Hepatoma-Derived Growth Factor Upregulation Is Correlated with Prognostic Factors of Early-Stage Cervical Adenocarcinoma
Abstract
:1. Introduction
2. Results and Discussion
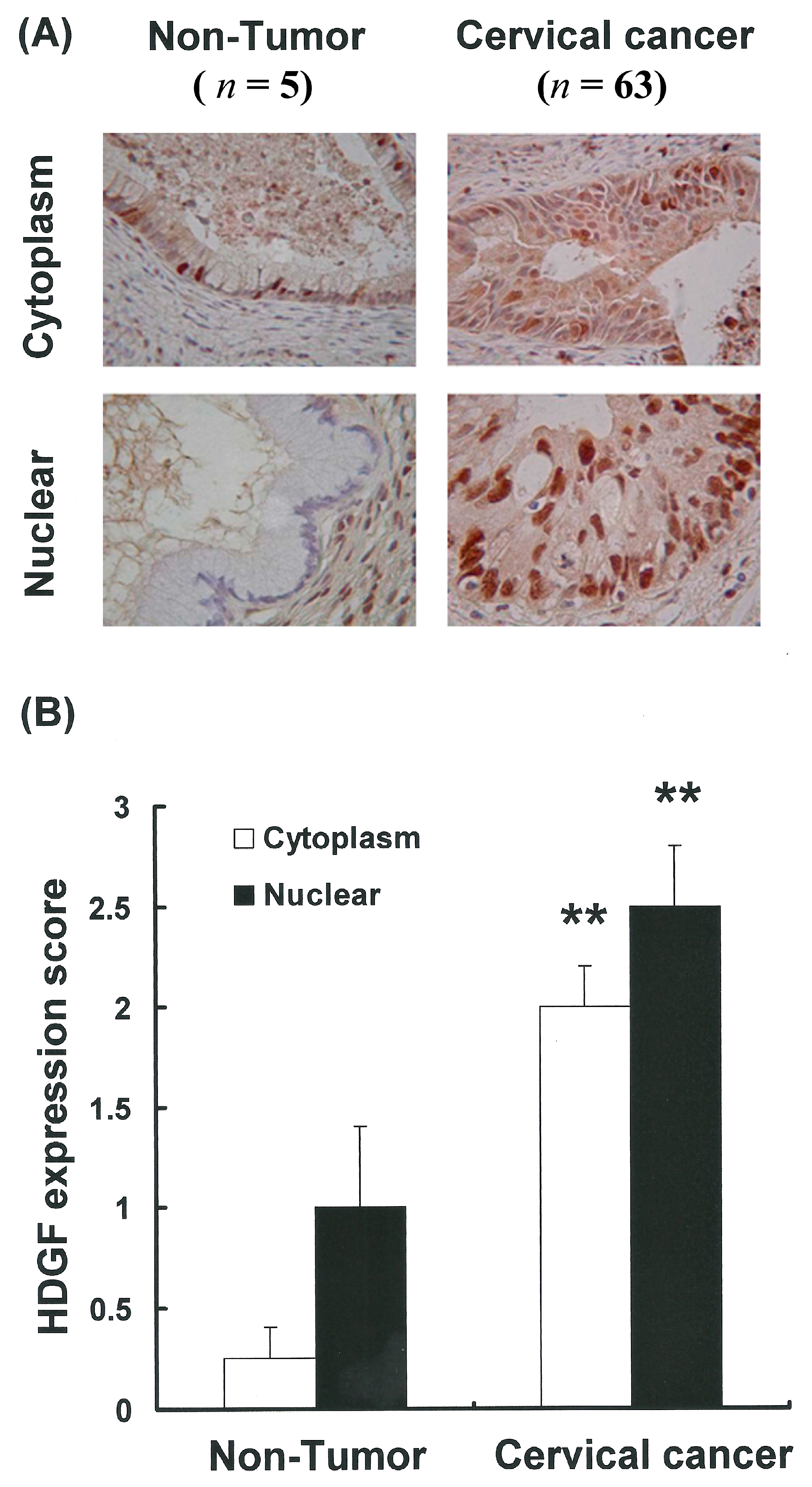
2.1. HDGF Expression and Location in the Tumor and Non-Tumor Specimens
2.2. Upregulation of HDGF Gene Expressions in Cervical Cancer Tissues
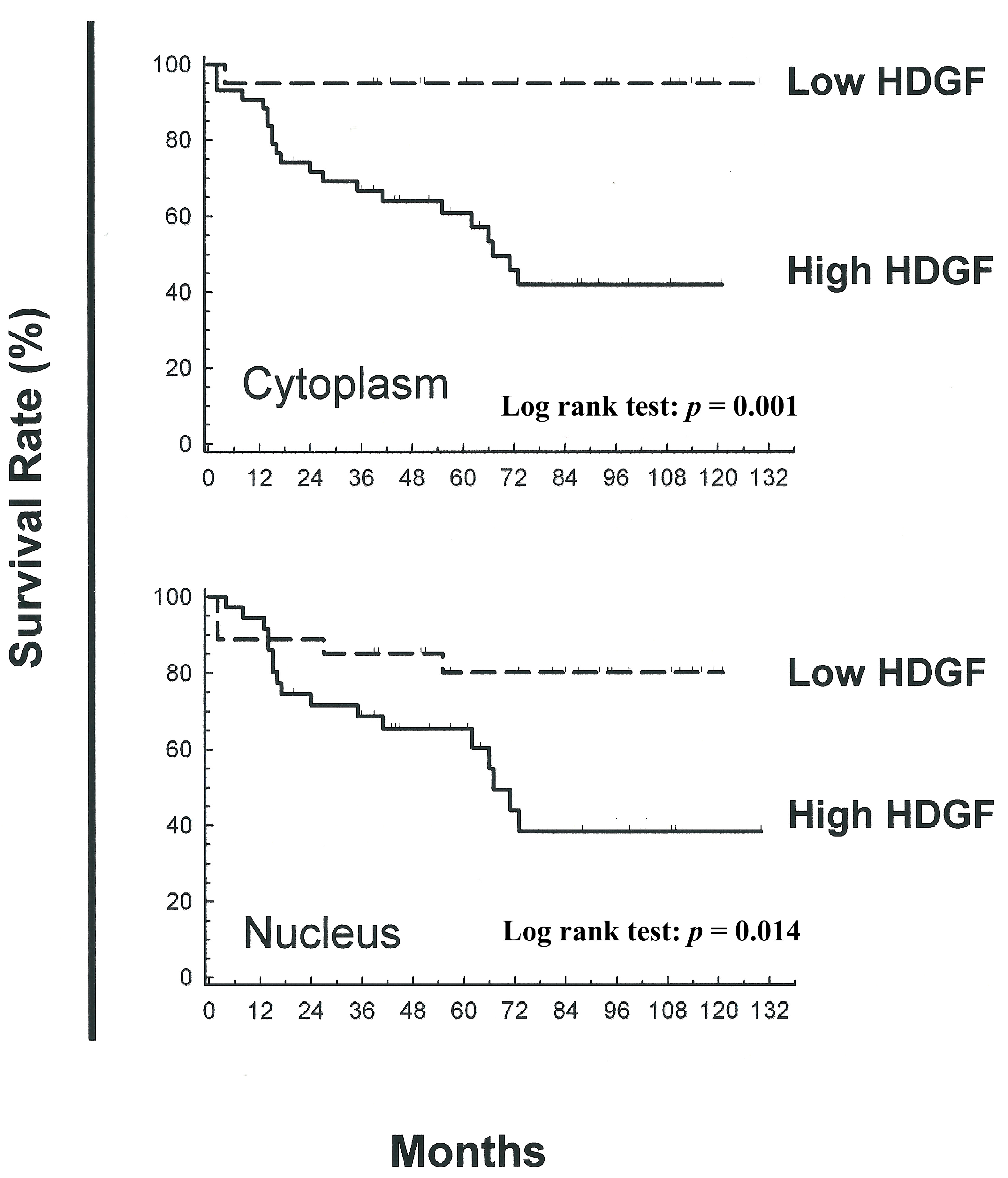
2.3. Association between Nuclear and Cytoplasmic HDGF and Patient Survival
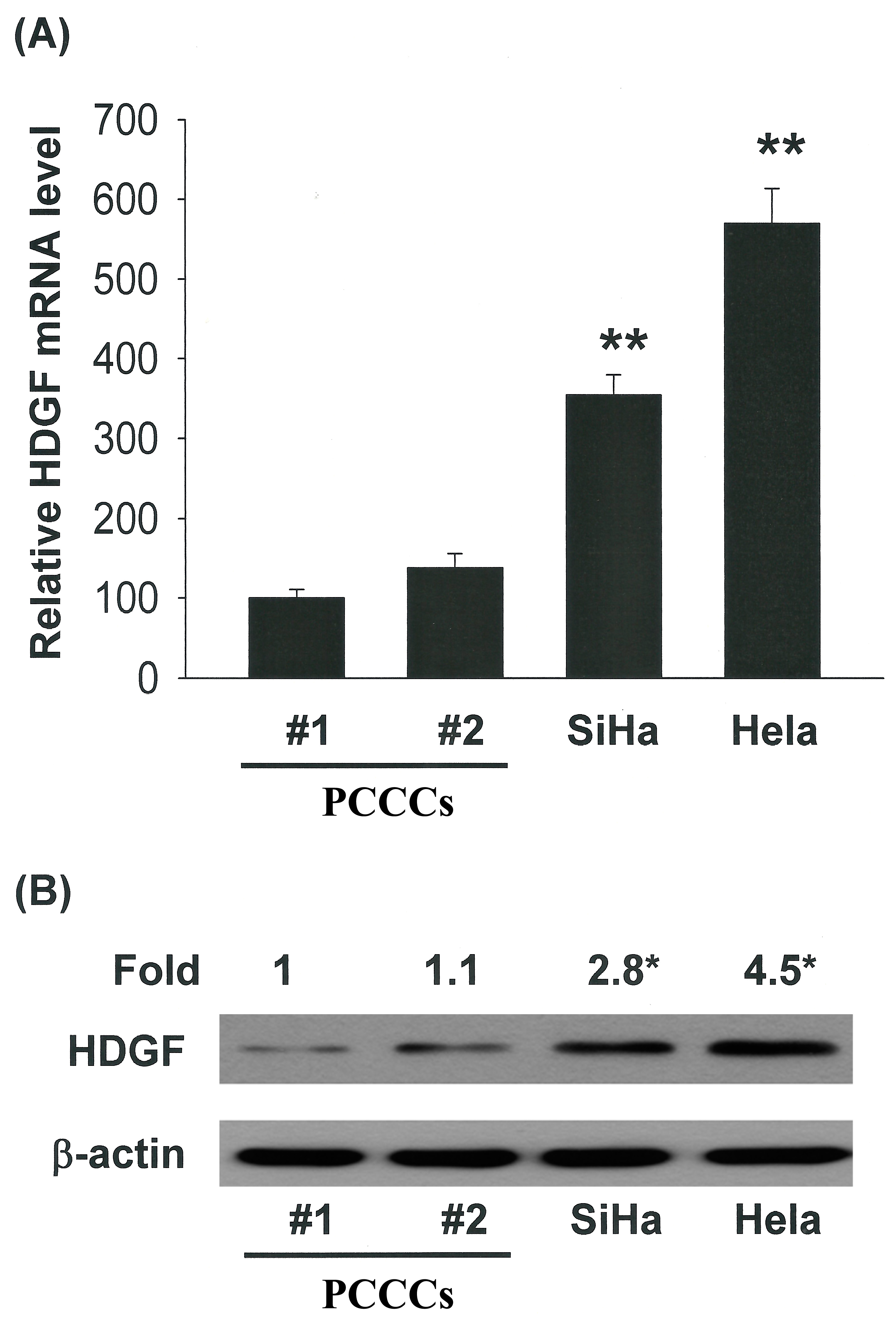
2.4. Correlation of Increased HDGF Expression with Tumorigenicity of Cervical Cancer Cells
2.5. HDGF Stimulated Cervical Cancer Cell Proliferation
2.6. The Cellular HDGF Level Regulates the Tumorigenicity of Cervical Cancer Cells
3. Experimental Section
3.1. Materials
3.2. Study Subjects
3.3. Immunohistochemistry of HDGF in Cervical Adenocarcinoma Clinical Samples
| HDGF (%) | |||
|---|---|---|---|
| Variable | Tumor | Normal | p value |
| LVSI | 85.33 | 45.75 | <0.001 |
| LNM | 86.83 | 50.00 | <0.001 |
| Recurrence | 87.14 | 58.0 | <0.001 |
| AG | 88.75 | 46.87 | <0.001 |
3.4. Immunohistochemical Scoring
3.5. Western Blotting
3.6. Cell Cultures
3.7. Cell Proliferation Assay
3.8. Adenoviruses Gene Delivery
3.9. Statistical Analysis
4. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lorusso, D.; Petrelli, F.; Coinu, A.; Raspagliesi, F.; Barni, S. A systematic review comparing cisplatin and carboplatin plus paclitaxel-based chemotherapy for recurrent or metastatic cervical cancer. Gynecol. Oncol. 2014, 133, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.Y.; Hsu, H.C.; Sun, L.M.; Chanchien, C.C.; Lin, H.; Chen, H.C.; Tseng, C.W.; Ou, Y.C.; Chang, H.Y.; Fang, F.M.; et al. Prognostic value of pretreatment carcinoembryonic antigen after definitive radiotherapy with or without concurrent chemotherapy for squamous cell carcinoma of the uterine cervix. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.C.; Liu, Y.S.; Huang, E.Y.; Huang, S.C.; Chang, H.W.; Tseng, C.W.; ChangChien, C.C. Value of preoperative serum CA125 in early-stage adenocarcinoma of the uterine cervix without pelvic lymph node metastasis. Gynecol. Oncol. 2006, 100, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.C.; Lin, H.; Huang, E.Y.; Huang, S.C.; Hsieh, C.H.; Chang, S.Y.; Chien, C.C. The role of the preoperative serum carcinoembryonic antigen level in early-stage adenocarcinoma of the uterine cervix. Gynecol. Oncol. 2004, 94, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.T.; Palme, C.E.; Morgan, G.J.; Gebski, V.; Wang, A.Y.; Veness, M.J. Predictors of outcome in patients with metastatic cutaneous head and neck squamous cell carcinoma involving cervical lymph nodes: Improved survival with the addition of adjuvant radiotherapy. Head Neck 2012, 34, 1524–1528. [Google Scholar] [CrossRef]
- Lutgendorf, S.K.; Mullen-Houser, E.; Russell, D.; Degeest, K.; Jacobson, G.; Hart, L.; Bender, D.; Anderson, B.; Buekers, T.E.; Goodheart, M.J.; et al. Preservation of immune function in cervical cancer patients during chemoradiation using a novel integrative approach. Brain Behav. Immun. 2010, 24, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Kishima, Y.; Yoshida, K.; Enomoto, H.; Yamamoto, M.; Kuroda, T.; Okuda, Y.; Uyama, H.; Nakamura, H. Antisense oligonucleotides of hepatoma-derived growth factor (HDGF) suppress the proliferation of hepatoma cells. Hepatogastroenterology 2002, 49, 1639–1644. [Google Scholar] [PubMed]
- Enomoto, H.; Yoshida, K.; Kishima, Y.; Okuda, Y.; Nakamura, H. Participation of hepatoma-derived growth factor in the regulation of fetal hepatocyte proliferation. J. Gastroenterol. 2002, 37, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Clermont, F.; Gonzalez, N.S.; Communi, D.; Franken, S.; Dumont, J.E.; Robaye, B. HDGF is dephosphorylated during the early steps of endothelial cell apoptosis in a caspase-dependent way. J. Cell. Biochem. 2008, 104, 1161–1171. [Google Scholar] [CrossRef] [PubMed]
- Everett, A.D.; Lobe, D.R.; Matsumura, M.E.; Nakamura, H.; McNamara, C.A. Hepatoma-derived growth factor stimulates smooth muscle cell growth and is expressed in vascular development. J. Clin. Investig. 2000, 105, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Huang, T.; Jiang, J.; Lv, L.; Li, H.; Xia, S. miR-141 suppresses proliferation and motility of gastric cancer cells by targeting HDGF. Mol. Cell. Biochem. 2014, 388, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Han, Z.; Liu, J.; Zhang, X.; Ren, J.; Yan, L.; Liu, H.; Xu, Z. Upregulation of nucleus HDGF predicts poor prognostic outcome in patients with penile squamous cell carcinoma bypass VEGF-A and Ki-67. Med. Oncol. 2013, 30. [Google Scholar] [CrossRef]
- Zhao, J.; Ma, M.Z.; Ren, H.; Liu, Z.; Edelman, M.J.; Pan, H.; Mao, L. Anti-HDGF targets cancer and cancer stromal stem cells resistant to chemotherapy. Clin. Cancer Res. 2013, 19, 3567–3576. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Shen, J.; Wu, X.; Zhang, B.; Zhang, R.; Weng, H.; Ding, Q.; Tan, Z.; Gao, G.; Mu, J.; et al. Downregulated expression of hepatoma-derived growth factor (HDGF) reduces gallbladder cancer cell proliferation and invasion. Med. Oncol. 2013, 30. [Google Scholar] [CrossRef]
- Ha, G.H.; Kim, J.L.; Breuer, E.K. Correction: TACC3 is essential for EGF-mediated EMT in cervical cancer. PLoS One 2013, 8, e70353. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.F.; Xu, Q.; Ding, J.B.; Zhang, Y.; Du, R.; Ding, Y. CD4+CD25+Foxp3+ Treg and TGF-beta play important roles in pathogenesis of Uygur cervical carcinoma. Eur. J. Gynaecol. Oncol. 2012, 33, 502–507. [Google Scholar] [PubMed]
- Sam, M.R.; Elliott, B.E.; Mueller, C.R. A novel activating role of SRC and STAT3 on HGF transcription in human breast cancer cells. Mol. Cancer 2007, 6. [Google Scholar] [CrossRef]
- Nakagami, H.; Kaneda, Y.; Ogihara, T.; Morishita, R. Endothelial dysfunction in hyperglycemia as a trigger of atherosclerosis. Curr. Diabetes Rev. 2005, 1, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Burgazli, K.M.; Bui, K.L.; Mericliler, M.; Albayrak, A.T.; Parahuleva, M.; Erdogan, A. The effects of different types of statins on proliferation and migration of HGF-induced Human Umbilical Vein Endothelial Cells (HUVECs). Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 2874–2883. [Google Scholar] [PubMed]
- Kusunoki, H.; Taniyama, Y.; Otsu, R.; Rakugi, H.; Morishita, R. Anti-inflammatory effects of hepatocyte growth factor on the vicious cycle of macrophages and adipocytes. Hypertens. Res. 2014, 37, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.M.; Chou, C.Y.; Hsu, Y.C.; Chen, M.J. Influence of HPV16 E6/7 on the expression of FGF2 and FGFR type B in cervical carcinogenesis. Reprod. Sci. 2012, 19, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.M.; Chou, C.Y.; Hsu, Y.C.; Chen, M.J.; Wing, L.Y. The role of human papillomavirus type 16 E6/E7 oncoproteins in cervical epithelial-mesenchymal transition and carcinogenesis. Oncol. Lett. 2012, 3, 667–671. [Google Scholar] [PubMed]
- Cheng, Y.M.; Chen, M.J.; Chen, Y.; Hsu, Y.C. Regulation of Metastatic Action through CXCR4 and HPV16 E6/7 in Cervical Carcinogenesis. Cancer Cell. Microenviron. 2014, 1, 129–133. [Google Scholar]
- Hsu, Y.Y.; Cheng, Y.M.; Hsu, K.F.; Fetzer, S.J.; Chou, C.Y. Knowledge and beliefs about cervical cancer and human papillomavirus among Taiwanese undergraduate women. Oncol. Nurs. Forum. 2011, 38, E297–E304. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.S.; Chen, C.H.; Liu, G.S.; Tai, M.H.; Wang, J.S.; Wu, J.C.; Kung, M.L.; Chan, E.C.; Liu, L.F. Tumorigenesis and prognostic role of hepatoma-derived growth factor in human gliomas. J. Neurooncol. 2012, 107, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Negishi, H.; Idogawa, M.; Yokota, I.; Koyama, R.; Kusano, M.; Suzuki, H.; Fujita, M.; Maruyama, R.; Toyota, M.; et al. p53 negatively regulates the hepatoma growth factor HDGF. Cancer Res. 2011, 71, 7038–7047. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, C.-C.; Huang, S.-C.; Tai, M.H.; Chien, C.-C.C.; Huang, C.-C.; Hsu, Y.-C. Hepatoma-Derived Growth Factor Upregulation Is Correlated with Prognostic Factors of Early-Stage Cervical Adenocarcinoma. Int. J. Mol. Sci. 2014, 15, 21492-21504. https://doi.org/10.3390/ijms151121492
Tsai C-C, Huang S-C, Tai MH, Chien C-CC, Huang C-C, Hsu Y-C. Hepatoma-Derived Growth Factor Upregulation Is Correlated with Prognostic Factors of Early-Stage Cervical Adenocarcinoma. International Journal of Molecular Sciences. 2014; 15(11):21492-21504. https://doi.org/10.3390/ijms151121492
Chicago/Turabian StyleTsai, Ching-Chou, Shun-Chen Huang, Ming Hong Tai, Chan-Chao Chang Chien, Chao-Cheng Huang, and Yi-Chiang Hsu. 2014. "Hepatoma-Derived Growth Factor Upregulation Is Correlated with Prognostic Factors of Early-Stage Cervical Adenocarcinoma" International Journal of Molecular Sciences 15, no. 11: 21492-21504. https://doi.org/10.3390/ijms151121492
APA StyleTsai, C.-C., Huang, S.-C., Tai, M. H., Chien, C.-C. C., Huang, C.-C., & Hsu, Y.-C. (2014). Hepatoma-Derived Growth Factor Upregulation Is Correlated with Prognostic Factors of Early-Stage Cervical Adenocarcinoma. International Journal of Molecular Sciences, 15(11), 21492-21504. https://doi.org/10.3390/ijms151121492




