TPX2 Is a Prognostic Marker and Contributes to Growth and Metastasis of Human Hepatocellular Carcinoma
Abstract
:1. Introduction
2. Results and Discussion
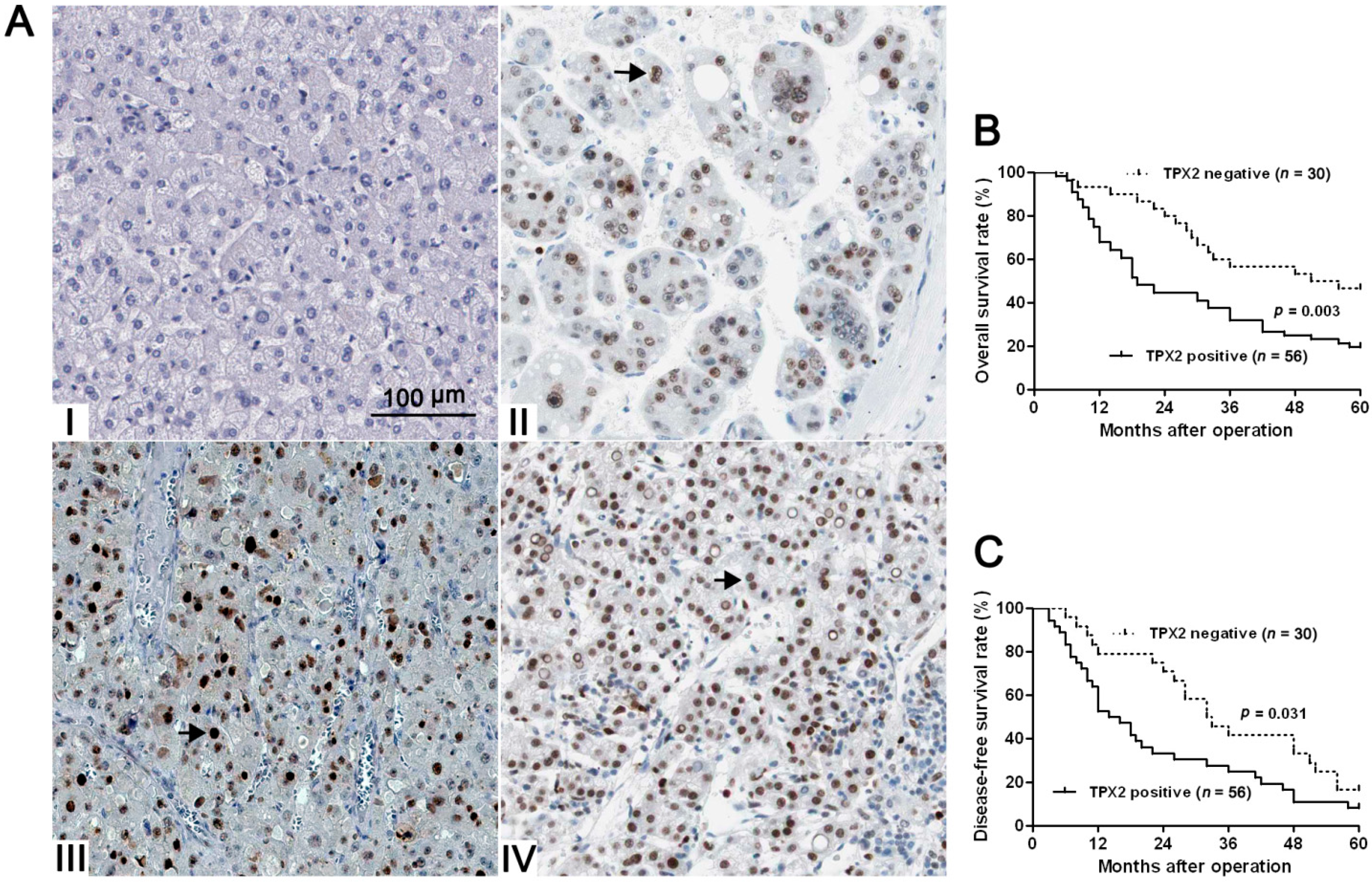
2.1. Clinical Significance of TPX2 (Targeting Protein for Xenopus Kinesin-Like Protein 2) in HCC (Hepatocellular Carcinoma) Specimens

| Clinicopathologic Features | Total No. of Patients, n = 86 | No. of Patients | p | ||
|---|---|---|---|---|---|
| TPX2 positive | TPX2 negative | ||||
| Age (year) | <50 | 27 | 15 | 12 | 0.208 |
| ≥50 | 59 | 41 | 18 | ||
| Sex | Male | 69 | 44 | 25 | 0.597 |
| Female | 17 | 12 | 5 | ||
| HBV | Absent | 30 | 19 | 11 | 0.800 |
| Present | 56 | 37 | 19 | ||
| Serum AFP level (ng/mL) | <400 | 34 | 24 | 10 | 0.389 |
| ≥400 | 52 | 32 | 20 | ||
| Tumor size (cm) | <5 | 30 | 22 | 8 | 0.242 |
| ≥5 | 56 | 34 | 22 | ||
| No. of tumor nodules | 1 | 66 | 36 | 17 | 0.489 |
| ≥2 | 20 | 20 | 13 | ||
| Cirrhosis | Absent | 37 | 26 | 11 | 0.384 |
| Present | 49 | 30 | 19 | ||
| Venous infiltration | Absent | 42 | 21 | 21 | 0.004 * |
| Present | 44 | 35 | 9 | ||
| Edmondson-Steiner grading | I + II | 29 | 14 | 15 | 0.019 * |
| III + IV | 57 | 42 | 15 | ||
| TNM tumor stage | I + II | 61 | 34 | 27 | 0.004 * |
| III + IV | 25 | 22 | 3 | ||
2.2. Positive TPX2 Expression Confers a Worse 5-Year Survival for HCC Patients
| Variables | OS | DFS | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| Venous infiltration (no vs. yes) | 2.9 | 1.1–7.4 | 0.022 * | 1.5 | 0.8–3.1 | 0.176 |
| Edmondson-Steiner grading (I/II vs. III/IV) | 1.6 | 0.7–3.7 | 0.256 | 3.0 | 1.7–5.3 | <0.001 * |
| TNM tumor stage (I/II vs. III/IV) | 3.7 | 1.8–7.5 | <0.001 * | 4.6 | 2.5–8.4 | <0.001 * |
| TPX2 (negative vs. positive) | 3.7 | 1.7–8.1 | 0.001 * | 2.2 | 1.2–3.9 | 0.006 * |
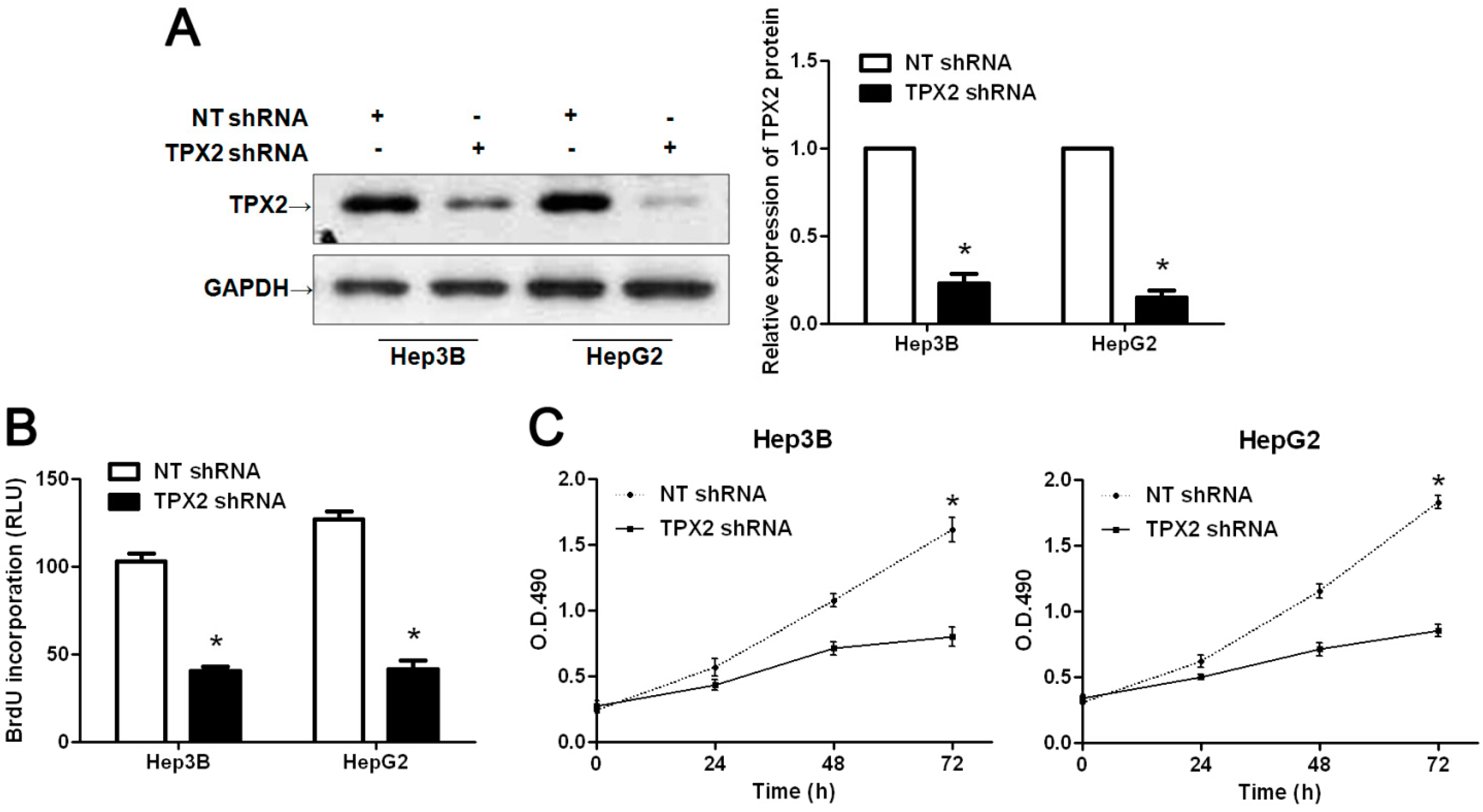
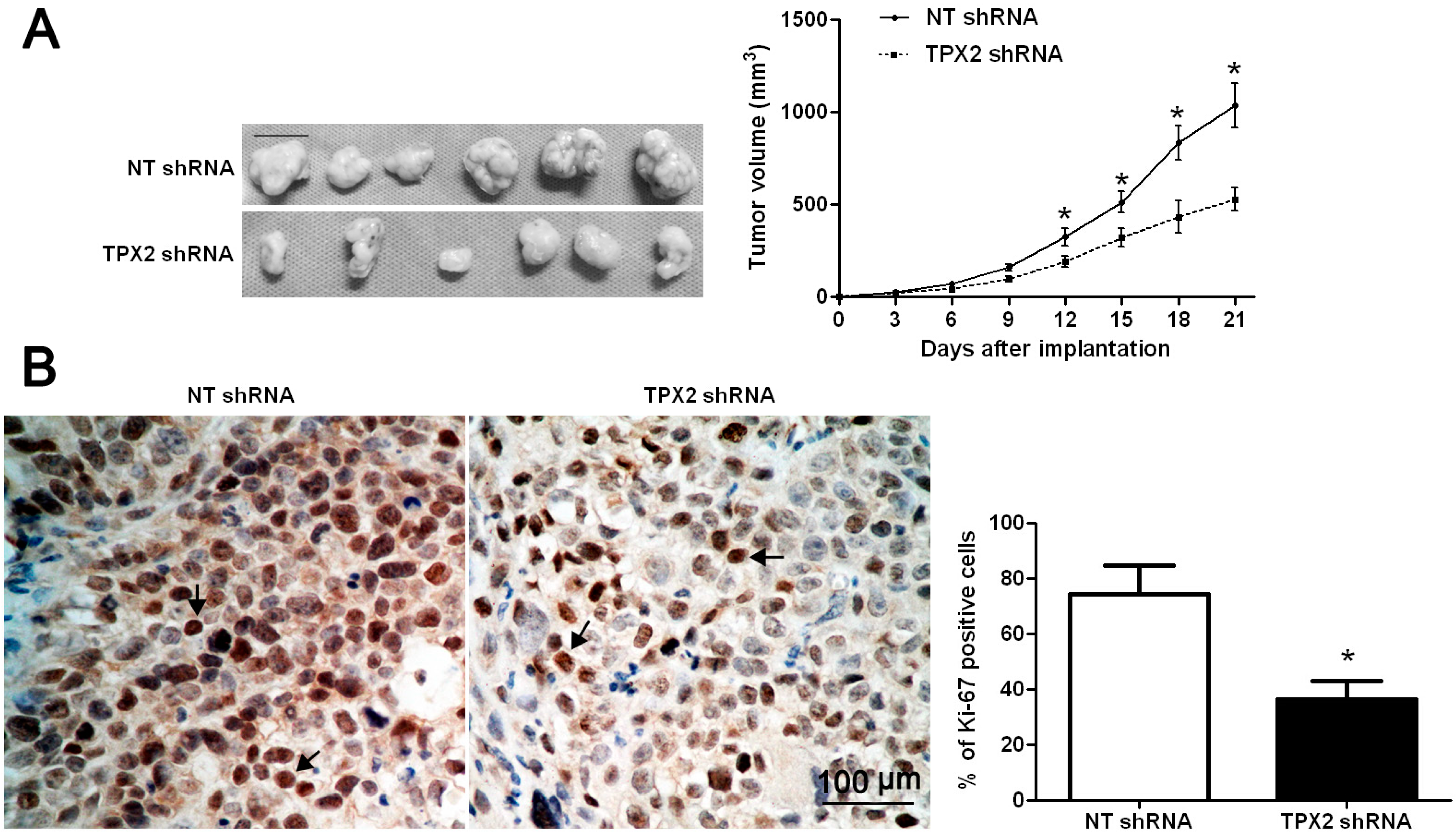
2.3. TPX2 Promotes Tumor Growth in Vitro and in Vivo
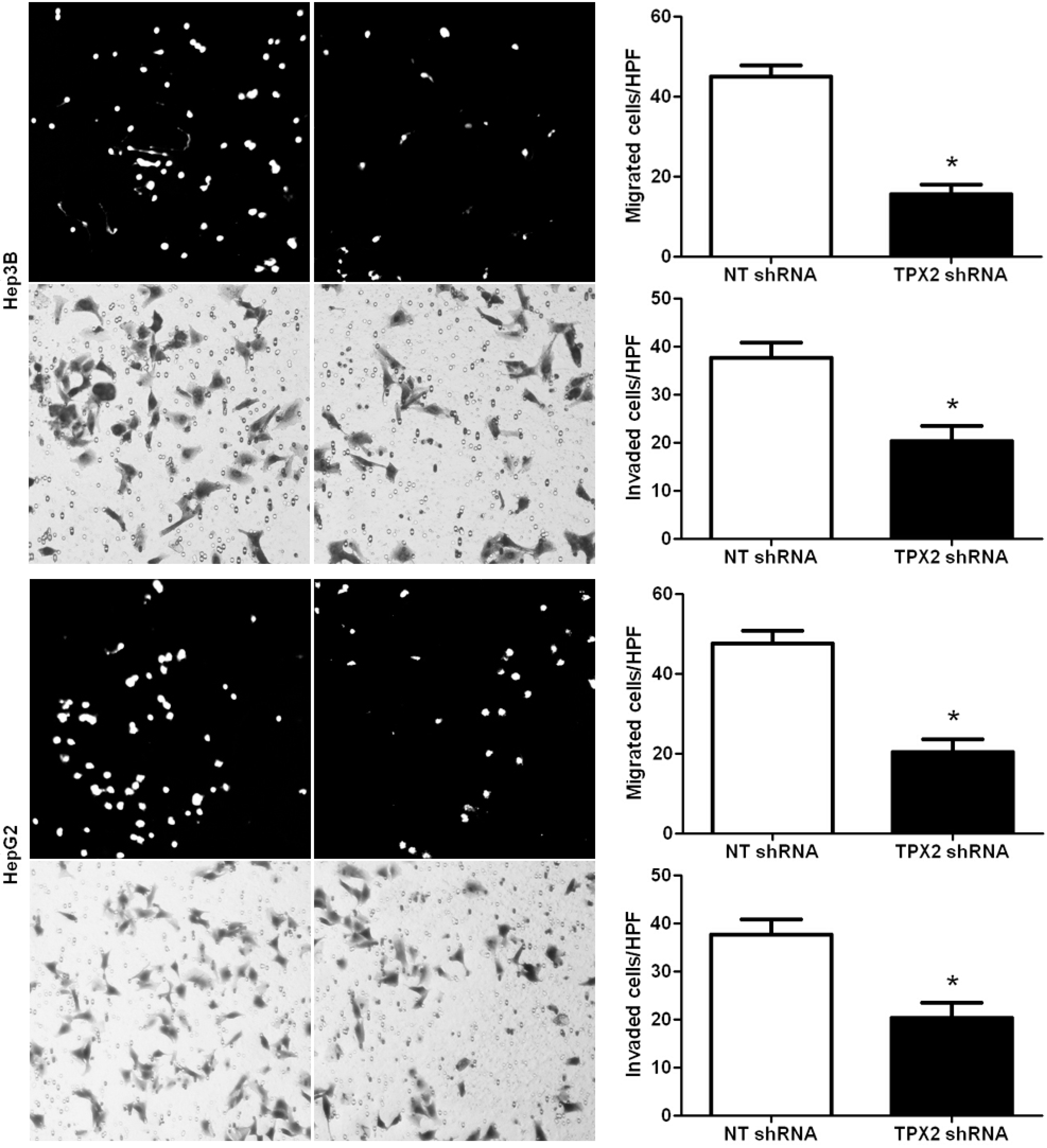
2.4. Promoting Effect of TPX2 on HCC Cell Migration and Invasion
3. Experimental Section
3.1. Ethical Review
3.2. Clinical Samples
3.3. Immunohistochemical Staining
3.4. Cell Lines and Transfection
3.5. Western Blot
3.6. BrdU Cell Proliferation Assay and MTT Assays
3.7. In Vivo Experiments
3.8. Real Time Quantitative Reverse Transcription-PCR (qRT-PCR)
3.9. Boyden Chamber and Transwell Assays
3.10. Statistical Analysis
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 2010, 127, 2893–2917. [Google Scholar] [CrossRef]
- Bruix, J.; Sherman, M. Management of hepatocellular carcinoma: An update. Hepatology 2011, 53, 1020–1022. [Google Scholar] [CrossRef]
- Tu, K.; Li, C.; Zheng, X.; Yang, W.; Yao, Y.; Liu, Q. Prognostic significance of miR-218 in human hepatocellular carcinoma and its role in cell growth. Oncol. Rep. 2014, 32, 1571–1577. [Google Scholar]
- Heidebrecht, H.J.; Buck, F.; Steinmann, J.; Sprenger, R.; Wacker, H.H.; Parwaresch, R. p100: A novel proliferation-associated nuclear protein specifically restricted to cell cycle phases S, G2, and M. Blood 1997, 90, 226–233. [Google Scholar]
- Wittmann, T.; Wilm, M.; Karsenti, E.; Vernos, I. TPX2, A novel xenopus MAP involved in spindle pole organization. J. Cell Biol. 2000, 149, 1405–1418. [Google Scholar] [CrossRef]
- Kufer, T.A.; Sillje, H.H.; Korner, R.; Gruss, O.J.; Meraldi, P.; Nigg, E.A. Human TPX2 is required for targeting Aurora-A kinase to the spindle. J. Cell Biol. 2002, 158, 617–623. [Google Scholar] [CrossRef]
- Gruss, O.J.; Wittmann, M.; Yokoyama, H.; Pepperkok, R.; Kufer, T.; Sillje, H.; Karsenti, E.; Mattaj, I.W.; Vernos, I. Chromosome-induced microtubule assembly mediated by TPX2 is required for spindle formation in HeLa cells. Nat. Cell Biol. 2002, 4, 871–879. [Google Scholar] [CrossRef]
- Liu, H.C.; Zhang, Y.; Wang, X.L.; Qin, W.S.; Liu, Y.H.; Zhang, L.; Zhu, C.L. Upregulation of the TPX2 gene is associated with enhanced tumor malignance of esophageal squamous cell carcinoma. Biomed. Pharmacother. 2013, 67, 751–755. [Google Scholar] [CrossRef]
- Neumayer, G.; Belzil, C.; Gruss, O.J.; Nguyen, M.D. TPX2: Of spindle assembly, DNA damage response, and cancer. Cell Mol. Life Sci. 2014, 71, 3027–3047. [Google Scholar] [CrossRef]
- Chang, H.; Wang, J.; Tian, Y.; Xu, J.; Gou, X.; Cheng, J. The TPX2 gene is a promising diagnostic and therapeutic target for cervical cancer. Oncol. Rep. 2012, 27, 1353–1359. [Google Scholar]
- Li, Y.; Tang, H.; Sun, Z.; Bungum, A.O.; Edell, E.S.; Lingle, W.L.; Stoddard, S.M.; Zhang, M.; Jen, J.; Yang, P.; et al. Network-based approach identified cell cycle genes as predictor of overall survival in lung adenocarcinoma patients. Lung. Cancer 2013, 80, 91–98. [Google Scholar] [CrossRef]
- Wei, P.; Zhang, N.; Xu, Y.; Li, X.; Shi, D.; Wang, Y.; Li, D.; Cai, S. TPX2 is a novel prognostic marker for the growth and metastasis of colon cancer. J. Transl. Med. 2013, 11. [Google Scholar] [CrossRef]
- Yan, L.; Li, S.; Xu, C.; Zhao, X.; Hao, B.; Li, H.; Qiao, B. Target protein for Xklp2 (TPX2), a microtubule-related protein, contributes to malignant phenotype in bladder carcinoma. Tumour Biol. 2013, 34, 4089–4100. [Google Scholar] [CrossRef]
- Jiang, P.; Shen, K.; Wang, X.; Song, H.; Yue, Y.; Liu, T. TPX2 regulates tumor growth in human cervical carcinoma cells. Mol. Med. Rep. 2014, 9, 2347–2351. [Google Scholar]
- Warner, S.L.; Stephens, B.J.; Nwokenkwo, S.; Hostetter, G.; Sugeng, A.; Hidalgo, M.; Trent, J.M.; Han, H.; von Hoff, D.D. Validation of TPX2 as a potential therapeutic target in pancreatic cancer cells. Clin. Cancer Res. 2009, 15, 6519–6528. [Google Scholar]
- Hsu, P.K.; Chen, H.Y.; Yeh, Y.C.; Yen, C.C.; Wu, Y.C.; Hsu, C.P.; Hsu, W.H.; Chou, T.Y. TPX2 expression is associated with cell proliferation and patient outcome in esophageal squamous cell carcinoma. J. Gastroenterol. 2014, 49, 1231–1240. [Google Scholar] [CrossRef]
- Caceres-Gorriti, K.Y.; Carmona, E.; Barres, V.; Rahimi, K.; Letourneau, I.J.; Tonin, P.N.; Provencher, D.; Mes-Masson, A.M. RAN nucleo-cytoplasmic transport and mitotic spindle assembly partners XPO7 and TPX2 are new prognostic biomarkers in serous epithelial ovarian cancer. PLoS One 2014, 9, e91000. [Google Scholar]
- Shigeishi, H.; Ohta, K.; Hiraoka, M.; Fujimoto, S.; Minami, M.; Higashikawa, K.; Kamata, N. Expression of TPX2 in salivary gland carcinomas. Oncol. Rep. 2009, 21, 341–344. [Google Scholar]
- Satow, R.; Shitashige, M.; Kanai, Y.; Takeshita, F.; Ojima, H.; Jigami, T.; Honda, K.; Kosuge, T.; Ochiya, T.; Hirohashi, S.; et al. Combined functional genome survey of therapeutic targets for hepatocellular carcinoma. Clin. Cancer Res. 2010, 16, 2518–2528. [Google Scholar]
- Aguirre-Portoles, C.; Bird, A.W.; Hyman, A.; Canamero, M.; Perez de Castro, I.; Malumbres, M. Tpx2 controls spindle integrity, genome stability, and tumor development. Cancer Res. 2012, 72, 1518–1528. [Google Scholar] [CrossRef]
- Vainio, P.; Mpindi, J.P.; Kohonen, P.; Fey, V.; Mirtti, T.; Alanen, K.A.; Perala, M.; Kallioniemi, O.; Iljin, K. High-throughput transcriptomic and RNAi analysis identifies AIM1, ERGIC1, TMED3 and TPX2 as potential drug targets in prostate cancer. PLoS One 2012, 7, e39801. [Google Scholar] [CrossRef]
- Tu, K.; Zheng, X.; Zan, X.; Han, S.; Yao, Y.; Liu, Q. Evaluation of Fbxw7 expression and its correlation with the expression of c-Myc, cyclin E and p53 in human hepatocellular carcinoma. Hepatol. Res. 2012, 42, 904–910. [Google Scholar] [CrossRef]
- Tu, K.; Yang, W.; Li, C.; Zheng, X.; Lu, Z.; Guo, C.; Yao, Y.; Liu, Q. Fbxw7 is an independent prognostic marker and induces apoptosis and growth arrest by regulating YAP abundance in hepatocellular carcinoma. Mol. Cancer 2014, 13. [Google Scholar] [CrossRef]
- Tu, K.; Zheng, X.; Zhou, Z.; Li, C.; Zhang, J.; Gao, J.; Yao, Y.; Liu, Q. Recombinant human adenovirus-p53 injection induced apoptosis in hepatocellular carcinoma cell lines mediated by p53-Fbxw7 pathway, which controls c-Myc and cyclin E. PLoS One 2013, 8, e68574. [Google Scholar] [CrossRef]
- Friedman, S.L. Mechanisms of disease: Mechanisms of hepatic fibrosis and therapeutic implications. Nat. Clin. Pract. Gastroenterol. Hepatol. 2004, 1, 98–105. [Google Scholar] [CrossRef]
- Li, C.; Yang, W.; Zhang, J.; Zheng, X.; Yao, Y.; Tu, K.; Liu, Q. SREBP-1 has a prognostic role and contributes to invasion and metastasis in human hepatocellular carcinoma. Int. J. Mol. Sci. 2014, 15, 7124–7138. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.; Guo, W.; Kan, H. TPX2 Is a Prognostic Marker and Contributes to Growth and Metastasis of Human Hepatocellular Carcinoma. Int. J. Mol. Sci. 2014, 15, 18148-18161. https://doi.org/10.3390/ijms151018148
Huang Y, Guo W, Kan H. TPX2 Is a Prognostic Marker and Contributes to Growth and Metastasis of Human Hepatocellular Carcinoma. International Journal of Molecular Sciences. 2014; 15(10):18148-18161. https://doi.org/10.3390/ijms151018148
Chicago/Turabian StyleHuang, Yuqi, Wenbin Guo, and Heping Kan. 2014. "TPX2 Is a Prognostic Marker and Contributes to Growth and Metastasis of Human Hepatocellular Carcinoma" International Journal of Molecular Sciences 15, no. 10: 18148-18161. https://doi.org/10.3390/ijms151018148
APA StyleHuang, Y., Guo, W., & Kan, H. (2014). TPX2 Is a Prognostic Marker and Contributes to Growth and Metastasis of Human Hepatocellular Carcinoma. International Journal of Molecular Sciences, 15(10), 18148-18161. https://doi.org/10.3390/ijms151018148




