Improvement of Radiotherapy-Induced Lacrimal Gland Injury by Induced Pluripotent Stem Cell-Derived Conditioned Medium via MDK and Inhibition of the p38/JNK Pathway
Abstract
:1. Introduction
2. Results and Discussion
2.1. Results
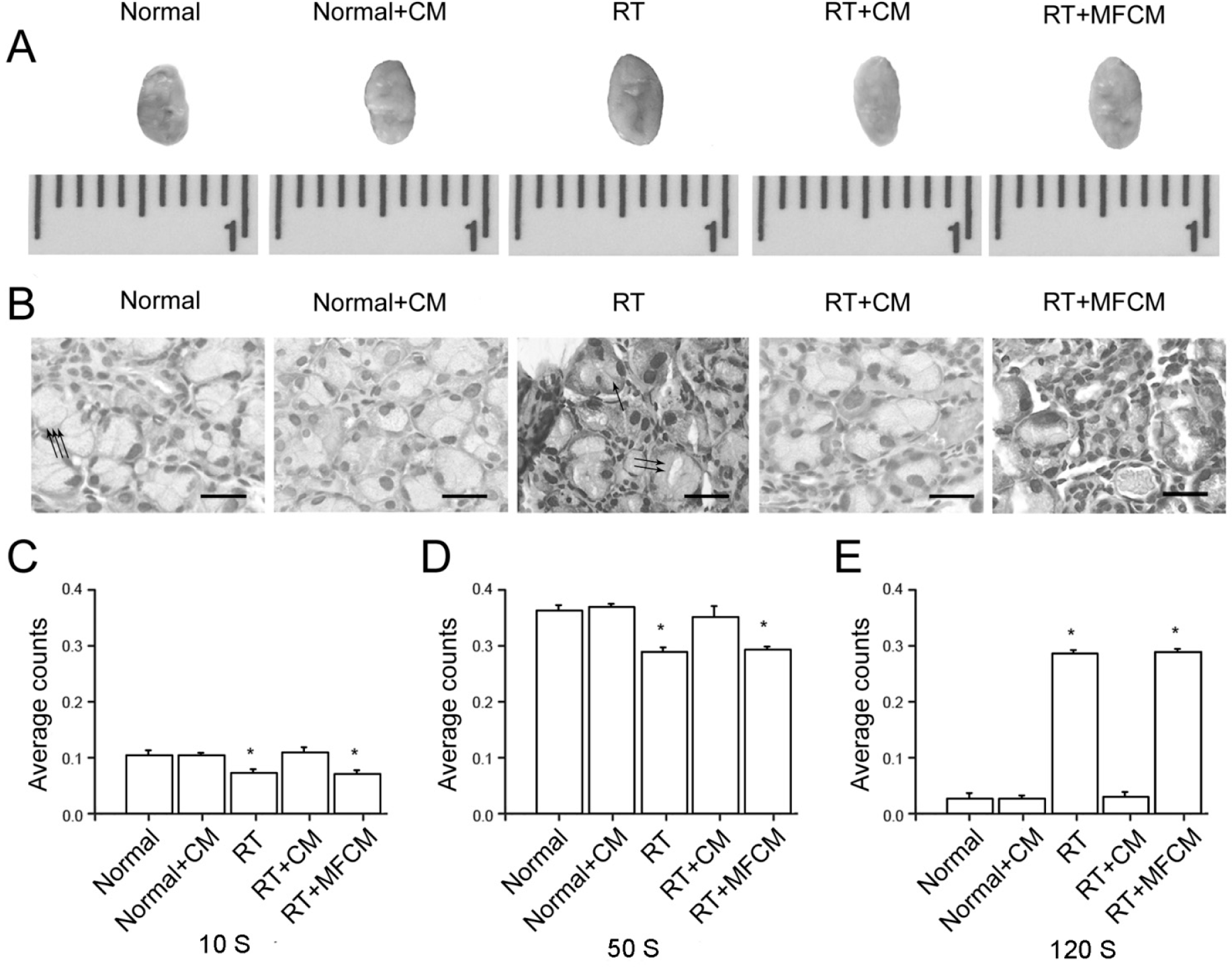
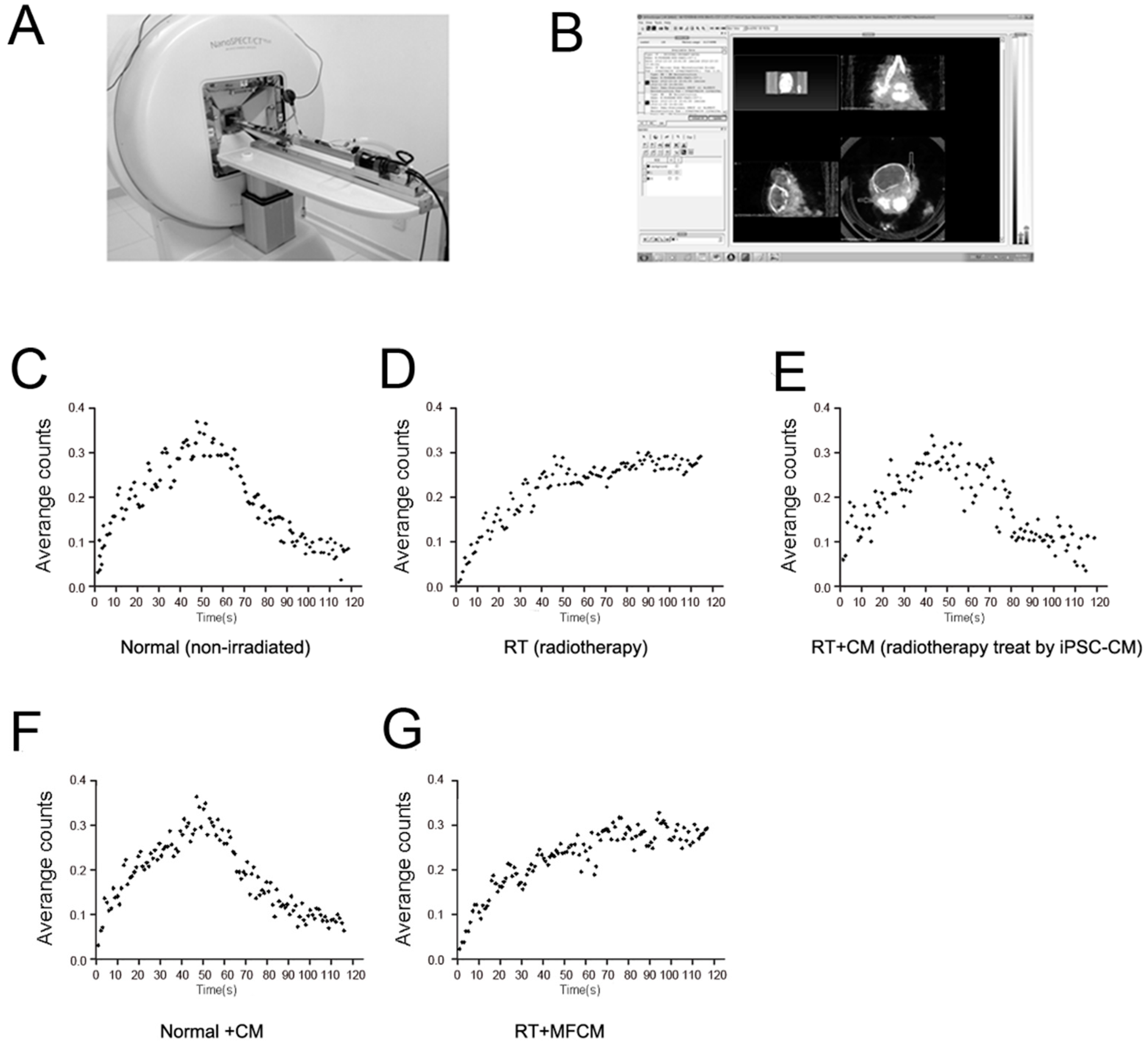
2.1.1. Improvement of a RILI Mouse Model by iPSC-CM
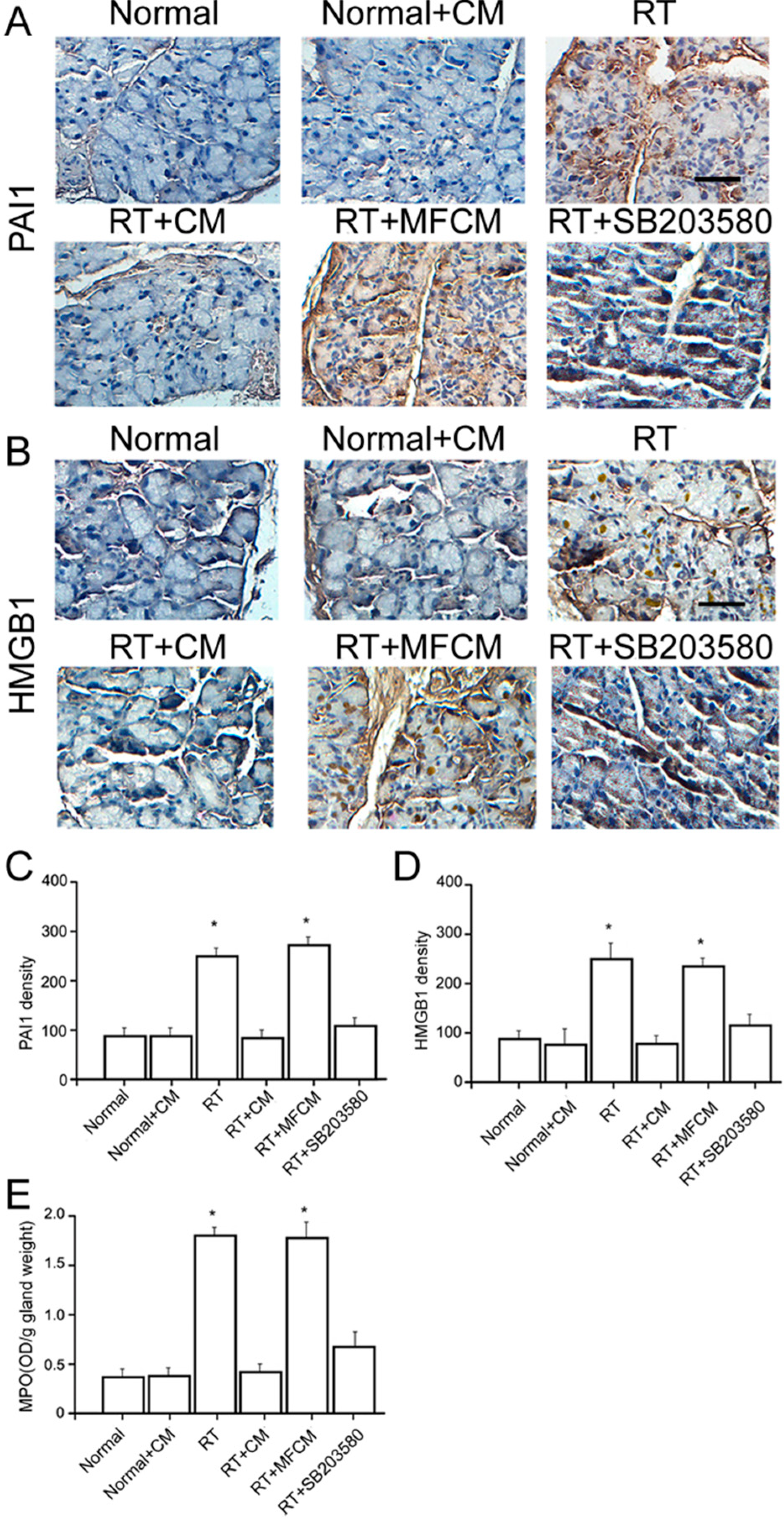
2.1.2. iPSC-CM Suppressed the RILI-Associated Inflammatory Response
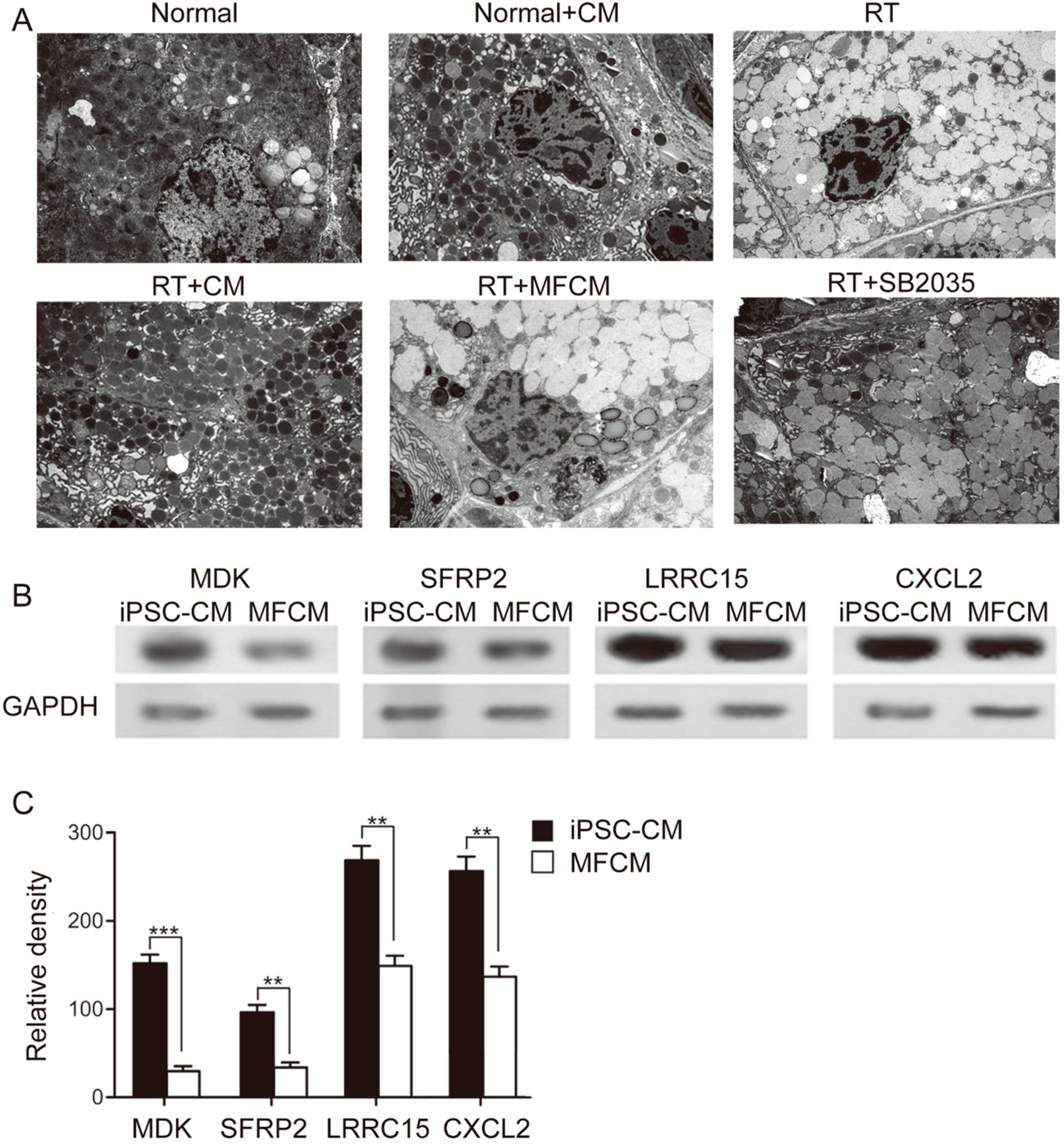
2.1.3. Ultramicrostructural Restoration by iPSC-CM
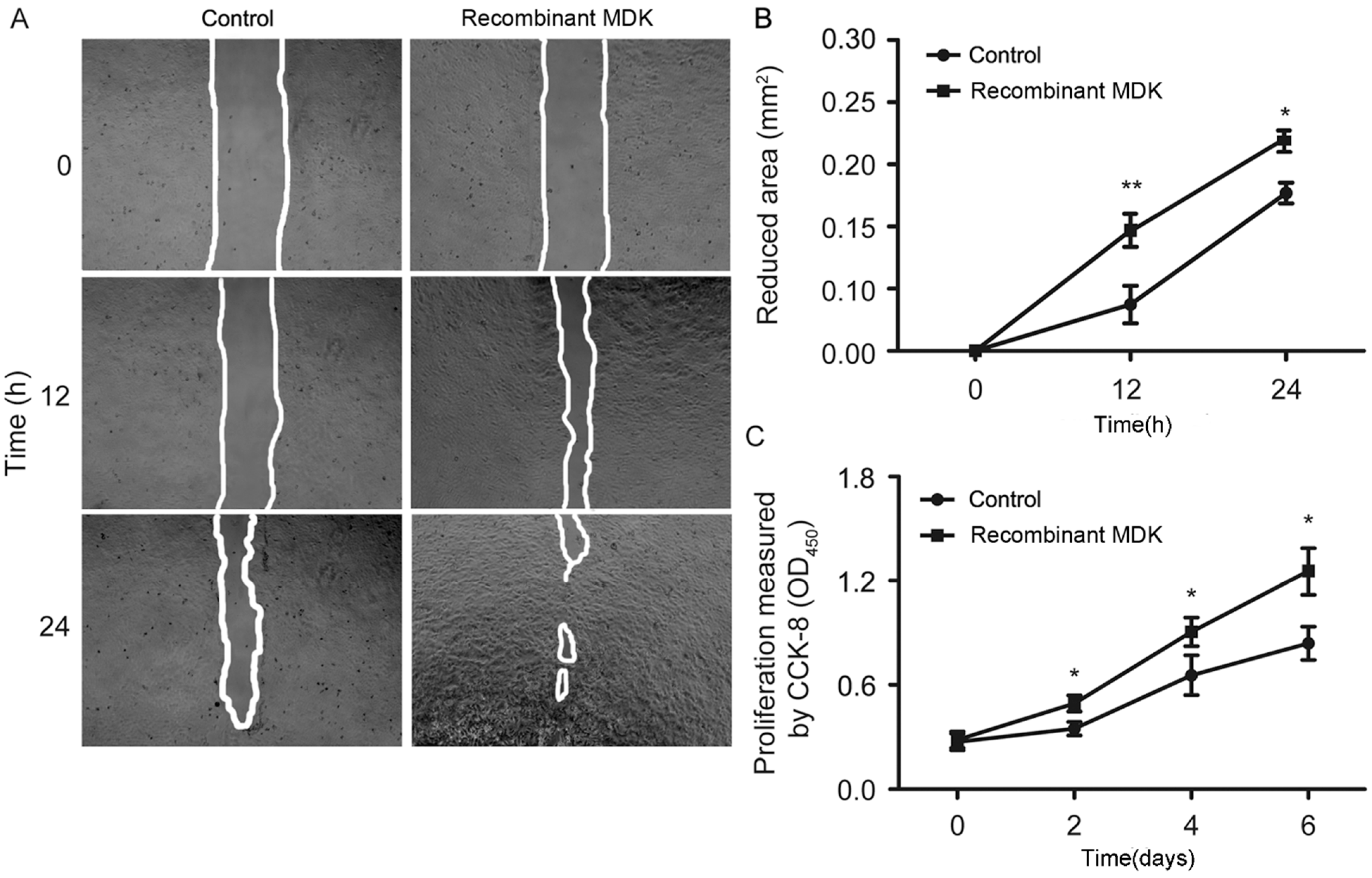
2.1.4. Recombinant MDK Promotes LGE Cell Migration and Proliferation
2.1.5. iPSCM Inhibits JNK, p38 and Akt Phosphorylation in LGE Cells
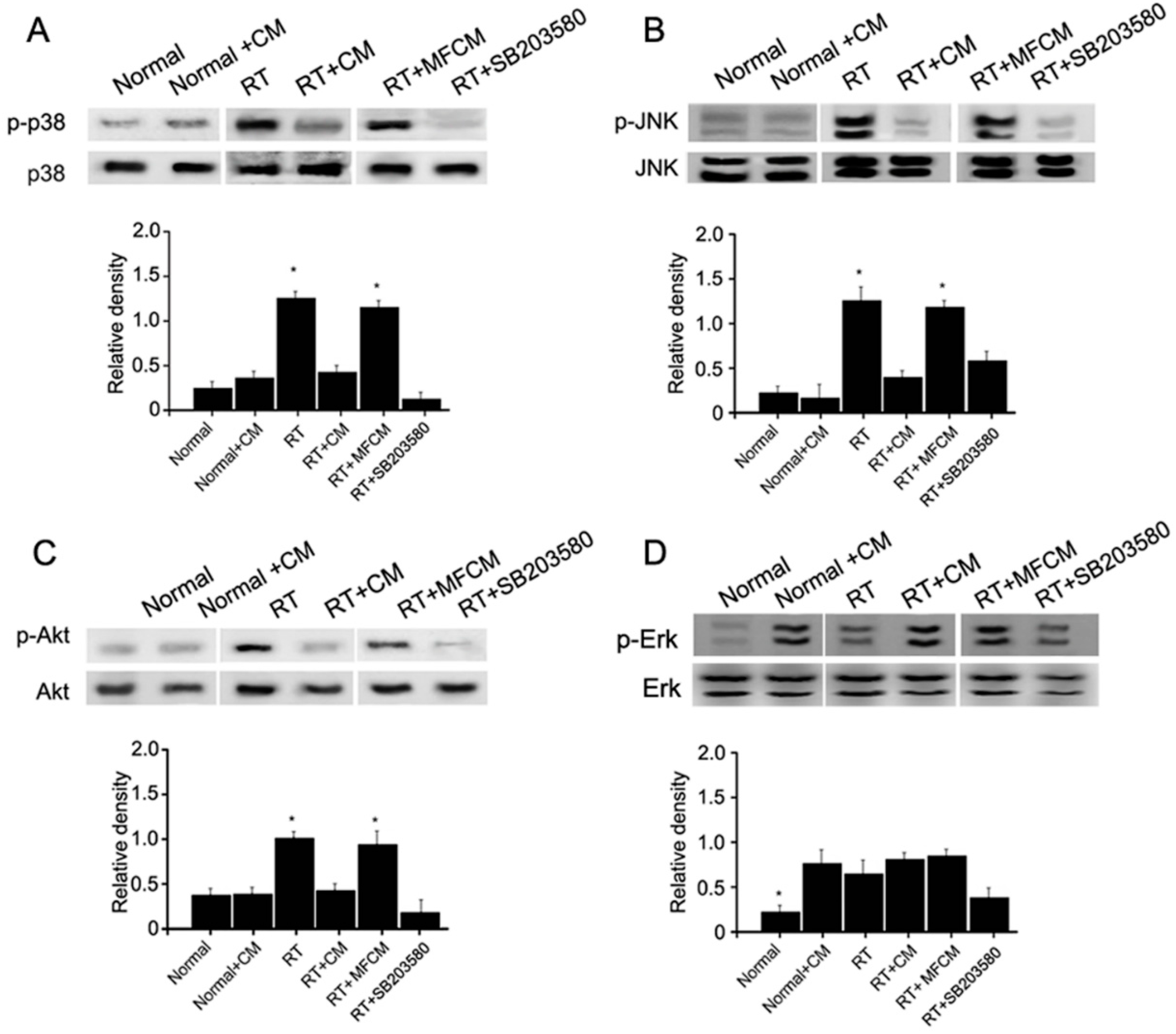
2.2. Discussion
3. Experimental Section
3.1. Animal Preparation and Irradiation
3.2. Ethics Statement
3.3. Surgical Harvesting of the Inferior Lacrimal Gland
3.4. Lacrimal Gland Scintigraphy
3.5. Mouse Embryonic Fibroblasts iPSCs and Conditioned Medium
3.6. Pharmacological Inhibitor
3.7. Transmission Electron Microscopy
3.8. Immunohistochemistry
3.9. Cell Isolation and Culture
3.10. Cell Proliferation Assay
3.11. Scratch-Wound Healing Assay
3.12. Western Blot Assay
3.13. Statistical Analysis
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Parsons, J.T.; Bova, F.J.; Fitzgerald, C.R.; Mendenhall, W.M.; Million, R.R. Severe dry-eye syndrome following external beam irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1994, 30, 775–780. [Google Scholar]
- Parsons, J.T.; Bova, F.J.; Mendenhall, W.M.; Million, R.R.; Fitzgerald, C.R. Response of the normal eye to high dose radiotherapy. Oncology 1996, 10, 837–847. [Google Scholar]
- Horwath-Winter, J.; Schneider, M.R.; Wackernagel, W.; Rabensteiner, D.; Boldin, I.; Haller-Schober, E.M.; Langmann, G. Influence of single-fraction gamma-knife radiosurgery on ocular surface and tear function in choroidal melanoma patients. Br. J. Ophthalmol. 2013, 97, 466–470. [Google Scholar] [CrossRef]
- Gazda, M.J.; Schultheiss, T.E.; Stephens, L.C.; Ang, K.K.; Peters, L.J. The relationship between apoptosis and atrophy in the irradiated lacrimal gland. Int. J. Radiat. Oncol. Biol. Phys. 1992, 24, 693–697. [Google Scholar] [CrossRef]
- Solans, R.; Bosch, J.A.; Galofre, P.; Porta, F.; Rosello, J.; Selva-O’Callagan, A.; Vilardell, M. Salivary and lacrimal gland dysfunction (sicca syndrome) after radioiodine therapy. J. Nucl. Med. 2001, 42, 738–743. [Google Scholar]
- Beutel, J.; Schroder, C.; von Hof, K.; Rades, D.; Kosmehl, H.; Wedel, T.; Sieg, P.; Geerling, G.; Hakim, S.G. Pharmacological prevention of radiation-induced dry eye-an experimental study in a rabbit model. Graefes. Arch. Clin. Exp. Ophthalmol. 2007, 245, 1347–1355. [Google Scholar] [CrossRef]
- Ruskell, G.L. Nerve terminals and epithelial cell variety in the human lacrimal gland. Cell. Tissue Res. 1975, 158, 121–136. [Google Scholar] [CrossRef]
- Zoukhri, D.; Fix, A.; Alroy, J.; Kublin, C.L. Mechanisms of murine lacrimal gland repair after experimentally induced inflammation. Investig. Ophthalmol. Vis. Sci. 2008, 49, 4399–4406. [Google Scholar] [CrossRef]
- You, S.; Avidan, O.; Tariq, A.; Ahluwalia, I.; Stark, P.C.; Kublin, C.L.; Zoukhri, D. Role of epithelial-mesenchymal transition in repair of the lacrimal gland after experimentally induced injury. Investig. Ophthalmol. Vis. Sci. 2012, 53, 126–135. [Google Scholar] [CrossRef]
- Bessout, R.; Semont, A.; Demarquay, C.; Charcosset, A.; Benderitter, M.; Mathieu, N. Mesenchymal stem cell therapy induces glucocorticoid synthesis in colonic mucosa and suppresses radiation-activated T cells: New insights into MSC immunomodulation. Mucosal. Immunol. 2013, 7, 656–659. [Google Scholar] [CrossRef]
- Li, L.F.; Liu, Y.Y.; Yang, C.T.; Chien, Y.; Twu, N.F.; Wang, M.L.; Wang, C.Y.; Huang, C.C.; Kao, K.C.; Hsu, H.S.; et al. Improvement of ventilator-induced lung injury by ips cell-derived conditioned medium via inhibition of pi3k/akt pathway and ip-10-dependent paracrine regulation. Biomaterials 2013, 34, 78–91. [Google Scholar]
- Pejchal, J.; Novotny, J.; Marak, V.; Osterreicher, J.; Tichy, A.; Vavrova, J.; Sinkorova, Z.; Zarybnicka, L.; Novotna, E.; Chladek, J.; et al. Activation of p38 mapk and expression of tgf-beta1 in rat colon enterocytes after whole body gamma-irradiation. Int. J. Radiat. Biol. 2012, 88, 348–358. [Google Scholar] [CrossRef]
- Li, D.; Wang, Y.; Wu, H.; Lu, L.; Wang, X.; Zhang, J.; Zhang, H.; Fan, S.; Fan, F.; Zhou, D.; et al. The effects of p38 mapk inhibition combined with g-csf administration on the hematoimmune system in mice with irradiation injury. PLoS One 2013, 8, e62921. [Google Scholar]
- Wang, Y.; Kellner, J.; Liu, L.; Zhou, D. Inhibition of p38 mitogen-activated protein kinase promotes ex vivo hematopoietic stem cell expansion. Stem. Cells Dev. 2011, 20, 1143–1152. [Google Scholar] [CrossRef]
- Perdiguero, E.; Sousa-Victor, P.; Ruiz-Bonilla, V.; Jardi, M.; Caelles, C.; Serrano, A.L.; Munoz-Canoves, P. P38/MKP-1-regulated akt coordinates macrophage transitions and resolution of inflammation during tissue repair. J. Cell. Biol. 2011, 195, 307–322. [Google Scholar] [CrossRef]
- Mitsiadis, T.A.; Muramatsu, T.; Muramatsu, H.; Thesleff, I. Midkine (MK), a heparin-binding growth/differentiation factor, is regulated by retinoic acid and epithelial-mesenchymal interactions in the developing mouse tooth, and affects cell proliferation and morphogenesis. J. Cell. Biol. 1995, 129, 267–281. [Google Scholar] [CrossRef]
- Huang, Y.; Sook-Kim, M.; Ratovitski, E. Midkine promotes tetraspanin-integrin interaction and induces fak-stat1alpha pathway contributing to migration/invasiveness of human head and neck squamous cell carcinoma cells. Biochem. Biophys. Res. Commun. 2008, 377, 474–478. [Google Scholar] [CrossRef]
- Hakim, S.G.; Schroder, C.; Geerling, G.; Lauer, I.; Wedel, T.; Kosmehl, H.; Driemel, O.; Jacobsen, H.C.; Trenkle, T.; Hermes, D.; et al. Early and late immunohistochemical and ultrastructural changes associated with functional impairment of the lachrymal gland following external beam radiation. Int. J. Exp. Pathol. 2006, 87, 65–71. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, Y.; Qian, J.; Zhang, M.; Wang, X. Radiotherapyinduced gadd45a impairs lacrimal gland epithelial cell migration and proliferation. Mol. Med. Rep. 2013, 8, 1049–1054. [Google Scholar]
- Xu, W.; Wang, X.T.; Xu, G.X.; Guo, J.; Huang, L.B. Stromal cell-derived factor 1 alpha-stimulated mesenchymal stem cells confer enhanced protection against light-induced retinal degeneration in rats. Curr. Eye Res. 2013, 39, 69–78. [Google Scholar] [CrossRef]
- De Santiago, J.; Bare, D.J.; Banach, K. Ischemia/reperfusion injury protection by mesenchymal stem cell derived antioxidant capacity. Stem. Cells Dev. 2013, 22, 2497–2507. [Google Scholar]
- Kotenko, K.; Moroz, B.; Nadezhina, N.; Galstyan, I.; Eremin, I.; Deshevoy, J.; Lebedev, V.; Slobodina, T.; Grinakovskaya, D.; Zhgutov, Y.; et al. Successful treatment of localised radiation lesions in rats and humans by mesenchymal stem cell transplantation. Radiat. Prot. Dosimetry 2012, 151, 661–665. [Google Scholar] [CrossRef]
- Acharya, M.M.; Christie, L.A.; Lan, M.L.; Giedzinski, E.; Fike, J.R.; Rosi, S.; Limoli, C.L. Human neural stem cell transplantation ameliorates radiation-induced cognitive dysfunction. Cancer Res. 2011, 71, 4834–4845. [Google Scholar] [CrossRef]
- Yang, K.Y.; Shih, H.C.; How, C.K.; Chen, C.Y.; Hsu, H.S.; Yang, C.W.; Lee, Y.C.; Perng, R.P.; Peng, C.H.; Li, H.Y.; et al. Iv delivery of induced pluripotent stem cells attenuates endotoxin-induced acute lung injury in mice. Chest 2011, 140, 1243–1253. [Google Scholar] [CrossRef]
- Sun, Y.Q.; Deng, M.X.; He, J.; Zeng, Q.X.; Wen, W.; Wong, D.S.; Tse, H.F.; Xu, G.; Lian, Q.; Shi, J.; et al. Human pluripotent stem cell-derived mesenchymal stem cells prevent allergic airway inflammation in mice. Stem Cells 2012, 30, 2692–2699. [Google Scholar] [CrossRef]
- Xiang, B.; Li, X.X.; Zhang, F.Y. Underlying protective mechanism of alpha1-adrenoceptor activation against irradiation-induced damage in rat submandibular gland. Arch. Oral Biol. 2013, 58, 1238–1245. [Google Scholar] [CrossRef]
- Khan, N.M.; Poduval, T.B. Bilirubin augments radiation injury and leads to increased infection and mortality in mice: Molecular mechanisms. Free Radic. Biol. Med. 2012, 53, 1152–1169. [Google Scholar] [CrossRef]
- Li, D.; Wang, Y.; Wu, H.; Lu, L.; Zhang, H.; Chang, J.; Zhai, Z.; Zhang, J.; Zhou, D.; Meng, A. Mitigation of ionizing radiation-induced bone marrow suppression by p38 inhibition and g-csf administration. J. Radiat. Res. 2011, 52, 712–716. [Google Scholar] [CrossRef]
- Segreto, H.R.; Oshima, C.T.; Franco, M.F.; Silva, M.R.; Egami, M.I.; Teixeira, V.P.; Segreto, R.A. Phosphorylation and cytoplasmic localization of mapk p38 during apoptosis signaling in bone marrow granulocytes of mice irradiated in vivo and the role of amifostine in reducing these effects. Acta Histochem. 2011, 113, 300–307. [Google Scholar] [CrossRef]
- Bohlen, P.; Kovesdi, I. Hbnf and mk, members of a novel gene family of heparin-binding proteins with potential roles in embryogenesis and brain function. Prog. Growth Factor Res. 1991, 3, 143–157. [Google Scholar] [CrossRef]
- Zhang, Z.H.; Li, H.X.; Qi, Y.P.; Du, L.J.; Zhu, S.Y.; Wu, M.Y.; Lu, H.L.; Yu, Y.; Han, W. Recombinant human midkine stimulates proliferation of articular chondrocytes. Cell. Prolif. 2010, 43, 184–194. [Google Scholar] [CrossRef]
- Monma, F.; Hozumi, Y.; Ikematsu, S.; Kawaguchi, M.; Kadomatsu, K.; Suzuki, T. Expression of midkine in normal human skin, dermatitis and neoplasms: Association with differentiation of keratinocytes. J. Dermatol. 2013, 40, 980–986. [Google Scholar] [CrossRef]
- Qi, M.; Ikematsu, S.; Maeda, N.; Ichihara-Tanaka, K.; Sakuma, S.; Noda, M.; Muramatsu, T.; Kadomatsu, K. Haptotactic migration induced by midkine. Involvement of protein-tyrosine phosphatase zeta. Mitogen-activated protein kinase, and phosphatidylinositol 3-kinase. J. Biol. Chem. 2001, 276, 15868–15875. [Google Scholar] [CrossRef]
- Satoh, J.; Muramatsu, H.; Moretto, G.; Muramatsu, T.; Chang, H.J.; Kim, S.T.; Cho, J.M.; Kim, S.U. Midkine that promotes survival of fetal human neurons is produced by fetal human astrocytes in culture. Brain Res. Dev. Brain Res. 1993, 75, 201–205. [Google Scholar] [CrossRef]
- Ikutomo, M.; Sakakima, H.; Matsuda, F.; Yoshida, Y. Midkine-deficient mice delayed degeneration and regeneration after skeletal muscle injury. Acta Histochem. 2013, 116, 319–326. [Google Scholar] [CrossRef]
- Li, H.Y.; Chien, Y.; Chen, Y.J.; Chen, S.F.; Chang, Y.L.; Chiang, C.H.; Jeng, S.Y.; Chang, C.M.; Wang, M.L.; Chen, L.K.; et al. Reprogramming induced pluripotent stem cells in the absence of c-myc for differentiation into hepatocyte-like cells. Biomaterials 2011, 32, 5994–6005. [Google Scholar]
- Chen, S.J.; Chang, C.M.; Tsai, S.K.; Chang, Y.L.; Chou, S.J.; Huang, S.S.; Tai, L.K.; Chen, Y.C.; Ku, H.H.; Li, H.Y.; et al. Functional improvement of focal cerebral ischemia injury by subdural transplantation of induced pluripotent stem cells with fibrin glue. Stem Cells Dev. 2010, 19, 1757–1767. [Google Scholar] [CrossRef]
- How, C.K.; Chien, Y.; Yang, K.Y.; Shih, H.C.; Juan, C.C.; Yang, Y.P.; Chiou, G.Y.; Huang, P.I.; Chang, Y.L.; Chen, L.K.; et al. Induced pluripotent stem cells mediate the release of interferon gamma-induced protein 10 and alleviate bleomycin-induced lung inflammation and fibrosis. Shock 2013, 39, 261–270. [Google Scholar] [CrossRef]
- Liu, Y.Y.; Li, L.F.; Yang, C.T.; Lu, K.H.; Huang, C.C.; Kao, K.C.; Chiou, S.H. Suppressing nf-kappab and nkrf pathways by induced pluripotent stem cell therapy in mice with ventilator-induced lung injury. PLoS One 2013, 8, e66760. [Google Scholar]
- Zhang, P.; Wu, Y.; Dai, Q.; Fang, B.; Jiang, L. P38-mapk signaling pathway is not involved in osteogenic differentiation during early response of mesenchymal stem cells to continuous mechanical strain. Mol. Cell.Cell Biochem. 2013, 378, 19–28. [Google Scholar] [CrossRef]
- Zhang, L.H.; Jia, Y.L.; Lin, X.X.; Zhang, H.Q.; Dong, X.W.; Zhao, J.M.; Shen, J.; Shen, H.J.; Li, F.F.; Yan, X.F.; et al. Ad-1, a novel ginsenoside derivative, shows anti-lung cancer activity via activation of p38 mapk pathway and generation of reactive oxygen species. Biochim. Biophys. Acta 2013, 1830, 4148–4159. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Deng, C.; Qian, J.; Zhang, M.; Li, X. Improvement of Radiotherapy-Induced Lacrimal Gland Injury by Induced Pluripotent Stem Cell-Derived Conditioned Medium via MDK and Inhibition of the p38/JNK Pathway. Int. J. Mol. Sci. 2014, 15, 18407-18421. https://doi.org/10.3390/ijms151018407
Zhang Y, Deng C, Qian J, Zhang M, Li X. Improvement of Radiotherapy-Induced Lacrimal Gland Injury by Induced Pluripotent Stem Cell-Derived Conditioned Medium via MDK and Inhibition of the p38/JNK Pathway. International Journal of Molecular Sciences. 2014; 15(10):18407-18421. https://doi.org/10.3390/ijms151018407
Chicago/Turabian StyleZhang, Yanqing, Chenliang Deng, Jiang Qian, Mingui Zhang, and Xiaofeng Li. 2014. "Improvement of Radiotherapy-Induced Lacrimal Gland Injury by Induced Pluripotent Stem Cell-Derived Conditioned Medium via MDK and Inhibition of the p38/JNK Pathway" International Journal of Molecular Sciences 15, no. 10: 18407-18421. https://doi.org/10.3390/ijms151018407
APA StyleZhang, Y., Deng, C., Qian, J., Zhang, M., & Li, X. (2014). Improvement of Radiotherapy-Induced Lacrimal Gland Injury by Induced Pluripotent Stem Cell-Derived Conditioned Medium via MDK and Inhibition of the p38/JNK Pathway. International Journal of Molecular Sciences, 15(10), 18407-18421. https://doi.org/10.3390/ijms151018407



