Polyamidoamine Dendron-Bearing Lipids as Drug-Delivery Excipients
Abstract
1. Introduction
2. Results and Discussion
2.1. Characterization
CMC Analysis
2.2. Drug Loading Studies
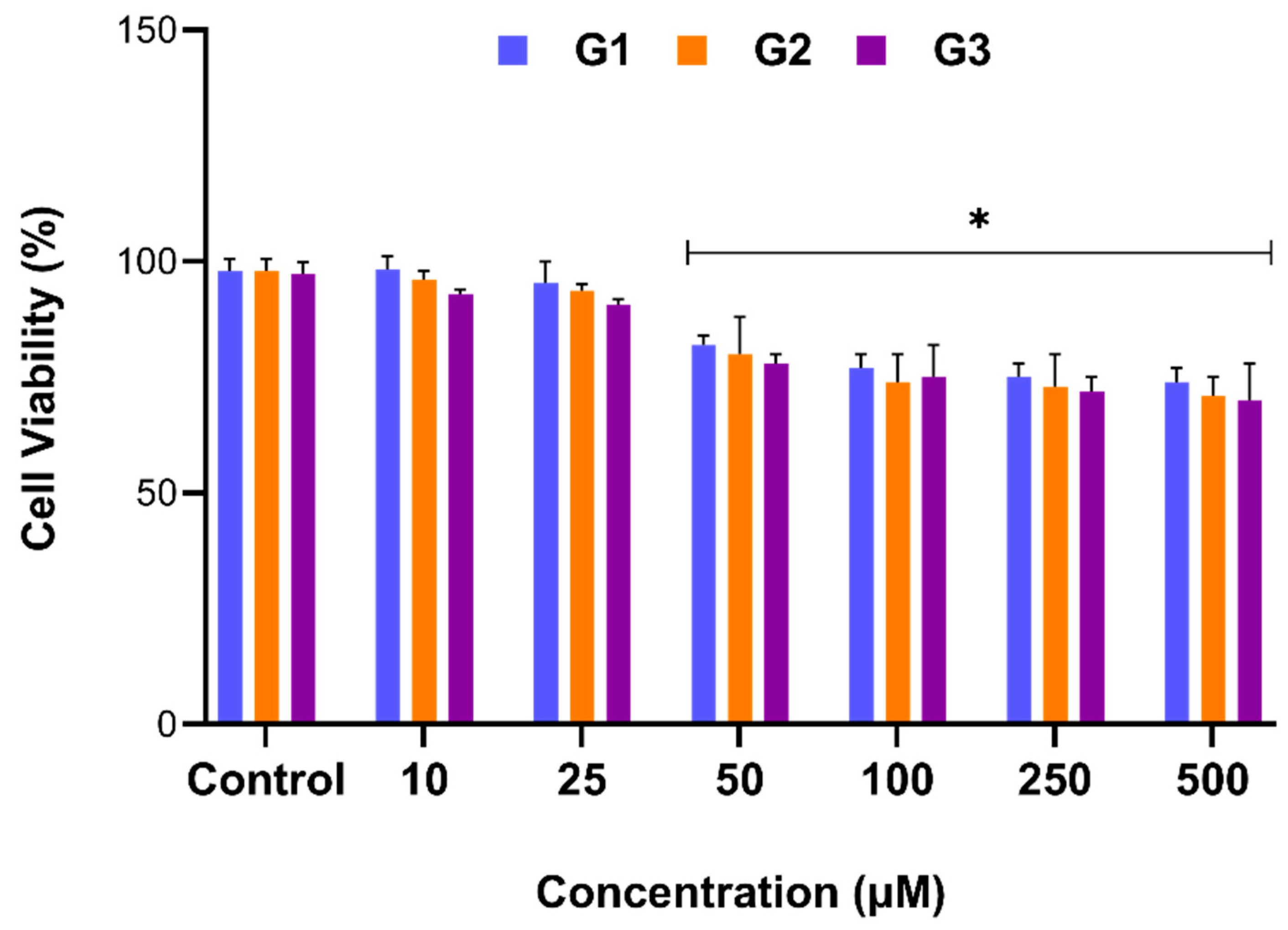
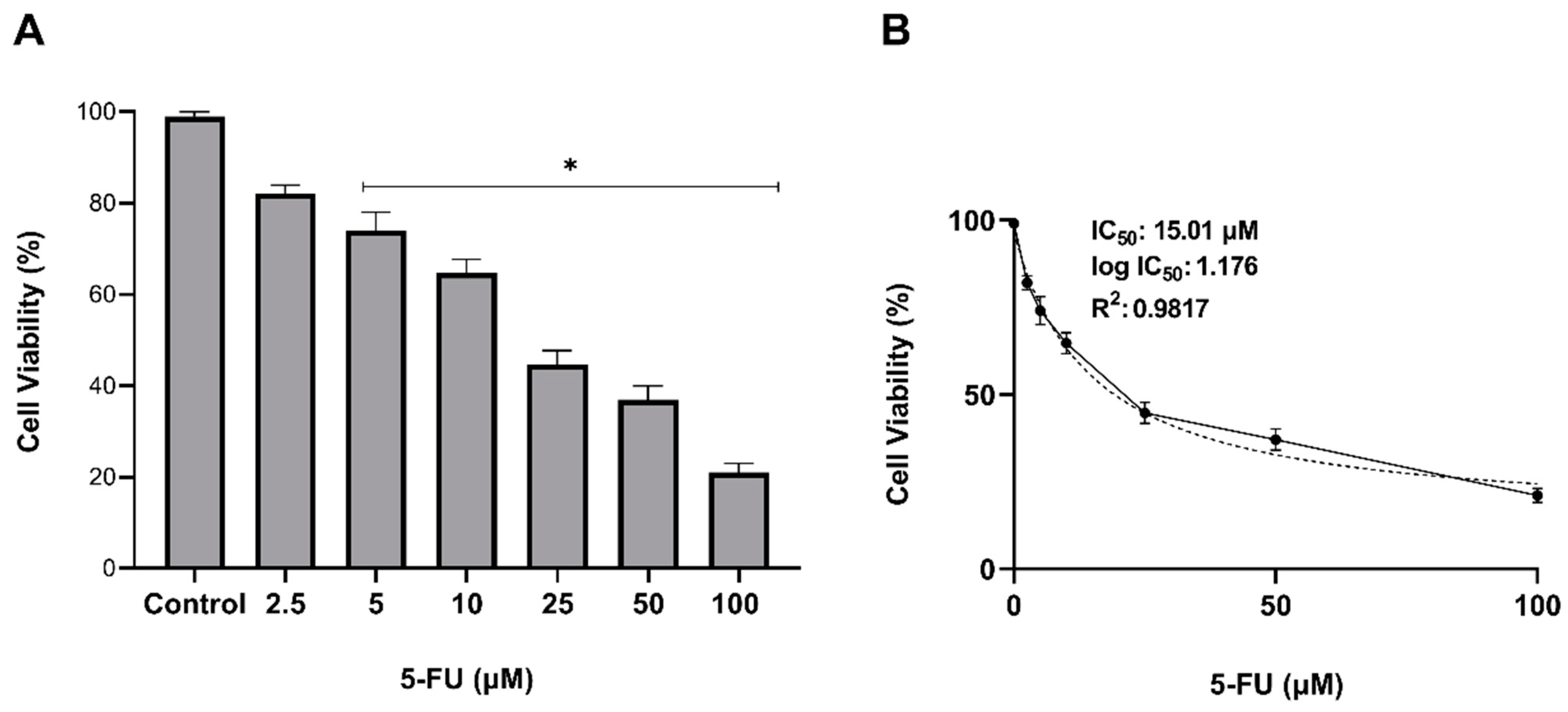
2.3. Cytotoxic Activity Results
3. Materials and Methods
3.1. Chemicals and Reagents
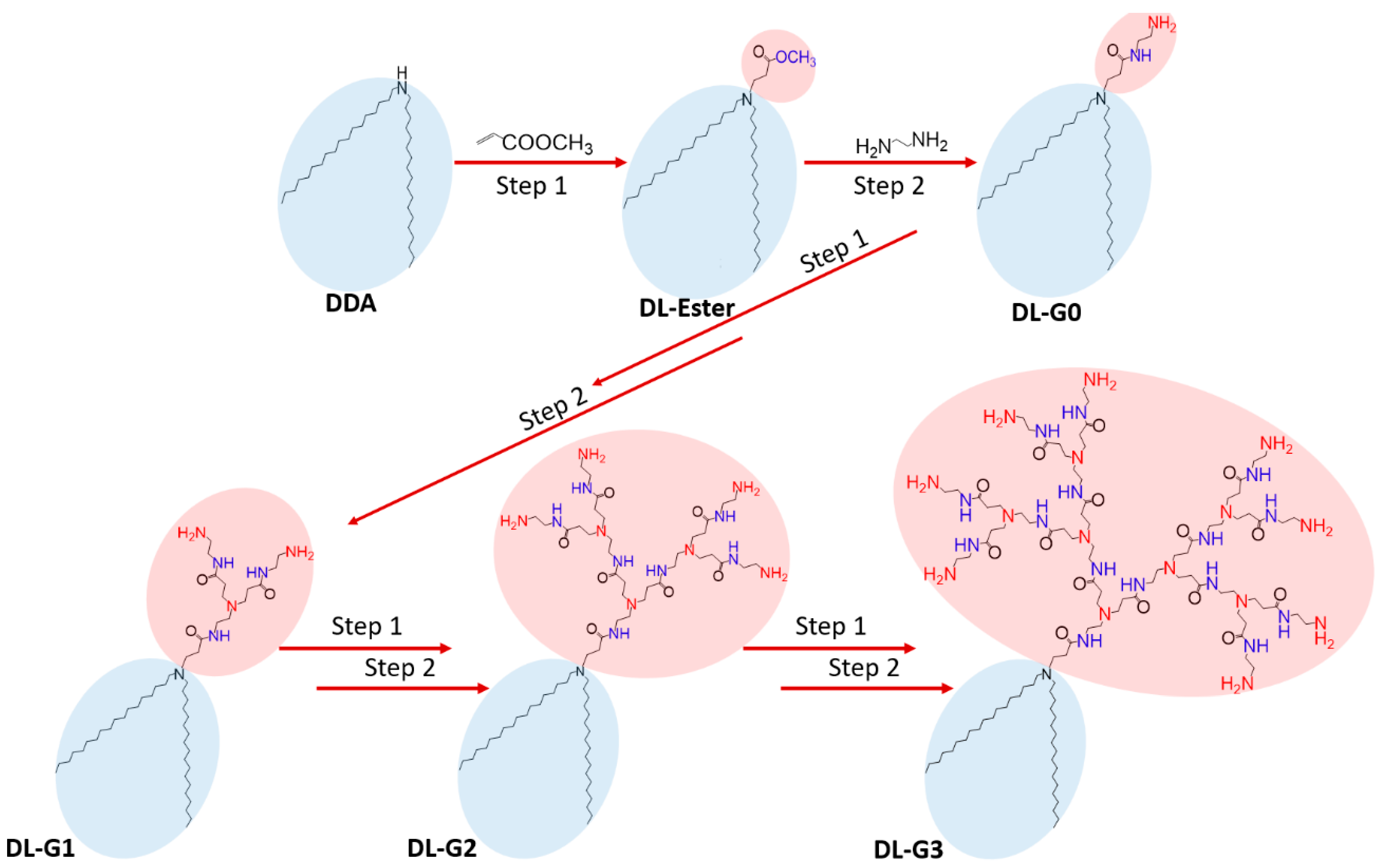
3.2. Synthesis of PAMAM Dendron Bearing Lipids
3.3. Preparation of PAMAM Dendron Lipid Containing Liposomes
3.4. Characterisation of Liposomes
3.5. Determination of Critical Micelle Concentration (CMC)
3.6. In Vitro Assays
3.6.1. Cell Culture
3.6.2. Cytotoxicity Assay
3.6.3. Statistical Analyses
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kavitha, K.; Srinivasa, A.; Nalini, C.N. An Investigation on Enchacement of Solubility of 5 Flourouracil by Applying Complexation Technique-Characterization, Dissolution and Molecular-Modeling Studies. J. Appl. Pharm. Sci. 2013, 3, 162–166. [Google Scholar]
- Presant, C.A.; Jacobson, J.; Wolf, W.; Waluch, V.; Weitz, I.C.; Macdonald, J.S. Does leucovorin alter the intratumoral pharmacokinetics of 5-fluorouracil (5-FU) A Southwest Oncology Group study. Investig. New Drugs 2002, 20, 369–376. [Google Scholar]
- Ychou, M.; Coroy, T.; Seitz, J.F.; Gourgous, S.; Hua, A.; Mery, D.; Kramer, A. An open phase I study assessing the feasibility of the triple combination: Oxaliplatin plus irinotecan plus leucovorin/ 5-fluorouracil every 2 weeks in patients with advanced solid tumors. Ann. Oncol. 2003, 14, 481–489. [Google Scholar] [PubMed]
- Van den Boogaard, W.M.C.; Komninos, D.S.J.; Vermeij, W.P. Chemotherapy Side-Effects: Not All DNA Damage Is Equal. Cancers 2022, 14(3), 627. [Google Scholar]
- Duncan, R. The dawning era of polymer therapeutics. Nat. Rev. Drug Discov. 2003, 2, 347–360. [Google Scholar]
- Richter, A.; Wiedekind, A.; Krause, M.; Kissel, T.; Haag, R.; Olbrich, C. Non-ionic dendritic glycerol based amphiphiles: Novel excipients for the solubilization of poorly water-soluble anticancer drug Sagopilone. Eur. J. Pharm. Sci. 2010, 40, 43–55. [Google Scholar]
- Li, P.; Zhao, L. Developing early formulations: Practice and perspective. Int. J. Pharm. 2007, 341, 1–19. [Google Scholar]
- Kesharwani, P.; Jain, K.; Jain, N.K. Dendrimers as nanocarrier for drug delivery. Prog. Polym. Sci. 2014, 39, 268–307. [Google Scholar]
- Jain, N.; Gupta, U. Application of Dendrimer-Drug Complexation in the Enhancement of Drug Solubility and Bioavailability. Expert Opin. Drug Metab. Toxicol. 2008, 4, 52–1035. [Google Scholar]
- Nanjwade, B.; Bechra, H.; Derkara, G.; Manvi, F.; Nanjwade, V. Dendrimers: Emerging Polymers for Drug Delivery Systems. Eur. J. Pharm. Sci. 2009, 38, 96–185. [Google Scholar]
- Robert, J.C.; Bhalgat, M.K.; Zera, R.T. Preliminary biological evaluation of Polyamidoamine (PAMAM) starburst dendrimers. J. Biomed. Mater. Res. 1996, 30, 53–65. [Google Scholar] [CrossRef]
- Koç, F.E.; Senel, M. Solubility Enhancement of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) Using Polypolypropylene Oxide Core PAMAM Dendrimers. Int. J. Pharm. 2013, 451, 18–22. [Google Scholar] [CrossRef]
- Sagir, T.; Huysal, M.; Senel, M.; Isık, S.; Burgucu, N.; Tabakoglu, O.; Zaim, M. Folic acid conjugated PAMAM-modified mesoporous silica-coated superparamagnetic iron oxide nanoparticles for potential cancer therapy. J. Colloid Interface Sci. 2022, 625, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.M. Stuart, Liposomes pharmacokinetics. Liposomes Ration. Des. 1999, 24, 63–87. [Google Scholar]
- Purohit, G.; Sakthivel, T.; Florence, A. Interaction of cationic partial dendrimers with charged and neutral liposomes. Int. Pharm. 2001, 214, 71–76. [Google Scholar] [CrossRef]
- Jhaveri, A.M.; Torchilin, V.P. Multifunctional polymeric micelles for delivery of drugs and siRNA. Front. Pharmacol. 2014, 5, 77. [Google Scholar] [CrossRef]
- Liu, Z.; Liu, D.; Wang, L.; Zhang, J.; Na, Z. Docetaxel-Loaded Pluronic P123 Polymeric Micelles: In Vitro and in Vivo Evaluation. Int. J. Mol. Sci. 2011, 12, 1684–1696. [Google Scholar] [CrossRef]
- Shakeel, F.; Haq, N.; Al-Dhfyan, A.; Alanazi, F.K.; Alsarra, I.A. Double w/o/w nanoemulsion of 5-fluorouracil for self-nanoemulsifying drug delivery system. J. Mol. Liq. 2014, 200 Pt B, 183–190. [Google Scholar] [CrossRef]
- Shishu; Kamalpreet; Maheshwari, M. Development and evaluation of novel microemulsion based oral formulations of 5-fluorouracil using non-everted rat intestine sac model. Drug Dev. Ind. Pharm. 2012, 38, 294–300. [Google Scholar] [CrossRef]
- Youssof, A.M.E.; Alanazi, F.K.; Salem-Bekhit, M.M.; Shakeel, F.; Haq, N. Bacterial Ghosts Carrying 5-Fluorouracil: A Novel Biological Carrier for Targeting Colorectal Cancer. AAPS PharmSciTech 2019, 20, 48. [Google Scholar] [CrossRef]
- Yassin, A.E.; Anwer, M.K.; Mowafy, H.A.; El-Bagory, I.M.; Bayomi, M.A.; Alsarra, I.A. Optimization of 5-flurouracil solid-lipid nanoparticles: A preliminary study to treat colon cancer. Int. J. Med. Sci. 2010, 7, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Sağir, T.; Huysal, M.; Durmus, Z.; Kurt, B.Z.; Senel, M. Preparation and in vitro evaluation of 5-flourouracil loaded magnetite-zeolite nanocomposite (5-FU-MZNC) for cancer drug delivery. Biomed. Pharmacother. 2016, 77, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Naha, P.C.; Mukherjee, S.P.; Byrne, H.J. Toxicology of Engineered Nanoparticles: Focus on Poly(amidoamine) Dendrimers. Int. J. Environ. Res. Public Health 2018, 15, 338. [Google Scholar] [CrossRef] [PubMed]
- Luong, D.; Kesharwani, P.; Deshmukh, R.; Mohd Amin, M.C.I.; Gupta, U.; Greish, K.; Iyer, A.K. PEGylated PAMAM dendrimers: Enhancing efficacy and mitigating toxicity for effective anticancer drug and gene delivery. Acta Biomater 2016, 43, 14–29. [Google Scholar] [CrossRef]
- Tomalia, D.A.; Baker, H.; Dewald, J.; Hall, M.; Kallos, G.; Martin, S.; Roeck, J.; Smith, P. A new class of polymers: Starburst-Dendritic Macromolecules. Polym. J. 1985, 17, 117–132. [Google Scholar] [CrossRef]
- Frechet, J.M.J.; Tomalia, D.A. Dendrimers and Other Dendritic Polymers; John Wiley & Sons, Inc.: New York, NY, USA, 2001. [Google Scholar]
- Takahashi, T.; Kono, K.; Itoh, T.; Nobuhiko, E.; Takagishi, T. Synthesis of Novel Cationic Lipids Having Polyamidoamine Dendron and Their Transfection Activity. Bioconjugate Chem. 2003, 14, 764–773. [Google Scholar] [CrossRef]
- Karakuş, K. Synthesis and Preparation of Polymeric Drug Carrier Micelles. Master’s Thesis, Istanbul Technical University, Istanbul, Turkey, 2011. [Google Scholar]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarigul, E.; Zaim, M.; Senel, M.; Sagir, T.; Isik, S. Polyamidoamine Dendron-Bearing Lipids as Drug-Delivery Excipients. Molecules 2022, 27, 7817. https://doi.org/10.3390/molecules27227817
Sarigul E, Zaim M, Senel M, Sagir T, Isik S. Polyamidoamine Dendron-Bearing Lipids as Drug-Delivery Excipients. Molecules. 2022; 27(22):7817. https://doi.org/10.3390/molecules27227817
Chicago/Turabian StyleSarigul, Ender, Merve Zaim, Mehmet Senel, Tugba Sagir, and Sevim Isik. 2022. "Polyamidoamine Dendron-Bearing Lipids as Drug-Delivery Excipients" Molecules 27, no. 22: 7817. https://doi.org/10.3390/molecules27227817
APA StyleSarigul, E., Zaim, M., Senel, M., Sagir, T., & Isik, S. (2022). Polyamidoamine Dendron-Bearing Lipids as Drug-Delivery Excipients. Molecules, 27(22), 7817. https://doi.org/10.3390/molecules27227817






