Circulating Long Noncoding RNA LNC-EPHA6 Associates with Acute Rejection after Kidney Transplantation
Abstract
1. Introduction
2. Results
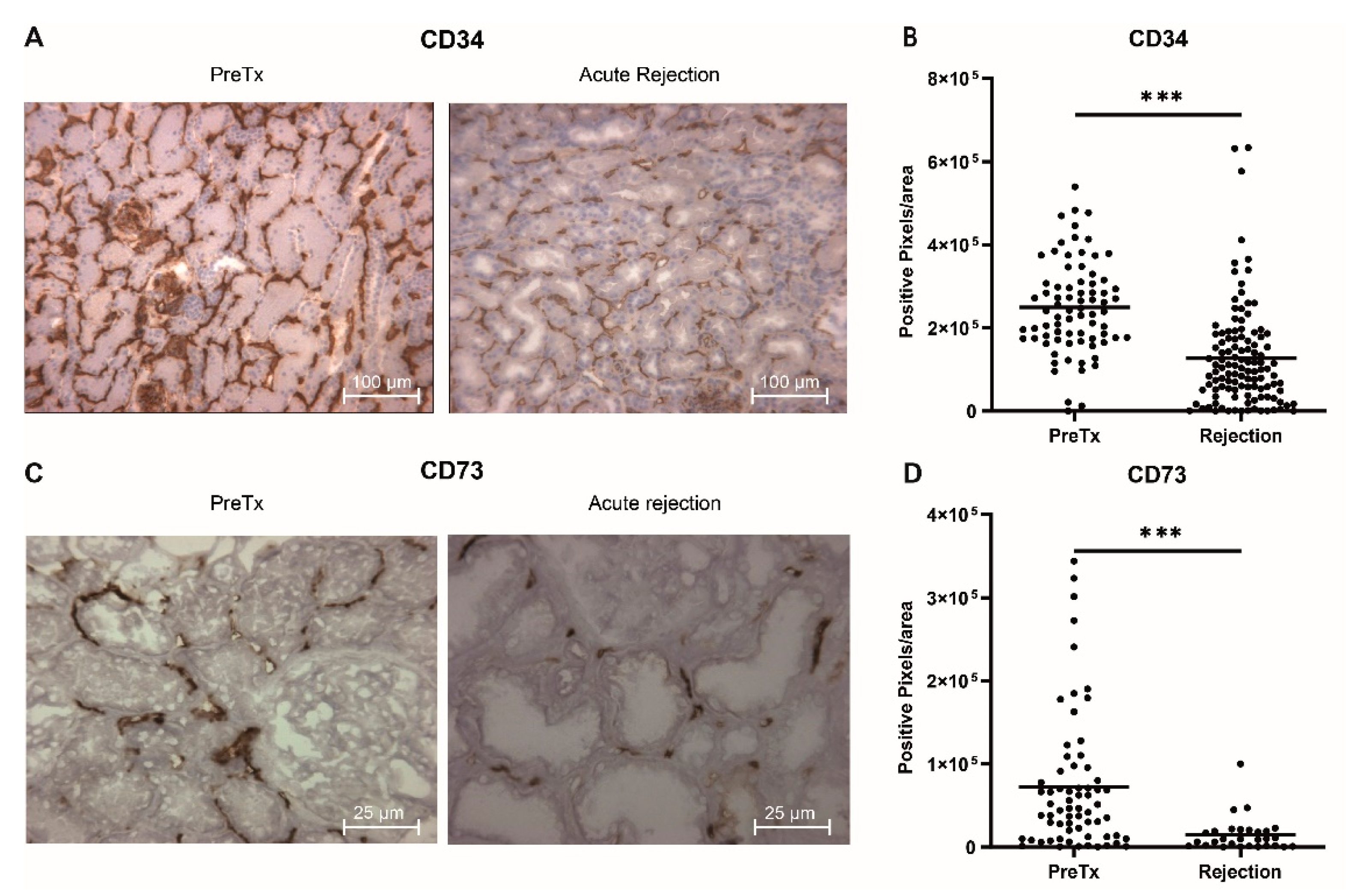
2.1. Decreased Capillary Density in Acute Rejection Biopsies
2.2. Patient Characteristics of Cross Sectional and Longitudinal AR Study Population
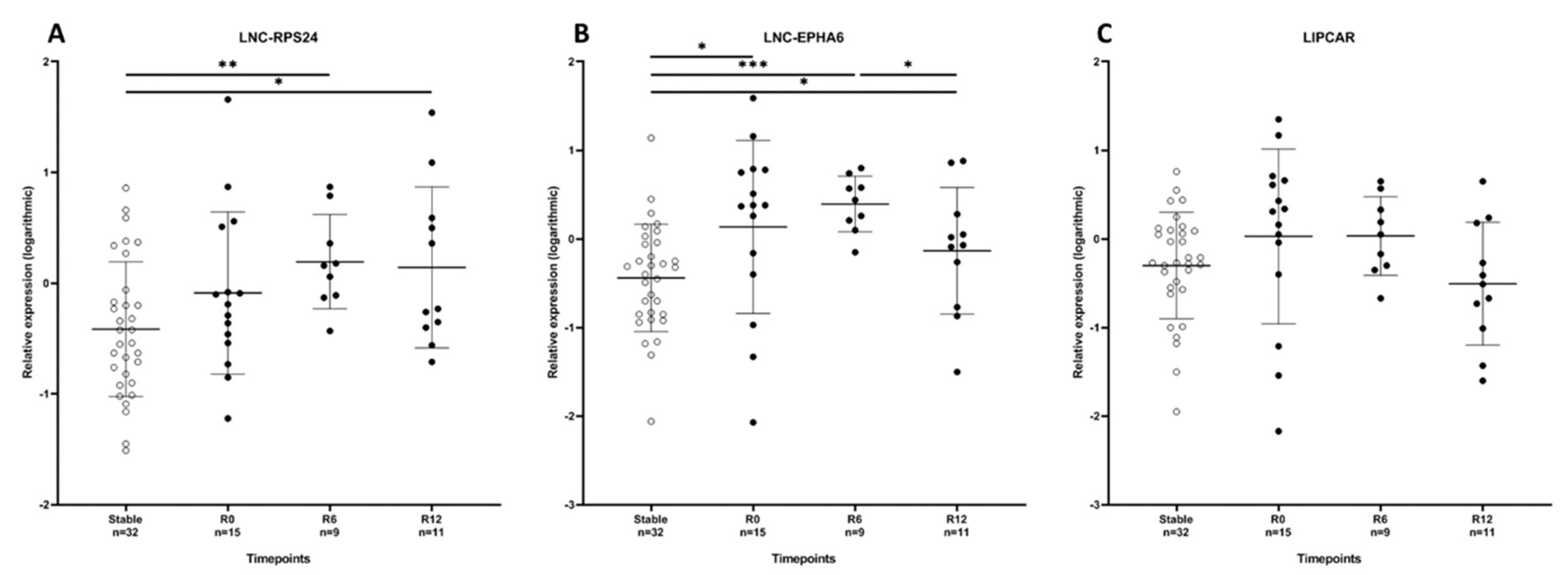
2.3. Circulating LNC-EPHA6 Levels Directly Correlate with Acute Rejection
2.4. Circulating LNC-EPHA6 Decreases in the First Year After Acute Rejection
2.5. LNC-RPS24, LNC-EPHA6 and LIPCAR Correlate with Soluble Thrombomodulin
3. Discussion
4. Materials and Methods
4.1. Renal Biopsy Study
4.2. Patient Study Cohort
4.3. Immunosuppressive Drugs, Rejection and Rejection Treatment
4.4. RNA Isolation
4.5. RT-qPCR
4.6. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Chand, S.; Atkinson, D.; Collins, C.; Briggs, D.; Ball, S.; Sharif, A.; Skordilis, K.; Vydianath, B.; Neil, D.; Borrows, R. The Spectrum of Renal Allograft Failure. PLoS ONE 2016, 11, e0162278. [Google Scholar] [CrossRef]
- Clayton, P.A.; McDonald, S.P.; Russ, G.R.; Chadban, S.J. Long-Term Outcomes after Acute Rejection in Kidney Transplant Recipients: An ANZDATA Analysis. J. Am. Soc. Nephrol. 2019, 30, 1697–1707. [Google Scholar] [CrossRef]
- El-Zoghby, Z.M.; Stegall, M.D.; Lager, D.J.; Kremers, W.K.; Amer, H.; Gloor, J.M.; Cosio, F.G. Identifying specific causes of kidney allograft loss. Am. J. Transpl. 2009, 9, 527–535. [Google Scholar] [CrossRef]
- Park, W.Y.; Paek, J.H.; Jin, K.; Park, S.B.; Choe, M.; Han, S. Differences in Pathologic Features and Graft Outcomes of Rejection on Kidney Transplant. Transpl. Proc. 2019, 51, 2655–2659. [Google Scholar] [CrossRef]
- Bruneau, S.; Woda, C.B.; Daly, K.P.; Boneschansker, L.; Jain, N.G.; Kochupurakkal, N.; Contreras, A.G.; Seto, T.; Briscoe, D.M. Key Features of the Intragraft Microenvironment that Determine Long-Term Survival Following Transplantation. Front Immunol. 2012, 3, 54. [Google Scholar] [CrossRef]
- Contreras, A.G.; Briscoe, D.M. Every allograft needs a silver lining. J. Clin. Investig. 2007, 117, 3645–3648. [Google Scholar] [CrossRef]
- Denton, M.D.; Davis, S.F.; Baum, M.A.; Melter, M.; Reinders, M.E.; Exeni, A.; Samsonov, D.V.; Fang, J.; Ganz, P.; Briscoe, D.M. The role of the graft endothelium in transplant rejection: Evidence that endothelial activation may serve as a clinical marker for the development of chronic rejection. Pediatr. Transpl. 2000, 4, 252–260. [Google Scholar] [CrossRef]
- Reinders, M.E.; Fang, J.C.; Wong, W.; Ganz, P.; Briscoe, D.M. Expression patterns of vascular endothelial growth factor in human cardiac allografts: Association with rejection. Transplantation 2003, 76, 224–230. [Google Scholar] [CrossRef]
- Reinders, M.E.; Rabelink, T.J.; Briscoe, D.M. Angiogenesis and endothelial cell repair in renal disease and allograft rejection. J. Am. Soc. Nephrol. 2006, 17, 932–942. [Google Scholar] [CrossRef]
- Reinders, M.E.; Sho, M.; Izawa, A.; Wang, P.; Mukhopadhyay, D.; Koss, K.E.; Geehan, C.S.; Luster, A.D.; Sayegh, M.H.; Briscoe, D.M. Proinflammatory functions of vascular endothelial growth factor in alloimmunity. J. Clin. Investig. 2003, 112, 1655–1665. [Google Scholar] [CrossRef]
- Bishop, G.A.; Waugh, J.A.; Landers, D.V.; Krensky, A.M.; Hall, B.M. Microvascular destruction in renal transplant rejection. Transplantation 1989, 48, 408–414. [Google Scholar] [CrossRef]
- Long, D.A.; Norman, J.T.; Fine, L.G. Restoring the renal microvasculature to treat chronic kidney disease. Nat. Rev. Nephrol. 2012, 8, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Bijkerk, R.; Florijn, B.W.; Khairoun, M.; Duijs, J.; Ocak, G.; de Vries, A.P.J.; Schaapherder, A.F.; Mallat, M.J.; de Fijter, J.W.; Rabelink, T.J.; et al. Acute Rejection After Kidney Transplantation Associates With Circulating MicroRNAs and Vascular Injury. Transpl. Direct. 2017, 3, e174. [Google Scholar] [CrossRef] [PubMed]
- Lorenzen, J.M.; Thum, T. Long noncoding RNAs in kidney and cardiovascular diseases. Nat. Rev. Nephrol. 2016, 12, 360–373. [Google Scholar] [CrossRef]
- Vierbuchen, T.; Fitzgerald, K.A. Long non-coding RNAs in antiviral immunity. In Seminars in Cell and Developmental Biology; Elsevier: London, England, 2020; E4977. [Google Scholar]
- Ignarski, M.; Islam, R.; Müller, R.U. Long Non-Coding RNAs in Kidney Disease. Int. J. Mol. Sci. 2019, 20, 3276. [Google Scholar] [CrossRef]
- Geisler, S.; Coller, J. RNA in unexpected places: Long non-coding RNA functions in diverse cellular contexts. Nat. Rev. Mol. Cell. Biol. 2013, 14, 699–712. [Google Scholar] [CrossRef] [PubMed]
- Nafar, M.; Kalantari, S.; Ghaderian, S.M.H.; Omrani, M.D.; Fallah, H.; Arsang-Jang, S.; Abbasi, T.; Samavat, S.; Dalili, N.; Taheri, M.; et al. Expression Levels of lncRNAs in the Patients with the Renal Transplant Rejection. Urol. J. 2019, 16, 572–577. [Google Scholar]
- Groeneweg, K.E.; Au, Y.W.; Duijs, J.M.; Florijn, B.W.; van Kooten, C.; de Fijter, J.W.; Reinders, M.E.; van Zonneveld, A.J.; Bijkerk, R. Diabetic nephropathy alters circulating long noncoding RNA Levels that normalize following simultaneous pancreas-kidney transplantation. Am. J. Transpl. 2020. [Google Scholar] [CrossRef]
- Zuidwijk, K.; de Fijter, J.W.; Mallat, M.J.; Eikmans, M.; van Groningen, M.C.; Goemaere, N.N.; Bajema, I.M.; Van Kooten, C. Increased influx of myeloid dendritic cells during acute rejection is associated with interstitial fibrosis and tubular atrophy and predicts poor outcome. Kidney Int. 2012, 81, 64–75. [Google Scholar] [CrossRef]
- Ge, Y.Z.; Xu, T.; Cao, W.J.; Wu, R.; Yao, W.T.; Zhou, C.C.; Wang, M.; Xu, L.W.; Lu, T.Z.; Zhao, Y.C.; et al. A Molecular Signature of Two Long Non-Coding RNAs in Peripheral Blood Predicts Acute Renal Allograft Rejection. Cell. Physiol. Biochem. 2017, 44, 1213–1223. [Google Scholar] [CrossRef]
- Zou, Y.; Zhang, W.; Zhou, H.H.; Liu, R. Analysis of long noncoding RNAs for acute rejection and graft outcome in kidney transplant biopsies. Biomark Med. 2019, 13, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.F.; Song, B.; Duan, J.H.; Hu, Z.D.; Cui, Z.L.; Yang, T. PRINS Long Noncoding RNA Involved in IP-10-Mediated Allograft Rejection in Rat Kidney Transplant. Transpl. Proc. 2018, 50, 1558–1565. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Hu, J.; Xu, H.; Zhou, H.; Liu, Z.; Zhou, Y.; Liu, R.; Zhang, W. Long Non-coding RNA Expression Profiling in Biopsy to Identify Renal Allograft at Risk of Chronic Damage and Future Graft Loss. Appl. Biochem. Biotechnol. 2020, 190, 660–673. [Google Scholar] [CrossRef]
- Cabili, M.N.; Trapnell, C.; Goff, L.; Koziol, M.; Tazon-Vega, B.; Regev, A.; Rinn, J.L. Integrative annotation of human large intergenic noncoding RNAs reveals global properties and specific subclasses. Genes Dev. 2011, 25, 1915–1927. [Google Scholar] [CrossRef]
- Das, G.; Yu, Q.; Hui, R.; Reuhl, K.; Gale, N.W.; Zhou, R. EphA5 and EphA6: Regulation of neuronal and spine morphology. Cell Biosci. 2016, 6, 48. [Google Scholar] [CrossRef]
- Li, S.; Ma, Y.; Xie, C.; Wu, Z.; Kang, Z.; Fang, Z.; Su, B.; Guan, M. EphA6 promotes angiogenesis and prostate cancer metastasis and is associated with human prostate cancer progression. Oncotarget 2015, 6, 22587–22597. [Google Scholar] [CrossRef] [PubMed]
| Stable (n = 32) | AR (n = 15) | p-Value | |
|---|---|---|---|
| Sex, Male, n (%) | 21 (66%) | 10 (67%) | 1.00 1 |
| Age, Years ± SD | 51 ± 14 | 54 ± 12 | 0.35 2 |
| BMI (kg/m2) | 26.4 ± 4.6 | 24.4 ± 3.5 | 0.15 1 |
| Preemptive, n (%) | 16 (50%) | 5 (33%) | 0.36 1 |
| Months Since KTx, Median(IQR) | 12 ± 1 | 12 ± 15 | 0.97 2 |
| PRA >5%, n (%) | 6 (19%) | 1 (7%) | 0.40 1 |
| Previous Transplantations, n (%) | 2 (6%) | 3 (20%) | 0.31 1 |
| Mismatch A/B/DR, Mean | 1.0/1.2/0.8 | 0.9/1.3/1.0 | 0.76/0.81/0.63 1 |
| Donor Characteristics | |||
| Sex, male, n (%) | 11 (34%) | 7 (47%) | 0.52 1 |
| Age, years ± SD | 50 ± 17 | 47 ± 12 | 0.64 2 |
| Induction Therapy, n (%) | 0.54 1 | ||
| Alemtuzumab | 3 (9%) | 0 | |
| IL-2 receptor inhibitor | 29 (91%) | 15 (100%) | |
| Immunosuppressive Drugs, n (%) | |||
| Tacrolimus | 22 (69%) | 8 (53%) | 0.20 1 |
| Cyclosporine | 5 (16%) | 3 (20%) | 1.00 1 |
| Prednisone | 32 (100%) | 14 (93%) | 0.32 1 |
| Mycophenolate mofetil | 25 (78%) | 8 (53%) | 0.07 1 |
| Everolimus | 6 (19%) | 1 (7%) | 0.40 1 |
| Acute Rejection Therapy, n (%) | |||
| ATG | 2 (13%) | ||
| methylprednisolone | - | 10 (67%) | |
| methylprednisolone + ATG | - | 2 (13%) | |
| methylprednisolone + alemtuzumab | - | 1 (7%) | |
| eGFR (mL/min/1.73 m2) | 54 ± 12 | 34 ± 14 | <0.001 2 |
| Proteinuria (g/24 h), Median(IQR) | 0.17 (0.13–0.25) | 0.36 (0.23–1.19) | 0.003 3 |
| LNC-RPS24 | LNC-EPHA6 | LIPCAR | |
|---|---|---|---|
| Vascular injury markers | |||
| sTM | 0.331 (p = 0.035) | 0.383 (p = 0.013) | 0.321 (p = 0.041) |
| Ang-2 | ns | ns | ns |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Groeneweg, K.E.; Duijs, J.M.G.J.; Florijn, B.W.; van Kooten, C.; de Fijter, J.W.; van Zonneveld, A.J.; Reinders, M.E.J.; Bijkerk, R. Circulating Long Noncoding RNA LNC-EPHA6 Associates with Acute Rejection after Kidney Transplantation. Int. J. Mol. Sci. 2020, 21, 5616. https://doi.org/10.3390/ijms21165616
Groeneweg KE, Duijs JMGJ, Florijn BW, van Kooten C, de Fijter JW, van Zonneveld AJ, Reinders MEJ, Bijkerk R. Circulating Long Noncoding RNA LNC-EPHA6 Associates with Acute Rejection after Kidney Transplantation. International Journal of Molecular Sciences. 2020; 21(16):5616. https://doi.org/10.3390/ijms21165616
Chicago/Turabian StyleGroeneweg, Koen E., Jacques M.G.J. Duijs, Barend W. Florijn, Cees van Kooten, Johan W. de Fijter, Anton Jan van Zonneveld, Marlies E.J. Reinders, and Roel Bijkerk. 2020. "Circulating Long Noncoding RNA LNC-EPHA6 Associates with Acute Rejection after Kidney Transplantation" International Journal of Molecular Sciences 21, no. 16: 5616. https://doi.org/10.3390/ijms21165616
APA StyleGroeneweg, K. E., Duijs, J. M. G. J., Florijn, B. W., van Kooten, C., de Fijter, J. W., van Zonneveld, A. J., Reinders, M. E. J., & Bijkerk, R. (2020). Circulating Long Noncoding RNA LNC-EPHA6 Associates with Acute Rejection after Kidney Transplantation. International Journal of Molecular Sciences, 21(16), 5616. https://doi.org/10.3390/ijms21165616





