High Levels of Serum Ubiquitin and Proteasome in a Case of HLA-B27 Uveitis
Abstract
:1. Introduction
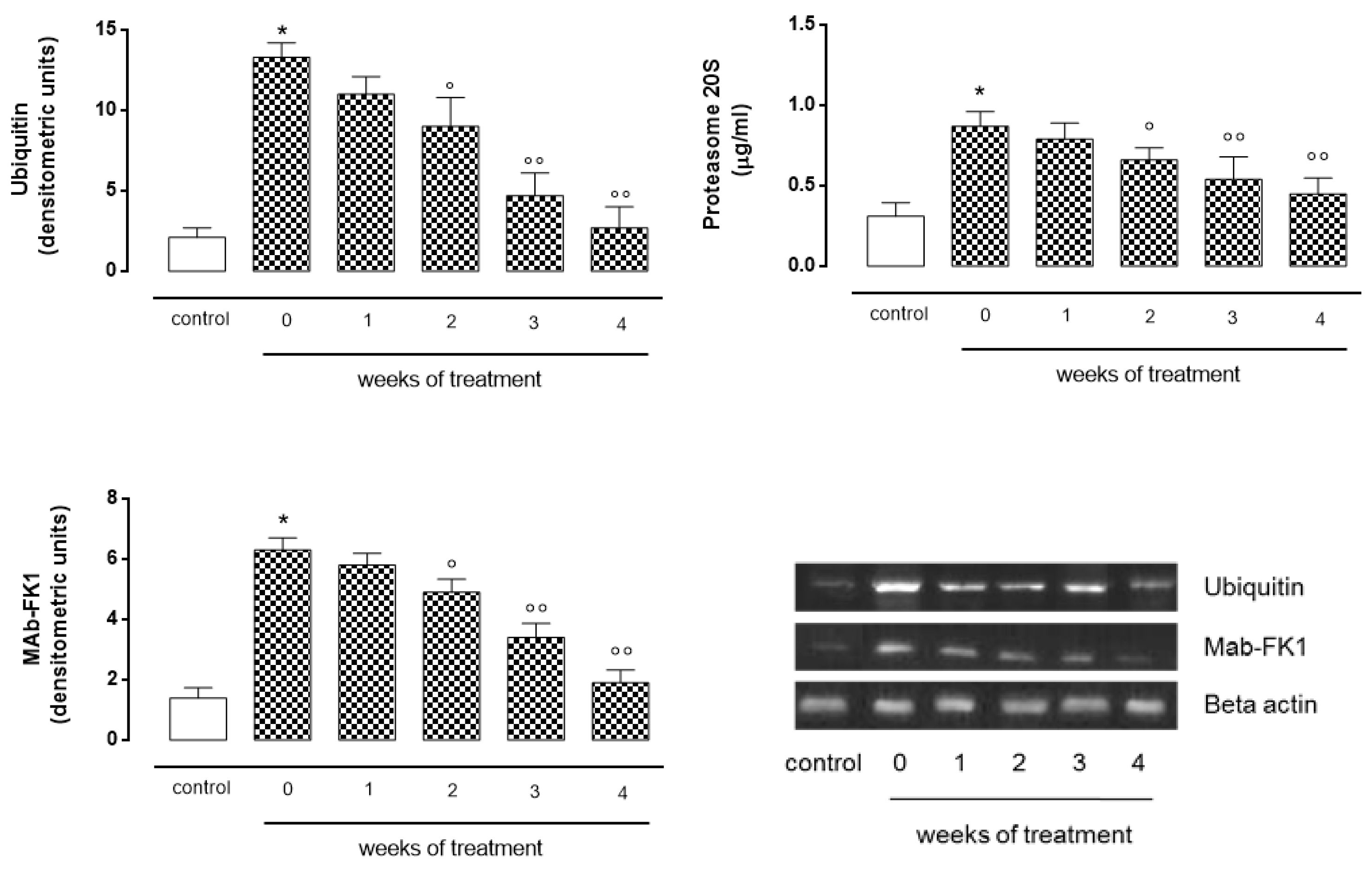
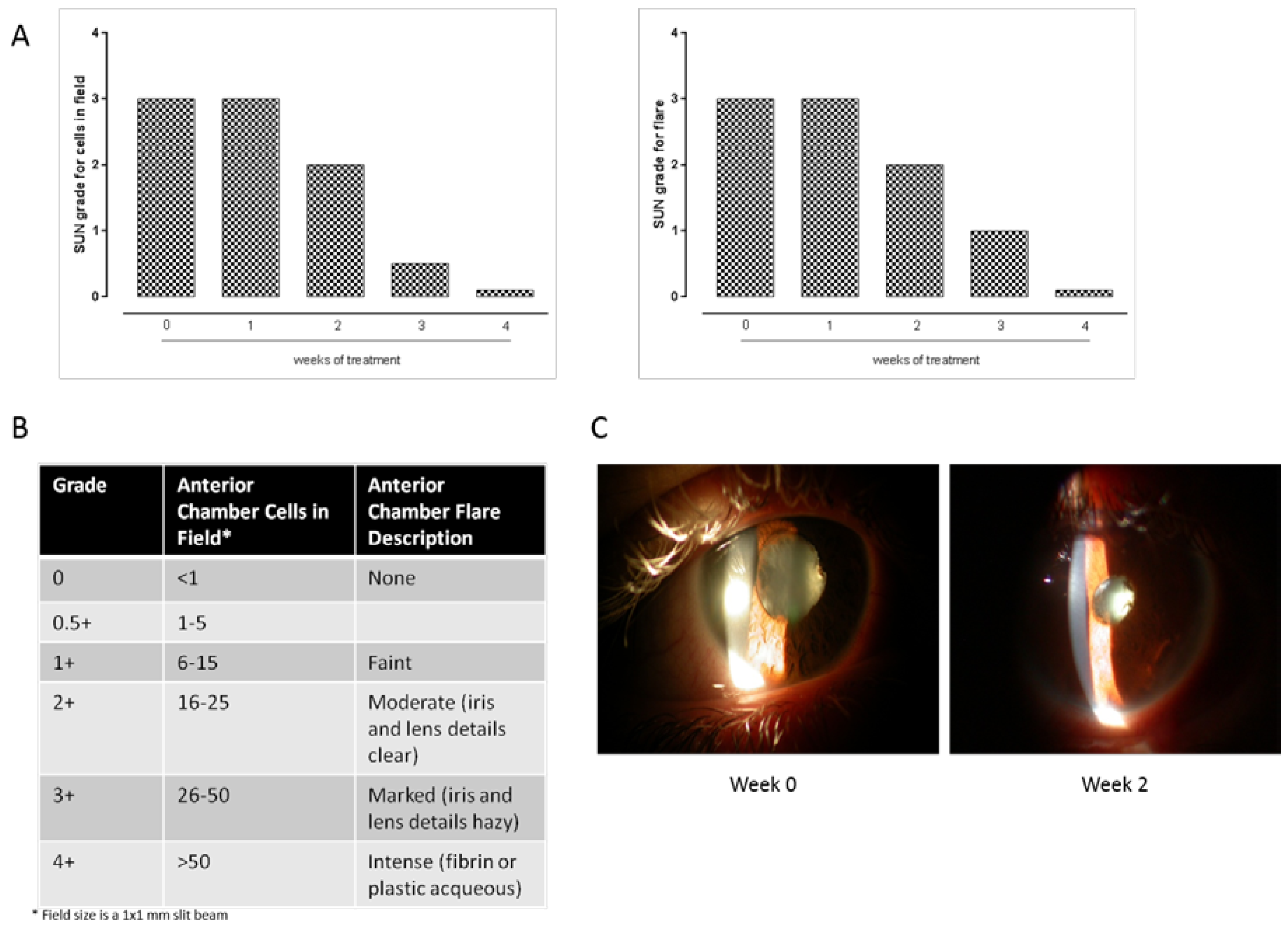
2. Case Presentation
3. Discussion
Author Contributions
Conflicts of Interest
References
- Marfella, R.; di Filippo, C.; Portoghese, M. The ubiquiti–proteasome system contributes to the inflammatory injury in ischemic diabetic myocardium: The role of glycemic control. Cardiovasc Pathol. 2009, 18, 332–345. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.T.; Liu, Y.C.; Yang, C.M.; Yang, C.H. Anti-inflammatory effect of the proteasome inhibitor bortezomib on endotoxin-induced uveitis in rats. Investig. Ophthalmol. Vis. Sci. 2012, 53, 3682–3694. [Google Scholar] [CrossRef] [PubMed]
- Hwee, D.T.; Gomes, A.V.; Bodine, S.C. Cardiac proteasome activity in muscle ring finger-1 null mice at rest and following synthetic glucocorticoid treatment. Am. J. Physiol. Endocrinol. Metab. 2011, 301, 967–977. [Google Scholar] [CrossRef] [PubMed]
- Jabs, D.A.; Rosenbaum, J.T.; Foster, C.S.; Holland, G.N.; Jaffe, G.J.; Louie, J.S.; Nussenblatt, R.B.; Stiehm, E.R.; Tessler, H.; van Gelder, R.N.; et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: Recommendations of an expert panel. Am. J. Ophthalmol. 2000, 130, 492–513. [Google Scholar] [CrossRef]
- Nussenblatt, R.B.; Fortin, E.; Schiffman, R.; Rizzo, L.; Smith, J.; van Veldhuisen, P.; Sran, P.; Yaffe, A.; Goldman, C.K.; Waldmann, T.A.; et al. Treatment of non-infectious intermediate and posterior uveitis with the humanized anti-Tac mAb: A phase I/II clinical trial. Proc. Natl. Acad. Sci. USA 1999, 96, 7462–7466. [Google Scholar] [CrossRef] [PubMed]
- Kotter, I.; Zierhut, M.; Eckstein, A.; Vonthein, R.; Ness, T.; Günaydin, I.; Grimbacher, B.; Blaschke, S.; Meyer-Riemann, W.; Peter, H.H.; et al. Human recombinant interferon-α2a (rhIFN α2a) for the treatment of Behçet’s disease with sight-threatening retinal vasculitis. Adv. Exp. Med. Biol. 2003, 528, 521–523. [Google Scholar] [PubMed]
- Hale, S.; Lightman, S. Anti-TNF therapies in the management of acute and chronic uveitis. Cytokine 2006, 33, 231–237. [Google Scholar] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, S.; Gesualdo, C.; Maisto, R.; Trotta, M.C.; Di Carluccio, N.; Brigida, A.; Di Iorio, V.; Testa, F.; Simonelli, F.; D’Amico, M.; et al. High Levels of Serum Ubiquitin and Proteasome in a Case of HLA-B27 Uveitis. Int. J. Mol. Sci. 2017, 18, 505. https://doi.org/10.3390/ijms18030505
Rossi S, Gesualdo C, Maisto R, Trotta MC, Di Carluccio N, Brigida A, Di Iorio V, Testa F, Simonelli F, D’Amico M, et al. High Levels of Serum Ubiquitin and Proteasome in a Case of HLA-B27 Uveitis. International Journal of Molecular Sciences. 2017; 18(3):505. https://doi.org/10.3390/ijms18030505
Chicago/Turabian StyleRossi, Settimio, Carlo Gesualdo, Rosa Maisto, Maria Consiglia Trotta, Nadia Di Carluccio, Annalisa Brigida, Valentina Di Iorio, Francesco Testa, Francesca Simonelli, Michele D’Amico, and et al. 2017. "High Levels of Serum Ubiquitin and Proteasome in a Case of HLA-B27 Uveitis" International Journal of Molecular Sciences 18, no. 3: 505. https://doi.org/10.3390/ijms18030505
APA StyleRossi, S., Gesualdo, C., Maisto, R., Trotta, M. C., Di Carluccio, N., Brigida, A., Di Iorio, V., Testa, F., Simonelli, F., D’Amico, M., & Di Filippo, C. (2017). High Levels of Serum Ubiquitin and Proteasome in a Case of HLA-B27 Uveitis. International Journal of Molecular Sciences, 18(3), 505. https://doi.org/10.3390/ijms18030505





