Long-Lasting Growth Hormone Regulated by the Ubiquitin-Proteasome System
Abstract
1. Introduction
2. Results
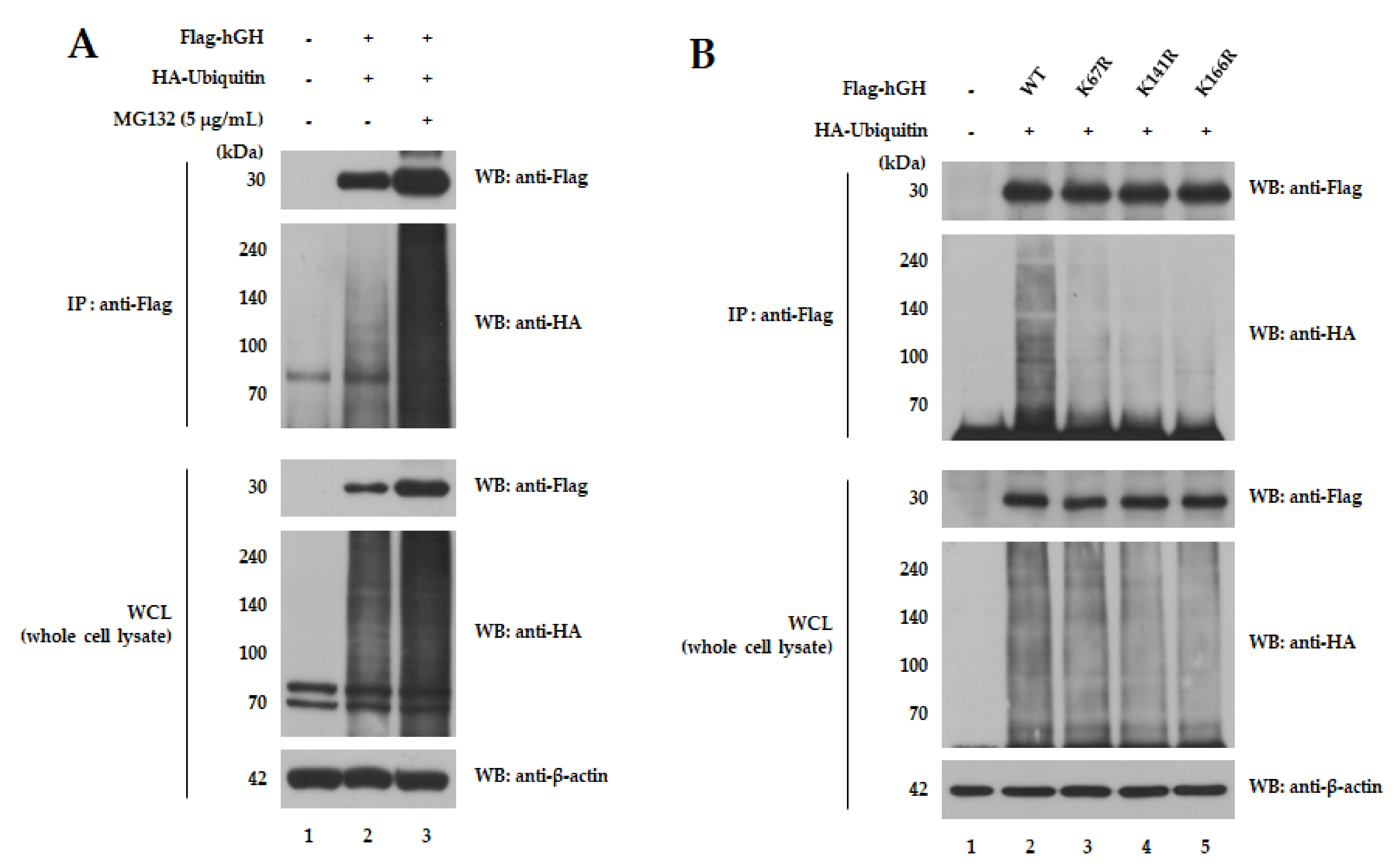
2.1. hGH Mutants Are Less Ubiquitinated
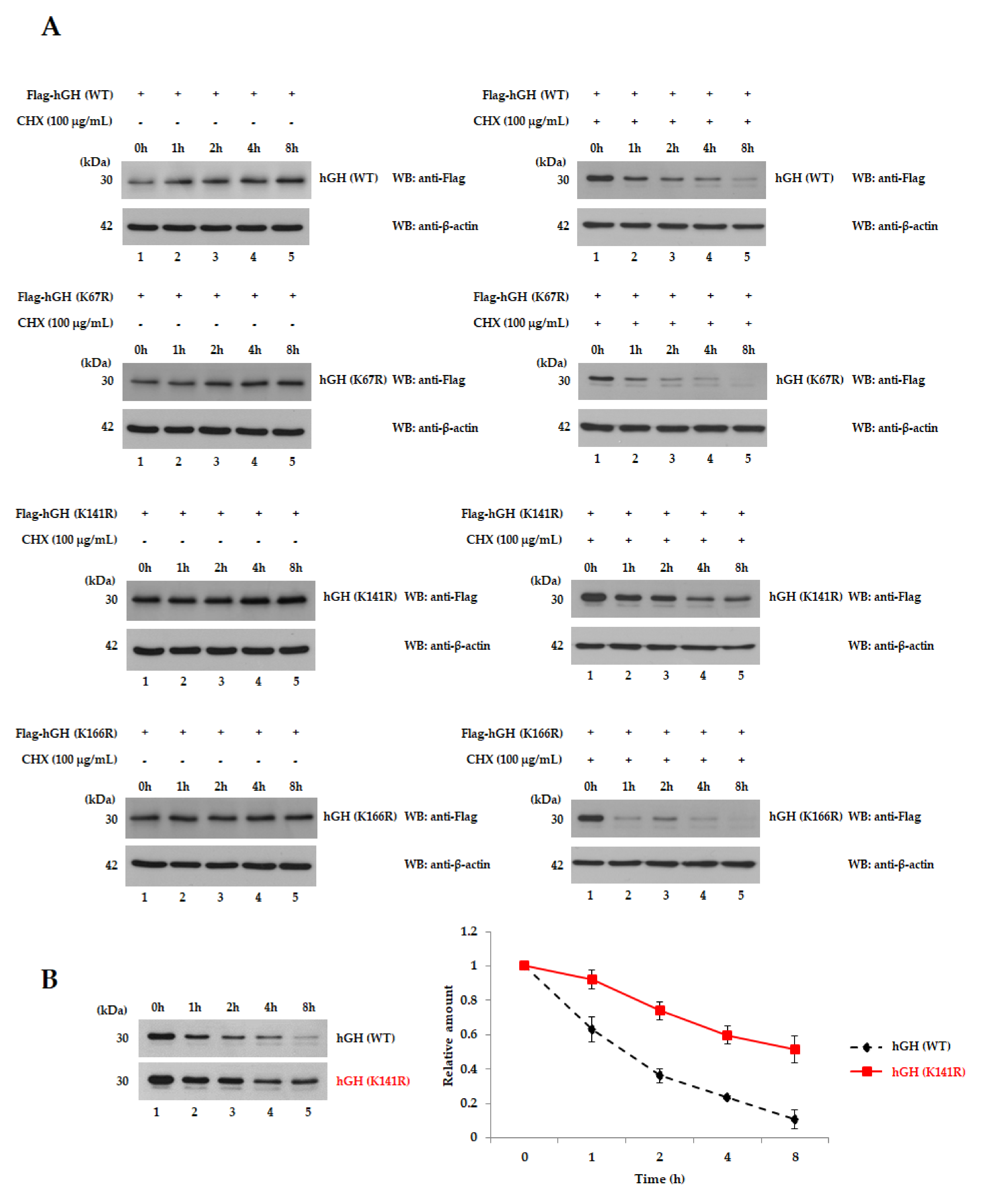
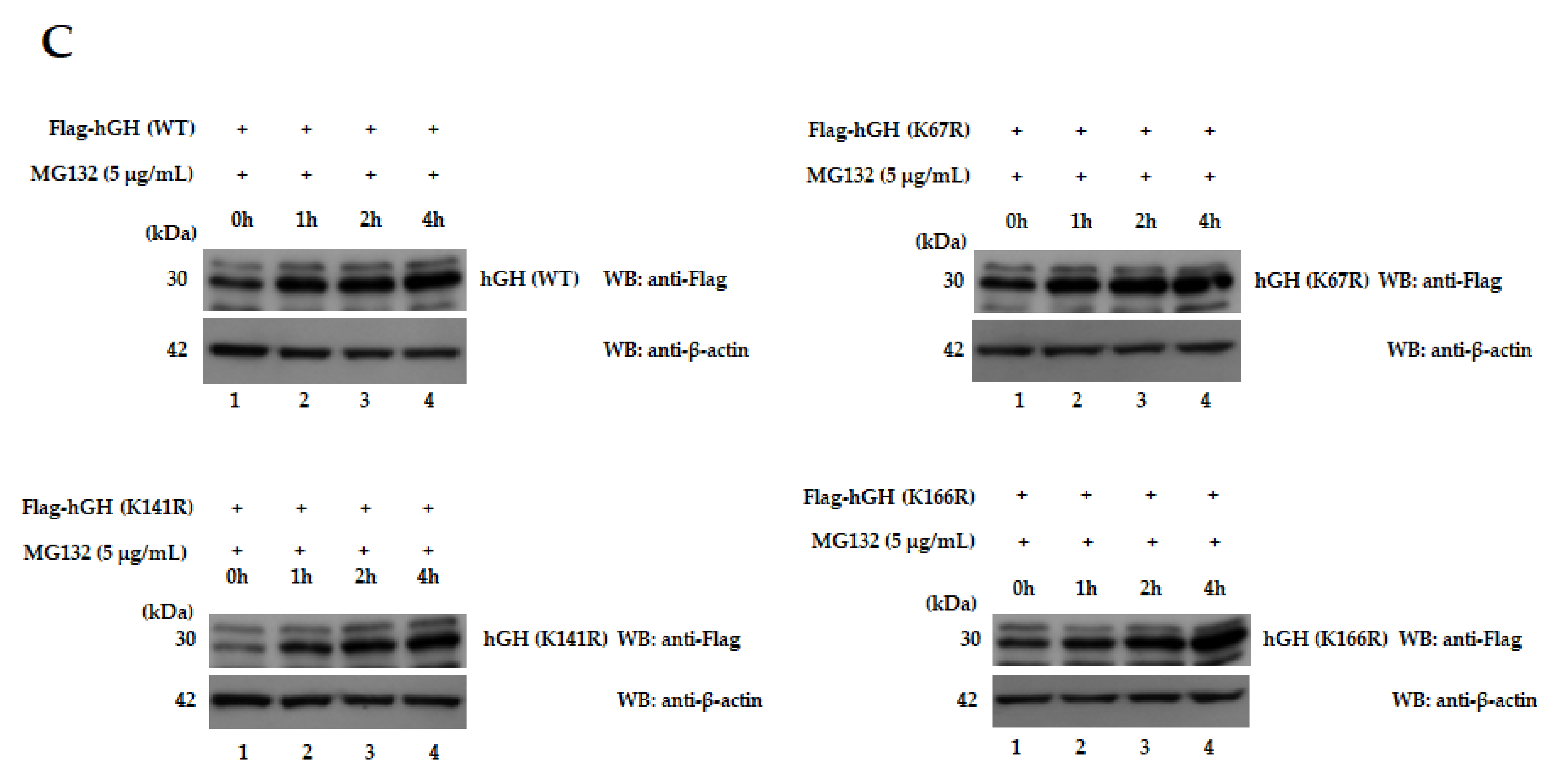
2.2. hGH (K141R) Extends Its Half-Life
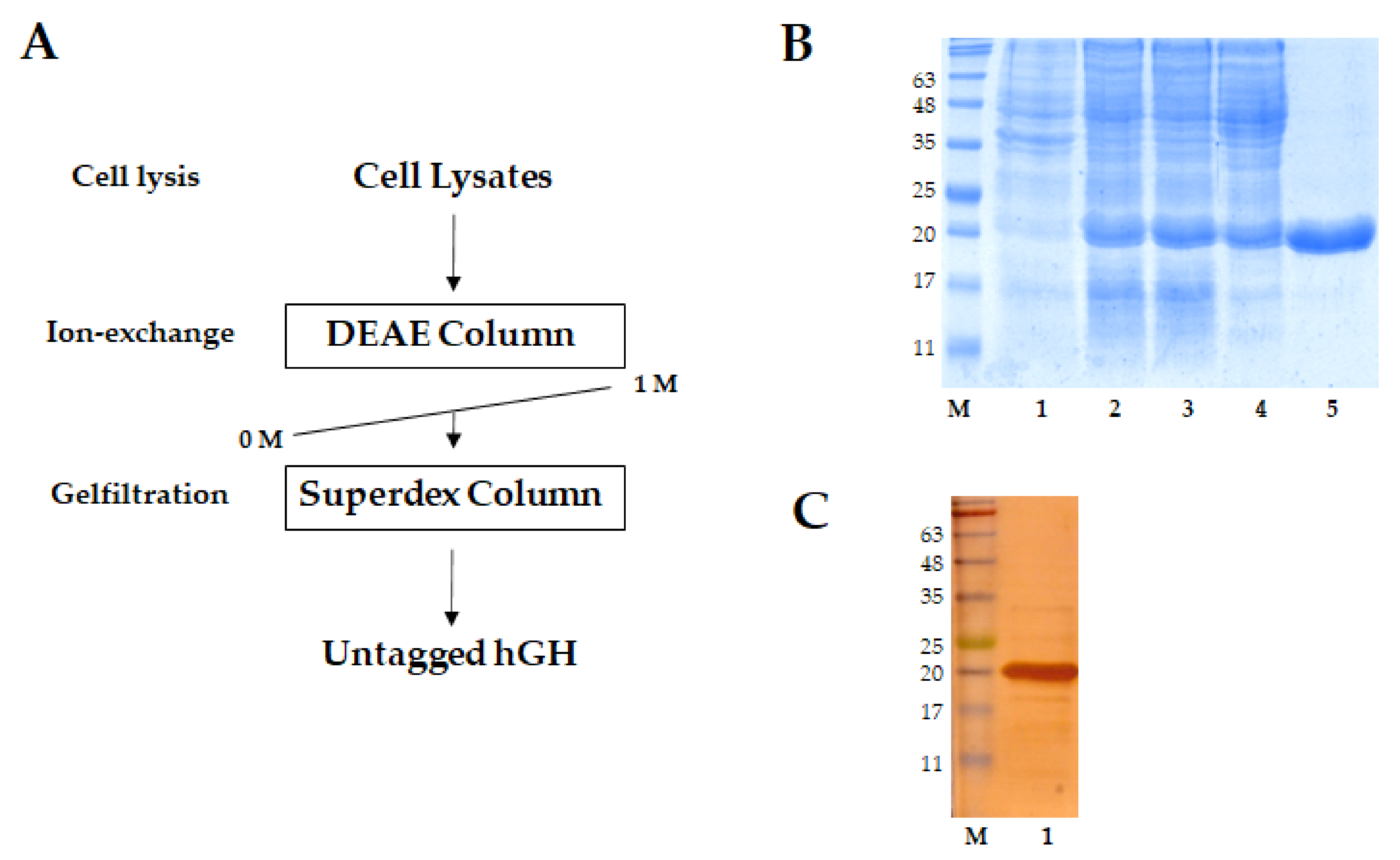
2.3. AUT-hGH and hGH Were Purified in Their Untagged Form
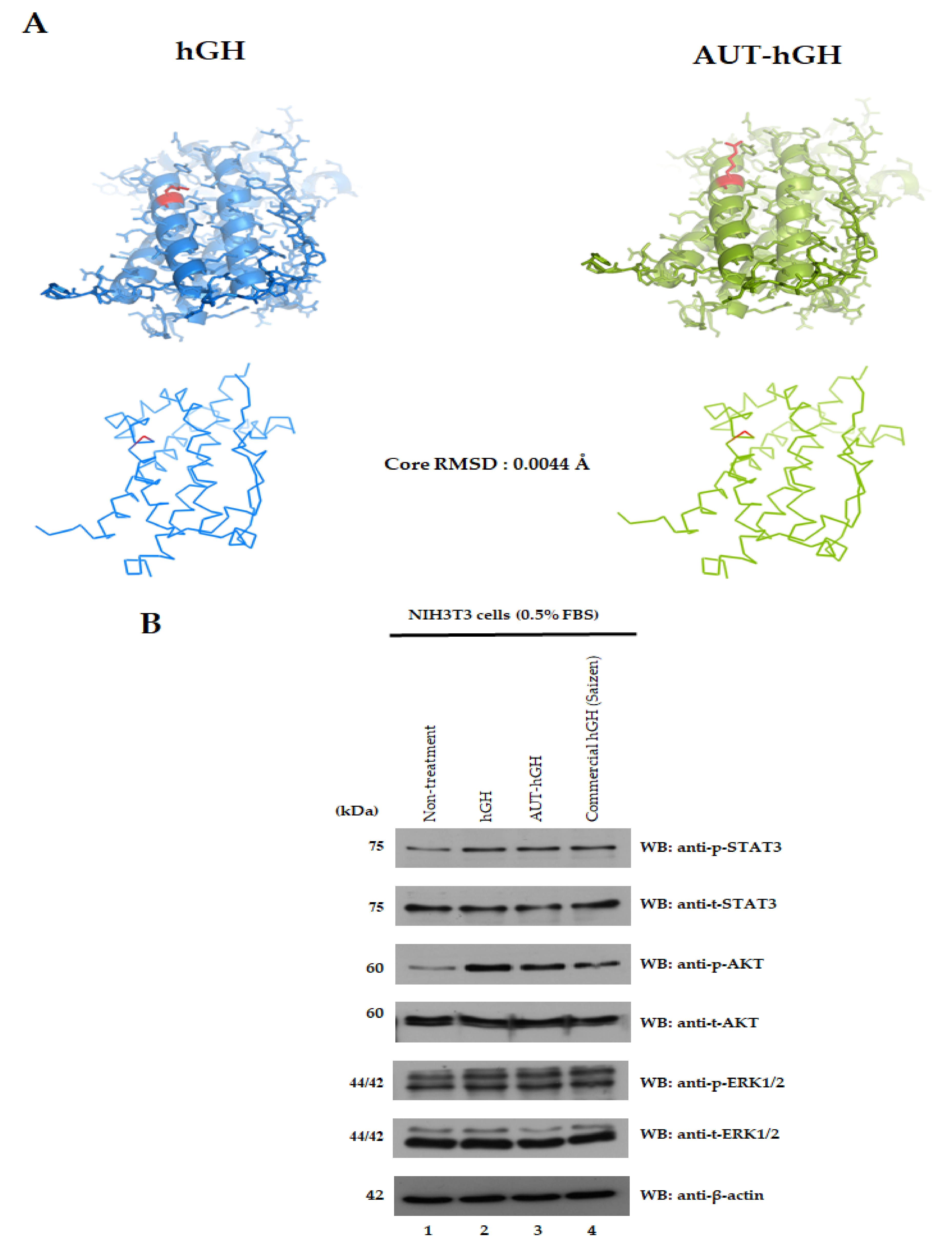
2.4. Structure and Biological Activity of hGH and AUT-hGH
2.5. hGH Ubiquitination in the Blood Stream
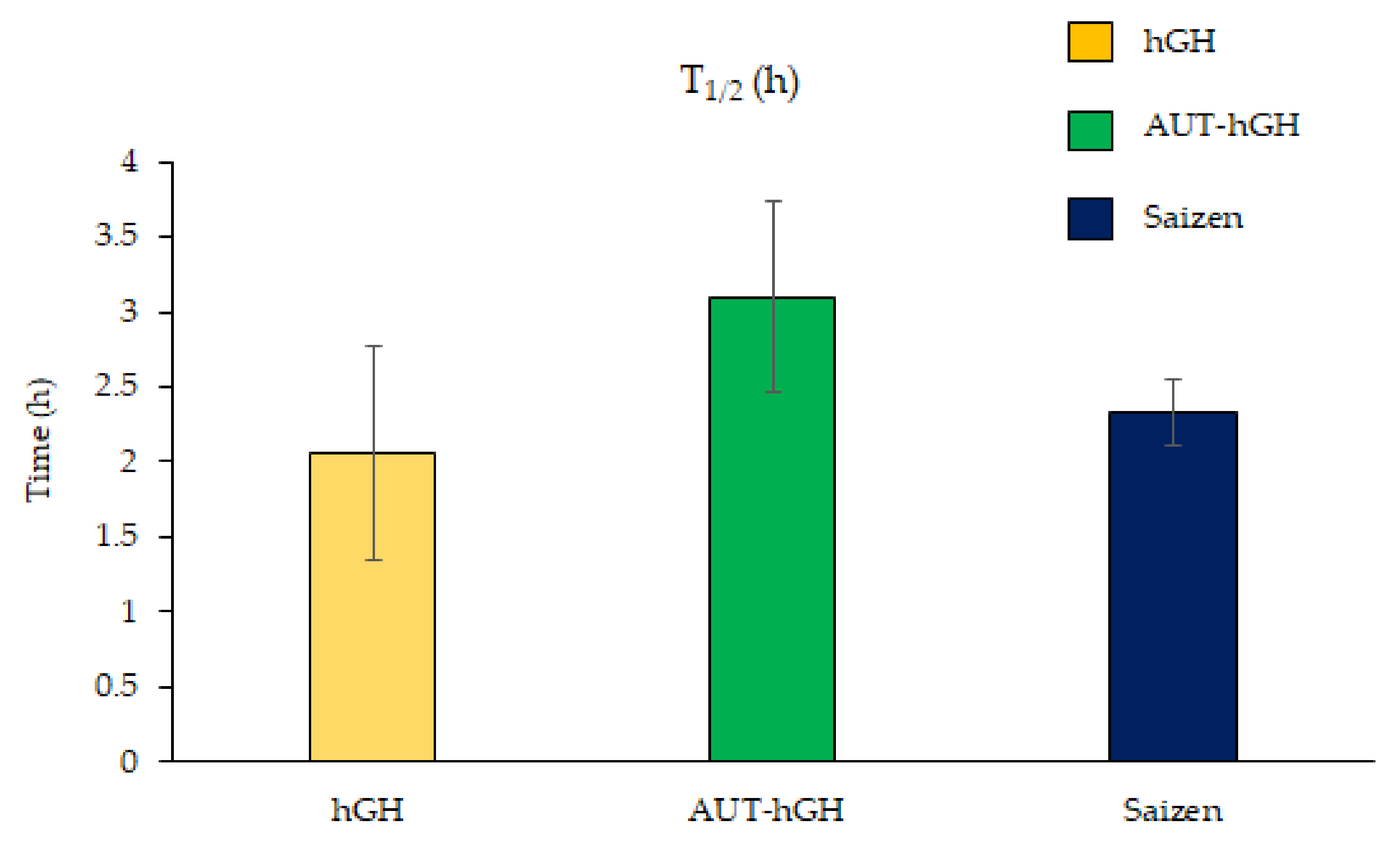
2.6. Increase in AUT-hGH Half-Life in the Blood Stream
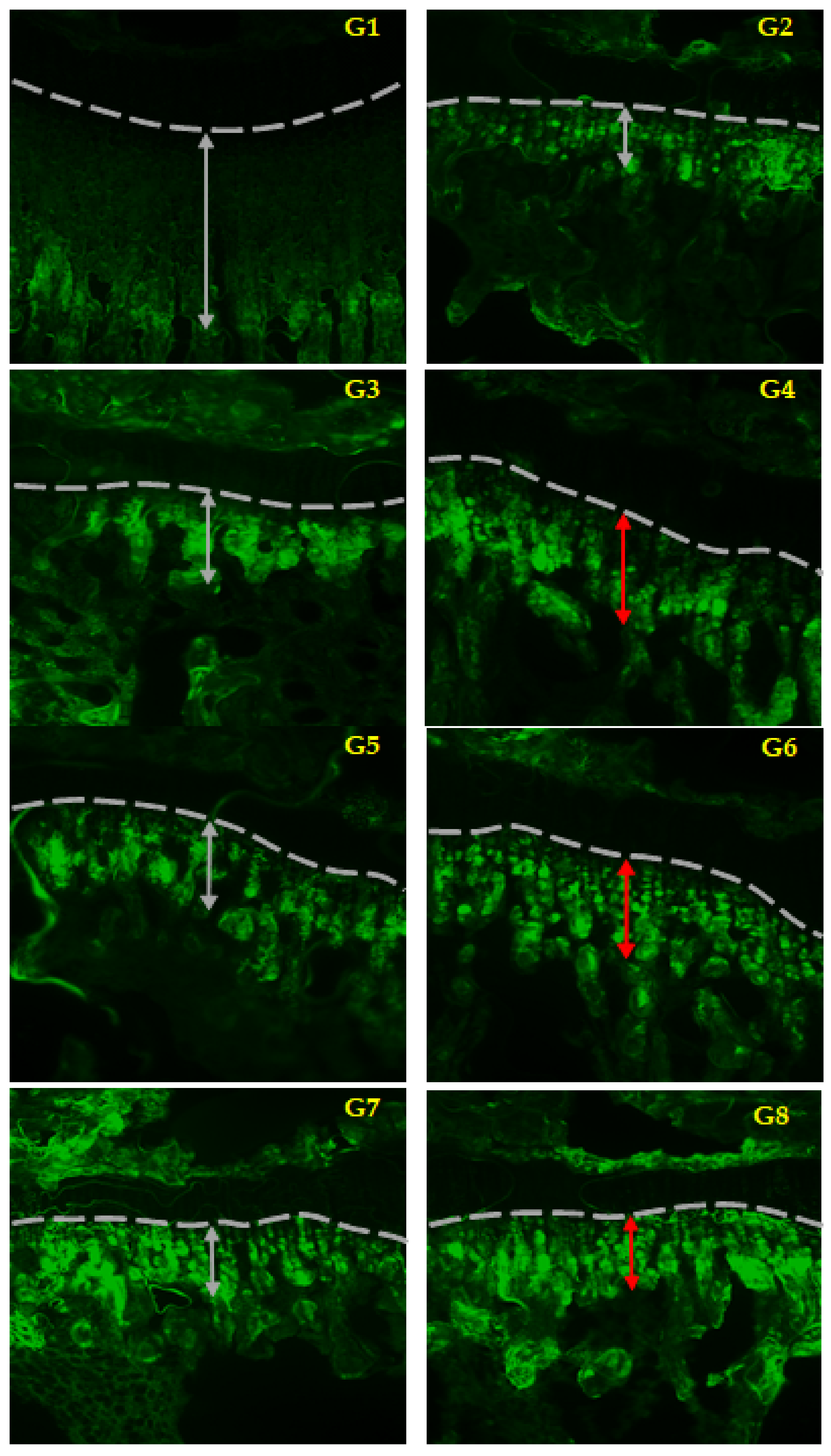
2.7. Maintaining the Efficacy of AUT-hGH
3. Discussion
4. Materials and Methods
4.1. hGH and Its Mutants for Expression
4.1.1. Preparation of hGH in Mammalian Cells
4.1.2. Isolation and Substitution of Lysine (K) Residue
4.2. Cell Lines
4.3. Ubiquitination Analysis in Cells
4.4. Analysis of Half-Life Using Protein Synthesis Inhibitor
4.5. Purification of rhGH and AUT-rhGH
4.6. Comparison of Structure of hGH and AUT-hGH
4.7. Signal Transduction by hGH and Its Mutant in Cells
4.8. Pharmacokinetic Study of AUT-hGH
4.8.1. Animals and Treatment
4.8.2. Blood Sampling
4.8.3. ELISA for the Detection of hGH in Plasma
4.8.4. Analysis for the Half-Life of AUT-hGH
4.9. Ubiquitination of hGH in Blood
4.9.1. Plasma Preparation and Pull-Down Assay Using Ni-NTA Beads
4.9.2. SDS-PAGE Separation
4.9.3. Enzymatic In-Gel Digestion
4.9.4. Nano-LC-ESI-MS/MS Analysis
4.9.5. Database Searching
4.9.6. Polyubiquitination of hGH in the Blood Stream
4.10. Efficacy Study of AUT-hGH
4.10.1. Animals and Treatment
4.10.2. Measurement of Length for Growth Plate
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUT | Anti-ubiquitination technology |
| CHX | Cycloheximide |
| DEAE | Diethylaminoethyl cellulose |
| DMEM | Dulbecco’s modified Eagle’s medium |
| E1 | Ubiquitin-activating |
| E2 E3 | Ubiquitin-conjugating Ubiquitin-ligase |
| ELISA | Enzyme-linked immunosorbent assay |
| FBS | Fetal bovine serum |
| hGH IPTG | Human growth hormone Isopropyl-b-D-thiogalactopyranoside |
| Nano-LC-ESI-MS/MS | Nano liquid chromatography-tandem mass spectrometry |
| PMSF SDS-PAGE | Phenylmethanesulfonyl fluoride Sodium dodecyl sulfate-polyacrylamide gel electrophoresis |
References
- Lan, H.; Nie, Z.; Liu, Y.; Lv, Z.; Liu, Y.; Quan, Y.; Chen, J.; Zhen, Q.; Chen, Q.; Wang, D.; et al. In Vivo Bioassay of Recombinant Human Growth Hormone Synthesized in B. Mori Pupae. J. Biomed. Biotechnol. 2010, 2010, 306462. [Google Scholar] [CrossRef]
- Le Roith, D.; Bondy, C.; Yakar, S.; Liu, J.-L.; Butler, A. The Somatomedin Hypothesis: 2001. Endocr. Rev. 2001, 22, 53–74. [Google Scholar] [CrossRef]
- Kang, J.; Wu, F.; Cai, Y.; Xu, M.; He, M.; Yuan, W. Development of Recombinant Human Growth Hormone (rhGH) sustained-release microspheres by a low temperature aqueous phase/aqueous phase emulsion method. Eur. J. Pharm. Sci. 2014, 62, 141–147. [Google Scholar] [CrossRef]
- Ghasemi, R.; Abdollahi, M.; Zadeh, E.E.; Khodabakhshi, K.; Badeli, A.; Bagheri, H.; Hosseinkhani, S. mPEG-PLA and PLA-PEG-PLA nanoparticles as new carriers for delivery of recombinant human Growth Hormone (rhGH). Sci. Rep. 2018, 8, 9854. [Google Scholar] [CrossRef] [PubMed]
- Govardhan, C.; Khalaf, N.; Jung, C.W.; Simeone, B.; Higbie, A.; Qu, S.; Chemmalil, L.; Pechenov, S.; Basu, S.K.; Margolin, A.L. Novel Long-Acting Crystal Formulation of Human Growth Hormone. Pharm. Res. 2005, 22, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Kwak, H.; Shim, W.; Choi, M.; Son, M.; Kim, Y.; Yang, H.; Kim, T.; Lee, G.; Kim, B.; Kang, S.; et al. Development of a sustained-release recombinant human growth hormone formulation. J. Control. Release 2009, 137, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Jordan, F.; Naylor, A.; Kelly, C.; Howdle, S.; Lewis, A.; Illum, L. Sustained release hGH microsphere formulation produced by a novel supercritical fluid technology: In vivo studies. J. Control. Release 2010, 141, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Seo, B.-B.; Park, M.-R.; Chun, C.; Lee, J.-Y.; Song, S.-C. The biological efficiency and bioavailability of human growth hormone delivered using injectable, ionic, thermosensitive poly(organophosphazene)-polyethylenimine conjugate hydrogels. Biomaterials 2011, 32, 8271–8280. [Google Scholar] [CrossRef]
- Park, M.-R.; Chun, C.; Ahn, S.-W.; Ki, M.-H.; Cho, C.-S.; Song, S.-C. Sustained delivery of human growth hormone using a polyelectrolyte complex-loaded thermosensitive polyphosphazene hydrogel. J. Control. Release 2010, 147, 359–367. [Google Scholar] [CrossRef]
- Park, M.-R.; Chun, C.; Ahn, S.-W.; Ki, M.-H.; Cho, C.-S.; Song, S.-C. Cationic and thermosensitive protamine conjugated gels for enhancing sustained human growth hormone delivery. Biomaterials 2010, 31, 1349–1359. [Google Scholar] [CrossRef]
- Garcı́a, J.T.; Dorta, M.J.; Munguı́a, O.; Llabrés, M.; Fariña, J.B. Biodegradable laminar implants for sustained release of recombinant human growth hormone. Biomaterials 2002, 23, 4759–4764. [Google Scholar] [CrossRef]
- Santoveña, A.; Garcia, J.; Oliva, A.; Llabres, M.; Fariña, J. A mathematical model for interpreting in vitro rhGH release from laminar implants. Int. J. Pharm. 2006, 309, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Yuen, K.C.; Miller, B.S.; Biller, B.M. The current state of long-acting growth hormone preparations for growth hormone therapy. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.-S.; Jang, D.S.; Yang, S.Y.; Lee, M.N.; Jin, K.S.; Cha, H.J.; Kim, J.K.; Sung, Y.C.; Choi, K.Y. Controlled release of human growth hormone fused with a human hybrid Fc fragment through a nanoporous polymer membrane. Nanoscale 2013, 5, 4262. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ku, C.R.; Brue, T.; Schilbach, K.; Ignatenko, S.; Magony, S.; Chung, Y.-S.; Kim, B.-J.; Hur, K.Y.; Kang, H.-C.; Kim, J.H.; et al. Long-acting FC-fusion rhGH (GX-H9) shows potential for up to twice-monthly administration in GH-deficient adults. Eur. J. Endocrinol. 2018, 179, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Fares, F.; Guy, R.; Bar-Ilan, A.; Felikman, Y.; Fima, E. Designing a Long-Acting Human Growth Hormone (hGH) by Fusing the Carboxyl-Terminal Peptide of Human Chorionic Gonadotropin Beta-Subunit to the Coding Sequence of hGH. Endocrinology 2010, 151, 4410–4417. [Google Scholar] [CrossRef] [PubMed]
- Zelinska, N.; Iotova, V.; Skorodok, J.; Malievsky, O.; Peterkova, V.; Samsonova, L.; Rosenfeld, R.G.; Zadik, Z.; Jaron-Mendelson, M.; Koren, R.; et al. Long-Acting CTP-Modified hGH (MOD-4023): Results of a Safety and Dose-Finding Study in GHD Children. J. Clin. Endocrinol. Metab. 2017, 102, 1578–1587. [Google Scholar] [CrossRef]
- Rasmussen, M.H.; Olsen, M.W.B.; Alifrangis, L.; Klim, S.; Suntum, M. A Reversible Albumin-Binding Growth Hormone Derivative is Well Tolerated and Possesses a Potential Once-Weekly Treatment Profile. J. Clin. Endocrinol. Metab. 2014, 99, E1819–E1829. [Google Scholar] [CrossRef] [PubMed]
- Johannsson, G.; Feldt-Rasmussen, U.; Håkonsson, I.H.; Biering, H.; Rodien, P.; Tahara, S.; A Toogood, A.; Rasmussen, M.H.; Karges, W.; Mann, A.; et al. Safety and convenience of once-weekly somapacitan in adult GH deficiency: A 26-week randomized, controlled trial. Eur. J. Endocrinol. 2018, 178, 491–499. [Google Scholar] [CrossRef]
- Juul, R.V.; Rasmussen, M.H.; Agersø, H.; Overgaard, R.V. Pharmacokinetics and Pharmacodynamics of Once-Weekly Somapacitan in Children and Adults: Supporting Dosing Rationales with a Model-Based Analysis of Three Phase I Trials. Clin. Pharmacokinet. 2018, 58, 63–75. [Google Scholar] [CrossRef]
- Luo, X.-P.; Hou, L.; Chen, Z.-H.; Liu, D.; Cheng, Y.-G. Comparative pharmacokinetics and pharmacodynamics of a PEGylated recombinant human growth hormone and daily recombinant human growth hormone in growth hormone-deficient children. Drug Des. Dev. Ther. 2015, 10, 13–21. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Luo, X.; Hou, L.; Liang, L.; Dong, G.; Shen, S.; Zhao, Z.; Gong, C.X.; Li, Y.; Du, M.-L.; Su, Z.; et al. Long-acting PEGylated recombinant human growth hormone (Jintrolong) for children with growth hormone deficiency: Phase II and phase III multicenter, randomized studies. Eur. J. Endocrinol. 2017, 177, 195–205. [Google Scholar] [CrossRef]
- Lim, K.-H.; Joo, J.-Y.; Baek, K.-H. The potential roles of deubiquitinating enzymes in brain diseases. Ageing Res. Rev. 2020, 61, 101088. [Google Scholar] [CrossRef]
- Suresh, B.; Lee, J.; Kim, H.; Ramakrishna, S. Regulation of pluripotency and differentiation by deubiquitinating enzymes. Cell Death Differ. 2016, 23, 1257–1264. [Google Scholar] [CrossRef]
- Sujashvili, R. Advantages of Extracellular Ubiquitin in Modulation of Immune Responses. Mediat. Inflamm. 2016, 2016, 4190390. [Google Scholar] [CrossRef]
- Takada, K.; Nasu, H.; Hibi, N.; Tsukada, Y.; Shibasaki, T.; Fujise, K.; Fujimoro, M.; Sawada, H.; Yokosawa, H.; Ohkawa, K. Serum Concentrations of Free Ubiquitin and Multiubiquitin Chains. Clin. Chem. 1997, 43, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Majetschak, M. Extracellular ubiquitin: Immune modulator and endogenous opponent of damage-associated molecular pattern molecules. J. Leukoc. Biol. 2010, 89, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-J.; Park, H.S.; Seo, K.H.; Yang, H.-J.; Kim, S.-K.; Choi, J.-H. Complete Solubilization and Purification of Recombinant Human Growth Hormone Produced in Escherichia coli. PLoS ONE 2013, 8, e56168. [Google Scholar] [CrossRef][Green Version]
- Francis, D.M.; Page, R. Strategies to Optimize Protein Expression in E. coli. Curr. Protoc. Protein Sci. 2010, 61, 5.24.1–5.24.29. [Google Scholar] [CrossRef] [PubMed]
- Baneyx, F.; Mujacic, M. Recombinant protein folding and misfolding in Escherichia coli. Nat. Biotechnol. 2004, 22, 1399–1408. [Google Scholar] [CrossRef]
- Jewett, A.I.; Huang, C.C.; Ferrin, T.E. MINRMS: An efficient algorithm for determining protein structure similarity using root-mean-squared-distance. Bioinformatics 2003, 19, 625–634. [Google Scholar] [CrossRef]
- Emsley, P.; Lohkamp, B.; Scott, W.G.; Cowtan, K.D. Features and development ofCoot. Acta Crystallogr. Sect. D Biol. Crystallogr. 2010, 66, 486–501. [Google Scholar] [CrossRef] [PubMed]
- Herrington, J.; Smit, L.S.; Schwartz, J.; Carter-Su, C. The role of STAT proteins in growth hormone signaling. Oncogene 2000, 19, 2585–2597. [Google Scholar] [CrossRef] [PubMed]
- Carter-Su, C.; Schwartz, J.; Argetsinger, L.S. Growth hormone signaling pathways. Growth Horm. IGF Res. 2016, 28, 11–15. [Google Scholar] [CrossRef] [PubMed]
- De Groot, M.C.H.; van Zwieten-Boot, B.J.; van Grootheest, A.C. Severe Adverse Reactions after the Use of Sulphur Hexafluoride (SonoVue) as an Ultrasonographic Contrast Agent. Ned. Tijdschr. Geneeskd. 2004, 148, 1887–1888. [Google Scholar] [PubMed]
- Pérez-Pérez, L.; García-Gavín, J.; Piñeiro, B.; Zulaica, A. Biologic-induced urticaria due to polysorbate 80: Usefulness of prick test. Br. J. Dermatol. 2011, 164, 1119–1120. [Google Scholar] [CrossRef] [PubMed]
- Sundy, J.S.; Baraf, H.S.B.; Yood, R.A.; Edwards, N.L.; Gutierrez-Urena, S.R.; Treadwell, E.L.; Vázquez-Mellado, J.; White, W.B.; Lipsky, P.E.; Horowitz, Z.; et al. Efficacy and Tolerability of Pegloticase for the Treatment of Chronic Gout in Patients Refractory to Conventional Treatment. JAMA 2011, 306, 711–720. [Google Scholar] [CrossRef] [PubMed]
- Bendele, A.; Seely, J.; Richey, C.; Sennello, G.; Shopp, G. Short Communication: Renal Tubular Vacuolation in Animals Treated with Polyethylene-Glycol-Conjugated Proteins. Toxicol. Sci. 1998, 42, 152–157. [Google Scholar] [CrossRef]
- Bukowski, R.; Ernstoff, M.S.; Gore, M.E.; Nemunaitis, J.J.; Amato, R.; Gupta, S.K.; Tendler, C.L. Pegylated Interferon Alfa-2b Treatment for Patients with Solid Tumors: A Phase I/II Study. J. Clin. Oncol. 2002, 20, 3841–3949. [Google Scholar] [CrossRef]
- Gregoriadis, G.; Jain, S.; Papaioannou, I.; Laing, P. Improving the therapeutic efficacy of peptides and proteins: A role for polysialic acids. Int. J. Pharm. 2005, 300, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Caliceti, P. Pharmacokinetic and biodistribution properties of poly(ethylene glycol)–protein conjugates. Adv. Drug Deliv. Rev. 2003, 55, 1261–1277. [Google Scholar] [CrossRef]
- Lim, K.-H.; Suresh, B.; Park, J.-H.; Kim, Y.-S.; Ramakrishna, S.; Baek, K.-H. Ubiquitin-specific protease 11 functions as a tumor suppressor by modulating Mgl-1 protein to regulate cancer cell growth. Oncotarget 2016, 7, 14441–14457. [Google Scholar] [CrossRef] [PubMed]
- Baek, K.-H.; Kim, M.-S.; Kim, Y.-S.; Shin, J.-M.; Choi, H.-K. DUB-1A, a Novel Deubiquitinating Enzyme Subfamily Member, Is Polyubiquitinated and Cytokine-inducible in B-lymphocytes. J. Biol. Chem. 2004, 279, 2368–2376. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; Krohn, R.; Hermanson, G.; Mallia, A.; Gartner, F.; Provenzano, M.; Fujimoto, E.; Goeke, N.; Olson, B.; Klenk, D. Measurement of protein using bicinchoninic acid. Anal. Biochem. 1985, 150, 76–85. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.-S.; Kim, K.; Oh, S.K.; Lee, G.; Kim, J.-O.; Li, L.; Park, J.-H.; Baek, K.-H. Long-Lasting Growth Hormone Regulated by the Ubiquitin-Proteasome System. Int. J. Mol. Sci. 2021, 22, 6268. https://doi.org/10.3390/ijms22126268
Kim M-S, Kim K, Oh SK, Lee G, Kim J-O, Li L, Park J-H, Baek K-H. Long-Lasting Growth Hormone Regulated by the Ubiquitin-Proteasome System. International Journal of Molecular Sciences. 2021; 22(12):6268. https://doi.org/10.3390/ijms22126268
Chicago/Turabian StyleKim, Myung-Sun, Kyunggon Kim, Su Kyung Oh, Gidae Lee, Jin-Ock Kim, Lan Li, Jung-Hyun Park, and Kwang-Hyun Baek. 2021. "Long-Lasting Growth Hormone Regulated by the Ubiquitin-Proteasome System" International Journal of Molecular Sciences 22, no. 12: 6268. https://doi.org/10.3390/ijms22126268
APA StyleKim, M.-S., Kim, K., Oh, S. K., Lee, G., Kim, J.-O., Li, L., Park, J.-H., & Baek, K.-H. (2021). Long-Lasting Growth Hormone Regulated by the Ubiquitin-Proteasome System. International Journal of Molecular Sciences, 22(12), 6268. https://doi.org/10.3390/ijms22126268







