Targeted α Therapies for the Treatment of Bone Metastases
Abstract
1. Introduction
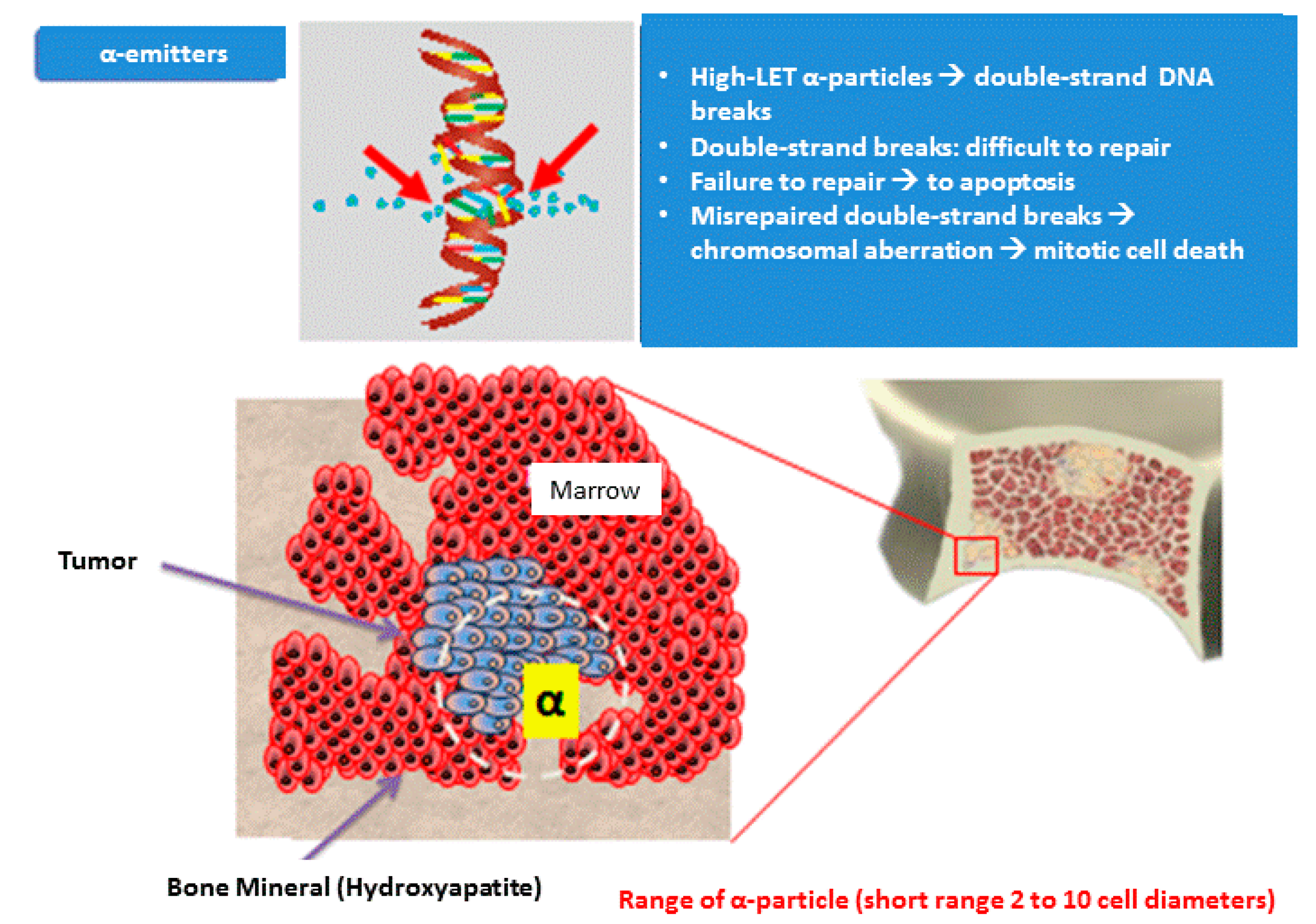
2. Targeted α Therapy
2.1. Targeted A Therapies and Skeleton
2.2. Targeted A Therapies after Radium-226
2.3. Targeted A Therapies Represent an Additional Class of Drugs in Prostate Cancer
3. Radium 223
3.1. Pivotal Studies
3.1.1. ALSYMPCA (Aradin in Symptomatic Prostate Cancer)
3.1.2. Expanded Access Program Studies
International Expanded Access Program
US-Expanded Access Program
3.2. Guidelines
3.3. Activity on Tumor Dormancy
3.4. Activity on Micro-Metastatic Clones of Visceral Tumor Cells
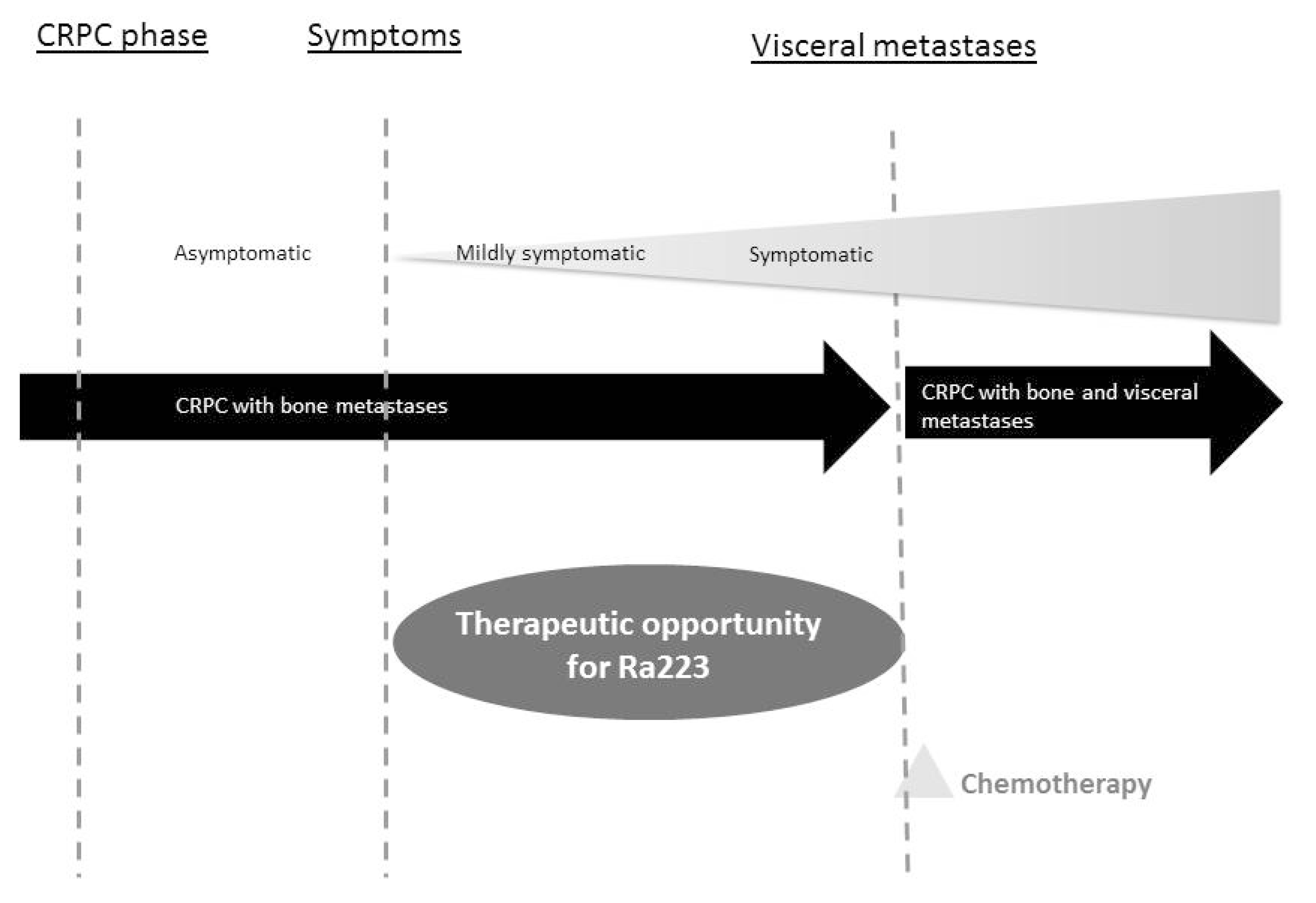
3.5. Place in Therapy
3.6. Ongoing Studies
4. Actinium-225
5. Thorium 227
6. Conclusions
Acknowledgments
Conflicts of Interest
References
- Kulakowski, A. The contribution of Marie Sklodowska-Curie to the development of modern oncology. Anal. Bioanal. Chem. 2011, 400, 1583–1586. [Google Scholar] [CrossRef] [PubMed]
- Dronsfield, A.; Elis, P. Radium—A key element in early cancer treatment. Educ. Chem. 2011, 48, 56–59. [Google Scholar]
- Srivastava, S.C. Paving the way to personalized medicine: Production of some promising theragnostic radionuclides at Brookhaven National Laboratory. Semin. Nucl. Med. 2012, 42, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.J.; Huang, C.Y.; Clarke, R.A. Targeted α anticancer therapies: Update and future prospects. Biol. Targets Ther. 2014, 8, 255–267. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. A Emitting Radionuclides and Radiopharmaceuticals for Therapy; Meeting Report; International Atomic Energy Agency: Vienna, Austria, 2013. [Google Scholar]
- Parker, C.; Nilsson, S.; Heinrich, D.; Helle, S.I.; O’Sullivan, J.M.; Fossa, S.D.; Chodacki, A.; Wiechno, P.; Logue, J.; Seke, M.; et al. A emitter radium-223 and survival in metastatic prostate cancer. N. Engl. J. Med. 2013, 369, 213–223. [Google Scholar] [CrossRef] [PubMed]
- McDonald, R.; Chow, E.; Rowbottom, L.; Bedard, G.; Lam, H.; Wong, E.; Popovic, M.; Pulenzas, N.; Tsao, M. Quality of life after palliative radiotherapy in bone metastases: A literature review. J. Bone Oncol. 2015, 4, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Elgqvist, J.; Frost, S.; Pouget, J.P.; Albertsson, P. The potential and hurdles of targeted α therapy—Clinical trials and beyond. Front. Oncol. 2014, 3, 324. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.; Kampen, W.U. Radionuclide therapy of bone metastases. Breast Care 2012, 7, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Emmett, L.; Willowson, K.; Violet, J.; Shin, J.; Blanksby, A.; Lee, J. Lutetium 177 PSMA radionuclide therapy for men with prostate cancer: A review of the current literature and discussion of practical aspects of therapy. J. Med. Radiat. Sci. 2017, 64, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Broecker, W.S.; Li, Y.H.; Cromwell, J. Radium-226 and radon-222: Concentration in atlantic and pacific oceans. Science 1967, 158, 1307–1310. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, G.; Zalutsky, M.R. Astatine radiopharmaceuticals: Prospects and problems. Curr. Radiopharm. 2008, 1, 177. [Google Scholar] [CrossRef] [PubMed]
- Yana, D. Targeted α therapy using short-lived α-particles and the promise of nanobodies as targeting vehicle. Expert Opin. Biol. Ther. 2016, 16, 1035–1047. [Google Scholar]
- Wadas, T.J.; Pandya, D.N.; Solingapuram Sai, K.K.; Mintz, A. Molecular targeted α-particle therapy for oncologic applications. AJR Am. J. Roentgenol. 2014, 203, 253–260. [Google Scholar] [CrossRef] [PubMed]
- NCT02581878. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- Kakhki, V.R.; Anvari, K.; Sadeghi, R.; Mahmoudian, A.S.; Torabian-Kakhki, M. Pattern and distribution of bone metastases in common malignant tumors. Nucl. Med. Rev. Cent. East. Eur. 2013, 16, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Blacksburg, S.R.; Witten, M.R.; Haas, J.A. Integrating bone targeting radiopharmaceuticals into the management of patients with castrate-resistant prostate cancer with symptomatic bone metastases. Curr. Treat. Options Oncol. 2015, 16, 325. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, G.; Breistol, K.; Bruland, O.S.; Fodstad, O.; Larsen, R.H. Significant antitumor effect from bone-seeking, α-particle-emitting (223)Ra demonstrated in an experimental skeletal metastases model. Cancer Res. 2002, 62, 3120–3125. [Google Scholar] [PubMed]
- Bruland, O.S.; Nilsson, S.; Fisher, D.R.; Larsen, R.H. High-linear energy transfer irradiation targeted to skeletal metastases by the α-emitter 223Ra: Adjuvant or alternative to conventional modalities? Clin. Cancer Res. 2006, 12 Pt 2, 6250s–6257s. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.C.; Coleman, R.E.; Sartor, O.; Vogelzang, N.J.; Bottomley, D.; Heinrich, D.; Helle, S.I.; O’Sullivan, J.M.; Fossa, S.D.; Chodacki, A.; et al. Three-year safety of radium-223 dichloride in patients with castration-resistant prostate cancer and symptomatic bone metastases from phase 3 randomized αradin in symptomatic prostate cancer trial. Eur. Urol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Saad, F.; Carles, J.; Gillessen, S.; Heidenreich, A.; Heinrich, D.; Gratt, J.; Levy, J.; Miller, K.; Nilsson, S.; Petrenciuc, O.; et al. Radium-223 International Early Access Program, I. Radium-223 and concomitant therapies in patients with metastatic castration-resistant prostate cancer: An international, early access, open-label, single-arm phase 3b trial. Lancet Oncol. 2016, 17, 1306–1316. [Google Scholar] [CrossRef]
- Saad, F.; Keizman, D.; O’Sullivan, J.M.; Carles, J.; Wirth, M.; Gillessen, S. Analysis of overall survival by number of radium-223 injections received in an international expanded access program (iEAP). J. Clin. Oncol. 2016. [Google Scholar] [CrossRef]
- Vogelzang, N.J.; Fernandez, D.C.; Morris, M.J.; Iagaru, A.; Brown, A.; Almeida, F.; Sweeney, C.; Smith, M.R.; Dicker, A.; Wong, Y.N.; et al. Radium-223 dichloride (Ra-223) in U.S. expanded access program (EAP). J. Clin. Oncol. 2015. [Google Scholar] [CrossRef]
- Shore, N.D. When to initiate treatment with radium-223 in patients with metastatic castration-resistant prostate cancer. Clin. Adv. Hematol. Oncol. 2016, 14, 26–29. [Google Scholar] [PubMed]
- Cherny, N.I.; Sullivan, R.; Dafni, U.; Kerst, J.M.; Sobrero, A.; Zielinski, C.; de Vries, E.G.; Piccart, M.J. A standardised, generic, validated approach to stratify the magnitude of clinical benefit that can be anticipated from anti-cancer therapies: The European society for medical oncology magnitude of clinical benefit scale (ESMO-MCBS). Ann. Oncol. 2017, 28, 2901–2905. [Google Scholar] [CrossRef] [PubMed]
- Suominen, M.I.; Fagerlund, K.M.; Rissanen, J.P.; Konkol, Y.M.; Morko, J.P.; Peng, Z.; Alhoniemi, E.J.; Laine, S.K.; Corey, E.; Mumberg, D.; et al. Radium-223 inhibits osseous prostate cancer growth by dual targeting of cancer cells and bone microenvironment in mouse models. Clin. Cancer Res. 2017, 23, 4335–4346. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.; Franzen, L.; Parker, C.; Tyrrell, C.; Blom, R.; Tennvall, J.; Lennernas, B.; Petersson, U.; Johannessen, D.C.; Sokal, M.; et al. Bone-targeted radium-223 in symptomatic, hormone-refractory prostate cancer: A randomised, multicentre, placebo-controlled phase II study. Lancet Oncol. 2007, 8, 587–594. [Google Scholar] [CrossRef]
- Coleman, R.; Aksnes, A.K.; Naume, B.; Garcia, C.; Jerusalem, G.; Piccart, M.; Vobecky, N.; Thuresson, M.; Flamen, P. A phase IIa, nonrandomized study of radium-223 dichloride in advanced breast cancer patients with bone-dominant disease. Breast Cancer Res. Treat. 2014, 145, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Miyahira, A.K.; Soule, H.R. The 23rd annual prostate cancer foundation scientific retreat report. Prostate 2017, 77, 1093–1106. [Google Scholar] [CrossRef] [PubMed]
- Suominen, M.I.; Rissanen, J.P.; Kakonen, R.; Fagerlund, K.M.; Alhoniemi, E.; Mumberg, D.; Ziegelbauer, K.; Halleen, J.M.; Kakonen, S.M.; Scholz, A. Survival benefit with radium-223 dichloride in a mouse model of breast cancer bone metastasis. J. Natl. Cancer Inst. 2013, 105, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Croucher, P.I.; McDonald, M.M.; Martin, T.J. Bone metastasis: The importance of the neighbourhood. Nat. Rev. Cancer 2016, 16, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Pezaro, C.; Omlin, A.; Lorente, D.; Rodrigues, D.N.; Ferraldeschi, R.; Bianchini, D.; Mukherji, D.; Riisnaes, R.; Altavilla, A.; Crespo, M.; et al. Visceral disease in castration-resistant prostate cancer. Eur. Urol. 2014, 65, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Gundem, G.; Van Loo, P.; Kremeyer, B.; Alexandrov, L.B.; Tubio, J.M.C.; Papaemmanuil, E.; Brewer, D.S.; Kallio, H.M.L.; Hognas, G.; Annala, M.; et al. The evolutionary history of lethal metastatic prostate cancer. Nature 2015, 520, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Chi, K.; Hotte, S.J.; Joshua, A.M.; North, S.; Wyatt, A.W.; Collins, L.L.; Saad, F. Treatment of mCRPC in the AR-axis-targeted therapy-resistant state. Ann. Oncol. 2015, 26, 2044–2056. [Google Scholar] [CrossRef] [PubMed]
- Sartor, O.; Hoskin, P.; Coleman, R.E.; Nilsson, S.; Vogelzang, N.J.; Petrenciuc, O.; Staudacher, K.; Thuresson, M.; Parker, C. Chemotherapy following radium-223 dichloride treatment in ALSYMPCA. Prostate 2016, 76, 905–916. [Google Scholar] [CrossRef] [PubMed]
- Sartor, O.; Heinrich, D.; Mariados, N.; Mendez Vidal, M.J.; Keizman, D.; Thellenberg Karlsson, C.; Peer, A.; Procopio, G.; Frank, S.J.; Pulkkanen, K.; et al. Re-treatment with radium-223: First experience from an international, open-label, phase I/II study in patients with castration-resistant prostate cancer and bone metastases. Ann. Oncol. 2017, 28, 2464–2471. [Google Scholar] [CrossRef] [PubMed]
- NCT02463799. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT03093428. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02456571. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02814669. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT03076203. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02258464. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02390934. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02406521. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02258451. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- NCT02366130. Available online: www.clinicaltrials.gov (accessed on 17 October 2017).
- Takalkar, A.; Paryani, B.; Adams, S.; Subbiah, V. Radium-223 dichloride therapy in breast cancer with osseous metastases. BMJ Case Rep. 2015. [Google Scholar] [CrossRef] [PubMed]
- Takalkar, A.; Adams, S.; Subbiah, V. Radium-223 dichloride bone-targeted α particle therapy for hormone-refractory breast cancer metastatic to bone. Exp. Hematol. Oncol. 2014, 3, 23. [Google Scholar] [CrossRef] [PubMed]
- Larson, S.M.; Carrasquillo, J.A.; Cheung, N.K.; Press, O.W. Radioimmunotherapy of human tumours. Nat. Rev. Cancer 2015, 15, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Kratochwil, C.; Bruchertseifer, F.; Giesel, F.L.; Weis, M.; Verburg, F.A.; Mottaghy, F.; Kopka, K.; Apostolidis, C.; Haberkorn, U.; Morgenstern, A. 225Ac-PSMA-617 for PSMA-targeted α-radiation therapy of metastatic castration-resistant prostate cancer. J. Nucl. Med. 2016, 57, 1941–1944. [Google Scholar] [CrossRef] [PubMed]
- Kratochwil, C.; Bruchertseifer, F.; Rathke, H.; Bronzel, M.; Apostolidis, C.; Weichert, W.; Haberkorn, U.; Giesel, F.L.; Morgenstern, A. Targeted α-therapy of metastatic castration-resistant prostate cancer with 225AC-PSMA-617: Dosimetry estimate and empiric dose finding. J. Nucl. Med. 2017, 58, 1624–1631. [Google Scholar] [CrossRef] [PubMed]
- European Commission, Joint Research Centre. Hope for Metastatic Prostate Cancer Patients: Targeted A Therapy Shows Impressive Results; European Commission, Joint Research Centre: London, UK, 2016. [Google Scholar]
- Hagemann, U.B.; Wickstroem, K.; Wang, E.; Shea, A.O.; Sponheim, K.; Karlsson, J.; Bjerke, R.M.; Ryan, O.B.; Cuthbertson, A.S. In Vitro and In Vivo Efficacy of a Novel CD33-Targeted Thorium-227 conjugate for the treatment of acute myeloid leukemia. Mol. Cancer Ther. 2016, 15, 2422–2431. [Google Scholar] [CrossRef] [PubMed]
- Hagemann, U.B.; Mihaylova, D.; Uran, S.R.; Borrebaek, J.; Grant, D.; Bjerke, R.M.; Karlsson, J.; Cuthbertson, A.S. Targeted α therapy using a novel CD70 targeted thorium-227 conjugate in in vitro and in vivo models of renal cell carcinoma. Oncotarget 2017, 8, 56311–56326. [Google Scholar] [CrossRef] [PubMed]
- Hammer, S.L.A.; Ellingsen, C.; Geraudie, S.; Grant, D. Preclinical pharmacology of the PSMA-targeted thorium-227 conjugate PSMA-TTC: A novel targeted α therapeutic for the treatment of prostate cancer. In Proceedings of the AACR Annual Meeting 2017, Washington, DC, USA, 1–5 April 2017. [Google Scholar]
| Parametres | β-Emitters Drugs | Targeted α Therapy |
|---|---|---|
| Overall survival (OS) benefit | Not proven for any β-emitters in prostate cancer (PC) | European Medicines Agency (EMA), Food and Drug Administration (FDA) label for Radium-223 |
| Therapy Precision | Wide Range (2–11 mm) and Low Linear Energy Transfer (LET) | Short Range (<100 μm) and high LET |
| Hematologic Side Effects | Dose limiting, risk of marrow ablation | limited hematological side effects |
| Radiation Risk Management | Often need for patient isolation due to irradiation concerns | Outpatient treatment for Radium-223 |
| Androgen Receptor Inhibitors | Targeted α Therapy | Chemotherapy | Immuno-Therapy | Supportive Therapy |
|---|---|---|---|---|
| Traditional Androgen Deprivation Therapy (ADT) Abiraterone Enzalutamide | Radium-223 dichloride | Docetaxel Cabazitaxel | Sipuleucel-T | Strontium-89 |
| Samarium-153 | ||||
| Rhenium-186 | ||||
| Zoledronic acid | ||||
| Denosumab | ||||
| Steroids | ||||
| Drugs with proven survival benefit | Supportive drug | |||
| AR Inhibitors | Targeted α Therapy | Chemotherapy | Immuno-Therapy | Supportive Therapy |
|---|---|---|---|---|
| ODM 201 Apalutamide | PSMA mAb Thorium-227 | Pembrolizumab | Strontium-89 | |
| Actinium-225 conjugates | Atezolizumab | |||
| Drugs with proven survival benefit | Supportive drug | |||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zustovich, F.; Barsanti, R. Targeted α Therapies for the Treatment of Bone Metastases. Int. J. Mol. Sci. 2018, 19, 74. https://doi.org/10.3390/ijms19010074
Zustovich F, Barsanti R. Targeted α Therapies for the Treatment of Bone Metastases. International Journal of Molecular Sciences. 2018; 19(1):74. https://doi.org/10.3390/ijms19010074
Chicago/Turabian StyleZustovich, Fable, and Roberto Barsanti. 2018. "Targeted α Therapies for the Treatment of Bone Metastases" International Journal of Molecular Sciences 19, no. 1: 74. https://doi.org/10.3390/ijms19010074
APA StyleZustovich, F., & Barsanti, R. (2018). Targeted α Therapies for the Treatment of Bone Metastases. International Journal of Molecular Sciences, 19(1), 74. https://doi.org/10.3390/ijms19010074




