Abstract
Post-traumatic meningitis is a dreadful condition that presents additional challenges, in terms of both diagnosis and management, when compared with community-acquired cases. Post-traumatic meningitis refers to a meningeal infection causally related to a cranio-cerebral trauma, regardless of temporal proximity. The PICO (participants, intervention, control, and outcomes) question was as follows: “Is there an association between traumatic brain injury and post-traumatic meningitis?” The present systematic review was carried out according to the Preferred Reporting Items for Systematic Review (PRISMA) standards. Studies examining post-traumatic meningitis, paying particular attention to victims of traumatic brain injury, were included. Post-traumatic meningitis represents a high mortality disease. Diagnosis may be difficult both because clinical signs are nonspecific and blurred and because of the lack of pathognomonic laboratory markers. Moreover, these markers increase with a rather long latency, thus not allowing a prompt diagnosis, which could improve patients’ outcome. Among all the detectable clinical signs, the appearance of cranial cerebrospinal fluid (CSF) leakage (manifesting as rhinorrhea or otorrhea) should always arouse suspicion of meningitis. On one hand, microbiological exams on cerebrospinal fluid (CSF), which represent the gold standard for the diagnosis, require days to get reliable results. On the other hand, radiological exams, especially CT of the brain, could represent an alternative for early diagnosis. An update on these issues is certainly of interest to focus on possible predictors of survival and useful tools for prompt diagnosis.
1. Introduction
Despite the dramatic decrease in incidence and mortality rates observed over the past decades, especially in high-income countries [1], meningitis still represents a medical emergency, which requires early diagnosis and prompt treatment in order to avoid death or serious neurological sequelae. The occurrence of meningitis is mostly related to microbial agents, particularly bacteria (so-called pyogenic meningitis), but meningeal involvement may also be secondary to solid/hematological malignancies, autoimmune diseases (including the recently described IgG4-related hypertrophic pachymeningitis), and other causes of aseptic inflammation (e.g., drug-induced) [2]. Among several predisposing factors, traumatic brain injury (TBI) is of particular interest, not only owing to its prevalence and its potential intrinsic severity; indeed, post-traumatic meningitis is a dreadful condition that presents additional challenges, in terms of both diagnosis and management, when compared with community-acquired cases. Post-traumatic meningitis stricto sensu refers to a meningeal infection causally related to a cranio-cerebral trauma, regardless of temporal proximity; therefore, meningitis following neurosurgical procedures (e.g., craniotomy, in-dwelling catheter placement), even those performed because of severe TBI, will not be discussed here. Although the risk of meningitis is the highest within the first week after brain injury [3], it has been widely documented that meningeal infection might develop after several months, or even years, and a remote mild head trauma might be the only identifiable risk factor in otherwise unexplained cases [4], especially those recurring over time.
2. Methods
2.1. Eligibility Criteria
The present systematic review was carried out according to the Preferred Reporting Items for Systematic Review (PRISMA) standards [5]. We used an evidence-based model for framing a PICO question model (PICO: participants, intervention, control, and outcomes).
The question posed was the following: Is there an association between TBI and post-traumatic meningitis? (P) Participants: patients suffering to or death-related to post-traumatic meningitis. (I) Interventions: evaluation of clinical status in patients diagnosed with meningitis. (C) Control: healthy patients. (O) Outcome measures: clinical parameters and inflammatory and microbiological data in patients with post-traumatic meningitis. Studies examining post-traumatic meningitis, paying particular attention to victims of traumatic brain injury, were included. Study designs comprised case reports, case series, retrospective and prospective studies, letters to the editors, and reviews. The latter were downloaded to search their reference lists similarly to other papers, but yielded no other potentially eligible papers. The search was limited to human studies.
2.2. Search Criteria and Critical Appraisal
A systematic literature search and a critical appraisal of the collected studies were conducted. An electronic search of PubMed, Science Direct Scopus, and Excerpta Medica Database (EMBASE) from the inception of these databases to 15 April 2020 was performed.
Search terms were (“post-traumatic meningitis” OR “nosocomial meningitis”) AND (“community-acquired meningitis” OR “recurrent meningitis” OR “neurological infections in intensive care unit”) in title, abstract, and keywords. The bibliographies of all located papers were examined and cross-referenced for further relevant literature.
Methodological appraisal of each study was conducted according to the PRISMA standards, including evaluation of bias. Data collection entailed study selection and data extraction. Two researchers (R.L.R., P.F.) independently examined those papers whose title or abstract appeared to be relevant and selected the ones that analyzed post-traumatic meningitis. Disagreements concerning eligibility between the researchers were resolved by consensus process. No unpublished or grey literature was searched. Data extraction was performed by one investigator (A.M.) and verified by another investigator (V.F.). This study was exempt from institutional review board approval as it did not involve human subjects. Only papers in English were included in the search.
3. Results
3.1. Search Results and Included Studies
An appraisal based on titles and abstracts as well as a hand search of reference lists were carried out. The reference lists of all located articles were reviewed to detect still unidentified literature. This search identified 321 articles, which were then screened based on their abstract to identify their relevance in respect to the following:
- the human study so we excluded animal studies,
- clinical features,
- diagnosis,
- post-mortem findings,
- management of the study so we excluded methodologically incomplete design studies and those with no explicit mention about ethical issues.
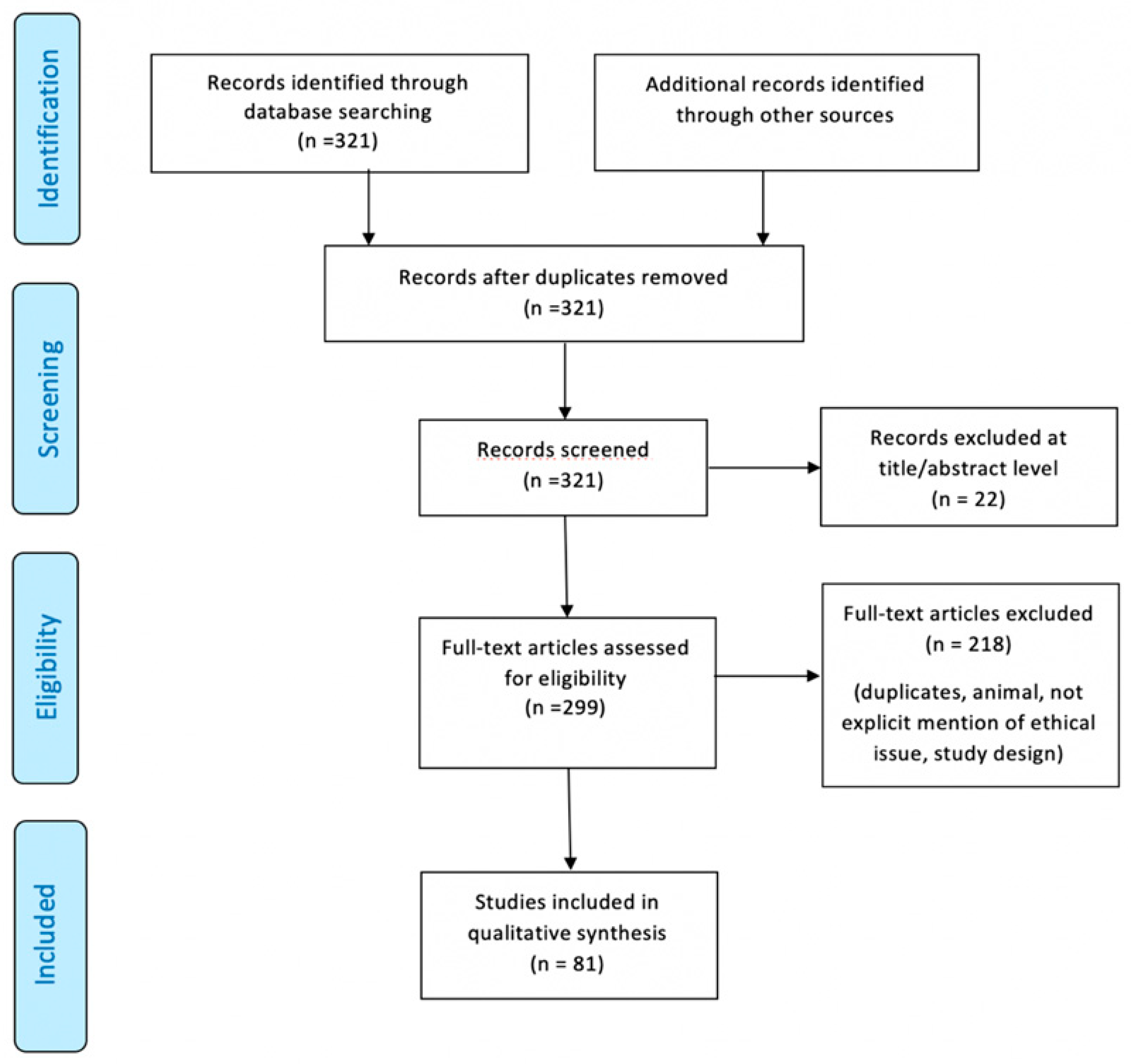
With regard to ethical issues, we discarded the papers where the obtaining of informed consent on patients was not mentioned, where the approval of the ethics committee was not found and, finally, where the permission to publish personal data was not clearly explicit. Figure 1 illustrates our search strategy.
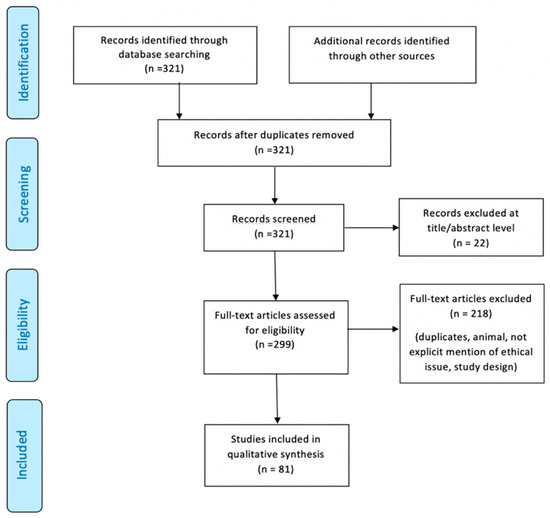
Figure 1.
Preferred Reporting Items for Systematic Review (PRISMA) flow chart—search strategy. Study designs comprised case reports, case series, retrospective and prospective studies, letters to the editors, and reviews. An appraisal based on titles and abstracts as well as a hand search of reference lists were carried out. The reference lists of all located articles were reviewed to detect still unidentified literature. A total of 81 studies fulfilled the inclusion criteria.
A total of 81 studies fulfilled the inclusion criteria (Table 1).

Table 1.
A total of 81 studies fulfilled the inclusion criteria. Details of all studies included in this systematic review.
3.2. Risk of Bias
This systematic review has a number of strengths that include the amount and breadth of the studies, which span the globe; the hand search and scan of reference lists for the identification of all relevant studies; and a flowchart that describe in detail the study selection process. It must be noted that this review includes studies that were published in a time frame of 59 years; thus, despite our efforts to fairly evaluate the existing literature, study results should be interpreted taking into account that the accuracy of the clinical procedures, where reported, has changed over the years.
4. Discussion
4.1. Epidemiology and Risk Factors
In recent years, the incidence and morbidity of meningitis have been decreasing thanks to widespread vaccination programs, timely diagnosis, and more effective treatments. Nevertheless, this condition still represents a heavy burden, in terms of both global health and expenditures, with an estimated 2.82 million cases in 2016, the highest toll being paid in the so-called “meningitis belt”, including peri-Sahelian countries of sub-Saharan Africa [1]. In high-income areas, such as the United States and Western Europe, annual incidence is about 1–3 cases/100,000 people [6]. The above-mentioned public health policies have also produced remarkable changes in the distribution and prevalence of microbial agents commonly underlying the development of meningitis. More specifically, the number of cases related to Haemophilus influenzae type b and Neisseria meningitidis (which is responsible for seasonal outbreaks, especially affecting young adults) have dramatically dropped thanks to the introduction of conjugate vaccines, so that nowadays, Streptococcus pneumoniae is by far the most common causative organism of community-acquired meningitis among immunocompetent subjects [6], particularly adults over 50 years of age and children under 2. Apart from age-specificity, well-known risk factors for pneumococcal meningitis are immunocompromised states, either congenital (mainly defects of innate immunity) or acquired, such as diabetes, alcoholism, human immunodeficiency virus (HIV), cancer, splenectomy, and immunosuppressant medications [7]. Another common cause of meningitis in immunodeficient and elderly patients is Listeria monocytogenes, which is the third most frequent pathogen in adult cases of meningitis, after S. pneumoniae and meningococcus serogroup B [8]. Along with immunological factors, anatomical defects also represent a crucial predisposing condition for intracranial infections, as they produce a breach in the complex defense systems (e.g., skull, cerebrospinal fluid (CSF) spaces, blood–brain barrier, CSF–brain barrier) aimed to guarantee central nervous system (CNS) integrity and homeostasis. TBI, mainly owing to motor vehicle accidents and falls, is the leading cause of acquired anatomical defects, with an incidence of meningitis following moderate-to-severe head trauma estimated to be around 1.4% [9]. Among adults (6.2–12.14%) with trauma-related skull fractures, 20% present with fractures of the skull base, more frequently involving the anterior cerebral fossa (ACF) (47%), followed by middle fossa (22–37%), and posterior one (0.21–3%) (Figure 2 A–D) [10].
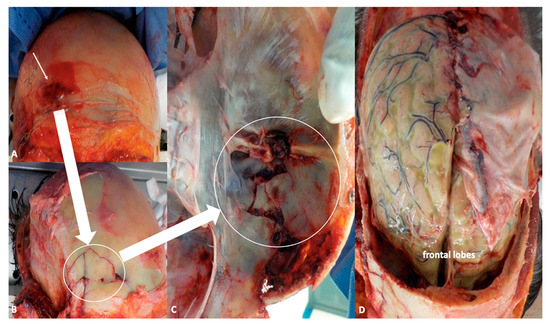
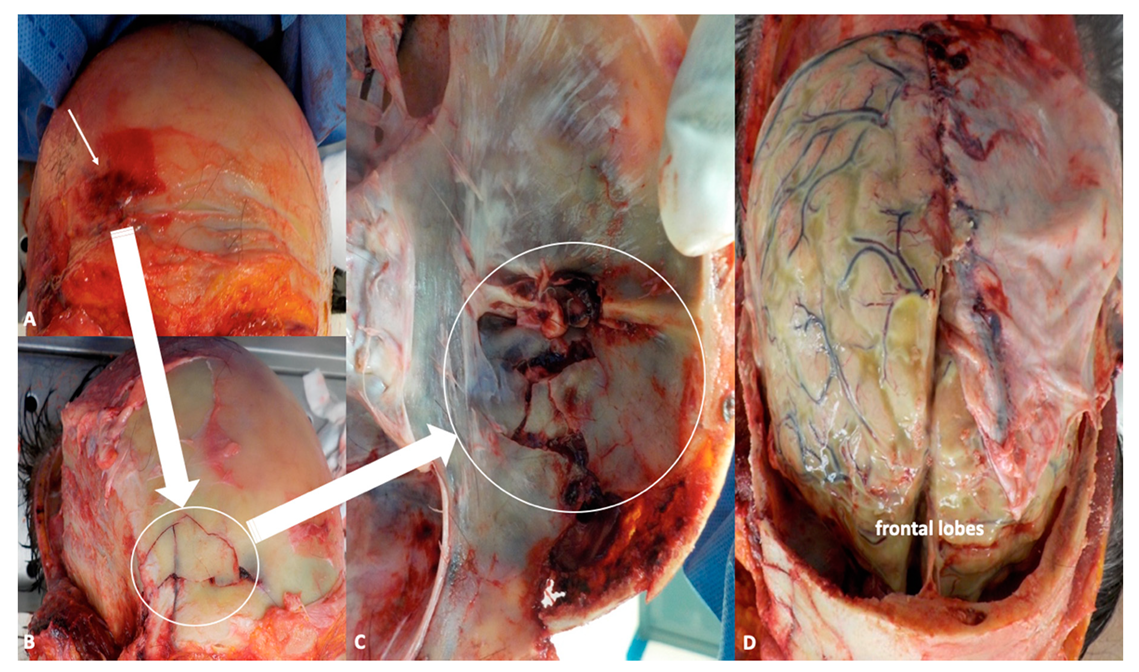
Figure 2.
(A,B) Autoptical findings: exposure of the skull by facial skin overturning. This technique allows to evaluate the periorbital region as well as zygomatic and nasal bones (white arrow indicates fractures of the frontal region). (C) Fractures of the anterior fossa are easily detectable after removal of the brain (white arrow), while inspecting the basal skull. (D) In situ inspection of the brain. The leptomeninges shows frank green color owing to the presence of purulent material stratified under the meninges.
Basilar skull fractures are associated with higher risk of CSF leak, which occurs in 12–30% of these cases (compared with 2% of all head traumas), especially if ACF structures are damaged, where both bone and dura are thinner, and the latter is more adherent to the skull [11]. CSF leak is an ominous sign, as it depends on the presence of a direct communication between subarachnoid space and external environment, and thus facilitates the penetration of microbial agents (e.g., resident flora in nasopharyngeal mucosa), which might be responsible for meningitis and other intracranial infections. CSF leak may appear as rhinorrhea or, less frequently, as otorrhea, and is more commonly observed in frontal and sphenoid sinus involvement (30%), followed by ethmoid (15–19%) and cribriform plate (7.7%) fractures. Rhinorrhea and/or otorrhea might occur immediately after the trauma or be delayed, or even present as low-volume, intermittent discharges, which makes them difficult to detect. Although CSF leaks tend to resolve spontaneously after TBI, they might persist over days, increasing the risk of developing meningitis, especially when exceeding one week [12]. In cases of traumatic CSF fistulas, the rate of meningeal infection is about 9.1% in the first week, when the patient is generally hospitalized—so that a diagnosis of “nosocomial meningitis” is to be made; this proportion decreases to 8% per month for the first six months after TBI, and then drops to 8% per year [3]. As previously stated, meningitis might actually develop as a late consequence of trauma, after several months or years, and present as a periodic phenomenon. The so-called recurrent meningitis, which differs from relapsing or recrudescent ones, is generally defined as the occurrence of at least two episodes of meningeal infection sustained by different pathogens, or by the same organism, but with an interval superior to 3 weeks after the termination of antibiotic course for the first episode [13]. Recurrent meningitis accounts for 5–6% of adult community-acquired cases, with an estimated incidence of 0.12 cases/100,000/year [14,15]. In the review by Tebruegge and Curtis, more than a half of cases of recurrent meningitis were associated with anatomical defects, 47% of which were related to remote head trauma, accounting for an overall proportion of 28% [13]. In consideration of these findings, it not surprising that S. pneumoniae is by far the most common causative in recurrent meningitides, and in post-traumatic ones overall, with a detection rate in CSF cultures up to 85% in the paper by Adriani and colleagues [15]. Such evidence might be easily explained in light of the anatomical proximity between intracranial space and nasal cavities/paranasal sinuses, whose mucosa is normally colonized by microbial flora, including S. pneumoniae. In the case of penetrating brain injuries, other pathogens, generally present on the skin, such as S. aureus, coagulase-negative staphylococci (especially S. epidermidis), and facultative and aerobic gram-negative bacilli, might be involved in the genesis of meningitis [16,17,18,19,20,21,22,23,24,25].
4.2. Pathogenesis and Pathophysiology: A Brief Outline
Meningitis is defined as inflammation of the meningeal linings, in particular arachnoid and pia mater, and the subarachnoid space. Bacterial meningitis is the result of the penetration of pathogenic microorganisms within the subarachnoid space, which generates an inflammatory cascade with dramatic consequences. Microbial agents can reach meninges and contiguous spaces via different mechanisms, the most common being hematogenous spread from a distant infectious reservoir or after mucosal/skin penetration. This route of CNS invasion implies a complex process, including sequential steps: (1) microorganism adhesion to mucosal surfaces; (2) penetration, survival, and replication in the bloodstream; and (3) breaking through the blood–brain barrier (BBB) [6,26]. The main sites of bacterial penetration (either trans-cellular or para-cellular) are likely post-capillary venules and veins, which are supposed to be more permeable than arterial vessels. Within the subarachnoid space, there is a low concentration of complement components, which hampers opsonization and phagocytosis; therefore, once penetrated, bacteria can easily survive and proliferate. When microorganisms start to die (either because of nutrient deficiency or medications), their by-products tend to accumulate in the CSF, thus contributing to the activation of the inflammatory cascade [6,26].
Apart from hematogenous dissemination, there are other less common routes of CNS invasion potentially leading to meningitis; for instance, microorganisms may spread to meninges from contiguous infected sites, as happens in the case of otitis, mastoiditis, sinusitis, endophthalmitis, and so on. Moreover, bacterial penetration into the subarachnoid space might occur directly through a breach in the skull and adjacent soft tissues; this is the case of post-traumatic and iatrogenic meningitis (the latter being caused by neurosurgical procedures). In such circumstances, bacteria that physiologically colonize naso-pharyngeal epithelium and sinus mucosa are mainly responsible for the infectious process. Conversely, in the case of penetrating injuries, microorganisms normally present on the skin are likely to be involved [27,28,29,30].
The thorough revision of the complex pathophysiological mechanisms underlying meningitis is beyond the purpose of this review. However, some key concepts will be briefly highlighted.
The first consideration is that both host-related and pathogen-related factors play a crucial role in determining the onset and the severity of the disease. On the host’s side, either acquired (e.g., diabetes, HIV, cancer, medications) or congenital features (including single nucleotide polymorphisms, as recently documented) could contribute to immunological deficits and increase the susceptibility to meningitis, especially when involving the complement system and innate immunity in general. On the other side, not all microorganisms can cause meningitis; in fact, encapsulated bacteria (such as S. pneumonia and N. meningitidis) are more resistant to opsonization and phagocytosis, which facilitates their “escape” and survival within the bloodstream and the CSF, favoring the development of meningitis. Moreover, different serotypes of the same microorganism apparently have a different pathogenic potential, probably owing to peculiar molecular patterns (e.g., surface antigens) [6]. Besides, in order to survive to host’s defenses, bacteria can spontaneously change during the infection course, becoming more virulent and resistant to therapy [31,32,33].
Another important point that should be kept in mind is that meningitis-related brain injury is the result of not only the infection per se, but also the host’s inflammatory response. Indeed, when mediators of inflammation (e.g., tumor necrosis factor-α, interleukin-1, interleukin-6) are released in the CNS in response to infection, they can induce chemotactic and adhesion molecules that, along with bacterial components, lead to the influx and/or activation of leukocytes and glial cells. Polymorphonucleocytes and macrophages then produce tissue-damaging substances, such as proteases and oxidants, and trigger several processes (e.g., vasculature changes, cytotoxic/vasogenic edema) contributing to brain damage [26,27].
4.3. Clinical Manifestations
The clinical triad classically associated with pyogenic meningitis consists of fever, nuchal rigidity (“neck stiffness”), and alteration in mental status. Other frequent manifestations are headache and photophobia, whereas a variable proportion of patients might present with focal neurological deficits owing to the involvement of cranial nerves or brain parenchyma (so-called meningo-encephalitis). Some additional clinical features might also hint at the specific etiology; for instance, petechial rash is highly suggestive of meningococcal infection. However, it is widely acknowledged that typical clinical signs/symptoms may be far less apparent in children, especially in neonates, who generally present with nonspecific manifestations such as lethargia, irritability, poor feeding, respiratory distress, and hypo/hypertonia. Moreover, in adults themselves, the historical semiological triad might not be as sensitive as commonly thought; in the Dutch Cohort Study performed on 671 adult patients with community-acquired meningitis, only 44% of the population presented fever, neck stiffness, and altered awareness at disease onset [17]. When considering headache (reported by 87% of subjects) in addition to the other classical clinical features, the percentage of patients showing at least two of them raised to 85%. Regarding the specific etiology, the classical symptoms were more common during pneumococcal rather than meningococcal infection (58% vs 27%). S. pneumoniae was actually associated with a more severe disease course and worse outcome in comparison with other causative organisms. In accordance with these findings, a more severely impaired mental status and a higher incidence of seizures have been documented in pneumococcal meningitis, along with a greater proportion of focal neurological deficits related to the development of serious complications.
Notwithstanding, the sensitivity of clinical evaluation in the diagnostic process of bacterial meningitis can be greatly influenced by factors other than the patient’s age and the specific etiology, such as the subject’s immunological state and the use of specific medications (e.g., pain-killers). Besides, meningism might be related to several other neurological diseases apart from meningeal infection, first of all, subarachnoid hemorrhage (SAH).
Some semiological maneuvers should be mentioned because of their historical value, although their diagnostic accuracy has been proven to be very limited. The most popular signs among physicians include the following: (1) Kernig sign: when the subject is lying (or sitting) with flexed hip and knee, a resistance to passive knee extension can be appreciated. (2) Brudzinski signs: “nape of the neck sign”: neck flexion elicits the flexion of the ipsilateral hip and knee; “identical contralateral reflex”: the flexion of hip and knee on one side induces an identical contralateral response; “symphyseal sign”: the pressure applied over the pubic symphysis determines bilateral hip and knee flexion and leg abduction. (3) Jolt accentuation maneuver: the rapid horizontal rotation of the head (2–3 times/second) exacerbates headache [18]. These maneuvers have poor specificity as they reflect meningeal irritation, which might be related to causes other than infectious meningitis. Moreover, recent studies have demonstrated their sensitivity to be very low as well, ranging from 2% to 20%. In in this respect, jolt accentuation shows the highest sensitivity (up to 33% in subjects with moderate CSF pleocytosis); still, its diagnostic value is rather poor, and it might be risky in patients with recent cranio-cervical trauma [19,20].
As far as clinical features are concerned, post-traumatic meningitis does not differ from community-acquired cases; however, awareness impairment is generally more severe, and the clinical picture might be clouded by the presence of other brain lesions (e.g., intracranial bleeding, cerebral edema) or concomitant medical conditions, which makes the early recognition of meningitis even more challenging. In severe TBI (defined as Glasgow Coma Scale score < 8), general anesthesia and assisted ventilation are often required for patients’ management (as well as neuroprotection), which hampers the timely evaluation of changes in mental status and vital functions. Moreover, some compounds (e.g., opioids, neuromuscular blockers) might alter pupil diameter and reactivity, or muscle tone, sometimes masquerading impending neurological complications. Finally, infections are a common occurrence in critically ill patients, the most frequent being ventilator-associated pneumonia, urinary tract, and bloodstream infections, followed by meningitis/ventriculitis [21]; in this setting, it might be difficult to attribute fever specifically to intracranial infections, or to any infection, considering the chance of central hyperthermia in severely brain injured patients.
In subjects with recent head trauma, CSF leaks should be properly investigated: patients with rhinorrhea might report a salty taste (or sweet, at times) in their mouth, and “running nose”, that is, the occurrence of watery discharges, often experienced on standing, coughing, or sneezing [11]. Rhinorrhea is generally unilateral, occurring on the same side of the skull fracture, but it might seldom be paradoxically contralateral to the fracture, when the nostril of the affected side is obstructed by either a bone fragment or meningocele, or in the case of midline lesions [10]. When not immediately apparent, rhinorrhea could be elicited by flexing the subject’s neck or leaning the patient forward, what is usually called the “reservoir sign” [10]. However, CSF leaks might be of limited volume, delayed, or intermittent; therefore, their absence does not rule out the possibility of a skull fracture.
In conclusion, although pyogenic meningitis can be suspected when patients are admitted to the emergency department, especially when predisposing factors are identified (e.g., remote/recent head trauma, immunocompromised status), it cannot be diagnosed on clinical grounds only, and requires laboratory confirmation through CSF analysis.
4.4. Diagnostic Approach
4.4.1. CSF Analysis
CSF examination is the gold standard for the diagnosis of infectious meningitis, whose etiological definition can be achieved only by CSF culture [6,8]. CSF analysis requires sample collection through lumbar puncture, a minimally invasive, easily manageable procedure. Lumbar puncture should be postponed to brain neuroimaging (CT scan) only for safety concerns, when clinical signs suggest the existence of conditions (e.g., space-occupying lesions, obstructive hydrocephalus) that might absolutely contraindicate lumbar puncture due to risk of intracranial hypertension with consequent brain herniation. This precaution is crucial in TBI patients, who might also have intracranial bleeding, skull or spine fractures with bone dislocations, or cerebral edema, and always undergo CT scan on admission. However, the need for a preliminary radiological exam must not hinder the timely introduction of antibiotic treatment, which should be empirically started even before lumbar puncture is performed, when deemed necessary. As for CSF analysis, findings typically observed in pyogenic meningitis include the following: reduced glucose level with low CSF/blood glucose ratio (<0.4); increased protein level (>2g/L); and polymorphonucleate pleocytosis, generally exceeding 1000 cells/mm3 [6]. Each of these findings is an independent predictor of bacterial meningitis, and at least one of them is detected in about 96% of patients with pyogenic meningeal infection. Nevertheless, the extent of CSF abnormalities is closely related to the subject’s age, immunological state (e.g., cancer patients have less marked CSF pleocytosis, as well as those with ongoing septic shock), causative agent, and concomitant medications. CSF culture is essential for organism identification and has a high sensitivity (ranging from 60% to 96%, depending on the specific organism), although its diagnostic accuracy is affected by antibiotic pre-treatment [34]. CSF Gram stains could play a crucial role in cases with negative cultures thanks to its high specificity, which makes it suitable for directing prompt therapeutic choices. Once again, etiological factors and antibiotic treatment could lower the diagnostic yield of this technique. Ancillary tests, such as polymerase chain reaction (PCR) on CSF, might be of help in double-negative cases, whereas latex agglutination test is of limited value [35].
4.4.2. Surrogate Serum Markers
When CSF cannot be obtained (e.g., owing to the high risk of intracranial hypertension, or for difficulties in performing the lumbar puncture related to the spine anatomy, prior back surgery, obesity, and so on), surrogate serum markers supporting the clinical suspicion of meningitis are needed. In this regard, C-reactive protein (CRP) has recently gathered considerable attention, and even more so, procalcitonin (PCT). The latter is a 116-aminoacid protein physiologically synthesized by thyroid C cells as a precursor of calcitonin, and its level raises during sepsis thanks to increased extra-thyroidal production (e.g., in adipocytes, hepatocytes, different parenchymal cells), probably induced by bacterial products (i.e., endotoxin) and pro-inflammatory cytokines (e.g., tumor necrosis factor-α, interleukin-6) [36,37]. A recent meta-analysis demonstrated its high accuracy in distinguishing between viral and bacterial etiology in cases of suspected meningitis, proving PCT to be superior to all CSF parameters (i.e., low glucose level, high protein concentration, leukocytes) [37]. Moreover, this marker has been demonstrated to rise 4 h after the onset of meningitis, peak at 6 h, and persist over 24 h, thus representing a useful tool in the early phase of the disease. However, PCT is not useful for etiological definition, nor is it specific for intracranial infections. Besides, as previously discussed, infections and sepsis are common complications in critically ill patients, like those with severe TBI hospitalized in intensive care unit (ICU); therefore, increased levels of PCT (>10 ng/L), however suggestive, cannot specifically point to meningitis. Conversely, blood cultures might be a useful tool for organism isolation when CSF samples are not available or CSF cultural tests are negative [36]. Finally, several works have also investigated the use of serum leukocytosis (common cut-off 10 × 103/μL) for the diagnosis of pyogenic meningeal involvement; so far, the bulk of literature data has proved the poor sensitivity and specificity of this parameter, whose positive predictive value is about 13–56% [38].
4.4.3. The Role of Neuroimaging in Meningitis
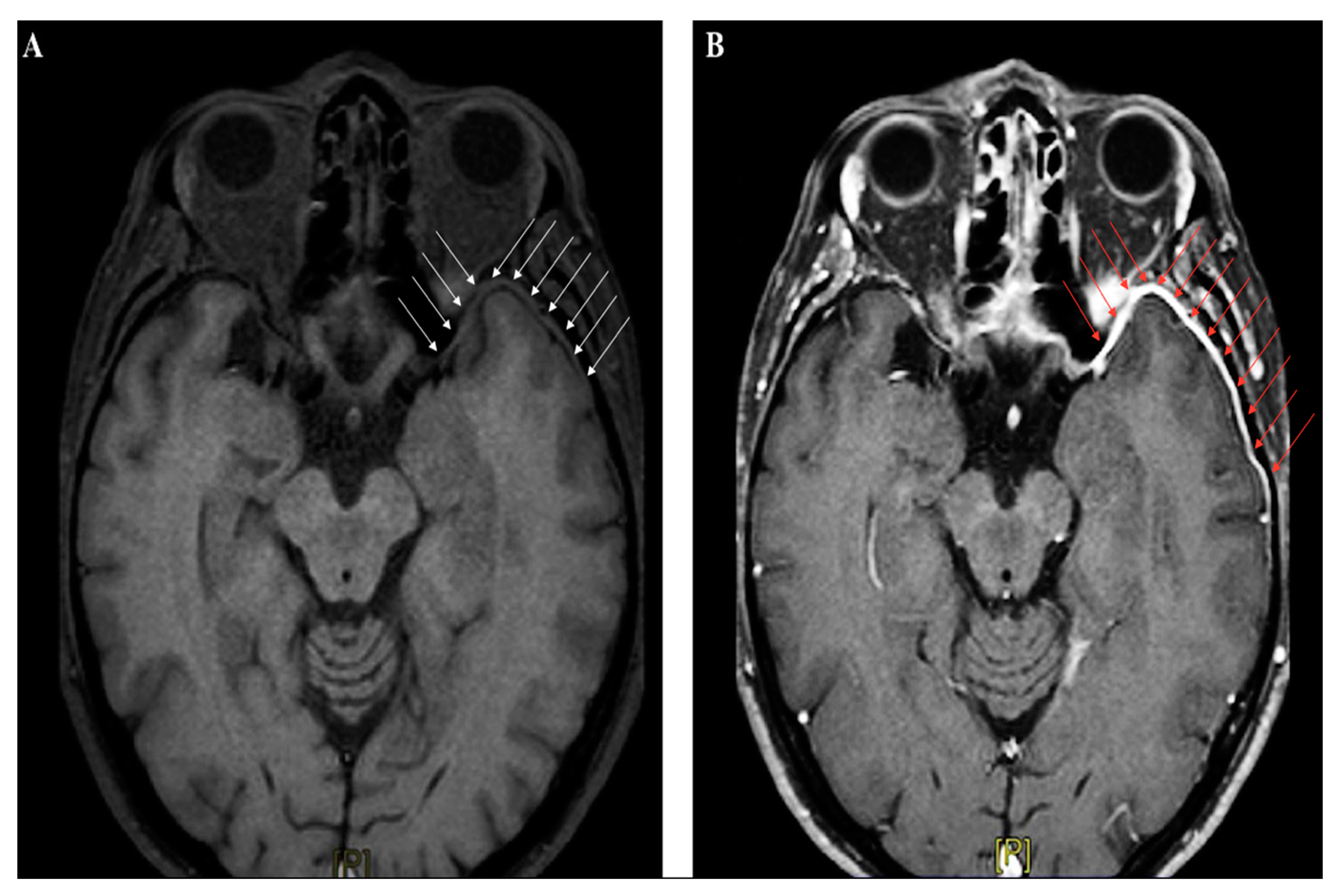
Neuroimaging studies are not crucial for meningitis diagnosis, apart from their role in identifying patients at risk for brain herniation, who should not undergo lumbar puncture. In the early phase, abnormal findings are seldom detected by CT scan; in the Dutch cohort study on community-acquired meningitis, CT was performed on admission in 71% of subjects, and was unremarkable in almost 66% of them [17]. Contrast-CT might identify meningeal enhancement in a minor proportion of cases later on in the disease course. Magnetic resonance imaging (MRI) is not immediately required in uncomplicated meningitides, although gadolinium-enhanced MRI (Gd-MRI) can clearly document the meningeal involvement (Figure 3A–B).
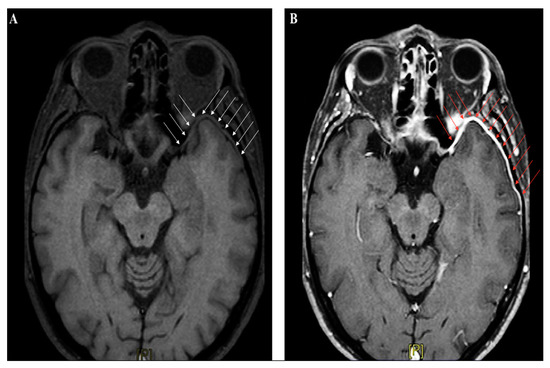
Figure 3.
Brain magnetic resonance imaging (MRI) (axial section, T1-weighted images) performed in a patient with recurrent headache and diplopia, and a history of remote head trauma; a definite thickening of the meningeal lining over the left anterior temporal lobe (white arrow panel A), with following contrast enhancement (red arrow panel B), can be clearly identified.
However, Gd-MRI is crucial for detection of harmful complications such as cerebral ischemia, sinus thrombosis, brain abscess, hydrocephalus, and cerebral edema. Therefore, it should be promptly performed in patients with new-onset focal neurological deficits and seizures, or other signs of clinical deterioration [38,39]. In subjects presenting with TBI, neuroimaging studies are mandatory to detect skull fractures, intracranial bleeding, cerebral edema, and diffuse axonal injury. Brain imaging also play a pivotal role in localizing CSF fistulas, even when no CSF leak is clinically evident (because of meningocele, herniation, bone fragments, or blood clots temporarily obstructing the dural tear) [10]. The early identification of CSF fistulas is strategic to plan therapeutic approaches and estimate the risk of developing post-traumatic meningitis. With this aim, several advanced techniques have been applied, such as high-resolution CT (HRCT), which uses 1–2 mm sections in both the coronal and axial planes to obtain detailed images of the bone structures, or MRI cisternography, a non-invasive technique where T2-weighted images with fat suppression and image reversal allow to highlight CSF and brain parenchyma, despite poor bone definition [10]. However, the current radiological gold standard for identification of the exact site of CSF leak implies the intrathecal injection of a detectable dye, such as fluoresceine (used off-label) or radiopaque contrast followed by CT scanning (so-called CT cisternography), or even (less common) a radioactive substance, used in radionuclide cisternograms [11]. Despite their good sensitivity, these techniques have serious potential complications, including aseptic meningitis due to intrathecal injections of chemical compounds.
4.4.4. Novel Diagnostic Tools
Finally, when CSF leak is suspected, a novel interesting, non-invasive approach consists of the (qualitative) identification in nasal discharges of β2-transferrin, a desialidated isoform of transferrin almost exclusively detected in CSF, with sensitivity and specificity about 99% and 97%, respectively [10,11]. The drawbacks of this assay are the time (24–48 h) needed to obtain the results and the evidence that β2-transferrin can be also found in aqueous humor and in the sera from patients with alcohol-related cirrhosis. A less expensive and much quicker approach is the quantitative measure of the levels of β-trace protein, a protein synthesized by meninges and choroid plexus, which has 100% sensitivity in the case of active rhinorrhea, but unfortunately is also increased in the serum of subjects with kidney failure [11].
4.5. Therapeutic Management
4.5.1. Antibiotic and Steroid Treatment in Post-Traumatic Meningitis
Antimicrobial treatment is the cornerstone of the therapeutic management of all pyogenic meningitides; antibiotics should be started as early as possible, even before the isolation of the causative microorganism through CSF culture (which takes 24–48 h), in order to minimize the risk of death and permanent sequelae. Indeed, therapeutic delay (mainly related to brain imaging) is strongly associated with poor outcome [40,41,42]. Before the specific pathogen is identified, empirical antimicrobial treatment should be decided based on the patient’s age, known risk factors (e.g., immunodeficiency), and local epidemiological data about pneumococcal resistance. As already stated, S. pneumoniae is the most common causative microorganism in adult subjects with both community-acquired and post-traumatic meningitis; therefore, penicillin and third-generation cephalosporins represent the main compounds used in empirical therapy. However, pneumococcal reduced susceptibility to third-generation cephalosporins has become an increasingly worrying phenomenon, so that, in regions with expected high resistance rates, either vancomycin or rifampicin should be added [8]. Moreover, considering Listeria resistance to cephalosporins, all patients above the age of 60 should receive amoxicillin or ampicillin, as well as immunocompromised subjects. After the identification of the causative pathogen, the patient should be switched to a targeted treatment (see specific recommendations on this topic). Antibiotics could be administered as either continuous infusion or repeated boli, without proven differences in patients’ outcome. Conversely, therapy duration is still a matter of debate, but in culture-negative patients, the antibiotic course should last at least two weeks [8]. Corticosteroids have been lately evaluated as adjunctive therapy for acute bacterial meningitis, with the aim to reduce neuronal damage due to infection-related inflammatory mechanisms. A recent Cochrane review, including 25 studies on a total of 4121 pediatric and adult subjects, demonstrated that, exclusively in high-income countries, early steroid treatment is effective in preventing hearing loss and short-term neurological sequelae [43,44]. No effect on mortality was observed; however, subgroup analysis revealed a reduction in mortality rates among patients with S. pneumoniae. On the basis of the findings of the most relevant included trials, corticosteroid treatment, started before or within 4 h after the first antibiotic dose, is currently recommended in cases of S. pneumoniae and H. influenzae meningitis [8,45]. At present, dexamethasone is the compound of choice, and should be administered at low dose (10 mg) every 6 h for a duration of 4 days. However, caution is warranted in the case of septic shock and recent cranio-cerebral trauma. As for adjunctive osmotic therapy, glycerol is the only agent that has been evaluated in acute bacterial meningitis; similar to corticosteroids, it was demonstrated to be potentially effective in reducing neurological sequelae, but not mortality, according to the cumulative findings of five trails gathering 1451 individuals [46,47,48].
4.5.2. Antibiotic Prophylaxis after TBI: A Matter of Debate
Another controversial issue in the therapeutic management of patients with meningitis is the need for antibiotic prophylaxis in subjects with head trauma, especially those presenting with severe TBI. Indeed, despite the relatively low incidence of meningeal involvement among patients with recent trauma, when well-known risk factors for meningitis (such as basilar skull fractures or persistent CSF leaks) can be identified, chemoprophylaxis seems a prudent choice, and is often used in clinical practice. Nevertheless, the potential adverse events related to antibiotics, and the risk of increased microbial resistance, require careful considerations. A recent Cochrane meta-analysis has attempted to cast light on such debated topic; in fact, the available evidence did not allow determining the actual utility of antibiotic prophylaxis in patients with basilar skull fractures, so that prophylactic treatment is not currently indicated [48,49,50,51]. More specifically, the meta-analysis included five randomized controlled trials (RCTs) performed on a total of 208 subjects; no differences—in terms of meningitis rate, meningitis-related mortality, and all cause-mortality—were found between patients receiving any antibiotics and those receiving placebo or no treatment at all, regardless of the presence of CSF leak (when specified). These findings were also confirmed after considering data from non-randomized trials for analysis. Another interesting question is whether subjects with post-traumatic meningitis might benefit from pneumococcal vaccination, considering the risk of recurrence. Despite the lack of RCTs properly investigating vaccination utility in recurrence prevention, the European Society for Clinical Microbiology and Infectious Diseases currently recommends vaccination in all patients with history of pneumococcal meningitis [8,52].
4.5.3. The Management of CSF Leaks
Finally, in subjects with recent TBI, CSF leaks require careful monitoring and particular consideration. Rhinorrhea and otorrhea generally tend to resolve spontaneously over a few days, and a conservative approach is thus preferred. The patient should lie in bed with 30° head elevation and should be advised against coughing, sneezing, nose blowing, performing Valsalva maneuver, and so on [53,54,55,56,57,58]. Blood pressure should be strictly controlled in order to avoid further leak and allow the dural tear to heal. When CSF leak persists beyond one week, a surgical repair of the anatomical breach could be attempted, using different approaches (e.g., transcranial, extra-cranial, trans-nasal, endoscopic endonasal, and so on) whose discussion is beyond the purpose of this paper.
4.6. Outcome and Neurological Complications
In spite of recent improvements in terms of diagnostic accuracy and therapeutic management, bacterial meningitis still represents a serious infectious disease worldwide, with high mortality and morbidity especially in low-income countries, where the impact on quality of life and health economy is not negligible. The Global Burden of Diseases, Injuries, and Risk Factors (GBD) 2016 study showed a decrease in overall mortality rates by 21% from 1990 to 2016 [1]. In 1990, the main cause of meningitis deaths was N. meningitidis, but thanks to the introduction of vaccine programs and chemoprophylaxis, the mortality related to meningococcal infection has dropped. In the already mentioned Dutch cohort study on community-acquired meningitis in adult subjects, the overall mortality rate was about 20%, and it raised to 30% when considering pneumococcal infections (compared with 7% of meningococcal ones) [17]. Indeed, it is widely acknowledged that S. pneumoniae is associated with more severe disease course, poorer outcome, and more frequent long-term complications. No specific data about fatalities in post-traumatic meningitis are currently available, which can be easily explained considering its low incidence and difficult diagnosis, and the great impact of concomitant TBI-related lesions on outcome. Interestingly, recurrent meningitis has a better prognosis than other forms of meningeal infections, probably because affected patients learn to recognize early symptoms and seek medical attention [13].
A remarkable proportion of subjects suffering from meningitis struggle with neurological sequelae; these are generally related to the development of serious complications during the disease course, which might lead to new-onset focal neurological deficits, seizures, and sudden worsening of the patient’s mental status. One of the main complications observed in meningitis is cerebral ischemia, documented in up to 25% of adult patients; cerebral infarction might be caused by either arterial or venous sinus thrombosis, which likely depends on abnormal coagulation mechanisms, vasculitis, or vasospasm induced by the host’s inflammatory response [59,60,61,62]. Nevertheless, heart ultrasound should be performed in order to rule out cardio-embolism as a possible cause of cerebral ischemia.
Meningeal infection could also extend, involving subdural space and cerebral parenchyma, leading to difficult-to-treat conditions such as subdural empyema and brain abscess, which sometimes require surgical treatment. Moreover, hydrocephalus might also develop as a consequence of meningitis; in such cases, it is often non-resorptive (communicating), related to impaired CSF re-absorption by subarachnoid granulations owing to exceeding protein and cell content in CSF, and could spontaneously resolve [63,64,65,66,67,68]. However, obstructive hydrocephalus might also occur, especially in children, contributing to intracranial hypertension. This is an ominous condition, often following brain edema, which might lead to brain herniation and death. It also represents an absolute contraindication to lumbar puncture, hampering the diagnosis of meningitis. Subjects with severe TBI are even more at risk of intracranial hypertension because of possible concomitant lesions such as intracranial bleeding and diffuse axonal injury; therefore, invasive intracranial pressure (ICP) monitoring might be indicated in ICU patients.
Seizures might occur during the acute phase of meningitis (reportedly, in 9–34% of subjects), and require emergency treatment to avoid cardio-respiratory complications and further brain injury. However, they might also present later on, and mark the onset of chronic epilepsy attributed to remote meningitis (and related brain lesions). Anti-epileptic prophylaxis appears effective only in preventing early seizures (i.e., those occurring during the first week), whereas it does not influence the development of late seizures and epilepsy; however, RCTs dealing with this issue are lacking [8].
Another common early complication in patients surviving meningitis is sensorineural hearing impairment (reported by 22% of adults), which is thought to depend on direct spreading of bacteria and pro-inflammatory molecules through sub-arachnoid space to cochlea, with consequent CSF–labyrinth barrier break and nerve damage [69,70,71,72,73,74,75,76,77]. Apart from the recent introduction of dexamethasone as adjunctive therapy, which seems beneficial on hearing impairment, an early careful hearing evaluation is warranted, in order to detect the problem and prevent cochlear ossification, which could jeopardize the utility of cochlear implants.
Finally, cognitive deficits have been equally observed in patients surviving pneumococcal and meningococcal infections, with rates up to 30%. The early recognition of cognitive impairment is particularly relevant for children, who might benefit from educational support.
Recently, at molecular level, new diagnostic and therapeutic approaches have been proposed. Rapidly after TBI, it provokes the activation of the endothelium and a neuroinflammatory response, as demonstrated by the recruitment and up-regulation of cytokines, chemokines, neutrophils, and other pro-inflammatory mediators [78,79,80]. Neuropeptides such as calcitonin gene-related peptide (CGRP), neurokinin A (NKA) and B (NKB), and substance P (SP) are central to the development of neurogenic inflammation [81,82,83]. Looking for specific biomarkers, SP is the most potent initiator of neurogenic inflammation, with CGRP is able to further potentiate the effects of SP. The mechanism of the release of interleukin (IL)-1β, tumor necrosis factor (TNF), transforming growth factor beta (TGFβ), and monocyte chemoattractant protein-1 (MCP-1) is linked to the innate resident immune cells that are subjected to the activation of albumin, entering the brain through transcytosis, which also causes the release of matrix metalloproteinase (MMP) [80,84,85]. The inhibition of MMPs and A disintegrin and metalloproteinases (ADAMs), central regulators and mediators, appears to be a promising therapeutic intervention to prevent the development of neuronal damage during neuroinflammation [86,87]. Ubiquitin C-terminal hydrolaseL1 (UCHL1) represents an important TBI biomarker to support therapeutic efficacy of drugs [88]. Neurofilaments (NFs) are fundamental players in structural support and regulating axon diameter. The heavy neurofilament (pNF-H) subunit has been claimed as sensitive marker of axonal injury following TBI [89]. Neuron specific enolase (NSE) is a glycolytic enzyme released into the extracellular space under pathological conditions during cell destruction. Levels are high in the CSF, but the serum concentration depends on the state of the BBB [90,91]. In pediatric TBI, NSE has been correlated with the Glasgow Outcome Score (GOS) [92]. The hypothesis is about a protective role against blood–brain barrier (BBB) damage, inhibiting neuronal apoptosis and promoting angiogenesis [93,94].
4.7. Forensic Pathology Approach in Cases of Post-Traumatic Meningitis-Related Death
In the evaluation of liability features in the case of decease following post-traumatic meningitis, there are two main forensic pathology issues: the identification of meningitis as cause of decease, and the need for establishing the correlation between meningitis and the traumatic event. Bacterial meningitis death is rarely attributed to the actual event that caused death. Fatal complications from primary infection, meningitis, present many differences in the complications that cause death, so that determining the clinical cause of death is essential for evaluating causal correlation and new therapeutic strategies [95].
A correct methodological approach plays a fundamental role within the forensic pathology evaluation in the case of post-traumatic meningitis-related death.
These procedural criteria should include the following steps:
- -
- Complete autoptic examination;
- -
- Liquor sampling and microbiological investigations;
- -
- Brain in toto removal and formalin embedding;
- -
- Sampling of the intracranial structures;
- -
- Histological and immunohistochemical specimen’s microscopic evaluation.
4.7.1. Autopsy
The consolidated forensic pathology protocols state that, even in cases of post-traumatic meningitis, the execution of the autoptic examination cannot be separated from a preliminary and scrupulous external examination of the corpse. Special attention should be paid regarding the evaluation of both direct and indirect traumatism signs, especially referring to the cranial region. Apart from bruises, lacerated wounds, or skin abrasions assessment, the presence of otorrhea or rhinorrhoea should be searched, as those events are associated to a facilitate liquor penetration and contamination from pathogen microorganism, with an incidence as great as 20% [96].
In light of the necessity to evaluate traumatic lesions that occurred within the facial region, anterior scalp flap and facial skin overturning should be exercised, until the exposure of nasal bones. This allows to directly evaluate the periorbital region as well as zygomatic and nasal bones. Then, skull bone is opened, allowing to inspect the underlying meningeal structures, which are of special interest in the infectious disease investigated, before incision and removal of the dura matter.
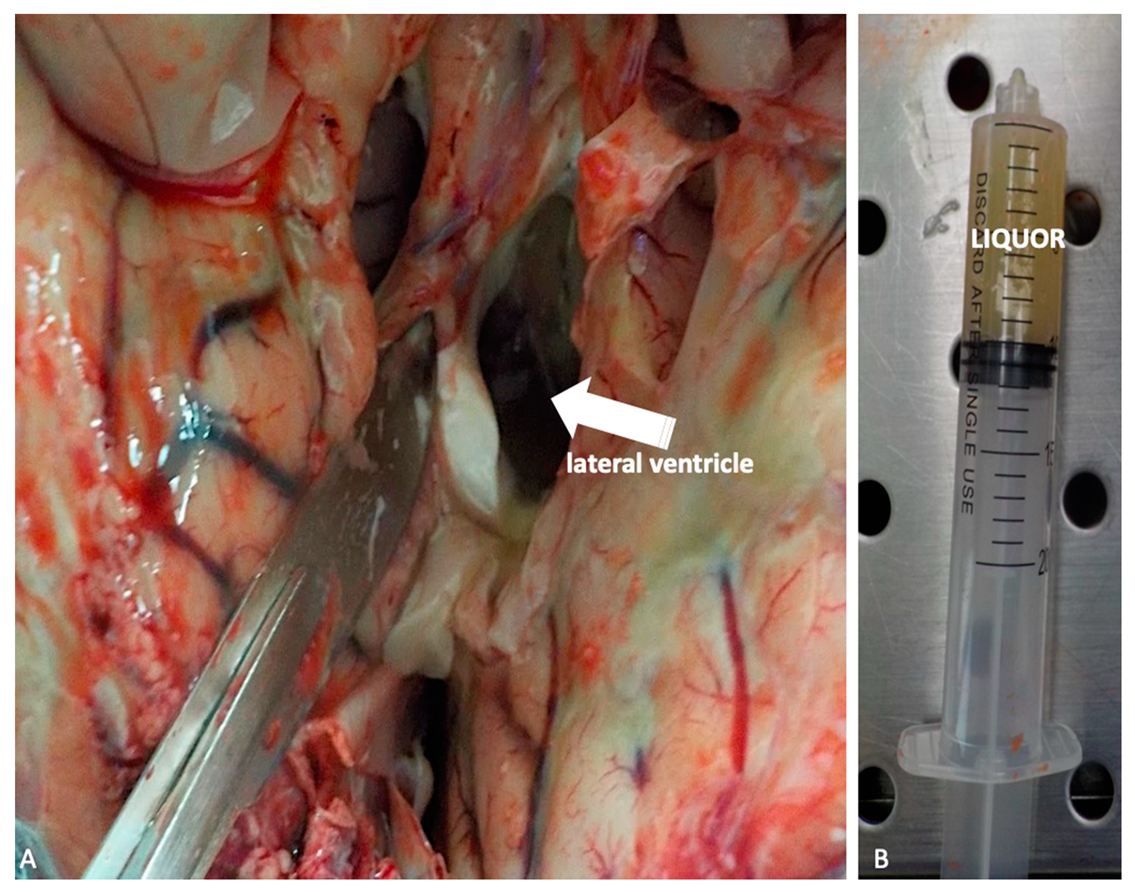
At this point, preliminary to the brain in toto removal, liquor should be collected in order to permit microbiological analysis. This is obtained by lateral ventriculi in situ incision, making two semicircular cuts laterally to cingulated gyrus (Figure 4A–B).
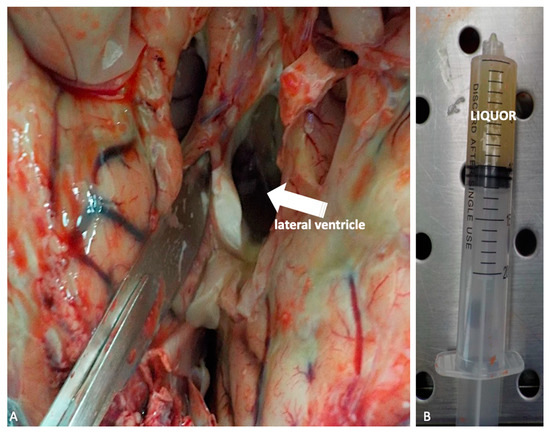
Figure 4.
(A,B) Liquor sampling by lateral ventriculi in situ (white arrow) incision intended for microbiological analysis.
Hence, the brain may be removed and inspected in order to evaluate the presence of haemorrhagic lesion or hematomas, which should be adequately described. At the end, a careful inspection of the skull base bone should be carried out because fractures in this area represent the preferred site of entrance to the endocranial cavity.
4.7.2. Tissues’ Sampling and Histological Examination
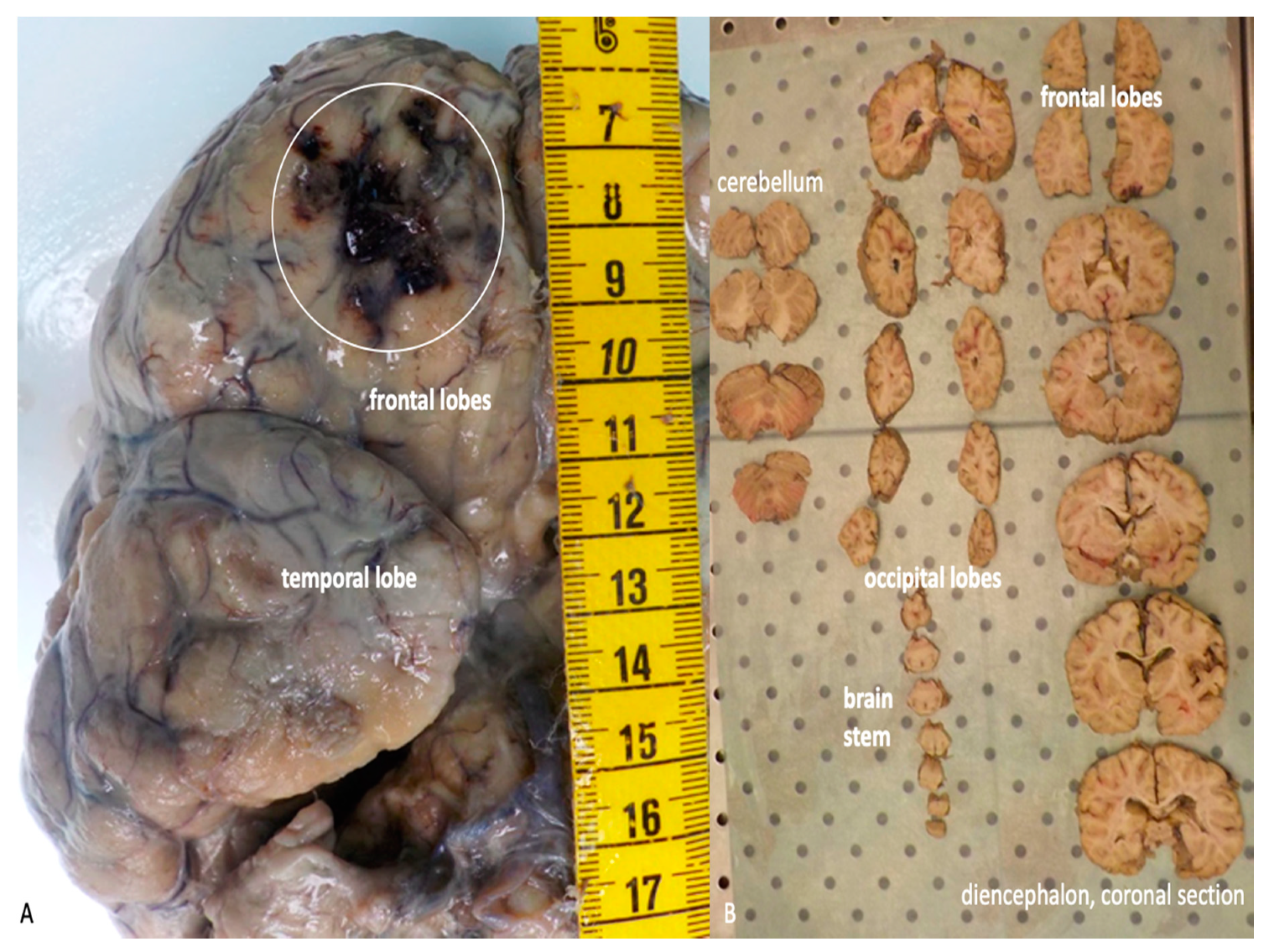
The brain, which has been previously removed during the autopsy, must be embedded in formalin and afterwards re-examined before sampling. The macroscopic exam of the structure must be conducted after sectioning using different typology of cuts, depending on the kind of lesivity detected (Figure 5A–B).
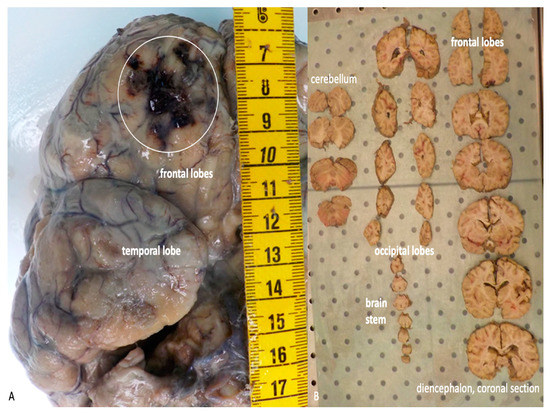
Figure 5.
(A) Macroscopic examination of the brain after formalin embedding. A traumatic contusion area at the level of the frontal lobe is evident (white circle). (B) Serial coronal sections of the brain.
Standard sampling is carried out with the addiction of sampling within the previously described injured areas. It follows the microscopic analysis of the samples where, at the hematoxylin-eosin staining, immunohistochemical staining can be associated in order to obtain a correct dating of the event. Then, microbiological exams on liquor permit to complete the diagnosis of the infectious process, whether this was not made when the patient was still alive.
4.7.3. Forensic Pathology Assessment
Regarding the assessment of a causal correlation between the traumatic event and the meningeal infection, this may result to be extremely complex. In fact, as described in the scientific literature, the time-lapse between trauma and clinical signs of infectious disease result can be extremely variable, from a minimum of a few hours to a maximum time of several years [96,97,98,99].
Concerning dating of both the traumatic event and the infective disease, this can be integrated with the execution of immunohistochemical investigations aimed to detect specific molecular markers. While evaluating brain injury several proteins such as Aquaporin4 (AQP4), CD58, CD68, and antibodies anti-glial fibrillary acid protein (GFAP) should be researched. Previous studies identified that these molecular markers expression show a temporal correlation with the event in the case of traumatic brain injury [96] (Table 2).

Table 2.
Semi-quantitative evaluation of immunohistochemical reaction to specific markers in brain samples with correlate timing.
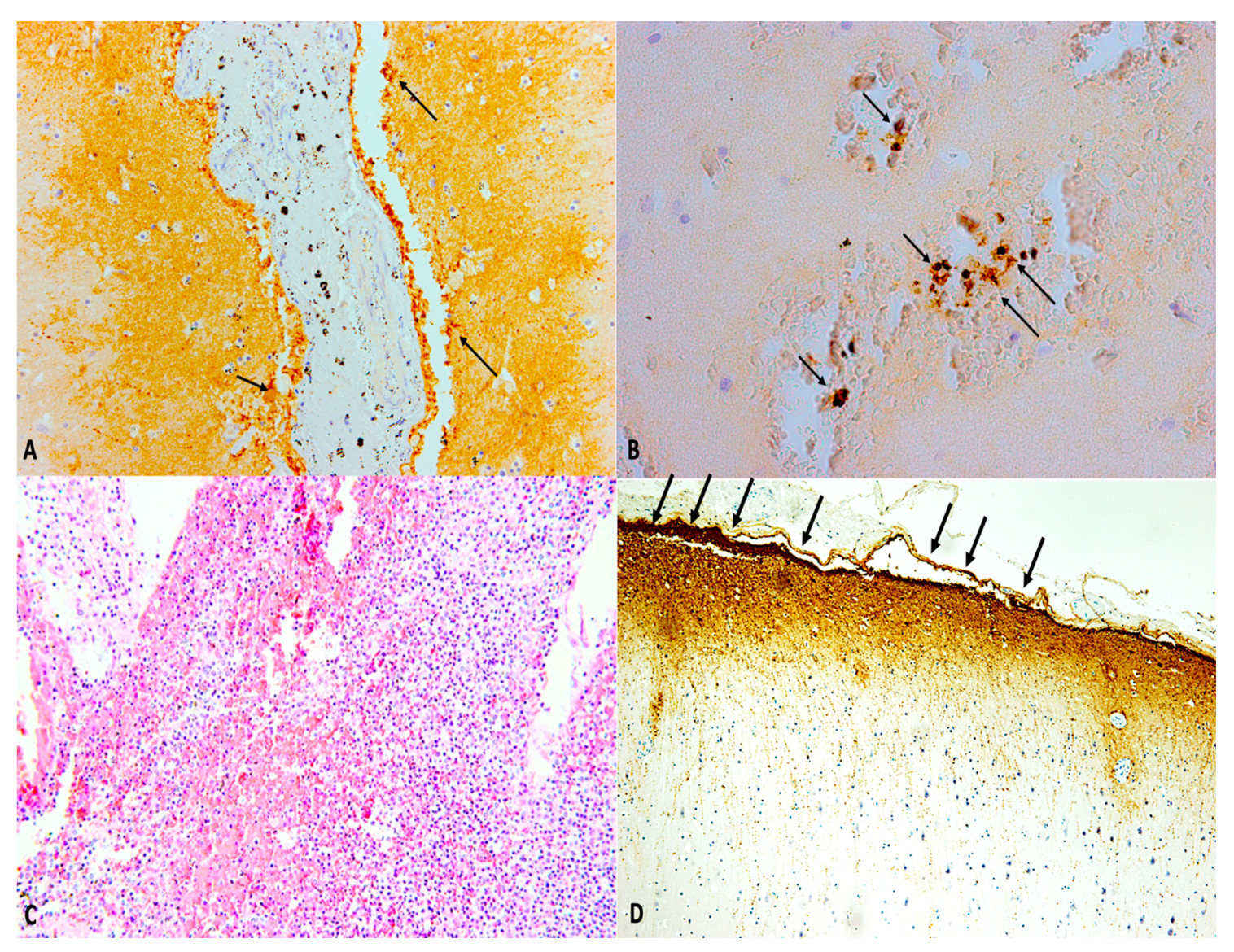
It is also possible to perform immunohistochemical studies for the post-mortem diagnosis of sepsis related to meningitis [97,98]. For the pathologist, the historical immunohistochemical markers used (β-APP, GFAP) will continue to play an important role in the diagnostic evaluation process; the best understanding of the molecular mechanisms involved in the pathogenesis of the resulting damage to a TBI, however, as well as the understanding of oxidative stress leading to apoptosis, will assume greater importance, as the potential to allow for a more precise diagnosis in time compared with classic markers (Figure 6).
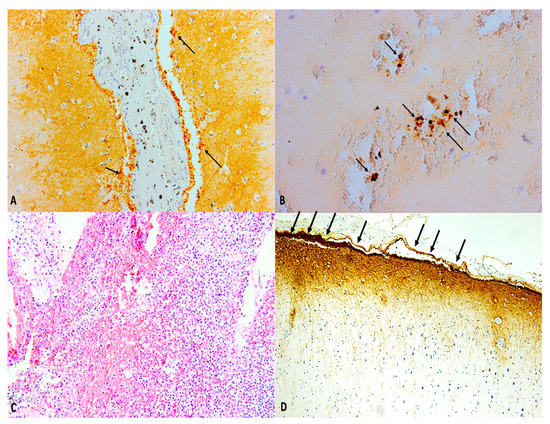
Figure 6.
(A,B) Immunohistochemistry of both brain and meninges allows dating of the traumatic event post traumatic brain injury. (A) Aquaporin-4 (AQP4) and (B) hypoxia induced factor-1α (HIF-1α) immunopositivity (black arrows) in post-traumatic meningitis after traumatic brain injury (30-day survival) (×40 and ×100, respectively). (C) Post-traumatic meningitis: histological staining of the brain and meningeal tissues showing strong inflammatory response (hematoxylin and eosin (H&E), ×60). (D) Glial fibrillary acid protein (GFAP) showed its highest expression in post-traumatic meningitis after traumatic brain injury, a definite thickening of the meningeal lining (black arrows) is clearly observable (30-day survival) (×40).
5. Conclusions
Post-traumatic meningitis represents a high mortality disease. Proper survival of the clinical course of the brain traumatic injury today still represents a great challenge for the clinicians, with the considerable implications that proper dating takes in assessing the clinical case. Diagnosis, which is often made post-mortem, may be difficult either because clinical signs are nonspecific and blurred or because of the lack of pathognomonic laboratory markers. Moreover, these markers increase with a rather long latency, thus not allowing a prompt diagnosis, which could improve patients’ outcome.
Among all the detectable clinical signs, the appearance of cranial CSF leakage (manifesting as rhinorrhea or otorrhea) should always arouse suspicion of meningitis. In fact, even though CSF leaks tend to resolve spontaneously after TBI, they might persist over days, increasing the risk of developing meningitis, especially when exceeding one week.
On one hand, microbiological exams on CSF, which represent the gold standard for the diagnosis, require days to get reliable results. For this purpose, CRP and PCT have been evaluated as early meningitis markers, being sensitive, but not specific enough. On the other hand, radiological exams, especially CT of the brain, could represent an alternative for early diagnosis. Indeed, CT can detect those alterations related to trauma, but is not specific in assessing the infectious disease.
Difficulty in the use of inflammatory markers such as immunohistochemical markers of TBI in early stage is the result of the overlap of secondary changes after a traumatic event (es. hypoxia, edema) that can lead to difficulty with errors in estimating the survival time [99]. Research to identify the miRNA expression profile secreted by astrocytes in response to acute neuroinflammatory stress has been performed recently [100]. Five miRNAs released by astrocytes under IL-1β-stimulated acute neuroinflammatory stress have been identified and extensively characterized [96]. These miRNAs may serve as potential biomarkers of CNS inflammation [101,102,103,104]. An increased expression of miR-21 after traumatic brain injury (TBI) has been described. Data indicate that miR-21, miR-92, and miR-16 have a high predictive power in discriminating trauma brain cases from controls and could represent promising biomarkers as strong predictor of survival, and a useful tool for postmortem diagnosis of traumatic brain injury [104]. More recently, miR-124-3p, miR-219a-5p, miR-9-5p, miR-9-3p, miR-137, and miR-128-3p exhibited dramatically greater brain specificity as blood biomarkers of TBI [105].
Author Contributions
R.L.R. and A.M. (Aniello Maiese). conceived the study; A.M. (Alessandra Morano). and C.D.B. performed the study; V.F. (Vittorio Fineschi). and P.F. designed the study and analyzed the data; N.D.F., A.D.M., and V.F. (Vittorio Fineschi) wrote the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors want to thank Ilaria De Casamassimi for her daily support in autoptic activity.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| PRISMA | Preferred Reporting Items For Systematic Reviews And Meta-Analyses |
| PICO | Participants, Intervention, Control, and Outcomes |
| CSF | Cerebrospinal Fluid |
| MDPI | Multidisciplinary Digital Publishing Institute |
| CT | Computed Tomography |
| DOAJ | Directory Of Open Access Journals |
| TLA | Three Letter Acronym |
| LD | Linear Dichroism |
| TBI | Traumatic Brain Injury |
| EMBASE | Excerpta Medica Database |
| HIV | Human Immunodeficiency Virus |
| CNS | Central Nervous System |
| ACF | Anterior Cerebral Fossa |
| BBB | Blood–Brain Barrier |
| SAH | Subarachnoid Hemorrhage |
| PCR | Polymerase Chain Reaction |
| CRP | C-Reactive Protein |
| PCT | Procalcitonin |
| ICU | Intensive Care Unit |
| MRI | Magnetic Resonance Imaging |
| Gd | Gadolium |
| HRCT | High-Resolution Computed Tomography |
| RCTs | Randomized Controlled Trials |
| GBD | Global Burden of Disease |
| ICP | Invasive Intracranial Pressure |
| AQP4 | Aquaporin4 |
| HIF-1α | Hypoxia Induced-Factor 1α |
| CD | Custer Differentiation |
| GFAP | Glial Fibrillary Acid Protein |
| IBA-1 | Ionized Calcium Binding Adapter Molecule 1 |
| β-APP | Beta-Amyloid Precursor Protein |
| H&E | Hematoxylin and Eosin |
| TNF | Tumor necrosis factor |
| TGFβ | Transforming growth factor beta |
| MCP-1 | Monocyte chemoattractant protein-1 |
References
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Aboyans, V. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Yelehe-Okouma, M.; Czmil-Garon, J.; Pape, E.; Petitpain, N.; Gillet, P. Drug-induced aseptic meningitis: A mini-review. Fundam. Clin. Pharmacol. 2018, 32, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Eljamel, M.S.; Foy, P.M. Acute traumatic CSF fistulae: The risk of intracranial infection. Br. J. Neurosurg. 1990, 4, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Matschke, J.; Tsokos, M. Post-traumatic meningitis: Histomorphological findings, postmortem microbiology and forensic implications. Forensic. Sci. Int. 2001, 115, 199–205. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 62, e1–e34. [Google Scholar]
- Van de Beek, D.; de Gans, J.; Tunkel, A.R.; Wijdicks, E.F. Community-acquired bacterial meningitis in adults. N. Engl. J. Med. 2006, 354, 44–53. [Google Scholar] [CrossRef]
- Adriani, K.S.; Brouwer, M.C.; Van de Beek, D. Risk factors for community-acquired bacterial meningitis in adults. Neth. J. Med. 2015, 73, 53–60. [Google Scholar]
- Van de Beek, D.; Cabellos, C.; Dzupova, O.; Esposito, S.; Klein, M.; Kloek, A.T.; Pfister, H.W. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis. Clin. Microbiol. Infect. 2016, 22, S37–S62. [Google Scholar] [CrossRef]
- Van de Beek, D.; Drake, J.M.; Tunkel, A.R. Nosocomial bacterial meningitis. N. Engl. J. Med. 2010, 362, 146–154. [Google Scholar] [CrossRef]
- Phang, S.Y.; Whitehouse, K.; Lee, L.; Khalil, H.; McArdle, P.; Whitfield, P.C. Management of CSF leak in base of skull fractures in adults. Br. J. Neurosurg. 2016, 30, 596–604. [Google Scholar] [CrossRef]
- Prosser, J.D.; Vender, J.R.; Solares, C.A. Traumatic cerebrospinal fluid leaks. Otolaryngol. Clin. North. Am. 2011, 44, 857–873. [Google Scholar] [CrossRef]
- Sonig, A.; Thakur, J.D.; Chittiboina, P.; Khan, I.S.; Nanda, A. Is posttraumatic cerebrospinal fluid fistula a predictor of posttraumatic meningitis? A US Nationwide Inpatient Sample database study. Neurosurg. Focus 2012, 32, E4. [Google Scholar] [CrossRef]
- Tebruegge, M.; Curtis, N. Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitis. Clin. Microbial. Rev. 2008, 21, 519–537. [Google Scholar] [CrossRef]
- Durand, M.L.; Calderwood, S.B.; Weber, D.J.; Miller, S.I.; Southwick, F.S.; Caviness Jr, V.S.; Swartz, M.N. Acute Bacterial Meningitis in Adults--A Review of 493 Episodes. N. Engl. J. Med. 1993, 328, 21–28. [Google Scholar] [CrossRef]
- Adriani, K.S.; Van de Beek, D.; Brouwer, M.C.; Spanjaard, L.; de Gans, J. Community-acquired recurrent bacterial meningitis in adults. Clin. Infect. Dis. 2007, 45, e46–e51. [Google Scholar] [CrossRef]
- Heckenberg, S.G.; Brouwer, M.C.; van de Beek, D. Bacterial meningitis. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2014; Volume 121, pp. 1361–1375. [Google Scholar]
- Sağlam, M.; Zer, Y.; Balci, I. Causative agents of bacterial meningitis. Afr. J. Microbiol. Res. 2013, 7, 2221–2227. [Google Scholar]
- Hernandez, J.L.; Calvo, J.; Sota, R.; Agüero, J.; Garcia-Palomo, J.; Farinas, M. Clinical and microbiological characteristics of 28 patients with Staphylococcus schleiferi infection. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 153–158. [Google Scholar] [CrossRef]
- Chang, W.N.; Lu, C.H.; Huang, C.R.; Chuang, Y.C.; Tsai, N.W.; Chen, S.F.; Chang, C.C.; Wang, H.C.; Chien, C.C.; Wu, J.J. Epidemiology of Adult Staphylococcal Meningitis in Southern Taiwan: A Coaghlase-Negative Staphylococcal Infection. Jpn. J. Infect. Dis. 2007, 60, 262–266. [Google Scholar]
- Garg, R.K.; Malhotra, H.S.; Jain, M.; Kumar, N.; Lachuryia, G.; Mahajan, L. Brainstem infarct as a rare complication of coagulase-negative staphylococcus meningitis. Neurol. India. 2017, 65, 621. [Google Scholar] [CrossRef]
- Oud, L. Community-acquired meningitis due to Staphylococcus capitis in the absence of neurologic trauma, surgery, or implants. Heart Lung. 2011, 40, 467–471. [Google Scholar] [CrossRef]
- Lin, W.-S.; Kao, H.W.; Cheng, C.-A. Panspinal epidural abscess concomitant with meningitis. Am. J. Emerg. Med. 2013, 31, P1155.e5–P1155.e6. [Google Scholar] [CrossRef]
- Dumas, G.; Schmerber, S.; Atallah, I.; Brion, J.; Righini, C.A. Subacute tuberculous otitis media complicated by petrositis and meningitis. Rev. Laryngol. Otol. Rhinol. (Bord) 2012, 133, 221–224. [Google Scholar] [PubMed]
- Karagol, B.S.; Zencıroglu, A.; Kundak, A.; Okumus, N.; Aydin, M.; Uner, C.J.N. A linear fracture and meningitis associated with non-infected cephalohematoma in a neonate. Neuropediatrics 2010, 41, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Hedberg, A.; Hårdemark, H.G.; Olsson-Liljequist, B.; Sjölin, J. Penetration of fusidic acid and rifampicin into cerebrospinal fluid in low-grade inflammatory meningitis caused by Staphylococcus epidermidis. Clin. Microbiol. Infect. 2004, 10, 765–768. [Google Scholar] [CrossRef][Green Version]
- Van de Beek, D.; De Gans, J.; Spanjaard, L.; Weisfelt, M.; Reitsma, J.B.; Vermeulen, M. Clinical features and prognostic factors in adults with bacterial meningitis. N. Engl. J. Med. 2004, 351, 1849–1859. [Google Scholar] [CrossRef] [PubMed]
- Forgie, S.E. The history and current relevance of the eponymous signs of meningitis. Pediatr. Infect. Dis. J. 2016, 35, 749–751. [Google Scholar] [CrossRef] [PubMed]
- Mehndiratta, M.; Nayak, R.; Garg, H.; Kumar, M.; Pandey, S. Appraisal of Kernig’s and Brudzinski’s sign in meningitis. Ann. Indian Acad. Neurol. 2012, 15, 287. [Google Scholar] [CrossRef] [PubMed]
- Nakao, J.H.; Jafri, F.N.; Shah, K.; Newman, D.H. Jolt accentuation of headache and other clinical signs: Poor predictors of meningitis in adults. Am. J. Emerg. Med. 2014, 32, 24–28. [Google Scholar] [CrossRef]
- Busl, K.M. Nosocomial Infections in the Neurointensive Care Unit. Neurol. Clin. 2017, 35, 785–807. [Google Scholar] [CrossRef]
- Li, Y.M.; Blaskiewicz, D.J.; Hall, W.A. Shunt-related intracranial abscess caused by Staphylococcus lugdunensis in a hydranencephalic patient. World Neurosurg. 2013, 80, e387–e389. [Google Scholar] [CrossRef] [PubMed]
- Matas, A.; Veiga, A.; Gabriel, J. Brain Abscess due to Staphylococcus lugdunensis in the Absence of Endocarditis or Bacteremia. Case Rep. Neurol. 2015, 7, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, T.; Nagao, M.; Yamamoto, M.; Matsumura, Y.; Kitano, T.; Takaori-Kondo, A.; Ichiyama, S. Staphylococcus epidermidis meningitis in the absence of a neurosurgical device secondary to catheter-related bloodstream infection: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 106. [Google Scholar] [CrossRef] [PubMed]
- Bijlsma, M.W.; Brouwer, M.C.; Kasanmoentalib, E.S.; Kloek, A.T.; Lucas, M.J.; Tanck, M.W.; van der Ende, A.; van de Beek, D. Community-acquired bacterial meningitis in adults in the Netherlands, 2006–2014: A prospective cohort study. Lancet Infect. Dis. 2016, 16, 339–347. [Google Scholar] [CrossRef]
- Uzzan, B.; Cohen, R.; Nicolas, P.; Cucherat, M.; Perret, G.Y. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: A systematic review and meta-analysis. Crit. Care Med. 2006, 34, 1996–2003. [Google Scholar] [CrossRef]
- Schlenk, F.; Frieler, K.; Nagel, A.; Vajkoczy, P.; Sarrafzadeh, A.S. Cerebral microdialysis for detection of bacterial meningitis in aneurysmal subarachnoid hemorrhage patients: A cohort study. Crit. Care. 2009, 13, R2. [Google Scholar] [CrossRef]
- Vikse, J.; Henry, B.M.; Roy, J.; Ramakrishnan, P.K.; Tomaszewski, K.A.; Walocha, J.A. The role of serum procalcitonin in the diagnosis of bacterial meningitis in adults: A systematic review and meta-analysis. Int. J. Infect. Dis. 2015, 38, 68–76. [Google Scholar] [CrossRef]
- Khalili, H.; Yadollahikhales, G.; Isaee, M. Diagnostic Accuracy of Peripheral White Blood Cell Count, Fever and Acute Leukocutosis for Bacterial Meningitis in Patients with Severe Traumatic Brain Injury. Bull. Emerg. Trauma 2015, 3, 53. [Google Scholar]
- Kaabia, N.; Scauarda, D.; Lena, G.; Drancourt, M. Molecular identification of Staphylococcus lugdunensis in a patient with meningitis. J. Clin. Microbiol. 2002, 40, 1824–1825. [Google Scholar] [CrossRef]
- Kastrup, O.; Isabel, W.; Matthias, M. Neuroimaging of infections. NeuroRx 2005, 2, 324–332. [Google Scholar] [CrossRef]
- Proulx, N.; Frechette, D.; Toye, B.; Chan, J.; Kravcik, S. Delays in the administration of antibiotics are associated with mortality from adult acute bacterial meningitis. Qjm 2005, 98, 291–298. [Google Scholar] [CrossRef]
- Brouwer, M.C.; McIntyre, P.; de Gans, J.; Prasad, K.; van de Beek, D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst. Rev. 2007, 1. [Google Scholar] [CrossRef]
- Zhao, Z.; Hua, X.; Yu, J.; Zhang, H.; Li, J.; Li, Z. Duration of empirical therapy in neonatal bacterial meningitis with third generation cephalosporin: A multicenter retrospective study. Arch. Med. Sci. 2019, 15, 1482. [Google Scholar] [CrossRef]
- Brouwer, M.C.; Tunkel, A.R.; van de Beek, D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin. Microbiol. Rev. 2010, 23, 467–492. [Google Scholar] [CrossRef]
- Vijayan, P.; Srinivas, D.; Siddaiah, N.; Bahubali, V. Device-Associated Meningitis by Linezolid-Resistant Staphylococcus haemolyticus in a Vancomycin-Hypersensitive Patient. J. Neurosci. Rural. Pract. 2019, 10, 718–720. [Google Scholar] [CrossRef]
- World Health Organization. Control of Epidemic Meningococcal Disease: WHO Practical Guidelines; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Epidemiology of meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenza. Chapter 2; 2011. Available online: https://www.cdc.gov/meningitis/lab-manual/chpt02-epi.html (accessed on 18 May 2020).
- Jiang, H.; Su, M.; Kui, L.; Huang, H.; Qiu, L.; Li, L.; Ma, J.; Du, T.; Fan, M.; Sun, Q. Prevalence and antibiotic resistance profiles of cerebrospinal fluid pathogens in children with acute bacterial meningitis in Yunnan province, China, 2012–2015. PLoS ONE 2017, 12, e0180161. [Google Scholar] [CrossRef]
- De Gans, J.; Van de Beek, D. Dexamethasone in adults with bacterial meningitis. N. Engl. J. Med. 2002, 347, 1549–1556. [Google Scholar] [CrossRef]
- Wall, E.C.; Ajdukiewicz, K.M.; Bergman, H.; Heyderman, R.S.; Garner, P. Osmotic therapies added to antibiotics for acute bacterial meningitis. Cochrane Database Syst. Rev. 2018, 2, 576–585. [Google Scholar] [CrossRef]
- Ratilal, B.O.; Costa, J.; Pappamikail, L.; Sampaio, C. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst. Rev. 2015, 4. [Google Scholar] [CrossRef]
- Gianella, S.; Ulrich, S.; Huttner, B.; Speich, R. Conservative management of a brain abscess in a patient with Staphylococcus lugdunensis endocarditis. Eur. J. Clin. Microbiol. Infect. Dis. 2006, 25, 476–478. [Google Scholar] [CrossRef][Green Version]
- Rebai, L.; Fitouhi, N.; Daghmouri, M.A.; Bahri, K. Linezolid for the treatment of postneurosurgical infection caused by methicillin-resistant Staphylococcus. Surg. Neurol. Int. 2019, 10. [Google Scholar] [CrossRef]
- Mounier, R.; Lobo, D.; Hulin, A.; Nebbad, B.; Cook, F.; Dhonneur, G. Is First-Line Vancomycin Still the Best Option to Treat Staphylococcus Health Care–Associated Meningitis? World Neurosurg. 2017, 99, e1–e812. [Google Scholar] [CrossRef] [PubMed]
- Denetclaw, T.H.; Suehiro, I.; Wang, P.K.; Tolliver, G. Successful treatment of ventriculostomy-associated meningitis caused by multidrug resistant coagulase-negative Staphylococcus epidermidis using low-volume intrathecal daptomycin and loading strategy. Ann. Pharmacother. 2014, 48, 1376–1379. [Google Scholar] [CrossRef]
- Vena, A.; Falcone, M.; Comandini, E.; Meledandri, M.; Novelli, A.; Campanile, F.; Stefani, S.; Venditti, M. Daptomycin plus trimethoprim/sulfamethoxazole combination therapy in post-neurosurgical meningitis caused by linezolid-resistant Staphylococcus epidermidis. Diagn. Microbiol. Infect. Dis. 2013, 76, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Kui, L.; Huang, H.; Su, M.; Wen, B.P. Frequency distribution and antibiotic resistance of pathogens from the cerebrospinal fluid of 116 children with bacterial meningitis. Zhongguo Dang Dai Er Ke Za Zhi 2013, 15, 264–267. [Google Scholar]
- Watanabe, S.; Tanaka, A.; Ono, T.; Ohta, M.; Miyamoto, H.; Tauchi, H.; Tanaka, M.; Suemaru, K.; Araki, H. Treatment with linezolid in a neonate with meningitis caused by methicillin-resistant Staphylococcus epidermidis. Eur. J. Pediatr. 2013, 172, 1419–1421. [Google Scholar] [CrossRef] [PubMed]
- Lucas, M.J.; Brouwer, M.C.; van de Beek, D. Neurological sequelae of bacterial meningitis. J. Infect. 2016, 73, 18–27. [Google Scholar] [CrossRef]
- MacGee, E.E.; Cauthen, J.C.; Brackett, C.E. Meningitis following acute traumatic cerebrospinal fluid fistula. J. Neurosurg. 1970, 33, 312–316. [Google Scholar] [CrossRef]
- Crawford, C.; Kennedy, N.; Weir, W.R.C. Cerebrospinal fluid rhinorrhoea and Haemophilus influenzae meningitis 37 years after a head injury. J. Infect. 1994, 28, 93–97. [Google Scholar] [CrossRef]
- Appelbaum, E. Meningitis following trauma to the head and face. JAMA 1960, 173, 1818–1822. [Google Scholar] [CrossRef]
- Okada, J.; Tsuda, T.; Takasugi, S.; Nishida, K.; Tóth, Z.; Matsumoto, K. Unusually late onset of cerebrospinal fluid rhinorrhea after head trauma. Surg. Neurol. 1991, 35, 213–217. [Google Scholar] [CrossRef]
- Plaisier, B.R. Post-traumatic meningitis: Risk factors, clinical features, bacteriology, and outcome. Int. J. Neurosurg. 2005, 2, 1. [Google Scholar]
- Lai, W.-A.; Chen, S.-F.; Tsai, N.-W.; Chang, C.-C.; Chang, W.-N.; Lu, C.-H.; Chuang, Y.-C.; Chien, C.-C.; Huang, C. Clinical characteristics and prognosis of acute bacterial meningitis in elderly patients over 65: A hospital-based study. BMC Geriatr. 2011, 11, 91. [Google Scholar] [CrossRef]
- Tian, R.; Hao, S.; Hou, Z.; Gao, Z.; Liu, B. The characteristics of post-neurosurgical bacterial meningitis in elective neurosurgery in 2012: A single institute study. Clin. Neurol. Neurosurg. 2015, 139, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Lien, C.-Y.; Huang, C.-R.; Tsai, N.-W.; Chang, C.-C.; Lu, C.-H.; Chang, W. Clinical Characteristics and Therapeutic Outcomes of Postneurosurgical Bacterial Meningitis in Elderly Patients over 65: A Hospital-based Study. Acta Neurol. Taiwan 2017, 26, 144–153. [Google Scholar]
- Drinkovic, D.; Pottumarthy, S.; Knight, D.; Morris, A. Neonatal coagulase-negative staphylococcal meningitis: A report of two cases. Pathology 2002, 34, 586–588. [Google Scholar] [CrossRef]
- Tian, L.; Zhang, Z.; Sun, Z. Pathogen Analysis of Central Nervous System Infections in a Chinese Teaching Hospital from 2012–2018: A Laboratory-based Retrospective Study. Curr. Med. Sci. 2019, 39, 449–454. [Google Scholar] [CrossRef] [PubMed]
- AlDhaleei, W.A.; Bhagavathula, A.S.; Aldoghaither, R. Embolic Stroke and Meningitis Secondary to Staphylococcus lugdunensis Native Valve Endocarditis. Case Rep. Infect. Dis. 2019, 2019, 7910262. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Kanamaru, A.; Uchida, H.; Yano, M.; Tada, H. A case of bacterial meningitis caused by methicillin-resistant Staphylococcus lugdunensis after surgery. Rinsho Shinkeigaku 2016, 56, 773–776. [Google Scholar] [CrossRef]
- Chitnis, A.S.; Guh, A.Y.; Benowitz, I.; Srinivasan, V.; Gertz Jr, R.E.; Shewmaker, P.L.; Beall, B.W.; O’Connell, H.; Noble-Wang, J.; Gornet, M. Outbreak of bacterial meningitis among patients undergoing myelography at an outpatient radiology clinic. J. Am. Coll. Radiol. 2012, 9, 185–190. [Google Scholar] [CrossRef]
- Kawaguchi, Y.; Seki, S.; Yasuda, T.; Nakamura, Y.; Nakano, M.; Kimura, T. Postoperative meningitis in patients with cervical cord tumor: A case report. Asian Spine J. 2010, 4, 136. [Google Scholar] [CrossRef]
- Nagashima, G.; Okamoto, N.; Okuda, M.; Nakashima, K.; Noda, M.; Itokawa, H.; Suzuki, R.; Fujimoto, T.; Marumo, K. Chemotherapy, Effect of linezolid against postneurosurgical meningitis caused by methicillin-resistant Staphylococcus epidermidis: Case report. J. Infect. Chemother. 2008, 14, 147. [Google Scholar] [CrossRef] [PubMed]
- Stevens, N.T.; Tharmabala, M.; Dillane, T.; Greene, C.M.; O’Gara, J.P.; Humphreys, H. Biofilm and the role of the ica operon and aap in Staphylococcus epidermidis isolates causing neurosurgical meningitis. Clin. Microbiol. Infect. 2008, 14, 719–722. [Google Scholar] [CrossRef]
- Kruse, A.-J.; Peerdeman, S.; Bet, P.; Debets-Ossenkopp, Y. Successful treatment with linezolid and rifampicin of meningitis due to methicillin-resistant Staphylococcus epidermidis refractory to vancomycin treatment. Eur. J. Clin. Microbiol. Infect. Dis. 2006, 25, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.R.; Lu, C.H.; Wu, J.J.; Chang, H.W.; Chien, C.C.; Lei, C.B.; Chang, W.N. Coagulase-negative staphylococcal meningitis in adults: Clinical characteristics and therapeutic outcomes. Infection 2005, 33, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, F.; Mander, K.A.; Leonard, A.V.; Vink, R. Neurogenic inflammation after traumatic brain injury and its potentiation of classical inflammation. J. Neuroinflammation 2016, 13, 264. [Google Scholar] [CrossRef] [PubMed]
- Ziebell, J.M.; Morganti-Kossmann, M.C. Involvement of pro- and anti-inflammatory cytokines and chemokines in the pathophysiology of traumatic brain injury. Neurotherapeutics 2010, 7, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Cash, A.; Theus, M.H. Mechanisms of Blood–Brain Barrier Dysfunction in Traumatic Brain Injury. Int. J. Mol. Sci. 2020, 21, 3344. [Google Scholar] [CrossRef]
- Sorby-Adams, A.J.; Marcoionni, A.M.; Dempsey, E.R.; Woenig, J.A.; Turner, R.J. The Role of Neurogenic Inflammation in Blood-Brain Barrier Disruption and Development of Cerebral Oedema Following Acute Central Nervous System (CNS) Injury. Int. J. Mol. Sci. 2017, 18, 1788. [Google Scholar] [CrossRef] [PubMed]
- Lorente, L.; Martín, M.M.; Almeida, T.; Hernández, M.; Ramos, L.; Argueso, M.; Cáceres, J.J.; Solé-Violán, J.; Jiménez, A. Serum substance P levels are associated with severity and mortality in patients with severe traumatic brain injury. Crit Care 2015, 19, 192. [Google Scholar] [CrossRef]
- Lorente, L.; Martín, M.M.; Pérez-Cejas, A.; González-Rivero, A.F.; Argueso, M.; Ramos, L.; Solé-Violán, J.; Cáceres, J.J.; Jiménez, A.; García-Marín, V. Persistently High Serum Substance P Levels and Early Mortality in Patients with Severe Traumatic Brain Injury. World Neurosurg. 2019, 132, e613–e617. [Google Scholar] [CrossRef]
- Hooper, C.; Pinteaux-Jones, F.; Fry, V.A.; Sevastou, I.G.; Baker, D.; Heales, S.J.; Pocock, J.M. Differential effects of albumin on microglia and macrophages; implications for neurodegeneration following blood-brain barrier damage. J. Neurochem. 2009, 109, 694–705. [Google Scholar] [CrossRef] [PubMed]
- Ralay Ranaivo, H.; Hodge, J.N.; Choi, N.; Wainwright, M.S. Albumin induces upregulation of matrix metalloproteinase-9 in astrocytes via MAPK and reactive oxygen species-dependent pathways. J. Neuroinflamm. 2012, 9, 68. [Google Scholar] [CrossRef] [PubMed]
- Muri, L.; Leppert, D.; Grandgirard, D.; Leib, S.L. MMPs and ADAMs in neurological infectious diseases and multiple sclerosis. Cell. Mol. Life Sci. 2019, 76, 3097–3116. [Google Scholar] [CrossRef] [PubMed]
- Fields, G.B. The Rebirth of Matrix Metalloproteinase Inhibitors: Moving Beyond the Dogma. Cells 2019, 8, 984. [Google Scholar] [CrossRef] [PubMed]
- Crupi, R.; Cordaro, M.; Cuzzocrea, S.; Impellizzeri, D. Management of Traumatic Brain Injury: From Present to Future. Antioxidants 2020, 9, 297. [Google Scholar] [CrossRef]
- Yang, Z.; Zhu, T.; Mondello, S.; Akel, M.; Wong, A.T.; Kothari, I.M.; Lin, F.; Shear, D.A.; Gilsdorf, J.S.; Leung, L.Y.; et al. Serum-Based Phospho-Neurofilament-Heavy Protein as Theranostic Biomarker in Three Models of Traumatic Brain Injury: An Operation Brain Trauma Therapy Study. J. Neurotrauma 2019, 36, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Kövesdi, E.; Lückl, J.; Bukovics, P.; Farkas, O.; Pál, J.; Czeiter, E.; Szellár, D.; Dóczi, T.; Komoly, S.; Büki, A. Update on protein biomarkers in traumatic brain injury with emphasis on clinical use in adults and paediatrics. Acta Neurochir. (Wien.) 2010, 152, 1–17. [Google Scholar] [CrossRef]
- Berger, R.P.; Beers, S.R.; Richichi, R.; Wiesman, D.; Adelson, P.D. Serum biomarker concentrations and outcome after pediatric traumatic brain injury. J. Neurotrauma 2007, 24, 1793–1801. [Google Scholar] [CrossRef]
- Fineschi, V.; Viola, R.V.; La Russa, R.; Santurro, A.; Frati, P. A Controversial Medicolegal Issue: Timing the Onset of Perinatal Hypoxic-Ischemic Brain Injury. Mediators Inflamm. 2017, 2017, 6024959. [Google Scholar] [CrossRef]
- Neri, M.; Büttner, A.; Fineschi, V. Brain Injury due to Mechanical Trauma and Ischemic-Hypoxic Insult: Biomarkers of Brain Injury and Oxidative Stress. Oxid Med. Cell Longev. 2017, 2017, 8923472. [Google Scholar] [CrossRef]
- Frati, A.; Cerretani, D.; Fiaschi, A.I.; Frati, P.; Gatto, V.; La Russa, R.; Pesce, A.; Pinchi, E.; Santurro, A.; Fraschetti, F.; et al. Diffuse Axonal Injury and Oxidative Stress: A Comprehensive Review. Int. J. Mol. Sci. 2017, 18, 2600. [Google Scholar] [CrossRef]
- Sharew, A.; Bodilsen, J.; Hansen, B.R.; Nielsen, H.; Brandt, C.T. The cause of death in bacterial meningitis. BMC Infect. Dis. 2020, 20, 182. [Google Scholar] [CrossRef] [PubMed]
- Neri, M.; Frati, A.; Turillazzi, E.; Cantatore, S.; Cipolloni, L.; Di Paolo, M.; Frati, P.; La Russa, R.; Maiese, A.; Scopetti, M.; et al. Immunohistochemical evaluation of aquaporin-4 and its correlation with CD68, IBA-1, HIF-1α, GFAP, and CD15 expressions in fatal traumatic brain injury. Int. J. Mol. Sci. 2018, 19, 3544. [Google Scholar]
- La Russa, R.; Maiese, A.; Viola, R.V.; De Matteis, A.; Pinchi, E.; Frati, P.; Fineschi, V. Searching for highly sensitive and specific biomarkers for sepsis: State-of-the-art in post-mortem diagnosis of sepsis through immunohistochemical analysis. Int. J. Immunopathol. Pharmacol. 2019, 33, 2058738419855226. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Bolino, G.; Mastracchio, A.; Frati, P.; Fineschi, V. An immunohistochemical study of the diagnostic value of TREM-1 as marker for fatal sepsis cases. Biotech. Histochem. 2019, 94, 159–166. [Google Scholar] [CrossRef]
- Maiese, A.; Del Nonno, F.; Dell’Aquila, M.; Moauro, M.; Baiocchini, A.; Mastracchio, A.; Bolino, G. Postmortem diagnosis of sepsis: A preliminary immunohistochemical study with an anti-procalcitonin antibody. Leg. Med. (Tokyo) 2017, 28, 1–5. [Google Scholar] [CrossRef]
- Pinchi, E.; Frati, A.; Cipolloni, L.; Aromatario, M.; Gatto, V.; La Russa, R.; Pesce, A.; Santurro, A.; Fraschetti, F.; Frati, P.; et al. Clinical-pathological study on β-APP, IL-1β, GFAP, NFL, Spectrin II, 8OHdG, TUNEL, miR-21, miR-16, miR-92 expressions to verify DAI-diagnosis, grade and prognosis. Sci. Rep. 2018, 8, 1–13. [Google Scholar] [CrossRef]
- Gayen, M.; Bhomia, M.; Balakathiresan, N.; Knollmann-Ritschel, B. Exosomal MicroRNAs Released by Activated Astrocytes as Potential Neuroinflammatory Biomarkers. Int. J. Mol. Sci. 2020, 21, 2312. [Google Scholar] [CrossRef]
- Pinchi, E.; Frati, A.; Cantatore, S.; D’Errico, S.; La Russa, R.; Maiese, A.; Palmieri, M.; Pesce, A.; Viola, R.V.; Frati, P.; et al. Acute Spinal Cord Injury: A Systematic Review Investigating miRNA Families Involved. Int. J. Mol. Sci. 2019, 20, 1841. [Google Scholar] [CrossRef]
- Slota, J.A.; Booth, S.A. MicroRNAs in Neuroinflammation: Implications in Disease Pathogenesis, Biomarker Discovery and Therapeutic Applications. Non-Coding RNA 2019, 5, 35. [Google Scholar] [CrossRef]
- Sessa, F.; Maglietta, F.; Bertozzi, G.; Salerno, M.; Di Mizio, G.; Messina, G.; Montana, A.; Ricci, P.; Pomara, C. Human Brain Injury and miRNAs: An Experimental Study. Int. J. Mol. Sci. 2019, 20, 1546. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, G.C.; Smothers, C.G.; Winkelman, C. Bioinformatic analysis of brain-specific miRNAs for identification of candidate traumatic brain injury blood biomarkers [published online ahead of print, 2020 Jun 4]. Brain Inj. 2020, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).