Endothelium-Dependent Hyperpolarization (EDH) in Hypertension: The Role of Endothelial Ion Channels
Abstract
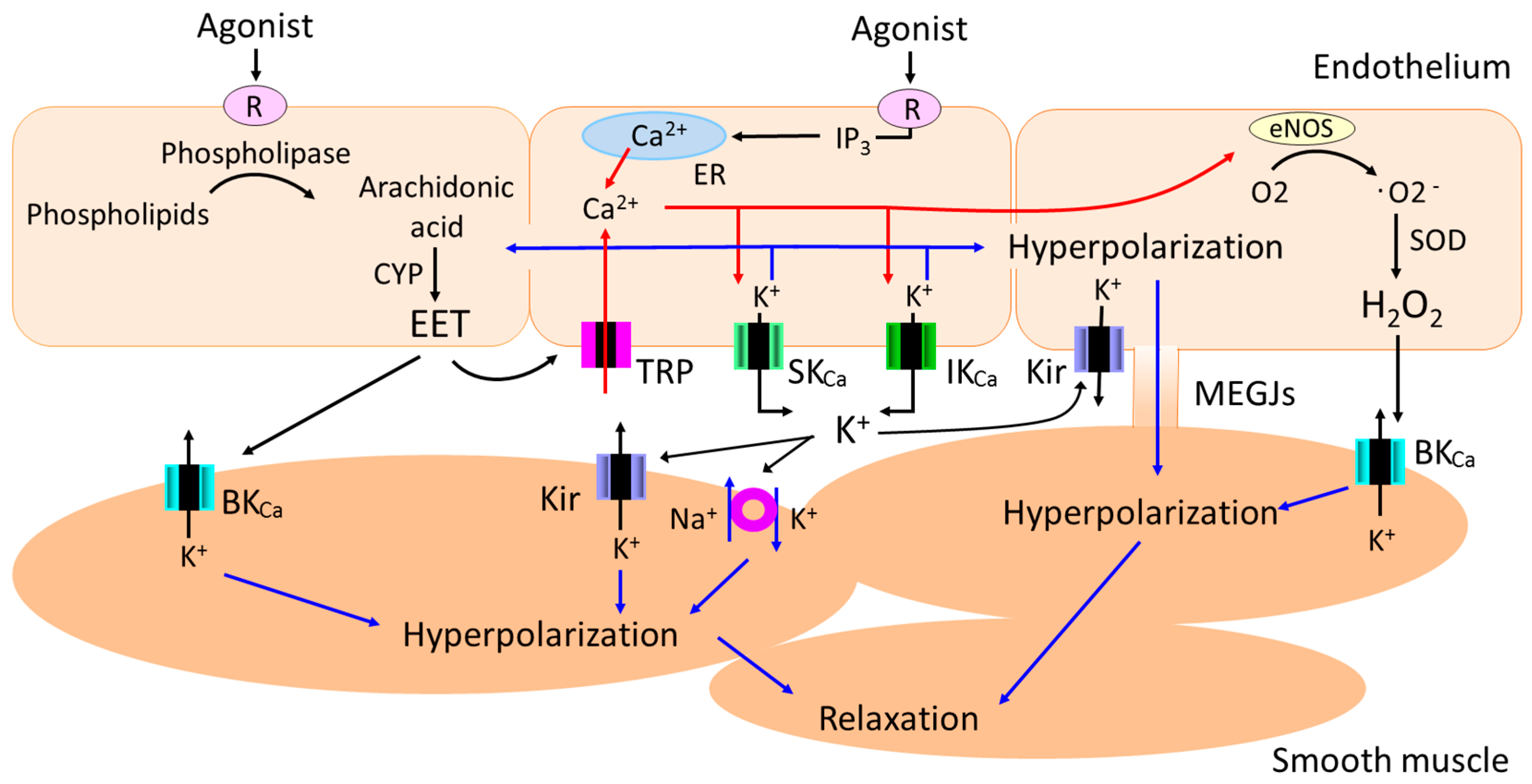
1. Introduction
2. Endothelium-Dependent Hyperpolarization (EDH) in Animal Models of Hypertension
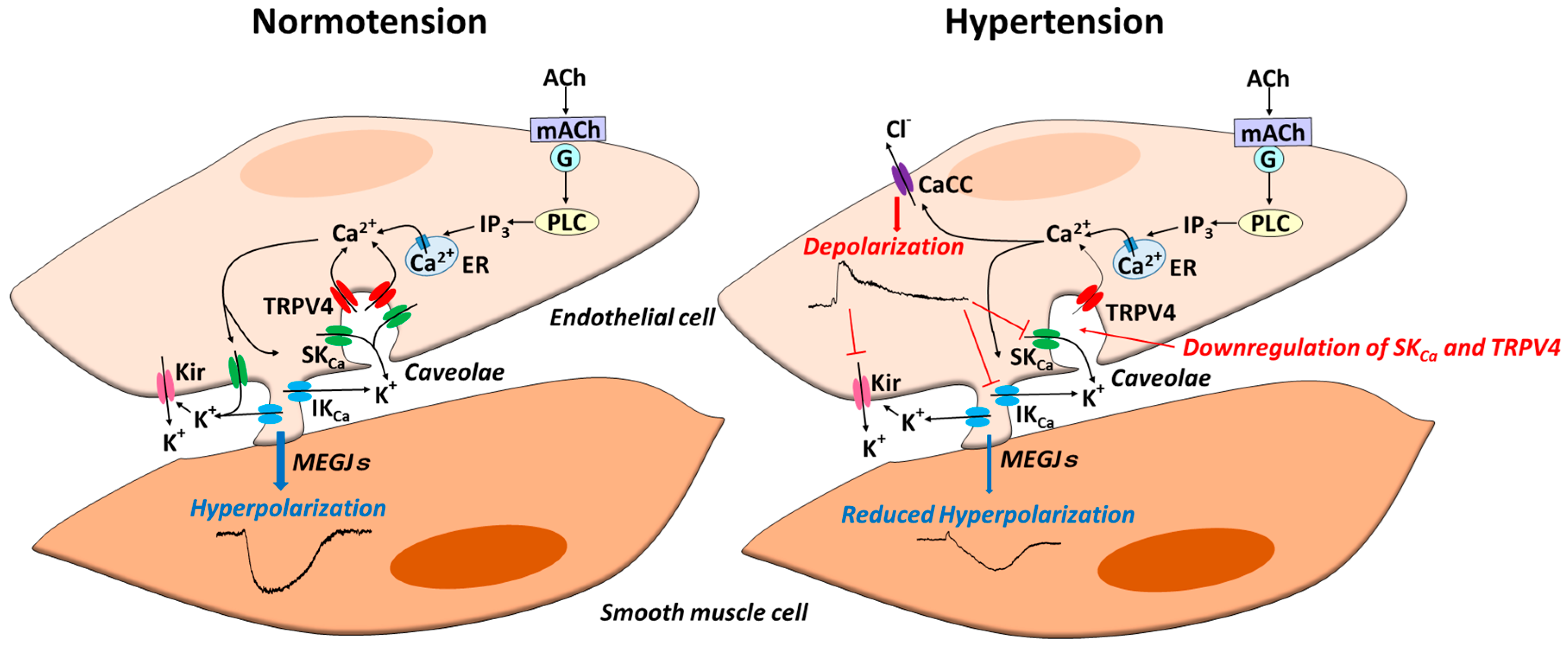
3. Role of Endothelial Ion Channels in Reduced EDH during Hypertension
3.1. Ca2+-Activated K+ (KCa) Channels
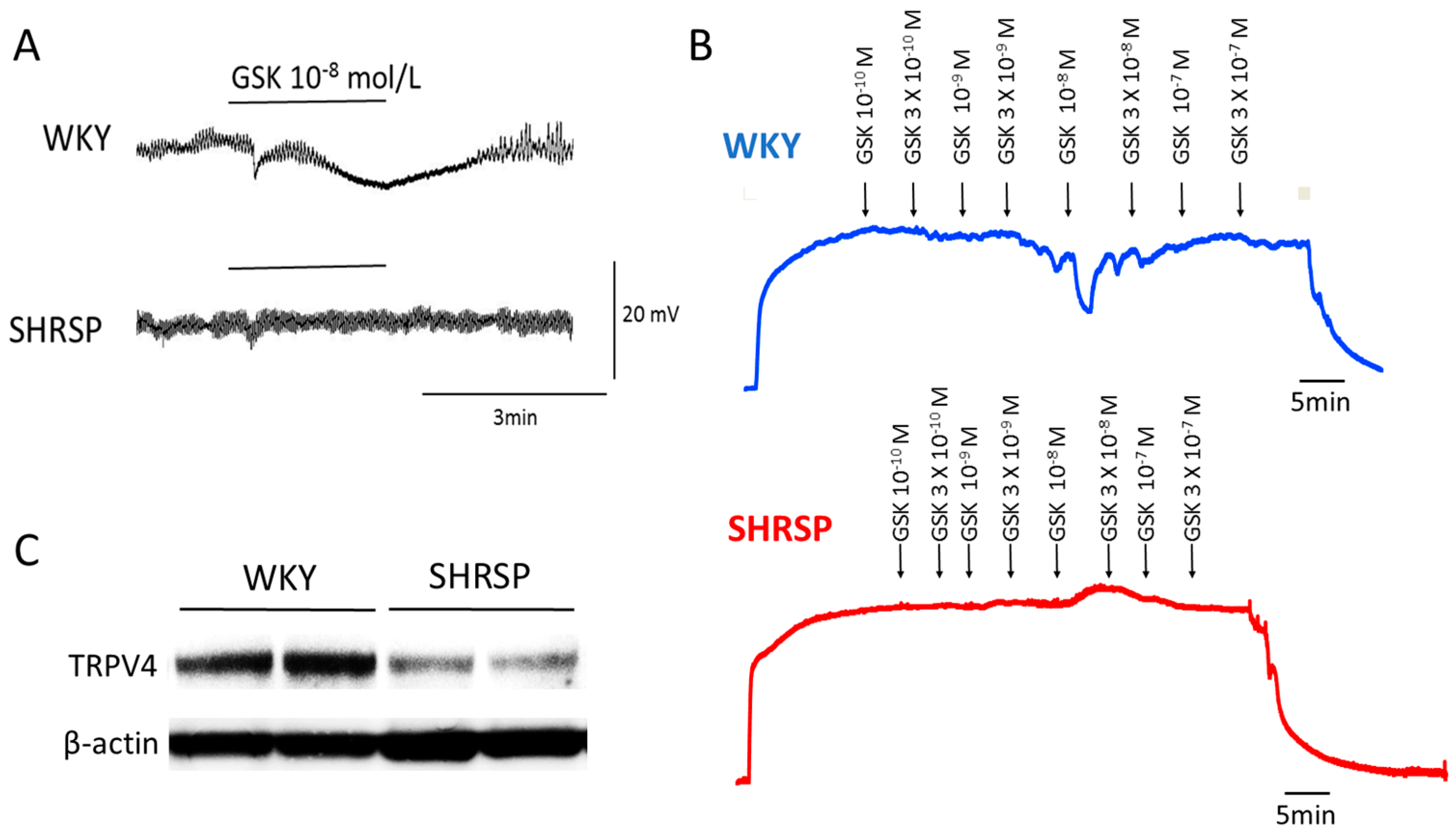
3.2. Transient Receptor Potential (TRP) Channels
3.3. Inward Rectifier K+ (Kir) Channels
3.4. Voltage-Gated K+ (Kv) Channels and ATP-Sensitive K+ (KATP) Channels
3.5. Ca2+-Activated Chloride Channels (CaCCs)
4. Therapeutic Implications
5. Endothelium-Dependent Hyperpolarization (EDH) in Human Hypertension
6. Conclusions
Acknowledgments
Conflicts of Interest
Abbreviations
| ACE | Angiotensin converting enzyme |
| ACh | Acetylcholine |
| AKAP150 | A-kinase anchoring protein 150 |
| BKCa | Large conductance Ca2+-activated K+ |
| CaCC | Ca2+-activated Cl− channel |
| CYP | Cytochrome P450 |
| DOCA | Deoxycorticosterone acetate |
| EDH | Endothelium-dependent hyperpolarization |
| EDHF | Endothelium-derived hyperpolarizing factor |
| EETs | Epoxyeicosatrienoic acids |
| eNOS | endothelial nitric oxide synthase |
| GSK | GSK1016790A |
| H2O2 | Hydrogen peroxide |
| H2S | Hydrogen sulfide |
| IKCa | Intermediate–conductance Ca2+-activated K+ |
| KATP | ATP-sensitive K+ |
| Kir | Inward rectifier K+ |
| Kv | Voltage-gated K+ |
| l-NAME | Nω-nitro-l-arginine |
| MEGJs | Myoendothelial gap junctions |
| MEPs | Myoendothelial projections |
| NADPH | Nicotinamide adenine dinucleotide phosphate |
| NO | Nitric oxide |
| PKC | Protein kinase C |
| RAS | Renin–angiotensin system |
| SHR | Spontaneously hypertensive rats |
| SHRSP | Stroke-prone spontaneously hypertensive rats |
| SKCa | Small-conductance Ca2+-activated K+ |
| TMEM16A | Transmembrane member 16A |
| TRP | Transient receptor potential |
| TRPC3 | TRP canonical type 3 |
| TRPV4 | TRP vanilloid type 4 |
| WKY | Wistar-Kyoto |
References
- Hill, C.E.; Phillips, J.K.; Sandow, S.L. Heterogeneous control of blood flow amongst different vascular beds. Med. Res. Rev. 2001, 21, 1–60. [Google Scholar] [CrossRef]
- Feletou, M.; Vanhoutte, P.M. Endothelium-dependent hyperpolarization of canine coronary smooth muscle. Br. J. Pharmacol. 1988, 93, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Suzuki, H.; Weston, H.A. Acetylcholine releases endothelium-derived hyperpolarizing factors and EDRF from rat blood vessels. Br. J. Pharmacol. 1988, 95, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Garland, C.J.; McPherson, G.A. Evidence that nitric oxide does not mediate the hyperpolarization and relaxation to acetylcholine in the rat small mesenteric artery. Br. J. Pharmacol. 1992, 105, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Busse, R.; Edwards, G.; Feletou, M.; Fleming, I.; Vanhoutte, P.M.; Weston, A.H. EDHF: Bringing the concepts together. Trends Pharmacol. Sci. 2002, 23, 374–380. [Google Scholar] [CrossRef]
- Sandow, S.L. Factors, fiction and endothelium-derived hyperpolarizing factor. Clin. Exp. Pharmacol. Physiol. 2004, 31, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Garland, C.J.; Dora, K.A. EDH: Endothelium-dependent hyperpolarization and microvascular signalling. Acta Physiol. 2017, 219, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Campbell, W.B.; Gebremedhin, D.; Pratt, P.F.; Harder, D.R. Identification of epoxyeicosatrienoic acids as endothelium-derived hyperpolarizing factors. Circ. Res. 1996, 78, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Fisslthaler, B.; Popp, R.; Kiss, L.; Potente, M.; Harder, D.R.; Fleming, I.; Busse, R. Cytochrome P450 2C is an EDHF synthase in coronary arteries. Nature 1999, 401, 493–497. [Google Scholar] [PubMed]
- Edwards, G.; Dora, K.A.; Gardener, M.J.; Garland, C.J.; Weston, A.H. K+ is an endothelium-derived hyperpolarizing factor in rat arteries. Nature 1998, 396, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, S.D.; Nilsson, H.; Ahluwalia, A.; Hobbs, A.J. Release of C-type natriuretic peptide accounts for the biological activity of endothelium-derived hyperpolarizing factor. Proc. Natl. Acad. Sci. USA 2003, 100, 1426–1431. [Google Scholar] [CrossRef] [PubMed]
- Matoba, T.; Shimokawa, H.; Nakashima, M.; Hirakawa, Y.; Mukai, Y.; Hirano, K.; Kanaide, H.; Takeshita, A. Hydrogen peroxide is an endothelium-derived hyperpolarizing factor in mice. J. Clin. Investig. 2000, 106, 1521–1530. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, A.K.; Sikka, G.; Gazi, S.K.; Steppan, J.; Jung, S.M.; Bhunia, A.K.; Barodka, V.M.; Gazi, F.K.; Barrow, R.K.; Wang, R.; et al. Hydrogen sulfide as endothelium-derived hyperpolarizing factor sulfhydrates potassium channels. Circ. Res. 2011, 109, 1259–1268. [Google Scholar] [CrossRef] [PubMed]
- Campbell, W.B.; Fleming, I. Epoxyeicosatrienoic acids and endothelium-dependent responses. Pflugers. Arch. 2010, 459, 881–895. [Google Scholar] [CrossRef] [PubMed]
- Larsen, B.T.; Campbell, W.B.; Gutterman, D.D. Beyond vasodilatation: Non-vasomotor roles of epoxyeicosatrienoic acids in the cardiovascular system. Trends Pharmacol. Sci. 2007, 28, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Node, K.; Huo, Y.; Ruan, X.; Yang, B.; Spiecker, M.; Ley, K.; Zeldin, D.C.; Liao, J.K. Anti-inflammatory properties of cytochrome P450 epoxygenase-derived eicosanoids. Science 1999, 285, 1276–1279. [Google Scholar] [CrossRef] [PubMed]
- Hashitani, H.; Suzuki, H. K+ channels which contribute to the acetylcholine-induced hyperpolarization in smooth muscle of the guinea-pig submucosal arteriole. J. Physiol. 1997, 501, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Crane, G.J.; Gallagher, N.; Dora, K.A.; Garland, C.J. Small- and intermediate-conductance calcium-activated K+ channels provide different facets of endothelium-dependent hyperpolarization in rat mesenteric artery. J. Physiol. 2003, 553, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Chaytor, A.T.; Evans, W.H.; Griffith, T.M. Central role of heterocellular gap junctional communication in endothelium-dependent relaxations of rabbit arteries. J. Physiol. 1998, 508, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Imaeda, K.; Suzuki, H. Endothelium-dependent hyperpolarization and intracellular electrical coupling in guinea-pig mesenteric arterioles. J. Physiol. 1999, 514, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Sandow, S.L.; Hill, C.E. Incidence of myoendothelial gap junctions in the proximal and distal mesenteric arteries of the rat is suggestive of a role in endothelium-derived hyperpolarizing factor-mediated responses. Circ. Res. 2000, 86, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Coleman, H.A.; Tare, M.; Parkington, H.C. K+ currents underlying the action of endothelium-derived hyperpolarizing factor in guinea-pig, rat and human blood vessels. J. Physiol. 2001, 531, 359–373. [Google Scholar] [CrossRef] [PubMed]
- Sandow, S.L.; Tare, M.; Coleman, H.A.; Hill, C.E.; Parkington, H.C. Involvement of myoendothelial gap junctions in the actions of endothelium-derived hyperpolarizing factor. Circ. Res. 2002, 90, 1108–1113. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Fujii, K.; Kansui, Y.; Abe, I.; Iida, M. Critical role of gap junctions in endothelium-dependent hyperpolarization in rat mesenteric arteries. Clin. Exp. Pharmacol. Physiol. 2002, 29, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Dora, K.A.; Sandow, S.L.; Gallagher, N.T.; Takano, H.; Rummery, N.M.; Hill, C.E.; Garland, C.J. Myoendothelial gap junctions may provide the pathway for EDHF in mouse mesenteric artery. J. Vasc. Res. 2003, 40, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Earley, S.; Gonzales, A.L.; Crnich, R. Endothelium-dependent cerebral artery dilation mediated by TRPA1 and Ca2+-Activated K+ channels. Circ. Res. 2009, 104, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Earley, S.; Gonzales, A.L.; Garcia, Z.I. A dietary agonist of transient receptor potential cation channel V3 elicits endothelium-dependent vasodilation. Mol. Pharmacol. 2010, 77, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Sonkusare, S.K.; Bonev, A.D.; Ledoux, J.; Liedtke, W.; Kotlikoff, M.I.; Heppner, T.J.; Hill-Eubanks, D.C.; Nelson, M.T. Elementary Ca2+ signals through endothelial TRPV4 channels regulate vascular function. Science 2012, 336, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Senadheera, S.; Kim, Y.; Grayson, T.H.; Toemoe, S.; Kochukov, M.Y.; Abramowitz, J.; Housley, G.D.; Bertrand, R.L.; Chadha, P.S.; Bertrand, P.P.; et al. Transient receptor potential canonical type 3 channels facilitate endothelium-derived hyperpolarization-mediated resistance artery vasodilator activity. Cardiovasc. Res. 2012, 95, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Kochukov, M.Y.; Balasubramanian, A.; Abramowitz, J.; Birnbaumer, L.; Marrelli, S.P. Activation of endothelial transient receptor potential C3 channel is required for small conductance calcium-activated potassium channel activation and sustained endothelial hyperpolarization and vasodilation of cerebral artery. J. Am. Heart Assoc. 2014, 3, E000913. [Google Scholar] [CrossRef] [PubMed]
- Jackson, W.F. Boosting the signal: Endothelial inward rectifier K+ channels. Microcirculation 2017, 24. [Google Scholar] [CrossRef] [PubMed]
- Nagao, T.; Illiano, S.; Vanhoutte, P.M. Heterogeneous distribution of endothelium-dependent relaxations resistant to NG-nitro-l-arginine in rats. Am. J. Physiol. 1992, 263, H1090–H1094. [Google Scholar] [CrossRef] [PubMed]
- Hwa, J.J.; Ghibaudi, L.; Williams, P.; Chatterjee, M. Comparison of acetylcholine-dependent relaxation in large and small arteries of rat mesenteric vascular bed. Am. J. Physiol. 1994, 266, H952–H958. [Google Scholar] [CrossRef] [PubMed]
- Shimokawa, H.; Yasutake, H.; Fujii, K.; Owada, M.K.; Nakaike, R.; Fukumoto, Y.; Takayanagi, T.; Nagao, T.; Egashira, K.; Fujishima, M.; et al. The importance of the hyperpolarizing mechanism increases as the vessel size decreases in endothelium-dependent relaxations in rat mesenteric circulation. J. Cardiovasc. Pharmacol. 1996, 28, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Lawers, C.M.; Hoorn, S.V.; Rodgers, A. Global burden of blood-pressure-related disease. Lancet 2008, 371, 1513–1518. [Google Scholar] [CrossRef]
- Vanhoutte, P.M. Endothelial dysfunction and atherosclerosis. Eur. Heart J. 1997, 18, E19–E29. [Google Scholar] [CrossRef]
- Schiffrin, E.L. Beyond blood pressure: The endothelium and atherosclerosis progression. Am. J. Hypertens. 2002, 15 (Suppl. 1), S115–S122. [Google Scholar] [CrossRef]
- Halcox, J.P.; Schenke, W.H.; Zalos, G.; Mincemoyer, R.; Prasad, A.; Waclawiw, M.A.; Nour, K.R.; Quyyumi, A.A. Prognostic value of coronary vascular endothelial dysfunction. Circulation 2002, 106, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Vanhoutte, P.M.; Feletou, M.; Taddei, S. Endothelium-dependent contractions in hypertension. Br. J. Pharmacol. 2005, 144, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Fujii, K.; Tominaga, M.; Ohmori, S.; Kobayashi, K.; Koga, T.; Takata, Y.; Fujishima, M. Decreased endothelium-dependent hyperpolarization to acetylcholine in smooth muscle of the mesenteric artery of spontaneously hypertensive rats. Circ. Res. 1992, 70, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Fujii, K.; Kansui, Y.; Iida, M. Changes in endothelium-derived hyperpolarizing factor in hypertension and ageing: Response to chronic treatment with renin-angiotensin system inhibitors. Clin. Exp. Pharmacol. Physiol. 2004, 31, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Nabika, T.; Nara, Y.; Ikeda, K.; Endo, J.; Yamori, Y. Genetic heterogeneity of the spontaneously hypertensive rat. Hypertension 1991, 18, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Sandow, S.L.; Bramich, N.J.; Bandi, H.P.; Rummery, N.M.; Hill, C.E. Structure, function, and endothelium-derived hyperpolarizing factor in the caudal artery of the SHR and WKY rat. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 822–828. [Google Scholar] [CrossRef] [PubMed]
- Ellis, A.; Goto, K.; Chaston, D.J.; Brackenbury, T.D.; Meaney, K.R.; Falck, J.R.; Wojcikiewicz, R.J.; Hill, C.E. Enalapril treatment alters the contribution of epoxyeicosatrienoic acids but not gap junctions to endothelium-derived hyperpolarizing factor activity in mesenteric arteries of spontaneously hypertensive rats. J. Pharmacol. Exp. Ther. 2009, 330, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.D.; Dora, K.A.; Ings, N.T.; Crane, G.J.; Garland, C.J. Activation of endothelial cell IK(Ca) with 1-ethyl-2-benzimidazolinone evokes smooth muscle hyperpolarization in rat isolated mesenteric artery. Br. J. Pharmacol. 2001, 134, 1548–1554. [Google Scholar] [CrossRef] [PubMed]
- Seki, T.; Goto, K.; Kiyohara, K.; Kansui, Y.; Murakami, N.; Haga, Y.; Ohtsubo, T.; Matsumura, K.; Kitazono, T. Downregulation of endothelial transient receptor potential vanilloid type 4 channel and small-conductance of Ca2+-activated K+ channels underpins impaired endothelium-dependent hyperpolarization in hypertension. Hypertension 2017, 69, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Nilius, B.; Droogmans, G. Ion channels and their functional role in vascular endothelium. Physiol. Rev. 2001, 81, 1415–1459. [Google Scholar] [CrossRef] [PubMed]
- Jackson, W.F. Potassium channels in the peripheral microcirculation. Microcirculation 2005, 12, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Earley, S.; Brayden, J.E. Transient receptor potential channels in the vasculature. Physiol. Rev. 2015, 95, 645–690. [Google Scholar] [CrossRef] [PubMed]
- Ohya, Y.; Fujishima, M. Alterations of ion channels in vascular muscle cells and endothelial cells during hypertension and aging. In Advances in Cell. Aging and Gerontology; Hagen, T., Ed.; Elsevier Science: Amsterdam, The Netherlands, 2002; Volume 11, pp. 165–182. ISBN 978-0-08-093020-6. [Google Scholar]
- Grgic, I.; Kaistha, B.P.; Hoyer, J.; Köhler, R. Endothelial Ca+-activated K+ channels in normal and impaired EDHF-dilator responses-relevance to cardiovascular pathologies and drug discovery. Br. J. Pharmacol. 2009, 157, 509–526. [Google Scholar] [CrossRef] [PubMed]
- Weston, A.H.; Porter, E.L.; Harno, E.; Edwards, G. Important of endothelial SKCa channels and of downstream hyperpolarizing pathways in mesenteric arteries from spontaneously hypertensive rats. Br. J. Pharmacol. 2010, 160, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Sonkusare, S.K.; Dalsgaard, T.; Bonev, A.D.; Hill-Eubanks, D.C.; Kotlikoff, M.I.; Scott, J.D.; Santana, L.F.; Nelson, M.T. AKAP150-dependent cooperative TRPV4 channel gating is central to endothelium-dependent vasodilation and is disrupted in hypertension. Sci. Signal. 2014, 7, ra66. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.S.; Bonev, A.D.; Gross, T.P.; Eckman, D.M.; Brayden, J.E.; Bond, C.T.; Adelman, J.P.; Nelson, M.T. Altered expression of small-conductance Ca2+-activated K+ (SK3) channels modulates arterial tone and blood pressure. Circ. Res. 2003, 93, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Brähler, S.; Kaistha, A.; Schmidt, V.J.; Wölfle, S.E.; Busch, C.; Kaistha, B.P.; Kacik, M.; Hasenau, A.L.; Grgic, I.; Si, H.; et al. Genetic deficit of SK3 and IK1 channels disrupts the endothelium-derived hyperpolarizing factor vasodilator pathway and causes hypertension. Circulation 2009, 119, 2323–2332. [Google Scholar] [CrossRef] [PubMed]
- Van de Voorde, J.; Vanheel, B.; Leusen, I. Endothelium-dependent relaxation and hyperpolarization in aorta from control and renal hypertensive rats. Circ. Res. 1992, 70, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tare, M.; Parkington, H.C.; Coleman, H.A.; Neild, T.O.; Dusting, G.J. Hyperpolarization and relaxation of arterial smooth muscle caused by nitric oxide derived from the endothelium. Nature 1990, 346, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Parkington, H.C.; Tare, M.; Tonta, M.A.; Coleman, H.A. Stretch revealed three components in the hyperpolarization of guinea-pig coronary artery in response to acetylcholine. J. Physiol. 1993, 465, 459–476. [Google Scholar] [CrossRef] [PubMed]
- Fujii, K.; Ohmori, S.; Tominaga, M.; Abe, I.; Takata, Y.; Ohya, Y.; Kobayashi, K.; Fujishima, M. Age-related changes in endothelium-dependent hyperpolarization in the rat mesenteric artery. Am. J. Physiol. 1993, 265, H509–H516. [Google Scholar] [CrossRef] [PubMed]
- Mantelli, L.; Amerini, S.; Ledda, F. Roles of nitric oxide and endothelium-derived hyperpolarizing factor in vasorelaxant effect of acetylcholine as influenced by aging and hypertension. J. Cardiovasc. Pharmacol. 1995, 25, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Kähönen, M.; Mäkynen, H.; Wu, X.; Arvola, P.; Pörsti, I. Endothelial function in spontaneously hypertensive rats: Influence of quinapril treatment. Br. J. Pharmacol. 1995, 115, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Sunano, S.; Watanabe, H.; Tanaka, S.; Sekiguchi, F.; Shimamura, K. Endothelium-derived relaxing, contracting and hyperpolarizing factors of mesenteric arteries of hypertensive and normotensive rats. Br. J. Pharmacol. 1999, 126, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Hayakawa, H.; Hirata, Y.; Suzuki, E.; Sugimoto, T.; Matsuoka, H.; Kikuchi, K.; Nagano, T.; Hirobe, M.; Sugimoto, T. Mechanisms for altered endothelium-dependent vasorelaxation in isolated kidneys from experimental hypertensive rats. Am. J. Physiol. 1993, 264, H1535–H1541. [Google Scholar] [CrossRef] [PubMed]
- Dohi, Y.; Kojima, M.; Sato, K. Benidipine improves endothelial function in renal resistance arteries of hypertensive rats. Hypertension 1996, 28, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Büssemaker, E.; Popp, R.; Fisslthaler, B.; Larson, C.M.; Fleming, I.; Busse, R.; Brandes, R.P. Aged spontaneously hypertensive rats exhibit a selective loss of EDHF-mediated relaxation in the renal artery. Hypertension 2003, 42, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Pérez, S.; Navarro-Cid, J.; de las Heras, N.; Cediel, E.; Sanz-Rosa, D.; Ruilope, L.M.; Cachofeiro, V.; Lahera, V. Relevance of endothelium-derived hyperpolarizing factor in the effects of hypertension on rat coronary relaxations. J. Hypertens. 2001, 19, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Ohyanagi, M.; Koida, S.; Ueda, A.; Ishiko, K.; Iwasaki, T. Effects of endothelium-derived hyperpolarizing factor and nitric oxide on endothelial function in femoral resistance arteries of spontaneously hypertensive rats. Hypertens. Res. 2006, 29, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Watabe, H.; Cui, J.; Abe, S.; Sato, N.; Ishikawa, H.; Yoshitomi, T. Reduced effects of endothelium-derived hyperpolarizing factor in ocular ciliary arteries from spontaneous hypertensive rats. Exp. Eye Res. 2010, 90, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Mäkynen, H.; Kähönen, M.; Wu, X.; Arvola, P.; Pörsti, I. Endothelial function in deoxycorticosterone-NaCl hypertension: Effect of calcium supplementation. Circulation 1996, 93, 1000–1008. [Google Scholar] [CrossRef] [PubMed]
- Adeagbo, A.S.; Joshua, I.G.; Falkner, C.; Matheson, P.J. Tempol, an antioxidant, restores endothelium-derived hyperpolarizing factor-mediated vasodilation during hypertension. Eur. J. Pharmacol. 2003, 481, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Dal-Ros, S.; Bronner, C.; Schott, C.; Kane, M.O.; Chataigneau, M.; Schini-Kerth, V.B.; Chataigneau, T. Angiotensin II-induced hypertension is associated with a selective inhibition of endothelium-derived hyperpolarizing factor-mediated responses in the rat mesenteric artery. J. Pharmacol. Exp. Ther. 2009, 328, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, Y.; Stepp, D.W.; Chilian, W.M. Nitric oxide exerts feedback inhibition on EDHF-induced coronary arteriolar dilation in vivo. Am. J. Physiol. Heart Circ. Physiol. 2000, 279, H459–H465. [Google Scholar] [CrossRef] [PubMed]
- Bund, S.J. Influence of mode of contraction on the mechanism of acetylcholine-mediated relaxation of coronary arteries from normotensive and spontaneously hypertensive rats. Clin. Sci. 1998, 94, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Sofola, O.A.; Knill, A.; Hainsworth, R.; Drinkhill, M. Change in endothelial function in mesenteric arteries of Sprague-Dawley rats fed a high salt diet. J. Physiol. 2002, 543, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Sendao, O.; Liveira, A.P.; Bendhack, L.M. Relaxation induced by acetylcholine involves endothelium-derived hyperpolarizing factor in 2-kidney 1-clip hypertensive rat carotid arteries. Pharmacology 2004, 72, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Kansui, Y.; Oniki, H.; Ohtsubo, T.; Matsumura, K.; Kitazono, T. Upregulation of endothelium-derived hyperpolarizing factor compensates for the loss of nitric oxide in mesenteric arteries of dahl salt-sensitive hypertensive rats. Hypertens. Res. 2012, 35, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Simonet, S.; Isabelle, M.; Bousquenaud, M.; Clavreul, N.; Félétou, M.; Vayssettes-Courchay, C.; Verbeuren, T.J. KCa 3.1 channels maintain endothelium-dependent vasodilatation in isolated perfused kidneys of spontaneously hypertensive rats after chronic inhibition of NOS. Br. J. Pharmacol. 2012, 167, 854–867. [Google Scholar] [CrossRef] [PubMed]
- Waldron, G.J.; Ding, H.; Lovren, F.; Kubes, P.; Triggle, C.R. Acetylcholine-induced relaxation of peripheral arteries isolated from mice lacking endothelial nitric oxide synthase. Br. J. Pharmacol. 1999, 128, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; McMahon, D.G. Modulation of hybrid bass retinal gap junctional channel gating by nitric oxide. J. Physiol. 1997, 499, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Dora, K.A.; Garland, C.J.; Kwan, H.Y.; Yao, X. Endothelial cell protein kinase G inhibits release of EDHF through a PKG-sensitive cation channel. Am. J. Physiol. Heart Circ. Physiol. 2001, 280, H1272–H1277. [Google Scholar] [CrossRef] [PubMed]
- Onaka, U.; Fujii, K.; Abe, I.; Fujishima, M. Antihypertensive therapy improves endothelium dependent hyperpolarization. In Endothelium-Dependent Hyperpolarization; Vanhoutt, P.M., Ed.; Harwood Academic Publishers: Amsterdam, The Netherlands, 1999; pp. 305–312. [Google Scholar]
- Köhler, R.; Ruth, P. Endothelial dysfunction and blood pressure alterations in K+-channel transgenic mice. Pflugers. Arch. 2010, 459, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Sandow, S.L.; Grayson, T.H. Limits of isolation and culture: Intact vascular endothelium and BKCa. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H1–H7. [Google Scholar] [CrossRef] [PubMed]
- Kong, B.W.; Man, R.Y.; Gao, Y.; Vanhoutte, P.M.; Leung, S.W. Reduced activity of SKC a and Na-K ATPase underlies the accelerated impairment of EDH-type relaxations in mesenteric arteries of aging spontaneously hypertensive rats. Pharmacol. Res. Perspect. 2015, 3, e00150. [Google Scholar] [CrossRef] [PubMed]
- Giachini, F.R.; Carneiro, F.S.; Lima, V.V.; Carneiro, Z.N.; Dorrance, A.; Webb, R.C.; Tostes, R.C. Upregulation of intermediate calcium-activated potassium channels counterbalance the impaired endothelium-dependent vasodilation in stroke-prone spontaneously hypertensive rats. Transl. Res. 2009, 154, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Hilgers, R.H.; Webb, R.C. Reduced expression of SKCa and IKCa channel proteins in rat small mesenteric arteries during angiotensin II-induced hypertension. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H2275–H2284. [Google Scholar] [CrossRef] [PubMed]
- Chinnathambi, V.; Yallampalli, C.; Sathishkumar, K. Prenatal testosterone induces sex-specific dysfunction in endothelium-dependent relaxation pathways in adult male and female rats. Biol. Reprod. 2013, 89, 97. [Google Scholar] [CrossRef] [PubMed]
- Chaston, D.J.; Haddock, R.E.; Howitt, L.; Morton, S.K.; Brown, R.D.; Matthaei, K.I.; Hill, C.E. Perturbation of chemical coupling by an endothelial Cx40 mutant attenuates endothelium-dependent vasodilation by KCa channels and elevates blood pressure in mice. Pflugers. Arch. 2015, 467, 1997–2009. [Google Scholar] [CrossRef] [PubMed]
- Kansui, Y.; Fujii, K.; Nakamura, K.; Goto, K.; Oniki, H.; Abe, I.; Shibata, Y.; Iida, M. Angiotensin II receptor blockade corrects altered expression of gap junctions in vascular endothelial cells from hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2004, 287, H216–H224. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Rummery, N.M.; Grayson, T.H.; Hill, C.E. Attenuation of conducted vasodilatation in rat mesenteric arteries during hypertension: Role of inwardly rectifying potassium channels. J. Physiol. 2004, 561, 215–231. [Google Scholar] [CrossRef] [PubMed]
- Sandow, S.L.; Neylon, C.B.; Chen, M.X.; Garland, C.J. Spatial separation of endothelial small- and intermediate-conductance calcium-activated potassium channels (K(Ca)) and connexins: Possible relationship to vasodilator function? J. Anat. 2006, 209, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Dora, K.A.; Gallagher, N.T.; McNeish, A.; Garland, C.J. Modulation of endothelial cell KCa3.1 channels during endothelium-derived hyperpolarizing factor signaling in mesenteric resistance arteries. Circ. Res. 2008, 102, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Coleman, H.A.; Tare, M.; Parkington, H.C. Nonlinear effects of potassium channel blockers on endothelium-dependent hyperpolarization. Acta Physiol. 2017, 219, 324–334. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.F.; Suzuki, H. Calcium dependency of the endothelium-dependent hyperpolarization in smooth muscle cells of the rabbit carotid artery. J. Physiol. 1990, 421, 521–534. [Google Scholar] [CrossRef] [PubMed]
- Fukao, M.; Hattori, Y.; Kanno, M.; Sakuma, I.; Kitabatake, A. Sources of Ca2+ in relation to generation of acetylcholine-induced endothelium-dependent hyperpolarization in rat mesenteric artery. Br. J. Pharmacol. 1997, 120, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Boudaka, A.; Al-Suleimani, M.; BaOmar, H.; Al-Lawati, I.; Zadjali, F. Impairment of transient receptor potential Vanilloid 4-Mediated dilation in Mesenteric arteries of spontaneously hypertensive rats. Proc. Physiol. Soc. 2016, 37, PCA124. [Google Scholar]
- Zhang, D.X.; Mendoza, S.A.; Bubolz, A.H.; Mizuno, A.; Ge, Z.D.; Li, R.; Warltier, D.C.; Suzuki, M.; Gutterman, D.D. Transient receptor potential vanilloid type 4-deficient mice exhibit impaired endothelium-dependent relaxation induced by acetylcholine in vitro and in vivo. Hypertension 2009, 53, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Sui, D.; Garavito, R.M.; Worden, R.M.; Wang, D.H. Salt intake augments hypotensive effects of transient receptor potential vanilloid 4: Functional significance and implication. Hypertension 2009, 53, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Nishijima, Y.; Zheng, X.; Lund, H.; Suzuki, M.; Mattson, D.L.; Zhang, D.X. Characterization of blood pressure and endothelial function in TRPV4-deficient mice with l-NAME- and angiotensin II-induced hypertension. Physiol. Rep. 2014, 2, e00199. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Pan, Q.; Chen, Z.; Sun, C.; Zhang, P.; Mao, A.; Zhu, Y.; Li, H.; Lu, C.; Xie, M.; et al. Treatment of hypertension by increasing impaired endothelial TRPV4-KCa2.3 interaction. EMBO Mol. Med. 2017, 9, 1491–1503. [Google Scholar] [CrossRef] [PubMed]
- Rath, G.; Dessy, C.; Feron, O. Caveolae, caveolin and control of vascular tone: Nitric oxide (NO) and endothelium derived hyperpolarizing factor (EDHF) regulation. J. Physiol. Pharmacol. 2009, 60 (Suppl. 4), 105–109. [Google Scholar] [PubMed]
- Haddy, F.J.; Vanhoutte, P.M.; Feletou, M. Role of potassium in regulating blood flow and blood pressure. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2006, 290, R546–R552. [Google Scholar] [CrossRef] [PubMed]
- McCarron, J.G.; Halpern, W. Impaired potassium-induced dilation in hypertensive rat cerebral arteries does not reflect altered Na+,K(+)-ATPase dilation. Circ. Res. 1990, 67, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Chrissobolis, S.; Sobey, C.G. Inwardly rectifying potassium channels in the regulation of vascular tone. Curr. Drug Targets 2003, 4, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Overbeck, H.W.; Derifield, R.S.; Pamnani, M.B.; Sözen, T. Attenuated vasodilator responses to K+ in essential hypertensive men. J. Clin. Investig. 1974, 53, 678–686. [Google Scholar] [CrossRef] [PubMed]
- Quayle, J.M.; Nelson, M.T.; Standen, N.B. ATP-sensitive and inwardly rectifying potassium channels in smooth muscle. Physiol. Rev. 1997, 77, 1165–1232. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.E. Inward rectification and vascular function: As it was in the beginning. J. Physiol. 2008, 586, 1465–1467. [Google Scholar] [CrossRef] [PubMed]
- Doughty, J.M.; Boyle, J.P.; Langton, P.D. Blockade of chloride channels reveals relaxations of rat small mesenteric arteries to raised potassium. Br. J. Pharmacol. 2001, 132, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Crane, G.J.; Walker, S.D.; Dora, K.A.; Garland, C.J. Evidence for a differential cellular distribution of inward rectifier K channels in the rat isolated mesenteric artery. J. Vasc. Res. 2003, 40, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Dora, K.A.; Garland, C.J. Properties of smooth muscle hyperpolarization and relaxation to K+ in the rat isolated mesenteric artery. Am. J. Physiol. Heart Circ. Physiol. 2001, 280, H2424–H2429. [Google Scholar] [CrossRef] [PubMed]
- Sonkusare, S.K.; Dalsgaard, T.; Bonev, A.D.; Nelson, M.T. Inward rectifier potassium (Kir2.1) channels as end-stage boosters of endothelium-dependent vasodilators. J. Physiol. 2016, 594, 3271–3285. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Fancher, I.S.; Bian, J.T.; Zhang, C.X.; Schwab, S.; Gaffin, R.; Phillips, S.A.; Levitan, I. Inwardly rectifying K+ channels are major contributors to flow-induced vasodilatation in resistance arteries. J. Physiol. 2017, 595, 2339–2364. [Google Scholar] [CrossRef] [PubMed]
- Iddings, J.A.; Kim, K.J.; Zhou, Y.; Higashimori, H.; Filosa, J.A. Enhanced parenchymal arteriole tone and astrocyte signaling protect neurovascular coupling mediated parenchymal arteriole vasodilation in the spontaneously hypertensive rat. J. Cereb. Blood Flow Metab. 2015, 35, 1127–1136. [Google Scholar] [CrossRef] [PubMed]
- Longden, T.A.; Nelson, M.T. Vascular inward rectifier K+ channels as external K+ sensors in the control of cerebral blood flow. Microcirculation 2015, 22, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Tajada, S.; Cidad, P.; Moreno-Domínguez, A.; Pérez-García, M.T.; López-López, J.R. High blood pressure associates with the remodelling of inward rectifier K+ channels in mice mesenteric vascular smooth muscle cells. J. Physiol. 2012, 590, 6075–6091. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Edwards, F.R.; Hill, C.E. Depolarization evoked by acetylcholine in mesenteric arteries of hypertensive rats attenuates endothelium-dependent hyperpolarizing factor. J. Hypertens. 2007, 25, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Kwan, Y.W.; Chan, S.W.; Lee, S.M.; Leung, G.P. Potentiation of EDHF-mediated relaxation by chloride channel blockers. Acta Pharmacol. Sin. 2010, 31, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Jackson, W.F. KV channels and the regulation of vascular smooth muscle tone. Microcirculation 2018, 25, e12421. [Google Scholar] [CrossRef] [PubMed]
- Nieves-Cintrón, M.; Syed, A.U.; Nystoriak, M.A.; Navedo, M.F. Regulation of voltage-gated potassium channels in vascular smooth muscle during hypertension and metabolic disorders. Microcirculation 2018, 25, e12423. [Google Scholar] [CrossRef] [PubMed]
- Quignard, J.F.; Feletou, M.; Edwards, G.; Duhault, J.; Weston, A.H.; Vanhoutte, P.M. Role of endothelial cell hyperpolarization in EDHF-mediated responses in the guinea-pig carotid artery. Br. J. Pharmacol. 2000, 129, 1103–1112. [Google Scholar] [CrossRef] [PubMed]
- Sadanaga, T.; Ohya, Y.; Ohtsubo, T.; Goto, K.; Fujii, K.; Abe, I. Decreased 4-aminopyridine sensitive K+ currents in endothelial cells from hypertensive rats. Hypertens. Res. 2002, 25, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Kitazono, T.; Heistad, D.D.; Faraci, F.M. ATP-sensitive potassium channels in the basilar artery during chronic hypertension. Hypertension 1993, 22, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Ohya, Y.; Setoguchi, M.; Fujii, K.; Nagao, T.; Abe, I.; Fujishima, M. Impaired action of levcromakalim on ATP-sensitive K+ channels in mesenteric artery cells from spontaneously hypertensive rats. Hypertension 1996, 27, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Ishizaka, H.; Kuo, L. Endothelial, ATP-sensitive potassium channels mediate coronary microvascular dilation to hyperosmolarity. Am. J. Physiol. 1997, 273, H104–H112. [Google Scholar] [CrossRef] [PubMed]
- Aziz, Q.; Li, Y.; Anderson, N.; Ojake, L.; Tsisanova, E.; Tinker, A. Molecular and functional characterization of the endothelial ATP-sensitive potassium channel. J. Biol. Chem. 2017, 292, 17587–17597. [Google Scholar] [CrossRef] [PubMed]
- Rogers, P.A.; Dick, G.M.; Knudson, J.D.; Focardi, M.; Bratz, I.N.; Swafford, A.N., Jr.; Saitoh, S.; Tune, J.D.; Chilian, W.M. H2O2-induced redox-sensitive coronary vasodilation is mediated by 4-aminopyridine-sensitive K+ channels. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H2473–H2482. [Google Scholar] [CrossRef] [PubMed]
- Lacza, Z.; Puskar, M.; Kis, B.; Perciaccante, J.V.; Miller, A.W.; Busija, D.W. Hydrogen peroxide acts as an EDHF in the piglet pial vasculature in response to bradykinin. Am. J. Physiol. Heart Circ. Physiol. 2002, 283, H406–H411. [Google Scholar] [CrossRef] [PubMed]
- Cheang, W.S.; Wong, W.T.; Shen, B.; Lau, C.W.; Tian, X.Y.; Tsang, S.Y.; Yao, X.; Chen, Z.Y.; Huang, Y. 4-aminopyridine-sensitive K+ channels contributes to NaHS-induced membrane hyperpolarization and relaxation in the rat coronary artery. Vascul. Pharmacol. 2010, 53, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.J.; Zhang, Y.; Hirota, S.; Janssen, L.J.; Lee, R.M. Vascular relaxation response to hydrogen peroxide is impaired in hypertension. Br. J. Pharmacol. 2004, 142, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Meng, G.; Ma, Y.; Xie, L.; Ferro, A.; Ji, Y. Emerging role of hydrogen sulfide in hypertension and related cardiovascular diseases. Br. J. Pharmacol. 2015, 172, 5501–5511. [Google Scholar] [CrossRef] [PubMed]
- Greaney, J.L.; Kutz, J.L.; Shank, S.W.; Jandu, S.; Santhanam, L.; Alexander, L.M. Impaired hydrogen sulfide-mediated vasodilation contributes to microvascular endothelial dysfunction in hypertensive adults. Hypertension 2017, 69, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Large, W.A.; Wang, Q. Characteristics and physiological role of the Ca(2+)-activated Cl- conductance in smooth muscle. Am. J. Physiol. 1996, 271, C435–C454. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Suzuki, H. Dependency of endothelial cell function on vascular smooth muscle cells in guinea-pig mesenteric arteries and arterioles. J. Smooth Muscle Res. 2005, 41, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Groschner, K.; Graier, W.F.; Kukovetz, W.R. Histamine induces K+, Ca2+, and Cl- currents in human vascular endothelial cells. Role of ionic currents in stimulation of nitric oxide biosynthesis. Circ. Res. 1994, 75, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Nilius, B.; Prenen, J.; Szücs, G.; Wei, L.; Tanzi, F.; Voets, T.; Droogmans, G. Calcium-activated chloride channels in bovine pulmonary artery endothelial cells. J. Physiol. 1997, 498, 381–396. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Suzuki, H. Effects of increased intracellular Cl- concentration on membrane responses to acetylcholine in the isolated endothelium of guinea pig mesenteric arteries. J. Physiol. Sci. 2007, 57, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.D.; Cho, H.; Koo, J.Y.; Tak, M.H.; Cho, Y.; Shim, W.S.; Park, S.P.; Lee, J.; Lee, B.; Kim, B.M.; et al. TMEM16A confers receptor-activated calcium-dependent chloride conductance. Nature 2008, 455, 1210–1215. [Google Scholar] [CrossRef] [PubMed]
- Caputo, A.; Caci, E.; Ferrera, L.; Pedemonte, N.; Barsanti, C.; Sondo, E.; Pfeffer, U.; Ravazzolo, R.; Zegarra-Moran, O.; Galietta, L.J. TMEM16A, a membrane protein associated with calcium-dependent chloride channel activity. Science 2008, 322, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, B.C.; Cheng, T.; Jan, Y.N.; Jan, L.Y. Expression cloning of TMEM16A as a calcium-activated chloride channel subunit. Cell 2008, 134, 1019–1029. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Li, C.; Huai, R.; Qu, Z. Overexpression of ANO1/TMEM16A, an arterial Ca2+-activated Cl- channel, contributes to spontaneous hypertension. J. Mol. Cell. Cardiol. 2015, 82, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.M.; Gao, M.; Guo, K.M.; Wang, M.; Li, X.Y.; Zeng, X.L.; Sun, L.; Lv, X.F.; Du, Y.H.; Wang, G.L.; et al. TMEM16A Contributes to Endothelial Dysfunction by Facilitating Nox2 NADPH Oxidase-Derived Reactive Oxygen Species Generation in Hypertension. Hypertension 2017, 69, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Hutri-Kähönen, N.; Kähönen, M.; Tolvanen, J.P.; Wu, X.; Sallinen, K.; Pörsti, I. Ramipril therapy improves arterial dilation in experimental hypertension. Cardiovasc. Res. 1997, 33, 188–195. [Google Scholar] [CrossRef]
- Onaka, U.; Fujii, K.; Abe, I.; Fujishima, M. Antihypertensive treatment improves endothelium-dependent hyperpolarization in the mesenteric artery of spontaneously hypertensive rats. Circulation 1998, 98, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Kähönen, M.; Tolvanen, J.P.; Kalliovalkama, J.; Wu, X.; Karjala, K.; Mäkynen, H.; Pörsti, I. Losartan and enalapril therapies enhance vasodilatation in the mesenteric artery of spontaneously hypertensive rats. Eur. J. Pharmacol. 1999, 368, 213–222. [Google Scholar] [CrossRef]
- Goto, K.; Fujii, K.; Onaka, U.; Abe, I.; Fujishima, M. Renin-angiotensin system blockade improves endothelial dysfunction in hypertension. Hypertension 2000, 36, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Vettoretti, S.; Ochodnicky, P.; Buikema, H.; Henning, R.H.; Kluppel, C.A.; de Zeeuw, D.; van Dokkum, R.P. Altered myogenic constriction and endothelium-derived hyperpolarizing factor-mediated relaxation in small mesenteric arteries of hypertensive subtotally nephrectomized rats. J. Hypertens. 2006, 24, 2215–2223. [Google Scholar] [CrossRef] [PubMed]
- Seki, T.; Goto, K.; Kansui, Y.; Ohtsubo, T.; Matsumura, K.; Kitazono, T. Angiotensin II Receptor-Neprilysin Inhibitor Sacubitril/Valsartan Improves Endothelial Dysfunction in Spontaneously Hypertensive Rats. J. Am. Heart Assoc. 2017, 6, E006617. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Fujii, K.; Onaka, U.; Abe, I.; Fujishima, M. Angiotensin-converting enzyme inhibitor prevents age-related endothelial dysfunction. Hypertension 2000, 36, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Kansui, Y.; Fujii, K.; Goto, K.; Abe, I.; Iida, M. Angiotensin II receptor antagonist improves age-related endothelial dysfunction. J. Hypertens. 2002, 20, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Albarwani, S.; Al-Siyabi, S.; Al-Husseini, I.; Al-Ismail, A.; Al-Lawati, I.; Al-Bahrani, I.; Tanira, M.O. Lisinopril alters contribution of nitric oxide and K(Ca) channels to vasodilatation in small mesenteric arteries of spontaneously hypertensive rats. Physiol. Res. 2015, 64, 39–49. [Google Scholar] [PubMed]
- More, A.S.; Mishra, J.S.; Hankins, G.D.; Yallampalli, C.; Sathishkumar, K. Enalapril normalizes endothelium-derived hyperpolarizing factor-mediated relaxation in mesenteric artery of adult hypertensive rats prenatally exposed to testosterone. Biol. Reprod. 2015, 92, 155. [Google Scholar] [CrossRef] [PubMed]
- Toro, L.; Amador, M.; Stefani, E. ANG II inhibits calcium-activated potassium channels from coronary smooth muscle in lipid bilayers. Am. J. Physiol. 1990, 258, H912–H915. [Google Scholar] [CrossRef] [PubMed]
- Minami, K.; Hirata, Y.; Tokumura, A.; Nakaya, Y.; Fukuzawa, K. Protein kinase C-independent inhibition of the Ca(2+)-activated K+ channel by angiotensin II and endothelin-1. Biochem. Pharmacol. 1995, 49, 1051–1056. [Google Scholar] [CrossRef]
- Zhao, L.M.; Wang, Y.; Ma, X.Z.; Wang, N.P.; Deng, X.L. Advanced glycation end products impair K(Ca)3.1- and K(Ca)2.3-mediated vasodilatation via oxidative stress in rat mesenteric arteries. Pflugers. Arch. 2014, 466, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Kaw, S.; Hecker, M. Endothelium-derived hyperpolarizing factor, but not nitric oxide or prostacyclin release, is resistant to menadione-induced oxidative stress in the bovine coronary artery. Naunyn. Schmiedebergs. Arch. Pharmacol. 1999, 359, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, C.A.; McPhaden, A.R.; Berg, G.; Pathi, V.; Dominiczak, A.F. Is hydrogen peroxide an EDHF in human radial arteries? Am. J. Physiol. Heart Circ. Physiol. 2001, 280, H2451–H2455. [Google Scholar] [CrossRef] [PubMed]
- Louis, W.J.; Howes, L.G. Genealogy of the spontaneously hypertensive rat and Wistar-Kyoto rat strains: Implications for studies of inherited hypertension. J. Cardiovasc. Pharmacol. 1990, 16 (Suppl. 7), S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Matthaei, K.I. Identification of therapeutic drug targets through genetically manipulated mice: Are we getting it right? Pharmacol. Ther. 2009, 123, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Bellien, J.; Thuillez, C.; Joannides, R. Contribution of endothelium-derived hyperpolarizing factors to the regulation of vascular tone in humans. Fundam. Clin. Pharmacol. 2008, 22, 363–377. [Google Scholar] [CrossRef] [PubMed]
- Taddei, S.; Ghiadoni, L.; Virdis, A.; Buralli, S.; Salvetti, A. Vasodilation to bradykinin is mediated by an ouabain-sensitive pathway as a compensatory mechanism for impaired nitric oxide availability in essential hypertensive patients. Circulation 1999, 100, 1400–1405. [Google Scholar] [CrossRef] [PubMed]
- Taddei, S.; Versari, D.; Cipriano, A.; Ghiadoni, L.; Galetta, F.; Franzoni, F.; Magagna, A.; Virdis, A.; Salvetti, A. Identification of a cytochrome P450 2C9-derived endothelium-derived hyperpolarizing factor in essential hypertensive patients. J. Am. Coll. Cardiol. 2006, 48, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, C.A.; Coleman, J.; Brady, A.J.; Connell, J.M.; Hillier, C.; Petrie, J.R. Endothelium-dependent relaxation is resistant to inhibition of nitric oxide synthesis, but sensitive to blockade of calcium-activated potassium channels in essential hypertension. J. Hum. Hypertens. 2007, 21, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhou, Z.; Jiang, D.J.; Li, D.; Tan, B.; Liu, H.; Li, Y.J. Reduction of NO- and EDHF-mediated vasodilatation in hypertension: Role of asymmetric dimethylarginine. Clin. Exp. Hypertens. 2007, 29, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Kenny, L.C.; Baker, P.N.; Kendall, D.A.; Randall, M.D.; Dunn, W.R. Differential mechanisms of endothelium-dependent vasodilator responses in human myometrial small arteries in normal pregnancy and pre-eclampsia. Clin. Sci. 2002, 103, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Luksha, L.; Luksha, N.; Kublickas, M.; Nisell, H.; Kublickiene, K. Diverse mechanisms of endothelium-derived hyperpolarizing factor-mediated dilatation in small myometrial arteries in normal human pregnancy and preeclampsia. Biol. Reprod. 2010, 83, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Goulopoulou, S. Maternal Vascular Physiology in Preeclampsia. Hypertension 2017, 70, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Kim, J.A.; Na, H.Y.; Kim, J.E.; Park, S.; Han, K.H.; Kim, Y.J.; Suh, S.H. NADPH oxidase 2-derived superoxide downregulates endothelial KCa3.1 in preeclampsia. Free Radic. Biol. Med. 2013, 57, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Deja, M.A.; Gołba, K.S.; Widenka, K.; Mrozek, R.; Biernat, J.; Kolowca, M.; Malinowski, M.; Woś, S. Angiotensin-converting enzyme inhibitors reveal non-NO-, non-prostacycline-mediated endothelium-dependent relaxation in internal thoracic artery of hypertensive patients. Int. J. Cardiol. 2005, 102, 455–460. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goto, K.; Ohtsubo, T.; Kitazono, T. Endothelium-Dependent Hyperpolarization (EDH) in Hypertension: The Role of Endothelial Ion Channels. Int. J. Mol. Sci. 2018, 19, 315. https://doi.org/10.3390/ijms19010315
Goto K, Ohtsubo T, Kitazono T. Endothelium-Dependent Hyperpolarization (EDH) in Hypertension: The Role of Endothelial Ion Channels. International Journal of Molecular Sciences. 2018; 19(1):315. https://doi.org/10.3390/ijms19010315
Chicago/Turabian StyleGoto, Kenichi, Toshio Ohtsubo, and Takanari Kitazono. 2018. "Endothelium-Dependent Hyperpolarization (EDH) in Hypertension: The Role of Endothelial Ion Channels" International Journal of Molecular Sciences 19, no. 1: 315. https://doi.org/10.3390/ijms19010315
APA StyleGoto, K., Ohtsubo, T., & Kitazono, T. (2018). Endothelium-Dependent Hyperpolarization (EDH) in Hypertension: The Role of Endothelial Ion Channels. International Journal of Molecular Sciences, 19(1), 315. https://doi.org/10.3390/ijms19010315



