Post-Traumatic Meningitis Is a Diagnostic Challenging Time: A Systematic Review Focusing on Clinical and Pathological Features
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Search Criteria and Critical Appraisal
3. Results
3.1. Search Results and Included Studies
- the human study so we excluded animal studies,
- clinical features,
- diagnosis,
- post-mortem findings,
- management of the study so we excluded methodologically incomplete design studies and those with no explicit mention about ethical issues.
3.2. Risk of Bias
4. Discussion
4.1. Epidemiology and Risk Factors
4.2. Pathogenesis and Pathophysiology: A Brief Outline
4.3. Clinical Manifestations
4.4. Diagnostic Approach
4.4.1. CSF Analysis
4.4.2. Surrogate Serum Markers
4.4.3. The Role of Neuroimaging in Meningitis
4.4.4. Novel Diagnostic Tools
4.5. Therapeutic Management
4.5.1. Antibiotic and Steroid Treatment in Post-Traumatic Meningitis
4.5.2. Antibiotic Prophylaxis after TBI: A Matter of Debate
4.5.3. The Management of CSF Leaks
4.6. Outcome and Neurological Complications
4.7. Forensic Pathology Approach in Cases of Post-Traumatic Meningitis-Related Death
- -
- Complete autoptic examination;
- -
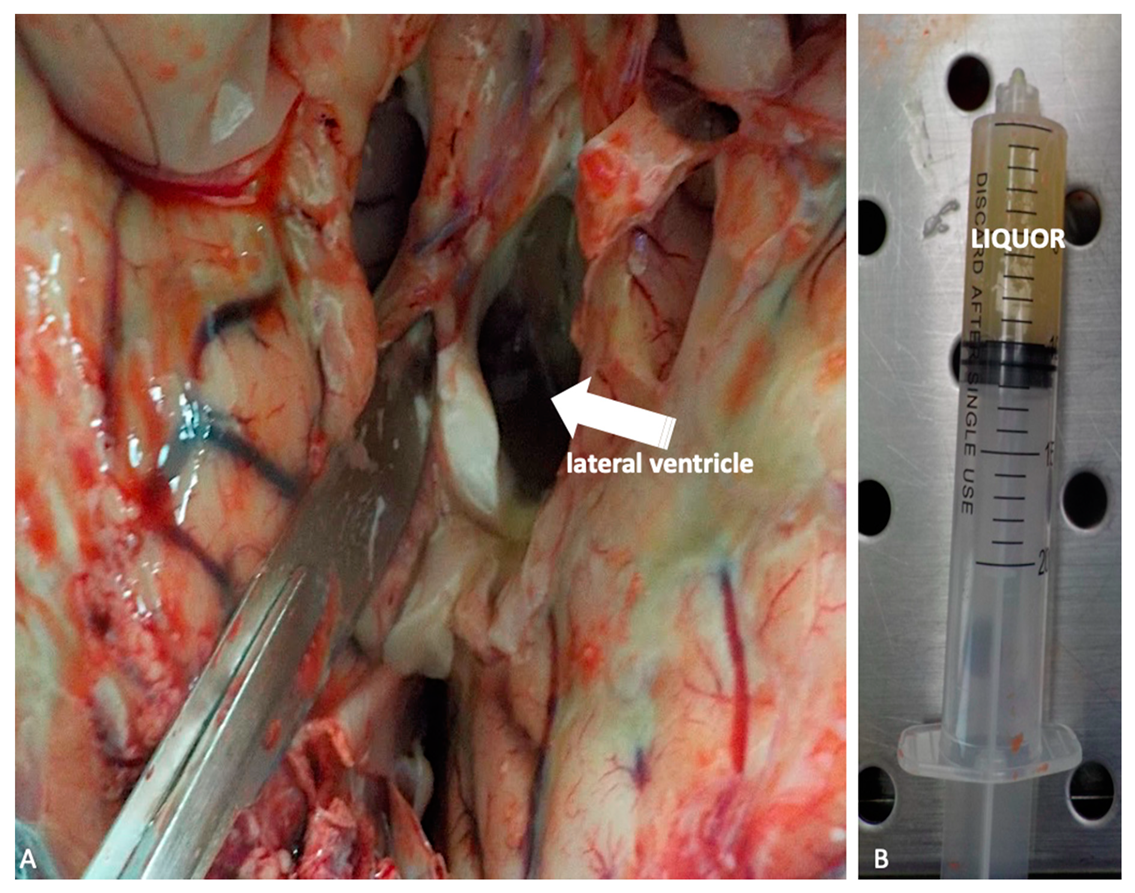
- Liquor sampling and microbiological investigations;
- -
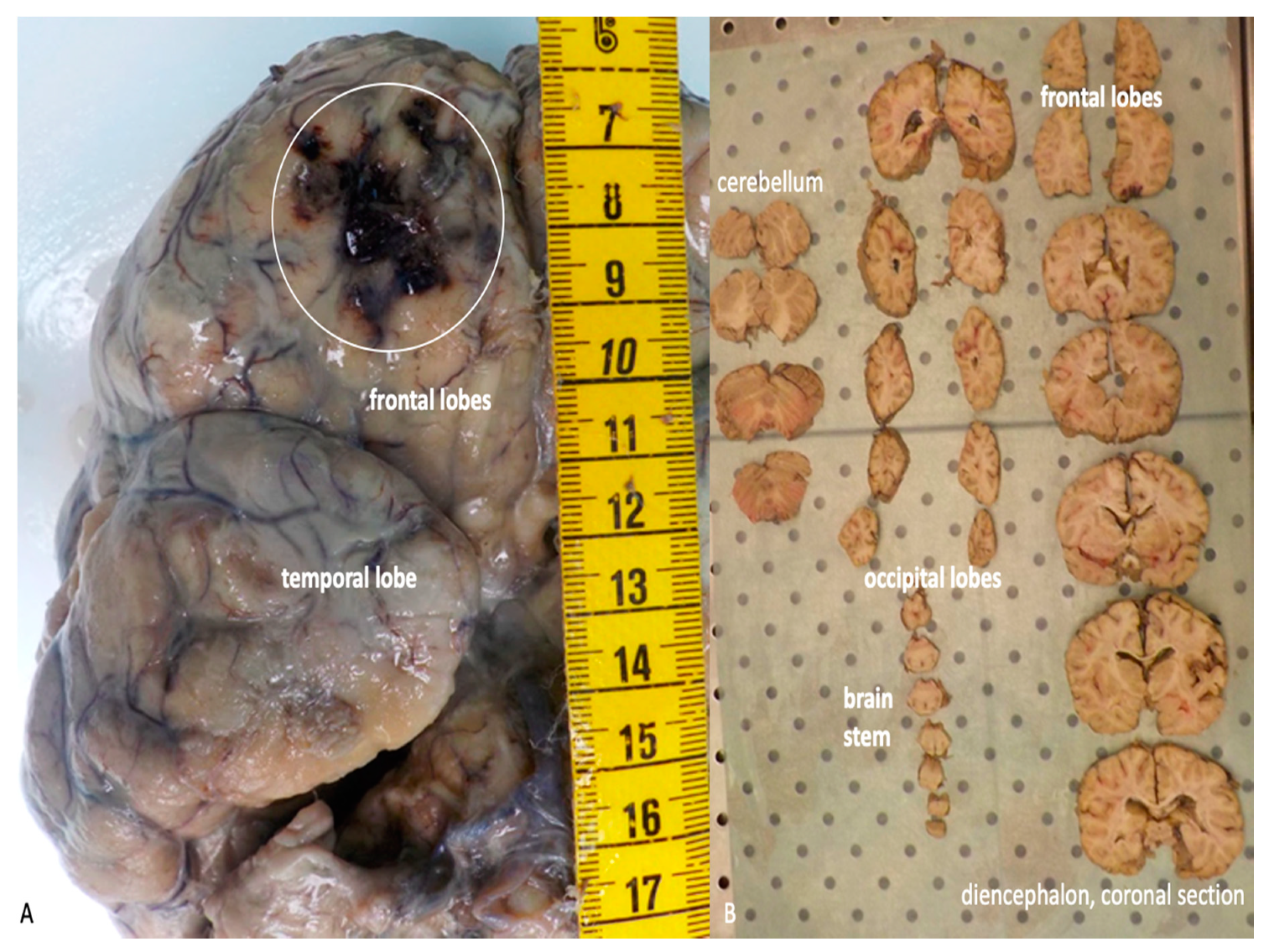
- Brain in toto removal and formalin embedding;
- -
- Sampling of the intracranial structures;
- -
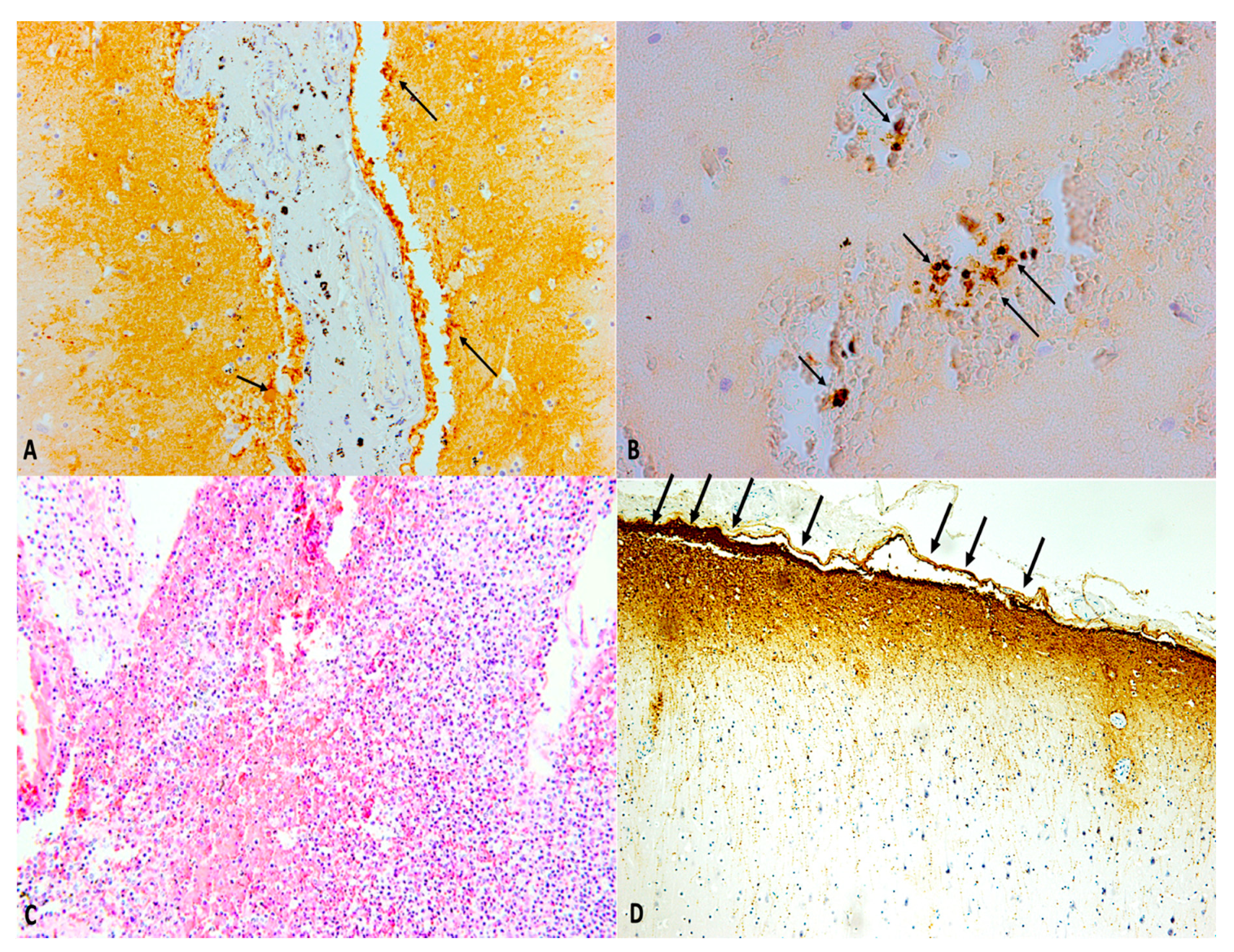
- Histological and immunohistochemical specimen’s microscopic evaluation.
4.7.1. Autopsy
4.7.2. Tissues’ Sampling and Histological Examination
4.7.3. Forensic Pathology Assessment
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| PRISMA | Preferred Reporting Items For Systematic Reviews And Meta-Analyses |
| PICO | Participants, Intervention, Control, and Outcomes |
| CSF | Cerebrospinal Fluid |
| MDPI | Multidisciplinary Digital Publishing Institute |
| CT | Computed Tomography |
| DOAJ | Directory Of Open Access Journals |
| TLA | Three Letter Acronym |
| LD | Linear Dichroism |
| TBI | Traumatic Brain Injury |
| EMBASE | Excerpta Medica Database |
| HIV | Human Immunodeficiency Virus |
| CNS | Central Nervous System |
| ACF | Anterior Cerebral Fossa |
| BBB | Blood–Brain Barrier |
| SAH | Subarachnoid Hemorrhage |
| PCR | Polymerase Chain Reaction |
| CRP | C-Reactive Protein |
| PCT | Procalcitonin |
| ICU | Intensive Care Unit |
| MRI | Magnetic Resonance Imaging |
| Gd | Gadolium |
| HRCT | High-Resolution Computed Tomography |
| RCTs | Randomized Controlled Trials |
| GBD | Global Burden of Disease |
| ICP | Invasive Intracranial Pressure |
| AQP4 | Aquaporin4 |
| HIF-1α | Hypoxia Induced-Factor 1α |
| CD | Custer Differentiation |
| GFAP | Glial Fibrillary Acid Protein |
| IBA-1 | Ionized Calcium Binding Adapter Molecule 1 |
| β-APP | Beta-Amyloid Precursor Protein |
| H&E | Hematoxylin and Eosin |
| TNF | Tumor necrosis factor |
| TGFβ | Transforming growth factor beta |
| MCP-1 | Monocyte chemoattractant protein-1 |
References
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Aboyans, V. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Yelehe-Okouma, M.; Czmil-Garon, J.; Pape, E.; Petitpain, N.; Gillet, P. Drug-induced aseptic meningitis: A mini-review. Fundam. Clin. Pharmacol. 2018, 32, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Eljamel, M.S.; Foy, P.M. Acute traumatic CSF fistulae: The risk of intracranial infection. Br. J. Neurosurg. 1990, 4, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Matschke, J.; Tsokos, M. Post-traumatic meningitis: Histomorphological findings, postmortem microbiology and forensic implications. Forensic. Sci. Int. 2001, 115, 199–205. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 62, e1–e34. [Google Scholar]
- Van de Beek, D.; de Gans, J.; Tunkel, A.R.; Wijdicks, E.F. Community-acquired bacterial meningitis in adults. N. Engl. J. Med. 2006, 354, 44–53. [Google Scholar] [CrossRef]
- Adriani, K.S.; Brouwer, M.C.; Van de Beek, D. Risk factors for community-acquired bacterial meningitis in adults. Neth. J. Med. 2015, 73, 53–60. [Google Scholar]
- Van de Beek, D.; Cabellos, C.; Dzupova, O.; Esposito, S.; Klein, M.; Kloek, A.T.; Pfister, H.W. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis. Clin. Microbiol. Infect. 2016, 22, S37–S62. [Google Scholar] [CrossRef]
- Van de Beek, D.; Drake, J.M.; Tunkel, A.R. Nosocomial bacterial meningitis. N. Engl. J. Med. 2010, 362, 146–154. [Google Scholar] [CrossRef]
- Phang, S.Y.; Whitehouse, K.; Lee, L.; Khalil, H.; McArdle, P.; Whitfield, P.C. Management of CSF leak in base of skull fractures in adults. Br. J. Neurosurg. 2016, 30, 596–604. [Google Scholar] [CrossRef]
- Prosser, J.D.; Vender, J.R.; Solares, C.A. Traumatic cerebrospinal fluid leaks. Otolaryngol. Clin. North. Am. 2011, 44, 857–873. [Google Scholar] [CrossRef]
- Sonig, A.; Thakur, J.D.; Chittiboina, P.; Khan, I.S.; Nanda, A. Is posttraumatic cerebrospinal fluid fistula a predictor of posttraumatic meningitis? A US Nationwide Inpatient Sample database study. Neurosurg. Focus 2012, 32, E4. [Google Scholar] [CrossRef]
- Tebruegge, M.; Curtis, N. Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitis. Clin. Microbial. Rev. 2008, 21, 519–537. [Google Scholar] [CrossRef]
- Durand, M.L.; Calderwood, S.B.; Weber, D.J.; Miller, S.I.; Southwick, F.S.; Caviness Jr, V.S.; Swartz, M.N. Acute Bacterial Meningitis in Adults--A Review of 493 Episodes. N. Engl. J. Med. 1993, 328, 21–28. [Google Scholar] [CrossRef]
- Adriani, K.S.; Van de Beek, D.; Brouwer, M.C.; Spanjaard, L.; de Gans, J. Community-acquired recurrent bacterial meningitis in adults. Clin. Infect. Dis. 2007, 45, e46–e51. [Google Scholar] [CrossRef]
- Heckenberg, S.G.; Brouwer, M.C.; van de Beek, D. Bacterial meningitis. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2014; Volume 121, pp. 1361–1375. [Google Scholar]
- Sağlam, M.; Zer, Y.; Balci, I. Causative agents of bacterial meningitis. Afr. J. Microbiol. Res. 2013, 7, 2221–2227. [Google Scholar]
- Hernandez, J.L.; Calvo, J.; Sota, R.; Agüero, J.; Garcia-Palomo, J.; Farinas, M. Clinical and microbiological characteristics of 28 patients with Staphylococcus schleiferi infection. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 153–158. [Google Scholar] [CrossRef]
- Chang, W.N.; Lu, C.H.; Huang, C.R.; Chuang, Y.C.; Tsai, N.W.; Chen, S.F.; Chang, C.C.; Wang, H.C.; Chien, C.C.; Wu, J.J. Epidemiology of Adult Staphylococcal Meningitis in Southern Taiwan: A Coaghlase-Negative Staphylococcal Infection. Jpn. J. Infect. Dis. 2007, 60, 262–266. [Google Scholar]
- Garg, R.K.; Malhotra, H.S.; Jain, M.; Kumar, N.; Lachuryia, G.; Mahajan, L. Brainstem infarct as a rare complication of coagulase-negative staphylococcus meningitis. Neurol. India. 2017, 65, 621. [Google Scholar] [CrossRef]
- Oud, L. Community-acquired meningitis due to Staphylococcus capitis in the absence of neurologic trauma, surgery, or implants. Heart Lung. 2011, 40, 467–471. [Google Scholar] [CrossRef]
- Lin, W.-S.; Kao, H.W.; Cheng, C.-A. Panspinal epidural abscess concomitant with meningitis. Am. J. Emerg. Med. 2013, 31, P1155.e5–P1155.e6. [Google Scholar] [CrossRef]
- Dumas, G.; Schmerber, S.; Atallah, I.; Brion, J.; Righini, C.A. Subacute tuberculous otitis media complicated by petrositis and meningitis. Rev. Laryngol. Otol. Rhinol. (Bord) 2012, 133, 221–224. [Google Scholar] [PubMed]
- Karagol, B.S.; Zencıroglu, A.; Kundak, A.; Okumus, N.; Aydin, M.; Uner, C.J.N. A linear fracture and meningitis associated with non-infected cephalohematoma in a neonate. Neuropediatrics 2010, 41, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Hedberg, A.; Hårdemark, H.G.; Olsson-Liljequist, B.; Sjölin, J. Penetration of fusidic acid and rifampicin into cerebrospinal fluid in low-grade inflammatory meningitis caused by Staphylococcus epidermidis. Clin. Microbiol. Infect. 2004, 10, 765–768. [Google Scholar] [CrossRef][Green Version]
- Van de Beek, D.; De Gans, J.; Spanjaard, L.; Weisfelt, M.; Reitsma, J.B.; Vermeulen, M. Clinical features and prognostic factors in adults with bacterial meningitis. N. Engl. J. Med. 2004, 351, 1849–1859. [Google Scholar] [CrossRef] [PubMed]
- Forgie, S.E. The history and current relevance of the eponymous signs of meningitis. Pediatr. Infect. Dis. J. 2016, 35, 749–751. [Google Scholar] [CrossRef] [PubMed]
- Mehndiratta, M.; Nayak, R.; Garg, H.; Kumar, M.; Pandey, S. Appraisal of Kernig’s and Brudzinski’s sign in meningitis. Ann. Indian Acad. Neurol. 2012, 15, 287. [Google Scholar] [CrossRef] [PubMed]
- Nakao, J.H.; Jafri, F.N.; Shah, K.; Newman, D.H. Jolt accentuation of headache and other clinical signs: Poor predictors of meningitis in adults. Am. J. Emerg. Med. 2014, 32, 24–28. [Google Scholar] [CrossRef]
- Busl, K.M. Nosocomial Infections in the Neurointensive Care Unit. Neurol. Clin. 2017, 35, 785–807. [Google Scholar] [CrossRef]
- Li, Y.M.; Blaskiewicz, D.J.; Hall, W.A. Shunt-related intracranial abscess caused by Staphylococcus lugdunensis in a hydranencephalic patient. World Neurosurg. 2013, 80, e387–e389. [Google Scholar] [CrossRef] [PubMed]
- Matas, A.; Veiga, A.; Gabriel, J. Brain Abscess due to Staphylococcus lugdunensis in the Absence of Endocarditis or Bacteremia. Case Rep. Neurol. 2015, 7, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, T.; Nagao, M.; Yamamoto, M.; Matsumura, Y.; Kitano, T.; Takaori-Kondo, A.; Ichiyama, S. Staphylococcus epidermidis meningitis in the absence of a neurosurgical device secondary to catheter-related bloodstream infection: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 106. [Google Scholar] [CrossRef] [PubMed]
- Bijlsma, M.W.; Brouwer, M.C.; Kasanmoentalib, E.S.; Kloek, A.T.; Lucas, M.J.; Tanck, M.W.; van der Ende, A.; van de Beek, D. Community-acquired bacterial meningitis in adults in the Netherlands, 2006–2014: A prospective cohort study. Lancet Infect. Dis. 2016, 16, 339–347. [Google Scholar] [CrossRef]
- Uzzan, B.; Cohen, R.; Nicolas, P.; Cucherat, M.; Perret, G.Y. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: A systematic review and meta-analysis. Crit. Care Med. 2006, 34, 1996–2003. [Google Scholar] [CrossRef]
- Schlenk, F.; Frieler, K.; Nagel, A.; Vajkoczy, P.; Sarrafzadeh, A.S. Cerebral microdialysis for detection of bacterial meningitis in aneurysmal subarachnoid hemorrhage patients: A cohort study. Crit. Care. 2009, 13, R2. [Google Scholar] [CrossRef]
- Vikse, J.; Henry, B.M.; Roy, J.; Ramakrishnan, P.K.; Tomaszewski, K.A.; Walocha, J.A. The role of serum procalcitonin in the diagnosis of bacterial meningitis in adults: A systematic review and meta-analysis. Int. J. Infect. Dis. 2015, 38, 68–76. [Google Scholar] [CrossRef]
- Khalili, H.; Yadollahikhales, G.; Isaee, M. Diagnostic Accuracy of Peripheral White Blood Cell Count, Fever and Acute Leukocutosis for Bacterial Meningitis in Patients with Severe Traumatic Brain Injury. Bull. Emerg. Trauma 2015, 3, 53. [Google Scholar]
- Kaabia, N.; Scauarda, D.; Lena, G.; Drancourt, M. Molecular identification of Staphylococcus lugdunensis in a patient with meningitis. J. Clin. Microbiol. 2002, 40, 1824–1825. [Google Scholar] [CrossRef][Green Version]
- Kastrup, O.; Isabel, W.; Matthias, M. Neuroimaging of infections. NeuroRx 2005, 2, 324–332. [Google Scholar] [CrossRef]
- Proulx, N.; Frechette, D.; Toye, B.; Chan, J.; Kravcik, S. Delays in the administration of antibiotics are associated with mortality from adult acute bacterial meningitis. Qjm 2005, 98, 291–298. [Google Scholar] [CrossRef]
- Brouwer, M.C.; McIntyre, P.; de Gans, J.; Prasad, K.; van de Beek, D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst. Rev. 2007, 1. [Google Scholar] [CrossRef]
- Zhao, Z.; Hua, X.; Yu, J.; Zhang, H.; Li, J.; Li, Z. Duration of empirical therapy in neonatal bacterial meningitis with third generation cephalosporin: A multicenter retrospective study. Arch. Med. Sci. 2019, 15, 1482. [Google Scholar] [CrossRef]
- Brouwer, M.C.; Tunkel, A.R.; van de Beek, D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin. Microbiol. Rev. 2010, 23, 467–492. [Google Scholar] [CrossRef]
- Vijayan, P.; Srinivas, D.; Siddaiah, N.; Bahubali, V. Device-Associated Meningitis by Linezolid-Resistant Staphylococcus haemolyticus in a Vancomycin-Hypersensitive Patient. J. Neurosci. Rural. Pract. 2019, 10, 718–720. [Google Scholar] [CrossRef]
- World Health Organization. Control of Epidemic Meningococcal Disease: WHO Practical Guidelines; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Epidemiology of meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenza. Chapter 2; 2011. Available online: https://www.cdc.gov/meningitis/lab-manual/chpt02-epi.html (accessed on 18 May 2020).
- Jiang, H.; Su, M.; Kui, L.; Huang, H.; Qiu, L.; Li, L.; Ma, J.; Du, T.; Fan, M.; Sun, Q. Prevalence and antibiotic resistance profiles of cerebrospinal fluid pathogens in children with acute bacterial meningitis in Yunnan province, China, 2012–2015. PLoS ONE 2017, 12, e0180161. [Google Scholar] [CrossRef]
- De Gans, J.; Van de Beek, D. Dexamethasone in adults with bacterial meningitis. N. Engl. J. Med. 2002, 347, 1549–1556. [Google Scholar] [CrossRef]
- Wall, E.C.; Ajdukiewicz, K.M.; Bergman, H.; Heyderman, R.S.; Garner, P. Osmotic therapies added to antibiotics for acute bacterial meningitis. Cochrane Database Syst. Rev. 2018, 2, 576–585. [Google Scholar] [CrossRef]
- Ratilal, B.O.; Costa, J.; Pappamikail, L.; Sampaio, C. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst. Rev. 2015, 4. [Google Scholar] [CrossRef]
- Gianella, S.; Ulrich, S.; Huttner, B.; Speich, R. Conservative management of a brain abscess in a patient with Staphylococcus lugdunensis endocarditis. Eur. J. Clin. Microbiol. Infect. Dis. 2006, 25, 476–478. [Google Scholar] [CrossRef][Green Version]
- Rebai, L.; Fitouhi, N.; Daghmouri, M.A.; Bahri, K. Linezolid for the treatment of postneurosurgical infection caused by methicillin-resistant Staphylococcus. Surg. Neurol. Int. 2019, 10. [Google Scholar] [CrossRef]
- Mounier, R.; Lobo, D.; Hulin, A.; Nebbad, B.; Cook, F.; Dhonneur, G. Is First-Line Vancomycin Still the Best Option to Treat Staphylococcus Health Care–Associated Meningitis? World Neurosurg. 2017, 99, e1–e812. [Google Scholar] [CrossRef] [PubMed]
- Denetclaw, T.H.; Suehiro, I.; Wang, P.K.; Tolliver, G. Successful treatment of ventriculostomy-associated meningitis caused by multidrug resistant coagulase-negative Staphylococcus epidermidis using low-volume intrathecal daptomycin and loading strategy. Ann. Pharmacother. 2014, 48, 1376–1379. [Google Scholar] [CrossRef]
- Vena, A.; Falcone, M.; Comandini, E.; Meledandri, M.; Novelli, A.; Campanile, F.; Stefani, S.; Venditti, M. Daptomycin plus trimethoprim/sulfamethoxazole combination therapy in post-neurosurgical meningitis caused by linezolid-resistant Staphylococcus epidermidis. Diagn. Microbiol. Infect. Dis. 2013, 76, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Kui, L.; Huang, H.; Su, M.; Wen, B.P. Frequency distribution and antibiotic resistance of pathogens from the cerebrospinal fluid of 116 children with bacterial meningitis. Zhongguo Dang Dai Er Ke Za Zhi 2013, 15, 264–267. [Google Scholar]
- Watanabe, S.; Tanaka, A.; Ono, T.; Ohta, M.; Miyamoto, H.; Tauchi, H.; Tanaka, M.; Suemaru, K.; Araki, H. Treatment with linezolid in a neonate with meningitis caused by methicillin-resistant Staphylococcus epidermidis. Eur. J. Pediatr. 2013, 172, 1419–1421. [Google Scholar] [CrossRef] [PubMed]
- Lucas, M.J.; Brouwer, M.C.; van de Beek, D. Neurological sequelae of bacterial meningitis. J. Infect. 2016, 73, 18–27. [Google Scholar] [CrossRef]
- MacGee, E.E.; Cauthen, J.C.; Brackett, C.E. Meningitis following acute traumatic cerebrospinal fluid fistula. J. Neurosurg. 1970, 33, 312–316. [Google Scholar] [CrossRef]
- Crawford, C.; Kennedy, N.; Weir, W.R.C. Cerebrospinal fluid rhinorrhoea and Haemophilus influenzae meningitis 37 years after a head injury. J. Infect. 1994, 28, 93–97. [Google Scholar] [CrossRef]
- Appelbaum, E. Meningitis following trauma to the head and face. JAMA 1960, 173, 1818–1822. [Google Scholar] [CrossRef]
- Okada, J.; Tsuda, T.; Takasugi, S.; Nishida, K.; Tóth, Z.; Matsumoto, K. Unusually late onset of cerebrospinal fluid rhinorrhea after head trauma. Surg. Neurol. 1991, 35, 213–217. [Google Scholar] [CrossRef]
- Plaisier, B.R. Post-traumatic meningitis: Risk factors, clinical features, bacteriology, and outcome. Int. J. Neurosurg. 2005, 2, 1. [Google Scholar]
- Lai, W.-A.; Chen, S.-F.; Tsai, N.-W.; Chang, C.-C.; Chang, W.-N.; Lu, C.-H.; Chuang, Y.-C.; Chien, C.-C.; Huang, C. Clinical characteristics and prognosis of acute bacterial meningitis in elderly patients over 65: A hospital-based study. BMC Geriatr. 2011, 11, 91. [Google Scholar] [CrossRef]
- Tian, R.; Hao, S.; Hou, Z.; Gao, Z.; Liu, B. The characteristics of post-neurosurgical bacterial meningitis in elective neurosurgery in 2012: A single institute study. Clin. Neurol. Neurosurg. 2015, 139, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Lien, C.-Y.; Huang, C.-R.; Tsai, N.-W.; Chang, C.-C.; Lu, C.-H.; Chang, W. Clinical Characteristics and Therapeutic Outcomes of Postneurosurgical Bacterial Meningitis in Elderly Patients over 65: A Hospital-based Study. Acta Neurol. Taiwan 2017, 26, 144–153. [Google Scholar]
- Drinkovic, D.; Pottumarthy, S.; Knight, D.; Morris, A. Neonatal coagulase-negative staphylococcal meningitis: A report of two cases. Pathology 2002, 34, 586–588. [Google Scholar] [CrossRef]
- Tian, L.; Zhang, Z.; Sun, Z. Pathogen Analysis of Central Nervous System Infections in a Chinese Teaching Hospital from 2012–2018: A Laboratory-based Retrospective Study. Curr. Med. Sci. 2019, 39, 449–454. [Google Scholar] [CrossRef] [PubMed]
- AlDhaleei, W.A.; Bhagavathula, A.S.; Aldoghaither, R. Embolic Stroke and Meningitis Secondary to Staphylococcus lugdunensis Native Valve Endocarditis. Case Rep. Infect. Dis. 2019, 2019, 7910262. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Kanamaru, A.; Uchida, H.; Yano, M.; Tada, H. A case of bacterial meningitis caused by methicillin-resistant Staphylococcus lugdunensis after surgery. Rinsho Shinkeigaku 2016, 56, 773–776. [Google Scholar] [CrossRef]
- Chitnis, A.S.; Guh, A.Y.; Benowitz, I.; Srinivasan, V.; Gertz Jr, R.E.; Shewmaker, P.L.; Beall, B.W.; O’Connell, H.; Noble-Wang, J.; Gornet, M. Outbreak of bacterial meningitis among patients undergoing myelography at an outpatient radiology clinic. J. Am. Coll. Radiol. 2012, 9, 185–190. [Google Scholar] [CrossRef]
- Kawaguchi, Y.; Seki, S.; Yasuda, T.; Nakamura, Y.; Nakano, M.; Kimura, T. Postoperative meningitis in patients with cervical cord tumor: A case report. Asian Spine J. 2010, 4, 136. [Google Scholar] [CrossRef]
- Nagashima, G.; Okamoto, N.; Okuda, M.; Nakashima, K.; Noda, M.; Itokawa, H.; Suzuki, R.; Fujimoto, T.; Marumo, K. Chemotherapy, Effect of linezolid against postneurosurgical meningitis caused by methicillin-resistant Staphylococcus epidermidis: Case report. J. Infect. Chemother. 2008, 14, 147. [Google Scholar] [CrossRef] [PubMed]
- Stevens, N.T.; Tharmabala, M.; Dillane, T.; Greene, C.M.; O’Gara, J.P.; Humphreys, H. Biofilm and the role of the ica operon and aap in Staphylococcus epidermidis isolates causing neurosurgical meningitis. Clin. Microbiol. Infect. 2008, 14, 719–722. [Google Scholar] [CrossRef]
- Kruse, A.-J.; Peerdeman, S.; Bet, P.; Debets-Ossenkopp, Y. Successful treatment with linezolid and rifampicin of meningitis due to methicillin-resistant Staphylococcus epidermidis refractory to vancomycin treatment. Eur. J. Clin. Microbiol. Infect. Dis. 2006, 25, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.R.; Lu, C.H.; Wu, J.J.; Chang, H.W.; Chien, C.C.; Lei, C.B.; Chang, W.N. Coagulase-negative staphylococcal meningitis in adults: Clinical characteristics and therapeutic outcomes. Infection 2005, 33, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, F.; Mander, K.A.; Leonard, A.V.; Vink, R. Neurogenic inflammation after traumatic brain injury and its potentiation of classical inflammation. J. Neuroinflammation 2016, 13, 264. [Google Scholar] [CrossRef] [PubMed]
- Ziebell, J.M.; Morganti-Kossmann, M.C. Involvement of pro- and anti-inflammatory cytokines and chemokines in the pathophysiology of traumatic brain injury. Neurotherapeutics 2010, 7, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Cash, A.; Theus, M.H. Mechanisms of Blood–Brain Barrier Dysfunction in Traumatic Brain Injury. Int. J. Mol. Sci. 2020, 21, 3344. [Google Scholar] [CrossRef]
- Sorby-Adams, A.J.; Marcoionni, A.M.; Dempsey, E.R.; Woenig, J.A.; Turner, R.J. The Role of Neurogenic Inflammation in Blood-Brain Barrier Disruption and Development of Cerebral Oedema Following Acute Central Nervous System (CNS) Injury. Int. J. Mol. Sci. 2017, 18, 1788. [Google Scholar] [CrossRef] [PubMed]
- Lorente, L.; Martín, M.M.; Almeida, T.; Hernández, M.; Ramos, L.; Argueso, M.; Cáceres, J.J.; Solé-Violán, J.; Jiménez, A. Serum substance P levels are associated with severity and mortality in patients with severe traumatic brain injury. Crit Care 2015, 19, 192. [Google Scholar] [CrossRef]
- Lorente, L.; Martín, M.M.; Pérez-Cejas, A.; González-Rivero, A.F.; Argueso, M.; Ramos, L.; Solé-Violán, J.; Cáceres, J.J.; Jiménez, A.; García-Marín, V. Persistently High Serum Substance P Levels and Early Mortality in Patients with Severe Traumatic Brain Injury. World Neurosurg. 2019, 132, e613–e617. [Google Scholar] [CrossRef]
- Hooper, C.; Pinteaux-Jones, F.; Fry, V.A.; Sevastou, I.G.; Baker, D.; Heales, S.J.; Pocock, J.M. Differential effects of albumin on microglia and macrophages; implications for neurodegeneration following blood-brain barrier damage. J. Neurochem. 2009, 109, 694–705. [Google Scholar] [CrossRef] [PubMed]
- Ralay Ranaivo, H.; Hodge, J.N.; Choi, N.; Wainwright, M.S. Albumin induces upregulation of matrix metalloproteinase-9 in astrocytes via MAPK and reactive oxygen species-dependent pathways. J. Neuroinflamm. 2012, 9, 68. [Google Scholar] [CrossRef] [PubMed]
- Muri, L.; Leppert, D.; Grandgirard, D.; Leib, S.L. MMPs and ADAMs in neurological infectious diseases and multiple sclerosis. Cell. Mol. Life Sci. 2019, 76, 3097–3116. [Google Scholar] [CrossRef] [PubMed]
- Fields, G.B. The Rebirth of Matrix Metalloproteinase Inhibitors: Moving Beyond the Dogma. Cells 2019, 8, 984. [Google Scholar] [CrossRef] [PubMed]
- Crupi, R.; Cordaro, M.; Cuzzocrea, S.; Impellizzeri, D. Management of Traumatic Brain Injury: From Present to Future. Antioxidants 2020, 9, 297. [Google Scholar] [CrossRef]
- Yang, Z.; Zhu, T.; Mondello, S.; Akel, M.; Wong, A.T.; Kothari, I.M.; Lin, F.; Shear, D.A.; Gilsdorf, J.S.; Leung, L.Y.; et al. Serum-Based Phospho-Neurofilament-Heavy Protein as Theranostic Biomarker in Three Models of Traumatic Brain Injury: An Operation Brain Trauma Therapy Study. J. Neurotrauma 2019, 36, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Kövesdi, E.; Lückl, J.; Bukovics, P.; Farkas, O.; Pál, J.; Czeiter, E.; Szellár, D.; Dóczi, T.; Komoly, S.; Büki, A. Update on protein biomarkers in traumatic brain injury with emphasis on clinical use in adults and paediatrics. Acta Neurochir. (Wien.) 2010, 152, 1–17. [Google Scholar] [CrossRef]
- Berger, R.P.; Beers, S.R.; Richichi, R.; Wiesman, D.; Adelson, P.D. Serum biomarker concentrations and outcome after pediatric traumatic brain injury. J. Neurotrauma 2007, 24, 1793–1801. [Google Scholar] [CrossRef]
- Fineschi, V.; Viola, R.V.; La Russa, R.; Santurro, A.; Frati, P. A Controversial Medicolegal Issue: Timing the Onset of Perinatal Hypoxic-Ischemic Brain Injury. Mediators Inflamm. 2017, 2017, 6024959. [Google Scholar] [CrossRef]
- Neri, M.; Büttner, A.; Fineschi, V. Brain Injury due to Mechanical Trauma and Ischemic-Hypoxic Insult: Biomarkers of Brain Injury and Oxidative Stress. Oxid Med. Cell Longev. 2017, 2017, 8923472. [Google Scholar] [CrossRef]
- Frati, A.; Cerretani, D.; Fiaschi, A.I.; Frati, P.; Gatto, V.; La Russa, R.; Pesce, A.; Pinchi, E.; Santurro, A.; Fraschetti, F.; et al. Diffuse Axonal Injury and Oxidative Stress: A Comprehensive Review. Int. J. Mol. Sci. 2017, 18, 2600. [Google Scholar] [CrossRef]
- Sharew, A.; Bodilsen, J.; Hansen, B.R.; Nielsen, H.; Brandt, C.T. The cause of death in bacterial meningitis. BMC Infect. Dis. 2020, 20, 182. [Google Scholar] [CrossRef] [PubMed]
- Neri, M.; Frati, A.; Turillazzi, E.; Cantatore, S.; Cipolloni, L.; Di Paolo, M.; Frati, P.; La Russa, R.; Maiese, A.; Scopetti, M.; et al. Immunohistochemical evaluation of aquaporin-4 and its correlation with CD68, IBA-1, HIF-1α, GFAP, and CD15 expressions in fatal traumatic brain injury. Int. J. Mol. Sci. 2018, 19, 3544. [Google Scholar]
- La Russa, R.; Maiese, A.; Viola, R.V.; De Matteis, A.; Pinchi, E.; Frati, P.; Fineschi, V. Searching for highly sensitive and specific biomarkers for sepsis: State-of-the-art in post-mortem diagnosis of sepsis through immunohistochemical analysis. Int. J. Immunopathol. Pharmacol. 2019, 33, 2058738419855226. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Bolino, G.; Mastracchio, A.; Frati, P.; Fineschi, V. An immunohistochemical study of the diagnostic value of TREM-1 as marker for fatal sepsis cases. Biotech. Histochem. 2019, 94, 159–166. [Google Scholar] [CrossRef]
- Maiese, A.; Del Nonno, F.; Dell’Aquila, M.; Moauro, M.; Baiocchini, A.; Mastracchio, A.; Bolino, G. Postmortem diagnosis of sepsis: A preliminary immunohistochemical study with an anti-procalcitonin antibody. Leg. Med. (Tokyo) 2017, 28, 1–5. [Google Scholar] [CrossRef]
- Pinchi, E.; Frati, A.; Cipolloni, L.; Aromatario, M.; Gatto, V.; La Russa, R.; Pesce, A.; Santurro, A.; Fraschetti, F.; Frati, P.; et al. Clinical-pathological study on β-APP, IL-1β, GFAP, NFL, Spectrin II, 8OHdG, TUNEL, miR-21, miR-16, miR-92 expressions to verify DAI-diagnosis, grade and prognosis. Sci. Rep. 2018, 8, 1–13. [Google Scholar] [CrossRef]
- Gayen, M.; Bhomia, M.; Balakathiresan, N.; Knollmann-Ritschel, B. Exosomal MicroRNAs Released by Activated Astrocytes as Potential Neuroinflammatory Biomarkers. Int. J. Mol. Sci. 2020, 21, 2312. [Google Scholar] [CrossRef]
- Pinchi, E.; Frati, A.; Cantatore, S.; D’Errico, S.; La Russa, R.; Maiese, A.; Palmieri, M.; Pesce, A.; Viola, R.V.; Frati, P.; et al. Acute Spinal Cord Injury: A Systematic Review Investigating miRNA Families Involved. Int. J. Mol. Sci. 2019, 20, 1841. [Google Scholar] [CrossRef]
- Slota, J.A.; Booth, S.A. MicroRNAs in Neuroinflammation: Implications in Disease Pathogenesis, Biomarker Discovery and Therapeutic Applications. Non-Coding RNA 2019, 5, 35. [Google Scholar] [CrossRef]
- Sessa, F.; Maglietta, F.; Bertozzi, G.; Salerno, M.; Di Mizio, G.; Messina, G.; Montana, A.; Ricci, P.; Pomara, C. Human Brain Injury and miRNAs: An Experimental Study. Int. J. Mol. Sci. 2019, 20, 1546. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, G.C.; Smothers, C.G.; Winkelman, C. Bioinformatic analysis of brain-specific miRNAs for identification of candidate traumatic brain injury blood biomarkers [published online ahead of print, 2020 Jun 4]. Brain Inj. 2020, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]



| Authors | Year | Description |
|---|---|---|
| Vos, T. | 2017 | The Global Burden of Diseases, Injuries, and Risk Factors Study 2016 (GBD 2016) provides a comprehensive assessment of prevalence, incidence, and years lived with disability (YLDs) for 328 causes in 195 countries and territories from 1990 to 2016. The decrease in death rates since 1990 for most causes has not been matched by a similar decline in age-standardised YLD rates |
| Yelehe-Okouma, M. | 2018 | Aseptic meningitis associates a typical clinical picture of meningitis with the absence of bacterial or fungal material in the cerebrospinal fluid. About 62 references were found, and only 18 were selected based on their type (case reports, review) and relevance (study characteristics, quality, and accuracy). DIAM remains a diagnosis of elimination. |
| Eljamel, M. S. | 1990 | The management of acute traumatic cerebrospinal fluid (CSF) fistulae is still a matter of debate and hinges on what is perceived to be the risk of subsequent intracranial infection. They have thus carried out a retrospective analysis of 160 cases of traumatic CSF leaks. The overall incidence of meningitis in this group before surgical dural repair was 30.6% (49/160), the cumulative risk exceeded 85% at 10-year follow-up, and the meningitis was fatal in 4.1% (2/49). |
| Matschke, J. | 2001 | Six cases of post-traumatic meningitis as the cause of death from the archives of the Institute of Legal Medicine in Hamburg are presented. There were all males; age varying between 24 and 90 years (mean 58 years); range of the interval between original trauma and beginning of symptoms was 2 days up to 8 years; in 50% of the cases, meningeal swabs yielded Streptococcus pneumoniae. |
| Van de Beek, D. | 2006 | In this review, they summarize the current concepts of the initial approach to the treatment of adults with bacterial meningitis, highlighting adjunctive dexamethasone therapy, and focusing on the management of neurologic complications. |
| Adriani, K. S. | 2015 | Bacterial meningitis is a life-threatening infectious disease with high mortality and disability rates, despite availability of antibiotics and adjunctive therapy with dexamethasone. Several risk factors and predisposing conditions have been identified that increase susceptibility to bacterial meningitis: immunodeficiency, host genetic factors, or anatomical defects of the natural barriers of the central nervous system. |
| Van de Beek, D. | 2016 | This is the ESCMID guideline for diagnosis and treatment of acute bacterial meningitis. |
| Van de Beek, D. | 2010 | Nosocomial bacterial meningitis may result from invasive procedures; complicated head trauma; or, in rare cases, metastatic infection in patients with hospital-acquired bacteremia. These cases of meningitis are caused by a different spectrum of microorganisms. |
| Phang, S. Y. | 2016 | Using an algorithm, the authors studied the most suitable management of cerebrospinal fluid losses after skull base fracture. The results obtained revealed some many unresolved questions, which will need further studies. |
| Prosser, J. D. | 2011 | A review proposed to evaluate both treatment for CSF leaks: conservative and operative one. Clinical decisions are taken based on the current literature. |
| Sonig, A. | 2012 | This study aims to analyze the risk factors associated with the development of posttraumatic meningitis through the analysis of the NIS database. It turned out that cerebrospinal fluid rhinorrhea and CSF otorrhea are independent predictors of posttraumatic meningitis. The second goal was to analyze the overall hospitalization cost related to posttraumatic meningitis and factors associated with that cost. Meningitis and CSF fistulas resulted as independent risk factors to significantly increased hospitalization cost. |
| Tebruegge, M. | 2008 | This review studies recurrent bacterial meningitis and its relations with anatomical anomalies (most common cause) and immunodeficiences. Early diagnosis is fundamental to prevent further episodes. |
| Durand, M. L. | 1993 | The authors studied the characteristics of acute bacterial meningitis, including epidemiology, eziology, and mortality. |
| Adriani, K. S. | 2007 | A prospective study evaluating episodes of recurrent bacterial meningitis. Remote head injury and CSF leakage are considered as predisposing conditions. |
| Heckenberg, S. G. | 2014 | A review of the epidemiology, pathophysiology, and management of bacterial meningitis that shows adequate and prompt treatment of bacterial meningitis (antibacterial) is critical to improve outcomes. |
| Sağlam, M. | 2013 | This article studies causative agents of bacterial meningitis by culturing CSF samples. Most frequently isolated agents were H. influenzae, N. meningitidis, and Str. Pneumoniae. |
| Hernandez, J.L. | 2001 | An analysis of both clinical and microbiological characteristics of a series of patients with infection by Staphylococcus schleiferi. The results showed the importance of careful identification of Staphylococcus schleiferi in the clinical microbiology laboratory. |
| Chang, W.N. | 2007 | A clinical comparison of meningitis caused by S. Aureaus and coagulase-negative Staphylococcus (CoNS). The study revealed an increase of methicillin-resistant, postneurosurgical staphylococcal infection in acute bacterial meningitis. Patients with CoNS infection presented younger age at onset and a lower mortality rate. |
| Garg, R. K. | 2017 | The article studies a complication of acute coagulase-negative Staphylococcus (CoNS) meningitis: brainsteam infarct. |
| Oud, L. | 2011 | A study about community acquired coagulase-negative Staphylococcus meningitis. |
| Lin, W.-S. | 2013 | A case report that underlines the importance of a prompt identification of panspinal epidural abscess with detailed clinical, neurologic, and neuroimaging studies. |
| Dumas, G. | 2012 | Subacute otitis media complicated by labyrinthitis, early onset of facial paralysis, or any other oranial nerve palsy should raise suspicion of tuberculosis. The diagnostic workup should include histological and bacteriologic samples, liver markers of intacellular damage, as well as ELlspot test. The prognosis remains poor especially in immunocompromised patients despite appropriate treatment. |
| Karagol, B.S. | 2010 | A study that reveales the utmost importance of screening studies in order to be aware of the pathogenic potential of cephalohematomas. |
| Hedberg, A. | 2004 | A study about rifampicin and fusidic acid therapy in a patient with severe hypersensitivity reaction to vancomycin. |
| Van de Beek, D. | 2004 | A nationwide study in the Netherlands determines clinical features and prognostic factors in adults with community-acquired acute bacterial meningitis: the mortality associated with bacterial meningitis is high, and the strongest risk factors for an unfavorable outcome are those that are indicative of systemic compromise, a low level of consciousness, and infection with S. pneumoniae. |
| Forgie, S. E. | 2016 | A review that helps the clinician to understand how the history related to sings of meningitis (Kernig, Brudzinski, Amoss) is still germane to clinical practice today. |
| Mehndiratta, M. | 2012 | Kernig’s and Brudzinski’s signs are not very sensitive for detecting meningitis and, when absent, should not be inferred as there is no evidence of meningitis. Although the sensitivity is quite low, the high specificity suggests that if Kernig’s or Brudzinski’s sign is present, there is a high likelihood for meningitis. The two signs, Kernig’s and Brudzinski’s, are often performed together in clinical practice. |
| Nakao, J. H. | 2014 | A prospective observational study of neurologically intact emergency department (ED) patients undergoing lumbar puncture in two inner city academic EDs to validate the sensitivity and specificity of jolt accentuation (exacerbation of a baseline headache with horizontal rotation of the neck) and to assess the sensitivity and specificity of Kernig sign, Brudzinski sign, and nuchal rigidity, in predicting cerebrospinal fluid (CSF) pleocytosis in individuals being assessed for meningitis. |
| Busl, K. M. | 2017 | This article reviews the concept of brain injury-induced immune modulation, and summarizes available data and knowledge on nosocomial meningitis and ventriculitis, and systemic infectious complications in patients with traumatic brain injury, ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, and status epilepticus. |
| Li, Y. M. | 2013 | When Staphylococcus lugdunensis is identified, a virulent and prolonged clinical course with the production of destructive lesions, similar to those with S. aureus, should be expected. A course of antibiotic therapy and aggressive management that may include surgical treatment will be needed. |
| Matas, A. | 2015 | A case report of a patient who presented with a single, large, right, frontoparietal abscess that evolved despite conventional antibiotic treatment, in the absence of bacteremia and endocarditis. Further studies highlighted the presence of Staphylococcus Ludgunensis. |
| Noguchi, T. | 2018 | A case report of Staphylococcus epidermidis meningitis in a patient with neutropenia without a neurosurgical device who was successfully treated. |
| Bijlsma, M.W. | 2016 | A study on causative pathogens, clinical characteristics, and outcome of adult community-acquired bacterial meningitis after the introduction of adjunctive dexamethasone treatment and nationwide implementation of paediatric conjugate vaccine. |
| Uzzan, B. | 2006 | This study demonstrates that procalcitonin is a good biological diagnostic marker for sepsis, severe sepsis, or septic shock; has difficult diagnoses in critically ill patients; and is superior to C-reactive protein. Procalcitonin should be included in diagnostic guidelines for sepsis and in clinical practice in intensive care units. |
| Schlenk, F. | 2009 | This study reveales that a decrease in microdialysis glucose combined with the presence of fever detected bacterial meningitis with acceptable sensitivity and specificity, while CSF chemistry failed to indicate bacterial meningitis. In patients with subarachnoid hemorrhage (SAH), where CSF cell count is not available or helpful, microdialysis might serve as an adjunct criterion for early diagnosis of bacterial meningitis. |
| Vikse, J. | 2015 | This study underlines the importance of serum procalcitonin (PCT) as a highly accurate diagnostic test for rapid differentiation between bacterial and viral causes of meningitis in adults. |
| Khalili, H. | 2015 | The results of the study indicate that peripheral blood leukocyte count, fever (>38 ˚C), and white blood cells rise (>10%) are non-reliable markers for diagnosis of bacterial meningitis in patients with severe traumatic brain injury (TBI). |
| Kaabia, N. | 2002 | This report describes a case of S. lugdunensis meningitis, occurring six days after a endoscopic ventriculostomy, in a 12-year-old child. Coagulase-negative Staphylococcus sp. was isolated in pure culture from the cerebrospinal fluid and was definitely identified as Staphylococcus lugdunensis after the 16S ribosomal DNA gene and rpoB gene were sequenced. |
| Kastrup, O. | 2005 | The review summarizes imaging findings and recent advances in the diagnosis of pyogenic brain abscess, ventriculitis, viral disease including exotic and emergent viruses, and opportunistic disease. For each condition, the ensuing therapeutic steps are presented. |
| Proulx, N. | 2005 | There is an independent incremental association between delays in administrating antibiotics and mortality from adult acute bacterial meningitis. Inappropriate diagnostic-treatment sequences were significant predictors of such treatment delays. |
| Brouwer, M. C. | 2007 | This article shows that corticosteroids significantly reduced hearing loss and neurological sequelae, but did not reduce overall mortality. Data support the use of corticosteroids in patients with bacterial meningitis in high-income countries. We found no beneficial effect in low-income countries. |
| Zhao, Z. | 2019 | Third-generation cephalosporin therapy does not have a different prognosis for negative CSF culture of neonatal bacterial meningitis in term infants in this study. |
| Brouwer, M. C. | 2010 | This review provides recommendations for empirical antimicrobial and adjunctive treatments for clinical subgroups and review available laboratory methods in making the etiological diagnosis of bacterial meningitis. It also summarizes risk factors, clinical features, and microbiological diagnostics. |
| Vijayan, P. | 2019 | Postsurgical device-related meningitis caused by multidrug-resistant coagulase-negative Staphylococci often complicates the treatment options. Monitoring the rational use of linezolid is crucial to avoid the spread of resistance and also comprehensive perioperative care to prevent health care-associated infection. |
| Organization, W. H. | 1998 | Practical guidelines that help clinicians in the control of epidemic meningococcal disease. |
| Jiang, H. | 2017 | This article aims to investigate the prevalence and antibiotic resistance profiles of cerebrospinal fluid (CSF) pathogens in children with acute bacterial meningitis in Southwest China. Gentamycin, ofloxacin, linezolid, and vancomycin were identified as the most effective antibiotics for Streptococcus pneumoniae, each with susceptibility rates of 100%. It was notable that other emerging pathogens, such as Listeria monocytogenes and group D streptococcus, cannot be underestimated in meningitis. |
| De Gans, J. | 2002 | The study demonstrates that early treatment with dexamethasone improves the outcome in adults with acute bacterial meningitis and does not increase the risk of gastrointestinal bleeding. |
| Wall, E. C. | 2018 | Osmotic therapies have been proposed as an adjunct to improve mortality and morbidity from bacterial meningitis. Data from trials to date have not demonstrated a benefit on death, but may reduce deafness. Osmotic diuretics, including glycerol, should not be given to adults and children with bacterial meningitis unless as part of a carefully conducted randomised controlled trial. |
| Ratilal, B. O. | 2015 | A study carried out to evaluate the effectiveness of prophylactic antibiotics for preventing meningitis in patients with basilar skull fractures. The evidence does not support prophylactic antibiotic use in patients with basilar skull fractures, whether or not there is evidence of CSF leakage. Until more research is available, the effectiveness of antibiotics in patients with basilar skull fractures cannot be determined because studies published to date are flawed by biases. |
| Gianella, S. | 2006 | A case of cerebral abscess as an embolic complication of infective endocarditis owing to S. Lugdunensis. Conservative methods were used and the efficacy of this approach is supported by the results of the literature review. The described treatment validates the thesis that, in select clinical settings, it is possible to cure such a serious disorder without surgical intervention. |
| Rebai, L. | 2019 | This article reveals that linezolid is an alternative to vancomycin for the treatment of postneurosurgical infection (PNSI) caused by methicillin-resistant Staphylococcus (MRS) with a high rate of efficacy. |
| Denetclaw, T. H. | 2014 | This case report shows the efficacy of low-volume intrathecal daptomycin in treatment of ventriculostomy-associated meningitis caused by multidrug resistant coagulase-negative staphylococcus epidermidis. |
| Vena, A. | 2013 | This article shows the efficacy of daptomycin plus trimethoprim/sulfamethoxazole combination therapy in post-neurosurgical meningitis caused by linezolid resistant staphylococcus epidermidis. |
| Jiang, H. | 2013 | The detected pathogens that cause bacterial meningitis to develop high resistance to commonly used antibiotics. To prevent misdiagnosis, careful attention should be paid to bacterial meningitis caused by Cryptococcus neoformans. |
| Watanabe, S. | 2013 | Linezolid may be a treatment option for neonates and infants for drain-associated meningitis caused by methicillin resistant Staphylococcus epidermidis. |
| Lucas, M. J., | 2016 | Neurological sequelae occur in a substantial amount of patients following bacterial meningitis. Most frequently reported sequelae are focal neurological deficits, hearing loss, cognitive impairment, and epilepsy. |
| Crawford, C. | 1994 | A case report of a bacterial meningitis (owing to H. Influenzae) in a 40-year-old patient that suffered an head injury at 3 years old. This study sets the longest recorded interval between head injury and meningitis. |
| Okada, J. | 1991 | Two cases of acute meningitis and cerebrospinal fluid rhinorrhea, in which the head trauma responsible occurred 10 and 30 years before, are presented. The causes of this late onset cannot be clearly explained. |
| Plaisier, B. R. | 2005 | A retrospective analysis of patients with post-traumatic meningitis that reveals that admission Glasgow Coma Scale was predictive of good functional outcome, but it plays no role in death prediction. |
| Lai, W.-A. | 2011 | This study shows that he relative frequency of implicated pathogens of elderly acute bacterial meningitis (ABM) is similar to that of non-elderly ABM. Compared with non-elderly patients, the elderly ABM patients have a significantly lower incidence of peripheral blood leukocytosis. The mortality rate of elderly ABM remains high, and the presence of shock and seizures represents important prognostic factors. |
| Tian, R. | 2015 | This article analyzes the epidemilogy of post-neurosurgical meningitis in the northern mainland of China. Post-neurosurgical meningitis usually occurs in the autumn and winter of the year. Gram-positive organisms, which are sensitive to compound sulfamethoxazole and vancomycin, are the most common causative pathogens of post-neurosurgical meningitis. |
| Drinkovic, D. | 2002 | Two cases report that describe the onset of coagulase negative Stafilococci meningitis in neonates without CSF shunts. The succesful therapy consisted of vancomycin and rifampicin. |
| Tian, L. | 2019 | A retrospective study based on analysis of samples from patients with CNS infection in a clinical microbiology laboratory at a teaching hospital in China over a 6-year period indicated that the most common etiological agents were the bacteria Acinetobacter Baumani and Staphylococcus Aureus. The antibiotic resistance levels of A. Baumanni were found to be high and of concern, whereas isolates of C. neoformans were found to be sensitive to antifungal antibiotics. |
| AlDhaleei, W. A. | 2019 | Case report of a S. Lugdunensis endocarditis complicated by both embolic stroke and meningitis. |
| Sasaki, Y. | 2016 | Case report of a 51-year-old man undergone surgery forn Rathke’s cleft cyst complicated with CSF rinhorrea. CSF microbiological findings led to a diagnosis of bacterial meningitis. |
| Chitnis, A. S. | 2012 | This study suggests hygienic and behaviral norms to decrease the rate of bacterial meningitis transmitted by health care personnel |
| Kawaguchi, Y. | 2010 | A case report of a postoperative meningitis in a patient with cervical cord tumor, treated with intravenous linozelid. This latter drugs were shown to be one of the first choices in methicillin-resistant Staphylococcus epidermidis (MRSE) meningitis. |
| Nagashima, G. | 2008 | A case report of postneurosurgical meningitis caused by methicillin-resistant Staphylococcus epidermidis. The patient was succesfully treated with Linezolid. |
| Stevens, N. T. | 2008 | This article shows the full role of biofilm in Staphylococcus epidermidis meningitis. |
| Huang, C.R. | 2005 | This article analyzes the clinical characteristics and therapeutic outcomes of adult meningitis caused by coagulase-negative staphylococci (CoNS). Epidermidis was the most common CoNS subtype involved. All involved CoNS strains were oxacillin resistant. The therapeutic result showed that adult CoNS meningitis had a high mortality rate. |
| Neri, M. | 2018 | This study analyzes the expression of Aquaporin-4 in fatal traumatic brain injury. Further studies evaluated the correlation with cluster differentiation (CD)68, ionized calcium binding adapter molecule 1 (IBA-1), hypoxia induced-factor 1α (HIF-1α), glial fibrillary acid protein (GFAP), and CD15. |
| La Russa R. | 2019 | This study evaluated 56 experimental studies for diagnostic usefulness of specific immunohistochemical assays in the diagnosis of sepsis as a cause of death. |
| Maiese A. | 2019 | In this article, for the first time, the usefulness of Procalcitonin as a specific target for immunohistochemical assays was shown, investigating the implementation of such a test for forensic purposes in different organs. |
| Maiese A. | 2017 | In this immunohistochemical study, s-TREM-1 antibodies are used. The findings indicate that immunohistochemical assays for s-TREM-1 in sections from multiple organ samples (brain, heart, lung, liver, and kidney) could enable post-mortem diagnosis of sepsis with good sensitivity and specificity. |
| Biomarkers | Post-Traumatic Interval /Time of Death After Trauma | |||||
|---|---|---|---|---|---|---|
| Almost Immediate | 1 Day (20 ± 6 h) | 3 Days (72 ± 10 h) | 7 Days (6 ± 2 Days) | 14 Days (14 ± 4 Days) | 30 Days (30 ± 10 Days) | |
| AQP4 | +/- | +++ | +++ | ++++ | ++++ | ++++ |
| HIF-1α | +/- | ++ | +++ | +++ | ++ | ++ |
| GFAP | +/- | ++ | +++ | +++ | ++++ | ++++ |
| CD68 | +/- | + | +++ | +++ | ++++ | ++++ |
| IBA-1 | +/- | ++ | +++ | +++ | +++ | +++ |
| CD-15 | +/- | ++ | +++ | +++ | ++ | ++ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Russa, R.; Maiese, A.; Di Fazio, N.; Morano, A.; Di Bonaventura, C.; De Matteis, A.; Fazio, V.; Frati, P.; Fineschi, V. Post-Traumatic Meningitis Is a Diagnostic Challenging Time: A Systematic Review Focusing on Clinical and Pathological Features. Int. J. Mol. Sci. 2020, 21, 4148. https://doi.org/10.3390/ijms21114148
La Russa R, Maiese A, Di Fazio N, Morano A, Di Bonaventura C, De Matteis A, Fazio V, Frati P, Fineschi V. Post-Traumatic Meningitis Is a Diagnostic Challenging Time: A Systematic Review Focusing on Clinical and Pathological Features. International Journal of Molecular Sciences. 2020; 21(11):4148. https://doi.org/10.3390/ijms21114148
Chicago/Turabian StyleLa Russa, Raffaele, Aniello Maiese, Nicola Di Fazio, Alessandra Morano, Carlo Di Bonaventura, Alessandra De Matteis, Valentina Fazio, Paola Frati, and Vittorio Fineschi. 2020. "Post-Traumatic Meningitis Is a Diagnostic Challenging Time: A Systematic Review Focusing on Clinical and Pathological Features" International Journal of Molecular Sciences 21, no. 11: 4148. https://doi.org/10.3390/ijms21114148
APA StyleLa Russa, R., Maiese, A., Di Fazio, N., Morano, A., Di Bonaventura, C., De Matteis, A., Fazio, V., Frati, P., & Fineschi, V. (2020). Post-Traumatic Meningitis Is a Diagnostic Challenging Time: A Systematic Review Focusing on Clinical and Pathological Features. International Journal of Molecular Sciences, 21(11), 4148. https://doi.org/10.3390/ijms21114148







