Tracking the Genetic Susceptibility Background of B-Cell Non-Hodgkin’s Lymphomas from Genome-Wide Association Studies
Abstract
1. Introduction
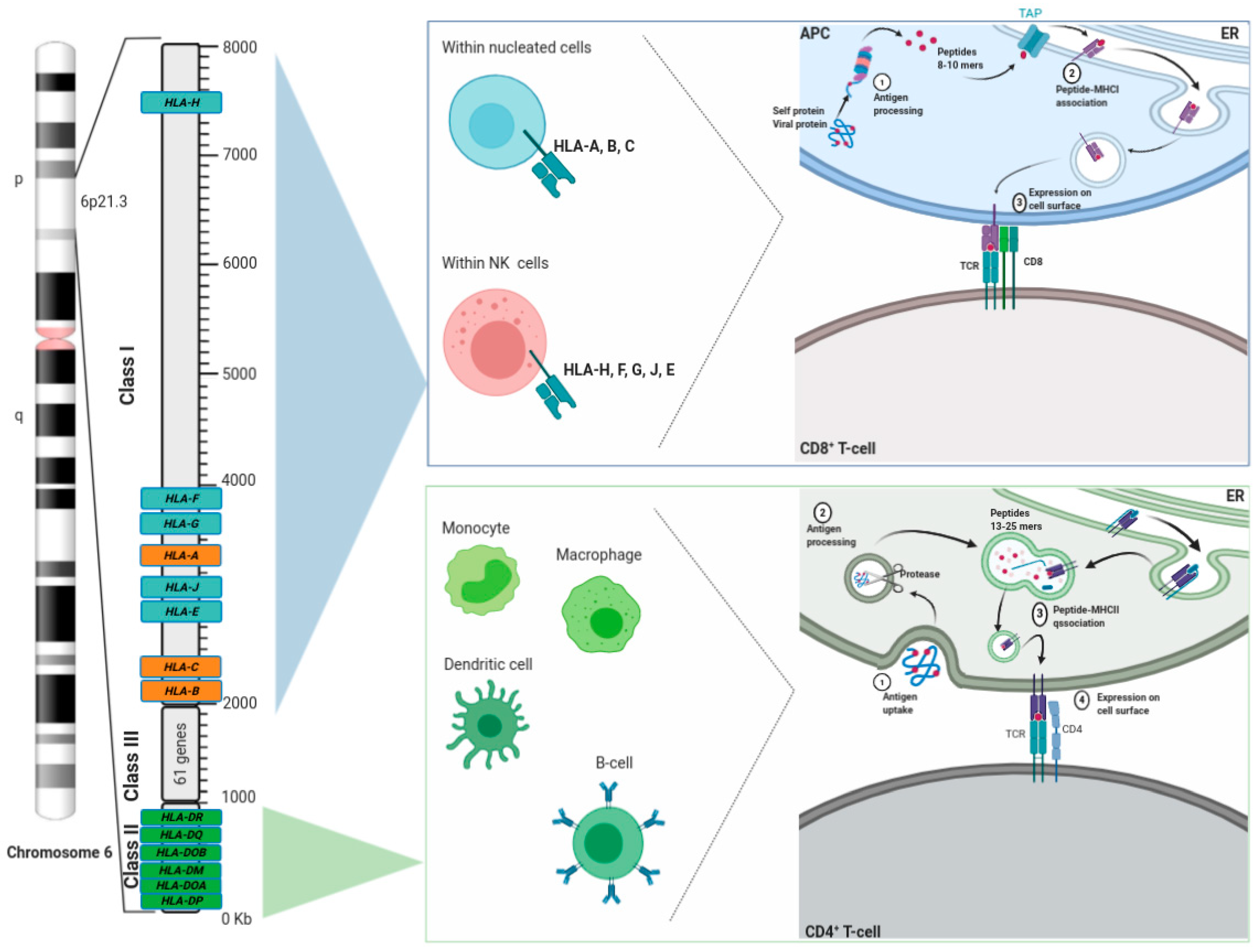
2. HLA Overview
3. GWAS in B-Cell NHL
3.1. DLBCL
3.2. FL
3.3. CLL
3.4. MZL
3.5. PCNSL
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| NHL | Non-Hodgkin’s lymphoma |
| HL | Hodgkin’s lymphoma |
| DLBCL | Diffuse large B-cell lymphoma |
| FL | Follicular lymphoma |
| CLL | Chronic lymphocytic leukemia |
| MZL | Marginal zone lymphoma |
| PCNSL | Primary central nervous system lymphoma |
| NGS | Next generation sequencing |
| GWAS | Genome-wide association studies |
| HLA | Human leukocyte antigen |
| MHC | Major histocompatibility complex |
| NK | Natural killer |
| R-CHOP | Rituximab combined with cyclophosphamide, doxorubicin, vincristine, and prednisolone treatment |
| GCB | Germinal center B-cell |
| ABC | Activated B-cell |
| OR | Odds ratio |
| CI | Confidence interval |
| LD | Linkage disequilibrium |
| SLE | Lupus erythematosus |
| MS | Multiple sclerosis |
| RA | Rheumatoid arthritis |
| AICDA | Activation-induced cytidine deaminase |
| GEO | Genome Expression Omnibus |
| ABC | ATP-binding cassette |
| EMZL | Extranodal MZL of mucosa-associated lymphoid tissue |
| HD-MTX | High dose methotrexate |
References
- Al-Naeeb, A.B.; Ajithkumar, T.; Behan, S.; Hodson, D. Non-Hodgkin lymphoma. BMJ 2018, 362, k3204. [Google Scholar] [CrossRef] [PubMed]
- Hoang-Xuan, K.; Bessell, E.; Bromberg, J.E.C.; Hottinger, A.F.; Preusser, M.; Rudà, R.; Schlegel, U.; Siegal, T.; Soussain, C.; Abacioglu, U.; et al. Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: Guidelines from the European Association for Neuro-Oncology. Lancet Oncol. 2015, 16, e322–e332. [Google Scholar] [CrossRef]
- Smedby, K.E. Epidemiology and etiology of non-Hodgkin lymphoma—A review. Acta Oncol. 2006, 45, 258–271. [Google Scholar] [CrossRef] [PubMed]
- Parihar, A.S.; Singh, R.; Shaik, S.; Negi, B.S.; Rajguru, J.P.; Patil, P.B.; Sharma, U. Non-Hodgkin’s lymphoma: A review. J. Fam. Med. Prim. Care 2020, 9, 1834–1840. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, S.H.; Campo, E.; Pileri, S.A.; Harris, N.L.; Stein, H.; Siebert, R.; Advani, R.; Ghielmini, M.; Salles, G.A.; Zelenetz, A.D.; et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016, 127, 2375–2390. [Google Scholar] [CrossRef] [PubMed]
- Braggio, E.; Van Wier, S.; Ojha, J.; McPhail, E.; Asmann, Y.W.; Egan, J.; Da Silva, J.A.; Schiff, D.; Lopes, M.B.; Decker, P.A.; et al. Genome-Wide Analysis Uncovers Novel Recurrent Alterations in Primary Central Nervous System Lymphomas. Clin. Cancer Res. 2015, 21, 3986–3994. [Google Scholar] [CrossRef] [PubMed]
- Zhong, C.; Cozen, W.; Bolanos, R.; Song, J.; Wang, S.S. The role ofHLAvariation in lymphoma aetiology and survival. J. Intern. Med. 2019, 286, 154–180. [Google Scholar] [CrossRef] [PubMed]
- Olszewski, A.J.; Castillo, J.J. Survival of patients with marginal zone lymphoma. Cancer 2012, 119, 629–638. [Google Scholar] [CrossRef]
- Morton, L.M.; Slager, S.L.; Cerhan, J.R.; Wang, S.S.; Vajdic, C.M.; Skibola, C.F.; Bracci, P.M.; De Sanjosé, S.; Smedby, K.E.; Chiu, B.C.H.; et al. Etiologic Heterogeneity Among Non-Hodgkin Lymphoma Subtypes: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Nat. Cancer Inst. Monogr. 2014, 2014, 130–144. [Google Scholar] [CrossRef]
- Moore, A.; Kane, E.; Wang, Z.; Panagiotou, O.A.; Teras, L.R.; Monnereau, A.; Doo, N.W.; Machiela, M.J.; Skibola, C.F.; Slager, S.L.; et al. Genetically Determined Height and Risk of Non-hodgkin Lymphoma. Front. Oncol. 2020, 9, 1539. [Google Scholar] [CrossRef]
- Din, L.; Sheikh, M.; Kosaraju, N.; Smedby, K.E.; Bernatsky, S.; Berndt, S.I.; Skibola, C.F.; Nieters, A.; Wang, S.; McKay, J.D.; et al. Genetic overlap between autoimmune diseases and non-Hodgkin lymphoma subtypes. Genet. Epidemiol. 2019, 43, 844–863. [Google Scholar] [CrossRef]
- Smedby, K.E.; Ponzoni, M. The aetiology of B-cell lymphoid malignancies with a focus on chronic inflammation and infections. J. Intern. Med. 2017, 282, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Hjalgrim, H.; Rostgaard, K.; Johnson, P.C.D.; Lake, A.; Shield, L.; Little, A.M.; Ekstrom-Smedby, K.; Adami, H.O.; Glimelius, B.; Hamilton-Dutoit, S.; et al. HLA-A alleles and infectious mononucleosis suggest a critical role for cytotoxic T-cell response in EBV-related Hodgkin lymphoma. Proc. Nat. Acad. Sci. USA 2010, 107, 6400–6405. [Google Scholar] [CrossRef]
- Mills, M.C.; Rahal, C. A scientometric review of genome-wide association studies. Commun. Biol. 2019, 2, 9. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xu, S. Statistical power in genome-wide association studies and quantitative trait locus mapping. Heredity 2019, 123, 287–306. [Google Scholar] [CrossRef]
- Di Paolo, A.; Arrigoni, E.; Luci, G.; Cucchiara, F.; Danesi, R.; Galimberti, S. Precision Medicine in Lymphoma by Innovative Instrumental Platforms. Front. Oncol. 2019, 9, 1417. [Google Scholar] [CrossRef]
- De Jong, M.R.W.; Visser, L.; Huls, G.; Diepstra, A.; Van Vugt, M.; Ammatuna, E.; Van Rijn, R.S.; Vellenga, E.; Berg, A.V.D.; Fehrmann, R.S.N.; et al. Identification of relevant drugable targets in diffuse large B-cell lymphoma using a genome-wide unbiased CD20 guilt-by association approach. PLoS ONE 2018, 13, e0193098. [Google Scholar] [CrossRef]
- Kleinstern, G.; Camp, N.J.; Berndt, S.I.; Birmann, B.M.; Nieters, A.; Bracci, P.M.; McKay, J.D.; Ghesquières, H.; Lan, Q.; Hjalgrim, H.; et al. Lipid Trait Variants and the Risk of Non-Hodgkin Lymphoma Subtypes: A Mendelian Randomization Study. Cancer Epidemiol. Biomark. Prev. 2020, 29, 1074–1078. [Google Scholar] [CrossRef]
- Bernatsky, S.; García, H.A.V.; Spinelli, J.J.; Gaffney, P.E.; Smedby, K.; Ramsey-Goldman, R.; Wang, S.S.; Adami, H.-O.; Albanes, D.; Angelucci, E.; et al. Lupus-related single nucleotide polymorphisms and risk of diffuse large B-cell lymphoma. Lupus Sci. Med. 2017, 4, e000187. [Google Scholar] [CrossRef] [PubMed]
- Trowsdale, J.; Knight, J.C. Major Histocompatibility Complex Genomics and Human Disease. Annu. Rev. Genom. Hum. Genet. 2013, 14, 301–323. [Google Scholar] [CrossRef] [PubMed]
- Amiel, J. Study of the Leukocyte Phenotypes in Hodgkin’s Disease. In Histocompatibility Testing; Munksgaard: Copenhagen, Denmark, 1967; pp. 79–81. [Google Scholar]
- Sanchez-Mazas, A. A review of HLA allele and SNP associations with highly prevalent infectious diseases in human populations. Swiss Med. Wkly. 2020, 150. [Google Scholar] [CrossRef] [PubMed]
- Dendrou, C.A.; Petersen, J.; Rossjohn, J.; Fugger, L. HLA variation and disease. Nat. Rev. Immunol. 2018, 18, 325–339. [Google Scholar] [CrossRef] [PubMed]
- Deakin, J.E.; Papenfuss, A.T.; Belov, K.; Cross, J.G.R.; Coggill, P.; Palmer, S.; Sims, S.; Speed, T.P.; Beck, S.; Graves, J.A.M. Evolution and comparative analysis of the MHC Class III inflammatory region. BMC Genom. 2006, 7, 281. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.; Soormally, A.R.; Hayhurst, J.D.; Marsh, S.G.E. The IPD-IMGT/HLA Database–New developments in reporting HLA variation. Hum. Immunol. 2016, 77, 233–237. [Google Scholar] [CrossRef]
- Sewell, A.K. Why must T cells be cross-reactive? Nat. Rev. Immunol. 2012, 12, 669–677. [Google Scholar] [CrossRef]
- Saunders, P.M.; Vivian, J.P.; O’Connor, G.M.; Sullivan, L.C.; Pymm, P.G.; Rossjohn, J.; Brooks, A.G. A bird’s eye view of NK cell receptor interactions with their MHC class I ligands. Immunol. Rev. 2015, 267, 148–166. [Google Scholar] [CrossRef]
- Ghesquieres, H.; Slager, S.L.; Jardin, F.; Veron, A.S.; Asmann, Y.W.; Maurer, M.J.; Fest, T.; Habermann, T.M.; Bene, M.C.; Novak, A.J.; et al. Genome-Wide Association Study of Event-Free Survival in Diffuse Large B-Cell Lymphoma Treated With Immunochemotherapy. J. Clin. Oncol. 2015, 33, 3930–3937. [Google Scholar] [CrossRef]
- Wright, G.; Tan, B.; Rosenwald, A.; Hurt, E.H.; Wiestner, A.; Staudt, L.M. A gene expression-based method to diagnose clinically distinct subgroups of diffuse large B cell lymphoma. Proc. Nat. Acad. Sci. USA 2003, 100, 9991–9996. [Google Scholar] [CrossRef]
- Cerhan, J.R.; Kricker, A.; Paltiel, O.; Flowers, C.R.; Wang, S.S.; Monnereau, A.; Blair, A.; Maso, L.D.; Kane, E.V.; Nieters, A.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Diffuse Large B-Cell Lymphoma: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Nat. Cancer Inst. Monogr. 2014, 2014, 15–25. [Google Scholar] [CrossRef]
- Park, H.Y.; Hong, Y.C.; Lee, K.; Koh, J. Vitamin D status and risk of non-Hodgkin lymphoma: An updated meta-analysis. PLoS ONE 2019, 14, e0216284. [Google Scholar] [CrossRef]
- Cerhan, J.R.; Berndt, S.I.; Vijai, J.; Ghesquières, H.; McKay, J.D.; Wang, S.S.; Wang, Z.; Yeager, M.; Conde, L.; De Bakker, P.I.; et al. Genome-wide association study identifies multiple susceptibility loci for diffuse large B cell lymphoma. Nat. Genet. 2014, 46, 1233–1238. [Google Scholar] [CrossRef] [PubMed]
- Bassig, B.A.; Cerhan, J.R.; Au, W.-Y.; Kim, H.N.; Sangrajrang, S.; Hu, W.; Tse, J.; Berndt, S.; Zheng, T.; Zhang, H.; et al. Genetic susceptibility to diffuse large B-cell lymphoma in a pooled study of three Eastern Asian populations. Eur. J. Haematol. 2015, 95, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Smedby, K.E.; Foo, J.N.; Skibola, C.F.; Darabi, H.; Conde, L.; Hjalgrim, H.; Kumar, V.; Chang, E.T.; Rothman, N.; Cerhan, J.R.; et al. GWAS of Follicular Lymphoma Reveals Allelic Heterogeneity at 6p21.32 and Suggests Shared Genetic Susceptibility with Diffuse Large B-cell Lymphoma. PLoS Genet. 2011, 7, e1001378. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.S.; Carrington, M.; Berndt, S.I.; Slager, S.L.; Bracci, P.M.; Voutsinas, J.; Cerhan, J.R.; Smedby, K.E.; Hjalgrim, H.; Vijai, J.; et al. HLA Class I and II Diversity Contributes to the Etiologic Heterogeneity of Non-Hodgkin Lymphoma Subtypes. Cancer Res. 2018, 78, 4086–4096. [Google Scholar] [CrossRef] [PubMed]
- Kleinstern, G.; Yan, H.; Hildebrandt, M.A.T.; Vijai, J.; Berndt, S.I.; Ghesquières, H.; McKay, J.; Wang, S.S.; Nieters, A.; Ye, Y.; et al. Inherited variants at 3q13.33 and 3p24.1 are associated with risk of diffuse large B-cell lymphoma and implicate immune pathways. Hum. Mol. Genet. 2019, 29, 70–79. [Google Scholar] [CrossRef]
- Aslan, K.; Turco, V.; Blobner, J.; Sonner, J.K.; Liuzzi, A.R.; Núñez, N.G.; De Feo, D.; Kickingereder, P.; Fischer, M.; Green, E.; et al. Heterogeneity of response to immune checkpoint blockade in hypermutated experimental gliomas. Nat. Commun. 2020, 11, 931. [Google Scholar] [CrossRef]
- Basso, K.; Dalla-Favera, R. BCL6. Adv. Immunol. 2010, 105, 193–210. [Google Scholar] [CrossRef]
- Kumar, V.; Matsuo, K.; Takahashi, A.; Hosono, N.; Tsunoda, T.; Kamatani, N.; Kong, S.Y.; Nakagawa, H.; Cui, R.; Tanikawa, C.; et al. Common variants on 14q32 and 13q12 are associated with DLBCL susceptibility. J. Hum. Genet. 2011, 56, 436–439. [Google Scholar] [CrossRef]
- Arthur, S.E.; Jiang, A.; Grande, B.M.; Alcaide, M.; Cojocaru, R.; Rushton, C.K.; Mottok, A.; Hilton, L.K.; Lat, P.K.; Zhao, E.Y.; et al. Genome-wide discovery of somatic regulatory variants in diffuse large B-cell lymphoma. Nat. Commun. 2018, 9, 4001. [Google Scholar] [CrossRef]
- Georgiou, K.; Chen, L.; Berglund, M.; Ren, W.; De Miranda, N.F.C.C.; Lisboa, S.; Fangazio, M.; Zhu, S.; Hou, Y.; Wu, K.; et al. Genetic basis of PD-L1 overexpression in diffuse large B-cell lymphomas. Blood 2016, 127, 3026–3034. [Google Scholar] [CrossRef]
- Muramatsu, M.; Kinoshita, K.; Fagarasan, S.; Yamada, S.; Shinkai, Y.; Honjo, T. Class Switch Recombination and Hypermutation Require Activation-Induced Cytidine Deaminase (AID), a Potential RNA Editing Enzyme. Cell 2000, 102, 553–563. [Google Scholar] [CrossRef]
- Duclos, C.M.; Champagne, A.; Carrier, J.C.; Saucier, C.; Lavoie, C.L.; Denault, J.-B. Caspase-mediated proteolysis of the sorting nexin 2 disrupts retromer assembly and potentiates Met/hepatocyte growth factor receptor signaling. Cell Death Discov. 2017, 3, 16100. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yu, Z.; Jiang, T.; Shao, L.; Liu, Y.; Li, N.; Wu, Y.; Zheng, C.; Wu, X.; Zhang, M.; et al. SNCA, a novel biomarker for Group 4 medulloblastomas, can inhibit tumor invasion and induce apoptosis. Cancer Sci. 2018, 109, 1263–1275. [Google Scholar] [CrossRef] [PubMed]
- Fong, L.W.R.; Yang, D.C.; Chen, C.-H. Myristoylated alanine-rich C kinase substrate (MARCKS): A multirole signaling protein in cancers. Cancer Metastasis Rev. 2017, 36, 737–747. [Google Scholar] [CrossRef]
- De Jong, M.R.W.; Langendonk, M.; Reitsma, B.; Herbers, P.; Nijland, M.; Huls, G.; Berg, A.V.D.; Ammatuna, E.; Visser, L.; Van Meerten, T. WEE1 Inhibition Enhances Anti-Apoptotic Dependency as a Result of Premature Mitotic Entry and DNA Damage. Cancers 2019, 11, 1743. [Google Scholar] [CrossRef]
- Baecklund, F.; Foo, J.N.; Bracci, P.M.; Darabi, H.; Karlsson, R.; Hjalgrim, H.; Rosenquist, R.; Adami, H.-O.; Glimelius, U.I.B.; Melbye, M.; et al. A comprehensive evaluation of the role of genetic variation in follicular lymphoma survival. BMC Med. Genet. 2014, 15, 113. [Google Scholar] [CrossRef]
- Skibola, C.F.; Akers, N.K.; Conde, L.; Ladner, M.; Hawbecker, S.K.; Cohen, F.; Ribas, F.; Erlich, H.A.; Goodridge, D.; Trachtenberg, E.A.; et al. Multi-locus HLA class I and II allele and haplotype associations with follicular lymphoma. Tissue Antigens 2012, 79, 279–286. [Google Scholar] [CrossRef]
- Linet, M.S.; Vajdic, C.; Morton, L.M.; De Roos, A.J.; Skibola, C.F.; Boffetta, P.; Cerhan, J.R.; Flowers, C.R.; De Sanjosé, S.; Monnereau, A.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Follicular Lymphoma: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Nat. Cancer Inst. Monogr. 2014, 2014, 26–40. [Google Scholar] [CrossRef]
- Conde, L.; Halperin, E.; Akers, N.K.; Brown, K.M.; Smedby, K.E.; Rothman, N.; Nieters, A.; Slager, S.L.; Brooks-Wilson, A.; Agana, L.; et al. Genome-wide association study of follicular lymphoma identifies a risk locus at 6p21.32. Nat. Genet. 2010, 42, 661–664. [Google Scholar] [CrossRef]
- Qiao, Y.; Zhou, Y.; Wu, C.; Zhai, K.; Han, X.; Chen, J.; Tian, X.; Chang, J.; Lu, Z.; Zhang, B.; et al. Risk of genome-wide association study-identified genetic variants for non-Hodgkin lymphoma in a Chinese population. Carcinogenesis 2013, 34, 1516–1519. [Google Scholar] [CrossRef]
- Cerhan, J.R.; Fredericksen, Z.S.; Novak, A.J.; Ansell, S.M.; Kay, N.E.; Liebow, M.; Doğan, A.; Cunningham, J.M.; Wang, A.H.; Witzig, T.E.; et al. A Two-Stage Evaluation of Genetic Variation in Immune and Inflammation Genes with Risk of Non-Hodgkin Lymphoma Identifies New Susceptibility Locus in 6p21.3 Region. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1799–1806. [Google Scholar] [CrossRef] [PubMed]
- Skibola, C.F.; Conde, L.; Foo, J.N.; Riby, J.; Humphreys, K.; Sillé, F.C.M.; Darabi, H.; Sanchez, S.; Hjalgrim, H.; Liu, J.; et al. A meta-analysis of genome-wide association studies of follicular lymphoma. BMC Genom. 2012, 13, 516. [Google Scholar] [CrossRef] [PubMed]
- Skibola, C.F.; Berndt, S.I.; Vijai, J.; Conde, L.; Wang, Z.; Yeager, M.; De Bakker, P.I.; Birmann, B.M.; Vajdic, C.M.; Foo, J.N.; et al. Genome-wide Association Study Identifies Five Susceptibility Loci for Follicular Lymphoma outside the HLA Region. Am. J. Hum. Genet. 2014, 95, 462–471. [Google Scholar] [CrossRef]
- Skibola, C.F.; Bracci, P.M.; Halperin, E.; Conde, L.; Craig, D.W.; Agana, L.; Iyadurai, K.; Becker, N.; Brookes-Wilson, A.; Curry, J.D.; et al. Genetic variants at 6p21.33 are associated with susceptibility to follicular lymphoma. Nat. Genet. 2009, 41, 873–875. [Google Scholar] [CrossRef]
- Di Bernardo, M.C.; Crowther-Swanepoel, D.; Broderick, P.; Webb, E.; Sellick, G.; Wild, R.; Sullivan, K.; Vijayakrishnan, J.; Wang, Y.; Pittman, A.M.; et al. A genome-wide association study identifies six susceptibility loci for chronic lymphocytic leukemia. Nat. Genet. 2008, 40, 1204–1210. [Google Scholar] [CrossRef]
- Crowther-Swanepoel, D.; Broderick, P.; Di Bernardo, M.C.; Dobbins, S.E.; Torres, M.P.; Mansouri, M.; Ruiz-Ponte, C.; Enjuanes, A.; Rosenquist, R.; Carracedo, A.; et al. Common variants at 2q37.3, 8q24.21, 15q21.3 and 16q24.1 influence chronic lymphocytic leukemia risk. Nat. Genet. 2010, 42, 132–136. [Google Scholar] [CrossRef]
- Slager, S.L.; Benavente, Y.; Blair, A.; Vermeulen, R.; Cerhan, J.R.; Costantini, A.S.; Monnereau, A.; Nieters, A.; Clavel, J.; Call, T.G.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Nat. Cancer Inst. Monogr. 2014, 2014, 41–51. [Google Scholar] [CrossRef]
- Sampson, J.N.; Wheeler, W.A.; Yeager, M.; Panagiotou, O.A.; Wang, Z.; Berndt, S.I.; Lan, Q.; Abnet, C.C.; Amundadottir, L.T.; Figueroa, J.D.; et al. Analysis of Heritability and Shared Heritability Based on Genome-Wide Association Studies for Thirteen Cancer Types. J. Nat. Cancer Inst. 2015, 107, djv279. [Google Scholar] [CrossRef]
- Gragert, L.; Fingerson, S.; Albrecht, M.; Maiers, M.; Kalaycio, M.; Hill, B.T. Fine-mapping of HLA associations with chronic lymphocytic leukemia in US populations. Blood 2014, 124, 2657–2665. [Google Scholar] [CrossRef]
- Machulla, H.; Schaaf, A.; Kujat, G.; Langner, J. Association of chronic lymphocytic leukemia with specific alleles of the HLA-DR4:DR53:DQ8 haplotype in German patients. Int. J. Cancer 2001, 92, 203–207. [Google Scholar] [CrossRef]
- Slager, S.L.; Rabe, K.G.; Achenbach, S.J.; Vachon, C.M.; Goldin, L.R.; Strom, S.S.; Lanasa, M.C.; Spector, L.G.; Rassenti, L.Z.; Leis, J.F.; et al. Genome-wide association study identifies a novel susceptibility locus at 6p21.3 among familial CLL. Blood 2011, 117, 1911–1916. [Google Scholar] [CrossRef] [PubMed]
- Mueller, L.P.; Machulla, H.K.G. Increased frequency of homozygosity for HLA class II loci in female patients with chronic lymphocytic leukemia. Leuk. Lymphoma 2002, 43, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Slager, S.L.; Skibola, C.F.; Di Bernardo, M.C.; Conde, L.; Broderick, P.; McDonnell, S.K.; Goldin, L.R.; Croft, N.; Holroyd, A.; Harris, S.; et al. Common variation at 6p21.31 (BAK1) influences the risk of chronic lymphocytic leukemia. Blood 2012, 120, 843–846. [Google Scholar] [CrossRef]
- Berndt, S.I.; Skibola, C.F.; Joseph, V.; Camp, N.J.; Nieters, A.; Wang, Z.; Cozen, W.; Monnereau, A.; Wang, S.S.; Kelly, R.S.; et al. Genome-wide association study identifies multiple risk loci for chronic lymphocytic leukemia. Nat. Genet. 2013, 45, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Speedy, H.E.; Di Bernardo, M.C.; Sava, G.P.; Dyer, M.J.S.; Holroyd, A.; Wang, Y.; Sunter, N.J.; Mansouri, L.; Juliusson, G.; Smedby, K.E.; et al. A genome-wide association study identifies multiple susceptibility loci for chronic lymphocytic leukemia. Nat. Genet. 2014, 46, 56–60. [Google Scholar] [CrossRef]
- Berndt, S.I.; Camp, N.J.; Skibola, C.F.; Vijai, J.; Wang, Z.; Gu, J.; Nieters, A.; Kelly, R.S.; Smedby, K.E.; Monnereau, A.; et al. Meta-analysis of genome-wide association studies discovers multiple loci for chronic lymphocytic leukemia. Nat. Commun. 2016, 7, 10933. [Google Scholar] [CrossRef]
- Law, P.J.; Berndt, S.I.; Speedy, H.E.; Camp, N.J.; Sava, G.P.; Skibola, C.F.; Holroyd, A.; Vijai, J.; Sunter, N.J.; Nieters, A.; et al. Genome-wide association analysis implicates dysregulation of immunity genes in chronic lymphocytic leukaemia. Nat. Commun. 2017, 8, 14175. [Google Scholar] [CrossRef]
- Law, P.J.; Sud, A.; Mitchell, J.S.; Henrion, M.; Orlando, G.; Lenive, O.; Broderick, P.; Speedy, H.E.; Johnson, D.C.; Kaiser, M.; et al. Genome-wide association analysis of chronic lymphocytic leukaemia, Hodgkin lymphoma and multiple myeloma identifies pleiotropic risk loci. Sci. Rep. 2017, 7, 41071. [Google Scholar] [CrossRef]
- Crowther-Swanepoel, D.; Mansouri, M.; Enjuanes, A.; Vega, A.; Smedby, K.E.; Ruiz-Ponte, C.; Jurlander, J.; Juliusson, G.; Montserrat, E.; Catovsky, D.; et al. Verification that common variation at 2q37.1, 6p25.3, 11q24.1, 15q23, and 19q13.32 influences chronic lymphocytic leukaemia risk. Br. J. Haematol. 2010, 150, 473–479. [Google Scholar] [CrossRef]
- Sava, G.P.E.; Speedy, H.; Di Bernardo, M.C.; Dyer, M.J.S.; Holroyd, A.; Sunter, N.J.; Marr, H.; Mansouri, L.; Deaglio, S.; Karabon, L.; et al. Common variation at 12q24.13 (OAS3) influences chronic lymphocytic leukemia risk. Leukemia 2014, 29, 748–751. [Google Scholar] [CrossRef]
- Vijai, J.; Wang, Z.; Berndt, S.I.; Skibola, C.F.; Slager, S.L.; De Sanjose, S.; Melbye, M.; Glimelius, B.; Bracci, P.M.; Conde, L.; et al. A genome-wide association study of marginal zone lymphoma shows association to the HLA region. Nat. Commun. 2015, 6, 5751. [Google Scholar] [CrossRef] [PubMed]
- Vijai, J.; Wang, Z.; Berndt, S.I.; Slager, S.L.; Cerhan, J.R.; Skibola, C.; Wang, S.S.; Brooks-Wilson, A.R.; De Sanjosé, S.; Bracci, P.M.; et al. Abstract 5071: A genome-wide association study suggests evidence of variants at 6p21.32 associated with marginal zone lymphoma. In Proceedings of the Epidemiology, American Association for Cancer Research (AACR), New Orleans, LA, USA, 20–23 September 2014; Volume 74, p. 5071. [Google Scholar]
- Bracci, P.M.; Benavente, Y.; Turner, J.J.; Paltiel, O.; Slager, S.L.; Vajdic, C.M.; Norman, A.D.; Cerhan, J.R.; Chiu, B.C.H.; Becker, N.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Marginal Zone Lymphoma: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Nat. Cancer Inst. Monogr. 2014, 2014, 52–65. [Google Scholar] [CrossRef] [PubMed]
- LaBreche, K.; Daniau, M.; Sud, A.; Law, P.J.; Royer-Perron, L.; Holroyd, A.; Broderick, P.; Went, M.; Benazra, M.; Ahle, G.; et al. A genome-wide association study identifies susceptibility loci for primary central nervous system lymphoma at 6p25.3 and 3p22.1: A LOC Network study. Neuro-Oncol. 2019, 21, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Garcilazo-Reyes, Y.; Ibáñez-Juliá, M.-J.; Hernández-Verdin, I.; Nguyen-Them, L.; Younan, N.; Houillier, C.; Hoang-Xuan, K.; Alentorn, A. Treating central nervous system lymphoma in the era of precision medicine. Expert Rev. Precis. Med. Drug Dev. 2020, 5, 275–281. [Google Scholar] [CrossRef]
- Yu, C.C.; Chen, L.C.; Huang, C.Y.; Lin, V.C.; Lu, T.L.; Lee, C.H.; Huang, S.; Bao, B.Y. Genetic association analysis identifies a role for ANO5 in prostate cancer progression. Cancer Med. 2020, 9, 2372–2378. [Google Scholar] [CrossRef]
- Tan, D.E.K.; Foo, J.N.; Bei, J.X.; Chang, J.; Peng, R.; Zheng, X.; Wei, L.; Huang, Y.; Lim, W.Y.; Li, J.; et al. Genome-wide association study of B cell non-Hodgkin lymphoma identifies 3q27 as a susceptibility locus in the Chinese population. Nat. Genet. 2013, 45, 804–807. [Google Scholar] [CrossRef]
- Slager, S.L.; Camp, N.J.; Conde, L.; Shanafelt, T.D.; Achenbach, S.J.; Rabe, K.G.; Kay, N.E.; Novak, A.J.; Call, T.G.; Bracci, P.M.; et al. Common variants within 6p21.31 locus are associated with chronic lymphocytic leukaemia and, potentially, other non-Hodgkin lymphoma subtypes. Br. J. Haematol. 2012, 159, 572–576. [Google Scholar] [CrossRef]
- Casellas, R.; Basu, U.; Yewdell, W.T.; Chaudhuri, W.T.Y.J.; Robbiani, D.F.; Di Noia, J.M. Mutations, kataegis and translocations in B cells: Understanding AID promiscuous activity. Nat. Rev. Immunol. 2016, 16, 164–176. [Google Scholar] [CrossRef]
- Kohli, R.M.; Maul, R.W.; Guminski, A.F.; McClure, R.L.; Gajula, K.S.; Saribasak, H.; McMahon, M.A.; Siliciano, R.F.; Gearhart, P.J.; Stivers, J.T. Local Sequence Targeting in the AID/APOBEC Family Differentially Impacts Retroviral Restriction and Antibody Diversification. J. Biol. Chem. 2010, 285, 40956–40964. [Google Scholar] [CrossRef]
- Kasar, S.; Kim, J.; Improgo, R.; Tiao, G.; Polak, P.; Haradhvala, N.; Lawrence, M.S.; Kiezun, A.; Fernandes, S.M.; Bahl, S.; et al. Whole-genome sequencing reveals activation-induced cytidine deaminase signatures during indolent chronic lymphocytic leukaemia evolution. Nat. Commun. 2015, 6, 8866. [Google Scholar] [CrossRef]
- Holmes, A.B.; Corinaldesi, C.; Shen, Q.; Kumar, R.; Compagno, N.; Wang, Z.; Nitzan, M.; Grunstein, E.; Pasqualucci, L.; Dalla-Favera, R.; et al. Single-cell analysis of germinal-center B cells informs on lymphoma cell of origin and outcome. J. Exp. Med. 2020, 217, e20200483. [Google Scholar] [CrossRef] [PubMed]
| Study | Year | Race/Ethnicity | #Cases/#Controls | SNP/Alteration | Chr | Gene(s) | OR (95% CI) | p-Value | Reference |
|---|---|---|---|---|---|---|---|---|---|
| DLBCL risk | 2009 | European | 783/3377 | rs6457327 | 6p21.33 | PSORS1 * | 1.69 (1.43–2.00) | 7.0 × 10−5 | [54] |
| 2011 | European | 1592/6581 | rs10484561 | 6p21.32 | HLA-DQB1 | 1.36 (1.21–1.52) | 1.4 × 10−7 | [34] | |
| 2011 | Asian | 399/4243 | rs751837 | 14q32 | CDC42BPB | 3.5 (2.127–5.88) | 3.3 × 10−7 | [39] | |
| rs7097 | 13q12 | LNX2 | 1.437 (1.23–1.67 | 6.5 × 10−6 | |||||
| rs4551233 | 7 | POU6F2 | 1.57 (1.32–1.88) | 7.05 × 10−7 | |||||
| rs4443228 | 4 | -- | 2.43 (1.70–3.45) | 7.03 × 10−7 | |||||
| 2013 | Asian | 1328/6930 | rs6773854 | 3q27 | BCL6 *, LPP * | 1.47 (1.32–1.65) | 1.14 × 10−11 | [69,78] | |
| 2014 | European | 3857/7666 | rs2523607 | 6p21.33 | HLA-B | 1.32 (1.21–1.44) | 2.40 × 10−10 | [32] | |
| rs116446171 | 6p25.3 | EXOC2 * | 2.20 (1.87–2.59) | 2.33 × 10−21 | |||||
| rs79480871 | 2p23.3 | NCOA1 | 1.34 (1.21–1.49) | 4.23 × 10−8 | |||||
| rs13255292 | 8q24.21 | PVT1 | 1.22 (1.15–1.29) | 9.98 × 10−13 | |||||
| rs4733601 | 1.18 (1.11–1.25) | 3.63 × 10−11 | |||||||
| rs79464052 | 5q31.3 | ARAP3 | 1.34 (1.21–1.49) | 5.57 × 10−8 | |||||
| rs2681416 | 3q13.33 | CD86 | 1.16 (1.10–1.23) | 8.17 × 10−8 | |||||
| 2015 | Asian | 1124/3596 | rs116446171 | 6p25.3 | EXOC2 * | 2.04 (1.63–2.56) | 3.9 × 10−10 | [33] | |
| rs13255292 | 8q24.21 | PVT1 | 1.34 (1.19–1.52) | 2.1 × 10−6 | |||||
| rs2523607 | 6p21.33 | HLA-B | 3.05 (1.32–7.05 | 9 × 10−3 | |||||
| 2018 | European | 3617/8753 | Homozygosity | 6p21.33 | HLA-B, HLA-C | 1.31 (1.06–1.60) | 8 × 10−4 | [35] | |
| 2018 | Homozygosity | HLA-DRB1 | 2.10 (1.24–3.55) | 1 × 10−4 | |||||
| 2019 | European | 5662/9237 | rs9831894 | 3q13.33 | CD86 *, ILDR1 * | 0.83 | 3.62 × 10−13 | [36] | |
| 5510/12,817 | rs6773363 | 3p24.1 | EOMES *, AZI2 * | 1.20 | 2.31 × 10−12 | ||||
| DLBCL-SLE | 2017 | European | 3857/7666 | rs4810485 | 20q13 | CD40 | 1.09 (1.02–1.16) | 0.013 | [19] |
| rs1270942 | 6p21.33 | HLA | 1.17 (1.01–1.36) | 0.036 | |||||
| 2019 | European | 3617/46,436 | rs1270942 | 6 | RDBP | NA | 5 × 10−8 | [11] | |
| rs3130557 | 6 | PSORS1C1 | NA | ||||||
| rs4733601 | 8 | PVT1 | NA | ||||||
| DLBCL-MS | rs2425752 | 20 | NCOA5 | 0.91 | 3.4 × 10−2 | ||||
| FL-risk | 2009 | European | 645/3377 | rs6457327 | 6p21.33 | PSORS1 * | 1.69 (1.43–2.00) | 4.7 × 10−11 | [54] |
| 2010 | European | 1465/6958 | rs10484561 | 6p21.32 | HLA-DQB1 | 1.95 (1.72–2.22) | 1.12 × 10−29 | [50] | |
| rs7755224 | 6p21.32 | 2.07 (1.76–2.42) | 2.0 × 10−19 | ||||||
| 2011 | European | 1428/6761 | rs10484561 | 6p21.32 | HLA-DQB1 | 1.64 (1.45–1.86) | 5 × 10−15 | [34] | |
| rs2647012 | 6p21.32 | 0.70 (0.67–0.78) | 4 × 10−12 | ||||||
| 2012 | Caucasians | 699/2222 | rs9275517 | 6p21.32 | HLA-DRB1 * | 0.63 (0.55–0.73) | 4.0 × 10−11 | [53] | |
| rs3117222 | HLA-DPB1 * | 0.66 (0.57–0.77) | 1.45 × 10−7 | ||||||
| 2013 | Caucasians | 238/1233 | rs2647012 | 6p21.32 | HLA-DQB1 | 0.56 (0.45–0.69) | 8.03 × 10−8 | [52] | |
| rs241447 | 6p21.3 | TAP2 | 1.82 (1.46–2.26) | 6.9 × 10−8 | |||||
| Asian | 792/1542 | rs2647012 | 6p21.32 | HLA-DQB1 | 1.20 (1.03–1.39) | 0.018 | [51] | ||
| rs872071 | 6p25.3 | IRF4 | 1.20 (1.05–1.38) | 0.009 | |||||
| 2014 | European | 4523/13,344 | rs12195582 | 6p21.32 | HLA-DRB5 | 1.78 (1.68–1.88) | 5.36 × 10−100 | [54] | |
| rs17203612 | 6p21.32 | HLA-DRB1 | 1.43 (1.32–1.57) | 4.59 × 10−16 | |||||
| rs4938573 | 11q23.3 | CXCR5 * | 1.34 (1.26–1.43) | 5.79 × 10−20 | |||||
| rs4937362 | 11q24.3 | ETS1 * | 1.19 (1.13–1.25) | 6.76 × 10−11 | |||||
| rs6444305 | 3q28 | LPP | 1.21 (1.14–1.28) | 1 × 10−10 | |||||
| rs17749561 | 18q21.33 | BCL2 * | 1.34 (1.22–1.47) | 8.28 × 10−10 | |||||
| rs13254990 | 8q24.21 | PVT1 * | 1.18 (1.11–1.24) | 1.06 × 10−8 | |||||
| rs3751913 | 17q25.3 | CYBC1 | 1.23 (1.14–1.33) | 2.24 × 10−7 | |||||
| rs2681416 | 3q13.33 | CD86 | 1.16 (1.09–1.22) | 2.33 × 10−7 | |||||
| rs11082438 | 18q12.3 | SLC14A2 | 1.33 (1.19–1.48) | 4.01 × 10−7 | |||||
| 2018 | European | 2686/8753 | Homozygosity | 6p21.32 | HLA-DRB1 | 1.54 (1.31–1.82) | 1 × 10−4 | [35] | |
| Homozygosity | 6p21.32 | HLA-DQB1 | 1.42 (1.23–1.65) | 1 × 10−4 | |||||
| FL-DLBCL | 2011 | European | 1428/6581 | rs2647012 | 6p21.32 | HLA-DQB1 | 1.36 | 1.4 × 10−7 | [50] |
| FL-SLE | 2019 | European | 2686/46,436 | rs1015166 | 6 | TAP2 | NA | 5 × 10−8 | [11] |
| rs1894406 | 6 | HLA-DOB | NA | ||||||
| rs2071475 | 6 | HLA-DOB | NA | ||||||
| rs2072634 | 6 | CFB | NA | ||||||
| rs2293861 | 6 | MSH5 | NA | ||||||
| rs7774197 | 6 | TNXB | NA | ||||||
| rs9271775 | 6 | HLA-DRB1 | NA | ||||||
| rs4938573 | 11 | LOC649925 | NA | ||||||
| rs7444 | 22 | UBE2L3 | NA | ||||||
| CLL-risk | 2001 | European | 101/157 | --- | 6 | HLA-DRB4 *0103 | 2.74 | 2.5 × 10−3 | [60] |
| 2008 | European | 1529/3115 | rs17483466 | 2q13 | ACOXL, BCL2L11 | 1.39 (1.25–1.53) | 2.36×10−10 | [55] | |
| rs13397985 | 2q37.1 | SP140 *, SP110 * | 1.41 (1.26–1.57) | 5.40 × 10−10 | |||||
| rs872071 | 6p25.3 | IRF4 | 1.54 (1.41–1.69) | 1.91 × 10−20 | |||||
| rs9378805 | 6p25.3 | IRF4 | 1.51 (1.38–1.65) | 4.62 × 10−19 | |||||
| rs735665 | 11q24.1 | GRAMD1B | 1.45 (1.31–1.61) | 3.78 × 10−12 | |||||
| rs7176508 | 15q23 | --- | 1.37 (1.26–1.50) | 4.54 × 10−12 | |||||
| rs11083846 | 19q13.32 | PRKD2 | 1.35 (1.22–1.49) | 3.96 × 10−9 | |||||
| 2010 | European | 824/850 | rs872071 | 6p25.3 | IRF4 | 1.42 (1.23–1.63) | 9.96 × 10−7 | [56] | |
| rs735665 | 11q24.1 | GRAMD1B | 1.59 (1.34–1.88) | 1.23 × 10−7 | |||||
| 2010 | 2503/5789 | rs757978 | 2q37.3 | FARP2 | 1.39 | 2.11 × 10−9 | [62] | ||
| rs2456449 | 8q24.21 | --- | 1.26 | 7.84 × 10−10 | |||||
| rs7169431 | 15q21.3 | IRF8 * | 1.36 | 4.74 × 10−7 | |||||
| rs305061 | 16q24.1 | NEDD4 *, RFX7 * | 1.22 | 3.60 × 10−7 | |||||
| 2011 | Caucasians | 690/1295 | rs305077 | 16q24.1 | IRF8 | 0.66 (0.57–0.77) | 3.37 × 10−8 | [62] | |
| rs391525 | 0.64 (0.55–0.74) | 3.16 × 10−9 | |||||||
| rs2292982 | 0.65 (0.56–0.75) | 6.48 × 10−9 | |||||||
| rs2292980 | 0.66 (0.56–0.76) | 1.89 × 10−8 | |||||||
| rs615672 | 6p21.3 | HLA-DRB5 | 1.42 (1.22–1.67) | 1.29 × 10−5 | |||||
| rs674313 | 1.69 (1.41–2.01) | 6.92 × 10−9 | |||||||
| rs502771 | 1.61 (1.36–1.91) | 5.58 × 10−8 | |||||||
| rs9272219 | HLA-DQA1 | 1.59 (1.34–1.90) | 1.84 × 10−7 | ||||||
| rs9272535 | 1.61 (1.35–1.92) | 9.31 × 10−8 | |||||||
| 2012 | European/American | 1982/5778 | rs210142 | 6p21.33 | BAK1 | 1.40 (1.25–1.57) | 9.47 × 10−16 | [64] | |
| 2012 | European/American | 1196/2410 | rs210142 | 6p21.33 | BAK1 | 0.73 (0.68–0.79) | 2.28 × 10−16 | [79] | |
| 2013 | European | 3100/7667 | rs4406737 | 10q23.31 | ACTA2 *, FAS * | 1.27 (1.19–1.33) | 1.22 × 10−14 | [65] | |
| rs4987855 | 18q21.33 | BCL2 | 1.47 (1.32–1.61) | 2.66 × 10−12 | |||||
| rs4987852 | 1.41 (1.27–1.56) | 7.76 × 10−11 | |||||||
| rs7944004 | 11p15.5 | C11orf21, * TSPAN32 * | 1.20 (1.13–1.27) | 2.15 × 10−10 | |||||
| rs898518 | 4q25 | LEF1 | 1.20 (1.14–1.27) | 4.24 × 10−10 | |||||
| rs3769825 | 2q33.1 | CASP10, CASP8 | 1.19 (1.12–1.25) | 2.50 × 10−9 | |||||
| rs1679013 | 9p21.3 | CDKN2B-AS1 | 1.19 (1.12–1.27) | 1.27 × 10−8 | |||||
| rs4368253 | 18q21.32 | PMAIP1 | 1.19 (1.12–1.27) | 2.51 × 10−8 | |||||
| rs8024033 | 15q15.1 | BMF | 1.22 (1.15–1.30) | 2.71 × 10−10 | |||||
| rs3770745 | 2p22.2 | QPCT *, PRKD3 * | 1.24 (1.15–1.33) 1.68 × 10−8 | 1.68 × 10−8 | |||||
| rs13401811 | 2q13 | ACOXL *, BCL2L11 * | 1.41 (1.30–1.52) | 2.08 × 10−18 | |||||
| 2014 | Europeans | 3748/8574 | rs10735079 | 12q24.13 | OAS3 | 1.18 (1.12–1.26) | 2.34 × 10−8 | [71] | |
| 2014 | Europeans | 2883/8350 | rs2236256 | 6q25.2 | IPCEF1 | 1.23 (1.15–1.30) | 1.5 × 10−10 | [66] | |
| rs10936599 | 3q26.2 | MYNN | 1.26 (1.17–1.35) | 1.74 × 10−9 | |||||
| rs6858698 | 4q26 | CAMK2D | 1.31 (1.20–1.44) | 3.07 × 10−9 | |||||
| rs17246404 | 7q31.33 | POT1 | 1.22 (1.14–1.31) | 3.40 × 10−8 | |||||
| rs1439287 | 2q13 | ACOXL | 1.37 | 5 × 10−15 | |||||
| rs13397985 | 2q37.1 | SP140 | 1.43 | 5 × 10−13 | |||||
| rs872071 | 6p25.3 | IRF4 | 1.39 | 3 × 10−16 | |||||
| rs735665 | 11q24.1 | GRAMD1B | 1.64 | 4 × 10−24 | |||||
| rs7176508 | 15q23 | DRAIC | 1.42 | 8 × 10−18 | |||||
| rs1044873 | 16.q24.1 | IRF8 | 1.29 | 1 × 10−9 | |||||
| 2014 | Caucasian | 3616/50,000 | --- | 6 | HLA-DRB4 *01:01∼DRB1 *07:01∼DQB1 *03:03 | 1.49 | 1.79 × 10−7 | [60] | |
| African-American | 413/50,000 | 6 | 28.03 | 2 × 10−16 | |||||
| Hispanic | 97/50,000 | 6 | 13.86 | 9.59 × 10−9 | |||||
| 2016 | Europeans | 5058/13,197 | rs9880772 | 3p24.1 | EOMES | 1.19 (1.13–1.25) | 2.5 × 10−11 | [67] | |
| rs73718779 | 6p25.2 | SERPINB6 | 1.26 (1.16–1.36) | 1.97 × 10−8 | |||||
| rs9815073 | 3q28 | LPP | 1.18 (1.11–1.25) | 3.26 × 10−8 | |||||
| rs9308731 | 2q13 | BCL2L11 | 1.19 (1.13–1.26) | 1 × 10–11 | |||||
| rs10028805 | 4q24 | BANK1 | 1.16 (1.10–1.22) | 7.19 × 10−8 | |||||
| rs1274963 | 3p22.2 | CSRNP1 | 1.18 (1.11–1.25) | 2.12 × 10−7 | |||||
| 2017 | Europeans | 6200/17,598 | rs34676223 | 1p36.11 | MDS2 | 1.19 (1.14–1.25) | 5.04 × 10−13 | [68] | |
| rs41271473 | 1q42.13 | RHOU | 1.19 (1.13–1.26) | 1.06 × 10−10 | |||||
| rs71597109 | 4q24 | BANK1 | 1.17 (1.11–1.22) | 1.37 × 10−10 | |||||
| rs57214277 | 4q35.1 | MYL12BP2 *, LINC02363 * | 1.13 (1.08–1.18) | 3.69 × 10−8 | |||||
| rs3800461 | 6p21.31 | ILRUN | 1.20 (1.13–1.28) | 1.97 × 10−8 | |||||
| rs61904987 | 11q23.2 | TMPRSS5 *, DRD2 * | 1.24 (1.16–1.32) | 2.46 × 10−11 | |||||
| rs1036935 | 18q21.1 | AC105227.1 *, AC105227.2 * | 1.15 (1.10–1.21) | 3.27 × 10−8 | |||||
| rs7254272 | 19p13.3 | ZBTB7A *, MAP2K2 * | 1.17 (1.10–1.23) | 4.67 × 10−8 | |||||
| rs140522 | 22q13.33 | ODF3B | 1.15 (1.10–1.20) | 2.7 × 10−9 | |||||
| 2017 | Europeans | 1842/7324 | rs11715604 | 3q22 | NCK1 | NA | 1.97 × 10−8 | [69] | |
| rs131821 | 22q13.33 | NCAPH2 | NA | 7.49 × 10−8 | |||||
| CLL-SLE | 2019 | European | 2492/46,436 | rs10028805 | 4 | BANK1 | NA | 5 × 10−8 | [11] |
| rs1270942 | 6 | RDBP | NA | ||||||
| rs17587 | 6 | PSMB9 | NA | ||||||
| rs3130557 | 6 | PSORS1C1 | NA | ||||||
| rs4987855 | 18 | BCL2 | NA | ||||||
| rs1439112 | 2 | MGAT5 | 0.88 | 4.7 × 10−2 | |||||
| rs10936599 | 3 | MYNN, ACTRT3, TERC, LRRC34 | 0.86 | 2.7 × 10−2 | |||||
| rs1317082 | 3 | 1.5 × 10−2 | |||||||
| rs13069553 | 3 | 1.07 × 10−2 | |||||||
| rs7621631 | 3 | 1.8 × 10−2 | |||||||
| rs10069690 | 5 | TERT | 1.16 | 3.06 × 10−2 | |||||
| CLL-MS | rs140522 | 22 | ODF3B | 0.90 | 4.32 × 10−4 | ||||
| rs6793295 | 3 | LRRC34 | 0.90 | 1.24 × 10−2 | |||||
| CLL-RA | rs3731714 | 2 | CASP10, PPIL3, CFLAR | 0.87 | 4.69 × 10−2 | ||||
| MZL-risk | 2015 | European | 1281/7127 | rs2922994 | 6p21.32 | HLA-B | 1.64 (1.39–1.92) | 2.43 × 10−9 | [63] |
| rs9461741 | 6p21.32 | BTNLA | 2.24 (1.64–3.07) | 3.95 × 10−15 | |||||
| 2018 | European | 741/8753 | Homozygosity | 6p21.33 | HLA-B | 1.34 (1.01–1.78) | 0.012 | [35] | |
| Homozygosity | 6p21.33 | HLA-C | 1.33 (1.04–1.70) | ||||||
| Homozygosity | 6p21.33 | HLA-DRB1 | 1.45 (1.05–1.91) | ||||||
| MZL-SLE | 2019 | European | 741/46,436 | rs1270942 | 6 | RDBP | NA | 5 × 10−8 | [11] |
| rs3130557 | 6 | PSORS1C1 | NA | ||||||
| rs532098 | 6 | HLA-DQA1 | NA | ||||||
| MZL-RA | rs16947122 | 12 | FBXW8, HRK, TESC | 1.86 | 3.35 × 10−2 | ||||
| rs1364229 | 16 | CDH8 | 1.35 | 1.10 × 10−3 | |||||
| rs7192064 | 16 | CDH8 | 0.76 | 4.36 × 10−2 | |||||
| rs2131402 | 16 | CDH8 | 0.75 | 1.01 × 10−2 | |||||
| PCNSL-risk | 2013 | European | 475/1134 | rs41289586 | 3p22.1 | ANO10 | 3.82 (2.39–6.09) | 2.17×10−8 | [66] |
| rs116446171 | 6p25.3 | EXOC2 * | 4.99 (3.26–7.65) | 1.95 × 10−13 | |||||
| rs2395192 | 6p21 | HLA-DRA *, HLA-DRB5 * | 1.51 (1.29–1.76) | 1.81×10−7 |
| Study | Year | Race/Ethnicity | # Cases | SNP/Alteration | Chr | Gene(s) | HR (95% CI) | p-Value | Outcome | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| DLBCL | 2015 | European | 1537 | rs7712513 | 5q23.2 | SNX2 *, SNCAIP * | 1.49 (1.29–1.72) | 3.53 × 10−8 | ↓ OS | [28] |
| 1.39 (1.23–1.57) | 2.08 × 10−7 | ↓ PFS | ||||||||
| rs7765004 | 6q21 | MARCK *, HDACS2 * | 1.47 (1.27–1.71) | 5.36 × 10−7 | ↓ OS | |||||
| 1.38 (1.22–1.57) | 7.09 × 10−7 | ↓ PFS | ||||||||
| 2018 | European | 210 | --- | 1q23.3 | FCGR2B | 2.18 | 5.7 × 10−3 | ↓ OS | [40] | |
| FL | 2014 | European | 586 | rs10491178 | 17q24 | ABCA10 *, ABCA6 * | 3.17 (2.09–4.79) | 5.24 ×10−8 | ↓ PFS | [47] |
| rs2466571 | 1q32.2 | CD46 | 0.73 (0.58–0.91) | 6 × 10−3 | ↑ EFS | |||||
| rs4073 | 4q13.3 | IL8 | 0.78 (0.62–0.97) | 0.02 | ↑ EFS | |||||
| rs1801131 | 1p36.22 | MTHFR | 0.59 (0.45–0.77) | 1 × 10−4 | ↑ EFS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Verdin, I.; Labreche, K.; Benazra, M.; Mokhtari, K.; Hoang-Xuan, K.; Alentorn, A. Tracking the Genetic Susceptibility Background of B-Cell Non-Hodgkin’s Lymphomas from Genome-Wide Association Studies. Int. J. Mol. Sci. 2021, 22, 122. https://doi.org/10.3390/ijms22010122
Hernández-Verdin I, Labreche K, Benazra M, Mokhtari K, Hoang-Xuan K, Alentorn A. Tracking the Genetic Susceptibility Background of B-Cell Non-Hodgkin’s Lymphomas from Genome-Wide Association Studies. International Journal of Molecular Sciences. 2021; 22(1):122. https://doi.org/10.3390/ijms22010122
Chicago/Turabian StyleHernández-Verdin, Isaias, Karim Labreche, Marion Benazra, Karima Mokhtari, Khê Hoang-Xuan, and Agusti Alentorn. 2021. "Tracking the Genetic Susceptibility Background of B-Cell Non-Hodgkin’s Lymphomas from Genome-Wide Association Studies" International Journal of Molecular Sciences 22, no. 1: 122. https://doi.org/10.3390/ijms22010122
APA StyleHernández-Verdin, I., Labreche, K., Benazra, M., Mokhtari, K., Hoang-Xuan, K., & Alentorn, A. (2021). Tracking the Genetic Susceptibility Background of B-Cell Non-Hodgkin’s Lymphomas from Genome-Wide Association Studies. International Journal of Molecular Sciences, 22(1), 122. https://doi.org/10.3390/ijms22010122




