The Persisting Significance of Oligoclonal Bands in the Dawning Era of Kappa Free Light Chains for the Diagnosis of Multiple Sclerosis
Abstract
:1. Introduction
2. Results
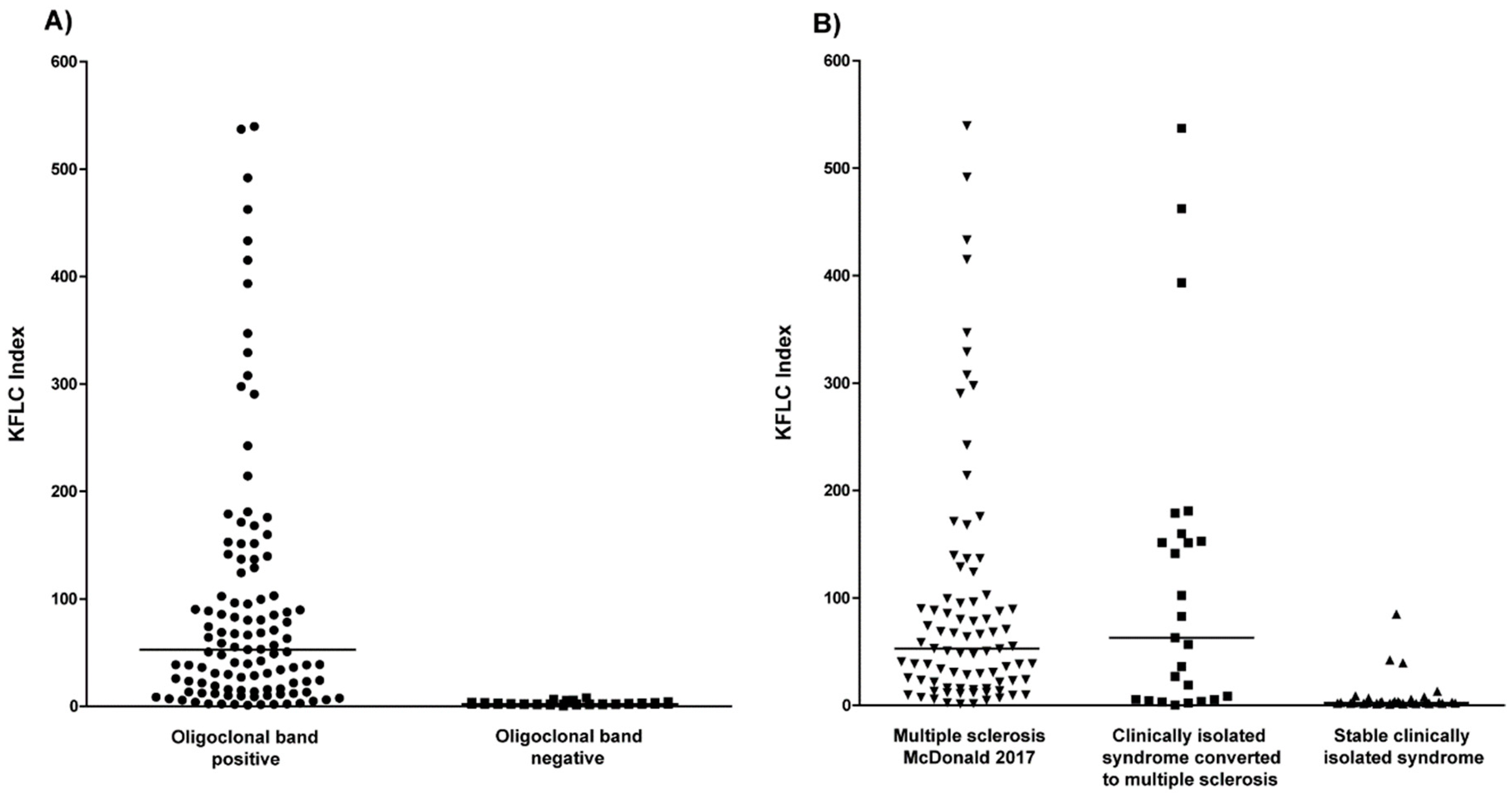
2.1. Oligoclonal Bands in Relation to KFLC Indices in All Patients
2.2. Oligoclonal Bands in Multiple Sclerosis and Clinically Isolated Syndrome
2.3. KFLC Indices in Multiple Sclerosis and Clinically Isolated Syndrome
2.4. KFLC Indices Compared to Oligoclonal Bands in Patients with Multiple Sclerosis
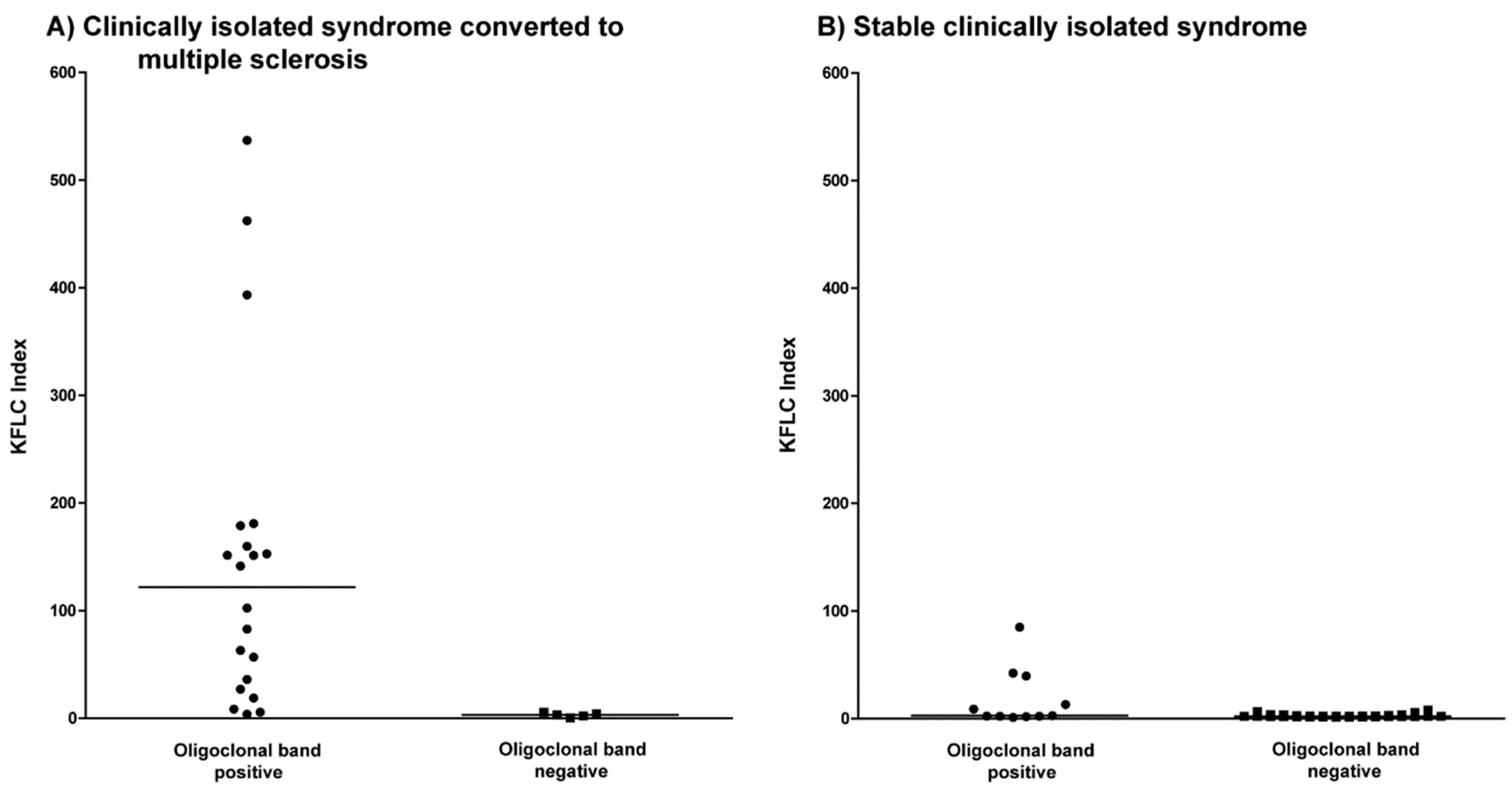
2.5. KFLC Indices Compared to Oligoclonal Bands in Patients with Clinically Isolated Syndrome Who Converted to Multiple Sclerosis
2.6. KFLC Indices Compared to Oligoclonal Bands in Patients with Stable Clinically Isolated Syndrome
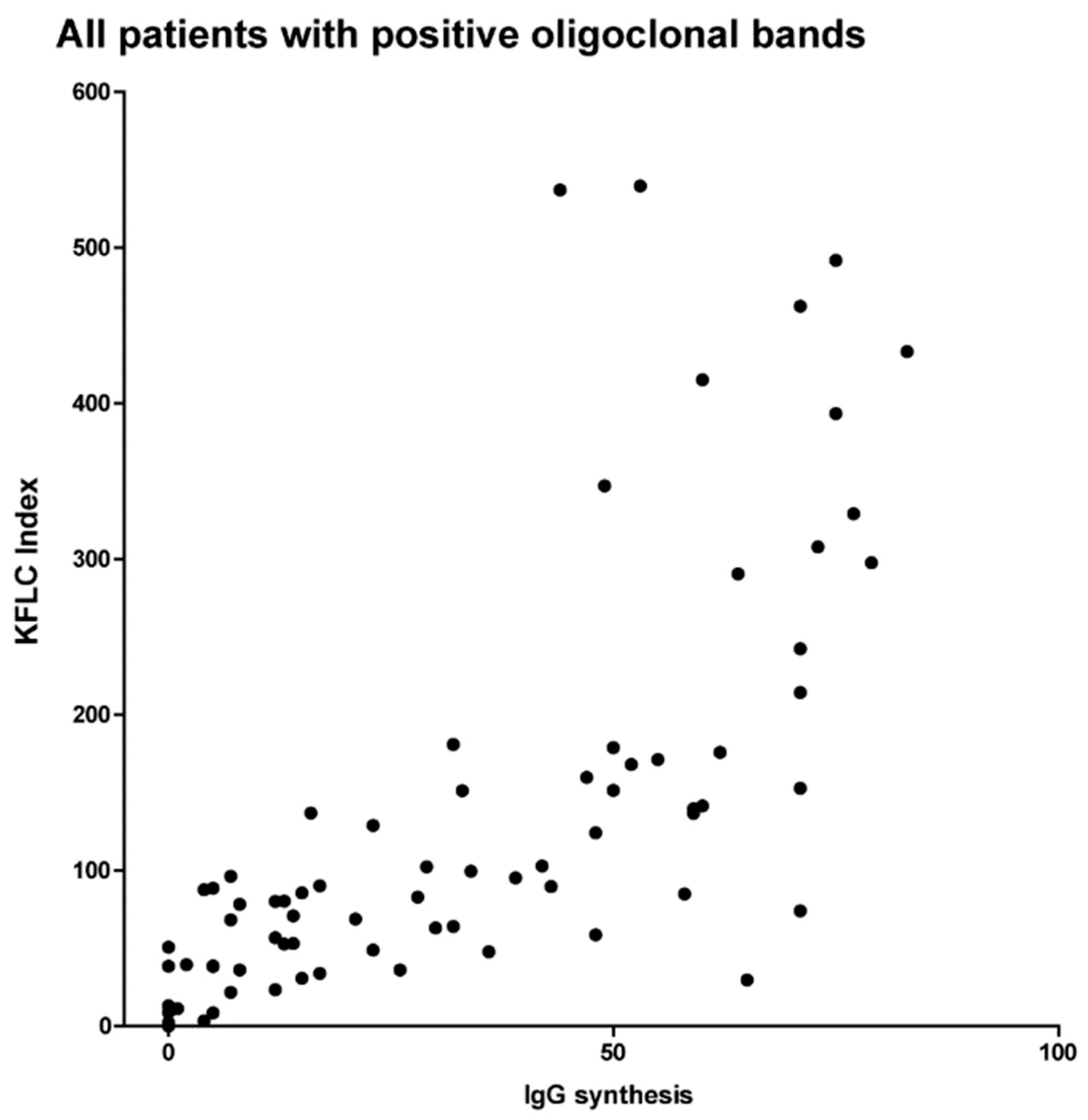
2.7. KFLC Indices Compared to Quantitative IgG Synthesis in Reiber-Graphs
3. Discussion
4. Methods
4.1. Patients
4.2. CSF and Serum Analytical Procedures
4.3. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stangel, M.; Fredrikson, S.; Meinl, E.; Petzold, A.; Stuve, O.; Tumani, H. The utility of cerebrospinal fluid analysis in patients with multiple sclerosis. Nat. Rev. Neurol. 2013, 9, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Petzold, A. Intrathecal oligoclonal IgG synthesis in multiple sclerosis. J. Neuroimmunol. 2013, 262, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2017, 17, 162–173. [Google Scholar] [CrossRef]
- Senel, M.; Tumani, H.; Lauda, F.; Presslauer, S.; Mojib-Yezdani, R.; Otto, M.; Brettschneider, J. Cerebrospinal fluid immunoglobulin kappa light chain in clinically isolated syndrome and multiple sclerosis. PLoS ONE 2014, 9, e88680. [Google Scholar] [CrossRef] [PubMed]
- Susse, M.; Hannich, M.; Petersmann, A.; Zylla, S.; Pietzner, M.; Nauck, M.; Dressel, A. Kappa free light chains in cerebrospinal fluid to identify patients with oligoclonal bands. Eur. J. Neurol. 2018, 25, 1134–1139. [Google Scholar] [CrossRef] [PubMed]
- Presslauer, S.; Milosavljevic, D.; Huebl, W.; Aboulenein-Djamshidian, F.; Krugluger, W.; Deisenhammer, F.; Senel, M.; Tumani, H.; Hegen, H. Validation of kappa free light chains as a diagnostic biomarker in multiple sclerosis and clinically isolated syndrome: A multicenter study. Mult. Scler. 2016, 22, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Bourahoui, A.; De Seze, J.; Guttierez, R.; Onraed, B.; Hennache, B.; Ferriby, D.; Stojkovic, T.; Vermersch, P. CSF isoelectrofocusing in a large cohort of MS and other neurological diseases. Eur. J. Neurol. 2004, 11, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.; Arneth, B.; Koehler, J.; Lotz, J.; Lackner, K.J. Kappa free light chains in cerebrospinal fluid as markers of intrathecal immunoglobulin synthesis. Clin. Chem. 2004, 50, 1809–1813. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, B.; Aizenbud, B.M.; Golderman, S.; Yaskariev, R.; Sela, B.A. Free light chain monomers in the diagnosis of multiple sclerosis. J. Neuroimmunol. 2010, 229, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, M.; Schaldemose Nielsen, H.; Jensen, J.; Sellebjerg, F. Intrathecal synthesis of free immunoglobulin light chains in multiple sclerosis. Acta Neurol. Scand. 1998, 98, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Meinl, E.; Derfuss, T.; Krumbholz, M.; Probstel, A.K.; Hohlfeld, R. Humoral autoimmunity in multiple sclerosis. J. Neurol. Sci. 2011, 306, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Presslauer, S.; Milosavljevic, D.; Brucke, T.; Bayer, P.; Hubl, W. Elevated levels of kappa free light chains in CSF support the diagnosis of multiple sclerosis. J. Neurol. 2008, 255, 1508–1514. [Google Scholar] [CrossRef] [PubMed]
- Rudick, R.A.; French, C.A.; Breton, D.; Williams, G.W. Relative diagnostic value of cerebrospinal fluid kappa chains in MS: Comparison with other immunoglobulin tests. Neurology 1989, 39, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Crespi, I.; Sulas, M.G.; Mora, R.; Naldi, P.; Vecchio, D.; Comi, C.; Cantello, R.; Bellomo, G. Combined use of Kappa Free Light Chain Index and Isoelectrofocusing of Cerebro-Spinal Fluid in Diagnosing Multiple Sclerosis: Performances and Costs. Clin. Lab. 2017, 63, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Wurster, U. Elektrophoreseverfahren—Nachweis und Bedeutung von oligoklonalen Banden. In Klinische Liquordiagnostik; Zettl, U.K., Lehmitz, R., Mix, E., Eds.; Walter de Gruyter: Berlin, Germany, 2005; Volume 2, pp. 208–238. [Google Scholar]
- Link, H.; Huang, Y.M. Oligoclonal bands in multiple sclerosis cerebrospinal fluid: An update on methodology and clinical usefulness. J. Neuroimmunol. 2006, 180, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Wurster, U.; Stachan, R.; Windhagen, A.; Petereit, H.F.; Leweke, F.M. Reference values for standard cerebrospinal fluid examinations in multiple sclerosis. Results from 99 healthy volunteers. Mult Scler 2006, 12, 1–228. [Google Scholar]
- Rathbone, E.; Durant, L.; Kinsella, J.; Parker, A.R.; Hassan-Smith, G.; Douglas, M.R.; Curnow, S.J. Cerebrospinal fluid immunoglobulin light chain ratios predict disease progression in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2018, 89, 1044–1049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwenkenbecher, P.; Sarikidi, A.; Bonig, L.; Wurster, U.; Bronzlik, P.; Suhs, K.W.; Pul, R.; Stangel, M.; Skripuletz, T. Clinically Isolated Syndrome According to McDonald 2010: Intrathecal IgG Synthesis Still Predictive for Conversion to Multiple Sclerosis. Int. J. Mol. Sci. 2017, 18, 2061. [Google Scholar] [CrossRef] [PubMed]
- Schwenkenbecher, P.; Sarikidi, A.; Wurster, U.; Bronzlik, P.; Suhs, K.W.; Raab, P.; Stangel, M.; Pul, R.; Skripuletz, T. McDonald Criteria 2010 and 2005 Compared: Persistence of High Oligoclonal Band Prevalence Despite Almost Doubled Diagnostic Sensitivity. Int. J. Mol. Sci. 2016, 17, 1592. [Google Scholar] [CrossRef] [PubMed]
- Reiber, H. Cerebrospinal fluid—Physiology, analysis and interpretation of protein patterns for diagnosis of neurological diseases. Mult. Scler. 1998, 4, 99–107. [Google Scholar] [PubMed]
- Andersson, M.; Alvarez-Cermeno, J.; Bernardi, G.; Cogato, I.; Fredman, P.; Frederiksen, J.; Fredrikson, S.; Gallo, P.; Grimaldi, L.M.; Gronning, M.; et al. Cerebrospinal fluid in the diagnosis of multiple sclerosis: A consensus report. J. Neurol. Neurosurg. Psychiatry 1994, 57, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Reiber, H. External quality assessment in clinical neurochemistry: Survey of analysis for cerebrospinal fluid (CSF) proteins based on CSF/serum quotients. Clin. Chem. 1995, 41, 256–263. [Google Scholar] [PubMed]
| Characteristics | Multiple Sclerosis McDonald 2017 | Clinically Isolated Syndrome Converted to Multiple Sclerosis | Stable Clinically Isolated Syndrome |
|---|---|---|---|
| Females, n (%) | 57/83 (69%) | 16/25 (64%) | 27/41 (66%) |
| Age, years (range) | 31 (17–73) | 33 (17–73) | 37 (16–54) |
| Optic neuritis, n (%) | 34/83 (41%) | 10/25 (40%) | 38/41 (93%) |
| Paresis/sensory symptoms, n (%) | 13/83 (16%) | 3/25 (12%) | 2/41 (5%) |
| Brainstem symptoms, n (%) | 14/83 (17%) | 4/25 (16%) | 1/41 (2%) |
| Spinal cord symptoms, n (%) | 15/83 (18%) | 8/25 (32%) | 0 |
| Polysymptomatic, n (%) | 7/83 (8%) | 0 | 0 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwenkenbecher, P.; Konen, F.F.; Wurster, U.; Jendretzky, K.F.; Gingele, S.; Sühs, K.-W.; Pul, R.; Witte, T.; Stangel, M.; Skripuletz, T. The Persisting Significance of Oligoclonal Bands in the Dawning Era of Kappa Free Light Chains for the Diagnosis of Multiple Sclerosis. Int. J. Mol. Sci. 2018, 19, 3796. https://doi.org/10.3390/ijms19123796
Schwenkenbecher P, Konen FF, Wurster U, Jendretzky KF, Gingele S, Sühs K-W, Pul R, Witte T, Stangel M, Skripuletz T. The Persisting Significance of Oligoclonal Bands in the Dawning Era of Kappa Free Light Chains for the Diagnosis of Multiple Sclerosis. International Journal of Molecular Sciences. 2018; 19(12):3796. https://doi.org/10.3390/ijms19123796
Chicago/Turabian StyleSchwenkenbecher, Philipp, Franz Felix Konen, Ulrich Wurster, Konstantin Fritz Jendretzky, Stefan Gingele, Kurt-Wolfram Sühs, Refik Pul, Torsten Witte, Martin Stangel, and Thomas Skripuletz. 2018. "The Persisting Significance of Oligoclonal Bands in the Dawning Era of Kappa Free Light Chains for the Diagnosis of Multiple Sclerosis" International Journal of Molecular Sciences 19, no. 12: 3796. https://doi.org/10.3390/ijms19123796
APA StyleSchwenkenbecher, P., Konen, F. F., Wurster, U., Jendretzky, K. F., Gingele, S., Sühs, K.-W., Pul, R., Witte, T., Stangel, M., & Skripuletz, T. (2018). The Persisting Significance of Oligoclonal Bands in the Dawning Era of Kappa Free Light Chains for the Diagnosis of Multiple Sclerosis. International Journal of Molecular Sciences, 19(12), 3796. https://doi.org/10.3390/ijms19123796







