The Prognostic Value of the Combination of Low VEGFR-1 and High VEGFR-2 Expression in Endothelial Cells of Colorectal Cancer
Abstract
1. Introduction
2. Results
2.1. Study Population
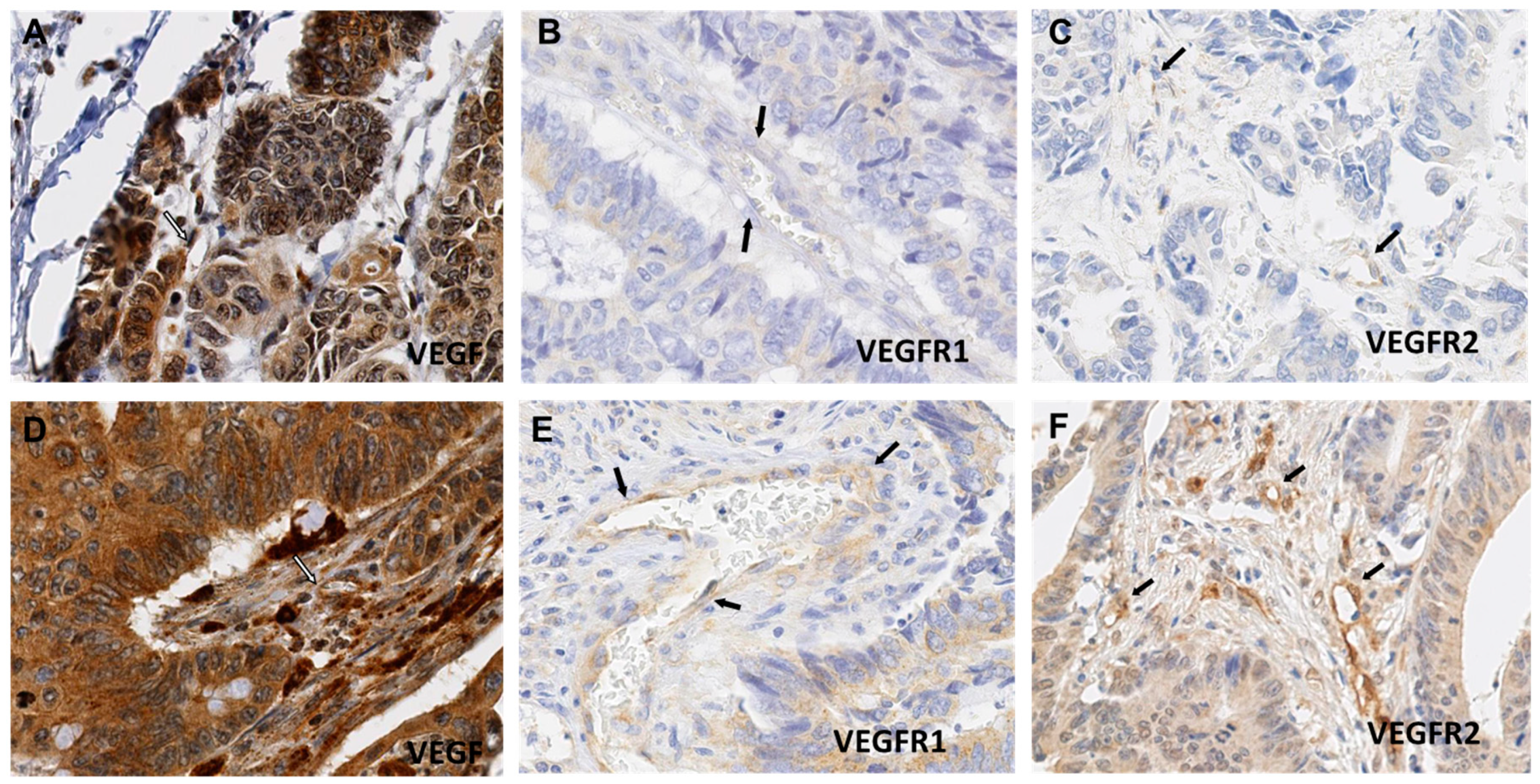
2.2. VEGF, VEGFR-1 and VEGFR-2 Expression in CRC ECs
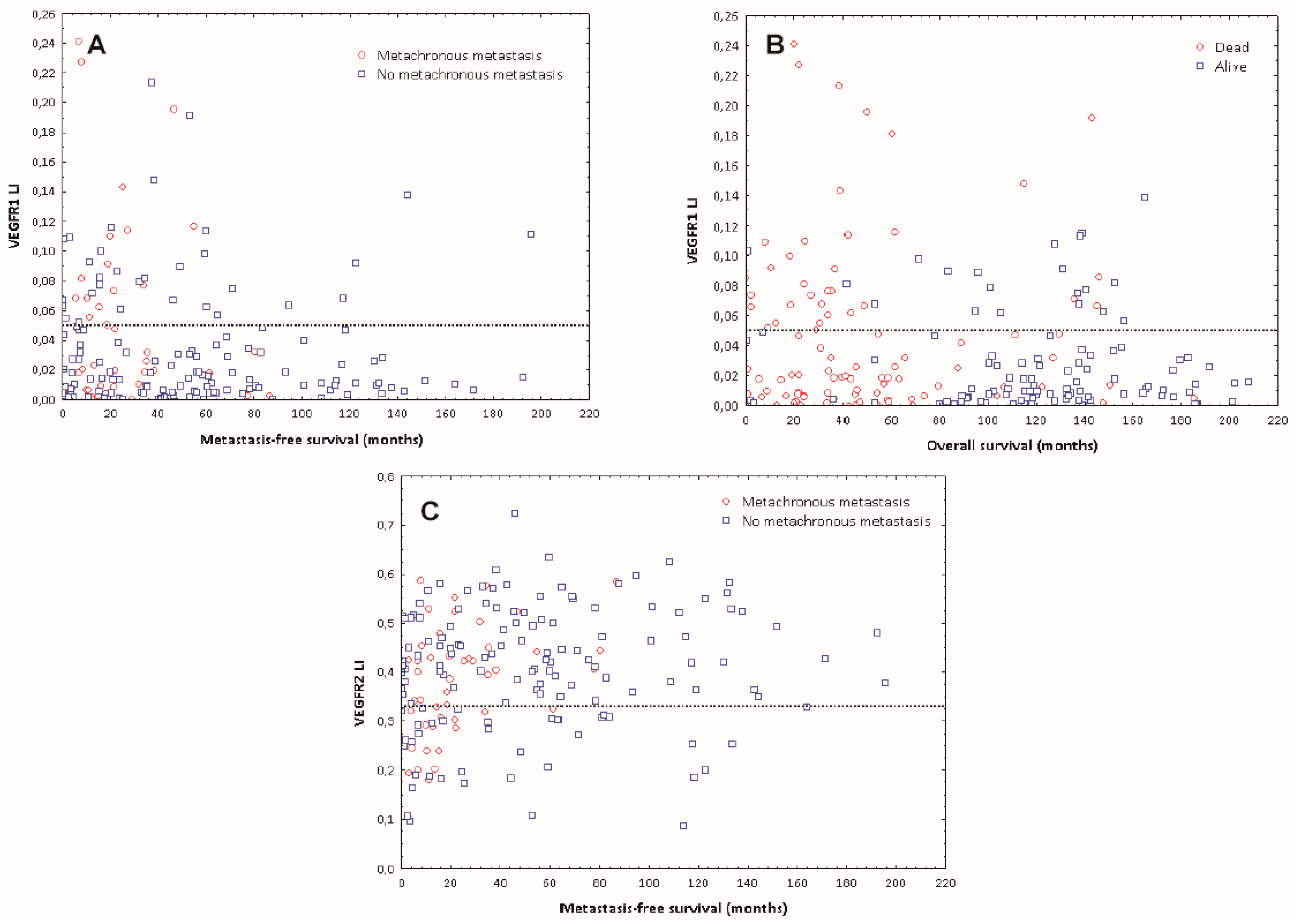
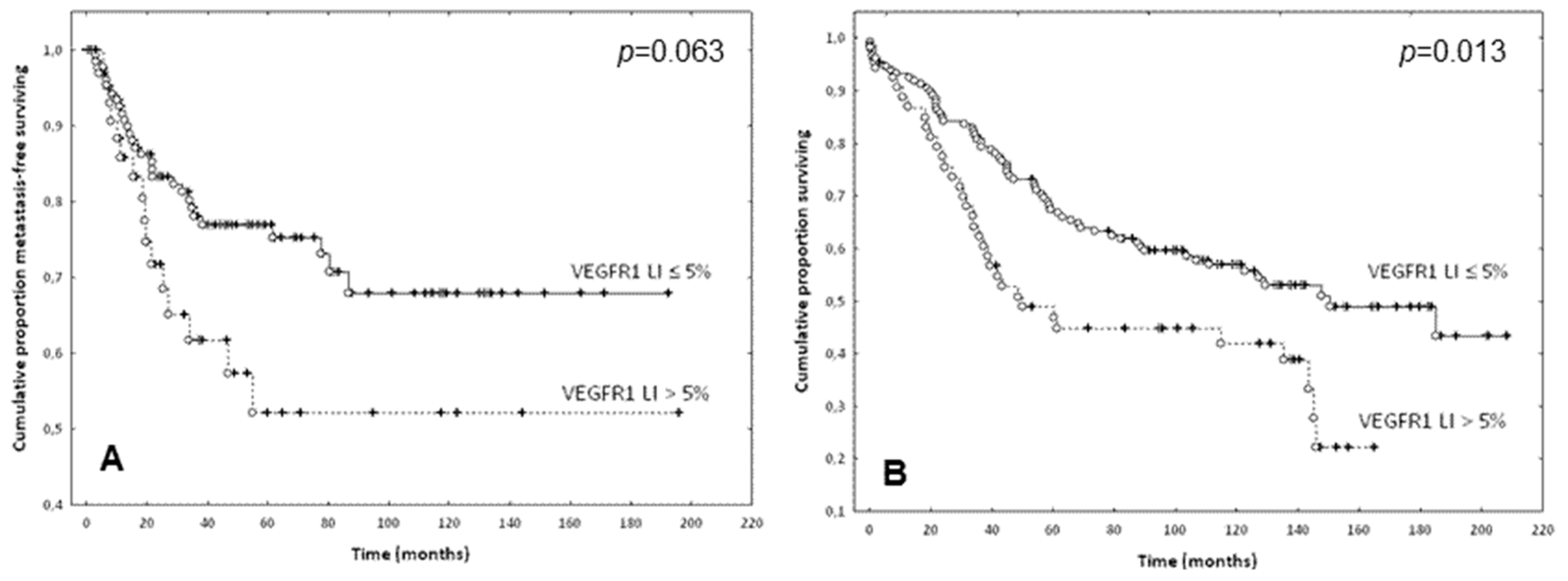
2.3. Prognostic Evaluation of VEGF, VEGFR-1 and VEGFR-2 Expression in ECs of CRCs
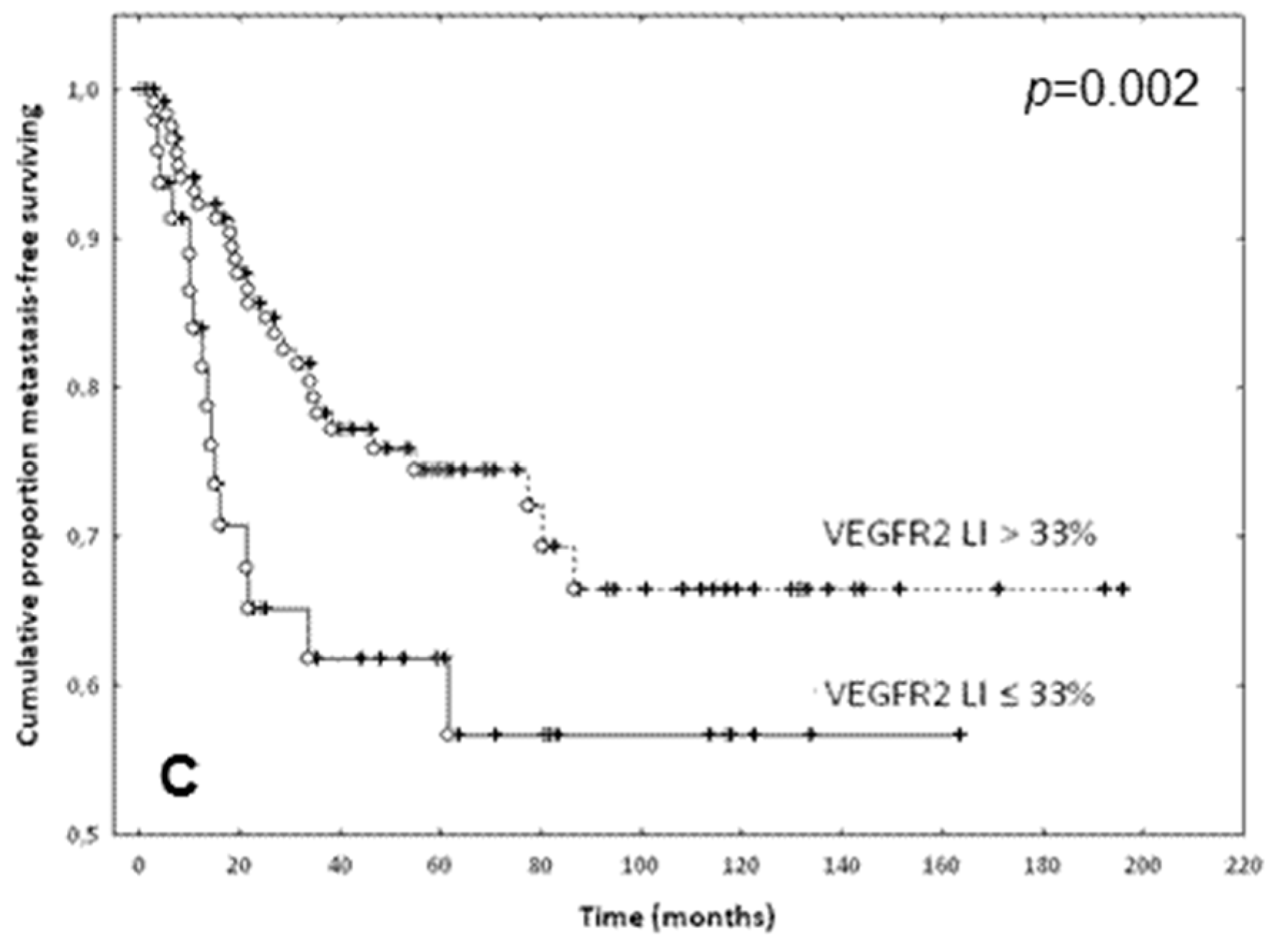
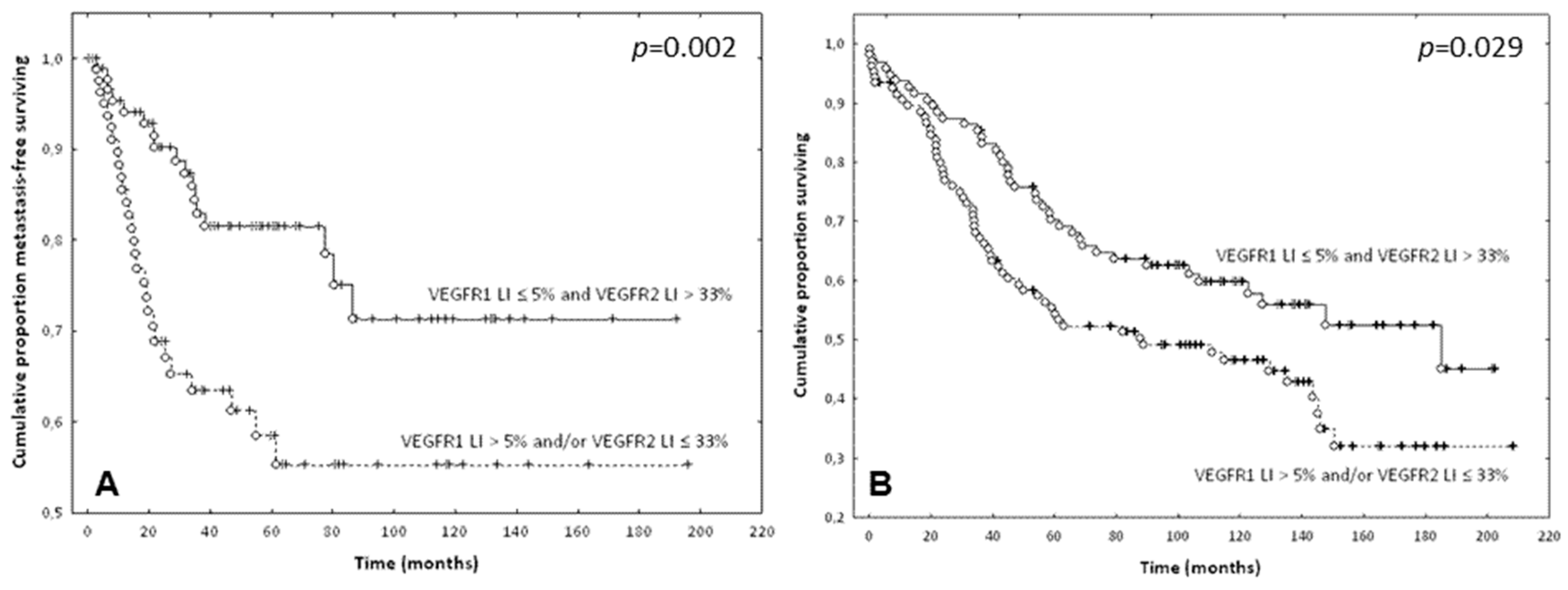
- The first group included cases with a VEGFR-1 LI ≤ 5% and a VEGFR-2 LI > 33% (n = 101)
- The second group included cases with a VEGFR-1 LI > 5% and/or a VEGFR-2 LI ≤ 33% (n = 103).
3. Discussion
4. Materials and Methods
4.1. Patient Data and Tissue Microarray (TMA) Design
4.2. Immunohistochemistry
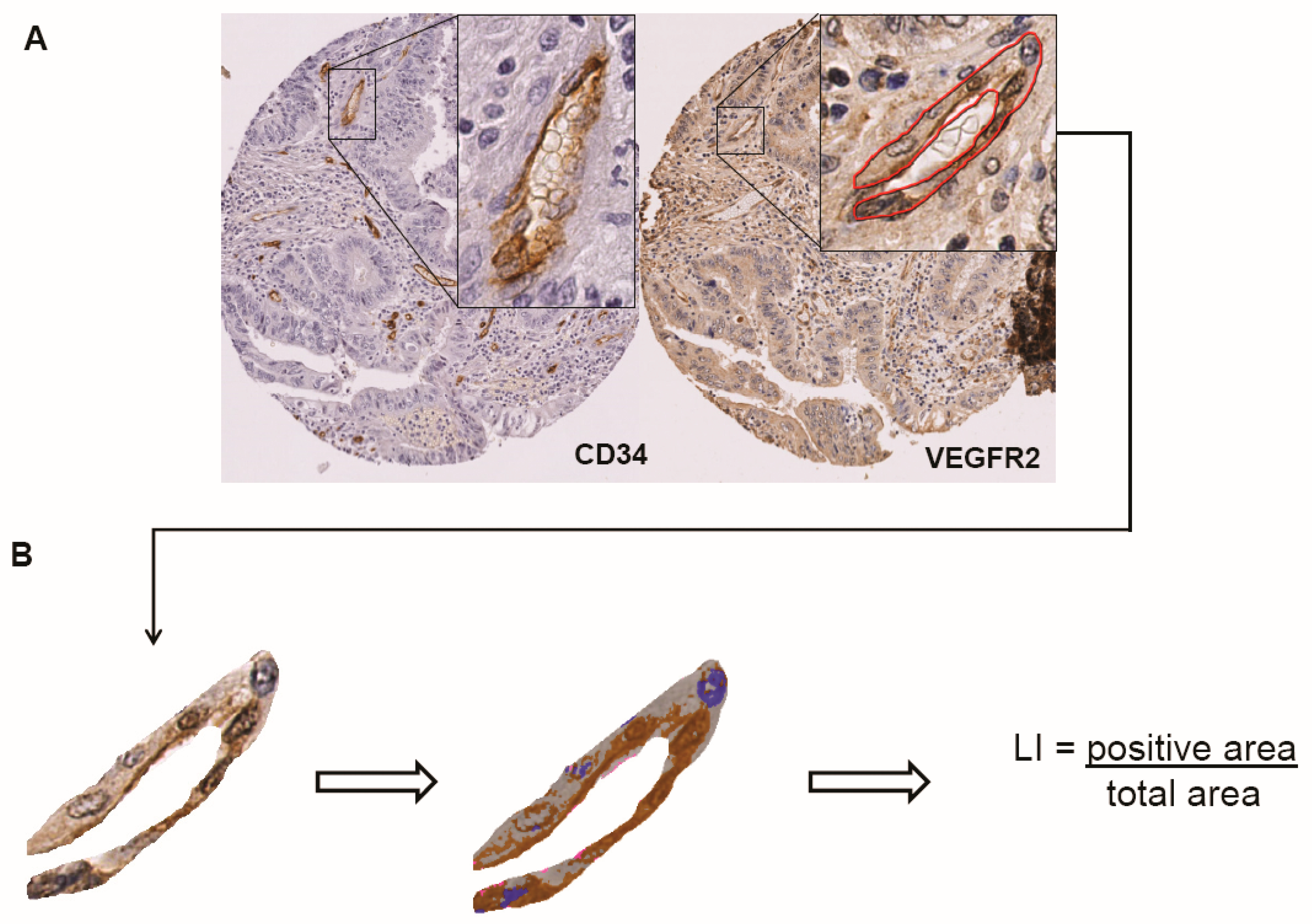
4.3. Quantitative Image Analysis
4.4. Statistical Analyses
Author Contributions
Funding
Conflicts of Interest
References
- Carmeliet, P.; Jain, R.K. Angiogenesis in cancer and other diseases. Nature 2000, 407, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Sun, W. Angiogenesis in metastatic colorectal cancer and the benefits of targeted therapy. J. Hematol. Oncol. 2012, 5, 63. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Neiva, K.G.; Lingen, M.W.; Ellis, L.M.; Nör, J.E. VEGF-dependent tumor angiogenesis requires inverse and reciprocal regulation of VEGFR-1 and VEGFR-2. Cell Death Differ. 2010, 17, 499–512. [Google Scholar] [CrossRef] [PubMed]
- Luttun, A.; Autiero, M.; Tjwa, M.; Carmeliet, P. Genetic dissection of tumor angiogenesis: Are PlGF and VEGFR-1 novel anti-cancer targets? Biochim. Biophys. Acta 2004, 1654, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Kerbel, R.S. Tumor angiogenesis. N. Engl. J. Med. 2008, 358, 2039–2049. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.; Mazzone, M.; Jonckx, B.; Carmeliet, P. FLT1 and its ligands VEGFB and PlGF: Drug targets for anti-angiogenic therapy? Nat. Rev. Cancer 2008, 8, 942–956. [Google Scholar] [CrossRef] [PubMed]
- Tammela, T.; Zarkada, G.; Wallgard, E.; Murtomäki, A.; Suchting, S.; Wirzenius, M.; Waltari, M.; Hellström, M.; Schomber, T.; Peltonen, R.; et al. Blocking VEGFR-3 suppresses angiogenic sprouting and vascular network formation. Nature 2008, 454, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Moens, S.; Goveia, J.; Stapor, P.C.; Cantelmo, A.R.; Carmeliet, P. The multifaceted activity of VEGF in angiogenesis—Implications for therapy responses. Cytokine Growth Factor Rev. 2014, 25, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Prenen, H.; Tejpar, S.; Van Cutsem, E. Impact of molecular markers on treatment selection in advanced colorectal cancer. Eur. J. Cancer 2009, 45 (Suppl. 1), 70–78. [Google Scholar] [CrossRef]
- Angelucci, A.; Delle Monache, S.; Cortellini, A.; Di Padova, M.; Ficorella, C. “Vessels in the Storm”: Searching for Prognostic and Predictive Angiogenic Factors in Colorectal Cancer. Int. J. Mol. Sci. 2018, 19. [Google Scholar] [CrossRef] [PubMed]
- Aird, W.C. Molecular heterogeneity of tumor endothelium. Cell Tissue Res. 2009, 335, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Patten, S.G.; Adamcic, U.; Lacombe, K.; Minhas, K.; Skowronski, K.; Coomber, B.L. VEGFR-2 heterogeneity and response to anti-angiogenic low dose metronomic cyclophosphamide treatment. BMC Cancer 2010, 10, 683. [Google Scholar] [CrossRef] [PubMed]
- Fathers, K.E.; Stone, C.M.; Minhas, K.; Marriott, J.J.; Greenwood, J.D.; Dumont, D.J.; Coomber, B.L. Heterogeneity of Tie2 expression in tumor microcirculation: Influence of cancer type, implantation site, and response to therapy. Am. J. Pathol. 2005, 167, 1753–1762. [Google Scholar] [CrossRef]
- Lee, S.H.; Jeong, D.; Han, Y.S.; Baek, M.J. Pivotal role of vascular endothelial growth factor pathway in tumor angiogenesis. Ann. Surg. Treat. Res. 2015, 89, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jayasinghe, C.; Simiantonaki, N.; Michel-Schmidt, R.; Kirkpatrick, C.J. Endothelial VEGFR-3 expression in colorectal carcinomas is associated with hematogenous metastasis. Oncol. Rep. 2009, 22, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Talagas, M.; Uguen, A.; Garlantezec, R.; Fournier, G.; Doucet, L.; Gobin, E.; Marcorelles, P.; Volant, A.; De Braekeleer, M. VEGFR-1 and NRP1 endothelial expressions predict distant relapse after radical prostatectomy in clinically localized prostate cancer. Anticancer Res. 2013, 33, 2065–2075. [Google Scholar] [PubMed]
- Eppenberger, M.; Zlobec, I.; Baumhoer, D.; Terracciano, L.; Lugli, A. Role of the VEGF ligand to receptor ratio in the progression of mismatch repair-proficient colorectal cancer. BMC Cancer 2010, 10, 93. [Google Scholar] [CrossRef] [PubMed]
- Simiantonaki, N.; Taxeidis, M.; Jayasinghe, C.; Kirkpatrick, C.J. Epithelial Expression of VEGF Receptors in Colorectal Carcinomas and their Relationship to Metastatic Status. Anticancer Res. 2007, 3250, 3245–3250. [Google Scholar]
- Zhang, S.D.; McCrudden, C.M.; Kwok, H.F. Prognostic significance of combining VEGFA, FLT1 and KDR mRNA expression in lung cancer. Oncol. Lett. 2015, 10, 1893–1901. [Google Scholar] [CrossRef] [PubMed]
- Carrillo de Santa Pau, E.; Arias, F.C.; Caso Peláez, E.; Muñoz Molina, G.M.; Sánchez Hernández, I.; Muguruza Trueba, I.; Moreno Balsalobre, R.; Sacristán López, S.; Gómez Pinillos, A.; del Val Toledo Lobo, M. Prognostic significance of the expression of vascular endothelial growth factors A, B, C, and D and their receptors R1, R2, and R3 in patients with nonsmall cell lung cancer. Cancer 2009, 115, 1701–1712. [Google Scholar] [CrossRef] [PubMed]
- Linardou, H.; Kalogeras, K.T.; Kronenwett, R.; Kouvatseas, G.; Wirtz, R.M.; Zagouri, F.; Gogas, H.; Christodoulou, C.; Koutras, A.K.; Samantas, E.; et al. The prognostic and predictive value of mRNA expression of vascular endothelial growth factor family members in breast cancer: A study in primary tumors of high-risk early breast cancer patients participating in a randomized Hellenic Cooperative Oncology Group trial. Breast Cancer Res. 2012, 14, R145. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.C.; Goekkurt, E.; Danenberg, P.V.; Lehmann, S.; Ehninger, G.; Aust, D.E.; Stoehlmacher-Williams, J. EGFR, FLT1 and heparanase as markers identifying patients at risk of short survival in cholangiocarcinoma. PLoS ONE 2013, 8, e64186. [Google Scholar] [CrossRef] [PubMed]
- Gratzinger, D.A.; Advani, R.; Zhao, S.; Talreja, N.; Tibshirani, R.; Shyam, R.; Horning, R.; Sehn, L.H.; Farinha, P.; Briones, J.R.; et al. Lymphoma cell VEGFR-2 expression detected by immunohistochemistry predicts poor overall survival in diffuse large B cell lymphoma treated with immunochemotherapy (R-CHOP). Br. J. Haematol. 2010, 148, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Mehta, S.; Haque, I.; Sengupta, K.; Dhar, K.; Kambhampati, S.; Van Veldhuizen, P.J.; Banerjee, S.K. VEGF-A165 induces human aortic smooth muscle cell migration by activating neuropilin-1-VEGFR-1-PI3K axis. Biochemistry 2008, 47, 3345–3351. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.H.; Ying, N.W.; Hong, T.M.; Chiang, W.F.; Lin, Y.T.; Chen, Y.L. Galectin-1 induces vascular permeability through the neuropilin-1/vascular endothelial growth factor receptor-1 complex. Angiogenesis 2014, 17, 839–849. [Google Scholar] [CrossRef] [PubMed]
- Hiratsuka, S.; Nakamura, K.; Iwai, S.; Murakami, M.; Itoh, T.; Kijima, H.; Shipley, J.M.; Senior, R.M.; Shibuya, M. MMP9 induction by vascular endothelial growth factor receptor-1 is involved in lung-specific metastasis. Cancer Cell 2002, 2, 289–300. [Google Scholar] [CrossRef]
- Kaplan, R.N.; Riba, R.D.; Zacharoulis, S.; Bramley, A.H.; Vincent, L.; Costa, C.; MacDonald, D.D.; Jin, D.K.; Shido, K.; Kerns, S.A.; et al. VEGFR-1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 2005, 438, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Raza, A.; Franklin, M.J.; Dudek, A.Z. Pericytes and vessel maturation during tumor angiogenesis and metastasis. Am. J. Hematol. 2010, 85, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, C.S.; Tabernero, J.; Tomášek, J.; Chau, I.; Melichar, B.; Safran, H.; Tehfe, MA.; Filip, D.; Topuzov, E.; Schlittler, L.; et al. Biomarker analyses in REGARD gastric/GEJ carcinoma patients treated with VEGFR-2-targeted antibody ramucirumab. Br. J. Cancer 2016, 115, 974–982. [Google Scholar] [CrossRef] [PubMed]
- El-Khoueiry, A.B.; Pohl, A.; Danenberg, K.D.; Cooc, J.; Zhang, W.; Yang, D.; Singh, H.; Shriki, J.E.; Iqbal, S.; Lenz, H.-J. Wt Kras and gene expression levels of VEGFR-2, EGFR, and ERCC-1 associated with progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC) treated with first-line 5-FU or capecitabine with oxaliplatin and bevacizumab (FOLFOX). J. Clin. Oncol. 2009, 27, 15. [Google Scholar] [CrossRef]
- Shah, C.H.; Viktorsson, K.; Kanter, L.; Sherif, A.; Asmundsson, J.; Rosenblatt, R.; Lewensohn, R.; Ullén, A. Vascular endothelial growth factor receptor 2, but not S100A4 or S100A6, correlates with prolonged survival in advanced urothelial carcinoma. Urol. Oncol. 2014, 32, 1215–1224. [Google Scholar] [CrossRef] [PubMed]
- Akhavan-Sigari, R.; Gaab, M.R.; Rohde, V.; Abili, M.; Ostertag, H. Prognostic significance of immunohistochemical expression of VEGFR-2 and iNOS in spinal chordoma. Eur. Spine J. 2014, 23, 2416–2422. [Google Scholar] [CrossRef] [PubMed]
- Holzer, T.R.; Fulford, A.D.; Nedderman, D.M.; Umberger, T.S.; Hozak, R.R.; Joshi, A.; Melemed, S.A.; Benjamin, L.E.; Plowman, G.D.; Schade, A.E.; et al. Tumor cell expression of vascular endothelial growth factor receptor 2 is an adverse prognostic factor in patients with squamous cell carcinoma of the lung. PLoS ONE 2013, 8, e80292. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zhang, X.; Tang, Q.; Zhang, F.; Li, Y.; Feng, Z.; Zhu, J. Prognostic significance and potential therapeutic target of VEGFR-2 in hepatocellular carcinoma. J. Clin. Pathol. 2011, 64, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Kuczynski, E.A.; Patten, S.G.; Coomber, B.L. VEGFR-2 expression and TGF-β signaling in initial and recurrent high-grade human glioma. Oncology 2011, 81, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Tabernero, J.; Yoshino, T.; Cohn, A.L.; Obermannova, R.; Bodoky, G.; Garcia-Carbonero, R.; Ciuleanu, T.E.; Portnoy, D.C.; Van Cutsem, E.; Grothey, A.; et al. Ramucirumab versus placebo in combination with second-line FOLFIRI in patients with metastatic colorectal carcinoma that progressed during or after first-line therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine (RAISE): A randomised, double-blind, multicentre, phase 3 study. Lancet Oncol. 2015, 16, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Ulyatt, C.; Walker, J.; Ponnambalam, S. Hypoxia differentially regulates VEGFR-1 and VEGFR-2 levels and alters intracellular signaling and cell migration in endothelial cells. Biochem. Biophys. Res. Commun. 2011, 404, 774–779. [Google Scholar] [CrossRef] [PubMed]
- Imoukhuede, P.I.; Popel, A.S. Quantification and cell-to-cell variation of vascular endothelial growth factor receptors. Exp. Cell Res. 2011, 317, 955–965. [Google Scholar] [CrossRef] [PubMed]
- Des Guetz, G.; Uzzan, B.; Nicolas, P.; Cucherat, M.; Morere, J.-F.; Benamouzig, R.; Breau, J.-L.; Perret, G.-Y. Microvessel density and VEGF expression are prognostic factors in colorectal cancer. Meta-analysis of the literature. Br. J. Cancer 2006, 94, 1823–1832. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.R.; Dawson, S.J.; Blows, F.M.; Provenzano, E.; Leung, S.; Nielsen, T.; Pharoah, P.D.; Caldas, C. A Ki67/BCL2 index based on immunohistochemistry is highly prognostic in ER-positive breast cancer. J. Pathol. 2012, 226, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Qin, R.; Smyrk, T.C.; Reed, N.R.; Schmidt, R.L.; Schnelldorfer, T.; Chari, S.T.; Petersen, G.M.; Tang, A.H. Combining clinicopathological predictors and molecular biomarkers in the oncogenic K-RAS/Ki67/HIF-1α pathway to predict survival in resectable pancreatic cancer. Br. J. Cancer 2015, 112, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhao, C.; Wang, L.; Cao, X.; Li, J.; Huang, R.; Lao, Q.; Yu, H.; Li, Y.; Du, H.; et al. A VEGFR-1 antagonistic peptide inhibits tumor growth and metastasis through VEGFR-1-PI3K-AKT signaling pathway inhibition. Am. J. Cancer Res. 2015, 5, 3149–3161. [Google Scholar] [PubMed]
- Decaestecker, C.; Lopez, X.M.; D’Haene, N.; Roland, I.; Guendouz, S.; Duponchelle, C.; Berton, A.; Debeir, O.; Salmon, I. Requirements for the valid quantification of immunostains on tissue microarray materials using image analysis. Proteomics 2009, 9, 4478–4494. [Google Scholar] [CrossRef] [PubMed]
- Allard, J.; Li, K.; Lopez, X.M.; Blanchard, S.; Barbot, P.; Rorive, S.; Decaestecker, C.; Pochet, R.; Bohl, D.; Lepore, A.C.; et al. Immunohistochemical toolkit for tracking and quantifying xenotransplanted human stem cells. Regen. Med. 2014, 9, 437–452. [Google Scholar] [CrossRef] [PubMed]
- D’Haene, N.; Maris, C.; Sandras, F.; Dehou, M.F.; Remmelink, M.; Decaestecker, C.; Salmon, I. The differential expression of Galectin-1 and Galectin-3 in normal lymphoid tissue and non-Hodgkin’s and Hodgkin’s lymphomas. Int. J. Immunopathol. Pharmacol. 2005, 18, 431–443. [Google Scholar] [CrossRef] [PubMed]
| VEGFR1/VEGFR2 Analysis (n = 204) | VEGF Analysis (n = 130) | |||||||
|---|---|---|---|---|---|---|---|---|
| Feature | No. of Patients | VEGFR-1 LI (mean ± SD) | p | VEGFR-2 LI (mean ± SD) | p | No. of Patients | VEGF LI (mean ± SD) | p |
| Age (med:70; min–max: 35–92) | ||||||||
| <70 | 101 | 0.04 ± 0.05 | 0.97 | 0.40 ± 0.12 | 0.57 | 62 | 0.47 ± 0.17 | 0.70 |
| >70 | 103 | 0.04 ± 0.04 | 0.41 ± 0.12 | 68 | 0.49 ± 0.19 | |||
| Sex | ||||||||
| Female | 95 | 0.04 ± 0.05 | 0.58 | 0.39 ± 0.13 | 0.32 | 64 | 0.48 ± 0.20 | 0.77 |
| Male | 109 | 0.04 ± 0.04 | 0.41 ± 0.12 | 66 | 0.47 ± 0.17 | |||
| Location | ||||||||
| Caecum | 18 | 0.04 ± 0.04 | 0.29 * | 0.44 ± 0.13 | 0.08 | 8 | 0.59 ± 0.17 | 0.17 ** |
| Ascending colon | 33 | 0.04 ± 0.05 | 0.4 ± 0.1 | 17 | 0.43 ± 0.18 | |||
| Hepatic flexure | 1 | 0.1 | 0.6 | 0 | NA | |||
| Transverse colon | 8 | 0.06 ± 0.06 | 0.47 ± 0.07 | 4 | 0.52 ± 0.18 | |||
| Splenic flexure | 7 | 0.02 ± 0.03 | 0.42 ± 0.14 | 5 | 0.48 ± 0.15 | |||
| Descending colon | 17 | 0.05 ± 0.06 | 0.4 ± 0.14 | 10 | 0.37 ± 0.20 | |||
| Sigmoid colon | 47 | 0.03 ± 0.04 | 0.4 ± 0.13 | 34 | 0.46 ± 0.17 | |||
| Rectosigmoid junction | 14 | 0.03 ± 0.03 | 0.38 ± 0.1 | 9 | 0.47 ± 0.19 | |||
| Rectum | 48 | 0.04 ± 0.04 | 0.37 ± 0.12 | 35 | 0.51 ± 0.19 | |||
| Multiple | 11 | 0.02 ± 0.02 | 0.46 ± 0.12 | 8 | 0.52 ± 0.21 | |||
| Tumor grading *** | ||||||||
| Well differentiated | 88 | 0.04 ± 0.05 | 0.66 | 0.4 ± 0.13 | 0.77 | 61 | 0.44 ± 0.19 | 0.007 |
| Moderately differentiated | 107 | 0.03 ± 0.04 | 0.4 ± 0.11 | 63 | 0.52 ± 0.16 | |||
| Poorly differentiated | 5 | 0.05 ± 0.03 | 0.51 ± 0.07 | 2 | 0.51 ± 0.39 | |||
| T status | ||||||||
| T1 | 15 | 0.02 ± 0.03 | 0.32 | 0.36 ± 0.12 | 0.10 | 10 | 0.42 ± 0.11 | 0.47 |
| T2 | 42 | 0.04 ± 0.05 | 0.44 ± 0.12 | 30 | 0.50 ± 0.17 | |||
| T3 | 136 | 0.04 ± 0.04 | 0.39 ± 0.13 | 83 | 0.48 ± 0.20 | |||
| T4 | 11 | 0.04 ± 0.06 | 0.38 ± 0.08 | 7 | 0.48 ± 0.15 | |||
| N status | ||||||||
| N0 | 135 | 0.04 ± 0.04 | 0.80 | 0.41 ± 0.13 | 0.36 | 89 | 0.48 ± 0.19 | 0.43 |
| N1 | 50 | 0.03 ± 0.04 | 0.40 ± 0.10 | 29 | 0.49 ± 0.18 | |||
| N2 | 19 | 0.05 ± 0.07 | 0.37 ± 0.11 | 12 | 0.45 ± 0.18 | |||
| Postoperative treatment | ||||||||
| No | 137 | 0.03 ± 0.04 | 0.43 | 0.41 ± 0.12 | 0.44 | 88 | 0.48 ± 0.19 | 0.49 |
| Yes | 62 | 0.04 ± 0.05 | 0.4 ± 0.12 | 40 | 0.46 ± 0.18 | |||
| Model p-Value | Prognostic Factors | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|---|
| <10−5 | Age | 1.04 | 1.02–1.06 | 0.001 |
| N stage | 2.72 | 1.97–3.75 | <10−6 | |
| Postoperative treatment | 0.45 | 0.25–0.80 | 0.007 | |
| VEGFR-1 LI | 1.06 | 1.02–1.10 | 0.004 |
| Model p-Value | Prognostic Factors | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|---|
| Metastasis-free survival | ||||
| <10−5 | N stage | 2.86 | 1.97–4.14 | <10−6 |
| VEGFR-1_VEGFR-2 * | 2.31 | 1.44–5.03 | 0.007 | |
| Overall survival | ||||
| <10−5 | Age | 1.04 | 1.02–1.06 | 0.001 |
| N stage | 2.78 | 2.01–3.85 | <10−6 | |
| Postoperative treatment | 0.42 | 0.24–0.74 | 0.003 | |
| VEGFR-1_VEGFR-2 * | 1.70 | 1.12–2.56 | 0.012 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Haene, N.; Koopmansch, C.; Van Eycke, Y.-R.; Hulet, F.; Allard, J.; Bouri, S.; Rorive, S.; Remmelink, M.; Decaestecker, C.; Maris, C.; et al. The Prognostic Value of the Combination of Low VEGFR-1 and High VEGFR-2 Expression in Endothelial Cells of Colorectal Cancer. Int. J. Mol. Sci. 2018, 19, 3536. https://doi.org/10.3390/ijms19113536
D’Haene N, Koopmansch C, Van Eycke Y-R, Hulet F, Allard J, Bouri S, Rorive S, Remmelink M, Decaestecker C, Maris C, et al. The Prognostic Value of the Combination of Low VEGFR-1 and High VEGFR-2 Expression in Endothelial Cells of Colorectal Cancer. International Journal of Molecular Sciences. 2018; 19(11):3536. https://doi.org/10.3390/ijms19113536
Chicago/Turabian StyleD’Haene, Nicky, Caroline Koopmansch, Yves-Rémi Van Eycke, Françoise Hulet, Justine Allard, Sarah Bouri, Sandrine Rorive, Myriam Remmelink, Christine Decaestecker, Calliope Maris, and et al. 2018. "The Prognostic Value of the Combination of Low VEGFR-1 and High VEGFR-2 Expression in Endothelial Cells of Colorectal Cancer" International Journal of Molecular Sciences 19, no. 11: 3536. https://doi.org/10.3390/ijms19113536
APA StyleD’Haene, N., Koopmansch, C., Van Eycke, Y.-R., Hulet, F., Allard, J., Bouri, S., Rorive, S., Remmelink, M., Decaestecker, C., Maris, C., & Salmon, I. (2018). The Prognostic Value of the Combination of Low VEGFR-1 and High VEGFR-2 Expression in Endothelial Cells of Colorectal Cancer. International Journal of Molecular Sciences, 19(11), 3536. https://doi.org/10.3390/ijms19113536






