Fulminant MS Reactivation Following Combined Fingolimod Cessation and Yellow Fever Vaccination
Abstract
:1. Introduction
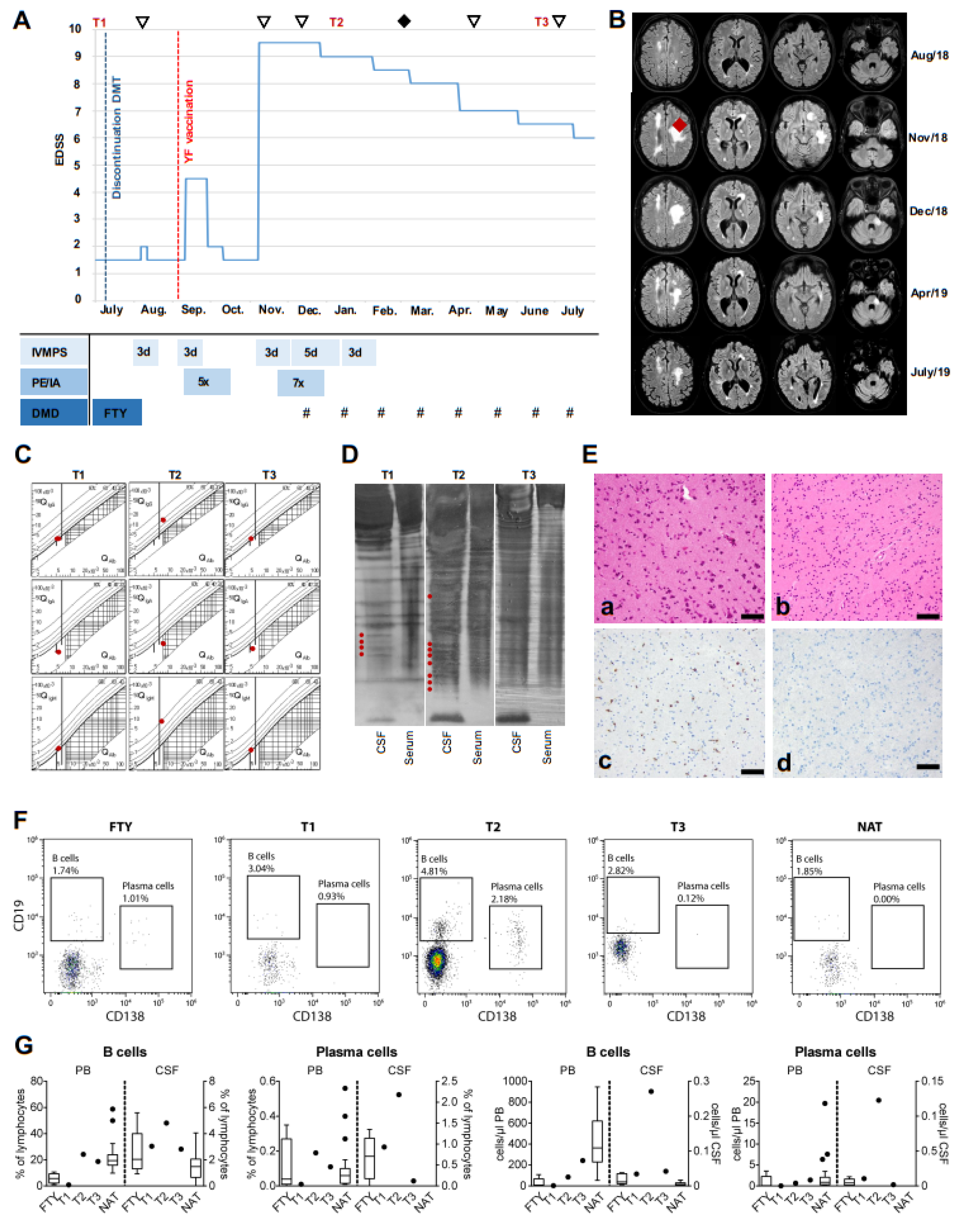
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Author Disclosures
References
- Cohen, J.A.; Khatri, B.; Barkhof, F.; Comi, G.; Hartung, H.-P.; Montalbon, X.; Pelletie, J.; Stites, T.; Ritter, S.; von Rosenstiel, P.; et al. Long-term (up to 4.5 years) treatment with fingolimod in multiple sclerosis: Results from the extension of the randomised TRANSFORMS study. J. Neurol. Neurosurg. Psychiatry 2016, 87, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, P.; Meca-Lallana, V.; Vivancos, J. Tumefactive multiple sclerosis lesions associated with fingolimod treatment: Report of 5 cases. Mult. Scler. Relat. Disord. 2018, 25, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Berger, B.; Baumgartner, A.; Rauer, S.; Mader, I.; Luetzen, N.; Farenkopf, U.; Stich, O. Severe disease reactivation in four patients with relapsing-remitting multiple sclerosis after fingolimod cessation. J. Neuroimmunol. 2015, 282, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Farez, M.F.; Correale, J. Yellow fever vaccination and increased relapse rate in travelers with multiple sclerosis. Arch. Neurol. 2011, 68, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Lueg, G.; Gross, C.C.; Lohmann, H.; Johnen, A.; Kemmling, A.; Deppe, M.; Groger, J.; Minnerup, J.; Wiendl, H.; Meuth, S.G. Clinical relevance of specific T-cell activation in the blood and cerebrospinal fluid of patients with mild Alzheimer’s disease. Neurobiol. Aging 2015, 36, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, S.E.; Waubant, E.; Nourbakhsh, B.; Crabtree-Hartman, E.; Graves, J.S. Rebound Syndrome in Patients with Multiple Sclerosis After Cessation of Fingolimod Treatment. JAMA Neurol. 2016, 73, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Confavreux, C.; Suissa, S.; Saddier, P.; Bourdes, V.; Vukusic, S.; Vaccines in Multiple Sclerosis Study Group. Vaccinations and the risk of relapse in multiple sclerosis. N. Engl. J. Med. 2001, 344, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Farez, M.F.; Correale, J.; Armstrong, M.J.; Rae-Grant, A.; Gloss, D.; Donley, D.; Holler-Managan, Y.; Kachuck, N.J.; Jeffery, D.; Beilman, M. Practice guideline update summary: Vaccine-preventable infections and immunization in multiple sclerosis: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2019, 93, 584–594. [Google Scholar] [CrossRef]
- Loebermann, M.; Winkelmann, A.; Hartung, H.; Hengel, H.; Reisinger, E.C.; Zettl, U.K. Vaccination against infection in patients with multiple sclerosis. Nat. Rev. Neurol. 2012, 8, 143–151. [Google Scholar] [CrossRef]
- Zrzavy, T.; Kollaritsch, H.; Rommer, P.S.; Boxberger, N.; Loebermann, M.; Wimmer, I.; Winkelmann, A.; Zettl, U.K. Vaccination in Multiple Sclerosis: Friend or Foe? Front. Immunol. 2019, 93, 584–594. [Google Scholar] [CrossRef] [PubMed]
| Variables | T1 | T2 | T3 |
|---|---|---|---|
| Lymphocytes (cells/µL) | 1 | 15 | 4 |
| Protein (mg/L) | 425 | 497 | 458 |
| QAlbumin (CSF/Serum) | 5.1 | 7.6 | 5.5 |
| BBB disturbance | no | yes | no |
| QIgG (CSF/Serum) | 3.8 | 14.4 | 3.9 |
| Intrathecal Synthesis (%) | 0 | 60 | 0 |
| QIgA (CSF/Serum) | 1.3 | 2.4 | 1.6 |
| Intrathecal Synthesis (%) | 0 | 0 | 0 |
| QIgM (CSF/Serum) | 1.3 | 8.0 | 1.2 |
| Intrathecal Synthesis (%) | 21 | 77 | |
| Oligoclonal bands | Type II | Type II | Type I |
| QGlucose (CSF/Serum) | 0.51 | 0.53 | 0.56 |
| Lactate (mmol/L) | 1.88 | 2.34 | 1.83 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rolfes, L.; Pawlitzki, M.; Pfeuffer, S.; Thomas, C.; Schmidt-Chanasit, J.; Gross, C.C.; Schulte-Mecklenbeck, A.; Wiendl, H.; Meuth, S.G.; M. Grauer, O.; et al. Fulminant MS Reactivation Following Combined Fingolimod Cessation and Yellow Fever Vaccination. Int. J. Mol. Sci. 2019, 20, 5985. https://doi.org/10.3390/ijms20235985
Rolfes L, Pawlitzki M, Pfeuffer S, Thomas C, Schmidt-Chanasit J, Gross CC, Schulte-Mecklenbeck A, Wiendl H, Meuth SG, M. Grauer O, et al. Fulminant MS Reactivation Following Combined Fingolimod Cessation and Yellow Fever Vaccination. International Journal of Molecular Sciences. 2019; 20(23):5985. https://doi.org/10.3390/ijms20235985
Chicago/Turabian StyleRolfes, Leoni, Marc Pawlitzki, Steffen Pfeuffer, Christian Thomas, Jonas Schmidt-Chanasit, Catharina C. Gross, Andreas Schulte-Mecklenbeck, Heinz Wiendl, Sven G. Meuth, Oliver M. Grauer, and et al. 2019. "Fulminant MS Reactivation Following Combined Fingolimod Cessation and Yellow Fever Vaccination" International Journal of Molecular Sciences 20, no. 23: 5985. https://doi.org/10.3390/ijms20235985
APA StyleRolfes, L., Pawlitzki, M., Pfeuffer, S., Thomas, C., Schmidt-Chanasit, J., Gross, C. C., Schulte-Mecklenbeck, A., Wiendl, H., Meuth, S. G., M. Grauer, O., & Ruck, T. (2019). Fulminant MS Reactivation Following Combined Fingolimod Cessation and Yellow Fever Vaccination. International Journal of Molecular Sciences, 20(23), 5985. https://doi.org/10.3390/ijms20235985






