Evaluation of the Antibacterial, Anti-Cervical Cancer Capacity, and Biocompatibility of Different Graphene Oxides
Abstract
1. Introduction
2. Results and Discussion
2.1. Characterization of Graphene Oxide
2.1.1. Fourier-Transform Infrared Spectroscopy (FT-IR)
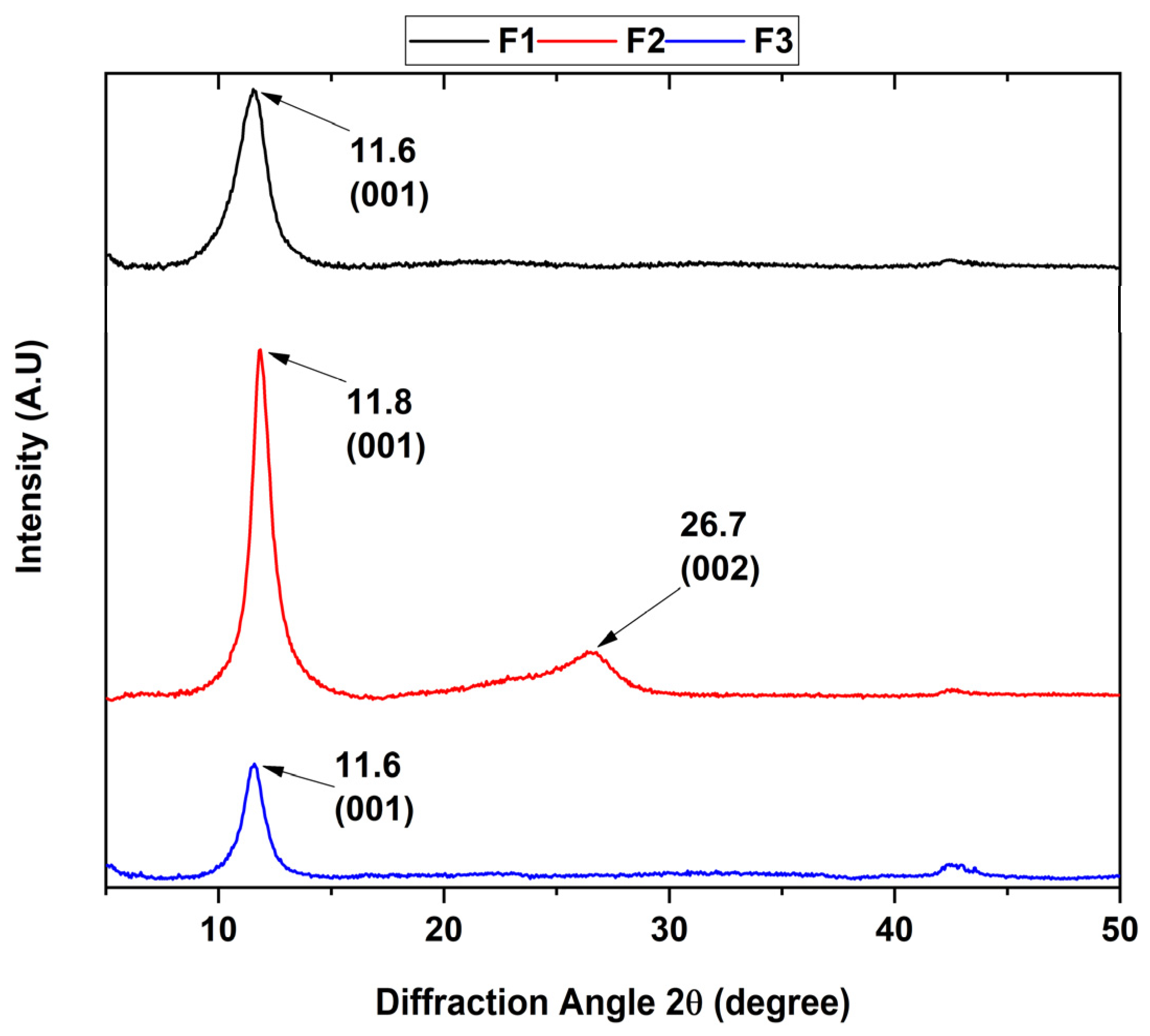
2.1.2. Diffractogram for the Different Graphene Oxides
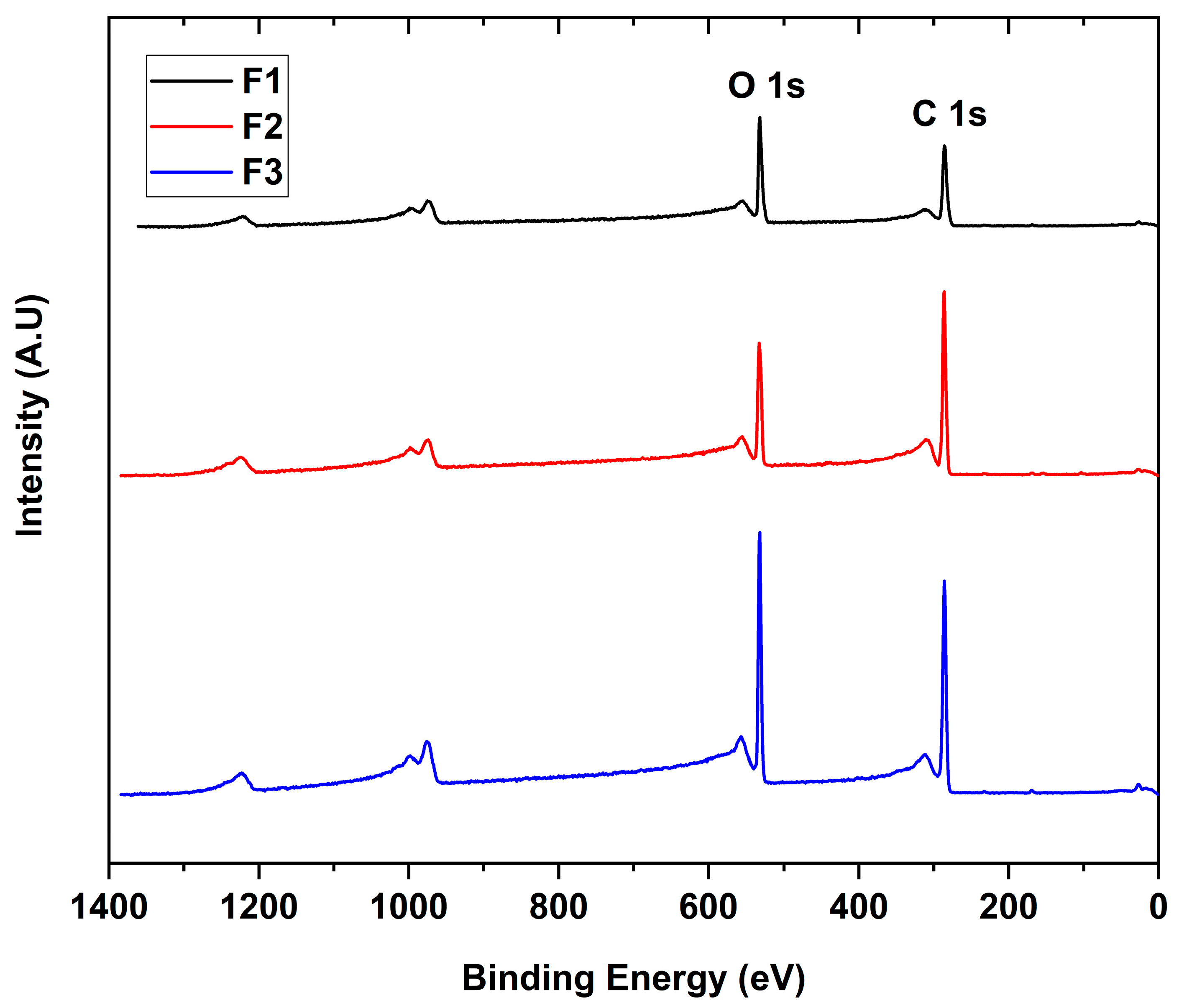
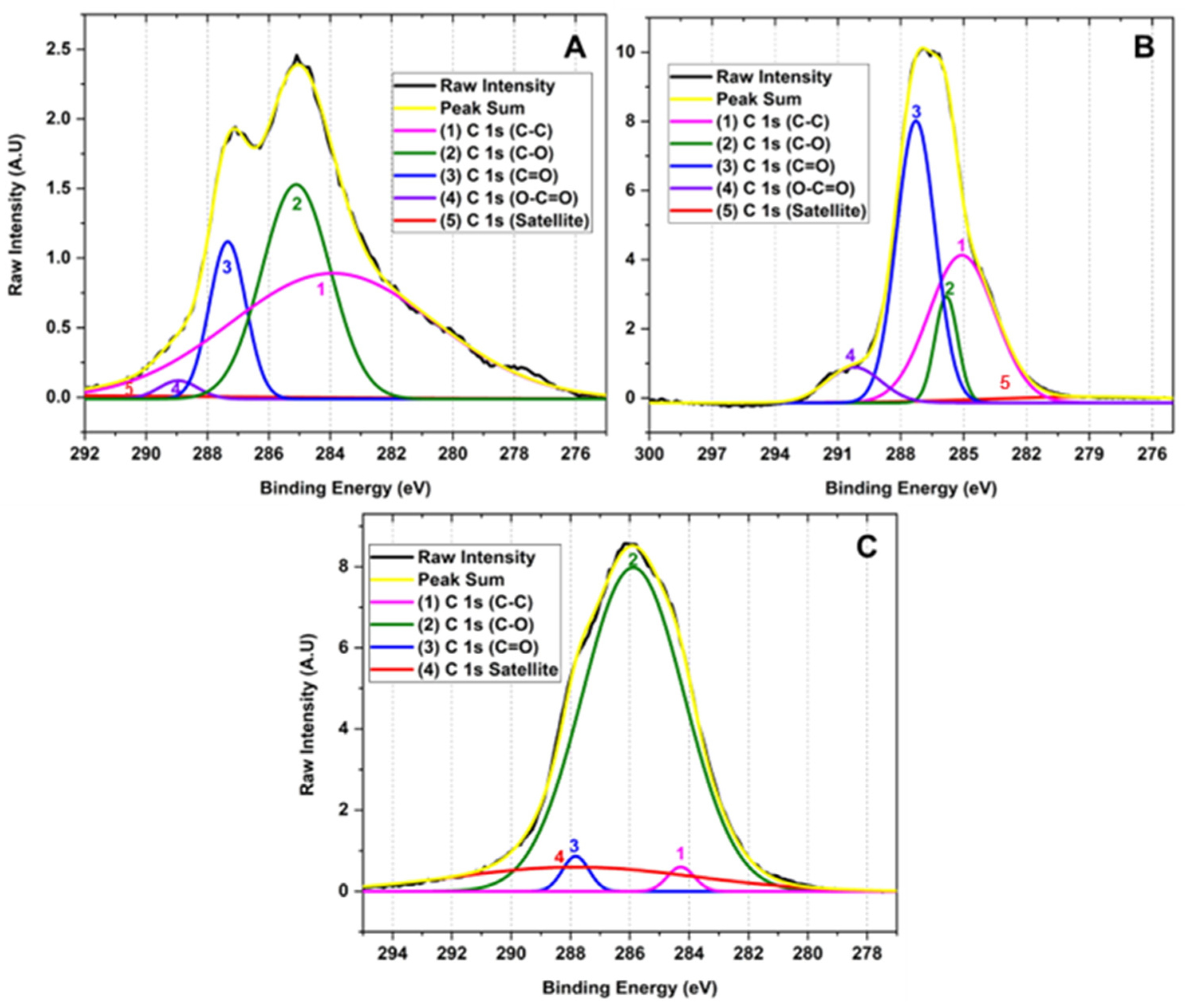
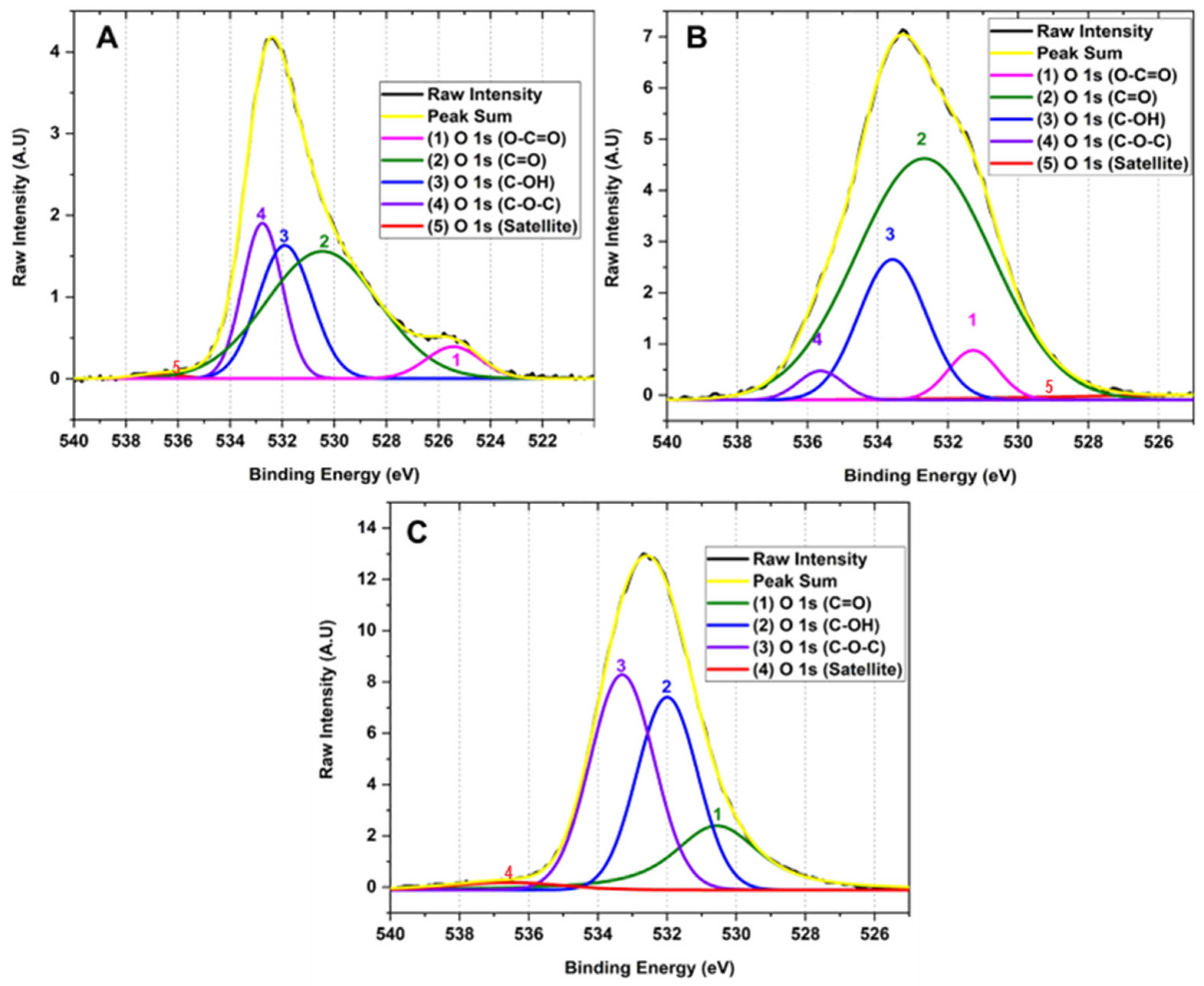
2.1.3. X-ray Photoelectron Spectroscopy
2.1.4. RAMAN Spectroscopy for the Different Synthesized GOs
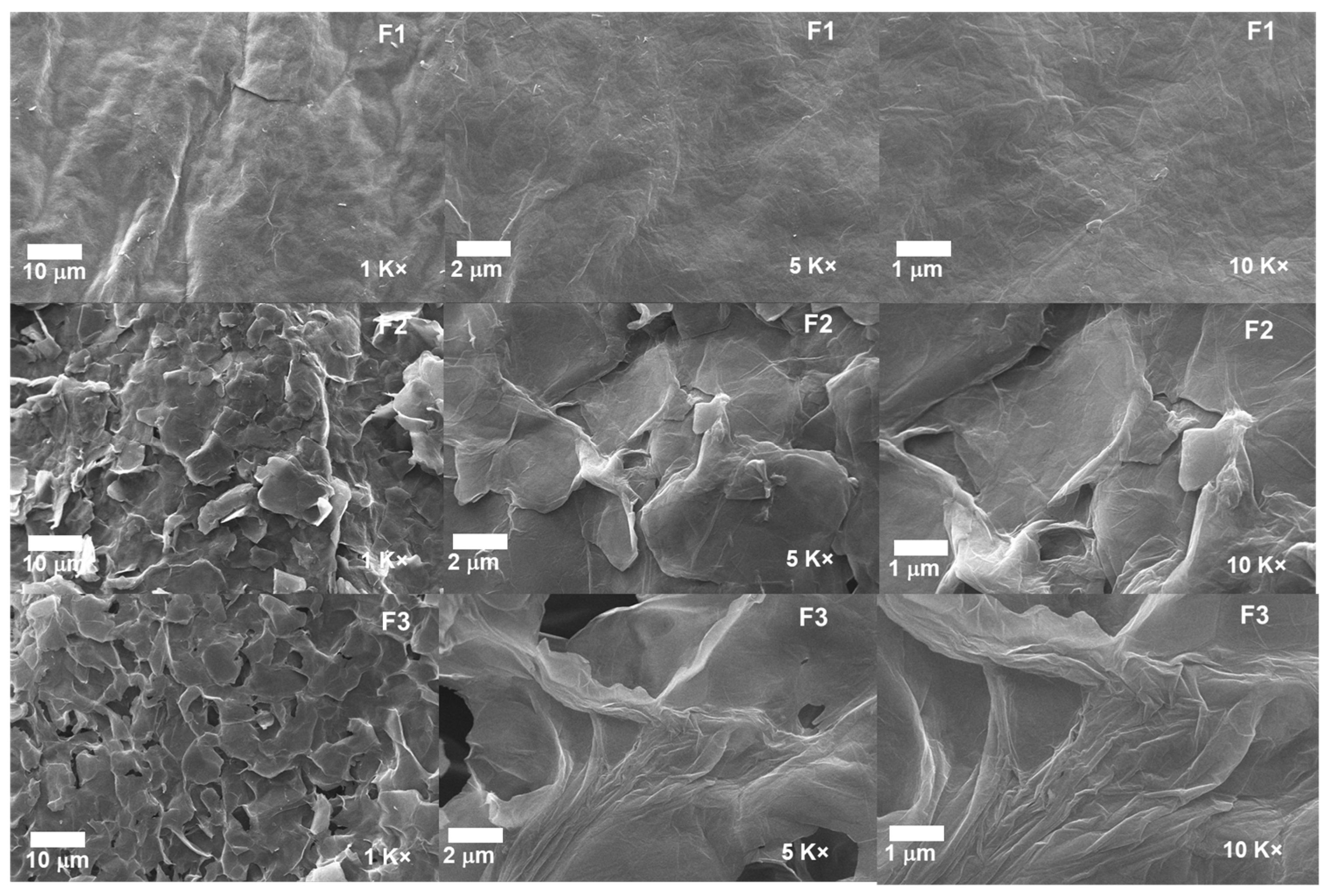
2.1.5. Scanning Electron Microscopy for the Different GOs
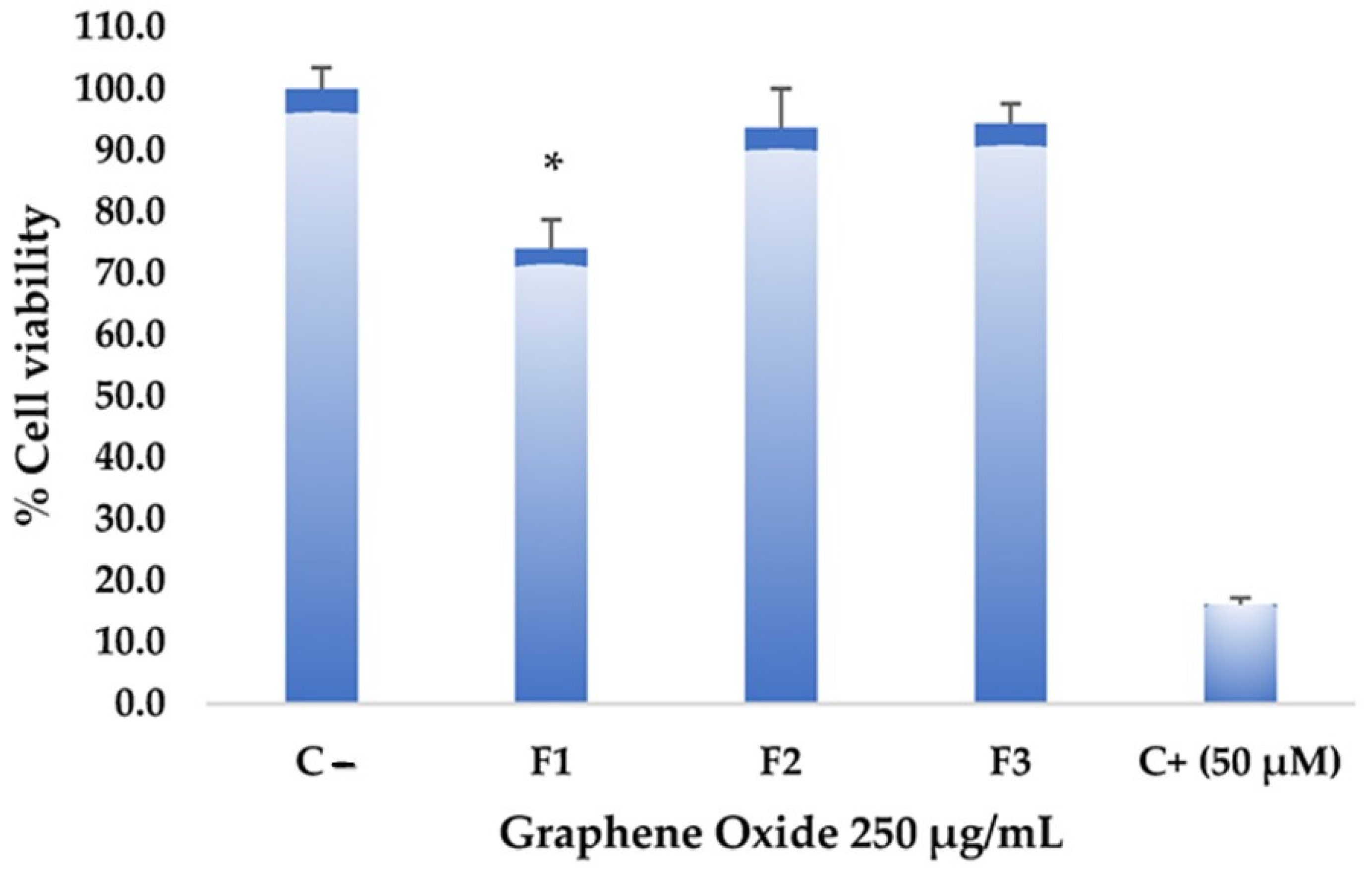
2.1.6. Test of Cytotoxic Activity of Graphene on Hep-2 Cell Line (Cervical Cancer)
2.1.7. Antimicrobial Activity Test of Graphene Oxides
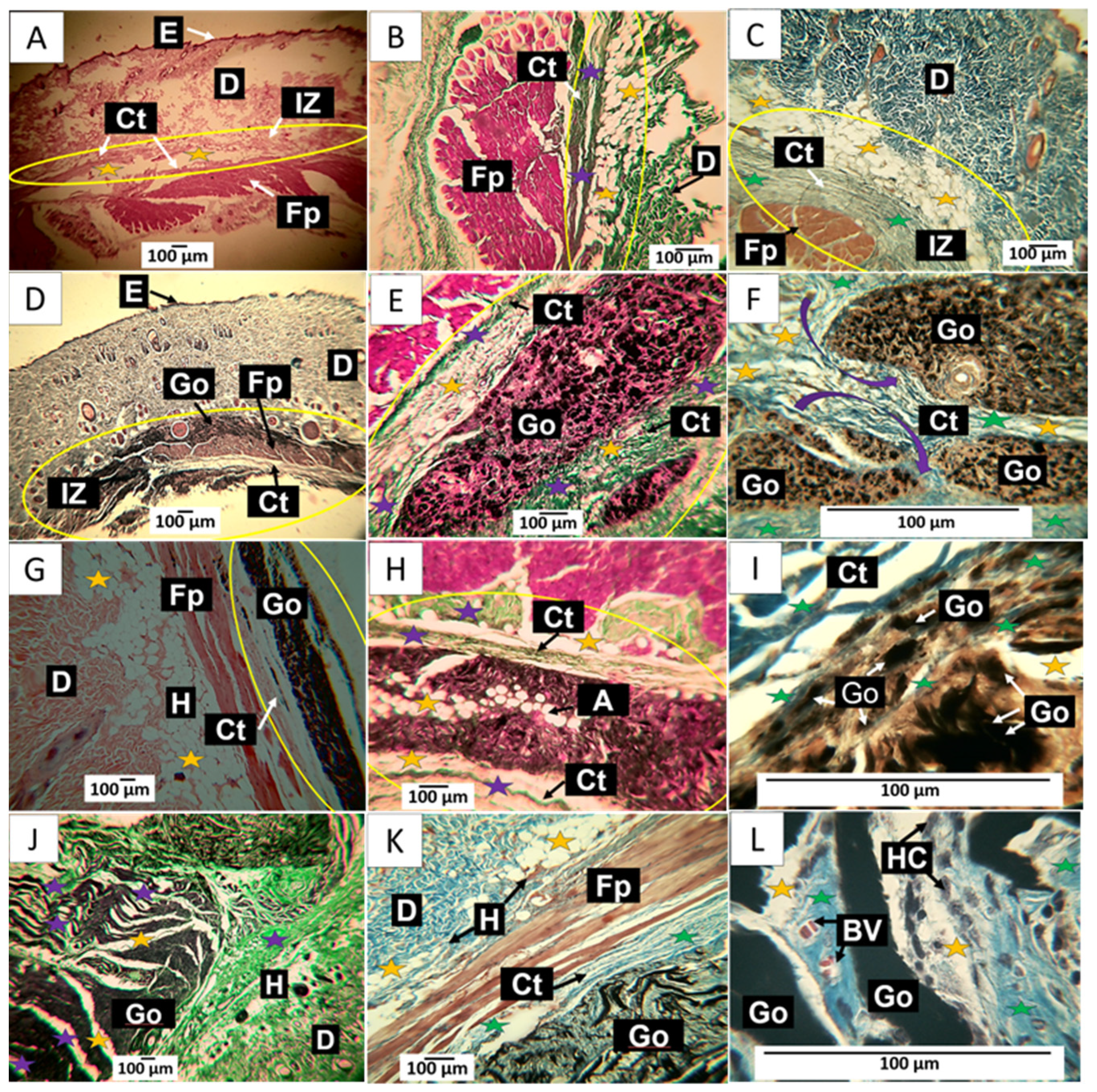
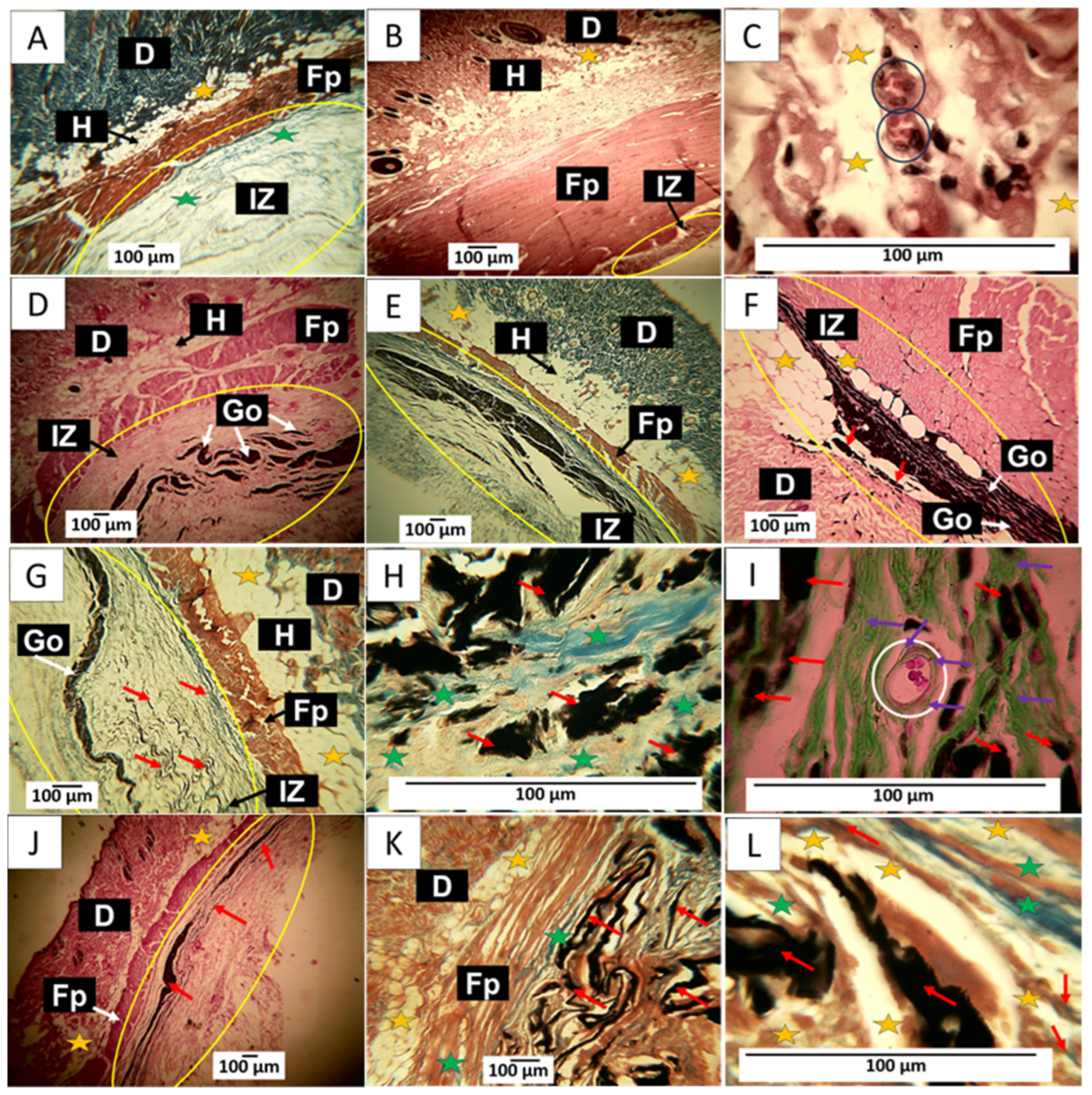
2.1.8. Histology (In Vivo Studies)
Graphene Oxide Implantation Results at 30 Days
Results of Material Implantation at 60 Days
90-Day Material Implementation Results
3. Materials and Methods
3.1. Materials
3.2. Synthesis of Graphene Oxide (GO)
3.3. Characterization of Graphene Oxide
3.3.1. Fourier-Transform Infrared Spectroscopy (FT-IR)
3.3.2. X-ray Diffraction (XRD)
3.3.3. X-ray Photoelectron Spectroscopy (XPS)
3.3.4. RAMAN Spectroscopy
3.3.5. Scanning Electron Microscopy (SEM)
3.3.6. Cultivation and Treatment Conditions
3.3.7. Antimicrobial Activity Test of Graphene Oxides
3.3.8. In Vivo Biocompatibility Study of the Different Graphene Oxides
3.3.9. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Burnett, M.; Abuetabh, Y.; Wronski, A.; Shen, F.; Persad, S.; Leng, R.; Eisenstat, D.; Sergi, C. Graphene oxide nanoparticles induce apoptosis in wild-type and CRISPR/Cas9-IGF/IGFBP3 knocked-out osteosarcoma cells. J. Cancer 2020, 11, 5007. [Google Scholar] [CrossRef] [PubMed]
- Orecchioni, M.; Cabizza, R.; Bianco, A.; Delogu, L.G. Graphene as cancer theranostic tool: Progress and future challenges. Theranostics 2015, 5, 710. [Google Scholar] [CrossRef] [PubMed]
- Berman, N.R.; Koeniger-Donohue, R. Cervical cancer. In Advanced Health Assessment of Women: Clinical Skills and Procedures; Springer Publishing Company: New York, NY, USA, 2018; Volume 431. [Google Scholar]
- Zhao, S.; Huang, L.; Basu, P.; Domingo, E.J.; Supakarapongkul, W.; Ling, W.Y.; Ocviyanti, D.; Rezhake, R.; Qiao, Y.; Tay, E.H.; et al. Cervical cancer burden, status of implementation and challenges of cervical cancer screening in Association of Southeast Asian Nations (ASEAN) countries. Cancer Lett. 2022, 525, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Anton, M.; Horký, M.; Kuchtickova, S.; Vojtĕsek, B.; Blaha, O. Immunohistochemical detection of acetylation and phosphorylation of histone H3 in cervical smears. Ces. Gynekol. 2004, 69, 3–6. [Google Scholar]
- Zhang, P.; Xi, M.; Zhao, L.; Qiu, B.; Liu, H.; Hu, Y.-H.; Liu, M.-Z. Clinical efficacy and failure pattern in patients with cervical esophageal cancer treated with definitive chemoradiotherapy. Radiother. Oncol. 2015, 116, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wu, X.; Cheng, X. Advances in diagnosis and treatment of metastatic cervical cancer. J. Gynecol. Oncol. 2016, 27, e43. [Google Scholar] [CrossRef]
- Baldrighi, M.; Trusel, M.; Tonini, R.; Giordani, S. Carbon nanomaterials interfacing with neurons: An in vivo perspective. Front. Neurosci. 2016, 10, 250. [Google Scholar] [CrossRef]
- Ahlawat, J.; Narayan, M. Introduction to Active, Smart, and Intelligent Nanomaterials for Biomedical Application. In Intelligent Nanomaterials for Drug Delivery Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1–16. [Google Scholar]
- Gurunathan, S.; Kim, J.-H. Synthesis, toxicity, biocompatibility, and biomedical applications of graphene and graphene-related materials. Int. J. Nanomed. 2016, 11, 1927. [Google Scholar] [CrossRef]
- Nejabat, M.; Charbgoo, F.; Ramezani, M. Graphene as multifunctional delivery platform in cancer therapy. J. Biomed. Mater. Res. Part A 2017, 105, 2355–2367. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Chan, C.; Shi, J.; Tsang, M.-K.; Pan, Y.; Cheng, C.; Gerile, O.; Yang, M. A graphene quantum dot@Fe3O4@SiO2 based nanoprobe for drug delivery sensing and dual-modal fluorescence and MRI imaging in cancer cells. Biosens. Bioelectron. 2017, 92, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.; Feng, P.; Wu, P.; Huang, W.; Yang, Y.; Guo, W.; Gao, C.; Shuai, C. Graphene oxide as an interface phase between polyetheretherketone and hydroxyapatite for tissue engineering scaffolds. Sci. Rep. 2017, 7, 46604. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Andrade, M.D.; Chata, G.; Rouholiman, D.; Liu, J.; Saltikov, C.; Chen, S. Antibacterial mechanisms of graphene-based composite nanomaterials. Nanoscale 2017, 9, 994–1006. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-W.; Su, Y.-L.; Hu, S.-H.; Chen, S.-Y. Functionalized graphene nanocomposites for enhancing photothermal therapy in tumor treatment. Adv. Drug Deliv. Rev. 2016, 105, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Yang, R.; Zhang, L.; Fan, Z.; Liu, S. Cytotoxicity effect of graphene oxide on human MDA-MB-231 cells. Toxicol. Mech. Methods 2015, 25, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Loutfy, S.A.; Salaheldin, T.A.; Ramadan, M.A.; Farroh, K.Y.; Abdallah, Z.F.; Youssef, T. Synthesis, characterization and cytotoxic evaluation of graphene oxide nanosheets: In vitro liver cancer model. Asian Pac. J. Cancer Prev. 2017, 18, 955. [Google Scholar] [PubMed]
- Xiao, H.; Jensen, P.E.; Chen, X. Elimination of osteosarcoma by necroptosis with graphene oxide-associated anti-HER2 antibodies. Int. J. Mol. Sci. 2019, 20, 4360. [Google Scholar] [CrossRef]
- Belaid, H.; Nagarajan, S.; Teyssier, C.; Barou, C.; Barés, J.; Balme, S.; Garay, H.; Huon, V.; Cornu, D.; Cavailles, V. Development of new biocompatible 3D printed graphene oxide-based scaffolds. Mater. Sci. Eng. C 2020, 110, 110595. [Google Scholar] [CrossRef]
- de Melo-Diogo, D.; Lima-Sousa, R.; Alves, C.G.; Costa, E.C.; Louro, R.O.; Correia, I.J. Functionalization of graphene family nanomaterials for application in cancer therapy. Colloids Surf. B Biointerfaces 2018, 171, 260–275. [Google Scholar] [CrossRef]
- Ou, L.; Song, B.; Liang, H.; Liu, J.; Feng, X.; Deng, B.; Sun, T.; Shao, L. Toxicity of graphene-family nanoparticles: A general review of the origins and mechanisms. Part. Fibre Toxicol. 2016, 13, 57. [Google Scholar] [CrossRef] [PubMed]
- Jakhar, R.; Yap, J.E.; Joshi, R. Microwave reduction of graphene oxide. Carbon 2020, 170, 277–293. [Google Scholar] [CrossRef]
- Guerrero-Contreras, J.; Caballero-Briones, F. Graphene oxide powders with different oxidation degree, prepared by synthesis variations of the Hummers method. Mater. Chem. Phys. 2015, 153, 209–220. [Google Scholar] [CrossRef]
- Claramunt, S.; Varea, A.; López-Díaz, D.; Velázquez, M.M.; Cornet, A.; Cirera, A. The importance of interbands on the interpretation of the raman spectrum of graphene oxide. J. Phys. Chem. C 2015, 119, 10123–10129. [Google Scholar] [CrossRef]
- Trömel, M.; Russ, M. Dimanganese heptoxide for the selective oxidation of organic substrates. Angew. Chem. Int. Ed. Engl. 1987, 26, 1007–1009. [Google Scholar] [CrossRef]
- Dash, S.; Patel, S.; Mishra, B.K. Oxidation by permanganate: Synthetic and mechanistic aspects. Tetrahedron 2009, 65, 707–739. [Google Scholar] [CrossRef]
- Santamaría-juarez, G.; Gómez-Barojas, E.; Quiroga-González, E.; Sánchez-Mora, E.; Quintana-Ruiz, M.; Santamaría-Juárez, J.D. Safer modified Hummer’s method for the synthesis of graphene oxide with high quality and high yield. Mater. Res. Express 2020, 6, 125631. [Google Scholar] [CrossRef]
- Liu, D.; Bian, Q.; Li, Y.; Wang, Y.; Xiang, A.; Tian, H. Effect of oxidation degrees of graphene oxide on the structure and properties of poly (vinyl alcohol) composite fi lms. Compos. Sci. Technol. 2016, 129, 146–152. [Google Scholar] [CrossRef]
- Itoo, A.M.; Vemula, S.L.; Gupta, M.T.; Giram, M.V.; Kumar, S.A.; Ghosh, B.; Biswas, S. Multifunctional graphene oxide nanoparticles for drug delivery in cancer. J. Control. Release 2022, 350, 26–59. [Google Scholar] [CrossRef]
- Dash, B.S.; Jose, G.; Lu, Y.-J.; Chen, J.-P. Functionalized reduced graphene oxide as a versatile tool for cancer therapy. Int. J. Mol. Sci. 2021, 22, 2989. [Google Scholar] [CrossRef]
- Báez, D.F. Graphene-Based Nanomaterials for Photothermal Therapy in Cancer Treatment. Pharmaceutics 2023, 15, 2286. [Google Scholar] [CrossRef] [PubMed]
- Dorsett-Martin, W.A. Rat models of skin wound healing: A review. Wound Repair Regen. 2004, 12, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Moeini, A.; Pedram, P.; Makvandi, P.; Malinconico, M.; Gomez d’Ayala, G. Wound healing and antimicrobial effect of active secondary metabolites in chitosan-based wound dressings: A review. Carbohydr. Polym. 2020, 233, 115839. [Google Scholar] [CrossRef] [PubMed]
- Vidinský, B.; Gál, P.; Toporcer, T.; Longauer, F.; Lenhardt, L.; Bobrov, N.; Sabo, J. Histological study of the first seven days of skin wound healing in rats. Acta Vet. Brno 2006, 75, 197–202. [Google Scholar] [CrossRef]
- Tottoli, E.M.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735. [Google Scholar] [CrossRef] [PubMed]
- Babensee, J.E. Inflammation, Wound Healing, the Foreign-Body Response, and Alternative Tissue Responses, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2020; ISBN 9780128161371. [Google Scholar]
- Klopfleisch, R.; Jung, F. The pathology of the foreign body reaction against biomaterials. J. Biomed. Mater. Res. Part A 2017, 105, 927–940. [Google Scholar] [CrossRef]
- Surekha, G.; Krishnaiah, K.V.; Ravi, N.; Suvarna, R.P. FTIR, Raman and XRD analysis of graphene oxide films prepared by modified Hummers method. J. Phys. Conf. Ser. 2020, 1495, 12012. [Google Scholar] [CrossRef]
- ISO 1093-6; Biological Evaluation of Medical Devices. Part 6: Tests for Local Effects after Implantation. ISO: Geneva, Switzerland, 2016.
- Grande-Tovar, C.D.; Castro, J.I.; Valencia Llano, C.H.; Tenorio, D.L.; Saavedra, M.; Zapata, P.A.; Chaur, M.N. Polycaprolactone (PCL)-Polylactic acid (PLA)-Glycerol (Gly) Composites Incorporated with Zinc Oxide Nanoparticles (ZnO-NPs) and Tea Tree Essential Oil (TTEO) for Tissue Engineering Applications. Pharmaceutics 2023, 15, 43. [Google Scholar] [CrossRef]
- Castro, J.I.; Valencia-llano, C.H.; Eliana, M.; Zapata, V.; Restrepo, Y.J.; Mina, H.; Navia-porras, D.P.; Valencia, Y.; Valencia, C.; Grande-tovar, C.D. Chitosan/Polyvinyl Alcohol/Tea Tree Essential Oil Composite Films for Biomedical Applications. Polymers 2021, 13, 3753. [Google Scholar] [CrossRef]

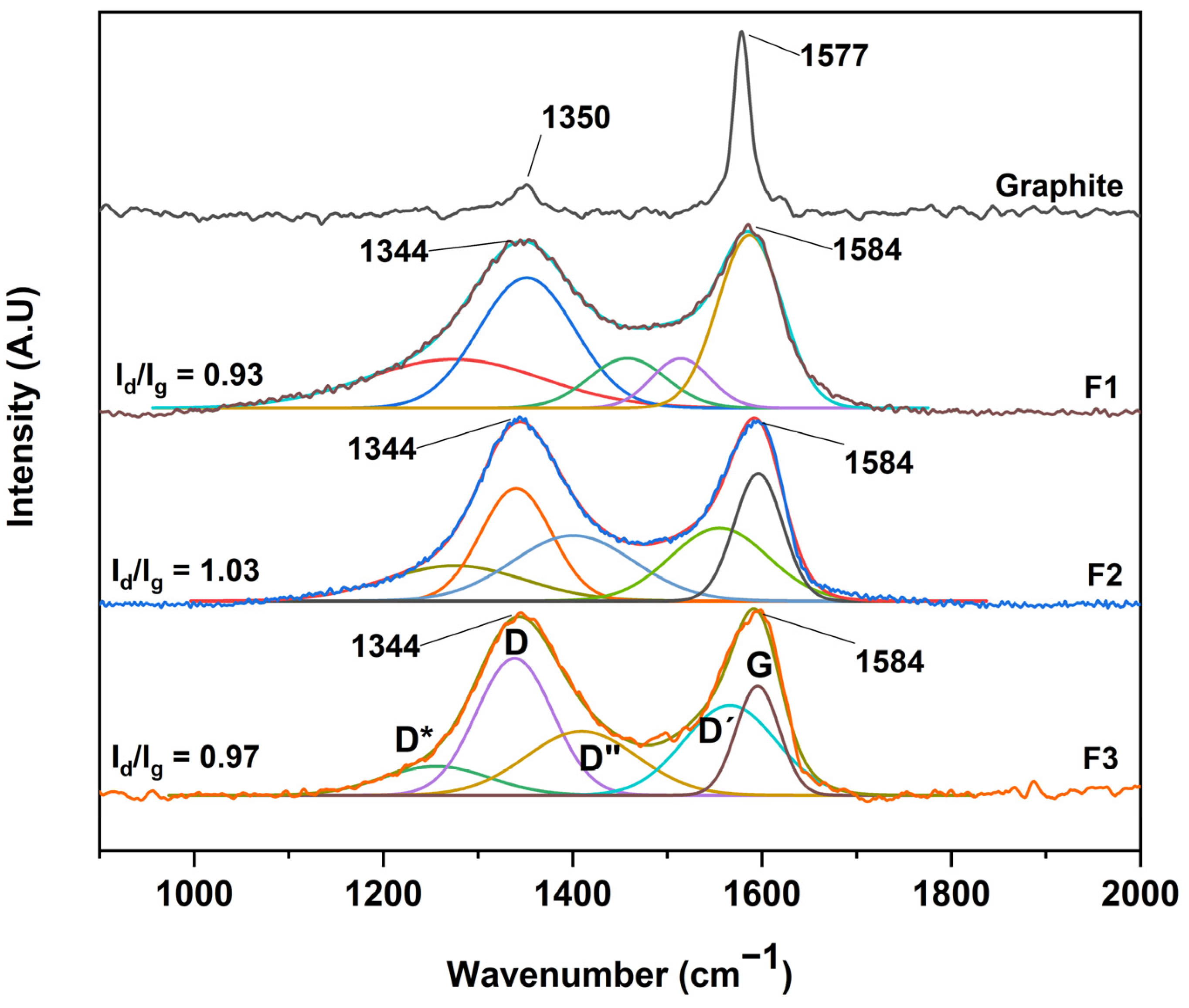


| F1 | F2 | F3 | ||||
|---|---|---|---|---|---|---|
| Band | A | PB (cm−1) | A | PB (cm−1) | A | PB (cm−1) |
| D* | 59.3 | 1274 | 33.7 | 1275 | 21.2 | 1256 |
| D | 86.0 | 1351 | 55.0 | 1340 | 71.8 | 1339 |
| D″ | 26.2 | 1457 | 54.6 | 1400 | 48.8 | 1410 |
| G | 76.2 | 1587 | 42.3 | 1596 | 32.4 | 1596 |
| D′ | 19.8 | 1514 | 49.1 | 1555 | 57.0 | 1566 |
| AD/AG | 2.646 | 0.852 | 2.267 | |||
| R2 | 0.997 | 0.997 | 0.996 | |||
| X2 | 0.00028 | 0.00024 | 0.00042 | |||
| Inhibition Percentages (%) | |||
|---|---|---|---|
| F1 | F2 | F3 | |
| S. aureus | 8.2 ± 2.8 | 8.1 ± 1.7 | 1.0 ± 0.1 |
| E. coli | 4.2 ± 0.4 | 1.16 ± 1.0 | 0.6 ± 0.3 |
| Components | F1 | F2 | F3 |
|---|---|---|---|
| Graphite (g) | 3 | 3 | 3 |
| KMnO4 (g) | 9 | 18 | 27 |
| H2SO4 (mL) | 90 | 90 | 90 |
| Time (h) | 24 | 48 | 72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro, J.I.; Payan-Valero, A.; Valencia-Llano, C.H.; Insuasty, D.; Rodríguez Macias, J.D.; Ordoñez, A.; Valencia Zapata, M.E.; Mina Hernández, J.H.; Grande-Tovar, C.D. Evaluation of the Antibacterial, Anti-Cervical Cancer Capacity, and Biocompatibility of Different Graphene Oxides. Molecules 2024, 29, 281. https://doi.org/10.3390/molecules29020281
Castro JI, Payan-Valero A, Valencia-Llano CH, Insuasty D, Rodríguez Macias JD, Ordoñez A, Valencia Zapata ME, Mina Hernández JH, Grande-Tovar CD. Evaluation of the Antibacterial, Anti-Cervical Cancer Capacity, and Biocompatibility of Different Graphene Oxides. Molecules. 2024; 29(2):281. https://doi.org/10.3390/molecules29020281
Chicago/Turabian StyleCastro, Jorge Ivan, Alana Payan-Valero, Carlos Humberto Valencia-Llano, Daniel Insuasty, Juan David Rodríguez Macias, Alejandra Ordoñez, Mayra Eliana Valencia Zapata, Jose Herminsul Mina Hernández, and Carlos David Grande-Tovar. 2024. "Evaluation of the Antibacterial, Anti-Cervical Cancer Capacity, and Biocompatibility of Different Graphene Oxides" Molecules 29, no. 2: 281. https://doi.org/10.3390/molecules29020281
APA StyleCastro, J. I., Payan-Valero, A., Valencia-Llano, C. H., Insuasty, D., Rodríguez Macias, J. D., Ordoñez, A., Valencia Zapata, M. E., Mina Hernández, J. H., & Grande-Tovar, C. D. (2024). Evaluation of the Antibacterial, Anti-Cervical Cancer Capacity, and Biocompatibility of Different Graphene Oxides. Molecules, 29(2), 281. https://doi.org/10.3390/molecules29020281








