thyroid (HPT) axis and the Hypothalamic-Pituitary-Adrenal (HPA) axis during repeated stress. Neuroendocrinology 2005, 81, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Montanelli, L.; Benvenga, S.; Hegedüs, L.; Vitti, P.; Latrofa, F.; Duntas, L.H. Drugs and other substances interfering with thyroid function. In Thyroid Diseases. Endocrinology; Vitti, P., Hegedüs, L., Eds.; Springer: Cham, Switzerland, 2018; pp. 733–761. [Google Scholar]
- Gore, A.C.; Chappell, V.A.; Fenton, S.E.; Flaws, J.A.; Nadal, A.; Prins, G.S.; Toppari, J.; Zoeller, R.T. EDC-2: The endocrine society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev. 2015, 36, E1–E150. [Google Scholar] [CrossRef] [PubMed]
- Otun, J.; Sahebkar, A.; Östlundh, L.; Atkin, S.L.; Sathyapalan, T. Systematic review and meta-analysis on the effect of soy on thyroid function. Sci. Rep. 2019, 9, 3964. [Google Scholar] [CrossRef]
- Dai, H.; Zhang, L.; Han, X.; Zhao, H.; Guo, J.; Li, Z.; Yang, A. Body mass index (BMI) is associated with serum thyroid stimulating hormone (TSH) level in infertile women: A cross-sectional study. Endocr. J. 2020, 67, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Gruppen, E.G.; Kootstra-Ros, J.; Kobold, A.M.; Connelly, M.A.; Touw, D.; Bos, J.H.J.; Hak, E.; Links, T.P.; Bakker, S.J.L.; Dullaart, R.P.F. Cigarette smoking is associated with higher thyroid hormone and lower TSH levels: The PREVEND study. Endocrine 2020, 67, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Medici, M.; Visser, T.J.; Peeters, R.P. Genetics of thyroid function. Best Pract. Res. Clin. Endocrinol. Metab. 2017, 31, 129–142. [Google Scholar] [CrossRef]
- Gunjača, I.; Matana, A.; Boutin, T.; Torlak, V.; Punda, A.; Polašek, O.; Boraska Perica, V.; Hayward, C.; Zemunik, T.; Barbalić, M. Genome-wide association meta-analysis for total thyroid hormone levels in Croatian population. J. Hum. Genet. 2019, 64, 473–480. [Google Scholar] [CrossRef]
- Popović, M.; Matana, A.; Torlak, V.; Boutin, T.; Brdar, D.; Gunjača, I.; Kaličanin, D.; Kolčić, I.; Boraska Perica, V.; Punda, A.; et al. Genome-wide meta-analysis identifies novel loci associated with free triiodothyronine and thyroid-stimulating hormone. J. Endocrinol. Investig. 2019, 42, 1171–1180. [Google Scholar] [CrossRef]
- Kus, A.; Chaker, L.; Teumer, A.; Peeters, R.P.; Medici, M. The genetic basis of thyroid function: Novel findings and new approaches. J. Clin. Endocrinol. Metab. 2020, 105, dgz225. [Google Scholar] [CrossRef]
- Kadkhodazadeh, H.; Amouzegar, A.; Mehran, L.; Gharibzadeh, S.; Azizi, F.; Tohidi, M. Smoking status and changes in thyroid-stimulating hormone and free thyroxine levels during a decade of follow-up: The Tehran thyroid study. Casp. J. Intern. Med. 2020, 11, 47–52. [Google Scholar] [CrossRef]
- Vejbjerg, P.; Knudsen, N.; Perrild, H.; Carlé, A.; Laurberg, P.; Pedersen, I.B.; Rasmussen, L.B.; Ovesen, L.; Jørgensen, T. The impact of smoking on thyroid volume and function in relation to a shift towards iodine sufficiency. Eur. J. Epidemiol. 2008, 23, 423–429. [Google Scholar] [CrossRef]
- Nyrnes, A.; Jorde, R.; Sundsfjord, J. Serum TSH is positively associated with BMI. Int. J. Obes. 2006, 30, 100–105. [Google Scholar] [CrossRef]
- Belin, R.M.; Astor, B.C.; Powe, N.R.; Ladenson, P.W. Smoke exposure is associated with a lower prevalence of serum thyroid autoantibodies and thyrotropin concentration elevation and a higher prevalence of mild thyrotropin concentration suppression in the Third National Health and Nutrition Examination Surve. J. Clin. Endocrinol. Metab. 2004, 89, 6077–6086. [Google Scholar] [CrossRef]
- Åsvold, B.O.; Bjøro, T.; Nilsen, T.I.L.; Vatten, L.J. Tobacco smoking and thyroid function: A population-based study. Arch. Intern. Med. 2007, 167, 1428–1432. [Google Scholar] [CrossRef] [PubMed]
- Cho, N.H.; Choi, H.S.; Kim, K.W.; Kim, H.-L.; Lee, S.-Y.; Choi, S.H.; Lim, S.; Park, Y.J.; Park, D.J.; Jang, H.C.; et al. Interaction between cigarette smoking and iodine-intake and their impact on thyroid function. Clin. Endocrinol. 2010, 73, 264–270. [Google Scholar] [CrossRef]
- Zhang, Y.; Shi, L.; Zhang, Q.; Peng, N.; Chen, L.; Lian, X.; Liu, C.; Shan, Z.; Shi, B.; Tong, N.; et al. The association between cigarette smoking and serum thyroid stimulating hormone, thyroid peroxidase antibodies and thyroglobulin antibodies levels in Chinese residents: A cross-sectional study in 10 cities. PLoS ONE 2019, 14, e0225435. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kim, M.J.; Yoon, S.G.; Myong, J.P.; Yu, H.W.; Chai, Y.J.; Choi, J.Y.; Lee, K.E. Impact of smoking on thyroid gland: Dose-related effect of urinary cotinine levels on thyroid function and thyroid autoimmunity. Sci. Rep. 2019, 9, 4213. [Google Scholar] [CrossRef] [PubMed]
- Fukayama, H.; Nasu, M.; Murakami, S.; Sugawara, M. Examination of antithyroid effects of smoking products in cultured thyroid follicles: Only thiocyanate is a potent antithyroid agent. Acta Endocrinol. 1992, 127, 520–525. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Langer, P. Extrathyroidal effect of thiocyanate and propylthiouracil: The depression of the protein-bound iodine level in intact and thyroidectomized rats. J. Endocrinol. 1971, 50, 367–372. [Google Scholar] [CrossRef]
- Wiersinga, W.M. Smoking and thyroid. Clin. Endocrinol. 2013, 79, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E.; Haymond, M.W.; Santiago, J.V.; Shah, S.D. Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events. N. Engl. J. Med. 1976, 295, 573–577. [Google Scholar] [CrossRef]
- Melander, A.; Westgren, U.; Ericson, L.E.; Sundler, F. Influence of the sympathetic nervous system on the secretion and metabolism of thyroid hormone. Endocrinology 1977, 101, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Filis, P.; Hombach-Klonisch, S.; Ayotte, P.; Nagrath, N.; Soffientini, U.; Klonisch, T.; O’Shaughnessy, P.; Fowler, P.A. Maternal smoking and high BMI disrupt thyroid gland development. BMC Med. 2018, 16, 194. [Google Scholar] [CrossRef]
- Balhara, Y.S.; Deb, K. Impact of alcohol use on thyroid function. Indian J. Endocrinol. Metab. 2013, 17, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Hegedüs, L.; Rasmussen, N.; Ravn, V.; Kastrup, J.; Krogsgaard, K.; Aldershvile, J. Independent effects of liver disease and chronic alcoholism on thyroid function and size: The possibility of a toxic effect of alcohol on the thyroid gland. Metabolism 1988, 37, 229–233. [Google Scholar] [CrossRef]
- Heinz, A.; Bauer, M.; Kuhn, S.; Krüger, F.; Gräf, K.J.; Rommelspacher, H.; Schmidt, L.G. Long-term observation of the hypgthalamic-pituitary-thyroid (HPT) axis in alcohol-dependent patients. Acta Psychiatr. Scand. 1996, 93, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Liappas, I.; Piperi, C.; Malitas, P.; Tzavellas, E.; Zisaki, A.; Liappas, A.; Kalofoutis, C.; Boufidou, F.; Bagos, P.; Rabavilas, A.; et al. Interrelationship of hepatic function, thyroid activity and mood status in alcohol-dependent individuals. In Vivo 2006, 20, 293–300. [Google Scholar]
- Ozsoy, S.; Esel, E.; Izgi, H.B.; Sofuoglu, S. Thyroid function in early and late alcohol withdrawal: Relationship with aggression, family history, and onset age of alcoholism. Alcohol Alcohol. 2006, 41, 515–521. [Google Scholar] [CrossRef]
- Valeix, P.; Faure, P.; Bertrais, S.; Vergnaud, A.C.; Dauchet, L.; Hercberg, S. Effects of light to moderate alcohol consumption on thyroid volume and thyroid function. Clin. Endocrinol. 2008, 68, 988–995. [Google Scholar] [CrossRef]
- Hegedüs, L. Decreased Thyroid gland volume in Alcoholic cirrhosis of the liver. J. Clin. Endocrinol. Metab. 1984, 58, 930–933. [Google Scholar] [CrossRef]
- Geurts, J.; Demeester-Mirkine, N.; Glinoer, D.; Prigogine, T.; Fernandez-Deville, M.; Corvilain, J. Alterations in circulating thyroid hormones and thyroxine binding globulin in chronic alcoholism. Clin. Endocrinol. 1981, 14, 113–118. [Google Scholar] [CrossRef]
- Anderson, D.L.; Nelson, J.C.; Haviland, M.G.; MacMurray, J.P.; Cummings, M.A.; McGhee, W.H.; Hubbard, R.W. Thyroid stimulating hormone and prolactin responses to thyrotropin releasing hormone in nondepressed alcoholic inpatients. Psychiatry Res. 1992, 43, 121–128. [Google Scholar] [CrossRef]
- Hegedüs, L.; Kastrup, J.; Feldt-Rasmussen, U.; Petersen, P. Serum thyroglobulin in acute and chronic liver disease. Clin. Endocrinol. 1983, 19, 231–237. [Google Scholar] [CrossRef]
- Aoun, E.G.; Lee, M.R.; Haass-Koffler, C.L.; Swift, R.M.; Addolorato, G.; Kenna, G.A.; Leggio, L. Relationship between the thyroid axis and alcohol craving. Alcohol Alcohol. 2015, 50, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Välimäki, M.; Pelkonen, R.; Härkönen, M.; Ylikahri, R. Hormonal changes in noncirrhotic male alcoholics during ethanol withdrawal. Alcohol Alcohol. 1984, 19, 235–242. [Google Scholar]
- Müller, N.; Hoehe, M.; Klein, H.E.; Nieberle, G.; Kapfhammer, H.P.; May, F.; Müller, O.A.; Fichter, M. Endocrinological studies in alcoholics during withdrawal and after abstinence. Psychoneuroendocrinology 1989, 14, 113–123. [Google Scholar] [CrossRef]
- Pienaar, W.; Roberts, M.; Emsley, R.; Aalbers, C.; Taljaard, F. The thyrotropin releasing hormone stimulation test in alcoholism. Alcohol Alcohol. 1995, 30, 661–667. [Google Scholar] [PubMed]
- Zoeller, R.T.; Fletcher, D.L.; Simonyi, A.; Rudeen, P.K. Chronic ethanol treatment reduces the responsiveness of the hypothalamic-pituitary-thyroid axis to central stimulation. Alcohol. Clin. Exp. Res. 1996, 20, 954–960. [Google Scholar] [CrossRef]
- Sheppard, M.C.; Shennan, K.I.J. Desensitization of rat anterior pituitary gland to thyrotrophin releasing hormone. J. Endocrinol. 1984, 101, 101–105. [Google Scholar] [CrossRef]
- Hermann, D.; Heinz, A.; Mann, K. Dysregulation of the hypothalamic-pituitary-thyroid axis in alcoholism. Addiction 2002, 97, 1369–1381. [Google Scholar] [CrossRef]
- Oliveira, K.J.; Chiamolera, M.I.; Giannocco, G.; Pazos-Moura, C.C.; Ortiga-Carvalho, T.M. Thyroid function disruptors: From nature to chemicals. J. Mol. Endocrinol. 2019, 62, R1–R19. [Google Scholar] [CrossRef]
- Åsvold, B.O.; Bjøro, T.; Vatten, L.J. Association of serum TSH with high body mass differs between smokers and never-smokers. J. Clin. Endocrinol. Metab. 2009, 94, 5023–5027. [Google Scholar] [CrossRef]
- Lundbäck, V.; Ekbom, K.; Hagman, E.; Dahlman, I.; Marcus, C. Thyroid-stimulating hormone, degree of obesity, and metabolic risk markers in a cohort of swedish children with obesity. Horm. Res. Paediatr. 2017, 88, 140–146. [Google Scholar] [CrossRef]
- Knudsen, N.; Laurberg, P.; Rasmussen, L.B.; Bülow, I.; Perrild, H.; Ovesen, L.; Jørgensen, T. Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population. J. Clin. Endocrinol. Metab. 2005, 90, 4019–4024. [Google Scholar] [CrossRef]
- Wolffenbuttel, B.H.R.; Wouters, H.J.C.M.; Slagter, S.N.; van Waateringe, R.P.; Muller Kobold, A.C.; van Vliet-Ostaptchouk, J.V.; Links, T.P.; van der Klauw, M.M. Thyroid function and metabolic syndrome in the population-based LifeLines cohort study. BMC Endocr. Disord. 2017, 17, 65. [Google Scholar] [CrossRef] [PubMed]
- De Pergola, G.; Ciampolillo, A.; Paolotti, S.; Trerotoli, P.; Giorgino, R. Free triiodothyronine and thyroid stimulating hormone are directly associated with waist circumference, independently of insulin resistance, metabolic parameters and blood pressure in overweight and obese women. Clin. Endocrinol. 2007, 67, 265–269. [Google Scholar] [CrossRef]
- Grandone, A.; Santoro, N.; Coppola, F.; Calabrò, P.; Perrone, L.; del Giudice, E.M. Thyroid function derangement and childhood obesity: An Italian experience. BMC Endocr. Disord. 2010, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Marras, V.; Casini, M.R.; Pilia, S.; Carta, D.; Civolani, P.; Porcu, M.; Uccheddu, A.P.; Loche, S. Thyroid function in obese children and adolescents. Horm. Res. Paediatr. 2010, 73, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Roef, G.L.; Rietzschel, E.R.; Van Daele, C.M.; Taes, Y.E.; De Buyzere, M.L.; Gillebert, T.C.; Kaufman, J.M. Triiodothyronine and free thyroxine levels are differentially associated with metabolic profile and adiposity-related cardiovascular risk markers in euthyroid middle-aged subjects. Thyroid 2014, 24, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.N.; Richmond, R.; Davies, N.; Sayers, A.; Stevenson, K.; Woltersdorf, W.; Taylor, A.; Groom, A.; Northstone, K.; Ring, S.; et al. Paradoxical relationship between body mass index and thyroid hormone levels: A study using mendelian randomization. J. Clin. Endocrinol. Metab. 2016, 101, 730–738. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Aypak, C.; Turedi, Ö.; Yüce, A.; Görpelioǧlu, S. Thyroid-stimulating hormone (TSH) level in nutritionally obese children and metabolic co-morbidity. J. Pediatr. Endocrinol. Metab. 2013, 26, 703–708. [Google Scholar] [CrossRef]
- Habib, A.; Molayemat, M.; Habib, A. Elevated serum TSH concentrations are associated with higher BMI Z-scores in southern Iranian children and adolescents. Thyroid Res. 2020, 13, 9. [Google Scholar] [CrossRef] [PubMed]
- Makepeace, A.E.; Bremner, A.P.; O’Leary, P.; Leedman, P.J.; Feddema, P.; Michelangeli, V.; Walsh, J.P. Significant inverse relationship between serum free T4 concentration and body mass index in euthyroid subjects: Differences between smokers and nonsmokers. Clin. Endocrinol. 2008, 69, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Huang, F.; Zhang, S.; Lv, Y.; Liu, Q. Thyroid function, body mass index, and metabolic risk markers in euthyroid adults: A cohort study. BMC Endocr. Disord. 2019, 19, 58. [Google Scholar] [CrossRef] [PubMed]
- Tarcin, O.; Abanonu, G.B.; Yazici, D.; Tarcin, O. Association of metabolic syndrome parameters with TT3 and FT3/FT4 ratio in obese Turkish population. Metab. Syndr. Relat. Disord. 2012, 10, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Milionis, A.; Milionis, C. Correlation between body mass index and thyroid function in euthyroid individuals in Greece. ISRN Biomark. 2013, 2013, 651494. [Google Scholar] [CrossRef]
- Ghergherehchi, R.; Hazhir, N. Thyroid hormonal status among children with obesity. Ther. Adv. Endocrinol. Metab. 2015, 6, 51–55. [Google Scholar] [CrossRef]
- Sanyal, D.; Raychaudhuri, M. Hypothyroidism and obesity: An intriguing link. Indian J. Endocrinol. Metab. 2016, 20, 554–557. [Google Scholar] [CrossRef]
- Flier, J.S.; Harris, M.; Hollenberg, A.N. Leptin, nutrition, and the thyroid: The why, the wherefore, and the wiring. J. Clin. Investig. 2000, 105, 859–861. [Google Scholar] [CrossRef]
- Paul, R.; Hassan, M.; Nazar, H.; Gillani, S.; Afzal, N.; Qayyum, I. Effect of body mass index on serum leptin levels. J. Ayub Med. Coll Abbottabad 2011, 23, 40–43. [Google Scholar]
- Krotkiewski, M. Thyroid hormones in the pathogenesis and treatment of obesity. Eur. J. Pharmacol. 2002, 440, 85–98. [Google Scholar] [CrossRef]
- Reinehr, T. Obesity and thyroid function. Mol. Cell. Endocrinol. 2010, 316, 165–171. [Google Scholar] [CrossRef]
- Burman, K.D.; Latham, K.R.; Djuh, Y.Y.; Smallridge, R.C.; Tseng, Y.C.L.; Lukes, Y.G.; Maunder, R.; Wartofsky, L. Solubilized nuclear thyroid hormone receptors in circulating human mononuclear cells. J. Clin. Endocrinol. Metab. 1980, 51, 106–116. [Google Scholar] [CrossRef]
- Biban, B.G.; Lichiardopol, C. Iodine deficiency, still a global problem? Curr. Health Sci. J. 2017, 43, 103–111. [Google Scholar] [CrossRef]
- Sullivan, K.M. The challenges of implementing and monitoring of salt iodisation programmes. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 101–106. [Google Scholar] [CrossRef]
- Román, G.C. Autism: Transient in utero hypothyroxinemia related to maternal flavonoid ingestion during pregnancy and to other environmental antithyroid agents. J. Neurol. Sci. 2007, 262, 15–26. [Google Scholar] [CrossRef]
- De Souza dos Santos, M.C.; Gonçalves, C.F.L.; Vaisman, M.; Ferreira, A.C.F.; de Carvalho, D.P. Impact of flavonoids on thyroid function. Food Chem. Toxicol. 2011, 49, 2495–2502. [Google Scholar] [CrossRef] [PubMed]
- Divi, R.L.; Chang, H.C.; Doerge, D.R. Anti-thyroid isoflavones from soybean. Isolation, characterization, and mechanisms of action. Biochem. Pharmacol. 1997, 54, 1087–1096. [Google Scholar] [CrossRef]
- Divi, R.L.; Doerge, D.R. Inhibition of thyroid peroxidase by dietary flavonoids. Chem. Res. Toxicol. 1996, 9, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.C.; Doerge, D.R. Dietary genistein inactivates rat thyroid peroxidase in vivo without an apparent hypothyroid effect. Toxicol. Appl. Pharmacol. 2000, 168, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Tahboub, R.; Arafah, B.M. Sex steroids and the thyroid. Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 769–780. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, M.G.; Kaplan, J.R.; Appt, S.E.; Register, T.C.; Shively, C.A. Effect of soy isoflavones on thyroid hormones in intact and ovariectomized cynomolgus monkeys (Macaca fascicularis). Menopause 2014, 21, 1136–1142. [Google Scholar] [CrossRef]
- Šošić-Jurjević, B.; Filipović, B.; Wirth, E.K.; Živanović, J.; Radulović, N.; Janković, S.; Milošević, V.; Köhrle, J. Soy isoflavones interfere with thyroid hormone homeostasis in orchidectomized middle-aged rats. Toxicol. Appl. Pharmacol. 2014, 278, 124–134. [Google Scholar] [CrossRef]
- Doerge, D.R.; Woodling, K.A.; Churchwell, M.I.; Fleck, S.C.; Helferich, W.G. Pharmacokinetics of isoflavones from soy infant formula in neonatal and adult rhesus monkeys. Food Chem. Toxicol. 2016, 92, 165–176. [Google Scholar] [CrossRef]
- Hydovitz, J.D. Occurrence of goiter in an infant on a soy diet. N. Engl. J. Med. 1960, 262, 351–353. [Google Scholar] [CrossRef] [PubMed]
- Shepard, T.H.; Pyne, G.E.; Kirschvink, J.F.; McLean, M. Soybean goiter. N. Engl. J. Med. 1960, 262, 1099–1103. [Google Scholar] [CrossRef]
- Ripp, J.A. Soybean-induced goiter. Am. J. Dis. Child. 1961, 102, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Bruce, B.; Messina, M.; Spiller, G.A. Isoflavone supplements do not affect thyroid function in iodine-replete postmenopausal women. J. Med. Food 2003, 6, 309–316. [Google Scholar] [CrossRef]
- Dillingham, B.L.; McVeigh, B.L.; Lampe, J.W.; Duncan, A.M. Soy protein isolates of varied isoflavone content do not influence serum thyroid hormones in healthy young men. Thyroid 2007, 17, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Khaodhiar, L.; Ricciotti, H.; Li, L.; Pan, W.; Schickel, M.; Zhou, J.; Blackburn, G. Daidzein-rich isoflavone aglycones are potentially effective in reducing hot flashes in menopausal women. Menopause 2008, 15, 125–132. [Google Scholar] [CrossRef]
- Bitto, A.; Polito, F.; Atteritano, M.; Altavilla, D.; Mazzaferro, S.; Marini, H.; Adamo, E.B.; D’Anna, R.; Granese, R.; Corrado, F.; et al. Genistein aglycone does not affect thyroid function: Results from a three-year, randomized, double-blind, placebo-controlled trial. J. Clin. Endocrinol. Metab. 2010, 95, 3067–3072. [Google Scholar] [CrossRef]
- Lazarevic, B.; Boezelijn, G.; Diep, L.M.; Kvernrod, K.; Ogren, O.; Ramberg, H.; Moen, A.; Wessel, N.; Berg, R.E.; Egge-Jacobsen, W.; et al. Efficacy and safety of short-term genistein intervention in patients with localized prostate cancer prior to radical prostatectomy: A randomized, placebo-controlled, double-blind phase 2 clinical trial. Nutr. Cancer 2011, 63, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, F.M.; Murray, M.J.; Lewis, R.D.; Cramer, M.A.; Amato, P.; Young, R.L.; Barnes, S.; Konzelmann, K.L.; Fischer, J.G.; Ellis, K.J.; et al. Clinical outcomes of a 2-y soy isoflavone supplementation in menopausal women. Am. J. Clin. Nutr. 2011, 93, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Sathyapalan, T.; Rigby, A.S.; Bhasin, S.; Thatcher, N.J.; Kilpatrick, E.S.; Atkin, S.L. Effect of soy in men with type 2 diabetes mellitus and subclinical hypogonadism: A randomized controlled study. J. Clin. Endocrinol. Metab. 2017, 102, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Sathyapalan, T.; Köhrle, J.; Rijntjes, E.; Rigby, A.S.; Dargham, S.R.; Kilpatrick, E.S.; Atkin, S.L. The effect of high dose isoflavone supplementation on serum reverse T3 in euthyroid men with type 2 diabetes and post-menopausal women. Front. Endocrinol. 2018, 9, 698. [Google Scholar] [CrossRef]
- Persky, V.W.; Turyk, M.E.; Wang, L.; Freels, S.; Chatterton, R.; Barnes, S.; Erdman, J.; Sepkovic, D.W.; Bradlow, H.L.; Potter, S. Effect of soy protein on endogenous hormones in postmenopausal women. Am. J. Clin. Nutr. 2002, 75, 145–153. [Google Scholar] [CrossRef]
- Jayagopal, V.; Albertazzi, P.; Kilpatrick, E.S.; Howarth, E.M.; Jennings, P.E.; Hepburn, D.A.; Atkin, S.L. Beneficial effects of soy phytoestrogen intake in postmenopausal women with type 2 diabetes. Diabetes Care 2002, 25, 1709–1714. [Google Scholar] [CrossRef]
- Duncan, A.M.; Underhill, K.E.W.; Xu, X.; LaValleur, J.; Phipps, W.R.; Kurzer, M.S. Modest hormonal effects of soy isoflavones in postmenopausal women. J. Clin. Endocrinol. Metab. 1999, 84, 3479–3484. [Google Scholar] [CrossRef]
- Mittal, N.; Hota, D.; Dutta, P.; Bhansali, A.; Suri, V.; Aggarwal, N.; Marwah, R.K.; Chakrabarti, A. Evaluation of effect of isoflavone on thyroid economy & autoimmunity in oophorectomised women: A randomised, double-blind, placebo-controlled trial. Indian J. Med. Res. 2011, 133, 633–640. [Google Scholar]
- Hüser, S.; Guth, S.; Joost, H.G.; Soukup, S.T.; Köhrle, J.; Kreienbrock, L.; Diel, P.; Lachenmeier, D.W.; Eisenbrand, G.; Vollmer, G.; et al. Effects of isoflavones on breast tissue and the thyroid hormone system in humans: A comprehensive safety evaluation. Arch. Toxicol. 2018, 92, 2703–2748. [Google Scholar] [CrossRef]
- Felker, P.; Bunch, R.; Leung, A.M. Concentrations of thiocyanate and goitrin in human plasma, their precursor concentrations in brassica vegetables, and associated potential risk for hypothyroidism. Nutr. Rev. 2016, 74, 248–258. [Google Scholar] [CrossRef]
- Babiker, A.; Alawi, A.; Atawi, M.; Alwan, I. The role of micronutrients in thyroid dysfunction. Sudan. J. Paediatr. 2020, 20, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Agerbirk, N.; De Vos, M.; Kim, J.H.; Jander, G. Indole glucosinolate breakdown and its biological effects. Phytochem. Rev. 2009, 8, 101–120. [Google Scholar] [CrossRef]
- Bischoff, K.L. Glucosinolates. In Nutraceuticals: Efficacy, Safety and Toxicity; Elsevier Inc.: Amsterdam, The Netherlands, 2016; pp. 551–554. ISBN 9780128021477. [Google Scholar]
- Tonacchera, M.; Pinchera, A.; Dimida, A.; Ferrarini, E.; Agretti, P.; Vitti, P.; Santini, F.; Crump, K.; Gibbs, J. Relative potencies and additivity of perchlorate, thiocyanate, nitrate, and iodide on the inhibition of radioactive iodide uptake by the human sodium iodide symporter. Thyroid 2004, 14, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Mcmillan, M.; Spinks, E.A.; Fenwick, G.R. Preliminary observations on the effect of dietary brussels sprouts on thyroid function. Hum. Exp. Toxicol. 1986, 5, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Meissner, H.O.; Reich-Bilinska, H.; Mscisz, A.; Kedzia, B. Therapeutic effects of pre-gelatinized maca (Lepidium Peruvianum Chacon) used as a non-hormonal alternative to HRT in perimenopausal women—Clinical pilot study. Int. J. Biomed. Sci. 2006, 2, 143–159. [Google Scholar]
- Chartoumpekis, D.V.; Ziros, P.G.; Chen, J.G.; Groopman, J.D.; Kensler, T.W.; Sykiotis, G.P. Broccoli sprout beverage is safe for thyroid hormonal and autoimmune status: Results of a 12-week randomized trial. Food Chem. Toxicol. 2019, 126, 1–6. [Google Scholar] [CrossRef]
- Pang, K.L.; Lumintang, J.N.; Chin, K.Y. Thyroid-modulating activities of olive and its polyphenols: A systematic review. Nutrients 2021, 13, 529. [Google Scholar] [CrossRef]
- Al-Qarawi, A.A.; Al-Damegh, M.A.; ElMougy, S.A. Effect of freeze dried extract of Olea europaea on the pituitary-thyroid axis in rats. Phyther. Res. 2002, 16, 286–287. [Google Scholar] [CrossRef]
- Mahmoudi, A.; Ghorbel, H.; Feki, I.; Bouallagui, Z.; Guermazi, F.; Ayadi, L.; Sayadi, S. Oleuropein and hydroxytyrosol protect rats’ pups against bisphenol A induced hypothyroidism. Biomed. Pharmacother. 2018, 103, 1115–1126. [Google Scholar] [CrossRef] [PubMed]
- Mekircha, F.; Chebab, S.; Gabbianelli, R.; Leghouchi, E. The possible ameliorative effect of Olea europaea L. oil against deltamethrin-induced oxidative stress and alterations of serum concentrations of thyroid and reproductive hormones in adult female rats. Ecotoxicol. Environ. Saf. 2018, 161, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Quitete, F.T.; Lisboa, P.C.; de Moura, E.G.; de Oliveira, E. Different oils used as supplement during lactation causes endocrine-metabolic dysfunctions in male rats. J. Funct. Foods 2018, 48, 43–53. [Google Scholar] [CrossRef]
- Oke, O.E.; Emeshili, U.K.; Iyasere, O.S.; Abioja, M.O.; Daramola, J.O.; Ladokun, A.O.; Abiona, J.A.; Williams, T.J.; Rahman, S.A.; Rotimi, S.O.; et al. Physiological responses and performance of broiler chickens offered olive leaf extract under a hot humid tropical climate. J. Appl. Poult. Res. 2017, 26, 376–382. [Google Scholar] [CrossRef]
- Ahmed, M.; El-Saadany, A.; Shreif, E.; El-Barbary, A. Effect of dietary olive leaves extract (oleuropein) supplementation on productive, physiological and immunological parameters in bandarah chickens 2-during production period. Egypt. Poult. Sci. J. 2018, 37, 277–292. [Google Scholar]
- Abd-Alla, O.; Abdel-Samee, A.; EL-Adawy, S. Effect of acacia saligna and olive pulp on growth, biochemical and hormonal status in lambs under heat stress in Sinai province. SCVMJ 2007, 7, 129–138. [Google Scholar]
- Farooq, M.; Ali, S.; Zubair, M.; Ullah, Q.; Jamil, H.; Haroon, M.; Ghaffar, A. Effect of feed supplementation with olive oil on serum testosterone, triiodothyronine, thyroxine and some biochemical metabolites in teddy goat bucks. Asian J. Agric. Biol. 2019, 7, 116–121. [Google Scholar] [CrossRef][Green Version]
- Abdalla, E.; El-Masry, K.A.; Khalil, F.A.; Teama, F.E.; Emara, S.S. Alleviation of oxidative stress by using olive pomace in crossbred (Brown Swiss X Baladi) calves under hot environmental conditions. Arab J. Nucl. Sci. Appl. 2015, 47, 88–99. [Google Scholar]
- Zupo, R.; Castellana, F.; Panza, F.; Lampignano, L.; Murro, I.; Di Noia, C.; Triggiani, V.; Giannelli, G.; Sardone, R.; De Pergola, G. Adherence to a mediterranean diet and thyroid function in obesity: A cross-sectional Apulian survey. Nutrients 2020, 12, 3173. [Google Scholar] [CrossRef] [PubMed]
- Gaitan, E.; Lindsay, R.H.; Reichert, R.D.; Ingbarf, S.H.; Cooksey, R.C.; Legan, J.; Meydrech, E.F.; Hill, J.; Kubota, K. Antithyroid and goitrogenic effects of millet: Role of C-Glycosylflavones. J. Clin. Endocrinol. Metab. 1989, 68, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Gaitan, E.; Cooksey, R.C.; Legan, J.; Lindsay, R.H. Antithyroid effects in vivo and in vitro of vitexin: A C-glucosylflavone in millet. J. Clin. Endocrinol. Metab. 1995, 80, 1144–1147. [Google Scholar] [CrossRef]
- Elnour, A.; Liedén, S.Å.; Bourdoux, P.; Eltom, M.; Khalid, S.A.; Hambraeus, L. Traditional fermentation increases goitrogenic activity in pearl millet. Ann. Nutr. Metab. 1998, 42, 341–349. [Google Scholar] [CrossRef]
- Abdel Gadir, W.; Adam, S. Effects of pearl millet (Pennisetum typhoides), and fermented and processed fermented millet on Nubian goats. Vet. Hum. Toxicol. 2000, 42, 133–136. [Google Scholar] [PubMed]
- Moreno-Reyes, R.; Boelaert, M.; El Badawi, S.; Eltom, M.; Vanderpas, J.B. Endemic juvenile hypothyroidism in a severe endemic goitre area of Sudan. Clin. Endocrinol. 1993, 38, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Brahmbhatt, S.; Fearnley, R.; Brahmbhatt, R.; Eastman, C.; Boyages, S. Study of biochemical prevalence indicators for the assessment of iodine deficiency disorders in adults at field conditions in Gujarat (India). Asia Pac. J. Clin. Nutr. 2001, 10, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Sartelet, H.; Serghat, S.; Lobstein, A.; Ingenbleek, Y.; Anton, R.; Petitfrère, E.; Aguie-Aguie, G.; Martiny, L.; Haye, B. Flavonoids extracted from fonio millet (Digitaria exilis) reveal potent antithyroid properties. Nutrition 1996, 12, 100–106. [Google Scholar] [CrossRef]
- Delange, F.; Ermans, A.M. Role of a dietary goitrogen in the etiology of endemic goiter on Idjwi Island. Am. J. Clin. Nutr. 1971, 24, 1354–1360. [Google Scholar] [CrossRef]
- Ermans, A.; Mbulamoko, N.; Delange, F.; Ahluwalia, R. Role of Cassava in the Etiology of Endemic Goitre and Cretinism; IDRC: Ottawa, ON, Canada, 1980. [Google Scholar]
- Delange, F.; Iteke, F.B.; Ermans, A.M. Nutritional factors involved in the goitrogenic action of cassava. J. Nucl. Med. 1983, 24, 90. [Google Scholar]
- Hershman, J.M.; Due, D.T.; Sharp, B.; My, L.; Kent, J.R.; Binh, L.N.; Reed, A.W.; Phuc, L.D.; Herle, A.J.V.; Thai, N.A.; et al. Endemic goiter in Vietnam. J. Clin. Endocrinol. Metab. 1983, 57, 243–249. [Google Scholar] [CrossRef]
- Cliff, J.; Lundquist, P.; Rosling, H.; Sörbo, B.; Wide, L. Thyroid function in a cassava-eating population affected by epidemic spastic paraparesis. Acta Endocrinol. 1986, 113, 523–528. [Google Scholar] [CrossRef]
- Thilly, C.H.; Swennen, B.; Bourdoux, P.; Ntambue, K.; Moreno-Reyes, R.; Gillies, J.; Vanderpas, J.B. The epidemiology of iodine-deficiency disorders in relation to goitrogenic factors and thyroid-stimulating-hormone regulation. Am. J. Clin. Nutr. 1993, 57, 267S–270S. [Google Scholar] [CrossRef]
- Bourdoux, P.; Delange, F.; Gerard, M.; Mafuta, M.; Hanson, A.; Ermans, A.M. Evidence that cassava ingestion increases thiocyanate formation: A possible etiologic factor in endemic goiter. J. Clin. Endocrinol. Metab. 1978, 46, 613–621. [Google Scholar] [CrossRef]
- Kittivachra, R. Effects of cassava on thyroid gland in rats. Thai J. Pharm. Sci. 2007, 30, 57–62. [Google Scholar]
- Chandra, A.K.; Singh, L.H.; Ghosh, S.; Pearce, E.N. Role of bamboo-shoot in the pathogenesis of endemic goiter in Manipur, north east India. Endocr. Pract. 2013, 19, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Singh, L.H.; Chandra, A.K.; Yumnam, S.D.; Sarkar, D.; Manglem, R.K.; Dhabali, T.; Mookerjee, S.; Ray, I. Thiocyanate in excess develops goiter followed by auto immune thyroid diseases even after effective salt iodization in a rural community of north east India. Ecotoxicol. Environ. Saf. 2021, 208, 111711. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, D.; Chandra, A.K.; Chattopadyay, S.; Biswas, M.; Das, S.; Singh, L.H.; Ray, I. Possible mechanism of bamboo shoots (Bambusa balcooa) induced thyroid disruption—An in vitro study. Hum. Exp. Toxicol. 2020, 40, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, D.; Chandra, A.K.; Chakraborty, A.; Ghosh, S.; Chattopadhyay, S.; Singh, L.H.; Ray, I. Effects of bamboo shoots (Bambusa balcooa) on thyroid hormone synthesizing regulatory elements at cellular and molecular levels in thyrocytes. J. Ethnopharmacol. 2020, 250, 112463. [Google Scholar] [CrossRef]
- Xu, D.; Brennan, G.; Xu, L.; Zhang, X.W.; Fan, X.; Han, W.T.; Mock, T.; McMinn, A.; Hutchins, D.A.; Ye, N. Ocean acidification increases iodine accumulation in kelp-based coastal food webs. Glob. Chang. Biol. 2019, 25, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Miyai, K.; Tokushige, T.; Kondo, M.; Kondo, M.; Takahashi, M.; Watanabe, R. Suppression of thyroid function during ingestion of seaweed “Kombu” (Laminaria japonoca) in normal Japanese adults. Endocr. J. 2008, 55, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.D.; Bassett, B.; Burge, M.R. Effects of kelp supplementation on thyroid function in euthyroid subjects. Endocr. Pract. 2003, 9, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Teas, J.; Braverman, L.E.; Kurzer, M.S.; Pino, S.; Hurley, T.G.; Hebert, J.R. Seaweed and soy: Companion foods in Asian cuisine and their effects on thyroid function in American women. J. Med. Food 2007, 10, 90–100. [Google Scholar] [CrossRef]
- Aakre, I.; Evensen, L.T.; Kjellevold, M.; Dahl, L.; Henjum, S.; Alexander, J.; Madsen, L.; Markhus, M.W. Iodine status and thyroid function in a group of seaweed consumers in Norway. Nutrients 2020, 12, 3483. [Google Scholar] [CrossRef]
- Noahsen, P.; Kleist, I.; Larsen, H.M.; Andersen, S. Intake of seaweed as part of a single sushi meal, iodine excretion and thyroid function in euthyroid subjects: A randomized dinner study. J. Endocrinol. Investig. 2020, 43, 431–438. [Google Scholar] [CrossRef]
- Brdar, D.; Gunjača, I.; Pleić, N.; Torlak, V.; Knežević, P.; Punda, A.; Polašek, O.; Hayward, C.; Zemunik, T. The effect of food groups and nutrients on plasma thyroid hormone levels in healthy individuals. Nutrition 2021, in press. [Google Scholar]
- Lambrinakou, S.; Katsa, M.E.; Zyga, S.; Ioannidis, A.; Sachlas, A.; Panoutsopoulos, G.; Pistikou, A.M.; Magana, M.; Kougioumtzi Dimoligianni, D.E.; Kolovos, P.; et al. Correlations between nutrition habits, anxiety and metabolic parameters in Greek healthy adults. In Advances in Experimental Medicine and Biology; Springer LLC: New York, NY, USA, 2017; Volume 987, pp. 23–34. [Google Scholar]
- Cheryl, H. Thyroid disease and diet—Nutrition plays a part in maintaining thyroid health. Today’s Dietit. 2012, 14, 40. [Google Scholar]
- Panda, S.; Kar, A. Piperine lowers the serum concentrations of thyroid hormones, glucose and hepatic 5′D activity in adult male mice. Horm. Metab. Res. 2003, 35, 523–526. [Google Scholar] [CrossRef]
- Gaique, T.G.; Lopes, B.P.; Souza, L.L.; Paula, G.S.M.; Pazos-Moura, C.C.; Oliveira, K.J. Cinnamon intake reduces serum T3 level and modulates tissue-specific expression of thyroid hormone receptor and target genes in rats. J. Sci. Food Agric. 2016, 96, 2889–2895. [Google Scholar] [CrossRef] [PubMed]
- Chandra, A.K.; De, N. Goitrogenic/antithyroidal potential of green tea extract in relation to catechin in rats. Food Chem. Toxicol. 2010, 48, 2304–2311. [Google Scholar] [CrossRef] [PubMed]
- Chandra, A.K.; De, N.; Choudhury, S.R. Effect of different doses of un-fractionated green and black tea extracts on thyroid physiology. Hum. Exp. Toxicol. 2011, 30, 884–896. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, Y.; Mikuriya, H.; Tayama, K.; Takahashi, H.; Nagasawa, A.; Yano, N.; Yuzawa, K.; Ogata, A.; Aoki, N. Goitrogenic effects of green tea extract catechins by dietary administration in rats. Arch. Toxicol. 2001, 75, 591–596. [Google Scholar] [CrossRef]
- Satoh, K.; Sakamoto, Y.; Ogata, A.; Nagai, F.; Mikuriya, H.; Numazawa, M.; Yamada, K.; Aoki, N. Inhibition of aromatase activity by green tea extract catechins and their endocrinological effects of oral administration in rats. Food Chem. Toxicol. 2002, 40, 925–933. [Google Scholar] [CrossRef]
- Hu, J.; Webster, D.; Cao, J.; Shao, A. The safety of green tea and green tea extract consumption in adults—Results of a systematic review. Regul. Toxicol. Pharmacol. 2018, 95, 412–433. [Google Scholar] [CrossRef]
- Zhao, Y.G.; Zhang, Y.; Wang, F.L.; Zhou, J.; Zhao, Q.M.; Zeng, X.Q.; Hu, M.Q.; Jin, M.C.; Zhu, Y. Determination of perchlorate from tea leaves using quaternary ammonium modified magnetic carboxyl-carbon nanotubes followed by liquid chromatography-tandem quadrupole mass spectrometry. Talanta 2018, 185, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Shi, Z.; Liu, M.; Liu, S.; Liu, S.; Wang, J. Association between the COMTVal158Met genotype and Alzheimer’s disease in the han chinese population. Dement. Geriatr. Cogn. Dis. Extra 2014, 4, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chen, H.; Zhu, L.; Liu, X.; Lu, C. Accurate, sensitive and rapid determination of perchlorate in tea by hydrophilic interaction chromatography-tandem mass spectrometry. Anal. Methods 2020, 12, 3592–3599. [Google Scholar] [CrossRef] [PubMed]
- Centre for Food Safety of the Food and Environmental Hygiene, Department (FEHD) of the Government of the Hong Kong Special Administrative Region. Chemical Hazard Evaluation, Report No. 59. Perchlorate in Tea and Tea Beverages; Centre for Food Safety of the Food and Environmental Hygiene, Department (FEHD) of the Government of the Hong Kong Special Administrative Region: Hong Kong, 2018; p. 35.
- Benvenga, S.; Bartolone, L.; Pappalardo, M.A.; Russo, A.; Lapa, D.; Giorgianni, G.; Saraceno, G.; Trimarchi, F. Altered intestinal absorption of L-thyroxine caused by coffee. Thyroid 2008, 18, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Clozel, M.; Branchaud, C.L.; Tannenbaum, G.S.; Dussault, J.H.; Aranda, J.V. Effect of caffeine on thyroid and pituitary function in newborn rats. Pediatr. Res. 1983, 17, 592–595. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, W.; Dasenbrock, C.; Ernst, H.; Kamino, K.; Mohr, U. Absence of effect of caffeine on the thyroid in the Syrian golden hamster: Results of a 90-day study. Food Chem. Toxicol. 1996, 34, 153–159. [Google Scholar] [CrossRef]
- Spindel, E.R.; Wurtman, R.J.; McCall, A.; Carr, D.B.; Conley, L.; Griffith, L.; Arnold, M.A. Neuroendocrine effects of caffeine in normal subjects. Clin. Pharmacol. Ther. 1984, 36, 402–407. [Google Scholar] [CrossRef]
- Friedrich, N.; Pietzner, M.; Cannet, C.; Thuesen, B.H.; Hansen, T.; Wallaschofski, H.; Grarup, N.; Skaaby, T.; Budde, K.; Pedersen, O.; et al. Urinary metabolomics reveals glycemic and coffee associated signatures of thyroid function in two population-based cohorts. PLoS ONE 2017, 12, e0173078. [Google Scholar] [CrossRef]
- Pietzner, M.; Homuth, G.; Budde, K.; Lehmphul, I.; Völker, U.; Völzke, H.; Nauck, M.; Köhrle, J.; Friedrich, N. Urine metabolomics by 1H-NMR spectroscopy indicates associations between serum 3,5-T2 Concentrations and intermediary metabolism in euthyroid humans. Eur. Thyroid J. 2015, 4, 92–100. [Google Scholar] [CrossRef]
- Pietzner, M.; Köhrle, J.; Lehmphul, I.; Budde, K.; Kastenmüller, G.; Brabant, G.; Völzke, H.; Artati, A.; Adamski, J.; Völker, U.; et al. A thyroid hormone-independent molecular fingerprint of 3,5-Diiodothyronine suggests a strong relationship with coffee metabolism in humans. Thyroid 2019, 29, 1743–1754. [Google Scholar] [CrossRef]
- Köhrle, J.; Lehmphul, I.; Pietzner, M.; Renko, K.; Rijntjes, E.; Richards, K.; Anselmo, J.; Danielsen, M.; Jonklaas, J. 3,5-T2—A janus-faced thyroid hormone metabolite exerts both canonical T3-mimetic endocrine and intracrine hepatic action. Front. Endocrinol. 2020, 10, 787. [Google Scholar] [CrossRef]
- Berg, J.P.; Liane, K.M.; Bjørhovde, S.B.; Bjøro, T.; Torjesen, P.A.; Haug, E. Vitamin D receptor binding and biological effects of cholecalciferol analogues in rat thyroid cells. J. Steroid Biochem. Mol. Biol. 1994, 50, 145–150. [Google Scholar] [CrossRef]
- Grundmann, M.; von Versen-Höynck, F. Vitamin D—Roles in women’s reproductive health? Reprod. Biol. Endocrinol. 2011, 9, 146. [Google Scholar] [CrossRef]
- Haug, E.; Pedersen, J.I.; Gautvik, K.M. Effects of vitamin D3 metabolites on production of prolactin and growth hormone in rat pituitary cells. Mol. Cell. Endocrinol. 1982, 28, 65–79. [Google Scholar] [CrossRef]
- Wark, J.D.; Tashjian, A.H. Vitamin D stimulates prolactin synthesis by GH4C1 cells incubated in chemically defined medium. Endocrinology 1982, 111, 1755–1757. [Google Scholar] [CrossRef]
- Stumpf, W.E.; Sar, M.; O’Brien, L.P. Vitamin D sites of action in the pituitary studied by combined autoradiography-immunohistochemistry. Histochemistry 1987, 88, 11–16. [Google Scholar] [CrossRef]
- Sar, M.; Stumpf, W.E.; DeLuca, H.F. Thyrotropes in the pituitary are target cells for 1,25 dihydroxy vitamin D3. Cell Tissue Res. 1980, 209, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Clinckspoor, I.; Gérard, A.-C.; Van Sande, J.; Many, M.-C.; Verlinden, L.; Bouillon, R.; Carmeliet, G.; Mathieu, C.; Verstuyf, A.; Decallonne, B. The Vitamin D receptor in thyroid development and function. Eur. Thyroid J. 2012, 1, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Chailurkit, L.O.; Aekplakorn, W.; Ongphiphadhanakul, B. High vitamin D status in younger individuals is associated with low circulatingthyrotropin. Thyroid 2013, 23, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Mackawy, A.M.H.; Al-Ayed, B.M.; Al-Rashidi, B.M. Vitamin D deficiency and its association with thyroid disease. Int. J. Health Sci. 2013, 7, 267–275. [Google Scholar] [CrossRef]
- Bizzaro, G.; Shoenfeld, Y. Vitamin D and autoimmune thyroid diseases: Facts and unresolved questions. Immunol. Res. 2015, 61, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lv, S.; Chen, G.; Gao, C.; He, J.; Zhong, H.; Xu, Y. Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients 2015, 7, 2485–2498. [Google Scholar] [CrossRef] [PubMed]
- D’Aurizio, F.; Villalta, D.; Metus, P.; Doretto, P.; Tozzoli, R. Is vitamin D a player or not in the pathophysiology of autoimmune thyroid diseases? Autoimmun. Rev. 2015, 14, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Talaei, A.; Ghorbani, F.; Asemi, Z. The effects of Vitamin D supplementation on thyroid function in hypothyroid patients: A randomized, double-blind, placebo-controlled trial. Indian J. Endocrinol. Metab. 2018, 22, 584–588. [Google Scholar] [CrossRef]
- Pan, Y.; Zhong, S.; Liu, Q.; Wang, C.-B.; Zhu, W.-H.; Shen, X.-A.; Lu, B.; Shen, L.-W.; Zeng, Y. Investigating the relationship between 25-hydroxyvitamin D and thyroid function in second-trimester pregnant women. Gynecol. Endocrinol. 2018, 34, 345–348. [Google Scholar] [CrossRef]
- Barchetta, I.; Baroni, M.G.; Leonetti, F.; De Bernardinis, M.; Bertoccini, L.; Fontana, M.; Mazzei, E.; Fraioli, A.; Cavallo, M.G. TSH levels are associated with vitamin D status and seasonality in an adult population of euthyroid adults. Clin. Exp. Med. 2015, 15, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, Z.; Sun, M.; Cao, M.; Zhu, Z.; Fu, Q.; Gao, Y.; Mao, J.; Li, Y.; Shi, Y.; et al. Association of high vitamin D status with low circulating thyroid-stimulating hormone independent of thyroid hormone levels in middle-aged and elderly males. Int. J. Endocrinol. 2014, 2014, 631819. [Google Scholar] [CrossRef]
- Mansorian, B.; Attari, M.M.A.; Vahabzadeh, D.; Mohebbi, I. Serum vitamin D level and its relation to thyroid hormone, blood sugar and lipid profiles in Iranian sedentary work staff. Nutr. Hosp. 2018, 35, 1107–1114. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Wegmüller, R.; Zeder, C.; Chaouki, N.; Torresani, T. The effects of vitamin A deficiency and vitamin A supplementation on thyroid function in goitrous children. J. Clin. Endocrinol. Metab. 2004, 89, 5441–5447. [Google Scholar] [CrossRef]
- Hess, S.Y. The impact of common micronutrient deficiencies on iodine and thyroid metabolism: The evidence from human studies. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 117–132. [Google Scholar] [CrossRef]
- Orzechowska-Pawilojc, A.; Sworczak, K.; Lewczuk, A.; Babinska, A. Homocysteine, folate and cobalamin levels in hypothyroid women before and after treatment. Endocr. J. 2007, 54, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Delitala, G.; Rovasio, P.; Lotti, G. Suppression of thyrotropin (TSH) and prolactin (PRL) release by pyridoxine in chronic primary hypothyroidism. J. Clin. Endocrinol. Metab. 1977, 45, 1019–1022. [Google Scholar] [CrossRef]
- Ren, S.G.; Melmed, S. Pyridoxal phosphate inhibits pituitary cell proliferation and hormone secretion. Endocrinology 2006, 147, 3936–3942. [Google Scholar] [CrossRef]
- Singer, E. Effects of vitamin E deficiency on the thyroid gland of the rat. J. Physiol. 1936, 87, 287–290. [Google Scholar] [CrossRef]
- Deshpande, U.; Joseph, L.; Patwardhan, U.; Samuel, A. Effect of antioxidants (vitamin C, E and turmeric extract) on methimazole induced hypothyroidism in rats. Indian J. Exp. Biol. 2002, 40, 735–738. [Google Scholar]
- Guerra, L.N.; Ríos De Molina, M.D.C.; Miler, E.A.; Moiguer, S.; Karner, M.; Burdman, J.A. Antioxidants and methimazole in the treatment of Graves’ disease: Effect on urinary malondialdehyde levels. Clin. Chim. Acta 2005, 352, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Jooste, P.L.; Mabapa, N.S.; Schoeman, S.; Biebinger, R.; Mushaphi, L.F.; Mbhenyane, X. Vitamin A supplementation in iodine-deficient African children decreases thyrotropin stimulation of the thyroid and reduces the goiter rate. Am. J. Clin. Nutr. 2007, 86, 1040–1044. [Google Scholar] [CrossRef] [PubMed]
- Aktaş, H.Ş. Vitamin B12 and Vitamin D levels in patients with autoimmune hypothyroidism and their correlation with anti-thyroid peroxidase antibodies. Med. Princ. Pract. 2020, 29, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Sworczak, K.; Wiśniewski, P. The role of vitamins in the prevention and treatment of thyroid disorders. Endokrynol. Pol. 2011, 62, 340–344. [Google Scholar] [PubMed]
- Winther, K.H.; Rayman, M.P.; Bonnema, S.J.; Hegedüs, L. Selenium in thyroid disorders—Essential knowledge for clinicians. Nat. Rev. Endocrinol. 2020, 16, 165–176. [Google Scholar] [CrossRef]
- Johnson, C.C.; Fordyce, F.M.; Rayman, M.P. Symposium on “Geographical and geological influences on nutrition”: Factors controlling the distribution of selenium in the environment and their impact on health and nutrition. Proc. Nutr. Soc. 2010, 69, 119–132. [Google Scholar] [CrossRef]
- Köhrle, J.; Jakob, F.; Contempré, B.; Dumont, J.E. Selenium, the thyroid, and the endocrine system. Endocr. Rev. 2005, 26, 944–984. [Google Scholar] [CrossRef]
- Schomburg, L. Selenium, selenoproteins and the thyroid gland: Interactions in health and disease. Nat. Rev. Endocrinol. 2012, 8, 160–171. [Google Scholar] [CrossRef]
- Stuss, M.; Michalska-Kasiczak, M.; Sewerynek, E. The role of selenium in thyroid gland pathophysiology. Endokrynol. Pol. 2017, 68, 440–465. [Google Scholar] [CrossRef]
- Contempré, B.; Duale, N.L.; Dumont, J.E.; Ngo, B.; Diplock, A.T.; Vanderpas, J. Effect of selenium supplementation on thyroid hormone metabolism in an iodine and selenium deficient population. Clin. Endocrinol. 1992, 36, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Olivieri, O.; Girelli, D.; Stanzial, A.M.; Rossi, L.; Bassi, A.; Corrocher, R. Selenium, zinc, and thyroid hormones in healthy subjects: Low T3/T4 ratio in the elderly is related to impaired selenium status. Biol. Trace Elem. Res. 1996, 51, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Duffield, A.J.; Thomson, C.D.; Hill, K.E.; Williams, S. An estimation of selenium requirements for New Zealanders. Am. J. Clin. Nutr. 1999, 70, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Rayman, M.P.; Thompson, A.J.; Bekaert, B.; Catterick, J.; Galassini, R.; Hall, E.; Warren-Perry, M.; Beckett, G.J. Randomized controlled trial of the effect of selenium supplementation on thyroid function in the elderly in the United Kingdom. Am. J. Clin. Nutr. 2008, 87, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Hoeg, A.; Gogakos, A.; Murphy, E.; Mueller, S.; Köhrle, J.; Reid, D.M.; Glüer, C.C.; Felsenberg, D.; Roux, C.; Eastell, R.; et al. Bone turnover and bone mineral density are independently related to selenium status in healthy euthyroid postmenopausal women. J. Clin. Endocrinol. Metab. 2012, 97, 4061–4070. [Google Scholar] [CrossRef] [PubMed]
- Winther, K.H.; Bonnema, S.J.; Cold, F.; Debrabant, B.; Nybo, M.; Cold, S.; Hegedüs, L. Does selenium supplementation affect thyroid function? Results froma randomized, controlled, double-blinded trial in a Danish population. Eur. J. Endocrinol. 2015, 172, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Fontenelle, L.C.; Feitosa, M.M.; Freitas, T.E.C.; Severo, J.S.; Morais, J.B.S.; Henriques, G.S.; Oliveira, F.E.; Moita Neto, J.M.; do Nascimento Marreiro, D. Selenium status and its relationship with thyroid hormones in obese women. Clin. Nutr. ESPEN 2021, 41, 398–404. [Google Scholar] [CrossRef]
- Jain, R.B. Thyroid function and serum copper, selenium, and zinc in general U.S. population. Biol. Trace Elem. Res. 2014, 159, 87–98. [Google Scholar] [CrossRef]
- Goldhaber, S.B. Trace element risk assessment: Essentiality vs. toxicity. Regul. Toxicol. Pharmacol. 2003, 38, 232–242. [Google Scholar] [CrossRef]
- Bhattacharya, P.T.; Misra, S.R.; Hussain, M. Nutritional aspects of essential trace elements in oral health and disease: An extensive review. Scientifica 2016, 2016, 5464373. [Google Scholar] [CrossRef]
- Pekary, A.E.; Lukaski, H.C.; Mena, I.; Hershman, J.M. Processing of TRH precursor peptides in rat brain and pituitary is zinc dependent. Peptides 1991, 12, 1025–1032. [Google Scholar] [CrossRef]
- Osterman, A.L.; Grishin, N.V.; Smulevitch, S.V.; Matz, M.V.; Zagnitko, O.P.; Revina, L.P.; Stepanov, V.M. Primary structure of carboxypeptidase T: Delineation of functionally relevant features in Zn-carboxypeptidase family. J. Protein Chem. 1992, 11, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Kralik, A.; Eder, K.; Kirchgessner, M. Influence of zinc and selenium deficiency on parameters relating to thyroid hormone metabolism. Horm. Metab. Res. 1996, 28, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Civitareale, D.; Saiardi, A.; Falasca, P. Purification and characterization of thyroid transcription factor 2. Biochem. J. 1994, 304, 981–985. [Google Scholar] [CrossRef]
- Freake, H.C.; Govoni, K.E.; Guda, K.; Huang, C.; Zinn, S.A. Actions and interactions of thyroid hormone and zinc status in growing rats. J. Nutr. 2001, 131, 1135–1141. [Google Scholar] [CrossRef]
- Talebi, S.; Ghaedi, E.; Sadeghi, E.; Mohammadi, H.; Hadi, A.; Clark, C.C.T.; Askari, G. Trace element status and hypothyroidism: A systematic review and meta-analysis. Biol. Trace Elem. Res. 2020, 197, 1–14. [Google Scholar] [CrossRef]
- Beserra, J.B.; Morais, J.B.S.; Severo, J.S.; Cruz, K.J.C.; De Oliveira, A.R.S.; De Oliveira, F.E.; De Matos Neto, E.M.; Henriques, G.S.; Marreiro, D.D.N. No association between zinc and thyroid activity in obese women. Int. J. Vitam. Nutr. Res. 2021, 91, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Meunier, N.; Beattie, J.H.; Ciarapica, D.; O’Connor, J.M.; Andriollo-Sanchez, M.; Taras, A.; Coudray, C.; Polito, A. Basal metabolic rate and thyroid hormones of late-middle-aged and older human subjects: The ZENITH study. Eur. J. Clin. Nutr. 2005, 59, S53–S57. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ravaglia, G.; Forti, P.; Maioli, F.; Nesi, B.; Pratelli, L.; Savarino, L.; Cucinotta, D.; Cavalli, G. Blood micronutrient and thyroid hormone concentrations in the oldest-old. J. Clin. Endocrinol. Metab. 2000, 85, 2260–2265. [Google Scholar] [CrossRef] [PubMed]
- Ertek, S.; Cicero, A.F.G.; Caglar, O.; Erdogan, G. Relationship between serum zinc levels, thyroid hormones and thyroid volume following successful iodine supplementation. Hormones 2010, 9, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Hess, S.Y.; Zimmermann, M.B.; Arnold, M.; Langhans, W.; Hurrell, R.F. Iron deficiency anemia reduces thyroid peroxidase activity in rats. J. Nutr. 2002, 132, 1951–1955. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; Johnson, P.E.; Lukaski, H.C. In vitro hepatic thyroid hormone deiodination in iron-deficient rats: Effect of dietary fat. Life Sci. 1993, 53, 603–609. [Google Scholar] [CrossRef]
- Surks, M.I. Effect of thyrotropin on thyroidal iodine metabolism during hypoxia. Am. J. Physiol. 1969, 216, 436–439. [Google Scholar] [CrossRef][Green Version]
- Wopereis, D.M.; Du Puy, R.S.; Van Heemst, D.; Walsh, J.P.; Bremner, A.; Bakker, S.J.L.; Bauer, D.C.; Cappola, A.R.; Ceresini, G.; Degryse, J.; et al. The relation between thyroid function and anemia: A pooled analysis of individual participant data. J. Clin. Endocrinol. Metab. 2018, 103, 3658–3667. [Google Scholar] [CrossRef]
- Fu, J.; Yang, A.; Zhao, J.; Zhu, Y.; Gu, Y.; Xu, Y.; Chen, D. The relationship between iron level and thyroid function during the first trimester of pregnancy: A cross-sectional study in Wuxi, China. J. Trace Elem. Med. Biol. 2017, 43, 148–152. [Google Scholar] [CrossRef]
- Isguven, P.; Arslanoglu, I.; Erol, M.; Yildiz, M.; Adal, E.; Erguven, M. Serum levels of ghrelin, leptin, IGF-I, IGFBP-3, insulin, thyroid hormones and cortisol in prepubertal children with iron deficiency. Endocr. J. 2007, 54, 985–990. [Google Scholar] [CrossRef]
- Ipek, I.O.; Kacmaz, E.; Bozaykut, A.; Sezer, R.G.; Seren, L.; Paketci, C. The effect of iron deficiency anemia on plasma thyroid hormone levels in childhood/Cocukluk caginda demir eksikligi anemisinin plazma tiroid hormonlari uzerine etkisi. Turk. Pediatr. Arch. 2011, 46, 129–133. [Google Scholar] [CrossRef]
- Maldonado-Araque, C.; Valdés, S.; Lago-Sampedro, A.; Lillo-Muñoz, J.A.; Garcia-Fuentes, E.; Perez-Valero, V.; Gutierrez-Repiso, C.; Goday, A.; Urrutia, I.; Peláez, L.; et al. Iron deficiency is associated with Hypothyroxinemia and Hypotriiodothyroninemia in the Spanish general adult population: Di@bet.es study. Sci. Rep. 2018, 8, 6571. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Kim, S.C.; Chung, S.; Kim, S.; Yoon, J.W.; Park, Y.J. Exploring the role of copper and selenium in the maintenance of normal thyroid function among healthy Koreans. J. Trace Elem. Med. Biol. 2020, 61, 126558. [Google Scholar] [CrossRef]
- Uriu-Adams, J.Y.; Keen, C.L. Copper, oxidative stress, and human health. Mol. Aspects Med. 2005, 26, 268–298. [Google Scholar] [CrossRef]
- Kazi, T.G.; Kandhro, G.A.; Afridi, H.I.; Kazi, N.; Baig, J.A.; Arain, M.B.; Shah, A.Q.; Syed, N.; Kumar, S.; Kolachi, N.F.; et al. Interaction of copper with iron, iodine, and thyroid hormone status in goitrous patients. Biol. Trace Elem. Res. 2010, 134, 265–279. [Google Scholar] [CrossRef]
- Rasic-Milutinovic, Z.; Jovanovic, D.; Bogdanovic, G.; Trifunovic, J.; Mutic, J. Potential influence of selenium, copper, zinc and cadmium on l-thyroxine substitution in patients with hashimoto thyroiditis and hypothyroidism. Exp. Clin. Endocrinol. Diabetes 2017, 125, 79–85. [Google Scholar] [CrossRef]
- Katagiri, R.; Yuan, X.; Kobayashi, S.; Sasaki, S. Effect of excess iodine intake on thyroid diseases in different populations: A systematic review and meta-analyses including observational studies. PLoS ONE 2017, 12, e0173722. [Google Scholar] [CrossRef]
- Farebrother, J.; Zimmermann, M.B.; Andersson, M. Excess iodine intake: Sources, assessment, and effects on thyroid function. Ann. N. Y. Acad. Sci. 2019, 1446, 44–65. [Google Scholar] [CrossRef]
- Gardbeer, D.F.; Centor, R.M.; Utiger, R.D. Effects of low dose oral iodide supplementation on thyroid function in normal men. Clin. Endocrinol. 1988, 28, 283–288. [Google Scholar] [CrossRef]
- Paul, T.; Meyers, B.; Witorsch, R.J.; Pino, S.; Chipkin, S.; Ingbar, S.H.; Braverman, L.E. The effect of small increases in dietary iodine on thyroid function in euthyroid subjects. Metabolism 1988, 37, 121–124. [Google Scholar] [CrossRef]
- Namba, H.; Yamashita, S.; Kimura, H.; Yokoyama, N.; Usa, T.; Otsuru, A.; Izumi, M.; Nagataki, S. Evidence of thyroid volume increase in normal subjects receiving excess iodide. J. Clin. Endocrinol. Metab. 1993, 76, 605–608. [Google Scholar] [CrossRef]
- Sang, Z.; Wang, P.P.; Yao, Z.; Shen, J.; Halfyard, B.; Tan, L.; Zhao, N.; Wu, Y.; Gao, S.; Tan, J.; et al. Exploration of the safe upper level of iodine intake in euthyroid Chinese adults: A randomized double-blind trial. Am. J. Clin. Nutr. 2012, 95, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Sang, Z.; Shen, J.; Liu, H.; Chen, W.; Zhao, N.; Wei, W.; Zhang, G.; Zhang, W. Prevalence of thyroid dysfunction with adequate and excessive iodine intake in Hebei Province, People’s Republic of China. Public Health Nutr. 2015, 18, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Wan, S.; Jin, B.; Ren, B.; Qu, M.; Wu, H.; Liu, L.; Boah, M.; Shen, H. The Relationship between high iodine consumption and levels of autoimmune thyroiditis-related biomarkers in a Chinese population: A meta-analysis. Biol. Trace Elem. Res. 2020, 196, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Teng, D.; Shi, X.; Li, Y.; Ba, J.; Chen, B.; Du, J.; He, L.; Lai, X.; Li, Y.; et al. The effect of increased iodine intake on serum thyrotropin: A cross-sectional, Chinese nationwide study. Thyroid 2020, 30, 1810–1819. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Isa, A.; de Sousa, G.; Dieffenbach, R.; Andler, W. Thyroid hormones and their relation to weight status. Horm. Res. 2008, 70, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.E.; Desper, P.C.; Shane, S.R.; Flink, E.B. Magnesium metabolism in hyperthyroidism and hypothyroidism. J. Clin. Investig. 1966, 45, 891–900. [Google Scholar] [CrossRef]
- Wang, K.; Wei, H.; Zhang, W.; Li, Z.; Ding, L.; Yu, T.; Tan, L.; Liu, Y.; Liu, T.; Wang, H.; et al. Severely low serum magnesium is associated with increased risks of positive anti-thyroglobulin antibody and hypothyroidism: A cross-sectional study. Sci. Rep. 2018, 8, 9904. [Google Scholar] [CrossRef]
- Ylli, D.; Wartofsky, L. Can we link thyroid status, energy expenditure, and body composition to management of subclinical thyroid dysfunction? J. Clin. Endocrinol. Metab. 2019, 104, 209–212. [Google Scholar] [CrossRef]
- Huang, W.S.; Yu, M.D.; Lee, M.S.; Cheng, C.Y.; Yang, S.P.; Chin, H.M.L.; Wu, S.Y. Effect of treadmill exercise on circulating thyroid hormone measurements. Med. Princ. Pract. 2004, 13, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Benso, A.; Broglio, F.; Aimaretti, G.; Lucatello, B.; Lanfranco, F.; Ghigo, E.; Grottoli, S. Endocrine and metabolic responses to extreme altitude and physical exercise in climbers. Eur. J. Endocrinol. 2007, 157, 733–740. [Google Scholar] [CrossRef]
- Altaye, K.Z.; Mondal, S.; Legesse, K.; Abdulkedir, M. Effects of aerobic exercise on thyroid hormonal change responses among adolescents with intellectual disabilities. BMJ Open Sport Exerc. Med. 2019, 5, 524. [Google Scholar] [CrossRef]
- Ciloglu, F.; Peker, I.; Pehlivan, A.; Karacabey, K.; Ilhan, N.; Sayglin, O.; Ozmerdivenli, R. Exercise intensity and its effects on thyroid hormones. Neuro Endocrinol. Lett. 2005, 26, 830–834. [Google Scholar]
- Roa Dueñas, O.H.; Koolhaas, C.; Voortman, T.; Franco, O.H.; Ikram, M.A.; Peeters, R.P.; Chaker, L. Thyroid function and physical activity: A population-based cohort study. Thyroid 2020, 31, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Kong, E.; Choi, J. Associations of urinary cotinine-verified active and passive smoking with thyroid function: Analysis of population-based nationally representative data. Thyroid 2018, 28, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kim, W.G.; Jeon, M.J.; Kim, M.; Oh, H.S.; Han, M.; Kim, T.Y.; Shong, Y.K.; Kim, W.B. Serum thyroid-stimulating hormone levels and smoking status: Data from the Korean National Health and Nutrition Examination Survey VI. Clin. Endocrinol. 2018, 88, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.J.; Bremner, A.P.; Hadlow, N.C.; Feddema, P.; Leedman, P.J.; O’Leary, P.C.; Walsh, J.P. The log TSH-free T4 relationship in a community-based cohort is nonlinear and is influenced by age, smoking and thyroid peroxidase antibody status. Clin. Endocrinol. 2016, 85, 789–796. [Google Scholar] [CrossRef]
- Jain, R.B. Association between thyroid profile and perfluoroalkyl acids: Data from NHNAES 2007–2008. Environ. Res. 2013, 126, 51–59. [Google Scholar] [CrossRef]
- Mehran, L.; Amouzgar, A.; Delshad, H.; Azizi, F. The Association of cigarette smoking with serum TSH concentration and thyroperoxidase antibody. Exp. Clin. Endocrinol. Diabetes 2012, 120, 80–83. [Google Scholar] [CrossRef]
- De Pergola, G.; Ciampolillo, A.; Alò, D.; Sciaraffia, M.; Guida, P. Free triiodothyronine is associated with smoking habit, independently of obesity, body fat distribution, insulin, and metabolic parameters. J. Endocrinol. Investig. 2010, 33, 815–818. [Google Scholar] [CrossRef]
- Soldin, O.P.; Goughenour, B.E.; Gilbert, S.Z.; Landy, H.J.; Soldin, S.J. Thyroid hormone levels associated with active and passive cigarette smoking. Thyroid 2009, 19, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Jorde, R.; Sundsfjord, J. Serum TSH levels in smokers and non-smokers. The 5th Tromsø study. Exp. Clin. Endocrinol. Diabetes 2006, 114, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.L.; Mannino, D.M.; Herman, W.H.; Frumkin, H. Cigarette smoking and thyroid hormone levels in males. Int. J. Epidemiol. 1997, 26, 972–977. [Google Scholar] [CrossRef]
- Petersen, K.; Lindstedt, G.; Lundberg, P.-A.; Bengtsson, C.; Lapidus, L.; Nyström, E. Thyroid disease in middle-aged and elderly Swedish women: Thyroid-related hormones, thyroid dysfunction and goitre in relation to age and smoking. J. Intern. Med. 1991, 229, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Ericsson, U.-B.; Lindgärde, F. Effects of cigarette smoking on thyroid function and the prevalence of goitre, thyrotoxicosis and autoimmune thyroiditis. J. Intern. Med. 1991, 229, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Karakaya, A.; Tunçel, N.; Alptuna, G.; Koçer, Z.; Erbay, G. Influence of cigarette smoking on thyroid hormone levels. Hum. Exp. Toxicol. 1987, 6, 507–509. [Google Scholar] [CrossRef]
- Hegedüs, L.; Karstrup, S.; Veiergang, D.; Jacobsen, B.; Skovsted, L.; Feldt-Rasmussen, U. High frequency of goitre in cigarette smokers. Clin. Endocrinol. 1985, 22, 287–292. [Google Scholar] [CrossRef]
- Edén, S.; Jagenburg, R.; Lindstedt, G.; Lundberg, P.-A.; Mellström, D. Thyroregulatory changes associated with smoking in 70-year-old men. Clin. Endocrinol. 1984, 21, 605–610. [Google Scholar] [CrossRef]
- Sepkovic, D.; Haley, N.; Wynder, E. Thyroid activity in cigarette smokers. Arch. Intern. Med. 1984, 144, 501–503. [Google Scholar] [CrossRef]
- Christensen, S.B.; Ericsson, U.B.; Janzon, L.; Tibblin, S.; Melander, A. Influence of cigarette smoking on goiter formation, thyroglobulin, and thyroid hormone levels in women. J. Clin. Endocrinol. Metab. 1984, 58, 615–618. [Google Scholar] [CrossRef]
- Layegh, P.; Asadi, A.; Jangjoo, A.; Layegh, P.; Nematy, M.; Salehi, M.; Shamsian, A.; Ranjbar, G. Comparison of thyroid volume, TSH, free t4 and the prevalence of thyroid nodules in obese and non-obese subjects and correlation of these parameters with insulin resistance status. Casp. J. Intern. Med. 2020, 11, 278–282. [Google Scholar] [CrossRef]
- Diniz, M.F.H.S.; Beleigoli, A.M.R.; Benseñor, I.M.; Lotufo, P.A.; Goulart, A.C.; Barreto, S.M. Association between TSH levels within the reference range and adiposity markers at the baseline of the ELSA–Brasil study. PLoS ONE 2020, 15, e0228801. [Google Scholar] [CrossRef] [PubMed]
- Priya, R.; Patel, S.; Dubey, S.S.; Nanda, R.; Mohapatra, E. Association of thyroid function with body mass index in adolescent girls. Indian J. Med. Biochem. 2020, 24, 55–58. [Google Scholar] [CrossRef]
- Kouidrat, Y.; Diouf, M.; Desailloud, R.; Louhou, R. Effects of a diet plus exercise program on thyroid function in patients with obesity. Metab. Open 2019, 2, 100008. [Google Scholar] [CrossRef] [PubMed]
- Ranabir, S.; Archana, N.; Ipsita, R.; Naorem, S.; Prasad, L. Is there a correlation between body mass index and thyroid stimulating hormone? Endocrinol. Int. J. 2019, 7, 151–154. [Google Scholar] [CrossRef]
- Kwon, H.; Cho, J.H.; Lee, D.Y.; Park, S.E.; Park, C.Y.; Lee, W.Y.; Oh, K.W.; Park, S.W.; Rhee, E.J. Association between thyroid hormone levels, body composition and insulin resistance in euthyroid subjects with normal thyroid ultrasound: The Kangbuk Samsung Health study. Clin. Endocrinol. 2018, 89, 649–655. [Google Scholar] [CrossRef]
- Rajini, B.; Haragopal, R. Study on the Association between the serum thyroid stimulating hormone levels and the body mass index. Physiol. Int. J. Contemp. Med. Res. 2018, 5, 2393–2915. [Google Scholar] [CrossRef]
- Chen, J.; Zhou, W.; Pan, F.; Cui, W.; Li, M.; Hu, Y. Age-related change in thyroid-stimulating hormone: A cross-sectional study in healthy euthyroid population. Endocr. J. 2018, 65, 1075–1082. [Google Scholar] [CrossRef]
- Abdi, H.; Kazemian, E.; Gharibzadeh, S.; Amouzegar, A.; Mehran, L.; Tohidi, M.; Rashvandi, Z.; Azizi, F. Association between thyroid function and body mass index: A 10-year follow-up. Ann. Nutr. Metab. 2017, 70, 338–345. [Google Scholar] [CrossRef]
- Reza Rahbar, A.; Kalantarhormozi, M.; Izadi, F.; Arkia, E.; Rashidi, M.; Pourbehi, F.; Daneshifard, F.; Rahbar, A. Relationship between body mass index, waist-to-hip ratio, and serum lipid concentrations and thyroid-stimulating hormone in the euthyroid adult population. Iran. J. Med. Sci. 2017, 42, 301–305. [Google Scholar]
- Ferrannini, E.; Iervasi, G.; Cobb, J.; Ndreu, R.; Nannipieri, M. Insulin resistance and normal thyroid hormone levels: Prospective study and metabolomic analysis. Am. J. Physiol. Metab. 2017, 312, E429–E436. [Google Scholar] [CrossRef] [PubMed]
- Temizkan, S.; Balaforlou, B.; Ozderya, A.; Avci, M.; Aydin, K.; Karaman, S.; Sargin, M. Effects of thyrotrophin, thyroid hormones and thyroid antibodies on metabolic parameters in a euthyroid population with obesity. Clin. Endocrinol. 2016, 85, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Bieler, B.M.; Gaughan, J.; Khan, M.; Rao, G.; Hunter, K.; Morgan, F.H. Lack of an association between BMI and TSH in treated hypothyroid patients and euthyroid controls. Endocr. Pract. 2016, 22, 555–560. [Google Scholar] [CrossRef]
- Bétry, C.; Challan-Belval, M.A.; Bernard, A.; Charrié, A.; Drai, J.; Laville, M.; Thivolet, C.; Disse, E. Increased TSH in obesity: Evidence for a BMI-independent association with leptin. Diabetes Metab. 2015, 41, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Bakiner, O.; Bozkirli, E.; Cavlak, G.; Ozsahin, K.; Ertorer, E. Are plasma thyroid-stimulating hormone levels associated with degree of obesity and metabolic syndrome in euthyroid obese patients? A Turkish cohort study. Int. Sch. Res. Not. 2014, 2014, 803028. [Google Scholar] [CrossRef]
- Sakurai, M.; Nakamura, K.; Miura, K.; Yoshita, K.; Takamura, T.; Nagasawa, S.Y.; Morikawa, Y.; Ishizaki, M.; Kido, T.; Naruse, Y.; et al. Association between a serum thyroid-stimulating hormone concentration within the normal range and indices of obesity in Japanese men and women. Intern. Med. 2014, 53, 669–674. [Google Scholar] [CrossRef]
- Shin, J.A.; Mo, E.Y.; Kim, E.S.; Moon, S.D.; Han, J.H. Association between lower normal free thyroxine concentrations and obesity phenotype in healthy euthyroid subjects. Int. J. Endocrinol. 2014, 2014, 104318. [Google Scholar] [CrossRef]
- Solanki, A.; Bansal, S.; Jindal, S.; Saxena, V.; Shukla, U. Relationship of serum thyroid stimulating hormone with body mass index in healthy adults. Indian J. Endocrinol. Metab. 2013, 17, 167. [Google Scholar] [CrossRef] [PubMed]
- Ittermann, T.; Thamm, M.; Schipf, S.; John, U.; Rettig, R.; Völzke, H. Relationship of smoking and/or passive exposure to tobacco smoke on the association between serum thyrotropin and body mass index in large groups of adolescents and children. Thyroid 2013, 23, 262–268. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Sorice, G.P.; Mezza, T.; Prioletta, A.; Lassandro, A.P.; Pirronti, T.; Della Casa, S.; Pontecorvi, A.; Giaccari, A. High-normal tsh values in obesity: Is it insulin resistance or adipose tissue’s guilt? Obesity 2013, 21, 101–106. [Google Scholar] [CrossRef]
- Ren, R.; Jiang, X.; Zhang, X.; Guan, Q.; Yu, C.; Li, Y.; Gao, L.; Zhang, H.; Zhao, J. Association between thyroid hormones and body fat in euthyroid subjects. Clin. Endocrinol. 2014, 80, 585–590. [Google Scholar] [CrossRef] [PubMed]
- Kitahara, C.M.; Platz, E.A.; Ladenson, P.W.; Mondul, A.M.; Menke, A.; Berrington de González, A. Body fatness and markers of thyroid function among U.S. men and women. PLoS ONE 2012, 7, e34979. [Google Scholar] [CrossRef] [PubMed]
- Díez, J.J.; Iglesias, P. Relationship between thyrotropin and body mass index in euthyroid subjects. Exp. Clin. Endocrinol. Diabetes 2011, 119, 144–150. [Google Scholar] [CrossRef]
- De Moura Souza, A.; Sichieri, R. Relationship between body mass index and thyrotropin in euthyroid women: Differences by smoking, race and menopausal status. Obes. Facts 2011, 4, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Svare, A.; Nilsen, T.I.L.; Bjøro, T.; Åsvold, B.O.; Langhammer, A. Serum TSH related to measures of body mass: Longitudinal data from the HUNT Study, Norway. Clin. Endocrinol. 2011, 74, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Ambrosi, B.; Masserini, B.; Iorio, L.; Delnevo, A.; Malavazos, A.E.; Morricone, L.; Sburlati, L.F.; Orsi, E. Relationship of thyroid function with body mass index and insulin-resistance in euthyroid obese subjects. J. Endocrinol. Investig. 2010, 33, 640–643. [Google Scholar] [CrossRef]
- Alevizaki, M.; Saltiki, K.; Voidonikola, P.; Mantzou, E.; Papamichael, C.; Stamatelopoulos, K. Free thyroxine is an independent predictor of subcutaneous fat in euthyroid individuals. Eur. J. Endocrinol. 2009, 161, 459–465. [Google Scholar] [CrossRef]
- Kim, B.-J.; Kim, T.Y.; Koh, J.-M.; Kim, H.-K.; Park, J.-Y.; Lee, K.-U.; Shong, Y.K.; Kim, W.B. Relationship between serum free T4 (FT4) levels and metabolic syndrome (MS) and its components in healthy euthyroid subjects. Clin. Endocrinol. 2009, 70, 152–160. [Google Scholar] [CrossRef]
- Shon, H.S.; Jung, E.D.; Kim, S.H.; Lee, J.H. Free T4 is negatively correlated with body mass index in euthyroid women. Korean J. Intern. Med. 2008, 23, 53–57. [Google Scholar] [CrossRef]
- Bastemir, M.; Akin, F.; Alkis, E.; Kaptanoglu, B. Obesity is associated with increased serum TSH level, independent of thyroid function. Swiss Med. Wkly. 2007, 137, 431–434. [Google Scholar]
- Chikunguwo, S.; Brethauer, S.; Nirujogi, V.; Pitt, T.; Udomsawaengsup, S.; Chand, B.; Schauer, P. Influence of obesity and surgical weight loss on thyroid hormone levels. Surg. Obes. Relat. Dis. 2007, 3, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, G.; Ribaudo, M.C.; Zappaterreno, A.; Iannucci, C.V.; Leonetti, F. Relationship of thyroid function with body mass index, leptin, insulin sensitivity and adiponectin in euthyroid obese women. Clin. Endocrinol. 2005, 62, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Teng, X.; Wang, W.; Chen, Y.; Yu, X.; Wang, S.; Li, J.; Zhu, L.; Li, C.; Fan, C.; et al. Effects of dietary soy intake on maternal thyroid functions and serum anti-thyroperoxidase antibody level during early pregnancy. J. Med. Food 2011, 14, 543–550. [Google Scholar] [CrossRef]
- Tousen, Y.; Ezaki, J.; Fujii, Y.; Ueno, T.; Nishimuta, M.; Ishimi, Y. Natural S-equol decreases bone resorption in postmenopausal, non-equol-producing Japanese women: A pilot randomized, placebo-controlled trial. Menopause 2011, 18, 563–574. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Alekel, D.L.; Dixon, P.M.; Messina, M.; Reddy, M.B. The effect of soy food intake on mineral status in premenopausal women. J. Women’s Health 2011, 20, 771–780. [Google Scholar] [CrossRef]
- Hooper, L.; Ryder, J.J.; Kurzer, M.S.; Lampe, J.W.; Messina, M.J.; Phipps, W.R.; Cassidy, A. Effects of soy protein and isoflavones on circulating hormone concentrations in pre- and post-menopausal women: A systematic review and meta-analysis. Hum. Reprod. Update 2009, 15, 423–440. [Google Scholar] [CrossRef] [PubMed]
- Ryan-Borchers, T.; Chew, B.; Park, J.S.; McGuire, M.; Fournier, L.; Beerman, K. Effects of dietary and supplemental forms of isoflavones on thyroid function in healthy postmenopausal women. Top. Clin. Nutr. 2008, 23, 13–22. [Google Scholar] [CrossRef]
- Lydeking-Olsen, E.; Beck-Jensen, J.E.; Setchell, K.D.R.; Holm-Jensen, T. Soymilk or progesterone for prevention of bone loss: A 2 year randomized, placebo-controlled trial. Eur. J. Nutr. 2004, 43, 246–257. [Google Scholar] [CrossRef]
- Mackey, R.; Ekangaki, A.; Eden, J.A. The effects of soy protein in women and men with elevated plasma lipids. BioFactors 2000, 12, 251–257. [Google Scholar] [CrossRef]
- Duncan, A.M.; Merz, B.E.; Xu, X.; Nagel, T.C.; Phipps, W.R.; Kurzer, M.S. Soy isoflavones exert modest hormonal effects in premenopausal women1. J. Clin. Endocrinol. Metab. 1999, 84, 192–197. [Google Scholar] [CrossRef]
- Key, T.J.A.; Thorogood, M.; Keenan, J.; Long, A. Raised thyroid stimulating hormone associated with kelp intake in British vegan men. J. Hum. Nutr. Diet. 1992, 5, 323–326. [Google Scholar] [CrossRef]
- Osman, B.; Ng, M.; Bakar, A.; Khalid, B. The effect of cassava leave intake on thyroid hormone and urinary iodine. East. Afr. Med. J. 1993, 70, 314–315. [Google Scholar] [PubMed]
- Verrusio, W.; Magro, V.M.; Renzi, A.; Casciaro, B.; Andreozzi, P.; Cacciafesta, M. Thyroid hormones, metabolic syndrome and Vitamin D in middle-aged and older euthyroid subjects: A preliminary study. Aging Clin. Exp. Res. 2019, 31, 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Cai, J.; Markowitz, M. Absence of a relationship between thyroid hormones and Vitamin D levels. J. Pediatr. Endocrinol. Metab. 2016, 29, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Beukhof, C.M.; Medici, M.; Van Den Beld, A.W.; Hollenbach, B.; Hoeg, A.; Visser, W.E.; De Herder, W.W.; Visser, T.J.; Schomburg, L.; Peeters, R.P. Selenium status is positively associated with bone mineral density in healthy aging European men. PLoS ONE 2016, 11, e0152748. [Google Scholar] [CrossRef]
- Alissa, E.M.; Ahmed, W.H.; Al-ama, N.; Ferns, G.A.A. Selenium status and cardiovascular risk profile in healthy adult Saudi males. Molecules 2009, 14, 141–159. [Google Scholar] [CrossRef] [PubMed]
- Combs, G.F.; Midthune, D.N.; Patterson, K.Y.; Canfield, W.K.; Hill, A.D.; Levander, O.A.; Taylor, P.R.; Moler, J.E.; Patterson, B.H. Effects of selenomethionine supplementation on selenium status and thyroid hormone concentrations in healthy adults. Am. J. Clin. Nutr. 2009, 89, 1808–1814. [Google Scholar] [CrossRef]
- Thomson, C.D.; Campbell, J.M.; Miller, J.; Skeaff, S.A.; Livingstone, V. Selenium and iodine supplementation: Effect on thyroid function of older New Zealanders. Am. J. Clin. Nutr. 2009, 90, 1038–1046. [Google Scholar] [CrossRef]
- Hawkes, W.C.; Keim, N.L.; Diane Richter, B.; Gustafson, M.B.; Gale, B.; Mackey, B.E.; Bonnel, E.L. High-selenium yeast supplementation in free-living North American men: No effect on thyroid hormone metabolism or body composition. J. Trace Elem. Med. Biol. 2008, 22, 131–142. [Google Scholar] [CrossRef]
- Thomson, C.D.; McLachlan, S.K.; Grant, A.M.; Paterson, E.; Lillico, A.J. The effect of selenium on thyroid status in a population with marginal selenium and iodine status. Br. J. Nutr. 2005, 94, 962–968. [Google Scholar] [CrossRef]
- Hawkes, W.C.; Keim, N.L. Dietary selenium intake modulates thyroid hormone and energy metabolism in men. J. Nutr. 2003, 133, 3443–3448. [Google Scholar] [CrossRef]
- Meeker, J.D.; Rossano, M.G.; Protas, B.; Diamond, M.P.; Puscheck, E.; Daly, D.; Paneth, N.; Wirth, J.J. Multiple metals predict prolactin and thyrotropin (TSH) levels in men. Environ. Res. 2009, 109, 869–873. [Google Scholar] [CrossRef]
- Eftekhari, M.H.; Simondon, K.B.; Jalali, M.; Keshavarz, S.A.; Elguero, E.; Eshraghian, M.R.; Saadat, N. Effects of administration of iron, iodine and simultaneous iron-plus-iodine on the thyroid hormone profile in iron-deficient adolescent Iranian girls. Eur. J. Clin. Nutr. 2006, 60, 545–552. [Google Scholar] [CrossRef]
- Beard, J.L.; Borel, M.J.; Derr, J. Impaired thermoregulation and thyroid function in iron-deficiency anemia. Am. J. Clin. Nutr. 1990, 52, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Jia, Q.; Zhang, X.; Guo, B.; Wen, X.; Zhang, F.; Wang, Y.; Wang, J. Epidemiological investigation on thyroid disease among fertile women in different iodine intake areas of Shanxi province. Zhonghua Liu Xing Bing Xue Za Zhi 2014, 35, 45–48. [Google Scholar]
- Loucks, A.B.; Heath, E.M. Induction of low-T3 syndrome in exercising women occurs at a threshold of energy availability. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1994, 266, R817–R822. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, M.; Knizia, K.; Gastmann, U.; Petersen, K.G.; Khalaf, A.N.; Bauer, S.; Kerp, L.; Keul, J. Influence of 6-week, 6 days per week, training on pituitary function in recreational athletes. Br. J. Sports Med. 1993, 27, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B.; Callister, R. Induction and prevention of low-T3 syndrome in exercising women. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1993, 264, R924–R930. [Google Scholar] [CrossRef]
- Liewendahl, K.; Helenius, T.; Näveri, H.; Tikkanen, H. Fatty acid-induced increase in serum dialyzable free thyroxine after physical exercise: Implication for nonthyroidal illness. J. Clin. Endocrinol. Metab. 1992, 74, 1361–1365. [Google Scholar] [CrossRef]
- Premachandra, B.N.; Winder, W.W.; Hickson, R.; Lang, S.; Holloszy, J.O. Circulating reverse triiodothyronine in humans during exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 47, 281–288. [Google Scholar] [CrossRef]
- O’Connell, M.; Robbins, D.C.; Horton, E.S.; Sims, E.A.H.; Danforth, E. Changes in serum concentrations of 3,3′,5′-triiodothyronine and 3,5,3′-triiodothyronine during prolonged moderate exercise. J. Clin. Endocrinol. Metab. 1979, 49, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Mason, J.W.; Hartley, L.H.; Kotchen, T.A.; Wherry, F.E.; Pennington, L.L.; Jones, L.G. Plasma thyroid-stimulating hormone response in anticipation of muscular exercise in the human. J. Clin. Endocrinol. Metab. 1973, 37, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Howdeshell, K.L. A model of the development of the brain as a construct of the thyroid system. Environ. Health Perspect. 2002, 110, 337–348. [Google Scholar] [CrossRef]
- Jacobson, J.L.; Jacobson, S.W. Intellectual impairment in children exposed to polychlorinated biphenyls in utero. N. Engl. J. Med. 1996, 335, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Ha, E.H.; Kim, E.J.; Park, H.; Ha, M.; Kim, J.H.; Hong, Y.C.; Chang, N.; Kim, B.N. Prenatal exposure to phthalates and infant development at 6 months: Prospective mothers and children’s environmental health (MOCEH) study. Environ. Health Perspect. 2011, 119, 1495–1500. [Google Scholar] [CrossRef] [PubMed]
- Koopman-Esseboom, C.; Weisglas-Kuperus, N.; de Ridder, M.A.J.; Van der Paauw, C.G.; Tuinstra, L.G.M.T.; Sauer, P.J.J. Effects of polychlorinated biphenyl/dioxin exposure and feeding type on infants’ mental and psychomotor development. Pediatrics 1996, 97, 700–706. [Google Scholar]
- Gascon, M.; Fort, M.; Martínez, D.; Carsin, A.E.; Forns, J.; Grimalt, J.O.; Marina, L.S.; Lertxundi, N.; Sunyer, J.; Vrijheid, M. Polybrominated diphenyl ethers (PBDEs) in breast milk and neuropsychological development in infants. Environ. Health Perspect. 2012, 120, 1760–1765. [Google Scholar] [CrossRef]
- Patandin, S.; Lanting, C.I.; Mulder, P.G.H.; Boersma, E.R.; Sauer, P.J.J.; Weisglas-Kuperus, N. Effects of environmental exposure to polychlorinated biphenyls and dioxins on cognitive abilities in Dutch children at 42 months of age. J. Pediatr. 1999, 134, 33–41. [Google Scholar] [CrossRef]
- Gascon, M.; Vrijheid, M.; Martínez, D.; Forns, J.; Grimalt, J.O.; Torrent, M.; Sunyer, J. Effects of pre and postnatal exposure to low levels of polybromodiphenyl ethers on neurodevelopment and thyroid hormone levels at 4 years of age. Environ. Int. 2011, 37, 605–611. [Google Scholar] [CrossRef]
- You, S.H.; Gauger, K.J.; Bansal, R.; Zoeller, R.T. 4-Hydroxy-PCB106 acts as a direct thyroid hormone receptor agonist in rat GH3 cells. Mol. Cell. Endocrinol. 2006, 257–258, 26–34. [Google Scholar] [CrossRef]
- Allen-Rowlands, C.F.; Castracane, V.D.; Hamilton, M.G.; Seifter, J. Effect of polybrominated biphenyls (PBB) on the pituitary-thyroid axis of the rat. Proc. Soc. Exp. Biol. Med. 1981, 166, 506–514. [Google Scholar] [CrossRef]
- Porta, M.; Zumeta, E. Implementing the Stockholm treaty on persistent organic pollutants. Occup. Environ. Med. 2002, 59, 651–652. [Google Scholar] [CrossRef]
- Hagmar, L.; Rylander, L.; Dyremark, E.; Klasson-Wehler, E.; Erfurth, E.M. Plasma concentrations of persistent organochlorines in relation to thyrotropin and thyroid hormone levels in women. Int. Arch. Occup. Environ. Health 2001, 74, 184–188. [Google Scholar] [CrossRef]
- Steuerwald, C.; Weihe, P.; Jørgensen, P.J.; Bjerve, K.; Brock, J.; Heinzow, B.; Budtz-Jørgensen, E.; Grandjean, P. Maternal seafood diet, methylmercury exposure, and neonatal neurologic function. J. Pediatr. 2000, 136, 599–605. [Google Scholar] [CrossRef]
- Rylander, L.; Wallin, E.; Jönssson, B.A.; Stridsberg, M.; Erfurth, E.M.; Hagmar, L. Associations between CB-153 and p,p′-DDE and hormone levels in serum in middle-aged and elderly men. Chemosphere 2006, 65, 375–381. [Google Scholar] [CrossRef]
- Langer, P.; Kočan, A.; Tajtaková, M.; Petrík, J.; Chovancová, J.; Drobná, B.; Jursa, S.; Rádiková, Ž.; Koška, J.; Kšinantová, L.; et al. Fish from industrially polluted freshwater as the main source of organochlorinated pollutants and increased frequency of thyroid disorders and dysglycemia. Chemosphere 2007, 67, S379–S385. [Google Scholar] [CrossRef]
- Meeker, J.D.; Altshul, L.; Hauser, R. Serum PCBs, p,p′-DDE and HCB predict thyroid hormone levels in men. Environ. Res. 2007, 104, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Dallaire, R.; Dewailly, É.; Pereg, D.; Dery, S.; Ayotte, P. Thyroid function and plasma concentrations of polyhalogenated compounds in inuit adults. Environ. Health Perspect. 2009, 117, 1380–1386. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S.; Bloom, M.S.; Yucel, R.; Seegal, R.F.; Wu, Q.; Kannan, K.; Rej, R.; Fitzgerald, E.F. Perfluoroalkyl substances and thyroid function in older adults. Environ. Int. 2015, 75, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Gaum, P.M.; Lang, J.; Esser, A.; Schettgen, T.; Neulen, J.; Kraus, T.; Gube, M. Exposure to polychlorinated biphenyls and the thyroid gland—Examining and discussing possible longitudinal health effects in humans. Environ. Res. 2016, 148, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, M.H.; Darrow, L.A.; Barr, D.B.; Howards, P.P.; Lyles, R.H.; Terrell, M.L.; Smith, A.K.; Conneely, K.N.; Marder, M.E.; Marcus, M. Serum polybrominated biphenyls (PBBs) and polychlorinated biphenyls (PCBs) and thyroid function among michigan adults several decades after the 1973–1974 pbb contamination of livestock feed. Environ. Health Perspect. 2017, 125, 097020. [Google Scholar] [CrossRef]
- Zheng, J.; He, C.T.; Chen, S.J.; Yan, X.; Guo, M.N.; Wang, M.H.; Yu, Y.J.; Yang, Z.Y.; Mai, B.X. Disruption of thyroid hormone (TH) levels and TH-regulated gene expression by polybrominated diphenyl ethers (PBDEs), polychlorinated biphenyls (PCBs), and hydroxylated PCBs in e-waste recycling workers. Environ. Int. 2017, 102, 138–144. [Google Scholar] [CrossRef]
- Curtis, S.W.; Terrell, M.L.; Jacobson, M.H.; Cobb, D.O.; Jiang, V.S.; Neblett, M.F.; Gerkowicz, S.A.; Spencer, J.B.; Marder, M.E.; Barr, D.B.; et al. Thyroid hormone levels associate with exposure to polychlorinated biphenyls and polybrominated biphenyls in adults exposed as children. Environ. Health Glob. Access Sci. Source 2019, 18, 75. [Google Scholar] [CrossRef]
- Emmett, E.A. Polychlorinated biphenyl exposure and effects in transformer repair workers. Environ. Health Perspect. 1985, 60, 185–192. [Google Scholar] [CrossRef]
- Abdelouahab, N.; Mergler, D.; Takser, L.; Vanier, C.; St-Jean, M.; Baldwin, M.; Spear, P.A.; Chan, H.M. Gender differences in the effects of organochlorines, mercury, and lead on thyroid hormone levels in lakeside communities of Quebec (Canada). Environ. Res. 2008, 107, 380–392. [Google Scholar] [CrossRef] [PubMed]
- Turyk, M.E.; Anderson, H.A.; Freels, S.; Chatterton, R.; Needham, L.L.; Patterson, D.G.; Steenport, D.N.; Knobeloch, L.; Imm, P.; Persky, V.W. Associations of organochlorines with endogenous hormones in male Great Lakes fish consumers and nonconsumers. Environ. Res. 2006, 102, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, A.; Nomiyama, K.; Minh Tue, N.; Trang, P.T.K.; Hung Viet, P.; Takahashi, S.; Tanabe, S. Residue profiles of organohalogen compounds in human serum from e-waste recycling sites in North Vietnam: Association with thyroid hormone levels. Environ. Res. 2015, 137, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Hagmar, L.; Björk, J.; Sjödin, A.; Bergman, Å.; Erfurth, E.M. Plasma levels of persistent organohalogens and hormone levels in adult male humans. Arch. Environ. Health 2001, 56, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Persky, V.; Turyk, M.; Anderson, H.A.; Hanrahan, L.P.; Falk, C.; Steenport, D.N.; Chatterton, R.; Freels, S. The effects of PCB exposure and fish consumption on endogenous hormones. Environ. Health Perspect. 2001, 109, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Turyk, M.E.; Anderson, H.A.; Persky, V.W. Relationships of thyroid hormones with polychlorinated biphenyls, dioxins, furans, and DDE in adults. Environ. Health Perspect. 2007, 115, 1197–1203. [Google Scholar] [CrossRef]
- Bahn, A.K.; Mills, J.L.; Snyder, P.J.; Gann, P.H.; Houten, L.; Bialik, O.; Hollmann, L.; Utiger, R.D. Hypothyroidism in workers exposed to polybrominated biphenyls. N. Engl. J. Med. 1980, 302, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Yard, E.E.; Terrell, M.L.; Hunt, D.R.; Cameron, L.L.; Small, C.M.; McGeehin, M.A.; Marcus, M. Incidence of thyroid disease following exposure to polybrominated biphenyls and polychlorinated biphenyls, Michigan, 1974–2006. Chemosphere 2011, 84, 863–868. [Google Scholar] [CrossRef] [PubMed]
- Gorini, F.; Iervasi, G.; Coi, A.; Pitto, L.; Bianchi, F. The role of polybrominated diphenyl ethers in thyroid carcinogenesis: Is it a weak hypothesis or a hidden reality? From facts to new perspectives. Int. J. Environ. Res. Public Health 2018, 15, 1834. [Google Scholar] [CrossRef] [PubMed]
- Bloom, M.; Spliethoff, H.; Vena, J.; Shaver, S.; Addink, R.; Eadon, G. Environmental exposure to PBDEs and thyroid function among New York anglers. Environ. Toxicol. Pharmacol. 2008, 25, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Makey, C.M.; McClean, M.D.; Braverman, L.E.; Pearce, E.N.; He, X.M.; Sjödin, A.; Weinberg, J.M.; Webster, T.F. Polybrominated diphenyl ether exposure and thyroid function tests in North American adults. Environ. Health Perspect. 2016, 124, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Byrne, S.C.; Miller, P.; Seguinot-Medina, S.; Waghiyi, V.; Buck, C.L.; Von Hippel, F.A.; Carpenter, D.O. Associations between serum polybrominated diphenyl ethers and thyroid hormones in a cross sectional study of a remote Alaska Native population. Sci. Rep. 2018, 8, 2198. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.; Chen, L.; Chen, D.; Guo, H.; Bi, X.; Ju, Y.; Jiang, P.; Shi, J.; Yu, Z.; Yang, J.; et al. Elevated serum polybrominated diphenyl ethers and thyroid-stimulating hormone associated with lymphocytic micronuclei in Chinese workers from an e-waste dismantling site. Environ. Sci. Technol. 2008, 42, 2195–2200. [Google Scholar] [CrossRef] [PubMed]
- Turyk, M.E.; Persky, V.W.; Imm, P.; Knobeloch, L.; Chatterton, R.; Anderson, H.A. Hormone disruption by PBDEs in adult male sport fish consumers. Environ. Health Perspect. 2008, 116, 1635–1641. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Park, Y.J. Bisphenols and thyroid hormone. Endocrinol. Metab. 2019, 34, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, K.; Tagami, T.; Akamizu, T.; Usui, T.; Saijo, M.; Kanamoto, N.; Hataya, Y.; Shimatsu, A.; Kuzuya, H.; Nakao, K. Thyroid hormone action is disrupted by bisphenol A as an antagonist. J. Clin. Endocrinol. Metab. 2002, 87, 5185–5190. [Google Scholar] [CrossRef]
- Sriphrapradang, C.; Chailurkit, L.O.; Aekplakorn, W.; Ongphiphadhanakul, B. Association between bisphenol A and abnormal free thyroxine level in men. Endocrine 2013, 44, 441–447. [Google Scholar] [CrossRef]
- Metwally, F.; Hasheesh, A.; Zaid, M.; Fattah El Sharkawy, S.; Abd Fattah, F.; Mazhar, M. Bisphenol A levels among workers in plastic processing industry and their relations to thyroid hormones. J. Appl. Pharm. Sci. 2019, 9, 107–111. [Google Scholar]
- Meeker, J.D.; Ferguson, K.K. Relationship between urinary phthalate and bisphenol a concentrations and serum thyroid measures in U.S. adults and adolescents from the national health and nutrition examination survey (NHANES) 2007–2008. Environ. Health Perspect. 2011, 119, 1396–1402. [Google Scholar] [CrossRef]
- Geens, T.; Dirtu, A.C.; Dirinck, E.; Malarvannan, G.; Van Gaal, L.; Jorens, P.G.; Covaci, A. Daily intake of bisphenol A and triclosan and their association with anthropometric data, thyroid hormones and weight loss in overweight and obese individuals. Environ. Int. 2015, 76, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Lu, J.; Xu, M.; Xu, Y.; Li, M.; Liu, Y.; Tian, X.; Chen, Y.; Dai, M.; Wang, W.; et al. Urinary bisphenol a concentration and thyroid function in Chinese adults. Epidemiology 2013, 24, 295–302. [Google Scholar] [CrossRef]
- Park, C.; Choi, W.; Hwang, M.; Lee, Y.; Kim, S.; Yu, S.; Lee, I.; Paek, D.; Choi, K. Associations between urinary phthalate metabolites and bisphenol A levels, and serum thyroid hormones among the Korean adult population—Korean National Environmental Health Survey (KoNEHS) 2012–2014. Sci. Total Environ. 2017, 584–585, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Meeker, J.D.; Calafat, A.M.; Hauser, R. Urinary bisphenol A concentrations in relation to serum thyroid and reproductive hormone levels in men from an infertility clinic. Environ. Sci. Technol. 2010, 44, 1458–1463. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Zhang, Z.; Liu, L.; Li, Y.; Ren, N.; Kannan, K. Occurrence and profiles of phthalates in foodstuffs from China and their implications for human exposure. J. Agric. Food Chem. 2012, 60, 6913–6919. [Google Scholar] [CrossRef] [PubMed]
- Shen, O.; Du, G.; Sun, H.; Wu, W.; Jiang, Y.; Song, L.; Wang, X. Comparison of in vitro hormone activities of selected phthalates using reporter gene assays. Toxicol. Lett. 2009, 191, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Ghisari, M.; Bonefeld-Jorgensen, E.C. Effects of plasticizers and their mixtures on estrogen receptor and thyroid hormone functions. Toxicol. Lett. 2009, 189, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Ha, M.; Yang, M.; Yue, P.; Xie, Z.; Liu, C. Di2-ethylhexyl phthalate disrupts thyroid hormone homeostasis through activating the Ras/Akt/TRHr pathway and inducing hepatic enzymes. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef]
- Meeker, J.D.; Calafat, A.M.; Hauser, R. Di(2-ethylhexyl) Phthalate metabolites may alter thyroid hormone levels in men. Environ. Health Perspect. 2007, 115, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-B.; Pan, W.H.; Chang, J.W.; Chiang, H.C.; Guo, Y.L.; Jaakkola, J.J.K.; Huang, P.C. Does exposure to phthalates influence thyroid function and growth hormone homeostasis? The Taiwan Environmental Survey for Toxicants (TEST) 2013. Environ. Res. 2017, 153, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Dirtu, A.C.; Geens, T.; Dirinck, E.; Malarvannan, G.; Neels, H.; Van Gaal, L.; Jorens, P.G.; Covaci, A. Phthalate metabolites in obese individuals undergoing weight loss: Urinary levels and estimation of the phthalates daily intake. Environ. Int. 2013, 59, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Mendez, W.; Eftim, S.E. Biomarkers of perchlorate exposure are correlated with circulating thyroid hormone levels in the 2007–2008 NHANES. Environ. Res. 2012, 118, 137–144. [Google Scholar] [CrossRef]
- Kim, M.J.; Moon, S.; Oh, B.-C.; Jung, D.; Choi, K.; Park, Y.J. Association between diethylhexyl phthalate exposure and thyroid function: A meta-analysis. Thyroid 2019, 29, 183–192. [Google Scholar] [CrossRef]
- Leung, A.M.; Pearce, E.N.; Braverman, L.E. Environmental perchlorate exposure: Potential adverse thyroid effects. Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 372–376. [Google Scholar] [CrossRef]
- Eskandari, S.; Loo, D.D.F.; Dai, G.; Levy, O.; Wright, E.M.; Carrasco, N. Thyroid Na+/I− symporter. Mechanism, stoichiometry, and specificity. J. Biol. Chem. 1997, 272, 27230–27238. [Google Scholar] [CrossRef]
- Blount, B.C.; Pirkle, J.L.; Osterloh, J.D.; Valentin-Blasini, L.; Caldwell, K.L. Urinary perchlorate and thyroid hormone levels in adolescent and adult men and women living in the United States. Environ. Health Perspect. 2006, 114, 1865–1871. [Google Scholar] [CrossRef]
- Steinmaus, C.; Miller, M.D.; Cushing, L.; Blount, B.C.; Smith, A.H. Combined effects of perchlorate, thiocyanate, and iodine on thyroid function in the National Health and Nutrition Examination Survey 2007–08. Environ. Res. 2013, 123, 17–24. [Google Scholar] [CrossRef]
- Suh, M.; Abraham, L.; Hixon, J.G.; Proctor, D.M. The effects of perchlorate, nitrate, and thiocyanate on free thyroxine for potentially sensitive subpopulations o. The 2001–2002 and 2007–2008 National Health and Nutrition Examination Surveys. J. Expo. Sci. Environ. Epidemiol. 2014, 24, 579–587. [Google Scholar] [CrossRef] [PubMed]
- McMullen, J.; Ghassabian, A.; Kohn, B.; Trasande, L. Identifying subpopulations vulnerable to the thyroid-blocking effects of perchlorateandthiocy anate. J. Clin. Endocrinol. Metab. 2017, 102, 2637–2645. [Google Scholar] [CrossRef] [PubMed]
- Buck, R.C.; Franklin, J.; Berger, U.; Conder, J.M.; Cousins, I.T.; De Voogt, P.; Jensen, A.A.; Kannan, K.; Mabury, S.A.; van Leeuwen, S.P.J. Perfluoroalkyl and polyfluoroalkyl substances in the environment: Terminology, classification, and origins. Integr. Environ. Assess. Manag. 2011, 7, 513–541. [Google Scholar] [CrossRef] [PubMed]
- Coperchini, F.; Awwad, O.; Rotondi, M.; Santini, F.; Imbriani, M.; Chiovato, L. Thyroid disruption by perfluorooctane sulfonate (PFOS) and perfluorooctanoate (PFOA). J. Endocrinol. Investig. 2017, 40, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Emmett, E.A.; Zhang, H.; Shofer, F.S.; Freeman, D.; Rodway, N.V.; Desai, C.; Shaw, L.M. Community exposure to perfluorooctanoate: Relationships between serum levels and certain health parameters. J. Occup. Environ. Med. 2006, 48, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Olsen, G.W.; Zobel, L.R. Assessment of lipid, hepatic, and thyroid parameters with serum perfluorooctanoate (PFOA) concentrations in fluorochemical production workers. Int. Arch. Occup. Environ. Health 2007, 81, 231–246. [Google Scholar] [CrossRef]
- Bloom, M.S.; Kannan, K.; Spliethoff, H.M.; Tao, L.; Aldous, K.M.; Vena, J.E. Exploratory assessment of perfluorinated compounds and human thyroid function. Physiol. Behav. 2010, 99, 240–245. [Google Scholar] [CrossRef]
- Knox, S.S.; Jackson, T.; Frisbee, S.J.; Javins, B.; Ducatman, A.M. Perfluorocarbon exposure, gender and thyroid function in the C8 health project. J. Toxicol. Sci. 2011, 36, 403–410. [Google Scholar] [CrossRef]
- Wen, L.L.; Lin, L.Y.; Su, T.C.; Chen, P.C.; Lin, C.Y. Association between serum perfluorinated chemicals and thyroid function in U.S. Adults: The national health and nutrition examination survey 2007–2010. J. Clin. Endocrinol. Metab. 2013, 98, E1456–E1464. [Google Scholar] [CrossRef]
- Webster, G.M.; Rauch, S.A.; Marie, N.S.; Mattman, A.; Lanphear, B.P.; Venners, S.A. Cross-sectional associations of serum perfluoroalkyl acids and thyroid hormones in U.S. Adults: Variation according to TPOAb and iodine status (NHANES 2007–2008). Environ. Health Perspect. 2016, 124, 935–942. [Google Scholar] [CrossRef]
- Crawford, N.M.; Fenton, S.E.; Strynar, M.; Hines, E.P.; Pritchard, D.A.; Steiner, A.Z. Effects of perfluorinated chemicals on thyroid function, markers of ovarian reserve, and natural fertility. Reprod. Toxicol. 2017, 69, 53–59. [Google Scholar] [CrossRef]
- Sohn, Y.S.; Moon, S.; Park, Y.J. Effect of multiple exposure to perfluorinated chemicals on thyroid function among adults in the US: The National Health and Nutrition Examination Survey 2007–2008 and 2011–2012. Int. J. Thyroidol. 2020, 13, 19–29. [Google Scholar] [CrossRef]
- Li, Y.; Xu, Y.; Fletcher, T.; Scott, K.; Nielsen, C.; Pineda, D.; Lindh, C.H.; Olsson, D.S.; Andersson, E.M.; Jakobsson, K. Associations between perfluoroalkyl substances and thyroid hormones after high exposure through drinking water. Environ. Res. 2021, 194, 110647. [Google Scholar] [CrossRef]
- Van Gerwen, M.; Alpert, N.; Alsen, M.; Ziadkhanpour, K.; Taioli, E.; Genden, E. The impact of smoking on the association between perfluoroalkyl acids (Pfas) and thyroid hormones: A national health and nutrition examination survey analysis. Toxics 2020, 8, 116. [Google Scholar] [CrossRef]
- Kim, M.J.; Moon, S.; Oh, B.C.; Jung, D.; Ji, K.; Choi, K.; Park, Y.J. Association between perfluoroalkyl substances exposure and thyroid function in adults: A meta-analysis. PLoS ONE 2018, 13, e0197244. [Google Scholar] [CrossRef]
- Lewis, R.C.; Johns, L.E.; Meeker, J.D. Serum biomarkers of exposure to perfluoroalkyl substances in relation to serum testosterone and measures of thyroid function among adults and adolescents from NHANES 2011–2012. Int. J. Environ. Res. Public Health 2015, 12, 6098–6114. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Wen, L.L.; Lin, L.Y.; Wen, T.W.; Lien, G.W.; Hsu, S.H.J.; Chien, K.L.; Liao, C.C.; Sung, F.C.; Chen, P.C.; et al. The associations between serum perfluorinated chemicals and thyroid function in adolescents and young adults. J. Hazard. Mater. 2013, 244–245, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Olsen, G.W.; Burris, J.M.; Burlew, M.M.; Mandel, J.H. Epidemiologic assessment of worker serum perfluorooctanesulfonate (PFOS) and perfluorooctanoate (PFOA) concentrations and medical surveillance examinations. J. Occup. Environ. Med. 2003, 45, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Ji, K.; Kim, S.; Kho, Y.; Paek, D.; Sakong, J.; Ha, J.; Kim, S.; Choi, K. Serum concentrations of major perfluorinated compounds among the general population in Korea: Dietary sources and potential impact on thyroid hormones. Environ. Int. 2012, 45, 78–85. [Google Scholar] [CrossRef]
- Byrne, S.C.; Miller, P.; Seguinot-Medina, S.; Waghiyi, V.; Buck, C.L.; Von Hippel, F.A.; Carpenter, D.O. Exposure to perfluoroalkyl substances and associations with serum thyroid hormones in a remote population of Alaska Natives. Environ. Res. 2018, 166, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Campos, É.; Freire, C. Exposure to non-persistent pesticides and thyroid function: A systematic review of epidemiological evidence. Int. J. Hyg. Environ. Health 2016, 219, 481–497. [Google Scholar] [CrossRef]
- Leemans, M.; Couderq, S.; Demeneix, B.; Fini, J.B. Pesticides with potential thyroid hormone-disrupting effects: A review of recent data. Front. Endocrinol. 2019, 10, 743. [Google Scholar] [CrossRef]
- McKinlay, R.; Plant, J.A.; Bell, J.N.B.; Voulvoulis, N. Endocrine disrupting pesticides: Implications for risk assessment. Environ. Int. 2008, 34, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Nankongnab, N.; Kongtip, P.; Kallayanatham, N.; Pundee, R.; Yimsabai, J.; Woskie, S. Longitudinal study of thyroid hormones between conventional and organic farmers in Thailand. Toxics 2020, 8, 82. [Google Scholar] [CrossRef] [PubMed]
- Steenland, K.; Cedillo, L.; Tucker, J.; Hines, C.; Sorensen, K.; Deddens, J.; Cruz, V. Thyroid hormones and cytogenetic outcomes in backpack sprayers using ethylenebis(dithiocarbamate) (EBDC) fungicides in Mexico. Environ. Health Perspect. 1997, 105, 1126–1130. [Google Scholar] [CrossRef] [PubMed]
- Garry, V.F.; Holland, S.E.; Erickson, L.L.; Burroughs, B.L. Male reproductive hormones and thyroid function in pesticide applicators in the Red River Valley of Minnesota. J. Toxicol. Environ. Health Part A 2003, 66, 965–986. [Google Scholar] [CrossRef] [PubMed]
- Meeker, J.D.; Barr, D.B.; Hauser, R. Thyroid hormones in relation to urinary metabolites of non-persistent insecticides in men of reproductive age. Reprod. Toxicol. 2006, 22, 437–442. [Google Scholar] [CrossRef]
- Lacasaña, M.; López-Flores, I.; Rodríguez-Barranco, M.; Aguilar-Garduño, C.; Blanco-Muñoz, J.; Pérez-Méndez, O.; Gamboa, R.; Bassol, S.; Cebrian, M.E. Association between organophosphate pesticides exposure and thyroid hormones in floriculture workers. Toxicol. Appl. Pharmacol. 2010, 243, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Fortenberry, G.Z.; Hu, H.; Turyk, M.; Barr, D.B.; Meeker, J.D. Association between urinary 3, 5, 6-trichloro-2-pyridinol, a metabolite of chlorpyrifos and chlorpyrifos-methyl, and serum T4 and TSH in NHANES 1999–2002. Sci. Total Environ. 2012, 424, 351–355. [Google Scholar] [CrossRef]
- Freire, C.; Koifman, R.J.; Sarcinelli, P.N.; Simões Rosa, A.C.; Clapauch, R.; Koifman, S. Long-term exposure to organochlorine pesticides and thyroid status in adults in a heavily contaminated area in Brazil. Environ. Res. 2013, 127, 7–15. [Google Scholar] [CrossRef]
- Farokhi, F.; Taravati, A. Pesticide exposure and thyroid function in adult male sprayers. Int. J. Med. Investig. 2014, 3, 127–132. [Google Scholar]
- Langer, P.; Tajtaková, M.; Kocan, A.; Vlcek, M.; Petrik, J.; Chovancova, J.; Drobna, B.; Jursa, S.; Pavuk, M.; Trnovec, T.; et al. Multiple organochlorine pollution and the thyroid. Endocr. Regul. 2006, 40, 46–52. [Google Scholar]
- Herin, F.; Boutet-Robinet, E.; Levant, A.; Dulaurent, S.; Manika, M.; Galatry-Bouju, F.; Caron, P.; Soulat, J.M. Thyroid function tests in persons with occupational exposure to fipronil. Thyroid 2011, 21, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Bernieri, T.; Rodrigues, D.; Barbosa, I.R.; Ardenghi, P.G.; Basso da Silva, L. Occupational exposure to pesticides and thyroid function in Brazilian soybean farmers. Chemosphere 2019, 218, 425–429. [Google Scholar] [CrossRef]
- Sala, M.; Sunyer, J.; Herrero, C.; To-Figueras, J.; Grimalt, J. Association between serum concentrations of hexachlorobenzene and polychlorobiphenyls with thyroid hormone and liver enzymes in a sample of the general population. Occup. Environ. Med. 2001, 58, 172–177. [Google Scholar] [CrossRef]
- Langer, P.; Kočan, A.; Tajtáková, M.; Rádiková, Ž.; Petrík, J.; Koška, J.; Kšinantová, L.; Imrich, R.; Hučková, M.; Chovancová, J.; et al. Possible effects of persistent organochlorinated pollutants cocktail on thyroid hormone levels and pituitary-thyroid interrelations. Chemosphere 2007, 70, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Schell, L.M.; Gallo, M.V.; Denham, M.; Ravenscroft, J.; DeCaprio, A.P.; Carpenter, D.O. Relationship of thyroid hormone levels to levels of polychlorinated biphenyls, lead, p,p′-DDE, and other toxicants in Akwesasne Mohawk Youth. Environ. Health Perspect. 2008, 116, 806–813. [Google Scholar] [CrossRef]
- Meeker, J.D.; Barr, D.B.; Hauser, R. Pyrethroid insecticide metabolites are associated with serum hormone levels in adult men. Reprod. Toxicol. 2009, 27, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Miranda-Contreras, L.; Gómez-Pérez, R.; Rojas, G.; Cruz, I.; Berrueta, L.; Salmen, S.; Colmenares, M.; Barreto, S.; Balza, A.; Zavala, L.; et al. Occupational exposure to organophosphate and carbamate pesticides affects sperm chromatin integrity and reproductive hormone levels among venezuelan farm workers. J. Occup. Health 2013, 55, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Khan, D.A.; Ahad, K.; Ansari, W.M.; Khan, H. Pesticide exposure and endocrine dysfunction in the cotton crop agricultural workers of Southern Punjab, Pakistan. Asia-Pac. J. Public Health 2013, 25, 181–191. [Google Scholar] [CrossRef]
- Jain, R. Association between thyroid function and urinary levels of 3,5,6-trichloro-2-pyridinol: Data from NHANES 2007–2008. Environ. Sci. Pollut. Res. 2017, 24, 2820–2826. [Google Scholar] [CrossRef]
- Medda, E.; Santini, F.; De Angelis, S.; Franzellin, F.; Fiumalbi, C.; Perico, A.; Gilardi, E.; Mechi, M.T.; Marsili, A.; Citroni, A.; et al. Iodine nutritional status and thyroid effects of exposure to ethylenebisdithiocarbamates. Environ. Res. 2017, 154, 152–159. [Google Scholar] [CrossRef]
- Hwang, M.; Lee, Y.; Choi, K.; Park, C. Urinary 3-phenoxybenzoic acid levels and the association with thyroid hormones in adults: Korean National Environmental Health Survey 2012–2014. Sci. Total Environ. 2019, 696, 133920. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.B. Variability in the levels of 3-phenoxybenzoic acid by age, gender, and race/ethnicity for the period of 2001–2002 versus 2009–2010 and its association with thyroid function among general US population. Environ. Sci. Pollut. Res. 2016, 23, 6934–6939. [Google Scholar] [CrossRef] [PubMed]
- Panganiban, L.R.; Cortes-Maramba, N.; Dioquino, C.; Suplido, M.L.; Ho, H.; Francisco-Rivera, A.; Manglicmot-Yabes, A. Correlation between blood enthylenethiourea and thyroid gland disorders among banana plantation workers in the Philippines. Environ. Health Perspect. 2004, 112, 42–45. [Google Scholar] [CrossRef]
- Rashidi, M.A.; Mahabadi, H.; Khavanin, A. Evaluation of the effects of chronic exposure to organophosphorus pesticides on thyroid function. Asia Pac. J. Med. Toxicol. 2020, 9, 35–43. [Google Scholar] [CrossRef]
- Toft, G.; Flyvbjerg, A.; Bonde, J.P. Thyroid function in Danish greenhouse workers. Environ. Health Glob. Access Sci. Source 2006, 5, 32. [Google Scholar] [CrossRef]
- Blanco-Muñoz, J.; Lacasaña, M.; López-Flores, I.; Rodríguez-Barranco, M.; González-Alzaga, B.; Bassol, S.; Cebrian, M.E.; López-Carrillo, L.; Aguilar-Garduño, C. Association between organochlorine pesticide exposure and thyroid hormones in floriculture workers. Environ. Res. 2016, 150, 357–363. [Google Scholar] [CrossRef]
- Bloom, M.S.; Jansing, R.L.; Kannan, K.; Rej, R.; Fitzgerald, E.F. Thyroid hormones are associated with exposure to persistent organic pollutants in aging residents of upper Hudson River communities. Int. J. Hyg. Environ. Health 2014, 217, 473–482. [Google Scholar] [CrossRef]
- Santos, R.; Piccoli, C.; Cremonese, C.; Freire, C. Thyroid and reproductive hormones in relation to pesticide use in an agricultural population in Southern Brazil. Environ. Res. 2019, 173, 221–231. [Google Scholar] [CrossRef]
- Zaidi, S.S.; Bhatnagar, V.K.; Gandhi, S.J.; Shah, M.P.; Kulkarni, P.K.; Saiyed, H.N. Assessment of thyroid function in pesticide formulators. Hum. Exp. Toxicol. 2000, 19, 497–501. [Google Scholar] [CrossRef]
- Pelletier, C.; Doucet, E.; Imbeault, P.; Tremblay, A. Associations between weight loss-induced changes in plasma organochlorine concentrations, serum T3 concentration, and resting metabolic rate. Toxicol. Sci. 2002, 67, 46–51. [Google Scholar] [CrossRef]
- García Torres, E.; Pérez Morales, R.; González Zamora, A.; Ríos Sánchez, E.; Olivas Calderón, E.H.; Alba Romero, J.d.J.; Calleros Rincón, E.Y. Consumption of water contaminated by nitrate and its deleterious effects on the human thyroid gland: A review and update. Int. J. Environ. Health Res. 2020, 1–18. [Google Scholar] [CrossRef]
- Ward, M.H.; Kilfoy, B.A.; Weyer, P.J.; Anderson, K.E.; Folsom, A.R.; Cerhan, J.R. Nitrate intake and the risk of thyroid cancer and thyroid disease. Epidemiology 2010, 21, 389–395. [Google Scholar] [CrossRef]
- Aschebrook-Kilfoy, B.; Heltshe, S.L.; Nuckols, J.R.; Sabra, M.M.; Shuldiner, A.R.; Mitchell, B.D.; Airola, M.; Holford, T.R.; Zhang, Y.; Ward, M.H. Modeled nitrate levels in well water supplies and prevalence of abnormal thyroid conditions among the Old Order Amish in Pennsylvania. Environ. Health Glob. Access Sci. Source 2012, 11, 6. [Google Scholar] [CrossRef]
- Van Maanen, J.M.S.; van Dijk, A.; Mulder, K.; de Baets, M.H.; Menheere, P.C.A.; van der Heide, D.; Mertens, P.L.J.M.; Kleinjans, J.C.S. Consumption of drinking water with high nitrate levels causes hypertrophy of the thyroid. Toxicol. Lett. 1994, 72, 365–374. [Google Scholar] [CrossRef]
- Bivolarska, A.V.; Maneva, A.I.; Gatseva, P.D.; Katsarova, M.N. Effect of nitrates, thiocyanates and selenium on the iron and iodine status of postpartum women. Folia Med. 2016, 58, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Lambers, A.; Koppeschaar, H.; van Isselt, J.; Schothorst, R.; Mensinga, T.; Meulenbelt, J. The Effect of Nitrate on the Thyroid Gland Function in Healthy Volunteers in a 4-Week Oral Toxicity Study. Rijksinst voor Volksgezond en Milieu; National Institute fot Public Health and the Environment: Utrecht, The Netherlands, 2000; p. 61. [Google Scholar]
- Dos Santos Pinheiro, V.; Volino-Souza, M.; Vieira de Oliveira, G.; Adam Conte-Junior, C.; Silveira Alvares, T. Effect of high-nitrate beetroot juice consumption on thyroid gland hormones and iodine levels in adults. Food Biosci. 2021, 40, 100869. [Google Scholar] [CrossRef]
- Palazzolo, D.L.; Jansen, K.P. The minimal arsenic concentration required to inhibit the activity of thyroid peroxidase activity in vitro. Biol. Trace Elem. Res. 2008, 126, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, N.; Bhattacharya, S. Thyrotoxicity of the chlorides of cadmium and mercury in rabbit. Biomed. Environ. Sci. 1992, 236–240. [Google Scholar]
- Yoshida, K.; Sugihira, N.; Suzuki, M.; Sakurada, T.; Saito, S.; Yoshinaga, K.; Saito, H. Effect of cadmium on T4 outer ring monodeiodination by rat liver. Environ. Res. 1987, 42, 400–405. [Google Scholar] [CrossRef]
- Chaurasia, S.S.; Gupta, P.; Kar, A.; Maiti, P.K. Lead induced thyroid dysfunction and lipid peroxidation in the fish Clarias batrachus with special reference to hepatic type I-5′-monodeiodinase activity. Bull. Environ. Contam. Toxicol. 1996, 56, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Soldin, O.P.; O’Mara, D.M.; Aschner, M. Thyroid hormones and methylmercury toxicity. Biol. Trace Elem. Res. 2008, 126, 1. [Google Scholar] [CrossRef] [PubMed]
- Ciarrocca, M.; Tomei, F.; Caciari, T.; Cetica, C.; Andrè, J.C.; Fiaschetti, M.; Schifano, M.P.; Scala, B.; Scimitto, L.; Tomei, G.; et al. Exposure to Arsenic in urban and rural areas and effects on thyroid hormones. Inhal. Toxicol. 2012, 24, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Molin, M.; Ulven, S.M.; Dahl, L.; Lundebye, A.K.; Holck, M.; Alexander, J.; Meltzer, H.M.; Ydersbond, T.A. Arsenic in seafood is associated with increased thyroid-stimulating hormone (TSH) in healthy volunteers—A randomized controlled trial. J. Trace Elem. Med. Biol. 2017, 44, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Jain, R. Association between arsenic exposure and thyroid function: Data from NHANES 2007–2010. Int. J. Environ. Health Res. 2016, 26, 101–129. [Google Scholar] [CrossRef]
- Jurdziak, M.; Gać, P.; Poręba, M.; Szymańska-Chabowska, A.; Mazur, G.; Poręba, R. Concentration of thyrotropic hormone in persons occupationally exposed to lead, cadmium and arsenic. Biol. Trace Elem. Res. 2018, 182, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Rosati, M.V.; Montuori, L.; Caciari, T.; Sacco, C.; Marrocco, M.; Tomei, G.; Scala, B.; Sancini, A.; Anzelmo, V.; Bonomi, S.; et al. Correlation between urinary cadmium and thyroid hormones in outdoor workers exposed to urban stressors. Toxicol. Ind. Health 2016, 32, 1978–1986. [Google Scholar] [CrossRef]
- Christensen, Y.K.L. Metals in blood and urine, and thyroid function among adults in the United States 2007–2008. Int. J. Hyg. Environ. Health 2013, 216, 624–632. [Google Scholar] [CrossRef]
- Chen, A.; Kim, S.S.; Chung, E.; Dietrich, K.N. Thyroid hormones in relation to lead, mercury, and cadmium exposure in the national health and nutrition examination survey, 2007–2008. Environ. Health Perspect. 2013, 121, 181–186. [Google Scholar] [CrossRef]
- Luo, J.; Hendryx, M. Relationship between blood cadmium, lead, and serum thyroid measures in US adults—The National Health and Nutrition Examination Survey (NHANES) 2007–2010. Int. J. Environ. Health Res. 2014, 24, 125–136. [Google Scholar] [CrossRef]
- Jain, R.B.; Choi, Y.S. Interacting effects of selected trace and toxic metals on thyroid function. Int. J. Environ. Health Res. 2016, 26, 75–91. [Google Scholar] [CrossRef] [PubMed]
- Mohammed Sherif, M.; Solyman Mohammed, Y.; Abd El-Moaty Zedan, H.; Abd El-hamid Kheder, M.; Hassan Abd EL-Salam Mohammed, A.; Author, C. Toxic Effect of Some Heavy Metals (Cadmium and Lead) on Thyroid Function. Egypt. J. Hosp. Med. 2017, 69, 2512–2515. [Google Scholar] [CrossRef]
- Nie, X.; Chen, Y.; Chen, Y.; Chen, C.; Han, B.; Li, Q.; Zhu, C.; Xia, F.; Zhai, H.; Wang, N.; et al. Lead and cadmium exposure, higher thyroid antibodies and thyroid dysfunction in Chinese women. Environ. Pollut. 2017, 230, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Akgöl, E.; Tutkun, E.; Yilmaz, H.; Yilmaz, F.; Gunduzoz, M.; Bal, C.; Ünlü, A.; Abusoglu, S. Alterations of thyroid hormone levels in cadmium exposure. J. Clin. Anal. Med. 2017, 8, 202–206. [Google Scholar] [CrossRef]
- Chung, S.M.; Moon, J.S.; Yoon, J.S.; Won, K.C.; Lee, H.W. Sex-specific effects of blood cadmium on thyroid hormones and thyroid function status: Korean nationwide cross-sectional study. J. Trace Elem. Med. Biol. 2019, 53, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Nishijo, M.; Nakagawa, H.; Morikawa, Y.; Tabata, M.; Senma, M.; Miura, K.; Tsuritani, I.; Honda, R.; Kido, T.; Teranishi, H.; et al. A study of thyroid hormone levels of inhabitants of the cadmium-polluted Kakehashi River basin. Jpn. J. Hyg. 1994, 49, 598–605. [Google Scholar] [CrossRef][Green Version]
- López, C.M.; Piñeiro, A.E.; Núñez, N.; Avagnina, A.M.; Villaamil, E.C.; Roses, O.E. Thyroid hormone changes in males exposed to lead in the Buenos Aires Area (Argentina). Pharmacol. Res. 2000, 42, 599–602. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Chandran, V.; Bandhu, H.K.; Mittal, B.R.; Bhattacharya, A.; Jindal, S.K.; Varma, S. Impact of lead exposure on pituitary-thyroid axis in humans. BioMetals 2000, 13, 187–192. [Google Scholar] [CrossRef]
- Pekcici, R.; Kavlakoğlu, B.; Yilmaz, S.; Şahin, M.; Delibaşi, T. Effects of lead on thyroid functions in lead-exposed workers. Cent. Eur. J. Med. 2010, 5, 215–218. [Google Scholar] [CrossRef]
- Fahim, Y.A.; Sharaf, N.E.; Hasani, I.W.; Ragab, E.A.; Abdelhakim, H.K. Assessment of thyroid function and oxidative stress state in foundry workers exposed to lead. J. Health Pollut. 2020, 10, 200903. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, C.; Brodkin, C.A.; Alexander, B.; Cullen, M.; Rainey, P.M.; Van Netten, C.; Faustman, E.; Checkoway, H. Thyroid function in lead smelter workers: Absence of subacute or cumulative effects with moderate lead burdens. Int. Arch. Occup. Environ. Health 1998, 71, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Tuppurainen, M.; Wagar, G.; Kurppa, K.; Sakari, W.; Wambugu, A.; Froseth, B.; Alho, J.; Nykyri, E. Thyroid function as assessed by routine laboratory tests of workers with long-term exposure. Scand. J. Work. Environ. Health 1988, 14, 175–180. [Google Scholar] [CrossRef]
- Erfurth, E.M.; Gerhardsson, L.; Nilsson, A.; Rylander, L.; Schütz, A.; Skerfving, S.; Börjesson, J. Effects of lead on the endocrine system in lead smelter workers. Arch. Environ. Health 2001, 56, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Liang, Q.; Liao, R.; Su, S.; Huang, S.; Pan, R.; Huang, J. Effects of lead on thyroid function of occupationally exposed workers. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2003, 21, 111–113. [Google Scholar] [PubMed]
- Dundar, B.; Öktem, F.; Arslan, M.K.; Delibas, N.; Baykal, B.; Arslan, Ç.; Gultepe, M.; Ilhan, I.E. The effect of long-term low-dose lead exposure on thyroid function in adolescents. Environ. Res. 2006, 101, 140–145. [Google Scholar] [CrossRef]
- Soltani, S.; Sharifiyan, A.; Ghasemi, M.; Chavoshi, F.; Sadeghniiat, K.; Bahaedini, L.; Amlnian, O.; Meisami, A.P. Assessment of thyroid function in male workers of battery recycling factory occupationally exposed to lead. J. Pharmacol. Toxicol. 2012, 7, 338–343. [Google Scholar] [CrossRef]
- Krieg, E.F. A meta-analysis of studies investigating the effects of occupational lead exposure on thyroid hormones. Am. J. Ind. Med. 2016, 59, 583–590. [Google Scholar] [CrossRef]
- Dursun, N.; Tutus, A. Chronic occupational lead exposure and thyroid function. J. Trace Elem. Exp. Med. 1999, 12, 45–49. [Google Scholar] [CrossRef]
- Saad-Hussein, A.; Hamdy, H.; Aziz, H.M.; Mahdy-Abdallah, H. Thyroid functions in paints production workers and the mechanism of oxidative-antioxidants status. Toxicol. Ind. Health 2011, 27, 257–263. [Google Scholar] [CrossRef]
- Bledsoe, M.L.; Pinkerton, L.E.; Silver, S.; Deddens, J.A.; Biagini, R.E. Thyroxine and free thyroxine levels in workers occupationally exposed to inorganic lead. Environ. Health Insights 2011, 5, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Correia, M.M.; Chammas, M.C.; Zavariz, J.D.; Arata, A.; Martins, L.C.; Marui, S.; Pereira, L.A.A. Evaluation of the effects of chronic occupational exposure to metallic mercury on the thyroid parenchyma and hormonal function. Int. Arch. Occup. Environ. Health 2020, 93, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Han, X.; Dong, G.; Yan, W.; Wang, X.; Bigambo, F.M.; Fang, K.; Xia, Y.; Chen, T.; Wang, X. Association between mercury exposure and thyroid hormones levels: A meta-analysis. Environ. Res. 2021, 196, 110928. [Google Scholar] [CrossRef]
- Barregard, L.; Lindstedt, G.; Schutz, A.; Sallsten, G. Endocrine function in mercury exposed chloralkali workers. Occup. Environ. Med. 1994, 51, 536–540. [Google Scholar] [CrossRef]
- Afrifa, J.; Ogbordjor, W.D.; Duku-Takyi, R. Variation in thyroid hormone levels is associated with elevated blood mercury levels among artisanal small-scale miners in Ghana. PLoS ONE 2018, 13, e0203335. [Google Scholar] [CrossRef]
- Ellingsen, D.G.; Efskind, J.; Haug, E.; Thomassen, Y.; Martinsen, I.; Gaarder, P.I. Effects of low mercury vapour exposure on the thyroid function in chloralkali workers. J. Appl. Toxicol. 2000, 20, 483–489. [Google Scholar] [CrossRef]
- Rádiková, Ž.; Tajtáková, M.; Kočan, A.; Trnovec, T.; Šeböková, E.; Klimeš, I.; Langer, P. Possible effects of environmental nitrates and toxic organochlorines on human thyroid in highly polluted areas in Slovakia. Thyroid 2008, 18, 353–362. [Google Scholar] [CrossRef]
- Bloom, M.S.; Weiner, J.M.; Vena, J.E.; Beehler, G.P. Exploring associations between serum levels of select organochlorines and thyroxine in a sample of New York state sportsmen: The New York State Angler Cohort study. Environ. Res. 2003, 93, 52–66. [Google Scholar] [CrossRef]
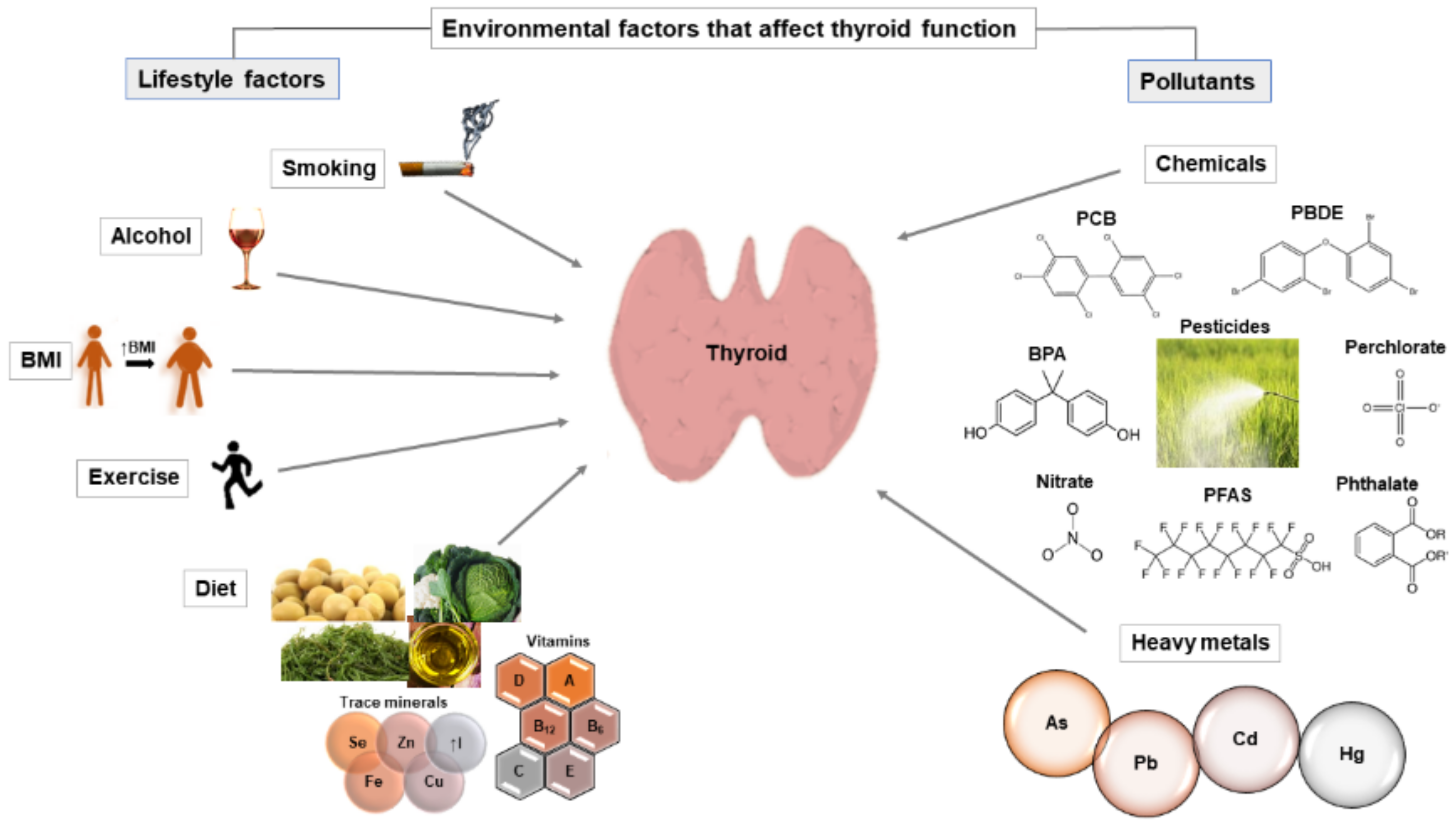
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babić Leko, M.; Gunjača, I.; Pleić, N.; Zemunik, T. Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. Int. J. Mol. Sci. 2021, 22, 6521. https://doi.org/10.3390/ijms22126521
Babić Leko M, Gunjača I, Pleić N, Zemunik T. Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. International Journal of Molecular Sciences. 2021; 22(12):6521. https://doi.org/10.3390/ijms22126521
Chicago/Turabian StyleBabić Leko, Mirjana, Ivana Gunjača, Nikolina Pleić, and Tatijana Zemunik. 2021. "Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels" International Journal of Molecular Sciences 22, no. 12: 6521. https://doi.org/10.3390/ijms22126521
APA StyleBabić Leko, M., Gunjača, I., Pleić, N., & Zemunik, T. (2021). Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. International Journal of Molecular Sciences, 22(12), 6521. https://doi.org/10.3390/ijms22126521







