Imaging Inflammation and Infection in the Gastrointestinal Tract
Abstract
1. Introduction
2. Infection
2.1. Shigella spp.
2.2. Escherichia coli
2.3. Clostridium Difficile
2.4. Salmonella
3. Inflammation
3.1. Diverticulitis
3.1.1. X-ray
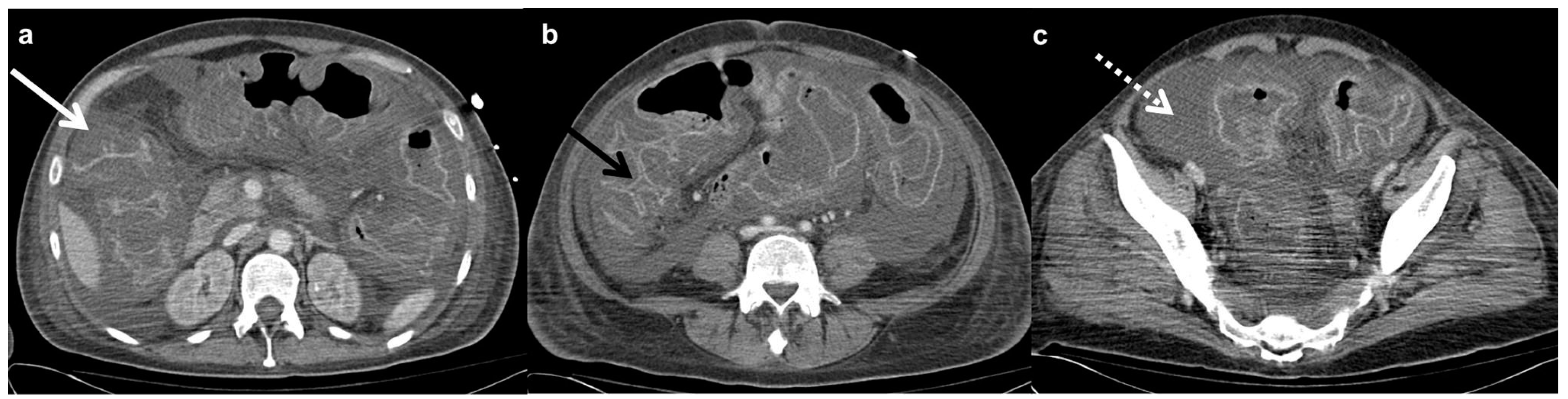
3.1.2. Computed Tomography
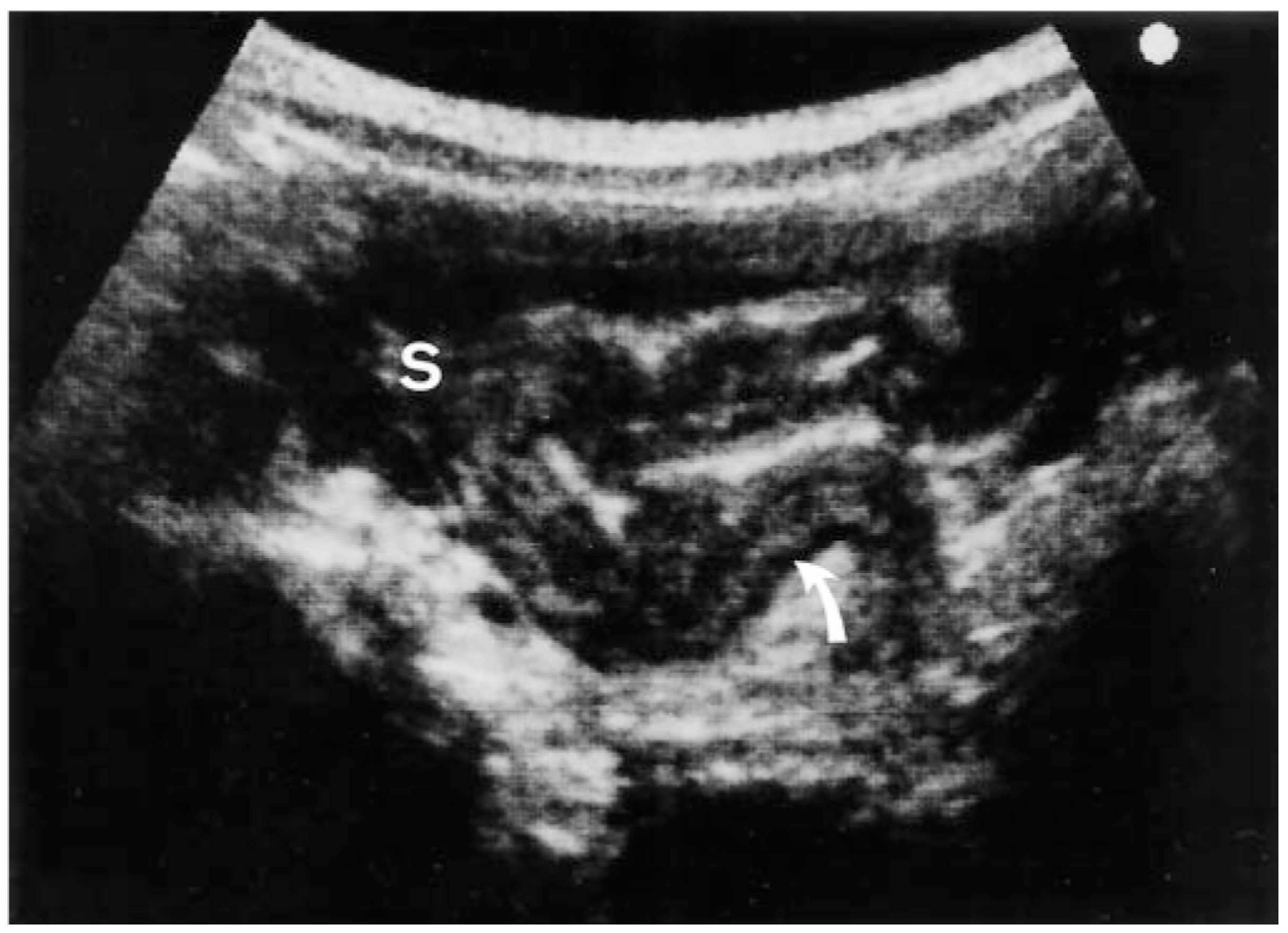
3.1.3. Ultrasonography
3.1.4. Magnetic Resonance Imaging
3.1.5. Endoscopy
3.2. Irritable Bowel Disease
3.2.1. Endoscopy
3.2.2. Chromoendoscopy
3.2.3. Computed Tomography
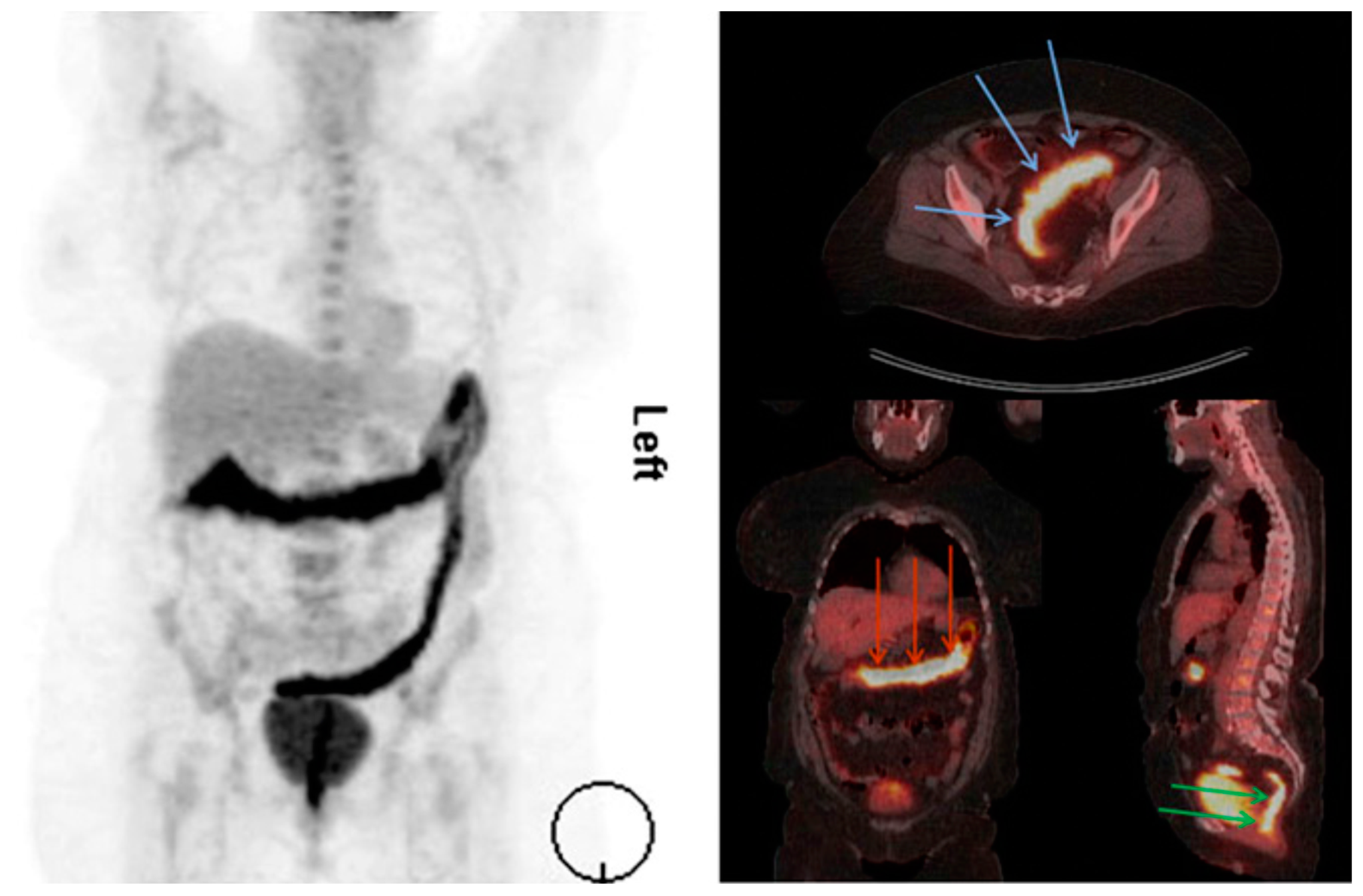
3.2.4. Positron Emission Tomography
3.2.5. Immuno-PET
3.2.6. Ultrasonography
3.2.7. Contrast-Enhanced US
3.2.8. Magnetic Resonance Imaging
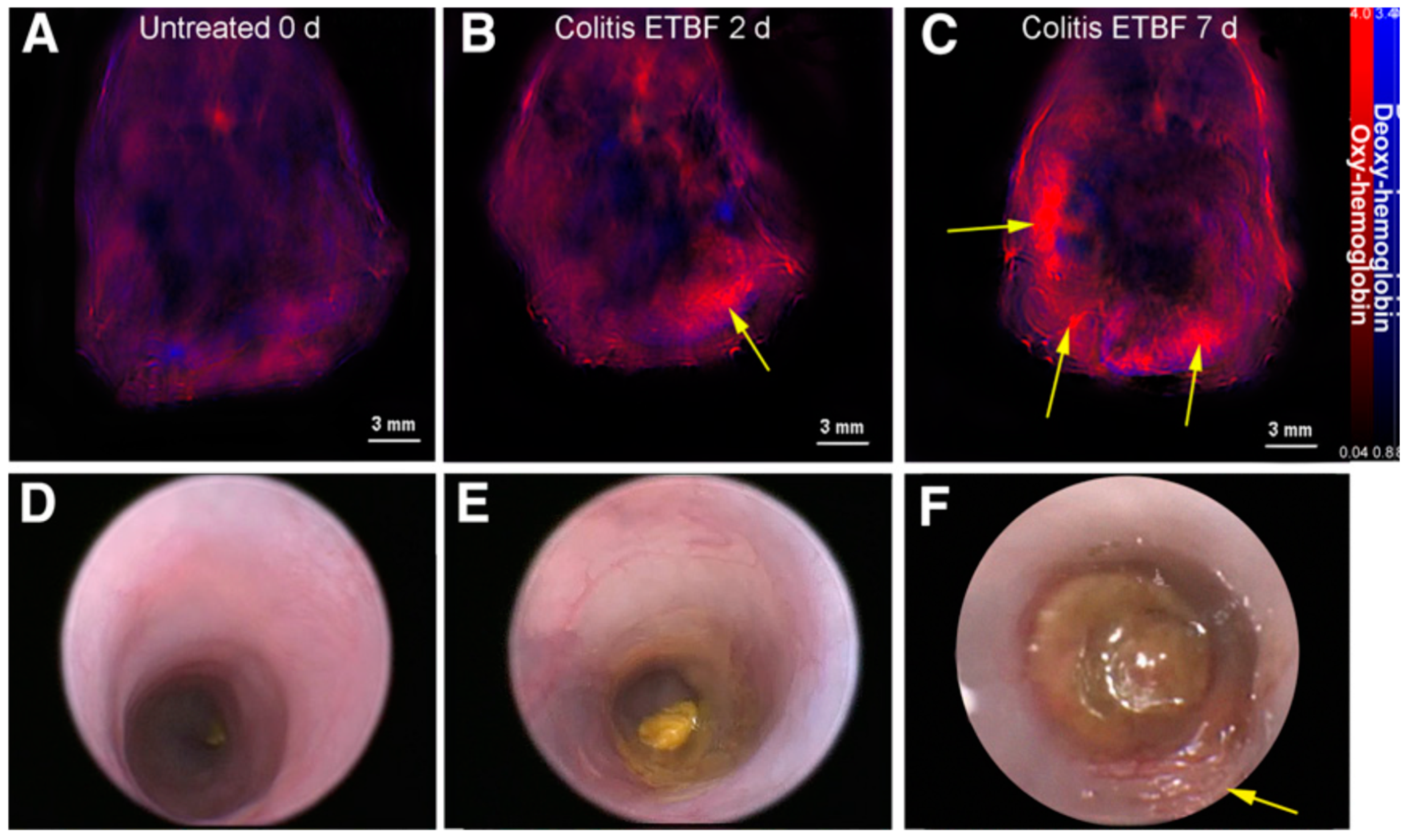
3.2.9. Multispectral Optoacoustic Tomography
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| GI | Gastrointestinal tract |
| ELISA | Enzymatically-linked immunosorbent assay |
| Ipa | Invasion plasmid antigen |
| EIEC | Enteroinvasive Escherichia coli |
| CDI | Clostridium difficile infection |
| EIA | Enzyme immunoassay |
| NAAT | Nucleic acid amplification |
| CT | Computed tomography |
| NTS | Nontyphoid Salmonella enterica |
| US | Ultrasonography |
| MRI | Magnetic resonance imaging |
| IBD | Irritable bowel disease |
| CD | Crohn’s disease |
| UC | Ulcerative colitis |
| CE | Chromoendoscopy |
| CTE | Computer tomography enterography |
| MRE | Magnetic resonance enterography |
| PET | Positron emission tomography |
| mAb | Monoclonal antibodies |
| CEUS | Contrast enhanced ultrasonography |
| MSOT | Multispectral optoacoustic tomography |
References
- Meltzer, A.C.; Pines, J.M.; Richards, L.M.; Mullins, P.; Mazer-Amirshahi, M. US emergency department visits for adults with abdominal and pelvic pain (2007-13): Trends in demographics, resource utilization and medication usage. Am. J. Emerg. Med. 2017, 35, 1966–1969. [Google Scholar] [CrossRef] [PubMed]
- Pant, C.; Deshpande, A.; Sferra, T.J.; Olyaee, M. Emergency department visits related to functional abdominal pain in the pediatric age group. J. Investig. Med. Off. Publ. Am. Fed. Clin. Res. 2017, 65, 803–806. [Google Scholar] [CrossRef] [PubMed]
- Macaluso, C.R.; McNamara, R.M. Evaluation and management of acute abdominal pain in the emergency department. Int. J. Gen. Med. 2012, 5, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Boendermaker, A.E.; Coolsma, C.W.; Emous, M.; Ter Avest, E. Efficacy of scheduled return visits for emergency department patients with non-specific abdominal pain. Emerg. Med. J. 2018, 35, 499–506. [Google Scholar] [CrossRef]
- Schiller, L.R.; Pardi, D.S.; Sellin, J.H. Chronic Diarrhea: Diagnosis and Management. Clin. Gastroenterol. Hepatol. 2017, 15, 182–193. [Google Scholar] [CrossRef]
- Ady, J.; Fong, Y. Imaging for infection: From visualization of inflammation to visualization of microbes. Surg. Infect. 2014, 15, 700–707. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Global Diarrhea Burden. Available online: https://www.cdc.gov/healthywater/global/diarrhea-burden.html (accessed on 8 October 2019).
- Liu, J.; Platts-Mills, J.A.; Juma, J.; Kabir, F.; Nkeze, J.; Okoi, C.; Operario, D.J.; Uddin, J.; Ahmed, S.; Alonso, P.L.; et al. Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: A reanalysis of the GEMS case-control study. Lancet 2016, 388, 1291–1301. [Google Scholar] [CrossRef]
- Ambrosetti, P.; Becker, C.; Terrier, F. Colonic diverticulitis: Impact of imaging on surgical management—A prospective study of 542 patients. Eur. Radiol. 2002, 12, 1145–1149. [Google Scholar] [CrossRef]
- Cho, K.C.; Morehouse, H.T.; Alterman, D.D.; Thornhill, B.A. Sigmoid diverticulitis: Diagnostic role of CT—Comparison with barium enema studies. Radiology 1990, 176, 111–115. [Google Scholar] [CrossRef]
- Rao, P.M.; Rhea, J.T.; Novelline, R.A.; Dobbins, J.M.; Lawrason, J.N.; Sacknoff, R.; Stuk, J.L. Helical CT with only colonic contrast material for diagnosing diverticulitis: Prospective evaluation of 150 patients. Am. J. Roentgenol. 1998, 170, 1445–1449. [Google Scholar] [CrossRef]
- Lameris, W.; van Randen, A.; Bipat, S.; Bossuyt, P.M.; Boermeester, M.A.; Stoker, J. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: Meta-analysis of test accuracy. Eur. Radiol. 2008, 18, 2498–2511. [Google Scholar] [CrossRef] [PubMed]
- Schwerk, W.B.; Schwarz, S.; Rothmund, M.; Arnold, R. Colon diverticulitis: Imaging diagnosis with ultrasound—A prospective study. Z. Gastroenterol. 1993, 31, 294–300. [Google Scholar] [PubMed]
- Heverhagen, J.T.; Sitter, H.; Zielke, A.; Klose, K.J. Prospective Evaluation of the Value of Magnetic Resonance Imaging in Suspected Acute Sigmoid Diverticulitis. Dis. Colon Rectum 2008, 51, 1810–1815. [Google Scholar] [CrossRef] [PubMed]
- Ajaj, W.; Ruehm, S.G.; Lauenstein, T.; Goehde, S.; Kuehle, C.; Herborn, C.U.; Goyen, M. Dark-lumen magnetic resonance colonography in patients with suspected sigmoid diverticulitis: A feasibility study. Eur. Radiol. 2005, 15, 2316–2322. [Google Scholar] [CrossRef] [PubMed]
- Ordás, I.; Rimola, J.; García-Bosch, O.; Rodríguez, S.; Gallego, M.; Etchevers, M.J.; Pellisé, M.; Feu, F.; González-Suárez, B.; Ayuso, C.; et al. Diagnostic accuracy of magnetic resonance colonography for the evaluation of disease activity and severity in ulcerative colitis: A prospective study. Gut 2013, 62, 1566. [Google Scholar] [CrossRef]
- Long, M.D.; Barnes, E.; Isaacs, K.; Morgan, D.; Herfarth, H.H. Impact of capsule endoscopy on management of inflammatory bowel disease: A single tertiary care center experience. Inflamm. Bowel Dis. 2011, 17, 1855–1862. [Google Scholar] [CrossRef] [PubMed]
- Civitelli, F.; Di Nardo, G.; Oliva, S.; Nuti, F.; Ferrari, F.; Dilillo, A.; Viola, F.; Pallotta, N.; Cucchiara, S.; Aloi, M. Ultrasonography of the Colon in Pediatric Ulcerative Colitis: A Prospective, Blind, Comparative Study with Colonoscopy. J. Pediatr. 2014, 165, 78–84. [Google Scholar] [CrossRef]
- Horsthuis, K.; Bipat, S.; Bennink, R.J.; Stoker, J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: Meta-analysis of prospective studies. Radiology 2008, 247, 64–79. [Google Scholar] [CrossRef]
- Wold, P.B.; Fletcher, J.G.; Johnson, C.D.; Sandborn, W.J. Assessment of Small Bowel Crohn Disease: Noninvasive Peroral CT Enterography Compared with Other Imaging Methods and Endoscopy—Feasibility Study. Radiology 2003, 229, 275–281. [Google Scholar] [CrossRef]
- Lemberg, D.A.; Issenman, R.M.; Cawdron, R.; Green, T.; Mernagh, J.; Skehan, S.J.; Nahmias, C.; Jacobson, K. Positron emission tomography in the investigation of pediatric inflammatory bowel disease. Inflamm. Bowel Dis. 2005, 11, 733–738. [Google Scholar] [CrossRef]
- Gemmel, F.; Dumarey, N.; Welling, M. Future diagnostic agents. Semin. Nucl. Med. 2009, 39, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Palestro, C.J.; Love, C.; Miller, T.T. Diagnostic imaging tests and microbial infections. Cell Microbiol. 2007, 9, 2323–2333. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, T.; Durand, D.J.; Subhawong, T.K.; Carrino, J.A.; Chhabra, A. Magnetic resonance imaging of musculoskeletal infections: Systematic diagnostic assessment and key points. Acad. Radiol. 2012, 19, 1434–1443. [Google Scholar] [CrossRef] [PubMed]
- Jelicks, L.A.; Lisanti, M.P.; Machado, F.S.; Weiss, L.M.; Tanowitz, H.B.; Desruisseaux, M.S. Imaging of small-animal models of infectious diseases. Am. J. Pathol. 2013, 182, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.; Fine, E.J.; Koba, W.; Zhao, D.; Rossi, M.A.; Tanowitz, H.B.; Jelicks, L.A. Micro-positron emission tomography in the evaluation of Trypanosoma cruzi-induced heart disease: Comparison with other modalities. Am. J. Trop. Med. Hyg. 2009, 81, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Thom, K.; Forrest, G. Gastrointestinal infections in immunocompromised hosts. Curr. Opin. Gastroenterol. 2006, 22, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Walker, W.A. Current Opinion in Gastroenterology. Curr. Opin. Gastroenterol. 2012, 28, 547–550. [Google Scholar] [CrossRef]
- Thomas, L.; Hale, G.T.K. Medical Microbiology; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996. Available online: https://www.ncbi.nlm.nih.gov/books/NBK7627/ (accessed on 5 October 2019).
- Hoerr, V.; Faber, C. Magnetic resonance imaging characterization of microbial infections. J. Pharm. Biomed. Anal. 2014, 93, 136–146. [Google Scholar] [CrossRef]
- O’Ryan, M.; Prado, V.; Pickering, L.K. A millennium update on pediatric diarrheal illness in the developing world. Semin. Pediatric Infect. Dis. 2005, 16, 125–136. [Google Scholar] [CrossRef]
- Eggleston, H.; Panizzi, P. Molecular imaging of bacterial infections in vivo: The discrimination of infection from inflammation. Informatics 2014, 1, 72–99. [Google Scholar] [CrossRef]
- Lupetti, A.; Welling, M.M.; Pauwels, E.K.; Nibbering, P.H. Radiolabelled antimicrobial peptides for infection detection. Lancet Infect. Dis. 2003, 3, 223–229. [Google Scholar] [CrossRef]
- Ueda, D.; Sato, T.; Yoshida, M. Ultrasonographic assessment of Salmonella enterocolitis in children. Pediatr. Radiol. 1999, 29, 469–471. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Smith, M.A.; Benjamin, W.H.; Kaminski, R.W.; Wenzel, H.; Nahm, M.H. Monoclonal Antibodies to Shigella Lipopolysaccharide Are Useful for Vaccine Production. Clin. Vaccine Immunol. 2016, 23, 681. [Google Scholar] [CrossRef]
- Mirzaei, E.Z.; Rajabnia, M.; Sadeghi, F.; Ferdosi-Shahandashti, E.; Sadeghi-Haddad-Zavareh, M.; Khafri, S.; Davoodabadi, A. Diagnosis of Clostridium difficile infection by toxigenic culture and PCR assay. Iran. J. Microbiol. 2018, 10, 287–293. [Google Scholar]
- Anderson, M.; Sansonetti, P.J.; Marteyn, B.S. Shigella Diversity and Changing Landscape: Insights for the Twenty-First Century. Front. Cell. Infect. Microbiol. 2016, 6, 45. [Google Scholar] [CrossRef]
- Kühn, S.; Lopez-Montero, N.; Chang, Y.Y.; Sartori-Rupp, A.; Enninga, J. Jost Enninga Imaging macropinosomes during Shigella infections. Methods 2017, 127, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Weiner, A.; Mellouk, N.; Lopez-Montero, N.; Chang, Y.Y.; Souque, C.; Schmitt, C.; Enninga, J. Macropinosomes are Key Players in Early Shigella Invasion and Vacuolar Escape in Epithelial Cells. PLoS Pathog. 2016, 12, e1005602. [Google Scholar] [CrossRef] [PubMed]
- Ud-Din, A.; Wahid, S. Relationship among Shigella spp. and enteroinvasive Escherichia coli (EIEC) and their differentiation. Braz. J. Microbiol. 2015, 45, 1131–1138. [Google Scholar] [CrossRef] [PubMed]
- McCrickard, L.S.; Crim, S.M.; Kim, S.; Bowen, A. Disparities in severe shigellosis among adults - Foodborne diseases active surveillance network, 2002–2014. BMC Public Health 2018, 18, 221. [Google Scholar] [CrossRef]
- Dohi, O.; Yagi, N.; Onozawa, Y.; Kimura-Tsuchiya, R.; Majima, A.; Kitaichi, T.; Horii, Y.; Suzuki, K.; Tomie, A.; Okayama, T.; et al. Linked color imaging improves endoscopic diagnosis of active Helicobacter pylori infection. Endosc. Int. Open 2016, 4, E800–E805. [Google Scholar] [CrossRef] [PubMed]
- Gentle, A.; Ashton, P.M.; Dallman, T.J.; Jenkins, C. Evaluation of Molecular Methods for Serotyping Shigella flexneri. J. Clin. Microbiol. 2016, 54, 1456–1461. [Google Scholar] [CrossRef] [PubMed]
- Sethabutr, O.; Echeverria, P.; Hanchalay, S.; Taylor, D.; Leksomboon, U. A Non-Radioactive DNA probe to identify shigella and enteroinvasive escherichia coli in stools of children with diarrhoea. Lancet 1985, 326, 1095–1097. [Google Scholar] [CrossRef]
- Rautureau, G.J.P.; Palama, T.L.; Canard, I.; Mirande, C.; Chatellier, S.; van Belkum, A.; Elena-Herrmann, B. Discrimination of Escherichia coli and Shigella spp. by Nuclear Magnetic Resonance-based Metabolomic Characterization of Culture Media. ACS Infect. Dis. 2019, 5, 1879–1886. [Google Scholar] [CrossRef]
- Gorski, L. Selective Enrichment Media Bias the Types of Salmonella enterica Strains Isolated from Mixed Strain Cultures and Complex Enrichment Broths. PLoS ONE 2012, 7, e34722. [Google Scholar] [CrossRef]
- Echeverria, P.; Sethabutr, O.; Pitarangsi, C. Microbiology and Diagnosis of Infections with Shigella and Enteroinvasive Escherichia coli. Clin. Infect. Dis. 1991, 13 (Suppl. S4), S220–S225. [Google Scholar] [CrossRef]
- Parodos, K.; McCarty, J. Nucleicacid Probes for the Detection of Shigella. U.S. Patent No. 5,648,481, 15 July 1997. [Google Scholar]
- Kaper, J.B.; Nataro, J.P.; Mobley, H.L.T. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2004, 2, 123–140. [Google Scholar] [CrossRef]
- Fratamico, P.M.; DebRoy, C.; Liu, Y.; Needleman, D.S.; Baranzoni, G.M.; Feng, P. Advances in Molecular Serotyping and Subtyping of Escherichia coli. Front. Microbiol. 2016, 7, 644. [Google Scholar] [CrossRef]
- Stevens, D.L.; Bryant, A.E.; Berger, A.; von Eichel-Streiber, C. Clostridium*. In Manual of Clinical Microbiology, 10th ed.; American Society of Microbiology: Washington, DC, USA, 2011. [Google Scholar]
- Peng, Z.; Ling, L.; Stratton, C.W.; Li, C.; Polage, C.R.; Wu, B.; Tang, Y.-W. Advances in the diagnosis and treatment of Clostridium difficile infections. Emerg. Microbes Infect. 2018, 7, 1–13. [Google Scholar] [CrossRef]
- Napolitano, L.M.; Edmiston, C.E. Clostridium difficile disease: Diagnosis, pathogenesis, and treatment update. Surgery 2017, 162, 325–348. [Google Scholar] [CrossRef]
- Leffler, D.A.; Lamont, J.T. Clostridium difficile Infection. N. Engl. J. Med. 2015, 372, 1539–1548. [Google Scholar] [CrossRef]
- Lucado, J.; Gould, C.; Elixhauser, A. Clostridium Difficile Infections (CDI) in Hospital Stays, 2009; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006–2012. [Google Scholar]
- Shin, J.H.; Chaves-Olarte, E.; Warren, C.A. Clostridium difficile Infection. Microbiol. Spectr. 2016, 4, 3. [Google Scholar]
- Wells, C.L.; Wilkins, T.D. Chapter 18 Clostridia: Sporeforming Anaerobic Bacilli. In Medical Micrbiology, 4th ed.; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996. [Google Scholar]
- Dunwoody, R.; Steel, A.; Landy, J.; Simmonds, N. Clostridium difficile and cystic fibrosis: Management strategies and the role of faecal transplantation. Paediatr. Respir. Rev. 2018, 26, 16–18. [Google Scholar] [CrossRef] [PubMed]
- Guerri, S.; Danti, G.; Frezzetti, G.; Lucarelli, E.; Pradella, S.; Miele, V. Clostridium difficile colitis: CT findings and differential diagnosis. Radiol. Med. 2019, 124, 1185–1198. [Google Scholar] [CrossRef] [PubMed]
- Ha, D.; Tsai, C.-J. Pneumatosis intestinalis in a patient with recurrent Clostridium difficile infection. BMJ Case Rep. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Kreiss, C.; Forohar, F.; Smithline, A.E.; Brandt, L.J. Pneumatosis Intestinalis Complicating C. Difficile Pseudomembranous Colitis. Am. J. Gastroenterol. 1999, 94, 2560–2561. [Google Scholar] [CrossRef]
- Schenk P1, M.C.; Kramer, L.; Ratheiser, K.; Kranz, A.; Zauner, C.; Stain, C.; Birsan, T.; Klepetko, W.; Müller, C. Pneumatosis intestinalis with Clostridium difficile colitis as a cause of acute abdomen after lung transplantation. Dig. Dis. Sci. 1998, 43, 2455–2458. [Google Scholar] [CrossRef]
- Wiener-Well, Y.; Kaloti, S.; Hadas-Halpern, I.; Munter, G.; Yinnon, A.M. Ultrasound diagnosis of Clostridium difficile-associated diarrhea. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 1975–1978. [Google Scholar] [CrossRef]
- Chachu, K.A.; Osterman, M.T. How to Diagnose and Treat IBD Mimics in the Refractory IBD Patient Who Does Not Have IBD. Inflamm. Bowel Dis. 2016, 22, 1262–1274. [Google Scholar] [CrossRef]
- Bula-Rudas, F.J.; Rathore, M.H.; Maraqa, N.F. Salmonella Infections in Childhood. Adv. Pediatr. 2015, 62, 29–58. [Google Scholar] [CrossRef]
- Giannella, R.A. Chapter 21: Salmonella. In Medical Microbiology, 4th ed.; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996. [Google Scholar]
- Bhutiani, N.; Grizzle, W.E.; Galandiuk, S.; Otali, D.; Dryden, G.W.; Egilmez, N.K.; McNally, L.R. Noninvasive Imaging of Colitis Using Multispectral Optoacoustic Tomography. J. Nucl. Med. 2017, 58, 1009–1012. [Google Scholar] [CrossRef]
- Andrews, J.R.; Ryan, E.T. Diagnostics for invasive Salmonella infections: Current challenges and future directions. Vaccine 2015, 33 (Suppl. S3), C8–C15. [Google Scholar] [CrossRef]
- Smith, J. The bacteriophage in the treatment of typhoid fever. Br. Med. J. 1924, 2, 47–49. [Google Scholar] [CrossRef] [PubMed]
- Hennedige, T.; Bindl, D.S.; Bhasin, A.; Venkatesh, S.K. Spectrum of Imaging Findings in Salmonella Infections. Am. J. Roentgenol. 2012, 198, W534–W539. [Google Scholar] [CrossRef] [PubMed]
- Farzan, A.; Friendship, R.M.; Dewey, C.E. Evaluation of enzyme-linked immunosorbent assay (ELISA) tests and culture for determining Salmonella status of a pig herd. Epidemiol. Infect. 2007, 135, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Goetz, M.; Wang, T.D. Molecular imaging in gastrointestinal endoscopy. Gastroenterology 2010, 138, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.L.; Oaks, E.V.; Formal, S.B. Identification and antigenic characterization of virulence-associated, plasmid-coded proteins of Shigella spp. and enteroinvasive Escherichia coli. Infect. Immun. 1985, 50, 620–629. [Google Scholar]
- Li, M.; Wang, T.D. Targeted endoscopic imaging. Gastrointest. Endosc. Clin. N. Am. 2009, 19, 283–298. [Google Scholar] [CrossRef]
- Gallo, A.; Ianiro, G.; Montalto, M.; Cammarota, G. The Role of Biomarkers in Diverticular Disease. J. Clin. Gastroenterol. 2016, 50, S26–S28. [Google Scholar] [CrossRef]
- Weizman, A.V.; Nguyen, G.C. Diverticular disease: Epidemiology and management. Can. J. Gastroenterol. 2011, 25, 385–389. [Google Scholar] [CrossRef]
- Ferreira-Aparicio, F.E.; Gutiérrez-Vega, R.; Gálvez-Molina, Y.; Ontiveros-Nevares, P.; Athie-Gútierrez, C.; Montalvo-Javé, E.E. Diverticular disease of the small bowel. Case Rep. Gastroenterol. 2012, 6, 668–676. [Google Scholar] [CrossRef]
- Wilkins, T.; Embry, K.; George, R. Diagnosis and management of acute diverticulitis. Am. Fam. Physician 2013, 87, 612–620. [Google Scholar] [PubMed]
- Transue, D.L.; Hanna, T.N.; Shekhani, H.; Rohatgi, S.; Khosa, F.; Johnson, J.O. Small bowel diverticulitis: An imaging review of an uncommon entity. Emerg. Radiol. 2017, 24, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Andeweg, C.S.; Knobben, L.; Hendriks, J.C.; Bleichrodt, R.P.; van Goor, H. How to Diagnose Acute Left-sided Colonic Diverticulitis: Proposal for a Clinical Scoring System. Ann. Surg. 2011, 253, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Laméris, W.; van Randen, A.; van Gulik, T.M.; Busch, O.R.; Winkelhagen, J.; Bossuyt, P.M.; Boermeester, M.A. A Clinical Decision Rule to Establish the Diagnosis of Acute Diverticulitis at the Emergency Department. Dis. Colon Rectum 2010, 53, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Tursi, A.; Brandimarte, G.; Elisei, W.; Giorgetti, G.M.; Inchingolo, C.D.; Aiello, F. Faecal calprotectin in colonic diverticular disease: A case–control study. Int. J. Colorectal Dis. 2009, 24, 49–55. [Google Scholar] [CrossRef]
- Buckley, O.; Geoghegan, T.; O’Riordain, D.S.; Lyburn, I.D.; Torreggiani, W.C. Computed tomography in the imaging of colonic diverticulitis. Clin. Radiol. 2004, 59, 977–983. [Google Scholar] [CrossRef]
- Hulnick, D.H.; Megibow, A.J.; Balthazar, E.J.; Naidich, D.P.; Bosniak, M.A. Computed tomography in the evaluation of diverticulitis. Radiology 1984, 152, 491–495. [Google Scholar] [CrossRef]
- Gottesman, L.; Zevon, S.J.; Brabbee, G.W.; Dailey, T.; Wichern, W.A. The use of water-soluble contrast enemas in the diagnosis of acute lower left quadrant peritonitis. Dis. Colon Rectum 1984, 27, 84–88. [Google Scholar] [CrossRef]
- Wexner, S.D.; Dailey, T.H. The Inital Management of Left Lower Quadrant Peritonitis. Dis. Colon Rectum 1986, 29, 635–638. [Google Scholar] [CrossRef]
- Halligan, S.; Saunders, B. Imaging diverticular disease. Best Pract. Res. Clin. Gastroenterol. 2002, 16, 595–610. [Google Scholar] [CrossRef]
- Destigter, K.K.; Keating, D.P. Imaging update: Acute colonic diverticulitis. Clin. Colon Rectal Surg. 2009, 22, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Hachigian, M.P.; Honickman, S.; Eisenstat, T.E.; Rubin, R.J.; Salvati, E.P. Computed Tomography in the Initial Management of Acute Left-Sided Diverticulitis. Dis. Colon Rectum 1992, 35, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Neff, C.C.; vanSonnenberg, E.; Casola, G.; Wittich, G.R.; Hoyt, D.B.; Halasz, N.A.; Martini, D.J. Diverticular abscesses: Percutaneous drainage. Radiology 1987, 163, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Rao, P.M.; Rhea, J.T.; Novelline, R.A. Helical CT of appendicitis and diverticulitis. Radiol. Clin. N. Am. 1999, 37, 895–910. [Google Scholar] [CrossRef]
- Bar-Meir, S.; Lahat, A.; Melzer, E. Role of Endoscopy in Patients with Diverticular Disease. Dig. Dis. 2012, 30, 60–63. [Google Scholar] [CrossRef]
- Snyder, M.J. Imaging of colonic diverticular disease. Clin. Colon Rectal Surg. 2004, 17, 155–162. [Google Scholar] [CrossRef][Green Version]
- Ramalho, M.; Ramalho, J.; Burke, L.M.; Semelka, R.C. Gadolinium Retention and Toxicity—An Update. Adv. Chronic Kidney Dis. 2017, 24, 138–146. [Google Scholar] [CrossRef]
- Rogosnitzky, M.; Branch, S. Gadolinium-based contrast agent toxicity: A review of known and proposed mechanisms. Biometals 2016, 29, 365–376. [Google Scholar] [CrossRef]
- Sai, V.F.; Velayos, F.; Neuhaus, J.; Westphalen, A.C. Colonoscopy after CT Diagnosis of Diverticulitis to Exclude Colon Cancer: A Systematic Literature Review. Radiology 2012, 263, 383–390. [Google Scholar] [CrossRef]
- Purysko, A.S.; Remer, E.M.; Filho, H.M.L.; Bittencourt, L.K.; Lima, R.V.; Racy, D.J. Beyond Appendicitis: Common and Uncommon Gastrointestinal Causes of Right Lower Quadrant Abdominal Pain at Multidetector CT. Radiographics 2011, 31, 927–947. [Google Scholar] [CrossRef]
- Lau, K.C.; Spilsbury, K.; Farooque, Y.; Kariyawasam, S.B.; Owen, R.G.; Wallace, M.H.; Makin, G.B. Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: Can colorectal cancer be confidently excluded? Dis. Colon Rectum 2011, 54, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Glaudemans, A.W.; Maccioni, F.; Mansi, L.; Dierckx, R.A.; Signore, A. Imaging of cell trafficking in Crohn’s disease. J. Cell Physiol. 2010, 223, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Kilcoyne, A.; Kaplan, J.L.; Gee, M.S. Inflammatory bowel disease imaging: Current practice and future directions. World J. Gastroenterol. 2016, 22, 917–932. [Google Scholar] [CrossRef] [PubMed]
- Molodecky, N.A.; Soon, I.S.; Rabi, D.M.; Ghali, W.A.; Ferris, M.; Chernoff, G.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Barkema, H.W.; et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012, 142, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Burisch, J.; Munkholm, P. Inflammatory bowel disease epidemiology. Curr. Opin. Gastroenterol. 2013, 29, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Loftus, E.V., Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology 2004, 126, 1504–1517. [Google Scholar] [CrossRef]
- Kappelman, M.D.; Rifas-Shiman, S.L.; Kleinman, K.; Ollendorf, D.; Bousvaros, A.; Grand, R.J.; Finkelstein, J.A. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin. Gastroenterol. Hepatol. 2007, 5, 1424–1429. [Google Scholar] [CrossRef]
- Kappelman, M.D.; Moore, K.R.; Allen, J.K.; Cook, S.F. Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Dig. Dis. Sci. 2013, 58, 519–525. [Google Scholar] [CrossRef]
- Axelrad, J.E.; Lichtiger, S.; Yajnik, V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J. Gastroenterol. 2016, 22, 4794–4801. [Google Scholar] [CrossRef]
- Stidham, R.W.; Higgins, P.D.R. Colorectal Cancer in Inflammatory Bowel Disease. Clin. Colon Rectal Surg. 2018, 31, 168–178. [Google Scholar]
- Eaden, J.A.; Abrams, K.R.; Mayberry, J.F. The risk of colorectal cancer in ulcerative colitis: A meta-analysis. Gut 2001, 48, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Beaugerie, L.; Itzkowitz, S.H. Cancers Complicating Inflammatory Bowel Disease. N. Engl. J. Med. 2015, 372, 1441–1452. [Google Scholar] [CrossRef] [PubMed]
- Spiceland, C.M.; Lodhia, N. Endoscopy in inflammatory bowel disease: Role in diagnosis, management, and treatment. World J. Gastroenterol. 2018, 24, 4014–4020. [Google Scholar] [CrossRef] [PubMed]
- Shergill, A.K.; Lightdale, J.R.; Bruining, D.H.; Acosta, R.D.; Chandrasekhara, V.; Chathadi, K.V.; Decker, G.A.; Early, D.S.; Evans, J.A.; Fanelli, R.D.; et al. The role of endoscopy in inflammatory bowel disease. Gastrointest. Endosc. 2015, 81, 1101–1121. [Google Scholar] [CrossRef]
- Bharadwaj, S.; Narula, N.; Tandon, P.; Yaghoobi, M. Role of endoscopy in inflammatory bowel disease. Gastroenterol. Rep. 2018, 6, 75–82. [Google Scholar] [CrossRef]
- Flynn, A.D.; Valentine, J.F. Chromoendoscopy for Dysplasia Surveillance in Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2018, 24, 1440–1452. [Google Scholar] [CrossRef]
- Carballal, S.; Maisterra, S.; López-Serrano, A.; Gimeno-García, A.Z.; Vera, M.I.; Marín-Garbriel, J.C.; Díaz-Tasende, J.; Márquez, L.; Álvarez, M.A.; Hernández, L.; et al. Real-life chromoendoscopy for neoplasia detection and characterisation in long-standing IBD. Gut 2018, 67, 70. [Google Scholar] [CrossRef]
- Har-Noy, O.; Katz, L.; Avni, T.; Battat, R.; Bessissow, T.; Yung, D.E.; Kopylov, U. Chromoendoscopy, Narrow-Band Imaging or White Light Endoscopy for Neoplasia Detection in Inflammatory Bowel Diseases. Dig. Dis. Sci. 2017, 62, 2982–2990. [Google Scholar] [CrossRef]
- Duigenan, S.; Gee, M.S. Imaging of pediatric patients with inflammatory bowel disease. AJR Am. J. Roentgenol. 2012, 199, 907–915. [Google Scholar] [CrossRef]
- Anupindi, S.A.; Grossman, A.B.; Nimkin, K.; Mamula, P.; Gee, M.S. Imaging in the evaluation of the young patient with inflammatory bowel disease: What the gastroenterologist needs to know. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 429–439. [Google Scholar] [CrossRef]
- Deepak, P.; Bruining, D.H. Radiographical evaluation of ulcerative colitis. Gastroenterol. Rep. 2014, 2, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, T.; Oliveira, M.I.; Castro, R.; Araujo, B.; Viamonte, B.; Cunha, R. Bowel wall thickening at CT: Simplifying the diagnosis. Insights Imaging 2014, 5, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Siddiki, H.A.; Fidler, J.L.; Fletcher, J.G.; Burton, S.S.; Huprich, J.E.; Hough, D.M.; Johnson, C.D.; Bruining, D.H.; Loftus, E.V., Jr.; Sandborn, W.J.; et al. Prospective comparison of state-of-the-art MR enterography and CT enterography in small-bowel Crohn’s disease. AJR Am. J. Roentgenol. 2009, 193, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D.; Ormstrup, T.; Vagn-Hansen, C.; Ostergaard, L.; Rafaelsen, S.R. Interobserver and intermodality agreement for detection of small bowel Crohn’s disease with MR enterography and CT enterography. Inflamm. Bowel Dis. 2011, 17, 1081–1088. [Google Scholar] [CrossRef]
- Desmond, A.N.; O’Regan, K.; Curran, C.; McWilliams, S.; Fitzgerald, T.; Maher, M.M.; Shanahan, F. Crohn’s disease: Factors associated with exposure to high levels of diagnostic radiation. Gut 2008, 57, 1524–1529. [Google Scholar] [CrossRef]
- Kroeker, K.I.; Lam, S.; Birchall, I.; Fedorak, R.N. Patients with IBD are exposed to high levels of ionizing radiation through CT scan diagnostic imaging: A five-year study. J. Clin. Gastroenterol. 2011, 45, 34–39. [Google Scholar] [CrossRef]
- Gotthardt, M.; Bleeker-Rovers, C.P.; Boerman, O.C.; Oyen, W.J. Imaging of inflammation by PET, conventional scintigraphy, and other imaging techniques. J. Nucl. Med. 2010, 51, 1937–1949. [Google Scholar] [CrossRef]
- Bettenworth, D.; Reuter, S.; Hermann, S.; Weckesser, M.; Kerstiens, L.; Stratis, A.; Nowacki, T.M.; Ross, M.; Lenze, F.; Edemir, B.; et al. Translational 18F-FDG PET/CT imaging to monitor lesion activity in intestinal inflammation. J. Nucl. Med. 2013, 54, 748–755. [Google Scholar] [CrossRef]
- Malham, M.; Hess, S.; Nielsen, R.G.; Husby, S.; Hoilund-Carlsen, P.F. PET/CT in the diagnosis of inflammatory bowel disease in pediatric patients: A review. Am. J. Nucl. Med. Mol. Imaging 2014, 4, 225–230. [Google Scholar]
- Skehan, S.J.; Issenman, R.; Mernagh, J.; Nahmias, C.; Jacobson, K. 18F-fluorodeoxyglucose positron tomography in diagnosis of paediatric inflammatory bowel disease. Lancet 1999, 354, 836–837. [Google Scholar] [CrossRef]
- Loffler, M.; Weckesser, M.; Franzius, C.; Schober, O.; Zimmer, K.P. High diagnostic value of 18F-FDG-PET in pediatric patients with chronic inflammatory bowel disease. Ann. N. Y. Acad. Sci. 2006, 1072, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Perlman, S.B.; Hall, B.S.; Reichelderfer, M. PET/CT imaging of inflammatory bowel disease. Semin. Nucl. Med. 2013, 43, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Neurath, M.F.; Vehling, D.; Schunk, K.; Holtmann, M.; Brockmann, H.; Helisch, A.; Orth, T.; Schreckenberger, M.; Galle, P.R.; Bartenstein, P. Noninvasive assessment of Crohn’s disease activity: A comparison of 18F-fluorodeoxyglucose positron emission tomography, hydromagnetic resonance imaging, and granulocyte scintigraphy with labeled antibodies. Am. J. Gastroenterol. 2002, 97, 1978–1985. [Google Scholar] [CrossRef] [PubMed]
- Meisner, R.S.; Spier, B.J.; Einarsson, S.; Roberson, E.N.; Perlman, S.B.; Bianco, J.A.; Taylor, A.J.; Einstein, M.; Jaskowiak, C.J.; Massoth, K.M.; et al. Pilot study using PET/CT as a novel, noninvasive assessment of disease activity in inflammatory bowel disease. Inflamm. Bowel Dis. 2007, 13, 993–1000. [Google Scholar] [CrossRef]
- Louis, E.; Ancion, G.; Colard, A.; Spote, V.; Belaiche, J.; Hustinx, R. Noninvasive assessment of Crohn’s disease intestinal lesions with (18) F-FDG PET/CT. J. Nucl. Med. 2007, 48, 1053–1059. [Google Scholar] [CrossRef]
- Das, C.J.; Makharia, G.; Kumar, R.; Chawla, M.; Goswami, P.; Sharma, R.; Malhotra, A. PET-CT enteroclysis: A new technique for evaluation of inflammatory diseases of the intestine. Eur. J. Nucl. Med. Mol. Imaging 2007, 34, 2106–2114. [Google Scholar] [CrossRef]
- Agriantonis, D.; Perlman, S.B.; Spier, B.J.; Jaskowiak, C.J.; Reichelderfer, M. FDG PET/CT aids the management of IBD patients suspected of disease flare-up. J. Nucl. Med. 2008, 49 (Suppl. S1). [Google Scholar]
- Dmochowska, N.; Tieu, W.; Keller, M.D.; Wardill, H.R.; Mavrangelos, C.; Campaniello, M.A.; Takhar, P.; Hughes, P.A. Immuno-PET of Innate Immune Markers CD11b and IL-1beta Detects Inflammation in Murine Colitis. J. Nucl. Med. 2019, 60, 858–863. [Google Scholar] [CrossRef]
- Freise, A.C.; Zettlitz, K.A.; Salazar, F.B.; Lu, X.; Tavare, R.; Wu, A.M. ImmunoPET Imaging of Murine CD4(+) T Cells Using Anti-CD4 Cys-Diabody: Effects of Protein Dose on T Cell Function and Imaging. Mol. Imaging Biol. 2017, 19, 599–609. [Google Scholar] [CrossRef]
- Van Dongen, G.A.; Visser, G.W.; Lub-de Hooge, M.N.; de Vries, E.G.; Perk, L.R. Immuno-PET: A navigator in monoclonal antibody development and applications. Oncologist 2007, 12, 1379–1389. [Google Scholar] [CrossRef]
- Kucharzik, T.; Kannengiesser, K.; Peterson, F. The use of ultrasound in inflammatory bowel disease. Ann. Gastroenterol. 2017, 30, 10. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, E.; Petruzziello, C.; Onali, S.; Condino, G.; Zorzi, F.; Pallone, F.; Biancone, L. Severity of postoperative recurrence in Crohn’s disease: Correlation between endoscopic and sonographic findings. Inflamm. Bowel Dis. 2009, 15, 1635–1642. [Google Scholar] [CrossRef] [PubMed]
- Rigazio, C.; Ercole, E.; Laudi, C.; Daperno, M.; Lavagna, A.; Crocella, L.; Bertolino, F.; Vigano, L.; Sostegni, R.; Pera, A.; et al. Abdominal bowel ultrasound can predict the risk of surgery in Crohn’s disease: Proposal of an ultrasonographic score. Scand. J. Gastroenterol. 2009, 44, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Darge, K.; Anupindi, S. Pancreatitis and the role of US, MRCP and ERCP. Pediatr. Radiol. 2009, 39 (Suppl. S2), S153–S157. [Google Scholar] [CrossRef]
- Conti, C.B.; Giunta, M.; Gridavilla, D.; Conte, D.; Fraquelli, M. Role of Bowel Ultrasound in the Diagnosis and Follow-up of Patients with Crohn’s Disease. Ultrasound Med. Biol. 2017, 43, 725–734. [Google Scholar] [CrossRef]
- Choi, D.; Jin Lee, S.; Ah Cho, Y.; Lim, H.K.; Hoon Kim, S.; Jae Lee, W.; Hoon Lim, J.; Park, H.; Rae Lee, Y. Bowel wall thickening in patients with Crohn’s disease: CT patterns and correlation with inflammatory activity. Clin. Radiol. 2003, 58, 68–74. [Google Scholar] [CrossRef]
- Sempere, G.A.; Martinez Sanjuan, V.; Medina Chulia, E.; Benages, A.; Tome Toyosato, A.; Canelles, P.; Bulto, A.; Quiles, F.; Puchades, I.; Cuquerella, J.; et al. MRI evaluation of inflammatory activity in Crohn’s disease. AJR Am. J. Roentgenol. 2005, 184, 1829–1835. [Google Scholar] [CrossRef]
- Medellin, A.; Merrill, C.; Wilson, S.R. Role of contrast-enhanced ultrasound in evaluation of the bowel. Abdom. Radiol. 2018, 43, 918–933. [Google Scholar] [CrossRef]
- Valette, P.J.; Rioux, M.; Pilleul, F.; Saurin, J.C.; Fouque, P.; Henry, L. Ultrasonography of chronic inflammatory bowel diseases. Eur. Radiol. 2001, 11, 1859–1866. [Google Scholar] [CrossRef]
- Roccarina, D.; Garcovich, M.; Ainora, M.E.; Caracciolo, G.; Ponziani, F.; Gasbarrini, A.; Zocco, M.A. Diagnosis of bowel diseases: The role of imaging and ultrasonography. World J. Gastroenterol. 2013, 19, 2144–2153. [Google Scholar] [CrossRef]
- Serra, C.; Menozzi, G.; Labate, A.M.; Giangregorio, F.; Gionchetti, P.; Beltrami, M.; Robotti, D.; Fornari, F.; Cammarota, T. Ultrasound assessment of vascularization of the thickened terminal ileum wall in Crohn’s disease patients using a low-mechanical index real-time scanning technique with a second generation ultrasound contrast agent. Eur. J. Radiol. 2007, 62, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Merrill, C.; Medellin, A.; Novak, K.; Wilson, S.R. Bowel Ultrasound State of the Art: Grayscale and Doppler Ultrasound, Contrast Enhancement, and Elastography in Crohn Disease. J. Ultrasound Med. 2019, 38, 271–288. [Google Scholar] [CrossRef] [PubMed]
- Gee, M.S.; Harisinghani, M.G. MRI in patients with inflammatory bowel disease. J. Magn. Reson. Imaging 2011, 33, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Prassopoulos, P.; Papanikolaou, N.; Grammatikakis, J.; Rousomoustakaki, M.; Maris, T.; Gourtsoyiannis, N. MR enteroclysis imaging of Crohn disease. Radiographics 2001, 21, S161–S172. [Google Scholar] [CrossRef]
- Gourtsoyiannis, N.C.; Grammatikakis, J.; Papamastorakis, G.; Koutroumbakis, J.; Prassopoulos, P.; Rousomoustakaki, M.; Papanikolaou, N. Imaging of small intestinal Crohn’s disease: Comparison between MR enteroclysis and conventional enteroclysis. Eur. Radiol. 2006, 16, 1915–1925. [Google Scholar] [CrossRef]
- Masselli, G.; Gualdi, G. MR imaging of the small bowel. Radiology 2012, 264, 333–348. [Google Scholar] [CrossRef]
- Bhutiani, N.; Samykutty, A.; McMasters, K.M.; Egilmez, N.K.; McNally, L.R. In vivo tracking of orally-administered particles within the gastrointestinal tract of murine mouse models using multispectral optoacoustic tomography. Photoacoustics 2018, 13, 46–52. [Google Scholar] [CrossRef]
- Waldner, M.J.; Rath, T.; Schurmann, S.; Bojarski, C.; Atreya, R. Imaging of Mucosal Inflammation: Current Technological Developments, Clinical Implications, and Future Perspectives. Front. Immunol. 2017, 8, 1256. [Google Scholar] [CrossRef]
- Knieling, F.; Neufert, C.; Hartmann, A.; Claussen, J.; Urich, A.; Egger, C.; Vetter, M.; Fischer, S.; Pfeifer, L.; Hagel, A.; et al. Multispectral Optoacoustic Tomography for Assessment of Crohn’s Disease Activity. N. Engl. J. Med. 2017, 376, 1292–1294. [Google Scholar] [CrossRef]
| Modality | Subjects | Sensitivity | Specificity | Study |
|---|---|---|---|---|
| Diverticulitis | ||||
| CT vs. contrast enema | 542 humans | 98% vs. 92% | Not Reported | Ambrosetti et al. (2002) [9] |
| CT vs. contrast enema | 56 humans | 93% vs. 80% | 100% | Cho et al. (1990) [10] |
| CT | 150 humans | 97% | 100% | Rao et al. (1997) [11] |
| CT vs. ultrasound | 684 humans vs. 630 humans | 94% vs. 92% | 99% vs. 90% | Lameris et al. (2007) [12] |
| Ultrasound | 161 humans | 98.6% | 96.5% | Schwerk et al. (1993) [13] |
| MRI | 55 humans | 95% | 88% | Heverhagen et al. (2008) [14] |
| MRI | 40 humans | 86% | 92% | Ajaj et al. (2005) [15] |
| Irritable Bowel Disease | ||||
| MRI | 50 humans | 87% | 88% | Ordás et al. (2013) [16] |
| Endoscopy | Unknown | 91% | 92% | Long et al. (2011) [17] |
| Ultrasonography | 60 humans | 75–96% | 100% | Civitelli et al. (2014) [18] |
| CT | 23 humans | 76.9% | 90% | Wold et al. (2003) [19,20] |
| PET/CT | 65 humans | 98% | 68% | Lemberg et al. (2005) [21] |
| Infectious Agent | Clinical Evaluation | Screening | Study |
|---|---|---|---|
| Shigella | LPS O-Antigen | ELISA/Serotyping | Lin et al. (2016) [42]; Gentle et al. (2015) [35] |
| Shigella and Escherichia coli | Stool blot | DNA Probing | Sethabutr et al. (1985) [43] |
| Shigella and Escherichia coli | Culture Media | NMR | Rautureau et al. (2019) [44] |
| Salmonella | Stool Sample | Selective Media | Gorski (2012) [45] |
| Clostridium difficile | Stool Sample | Toxigenic Culture Testing, PCR | Mirzaei (2018) [46] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frickenstein, A.N.; Jones, M.A.; Behkam, B.; McNally, L.R. Imaging Inflammation and Infection in the Gastrointestinal Tract. Int. J. Mol. Sci. 2020, 21, 243. https://doi.org/10.3390/ijms21010243
Frickenstein AN, Jones MA, Behkam B, McNally LR. Imaging Inflammation and Infection in the Gastrointestinal Tract. International Journal of Molecular Sciences. 2020; 21(1):243. https://doi.org/10.3390/ijms21010243
Chicago/Turabian StyleFrickenstein, Alex N., Meredith A. Jones, Bahareh Behkam, and Lacey R. McNally. 2020. "Imaging Inflammation and Infection in the Gastrointestinal Tract" International Journal of Molecular Sciences 21, no. 1: 243. https://doi.org/10.3390/ijms21010243
APA StyleFrickenstein, A. N., Jones, M. A., Behkam, B., & McNally, L. R. (2020). Imaging Inflammation and Infection in the Gastrointestinal Tract. International Journal of Molecular Sciences, 21(1), 243. https://doi.org/10.3390/ijms21010243





