Nasal Polyposis: Insights in Epithelial-Mesenchymal Transition and Differentiation of Polyp Mesenchymal Stem Cells
Abstract
1. Introduction
1.1. Chronic Rhinosinusitis (CRS) Classification
1.2. Etiology of Polyp Formation
1.3. Inflammation in Nasal CRS
1.4. Immunological-Based Therapies
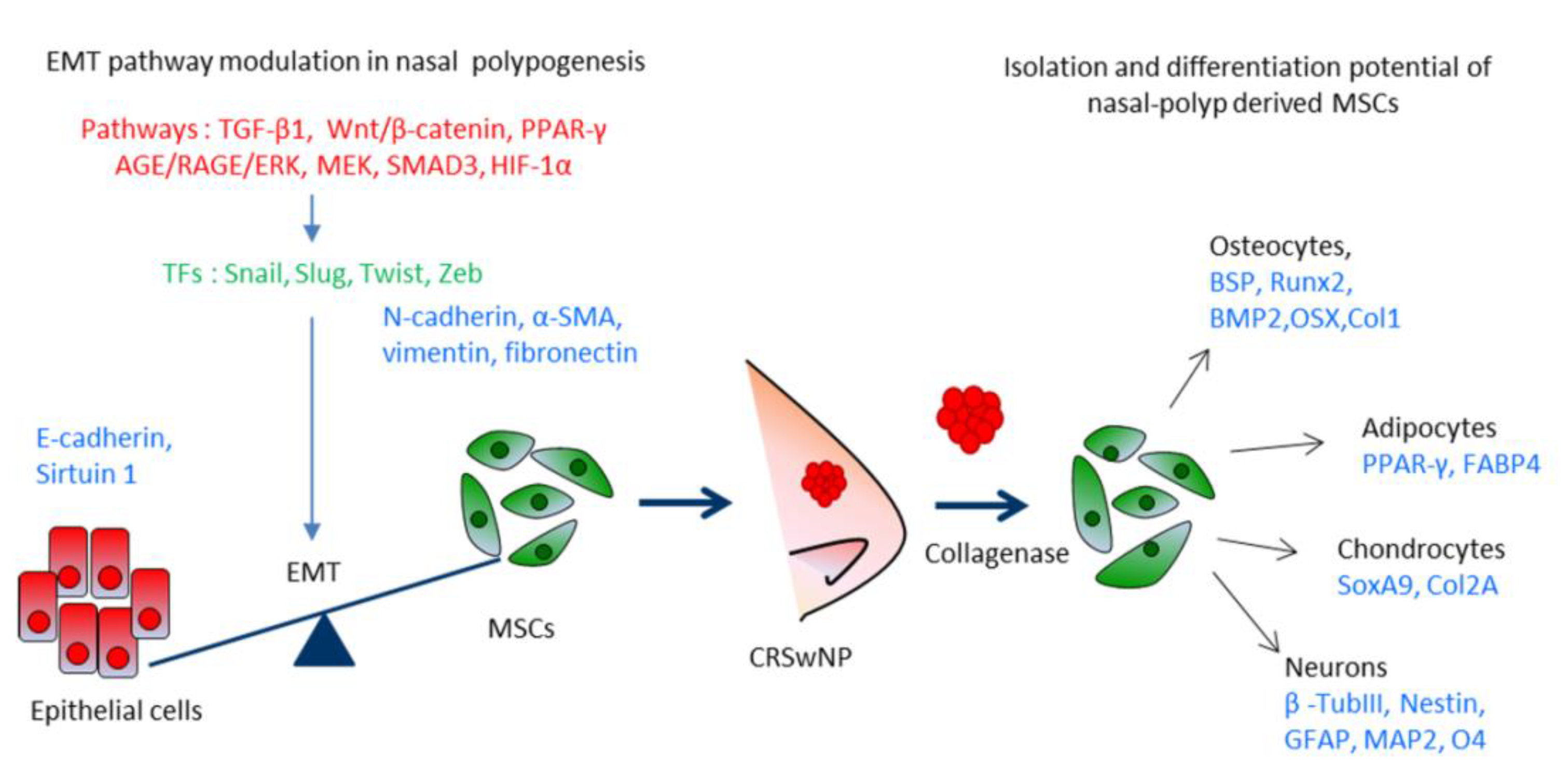
2. Intra-Cellular Signaling Transduction Mechanisms Underlying the Development of Nasal Polyps (CRSwNP)
2.1. TGF-β1 Is Involved in CRSwNP Pathogenesis
2.2. SMAD3 and HIF-1α Signaling Are Involved in CRSwNP
2.3. MEK1/2-ERK1/2 Signaling Pathways in CRSwNP
2.4. AGE/RAGE/ERK Signaling Pathways in CRSwNP
2.5. WNT/β-Catenin/GSK Signaling Are Involved in CRSwNP
2.6. PPARγ Signaling Pathway Plays a Role in CRSwNP
3. Gene Expression Studies on Nasal Polyps and Their Derived MSCs Cells
3.1. Characteristics of Nasal Polyp-Derived Mesenchymal Stem Cells
3.2. Osteogenic Differentiation
3.3. Adipocyte Differentiation
3.4. Chondrocyte Differentiation
3.5. Neural Differentiation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CRS | Chronic rhinosinusitis |
| EPOS | European Position Paper on Rhinosinusitus and Nasal Polyps |
| CRSwNP | CRS with nasal polyps |
| CRSsNP | CRS without nasal polyps |
| AFRS | allergic fungal rhinosinusitis |
| eCRS | eosinophilic CRS |
| CCAD | central compartment allergic disease |
| GPA | Granulomatosis with polypangiitis |
| PO-MSCs | Polyp derived mesenchymal stem cells |
| EMT | Epithelial-mesenchymal transition |
| α-SMA | alpha-smooth muscle actin |
| MMP | Matrix metalloproteinases |
| TGF-β | Transforming growth factor beta |
| SMAD | Small Mothers Against Decapentaplegic |
| IFNγ | Interferon γ |
| Th2 T helper | Type2 T helper |
| ILC2 | Type2 innate helper lymphoid cells |
| CCL11 | Eotaxin-1 |
| HIF-1α | Hypoxia-inducible factor |
| 2ME2 | Methoxyestradiol |
| 17-AAG | 17-allylaminogeldanamycin |
| AGE | Advanced Glycation Endproducts |
| RAGE | Receptor for advanced glycation endproducts |
| ERK | Extracellular signal-regulated kinases |
| MEK | Mitogen-Activated Protein Kinase Kinase |
| Wnt | Wingless-Type MMTV Integration Site Family |
| GSK3 | Glycogen synthase kinase 3 |
| PPARγ | Peroxisome proliferator-activated receptor gamma |
| XBP1 | X-box binding protein 1 |
| PBA | 4-phenylbutylic acid |
| PP2 | c-Src kinase inhibitor |
| GRP78 | Glucose-regulated protein 78 |
| PNECs | Primary nasal epithelial cells |
| PTEN | Phosphatase And Tensin Homolog |
| MAPK | Mitogen-Activated Protein Kinase |
| NF-κB | Nuclear factor-κB |
| JAK-STAT | Janus Kinase-Signal transducer and activator of transcription |
| HNEpCS | Human Nasal Epithelial Cells |
| ROG | Rosiglitazone |
| ZO-1 | Zonula occludens-1 |
| HDAC | Histone Deacetylase |
| LPS | Lipopolysaccharide |
| PROM1 | Prominin-1 |
| ABCB1 | ATP-binding cassette sub-family B member 1 |
| HNF1 | Hepatocyte nuclear factor 1-alpha |
| BM-MSCs | Bone marrow mesenchymal stem cells |
| POU2F1 | POU Class 2 Homeobox 1 |
| TFAP4 | Transcription Factor AP-4 |
| GDF6 | Growth Differentiation Factor 6 |
| KDR | Kinase Insert Domain Receptor |
| FGF10 | Fibroblast Growth Factor 10 |
| GDF5 | Growth/differentiation factor 5 |
| HLA-DR | Major Histocompatibility Complex, Class II, DR Alpha |
| PDL-1 | Programmed death-ligand 1 |
| PDL-2 | Programmed death-ligand 2 |
| RORC | RAR Related Orphan Receptor C |
| HMGB1 | High mobility group box 1 protein |
| FOXP3 -2 | Forkhead box protein 3-2 |
| CCL18 | C-C motif) ligand 18 |
| GALNT7 | N-acetylgalactosaminyltransferase 7 |
| RUNX2 | Runt-related transcription factor 2 |
| BMP2 | Bone morphogenetic protein-2 |
| BSP | Bone sialoprotein |
| OSX | Osterix |
| COL1 | type I collagen |
| FABP4 | Fatty acid-binding protein 4 |
| Sox9 | SRY-Box Transcription Factor 9 |
| Col2A | type IIA collagen |
| NF-H | Neurofilamen heavy chain |
| NF-L | Neurofilamen light chain |
| GFAP | Glial fibrillary acidic protein |
| MAP2 | Mutual protection of microtubule-associated protein 2 |
| O4 | Oct4 |
| ADSC | Adipose stem cell |
References
- McCormick, J.P.; Thompson, H.M.; Cho, D.Y.; Woodworth, B.A.; Grayson, J.W. Phenotypes in Chronic Rhinosinusitis. Curr. Allergy Asthma Rep. 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Akdis, C.A. Phenotypes and emerging endotypes of chronic rhinosinusitis. J. Allergy Clin. Immunol. Pract. 2016, 4, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European position paper on rhinosinusitis and nasal polyps. Rhinology 2020, 58 (Suppl. S29), 1–464. [Google Scholar] [CrossRef] [PubMed]
- Koennecke, M.; Klimek, L.; Mullol, J.; Gevaert, P.; Wollenberg, B. Subtyping of polyposis nasi: Phenotypes, endotypes and comorbidities. Allergo J. Int. 2018, 27, 56–65. [Google Scholar] [CrossRef]
- Brescia, G.; Zanotti, C.; Parrino, D.; Barion, U.; Marioni, G. Nasal polyposis pathophysiology: Endotype and phenotype open issues. Am. J. Otolaryngol. 2018, 39, 441–444. [Google Scholar] [CrossRef]
- Stevens, W.W.; Schleimer, R.P.; Kern, R.C. Chronic Rhinosinusitis with Nasal Polyps. J. Allergy Clin. Immunol. Pract. 2016, 4, 565–572. [Google Scholar] [CrossRef]
- Caruso, A.A.; Costigliola, F.; Salzano, J.; Del Prete, S.; Marasco, D.; Imperatore, C.; Telesca, D.A.; Sivero, L. Nasal and systemic eosinophilia associated with solid intestinal tumors, a case report and review of the literature. Ann. Ital. Chir. 2019, 8, pii: S2239253X19029608. [Google Scholar]
- Schleimer, R.P. Immunopathogenesis of Chronic Rhinosinusitis and Nasal Polyposis. Annu. Rev. Pathol. 2017, 12, 331–357. [Google Scholar] [CrossRef]
- Konstantinidis, I.; Witt, M.; Kaidoglou, K.; Constantinidis, J.; Gudziol, V. Olfactory mucosa in nasal polyposis: Implications for FESS outcome. Rhinology 2010, 48, 47–53. [Google Scholar] [CrossRef]
- Muluk, N.B.; Arikan, O.K.; Atasoy, P.; Kiliç, R.; Yalçinozan, E.T. The role of MMP-2, MMP-9, and TIMP-1 in the pathogenesis of nasal polyps: Immunohistochemical assessment at eight different levels in the epithelial, subepithelial, and deep layers of the mucosa. Ear Nose Throat J. 2015, 94, E1–E13. [Google Scholar]
- Fereshteh, E.; Mahdi, B. Recurrent sinonasal polyposis after the endoscopic sinus surgery. Rev. Clin. Med. 2014, 1, 86–92. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, N.; Bo, M.; Holtappels, G.; Zheng, M.; Lou, H.; Wang, H.; Zhang, L.; Bachert, C. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: A multicenter study in Europe, Asia, and Oceania. J. Allergy Clin. Immunol. 2016, 138, 1344–1353. [Google Scholar] [CrossRef] [PubMed]
- Upadhyaya, B.; Yin, Y.; Hill, B.J.; Douek, D.C.; Prussin, C. Hierarchical IL-5 expression defines a subpopulation of highly differentiated human Th2 cells. J. Immunol. 2011, 187, 3111–3120. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, J.C.; Van Dyken, S.J.; von Moltke, J.; Cheng, L.E.; Mohapatra, A.; Molofsky, A.B.; Thornton, E.E.; Krummel, M.F.; Chawla, A.; Liang, H.E.; et al. Type 2 innate lymphoid cells control eosinophil homeostasis. Nature 2013, 502, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Ishinaga, H.; Takeuchi, K. Pathogenesis of eosinophilic chronic rhinosinusitis. J. Inflamm. 2016, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Kariyawasam, H.H.; James, L.K.; Gane, S.B. Dupilumab: Clinical Efficacy of Blocking IL-4/IL-13 Signalling in Chronic Rhinosinusitis with Nasal Polyps. Drug Des. Deve.l Ther. 2020, 14, 1757–1769. [Google Scholar] [CrossRef]
- Avdeeva, K.; Fokkens, W. Precision Medicine in Chronic Rhinosinusitis with Nasal Polyps. Curr. Allergy Asthma Rep. 2018, 18, 25. [Google Scholar] [CrossRef]
- Lombardo, N.; Pelaia, C.; Ciriolo, M.; Della Corte, M.; Piazzetta, G.; Lobello, N.; Viola, P.; Pelaia, G. Real-life effects of benralizumab on allergic chronic rhinosinusitis and nasal polyposis associated with severe asthma. Int. J. Immunopathol. Pharmacol. 2020, 34, 2058738420950851. [Google Scholar] [CrossRef]
- Mukherjee, M.; Sehmi, R.; Nair, P. Anti-IL5 therapy for asthma and beyond. World Allergy Organ. J. 2014, 7, 32. [Google Scholar] [CrossRef]
- Gevaert, P.; Omachi, T.A.; Corren, J.; Mullol, J.; Han, J.; Lee, S.E.; Kaufman, D.; Ligueros-Saylan, M.; Howard, M.; Zhu, R.; et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 2020, 146, 595–605. [Google Scholar] [CrossRef]
- Steinke, J.W.; Crouse, C.D.; Bradley, D.; Hise, K.; Lynch, K.; Kountakis, S.E.; Borish, L. Characterization of interleukin-4-stimulated nasal polyp fibroblasts. Am. J. Respir. Cell Mol. Biol. 2004, 30, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Corren, J. Role of interleukin-13 in asthma. Curr. Allergy Asthma Rep. 2013, 13, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Zhang, N.; Zhang, L.; Bachert, C. Biologics for the treatment of chronic rhinosinusitis with nasal polyps - state of the art. World Allergy Organ. J. 2019, 12, 100050. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650. [Google Scholar] [CrossRef]
- Watelet, J.B.; Demetter, P.; Claeys, C.; Cauwenberge, P.; Cuvelier, C.; Bachert, C. Wound healing after paranasal sinus surgery: Neutrophilic inflammation influences the outcome. Histopathology 2006, 48, 174–181. [Google Scholar] [CrossRef]
- Yu, X.M.; Li, C.W.; Chao, S.S.; Li, Y.Y.; Yan, Y.; Zhao, X.N.; Yu, F.G.; Liu, J.; Shen, L.; Pan, X.L.; et al. Reduced growth and proliferation dynamics of nasal epithelial stem/progenitor cells in nasal polyps in vitro. Sci. Rep. 2014, 4, 4619. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Zhao, X.; Li, C.; Li, Y.; Yan, Y.; Shi, L.; Gordon, B.R.; Wang, D.Y. Airway stem cells: Review of potential impact on understanding of upper airway diseases. Laryngoscope 2012, 122, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.Y.; Li, C.W.; Chao, S.S.; Yu, F.G.; Yu, X.M.; Liu, J.; Yan, Y.; Shen, L.; Gordon, W.; Shi, L.; et al. Impairment of cilia architecture and ciliogenesis in hyperplastic nasal epithelium from nasal polyps. J. Allergy Clin. Immunol. 2014, 134, 1282–1292. [Google Scholar] [CrossRef]
- Klimek, L.; Koennecke, M.; Mullol, J.; Hellings, P.W.; Wang, D.Y.; Fokkens, W.; Gevaert, P.; Wollenberg, B. A possible role of stem cells in nasal polyposis. Allergy 2017, 72, 1868–1873. [Google Scholar] [CrossRef]
- Kalluri, R.; Weinberg, R.A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 2009, 119, 1420–1428. [Google Scholar] [CrossRef]
- Hackett, T.L.; Warner, S.M.; Stefanowicz, D.; Shaheen, F.; Pechkovsky, D.V.; Murray, L.A.; Argentieri, R.; Kicic, A.; Stick, S.M.; Bai, T.R.; et al. Induction of epithelial–mesenchymal transition in primary airway epithelial cells from patients with asthma by transforming growth factor-beta 1. Am. J. Respir. Crit. Care Med. 2009, 180, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Thiery, J.P.; Acloque, H.; Huang, R.Y.; Nieto, M.A. Epithelial-mesenchymal transitions in development and disease. Cell 2009, 139, 871–890. [Google Scholar] [CrossRef] [PubMed]
- Watelet, J.B.; Claeys, C.; Perez-Novo, C.; Gevaert, P.; Van Cauwenberge, P.; Bachert, C. Transforming growth factor beta1 in nasal remodeling: Differences between chronic rhinosinusitis and nasal polyposis. Am. J. Rhinol. 2004, 18, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Van Bruaene, N.; Derycke, L.; Perez-Novo, C.A.; Gevaert, P.; Holtappels, G.; De Ruyck, N.; Cuvelier, C.; Van Cauwenberge, P.; Bachert, C. TGF-beta signaling and collagen deposition in chronic rhinosinusitis. J. Allergy Clin. Immunol. 2009, 124, 253.e1–259.e2. [Google Scholar] [CrossRef]
- Park, I.H.; Kang, J.H.; Shin, J.M.; Lee, H.M. Trichostatin a Inhibits Epithelial Mesenchymal Transition Induced by TGF-β1 in Airway Epithelium. PLoS ONE 2016, 11, e0162058. [Google Scholar] [CrossRef]
- Lee, H.M.; Kang, J.H.; Shin, J.M.; Lee, S.A.; Park, I.H. Chemical Chaperone of Endoplasmic Reticulum Stress Inhibits Epithelial-Mesenchymal Transition Induced by TGF-β1 in Airway Epithelium via the c-Src Pathway. Mediat. Inflamm. 2017, 2017, 8123281. [Google Scholar] [CrossRef]
- Zhong, Q.; Zhou, B.; Ann, D.K.; Minoo, P.; Liu, Y.; Banfalvi, A.; Krishnaveni, M.S.; Dubourd, M.; Demaio, L.; Willis, B.C.; et al. Role of endoplasmic reticulum stress in epithelial-mesenchymal transition of alveolar epithelial cells: Effects of misfolded surfactant protein. Am. J. Respir. Cell Mol. Biol. 2011, 45, 498–509. [Google Scholar] [CrossRef]
- Li, X.; Li, C.; Zhu, G.; Yuan, W.; Xiao, Z.A. TGF-β1 Induces Epithelial-Mesenchymal Transition of Chronic Sinusitis with Nasal Polyps through MicroRNA-21. Int. Arch. Allergy Immunol. 2019, 179, 304–319. [Google Scholar] [CrossRef]
- Yang, H.W.; Lee, S.A.; Shin, J.M.; Park, I.H.; Lee, H.M. Glucocorticoids ameliorate TGF-β1-mediated epithelial-to-mesenchymal transition of airway epithelium through MAPK and Snail/Slug signaling pathways. Sci. Rep. 2017, 7, 3486. [Google Scholar] [CrossRef]
- Shin, H.W.; Cho, K.; Kim, D.W.; Han, D.H.; Khalmuratova, R.; Kim, S.W.; Jeon, S.Y.; Min, Y.G.; Lee, C.H.; Rhee, C.S.; et al. Hypoxia-inducible factor 1 mediates nasal polypogenesis by inducing epithelial-to-mesenchymal transition. Am. J. Respir. Crit. Care Med. 2012, 185, 944–954. [Google Scholar] [CrossRef]
- Linke, R.; Pries, R.; Könnecke, M.; Bruchhage, K.L.; Böscke, R.; Gebhard, M.; Wollenberg, B. The MEK1/2-ERK1/2 pathway is activated in chronic rhinosinusitis with nasal polyps. Arch. Immunol. Ther. Exp. 2014, 62, 217–229. [Google Scholar] [CrossRef] [PubMed]
- Vetuschi, A.; Pompili, S.; Di Marco, G.P.; Calvaruso, F.; Iacomino, E.; Angelosante, L.; Festuccia, C.; Colapietro, A.; Sferra, R. Can the AGE/RAGE/ERK signalling pathway and the epithelial-to-mesenchymal transition interact in the pathogenesis of chronic rhinosinusitis with nasal polyps? Eur. J. Histochem. 2020, 64, 3079. [Google Scholar] [CrossRef]
- Chen, Y.S.; Wang, X.J.; Feng, W.; Hua, K.Q. Advanced glycation end products decrease collagen I levels in fibroblasts from the vaginal wall of patients with POP via the RAGE, MAPK and NF-κB pathways. Int. J. Mol. Med. 2017, 40, 987–998. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Kim, D.W.; Khalmuratova, R.; Shin, S.H.; Kim, Y.M.; Han, D.H.; Kim, H.J.; Kim, D.Y.; Rhee, C.S.; Park, J.W.; et al. The IFN-γ-p38, ERK kinase axis exacerbates neutrophilic chronic rhinosinusitis by inducing the epithelial-to-mesenchymal transition. Mucosal Immunol. 2019, 12, 601–611. [Google Scholar] [CrossRef]
- Dobzanski, A.; Khalil, S.M.; Lane, A.P. Nasal polyp fibroblasts modulate epithelial characteristics via Wnt signaling. Int. Forum. Allergy Rhinol. 2018, 8, 1412–1420. [Google Scholar] [CrossRef]
- Böscke, R.; Vladar, E.K.; Könnecke, M.; Hüsing, B.; Linke, R.; Pries, R.; Reiling, N.; Axelrod, J.D.; Nayak, J.V.; Wollenberg, B. Wnt Signaling in Chronic Rhinosinusitis with Nasal Polyps. Am. J. Respir. Cell Mol. Biol. 2017, 56, 575–584. [Google Scholar] [CrossRef]
- Linke, R.; Pries, R.; Könnecke, M.; Bruchhage, K.L.; Böscke, R.; Gebhard, M.; Wollenberg, B. Glycogen synthase kinase 3 in chronic rhinosinusitis: Two faces of a single enzyme in one disease. Ann. Allergy Asthma Immunol. 2013, 110, 101–106. [Google Scholar] [CrossRef]
- Bruchhage, K.L.; Koennecke, M.; Drenckhan, M.; Plötze-Martin, K.; Pries, R.; Wollenberg, B. 1,8-cineol inhibits the Wnt/β-catenin signaling pathway through GSK-3 dephosphorylation in nasal polyps of chronic rhinosinusitis patients. Eur. J. Pharmacol. 2018, 835, 140–146. [Google Scholar] [CrossRef]
- Yang, P.; Chen, S.; Zhong, G.; Kong, W.; Wang, Y. Agonist of PPAR-γ Reduced Epithelial-Mesenchymal Transition in Eosinophilic Chronic Rhinosinusitis with Nasal Polyps via Inhibition of High Mobility Group Box1. Int. J. Med. Sci. 2019, 16, 1631–1641. [Google Scholar] [CrossRef]
- de Oliveira, P.W.; Pezato, R.; Agudelo, J.S.; Perez-Novo, C.A.; Berghe, W.V.; Câmara, N.O.; de Almeida, D.C.; Gregorio, L.C. Nasal Polyp-Derived Mesenchymal Stromal Cells Exhibit Lack of Immune-Associated Molecules and High Levels of Stem/Progenitor Cells Markers. Front. Immunol. 2017, 8, 39. [Google Scholar] [CrossRef]
- Yamamoto, A.; Shofuda, T.; Islam, M.O.; Nakamura, Y.; Yamasaki, M.; Okano, H.; Kanemura, Y. ABCB1 is predominantly expressed in human fetal neural stem/progenitor cells at an early development stage. J. Neurosci. Res. 2009, 87, 2615–2623. [Google Scholar] [CrossRef] [PubMed]
- Soklic, T.K.; Rijavec, M.; Silar, M.; Koren, A.; Kern, I.; Hocevar-Boltezar, I.; Korosec, P. Transcription factors gene expression in chronic rhinosinusitis with and without nasal polyps. Radiol. Oncol. 2019, 53, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Xie, S.; Wang, F. Identification of key genes and pathways in chronic rhinosinusitis with nasal polyps using bioinformatics analysis. Am. J. Otolaryngol. 2019, 40, 191–196. [Google Scholar] [CrossRef]
- Plager, D.A.; Kahl, J.C.; Asmann, Y.W.; Nilson, A.E.; Pallanch, J.F.; Friedman, O.; Kita, H. Gene transcription changes in asthmatic chronic rhinosinusitis with nasal polyps and comparison to those in atopic dermatitis. PLoS ONE 2010, 5, e11450. [Google Scholar] [CrossRef] [PubMed]
- Stankovic, K.M.; Goldsztein, H.; Reh, D.D.; Platt, M.P.; Metson, R. Gene expression profiling of nasal polyps associated with chronic sinusitis and aspirin-sensitive asthma. Laryngoscope 2008, 118, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Kim, J.; Sypek, J.P.; Wang, I.M.; Horton, H.; Oppenheim, F.G.; Bochner, B.S. Gene expression profiles in human nasal polyp tissues studied by means of DNA microarray. J. Allergy Clin. Immunol. 2004, 114, 783–790. [Google Scholar] [CrossRef]
- Liu, M.; Guo, P.; An, J.; Guo, C.; Lu, F.; Lei, Y. Genome wide profiling of lncRNA and mRNA expression in CRSwNP. Mol. Med. Rep. 2019, 19, 3855–3863. [Google Scholar] [CrossRef]
- Berebichez-Fridman, R.; Montero-Olvera, P.R. Sources and Clinical Applications of Mesenchymal Stem Cells: State-of-the-art review. Sultan Qaboos Univ. Med. J. 2018, 18, e264–e277. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; et al. Minimal criteria for defining multipotent mesenchymal stromal cells: The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Berebichez-Fridman, R.; Gómez-García, R.; Granados-Montiel, J.; Berebichez-Fastlicht, E.; Olivos-Meza, A.; Granados, J.; Velasquillo, C.; Ibarra, C. The holy grail of orthopedic surgery: Mesenchymal stem cells - Their current uses and potential applications. Stem Cells Int. 2017, 2017, 2638305. [Google Scholar] [CrossRef]
- Afanasyev, B.V.; Elstner, E.E.; Zander, A.R. A.J. Friedenstein, founder of the mesenchymal stem cell concept. Cell. Ther. Transplant. 2009, 1, 3. [Google Scholar] [CrossRef]
- Cho, J.S.; Park, J.H.; Kang, J.H.; Kim, S.E.; Park, I.H.; Lee, H.M. Isolation and characterization of multipotent mesenchymal stem cells in nasal polyps. Exp. Biol. Med. 2015, 240, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Di Vito, A.; Giudice, A.; Chiarella, E.; Malara, N.; Bennardo, F.; Fortunato, L. In Vitro Long-Term Expansion and High Osteogenic Potential of Periodontal Ligament Stem Cells: More Than a Mirage. Cell Transplant. 2019, 28, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Koennecke, M.; Böscke, R.; Pfannerstill, A.C.; Reers, S.; Elsner, M.; Fell, B.; Richter, A.; Bruchhage, K.L.; Schumann, S.; Pries, R.; et al. Neuronal Differentiation Capability of Nasal Polyps of Chronic Rhinosinusitis. Arch. Immunol. Ther. Exp. 2017, 65, 431–443. [Google Scholar] [CrossRef]
- Delorme, B.; Nivet, E.; Gaillard, J.; Häupl, T.; Ringe, J.; Devèze, A.; Magnan, J.; Sohier, J.; Khrestchatisky, M.; Roman, F.S.; et al. The human nose harbors a niche of olfactory ectomesenchymal stem cells displaying neurogenic and osteogenic properties. Stem Cells Dev. 2010, 19, 853–866. [Google Scholar] [CrossRef]
- Chiarella, E.; Aloisio, A.; Scicchitano, S.; Lucchino, V.; Montalcini, Y.; Galasso, O.; Greco, M.; Gasparini, G.; Mesuraca, M.; Bond, H.M.; et al. ZNF521 Represses Osteoblastic Differentiation in Human Adipose-Derived Stem Cells. Int. J. Mol. Sci. 2018, 19, 4095. [Google Scholar] [CrossRef]
- Di Vito, A.; Chiarella, E.; Baudi, F.; Scardamaglia, P.; Antonelli, A.; Giudice, D.; Barni, T.; Fortunato, L.; Giudice, A. Dose-dependent effects of zoledronic acid on human periodontal ligament stem cells: An in vitro pilot study. Cell Transplant. 2020. [Google Scholar] [CrossRef]
- Hwang, S.H.; Park, S.H.; Choi, J.; Lee, D.C.; Oh, J.H.; Kim, S.W.; Kim, J.B. Characteristics of mesenchymal stem cells originating from the bilateral inferior turbinate in humans with nasal septal deviation. PLoS ONE 2014, 9, e100219. [Google Scholar] [CrossRef][Green Version]
- Chiarella, E.; Aloisio, A.; Codispoti, B.; Nappo, G.; Scicchitano, S.; Lucchino, V.; Montalcini, Y.; Camarotti, A.; Galasso, O.; Greco, M.; et al. ZNF521 Has an Inhibitory Effect on the Adipogenic Differentiation of Human Adipose-Derived Mesenchymal Stem Cells. Stem Cell Rev. Rep. 2018, 14, 901–914. [Google Scholar] [CrossRef]
- Bond, H.M.; Scicchitano, S.; Chiarella, E.; Amodio, N.; Lucchino, V.; Aloisio, A.; Montalcini, Y.; Mesuraca, M.; Morrone, G. ZNF423: A New Player in Estrogen Receptor-Positive Breast Cancer. Front. Endocrinol. 2018, 9, 255. [Google Scholar] [CrossRef]
- Kang, S.; Akerblad, P.; Kiviranta, R.; Gupta, R.K.; Kajimura, S.; Griffin, M.J.; Min, J.; Baron, R.; Rosen, E.D. Regulation of early adipose commitment by Zfp521. PLoS Biol 2012, 10, e1001433. [Google Scholar] [CrossRef] [PubMed]
- Bernaudo, F.; Monteleone, F.; Mesuraca, M.; Krishnan, S.; Chiarella, E.; Scicchitano, S.; Cuda, G.; Morrone, G.; Bond, H.M.; Gaspari, M. Validation of a novel shotgun proteomic workflow for the discovery of protein-protein interactions: Focus on ZNF521. J. Proteome Res. 2015, 14, 1888–1899. [Google Scholar] [CrossRef] [PubMed]
- Mesuraca, M.; Galasso, O.; Guido, L.; Chiarella, E.; Scicchitano, S.; Vatrinet, R.; Morrone, G.; Bond, H.M.; Gasparini, G. Expression profiling and functional implications of a set of zinc finger proteins, ZNF423, ZNF470, ZNF521, and ZNF780B, in primary osteoarthritic articular chondrocytes. Mediat. Inflamm. 2014, 2014, 318793. [Google Scholar] [CrossRef] [PubMed]
- Kypriotou, M.; Fossard-Demoor, M.; Chadjichristos, C.; Ghayor, C.; de Crombrugghe, B.; Pujol, J.P.; Galéra, P. OX9 exerts a bifunctional effect on type II collagen gene (COL2A1) expression in chondrocytes depending on the differentiation state. DNA Cell Biol. 2003, 22, 119–129. [Google Scholar] [CrossRef]
- Girard, S.D.; Devéze, A.; Nivet, E.; Gepner, B.; Roman, F.S.; Féron, F. Isolating nasal olfactory stem cells from rodents or humans. J. Vis. Exp. 2011, 54, e2762. [Google Scholar] [CrossRef]
- Pezato, R.; de Almeida, D.C.; Bezerra, T.F.; de Sá Silva, F.; Perez-Novo, C.; Gregório, L.C.; Voegels, R.L.; Câmara, N.O.; Bachert, C. Immunoregulatory effects of bone marrow-derived mesenchymal stem cells in the nasal polyp microenvironment. Mediat. Inflamm. 2014, 2014, 583409. [Google Scholar] [CrossRef]
- Cho, K.S.; Park, M.K.; Kang, S.A.; Park, H.Y.; Hong, S.L.; Park, H.K.; Yu, H.S.; Roh, H.J. Adipose-derived stem cells ameliorate allergic airway inflammation by inducing regulatory T cells in a mouse model of asthma. Mediat. Inflamm. 2014, 2014, 436476. [Google Scholar] [CrossRef]
- Donizetti-Oliveira, C.; Semedo, P.; Burgos-Silva, M.; Cenedeze, M.A.; Malheiros, D.M.A.C.; Reis, M.A.; Pacheco-Silva, A.; Câmara, N.O.S. Adipose Tissue-Derived Stem Cell Treatment Prevents Renal Disease Progression. Cell Transplant. 2012, 21, 1727–1741. [Google Scholar] [CrossRef]
| PATHWAYS | CRSwNP | Inhibitors of EMT | Ref. |
|---|---|---|---|
| TGF-β1 | downregulated | HDAC1/2, TSA Chemical chaperones, PBA, PPB TGF-β1 miR-21 Glucocorticoids | [35,36,38,39] |
| SMAD3 and HIF-1α | upregulated | HIF-1α inhibitors 2ME2, 17-AAG | [40] |
| AGE/RAGE/ERK | upregulated | p38, MEK, ERK inhibitors | [41] |
| MEK1/2-ERK1/2 | upregulated | MEK, ERK inhibitors | [42,43,44] |
| WNT/ β-catenin/GSK | upregulated | Wnt inhibitors IWP2 oxide 1,8-cineol inhibitor GSK-3 | [45,46,47,48] |
| PPAR-γ | upregulated | agonist PPAR-γ Rosiglitazone | [49] |
| Differentiation | Markers | Ref. |
|---|---|---|
| Adipogenesis | PPARγ, FABP4, | [50,62] |
| Osteogenesis | Runx2, Osteocalcin | [62] |
| Chondrogenesis | Sox9, Col2A | [62] |
| Neuron-like cells | NF-H, NF-L, TuJ1, Nestin, GM-CSF | [62,64,65,75] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiarella, E.; Lombardo, N.; Lobello, N.; Aloisio, A.; Aragona, T.; Pelaia, C.; Scicchitano, S.; Bond, H.M.; Mesuraca, M. Nasal Polyposis: Insights in Epithelial-Mesenchymal Transition and Differentiation of Polyp Mesenchymal Stem Cells. Int. J. Mol. Sci. 2020, 21, 6878. https://doi.org/10.3390/ijms21186878
Chiarella E, Lombardo N, Lobello N, Aloisio A, Aragona T, Pelaia C, Scicchitano S, Bond HM, Mesuraca M. Nasal Polyposis: Insights in Epithelial-Mesenchymal Transition and Differentiation of Polyp Mesenchymal Stem Cells. International Journal of Molecular Sciences. 2020; 21(18):6878. https://doi.org/10.3390/ijms21186878
Chicago/Turabian StyleChiarella, Emanuela, Nicola Lombardo, Nadia Lobello, Annamaria Aloisio, Teodoro Aragona, Corrado Pelaia, Stefania Scicchitano, Heather Mandy Bond, and Maria Mesuraca. 2020. "Nasal Polyposis: Insights in Epithelial-Mesenchymal Transition and Differentiation of Polyp Mesenchymal Stem Cells" International Journal of Molecular Sciences 21, no. 18: 6878. https://doi.org/10.3390/ijms21186878
APA StyleChiarella, E., Lombardo, N., Lobello, N., Aloisio, A., Aragona, T., Pelaia, C., Scicchitano, S., Bond, H. M., & Mesuraca, M. (2020). Nasal Polyposis: Insights in Epithelial-Mesenchymal Transition and Differentiation of Polyp Mesenchymal Stem Cells. International Journal of Molecular Sciences, 21(18), 6878. https://doi.org/10.3390/ijms21186878









