Rewarming Injury after Cold Preservation
Abstract
1. Introduction
2. Cold Ischemic Preservation
3. Reoxygenation Injury
4. Rewarming Injury
5. Mitigation of Rewarming Injury
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ANT | Adenosine nucleotide transporter |
| ATP | Adenosine triphosphate |
| COR | Controlled oxygenated rewarming |
| MPT | Mitochondrial permeability transition |
| NAD | Nicotineamide dinucleotide |
| NMP | Normothermic machine perfusion |
| OFR | Oxygen free radicals |
| HNE | 4-Hydroxy-2-nonenal |
| RET | Reverse electron transport |
| XDH | Xanthine dehydrogenase |
| XOD | Xanthine oxidase |
References
- Belzer, F.O.; Southard, J.H. Principles of solid-organ preservation by cold storage. Transplantation 1988, 45, 673–676. [Google Scholar] [CrossRef] [PubMed]
- van’t Hoff, M.J.H. Etudes Sur La Dynamique Chimique; Müller & Co: Amsterdam, The Netherlands, 1884. [Google Scholar]
- Hearse, D.J.; Braimbridge, M.V.; Jynge, P. Hypothermia. In Protection of the Ischemic Myocardium; Raven Press: New York, NY, USA, 1981; pp. 167–208. [Google Scholar]
- Pegg, D.E.; Foreman, J.; Hunt, C.J.; Diaper, M.P. The mechanism of action of retrograde oxygen persufflation in renal preservation. Transplantation 1989, 48, 210–217. [Google Scholar] [CrossRef]
- Hoffmann, T.; Minor, T. New strategies and concepts in organ preservation. Eur. Surg. Res. 2015, 54, 114–126. [Google Scholar] [CrossRef]
- Kalogeris, T.; Baines, C.P.; Krenz, M.; Korthuis, R.J. Ischemia/reperfusion. Compr. Physiol. 2016, 7, 113–170. [Google Scholar] [PubMed]
- Minor, T.; Isselhard, W. Synthesis of high energy phosphates during cold ischemic rat liver preservation with gaseous oxygen insufflation. Transplantation 1996, 61, 20–22. [Google Scholar] [CrossRef] [PubMed]
- McCord, J.M. Oxygen-derived free radicals in postischemic tissue injury. N. Engl. J. Med. 1985, 312, 159–163. [Google Scholar] [PubMed]
- Harrison, R. Human xanthine oxidoreductase: In search of a function. Biochem. Soc. Trans. 1997, 25, 786–791. [Google Scholar] [CrossRef][Green Version]
- Chouchani, E.T.; Pell, V.R.; James, A.M.; Work, L.M.; Saeb-Parsy, K.; Frezza, C.; Krieg, T.; Murphy, M.P. A unifying mechanism for mitochondrial superoxide production during ischemia-reperfusion injury. Cell Metab. 2016, 23, 254–263. [Google Scholar] [CrossRef]
- Chouchani, E.T.; Pell, V.R.; Gaude, E.; Aksentijevic, D.; Sundier, S.Y.; Robb, E.L.; Logan, A.; Nadtochiy, S.M.; Ord, E.N.; Smith, A.C.; et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ros. Nature 2014, 515, 431–435. [Google Scholar] [CrossRef]
- Pell, V.R.; Chouchani, E.T.; Murphy, M.P.; Brookes, P.S.; Krieg, T. Moving forwards by blocking back-flow: The yin and yang of mi therapy. Circ. Res. 2016, 118, 898–906. [Google Scholar] [CrossRef]
- Gorenkova, N.; Robinson, E.; Grieve, D.J.; Galkin, A. Conformational change of mitochondrial complex i increases ros sensitivity during ischemia. Antioxid Redox Signal. 2013, 19, 1459–1468. [Google Scholar] [CrossRef]
- Drose, S.; Stepanova, A.; Galkin, A. Ischemic a/d transition of mitochondrial complex i and its role in ros generation. Biochim. Biophys Acta 2016, 1857, 946–957. [Google Scholar] [CrossRef]
- Minor, T.; Stegemann, J.; Hirner, A.; Koetting, M. Impaired autophagic clearance after cold preservation of fatty livers correlates with tissue necrosis upon reperfusion and is reversed by hypothermic reconditioning. Liver Transpl. 2009, 15, 798–805. [Google Scholar] [CrossRef]
- Dutkowski, P.; Graf, R.; Clavien, P.A. Rescue of the cold preserved rat liver by hypothermic oxygenated machine perfusion. Am. J. Transpl. 2006, 6, 903–912. [Google Scholar] [CrossRef]
- Gallinat, A.; Treckmann, J.; Luer, B.; Efferz, P.; Paul, A.; Minor, T. Preservation of porcine kidneys by sequential cold storage and brief hypothermic perfusion is equally effective as long term machine perfusion. Langenbeck’s Arch. Surg. 2011, 365. [Google Scholar]
- Dutkowski, P.; Furrer, K.; Tian, Y.; Graf, R.; Clavien, P.A. Novel short-term hypothermic oxygenated perfusion (hope) system prevents injury in rat liver graft from non-heart beating donor. Ann. Surg. 2006, 244, 968–976. [Google Scholar] [CrossRef]
- Minor, T.; Koetting, M.; Koetting, M.; Kaiser, G.; Efferz, P.; Luer, B.; Paul, A. Hypothermic reconditioning by gaseous oxygen improves survival after liver transplantation in the pig. Am. J. Transpl. 2011, 11, 2627–2634. [Google Scholar] [CrossRef]
- Minor, T.; von Horn, C.; Paul, A. Role of temperature in reconditioning and evaluation of cold preserved kidney and liver grafts. Curr. Opin. Organ. Transpl. 2017, 22, 267–273. [Google Scholar] [CrossRef]
- Leducq, N.; Delmas-Beauvieux, M.C.; Bourdel-Marchasson, I.; Dufour, S.; Gallis, J.L.; Canioni, P.; Diolez, P. Mitochondrial permeability transition during hypothermic to normothermic reperfusion in rat liver demonstrated by the protective effect of cyclosporin a. Biochem. J. 1998, 336, 501–506. [Google Scholar] [CrossRef]
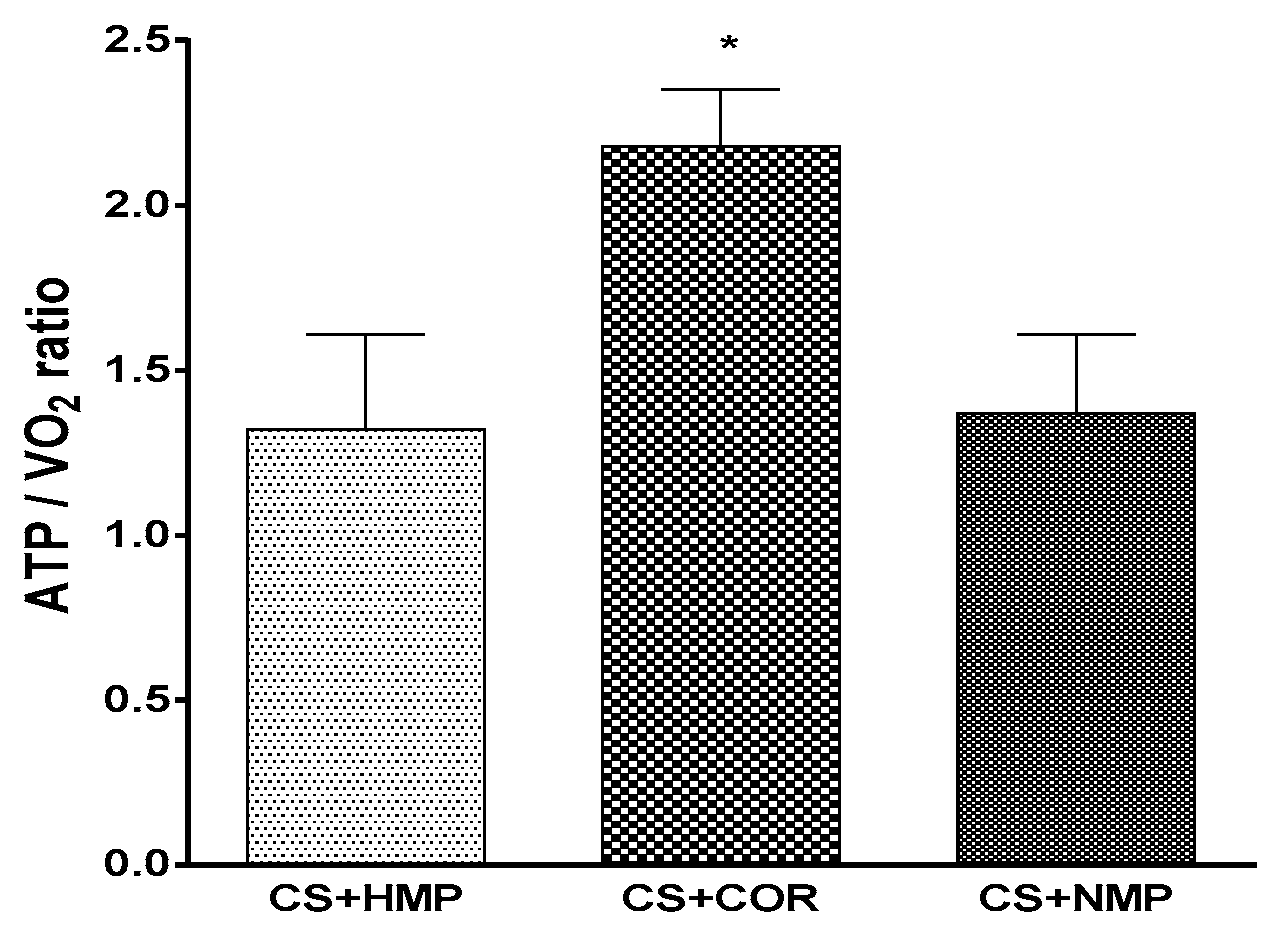
- Minor, T.; Efferz, P.; Fox, M.; Wohlschlaeger, J.; Luer, B. Controlled oxygenated rewarming of cold stored liver grafts by thermally graduated machine perfusion prior to reperfusion. Am. J. Transpl. 2013, 13, 1450–1460. [Google Scholar] [CrossRef]
- Leuvenink, H.G. Warming-up, not only essential for athletes? Transplantation 2015. [Google Scholar] [CrossRef] [PubMed]
- Echtay, K.S.; Esteves, T.C.; Pakay, J.L.; Jekabsons, M.B.; Lambert, A.J.; Portero-Otin, M.; Pamplona, R.; Vidal-Puig, A.J.; Wang, S.; Roebuck, S.J.; et al. A signalling role for 4-hydroxy-2-nonenal in regulation of mitochondrial uncoupling. EMBO J. 2003, 22, 4103–4110. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.P.; Echtay, K.S.; Blaikie, F.H.; Asin-Cayuela, J.; Cocheme, H.M.; Green, K.; Buckingham, J.A.; Taylor, E.R.; Hurrell, F.; Hughes, G.; et al. Superoxide activates uncoupling proteins by generating carbon-centered radicals and initiating lipid peroxidation: Studies using a mitochondria-targeted spin trap derived from alpha-phenyl-n-tert-butylnitrone. J. Biol. Chem. 2003, 278, 48534–48545. [Google Scholar] [CrossRef]
- Rauen, U.; Kerkweg, U.; de Groot, H. Iron-dependent vs. Iron-independent cold-induced injury to cultured rat hepatocytes: A comparative study in physiological media and organ preservation solutions. Cryobiology 2007, 54, 77–86. [Google Scholar] [CrossRef]
- von Horn, C.; Minor, T. Improved approach for normothermic machine perfusion of cold stored kidney grafts. Am. J. Transl. Res. 2018, 10, 1921–1929. [Google Scholar] [PubMed]
- Di Lisa, F.; Menabo, R.; Canton, M.; Barile, M.; Bernardi, P. Opening of the mitochondrial permeability transition pore causes depletion of mitochondrial and cytosolic nad+ and is a causative event in the death of myocytes in postischemic reperfusion of the heart. J. Biol. Chem. 2001, 276, 2571–2575. [Google Scholar] [CrossRef]
- Currin, R.T.; Caldwellkenkel, J.C.; Lichtman, S.N.; Bachmann, S.; Takei, Y.; Kawano, S.; Thurman, R.G.; Lemasters, J.J. Protection by carolina rinse solution, acidotic ph, and glycine against lethal reperfusion injury to sinusoidal endothelial cells of rat livers stored for transplantation. Transplantation 1996, 62, 1549–1558. [Google Scholar] [CrossRef]
- Pediaditakis, P.; Kim, J.S.; He, L.; Zhang, X.; Graves, L.M.; Lemasters, J.J. Inhibition of the mitochondrial permeability transition by protein kinase a in rat liver mitochondria and hepatocytes. Biochem. J. 2010, 431, 411–421. [Google Scholar] [CrossRef]
- Salahudeen, A.K.; Huang, H.; Joshi, M.; Moore, N.A.; Jenkins, J.K. Involvement of the mitochondrial pathway in cold storage and rewarming-associated apoptosis of human renal proximal tubular cells. Am. J. Transpl. 2003, 3, 273–280. [Google Scholar] [CrossRef]
- Minor, T.; Akbar, S.; Tolba, R.; Dombrowski, F. Cold preservation of fatty liver grafts: Prevention of functional and ultrastructural impairments by venous oxygen persufflation. J. Hepatol. 2000, 32, 105–111. [Google Scholar] [CrossRef]
- Kron, P.; Schlegel, A.; de Rougemont, O.; Oberkofler, C.E.; Clavien, P.A.; Dutkowski, P. Short, cool, and well oxygenated—hope for kidney transplantation in a rodent model. Ann. Surg. 2016, 264, 815–822. [Google Scholar] [CrossRef]
- Dutkowski, P.; Polak, W.G.; Muiesan, P.; Schlegel, A.; Verhoeven, C.J.; Scalera, I.; DeOliveira, M.L.; Kron, P.; Clavien, P.-A. First comparison of hypothermic oxygenated perfusion versus static cold storage of human donation after cardiac death liver transplants: An international-matched case analysis. Ann. Surg. 2015, 262, 764–771. [Google Scholar] [CrossRef]
- Schopp, I.; Reissberg, E.; Luer, B.; Efferz, P.; Minor, T. Controlled rewarming after hypothermia: Adding a new principle to renal preservation. Clin. Transl. Sci. 2015, 8, 475–478. [Google Scholar] [CrossRef]
- Hoyer, D.P.; Paul, A.; Luer, S.; Reis, H.; Efferz, P.; Minor, T. End-ischemic reconditioning of liver allografts: Controlling the rewarming. Liver Transpl. 2016, 22, 1223–1230. [Google Scholar] [CrossRef]
- Matsuno, N.; Obara, H.; Watanabe, R.; Iwata, S.; Kono, S.; Fujiyama, M.; Hirano, T.; Kanazawa, H.; Enosawa, S. Rewarming preservation by organ perfusion system for donation after cardiac death liver grafts in pigs. Transpl. Proc. 2014, 46, 1095–1098. [Google Scholar] [CrossRef]
- Mahboub, P.; Ottens, P.; Seelen, M.; t Hart, N.; Van Goor, H.; Ploeg, R.; Martins, P.N.; Leuvenink, H. Gradual rewarming with gradual increase in pressure during machine perfusion after cold static preservation reduces kidney ischemia reperfusion injury. PLoS ONE 2015, 10, e0143859. [Google Scholar] [CrossRef]
- Hoyer, D.P.; Mathe, Z.; Gallinat, A.; Canbay, A.C.; Treckmann, J.W.; Rauen, U.; Paul, A.; Minor, T. Controlled oxygenated rewarming of cold stored livers prior to transplantation: First clinical application of a new concept. Transplantation 2016, 100, 147–152. [Google Scholar] [CrossRef]
- de Vries, Y.; Matton, A.P.M.; Nijsten, M.W.N.; Werner, M.J.M.; van den Berg, A.P.; de Boer, M.T.; Buis, C.I.; Fujiyoshi, M.; de Kleine, R.H.J.; van Leeuwen, O.B.; et al. Pretransplant sequential hypo- and normothermic machine perfusion of suboptimal livers donated after circulatory death using a hemoglobin-based oxygen carrier perfusion solution. Am. J. Transpl. 2018. [Google Scholar] [CrossRef]
- von Horn, C.; Baba, H.A.; Hannaert, P.; Hauet, T.; Leuvenink, H.; Paul, A.; Minor, T.; Partners, C.c. Controlled oxygenated rewarming up to normothermia for pretransplant reconditioning of liver grafts. Clin. Transpl. 2017, 31, e13101. [Google Scholar] [CrossRef]
- Hosgood, S.A.; van Heurn, E.; Nicholson, M.L. Normothermic machine perfusion of the kidney: Better conditioning and repair? Transpl. Int. 2015, 28, 657–664. [Google Scholar] [CrossRef]
- Ceresa, C.D.L.; Nasralla, D.; Coussios, C.C.; Friend, P.J. The case for normothermic machine perfusion in liver transplantation. Liver Transpl. 2018, 24, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Brockmann, J.M.; Reddy, S.F.; Coussios, C.P.; Pigott, D.F.; Guirriero, D.M.; Hughes, D.P.; Morovat, A.P.; Roy, D.F.; Winter, L.M.; Friend, P.J.M. Normothermic perfusion: A new paradigm for organ preservation. [article]. Ann. Surg. 2009, 250, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Nasralla, D.; Coussios, C.C.; Mergental, H.; Akhtar, M.Z.; Butler, A.J.; Ceresa, C.D.L.; Chiocchia, V.; Dutton, S.J.; Garcia-Valdecasas, J.C.; Heaton, N.; et al. A randomized trial of normothermic preservation in liver transplantation. Nature 2018, 557, 50–56. [Google Scholar] [CrossRef]
- Hara, Y.; Akamatsu, Y.; Maida, K.; Kashiwadate, T.; Kobayashi, Y.; Ohuchi, N.; Satomi, S. A new liver graft preparation method for uncontrolled non-heart-beating donors, combining short oxygenated warm perfusion and prostaglandin e1. J. Surg. Res. 2013, 184, 1134–1142. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Ji, F.; Zhang, Z.; Tang, Y.; Yang, L.; Huang, S.; Li, W.; Su, Q.; Xiong, W.; Zhu, Z.; et al. Combined liver-kidney perfusion enhances protective effects of normothermic perfusion on liver grafts from donation after cardiac death. Liver Transpl. 2018, 24, 67–79. [Google Scholar] [CrossRef]
- Minor, T.; Sutschet, K.; Witzke, O.; Paul, A.; Gallinat, A. Prediction of renal function upon reperfusion by ex situ controlled oxygenated rewarming. Eur. J. Clin. Invest. 2016, 46, 1024–1030. [Google Scholar] [CrossRef] [PubMed]
- Minor, T.; von Horn, C.; Paul, A. Role of erythrocytes in short-term rewarming kidney perfusion after cold storage. Artif Organs 2019. [Google Scholar] [CrossRef]
- Kaths, J.M.; Cen, J.Y.; Chun, Y.M.; Echeverri, J.; Linares, I.; Ganesh, S.; Yip, P.; John, R.; Bagli, D.; Mucsi, I.; et al. Continuous normothermic ex vivo kidney perfusion is superior to brief normothermic perfusion following static cold storage in donation after circulatory death pig kidney transplantation. Am. J. Transpl. 2017, 17, 957–969. [Google Scholar] [CrossRef]
- Ciria, R.; Ayllon-Teran, M.D.; Gonzalez-Rubio, S.; Gomez-Luque, I.; Ferrin, G.; Moreno, A.; Sanchez-Frias, M.; Alconchel, F.; Herrera, C.; Martin, V.; et al. Rescue of discarded grafts for liver transplantation by ex vivo subnormothermic and normothermic oxygenated machine perfusion: First experience in spain. Transpl. Proc. 2019, 51, 20–24. [Google Scholar] [CrossRef]
- Okamura, Y.; Hata, K.; Tanaka, H.; Hirao, H.; Kubota, T.; Inamoto, O.; Kageyama, S.; Tamaki, I.; Yermek, N.; Yoshikawa, J.; et al. Impact of subnormothermic machine perfusion preservation in severely steatotic rat livers: A detailed assessment in an isolated setting. Am. J. Transpl. 2017, 17, 1204–1215. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minor, T.; von Horn, C. Rewarming Injury after Cold Preservation. Int. J. Mol. Sci. 2019, 20, 2059. https://doi.org/10.3390/ijms20092059
Minor T, von Horn C. Rewarming Injury after Cold Preservation. International Journal of Molecular Sciences. 2019; 20(9):2059. https://doi.org/10.3390/ijms20092059
Chicago/Turabian StyleMinor, Thomas, and Charlotte von Horn. 2019. "Rewarming Injury after Cold Preservation" International Journal of Molecular Sciences 20, no. 9: 2059. https://doi.org/10.3390/ijms20092059
APA StyleMinor, T., & von Horn, C. (2019). Rewarming Injury after Cold Preservation. International Journal of Molecular Sciences, 20(9), 2059. https://doi.org/10.3390/ijms20092059





