Ethnobotanical Uses, Phytochemistry, Toxicology, and Pharmacological Properties of Euphorbia neriifolia Linn. against Infectious Diseases: A Comprehensive Review
Abstract
:1. Introduction
- Morphological and phytopharmacological screening of E. neriifolia extracts;
- Ethnobotanical-based updates for medicinal and domestic usage of this plant;
- Antimicrobial activities with the mechanism of actions of different extracts of the plant and derived compounds;
- Toxicological profile with clinical updates and the potential treatment of toxicity.
2. Methods
3. Morphology
3.1. Leaves
3.2. Involucres
3.3. Flowers
3.4. Fruits
3.5. Seeds
3.6. Branch
3.7. Stem
3.8. Stippular Thorns
3.9. Glands
3.10. Powder
3.11. Latex
3.12. Taxonomy
3.13. Vernacular Name
4. Ethnobotanical Uses
4.1. Latex
4.2. Leaves
4.3. Stems
4.4. Roots
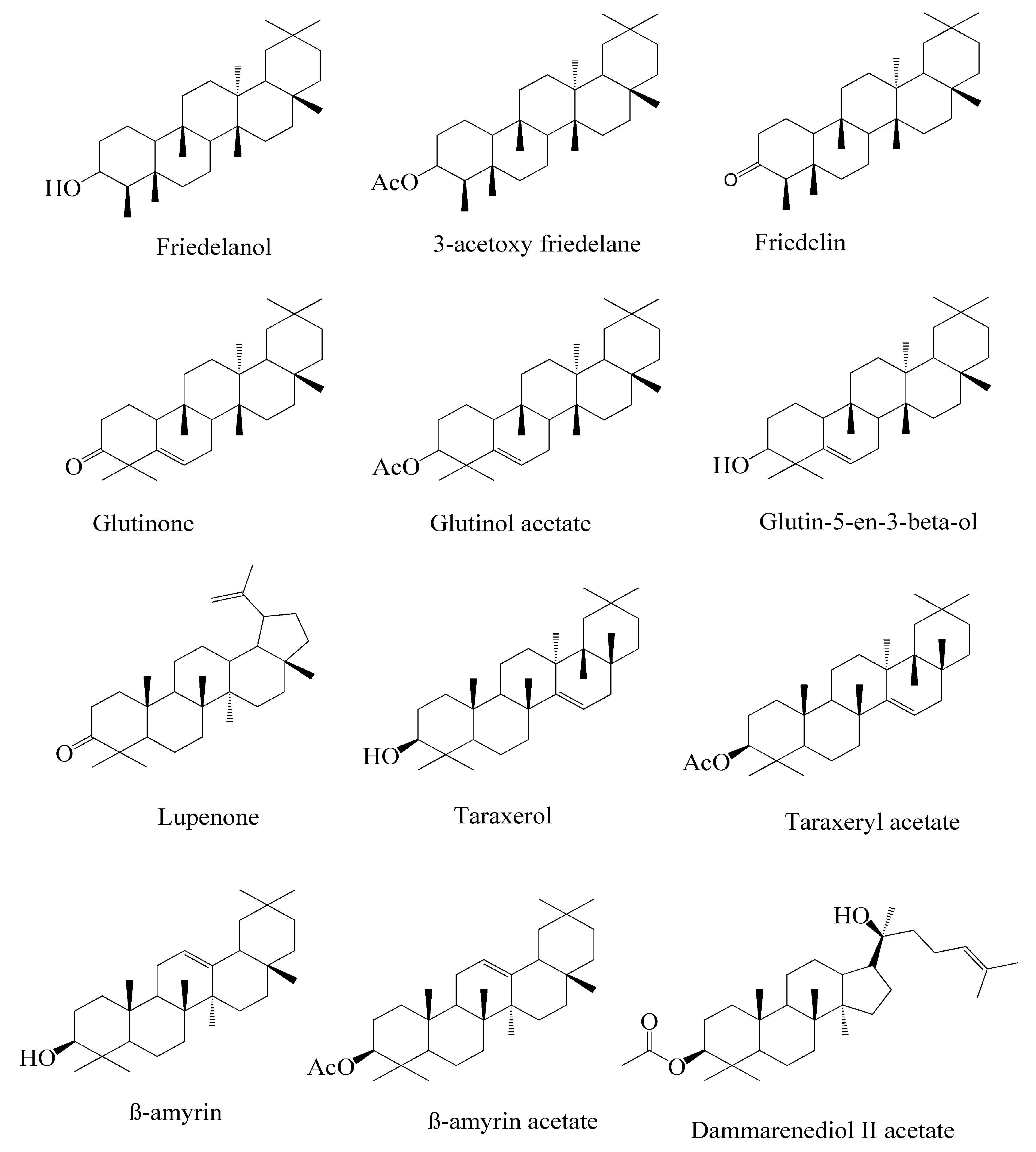
5. Phytoconstituents
6. Antimicrobial Activities of E. neriifolia and Its Constituents
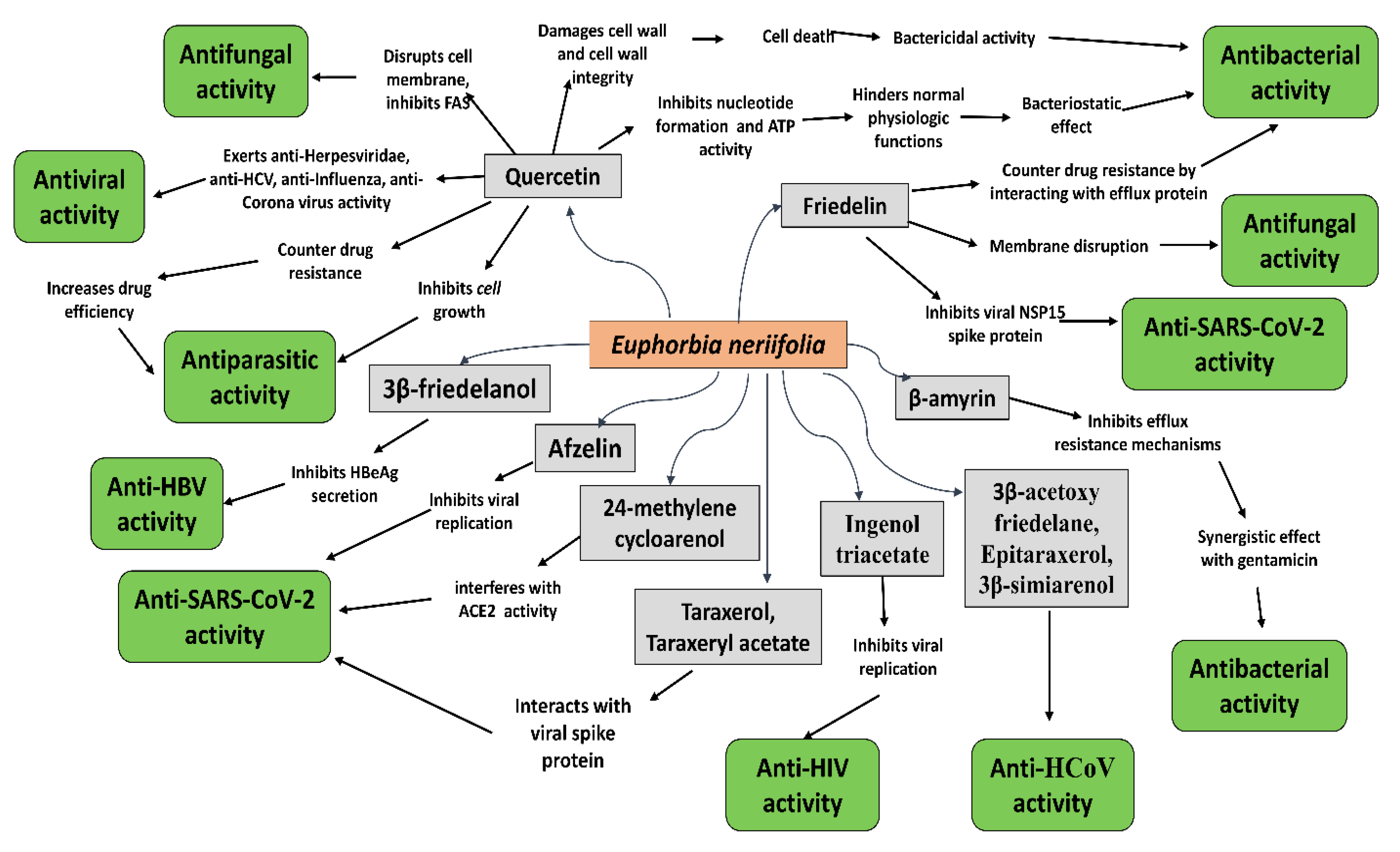
6.1. Antibacterial Activities
6.2. Antifungal Activities
6.3. Antiparasitic Activities
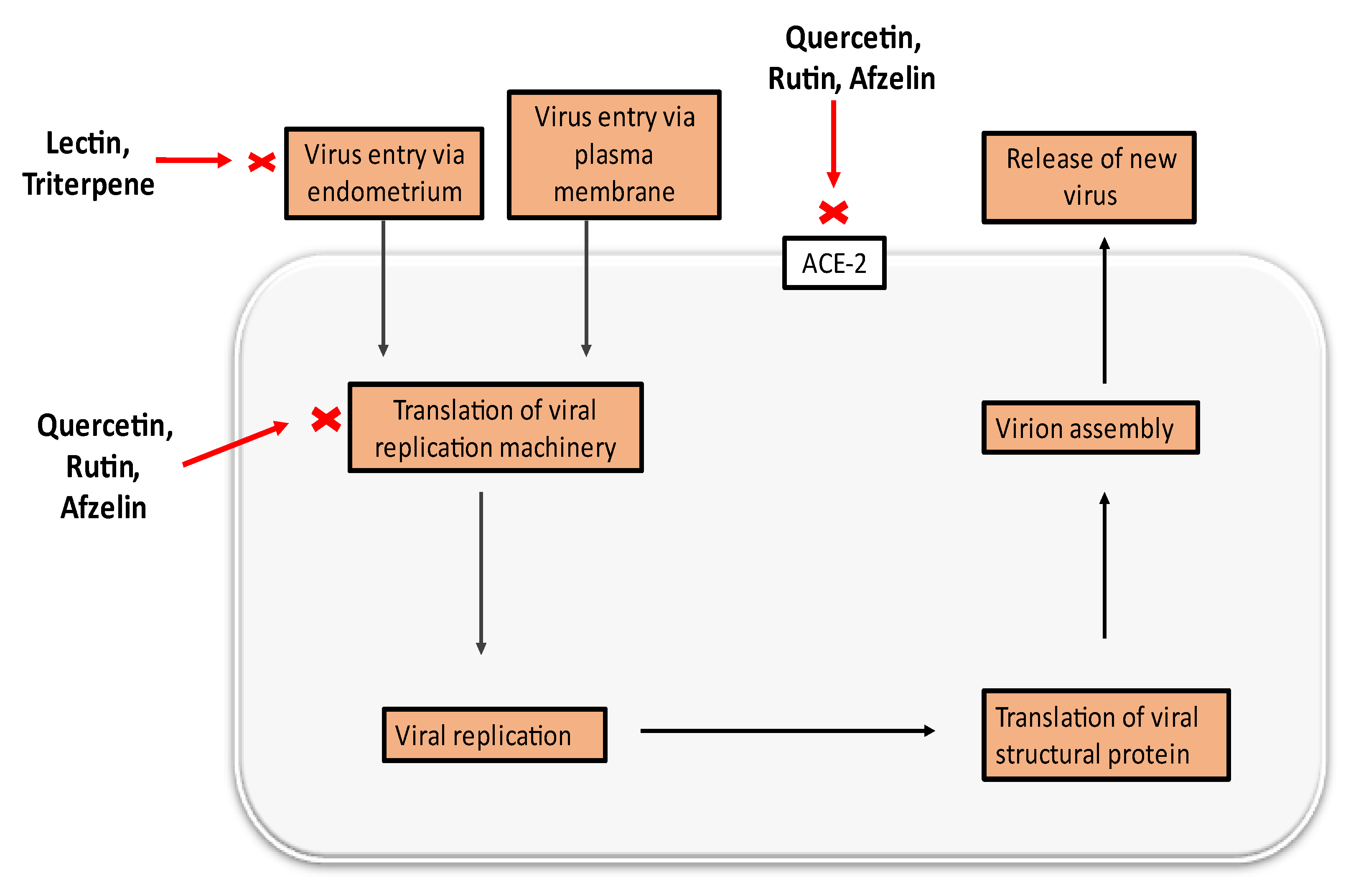
6.4. Antiviral Activities
6.5. Anti-SARS-CoV-2 Activity of E. neriifolia
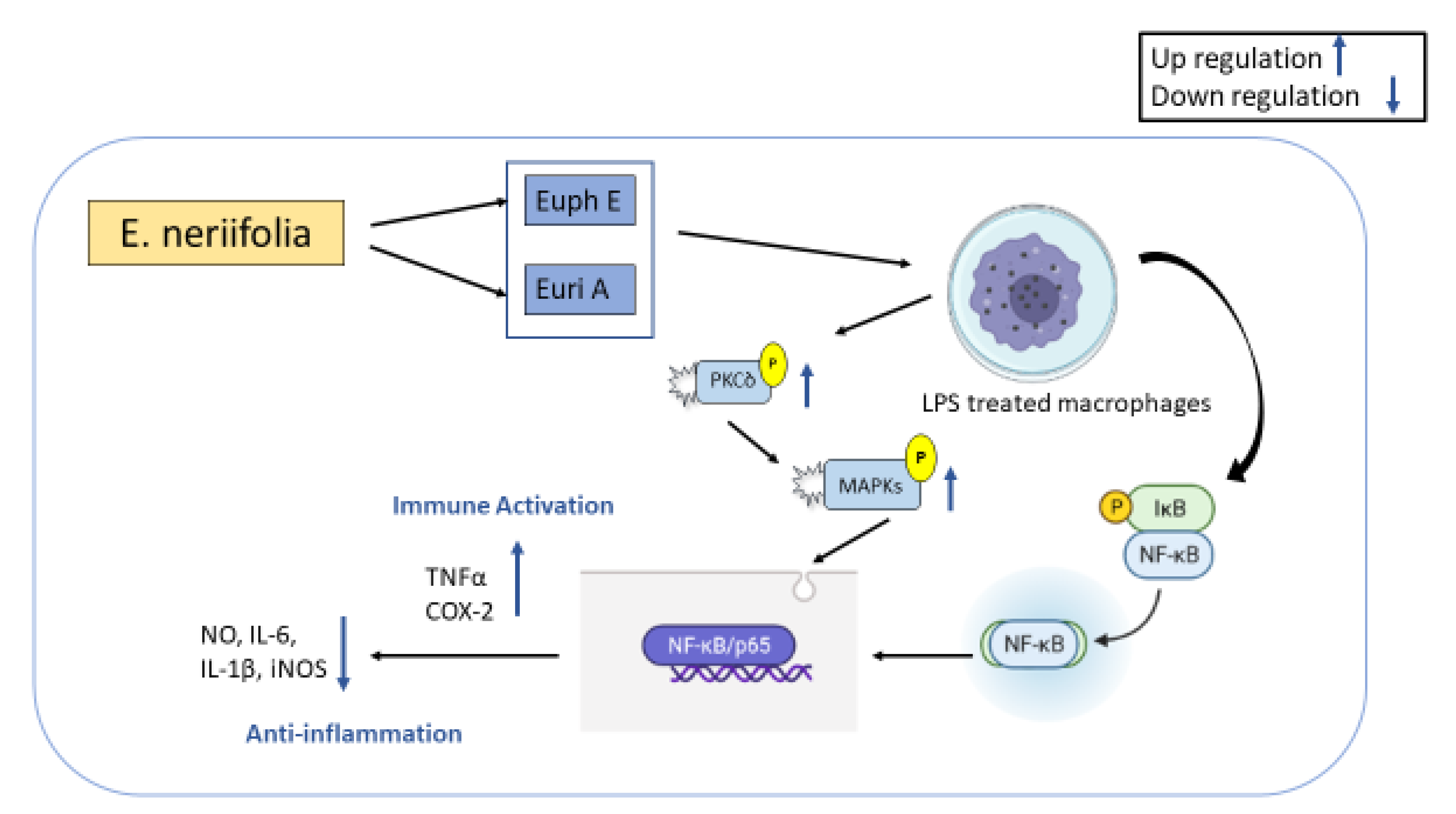
7. Immunomodulatory Activities of E. neriifolia
8. Toxicological Study
8.1. Traditional Evaluation
8.2. Pre-Clinical Studies
8.3. Clinical Studies
8.4. Treatment of the Toxicity
9. Discussion and Future Prospects
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Fauci, A.S.; Touchette, N.A.; Folkers, G.K. Emerging Infectious Diseases: A 10-Year Perspective from the National Institute of Allergy and Infectious Diseases. Int. J. Risk Saf. Med. 2005, 17, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.J.; Rahman, S. Repurposing therapeutic agents against SARS-CoV-2 infection: Most promising and neoteric progress. Expert Rev. Anti-Infect. Ther. 2021, 19, 1009–1027. [Google Scholar] [CrossRef] [PubMed]
- Sarker, M.T.; Hasan, A.Q.F.; Rafi, M.O.; Hossain, M.J.; El-Mageed, H.R.A.; Elsapagh, R.M.; Capasso, R.; Emran, T.B. A Comprehensive Overview of the Newly Emerged COVID-19 Pandemic: Features, Origin, Genomics, Epidemiology, Treatment, and Prevention. Biologics 2021, 1, 357–383. [Google Scholar] [CrossRef]
- Cunningham, A.A.; Daszak, P.; Wood, J.L.N. One Health, Emerging Infectious Diseases and Wildlife: Two Decades of Progress? Philos. Trans. R. Soc. B Biol. Sci. 2017, 372, 20160167. [Google Scholar] [CrossRef] [Green Version]
- de Rycker, M.; Horn, D.; Aldridge, B.; Amewu, R.K.; Barry, C.E., III; Buckner, F.S.; Cook, S.; Ferguson, M.A.J.; Gobeau, N.; Herrmann, J. Setting Our Sights on Infectious Diseases. ACS Infect. Dis. 2019, 6, 3–13. [Google Scholar] [CrossRef] [Green Version]
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The Challenge of Emerging and Re-Emerging Infectious Diseases. Nature 2004, 430, 242–249. [Google Scholar] [CrossRef]
- Yadav, S.; Rawal, G.; Baxi, M. An Overview of the Latest Infectious Diseases around the World. J. Community Health Manag. 2016, 3, 41–43. [Google Scholar]
- Marston, H.D.; Dixon, D.M.; Knisely, J.M.; Palmore, T.N.; Fauci, A.S. Antimicrobial Resistance. JAMA 2016, 316, 1193–1204. [Google Scholar] [CrossRef] [Green Version]
- Uddin, T.M.; Chakraborty, A.J.; Khusro, A.; Zidan, B.; Mitra, S.; Emran, T.B.; Dhama, K.; Ripon, M.; Gajdács, M.; Sahibzada, M.; et al. Antibiotic resistance in microbes: History, mechanisms, therapeutic strategies and future prospects. J. Infect. Public Health 2021, 14, 1750–1766. [Google Scholar] [CrossRef]
- Thomas, E.; Vandebroek, I.; Sanca, S.; van Damme, P. Cultural Significance of Medicinal Plant Families and Species among Quechua Farmers in Apillapampa, Bolivia. J. Ethnopharmacol. 2009, 122, 60–67. [Google Scholar] [CrossRef]
- Abidullah, S.; Rauf, A.; Khan, S.W.; Ayaz, A.; Liaquat, F.; Saqib, S. A Comprehensive Review on Distribution, Paharmacological Uses and Biological Activities of Argyrolobium Roseum (Cambess.) Jaub. & Spach. Acta Ecol. Sin. 2021, 42, 198–205. [Google Scholar]
- Das, R.; Mitra, S.; Tareq, A.M.; Emran, T.B.; Hossain, M.J.; Alqahtani, A.M.; Alghazwani, Y.; Dhama, K.; Simal-Gandara, J. Medicinal plants used against hepatic disorders in Bangladesh: A comprehensive review. J. Ethnopharmacol. 2022, 282, 114588. [Google Scholar] [CrossRef] [PubMed]
- Demain, A.L.; Fang, A. The Natural Functions of Secondary Metabolites. In History of Modern Biotechnology I; Springer: Berlin/Heidelberg, Germany, 2000; pp. 1–39. [Google Scholar]
- Wink, M. Modes of Action of Herbal Medicines and Plant Secondary Metabolites. Medicines 2015, 2, 251–286. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Wu, K.; Zhang, X.; Deng, S.; Peng, B. In Silico Screening of Chinese Herbal Medicines with the Potential to Directly Inhibit 2019 Novel Coronavirus. J. Integr. Med. 2020, 18, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Campisi, J.; Kapahi, P.; Lithgow, G.J.; Melov, S.; Newman, J.C.; Verdin, E. From Discoveries in Ageing Research to Therapeutics for Healthy Ageing. Nature 2019, 571, 183–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jannat, T.; Hossain, M.J.; El-Shehawi, A.M.; Kuddus, M.R.; Rashid, M.A.; Albogami, S.; Jafri, I.; El-Shazly, M.; Haque, M.R. Chemical and Pharmacological Profiling of Wrightia coccinea (roxb. Ex Hornem.) Sims Focusing Antioxidant, Cytotoxic, Antidiarrheal, Hypoglycemic, and Analgesic Properties. Molecules 2022, 27, 4024. [Google Scholar] [CrossRef]
- Baba, S.A.; Vahedi, M.; Ahmad, I.; Rajab, B.S.; Babalghith, A.O.; Irfan, S.; Hossain, M.J. Crocus sativus L. Tepal Extract Induces Apoptosis in Human U87 Glioblastoma Cells. BioMed Res. Int. 2022, 2022, 4740246. [Google Scholar] [CrossRef]
- Gaoue, O.G.; Yessoufou, K.; Mankga, L.; Vodouhe, F. Phylogeny Reveals Non-random Medicinal Plant Organ Selection by Local People in Benin. Plants People Planet 2021, 3, 710–720. [Google Scholar] [CrossRef]
- Zaman, W.; Ye, J.; Saqib, S.; Liu, Y.; Shan, Z.; Hao, D.; Chen, Z.; Xiao, P. Predicting Potential Medicinal Plants with Phylogenetic Topology: Inspiration from the Research of Traditional Chinese Medicine. J. Ethnopharmacol. 2021, 281, 114515. [Google Scholar] [CrossRef]
- Sánchez, T.; Salcedo, E.; Ceballos, H.; Dufour, D.; Mafla, G.; Morante, N.; Calle, F.; Pérez, J.C.; Debouck, D.; Jaramillo, G. Screening of Starch Quality Traits in Cassava (Manihot Esculenta Crantz). Starch-Stärke 2009, 61, 12–19. [Google Scholar] [CrossRef]
- Mwine, J.T.; van Damme, P. Why Do Euphorbiaceae Tick as Medicinal Plants? A Review of Euphorbiaceae Family and Its Medicinal Features. J. Med. Plants Res. 2011, 5, 652–662. [Google Scholar]
- Ramdas, W.P.; Madhav, P.S.; Sagar, N. Comprehensive study of sthavar visha snuhi ksheera (Euphorbia neriifolia Linn.) And its detoxification. Int. Res. J. Pharm. 2011, 2, 41–48. [Google Scholar]
- Ved, D.K.; Sureshchandra, S.T.; Barve, V.; Srinivas, V.; Sangeetha, S.; Ravikumar, K.; Kartikeyan, R.; Kulkarni, V.; Ajith, S. FRLHT’s ENVIS Centre on Medicinal Plants. FRLHT: Bengaluru, India, 2016. [Google Scholar]
- Bigoniya, P.; Rana, A. A Comprehensive Phyto-Pharmacological Review of Euphorbia neriifolia Linn. Pharmacogn. Rev. 2008, 2, 57. [Google Scholar]
- Kirtikar, K.R.; das Basu, B. Indian Medicinal Plants; Sudhindra Nath Basu, M.B. Panini Office, Bhuwanéswari Asrama: Bahadurganj, Allahabad, India, 1918. [Google Scholar]
- Oommachan, M. The Flora of Bhopal (Angiosperms); JK Jain Bros.: Bhopal, India, 1976; pp. 21–25. [Google Scholar]
- Shah, J.J.; Jani, P.M. Shoot Apex of Euphorbia neriifolia L. Proc. Natl. Inst. Sci. India 1964, 30, 81–91. [Google Scholar]
- Upadhyaya, C.; Sathish, S. A Review on Euphorbia neriifolia Plant. Int. J. Pharm. Chem. Res. 2017, 3, 149–154. [Google Scholar]
- Bigoniya, P. Euphorbia Latex: A Magic Potion or Poison. In Traditional and Folk Herbal Medicine: Recent Researches; Daya Publishing House: New Delhi, India, 2012; Volume 1. [Google Scholar]
- Sharma, V.; Janmeda, P.; Singh, L. A Review on Euphorbia neriifolia (Sehund). Spatulla DD 2011, 1, 107–111. [Google Scholar] [CrossRef]
- Sharma, V. Microscopic Studies and Preliminary Pharmacognostical Evaluation of Euphorbia neriifolia L. Leaves. Indian J. Nat. Prod. Resour. 2013, 4, 348–357. [Google Scholar]
- Ahmed, S.A.; Nazim, S.; Siraj, S.; Siddik, P.M.; Wahid, C.A. Euphorbia neriifolia Linn: A Phytopharmacological Review. Int. Res. J. Pharm. 2011, 2, 41–48. [Google Scholar]
- Shamim, S.A.; Fatima, L. Pharmacological Actions and Therapeutic Benefits of Thuhar (Euphorbia neriifolia): A Review. World J. Pharm. Res. 2018, 10, 1337–1349. [Google Scholar]
- Mali, P.Y.; Panchal, S.S. Euphorbia Neriifolia L.: Review on Botany, Ethnomedicinal Uses, Phytochemistry and Biological Activities. Asian Pac. J. Trop. Med. 2017, 10, 430–438. [Google Scholar] [CrossRef]
- Pracheta, S.V.; Paliwal, R.; Sharma, S. Preliminary Phytochemical Screening and in Vitro Antioxidant Potential of Hydro-Ethanolic Extract of Euphorbia Neriifolia Linn. Int. J. PharmTech Res. 2011, 3, 124–132. [Google Scholar]
- Hasan, M.; Ganeshpurkar, A.; Bansal, D.; Dubey, N. Protective Effect of Euphorbia neriifolia Extract on Experimentally Induced Thrombosis in Murine Model. Niger. J. Exp. Clin. Biosci. 2014, 2, 86. [Google Scholar]
- Yen, G.-C.; Chen, H.-Y. Antioxidant Activity of Various Tea Extracts in Relation to Their Antimutagenicity. J. Agric. Food Chem. 1995, 43, 27–32. [Google Scholar] [CrossRef]
- Khare, C.P. Indian Medicinal Plants: An Illustrated Dictionary; Springer Science & Business Media: New Delhi, India, 2008; Available online: https://books.google.com.bd/books?hl=en&lr=&id=gMwLwbUwtfkC&oi=fnd&pg=PA1&dq=Glossary+of+Indian+Medicinal+Plants.+&ots=_DCZB3B_QM&sig=3RVYftLogJIwdajjeXEJnqhJ9AM&redir_esc=y#v=onepage&q=Glossary%20of%20Indian%20Medicinal%20Plants.&f=false (accessed on 1 January 2022).
- Sharma, D.K. Bioprospecting for Drug Research and Functional Foods for the Prevention of Diseases—Role of Flavonoids in Drug Development; CSIR: New Delhi, India, 2006; Available online: http://nopr.niscpr.res.in/handle/123456789/4836 (accessed on 1 January 2022).
- Sharma, G.K.; Dhanawat, M. Effectual Qualitative Chemical Evaluation of Euphorbia Neriifolia Linn. by Using Fluorescence Analysis. J. Drug Deliv. Ther. 2019, 9, 44–47. [Google Scholar] [CrossRef]
- Radhakrishna, S. Multicentric Randomized Controlled Clinical Trial of Kshaarasootra (Ayurvedic Medicated Thread) in the Management of Fistula-in-Ano. Indian J. Med. Res. Sect. B Biomed. Res. Other Than Infect. Dis. 1991, 94, 177–185. [Google Scholar]
- Nadkarni, K.M. Indian Materia Medica; Bombay Popular Prakashan: Mumbai, India, 1954; 629p. [Google Scholar]
- Gaur, K.; Rana, A.C.; Nema, R.K.; Kori, M.L.; Sharma, C.S. Anti-Inflammatory and Analgesic Activity of Hydro-Alcoholic Leaves Extract of Euphorbia neriifolia Linn. Asian J. Pharm. Clin. Res. 2009, 2, 26–28. [Google Scholar]
- Mali, P.Y.; Panchal, S.S. Pharmacognostical and Physico-Chemical Standardization of Euphorbia neriifolia Leaves. Pharmacogn. J. 2017, 9, 695–705. [Google Scholar] [CrossRef] [Green Version]
- Oudhia, P. Medicinal Herbs of Chhattisgarh, India Having Less Known Uses of XXXIV. Brahmadandi. 2003. Available online: http://www.botanical.com/site/column_poudhia/250_brahmadandi.html (accessed on 1 January 2022).
- Mallavadhani, U.V.; Satyanarayana, K.V.S.; Mahapatra, A.; Sudhakar, A.V.S. A New Tetracyclic Triterpene from the Latex of Euphorbia Nerifolia. Nat. Prod. Res. 2004, 18, 33–37. [Google Scholar] [CrossRef]
- Bigoniya, P.; Rana, A.C. Immunomodulatory Activity of Euphorbia neriifolia Leaf Alcoholic Extract on Rats. Indian Drugs 2008, 45, 90. [Google Scholar]
- Burkill, I.H.; Haniff, M. Malay Village Medicine. In The Garden’s Bulletin Stairs Settlements; Part 2; Straits Times Press: Singapore, 1930; Volume VI, p. 212. [Google Scholar]
- Ravishankar, B.; Shukla, V.J. Indian Systems of Medicine: A Brief Profile. Afr. J. Tradit. Complement. Altern. Med. 2007, 4, 319–337. [Google Scholar] [CrossRef] [Green Version]
- Dash, V.B. Materia Medica of Ayurveda: Based on: Madanapala’s Nighantu; B. Jain Publishers: New Delhi, India, 2002. [Google Scholar]
- Takasaki, M.; Konoshima, T.; Tokuda, K.; Masuda, K.; Arai, Y.; Shiojima, K.; Ageta, H. Anti-Carcinogenic Activity of Taraxacum Plant. II. Biol. Pharm. Bull. 1999, 22, 606–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salazar, G.C.M.; Silva, G.D.F.; Duarte, L.P.; Vieira Filho, S.A.; Lula, I.S. Two Epimeric Friedelane Triterpenes Isolated from Maytenus Truncata Reiss: 1H and 13C Chemical Shift Assignments. Magn. Reson. Chem. 2000, 38, 977–980. [Google Scholar] [CrossRef]
- Anjeneyulu, A.S.R.; Row, L.R.; Subrahmanyam, C.; Murty, K.S. Crystalline Constituents from Euphorbiaceae—XIII: The Structure of a New Triterpene from Euphorbia nerifolia L. Tetrahedron 1973, 29, 3909–3914. [Google Scholar] [CrossRef]
- Hisham, A.; Ajitha Bai, M.D.; Fujimoto, Y.; Hara, N.; Shimada, H. Complete 1H and 13C NMR Spectral Assignment of Cabraleadiol, a Dammarane Triterpene from Dysoxylum Malabaricum Bedd. Magn. Reson. Chem. 1996, 34, 146–150. [Google Scholar] [CrossRef]
- Morikawa, T.; Oominami, H.; Matsuda, H.; Yoshikawa, M. Four New Ursane-Type Triterpenes, Olibanumols K, L, M, and N, from Traditional Egyptian Medicine Olibanum, the Gum-Resin of Boswellia Carterii. Chem. Pharm. Bull. 2010, 58, 1541–1544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seshagirirao, K.; Prasad, M.N. Purification and Partial Characterization of a Lectin from Euphorbia neriifolia Latex. Biochem. Mol. Biol. Int. 1995, 35, 1199–1204. [Google Scholar] [PubMed]
- Chatterjee, A.; Saha, S.K.; Mukhopadhyay, S. Lewis acid-catalyzed rearrangement of glut-5-en-3-beta-yl acetate and glut-5-en-3-beta-yl acetate. Indian J. Chem. Sect. B-Org. Chem. Med. Chem. 1978, 16, 1038–1039. [Google Scholar]
- Baslas, R.K.; Agarwal, R. Chemical investigation of some anti-cancer plants of euphorbia genus. Indian J. Chem. Sect. B-Org. Chem. Med. Chem. 1980, 19, 717–718. [Google Scholar]
- Ng, A.S. Diterpenes from Euphorbia neriifolia. Phytochemistry 1990, 29, 662–664. [Google Scholar] [CrossRef]
- Sharma, V.; Janmeda, P. Chromatography Fingerprinting Profile Studies on the Flavonoids of Euphorbia neriifolia (Linn.) Leaves. Int. J. Drug Dev. Res. 2013, 5, 286–296. [Google Scholar]
- Chen, L.; Li, J.; Luo, C.; Liu, H.; Xu, W.; Chen, G.; Liew, O.W.; Zhu, W.; Puah, C.M.; Shen, X. Binding Interaction of Quercetin-3-β-Galactoside and Its Synthetic Derivatives with SARS-CoV 3CLpro: Structure–Activity Relationship Studies Reveal Salient Pharmacophore Features. Bioorg. Med. Chem. 2006, 14, 8295–8306. [Google Scholar] [CrossRef] [PubMed]
- Batiha, G.E.-S.; Beshbishy, A.M.; Ikram, M.; Mulla, Z.S.; El-Hack, M.E.A.; Taha, A.E.; Algammal, A.M.; Elewa, Y.H.A. The Pharmacological Activity, Biochemical Properties, and Pharmacokinetics of the Major Natural Polyphenolic Flavonoid: Quercetin. Foods 2020, 9, 374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganeshpurkar, A.; Saluja, A.K. The Pharmacological Potential of Rutin. Saudi Pharm. J. 2017, 25, 149–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizzuti, B.; Grande, F.; Conforti, F.; Jimenez-Alesanco, A.; Ceballos-Laita, L.; Ortega-Alarcon, D.; Vega, S.; Reyburn, H.T.; Abian, O.; Velazquez-Campoy, A. Rutin Is a Low Micromolar Inhibitor of SARS-CoV-2 Main Protease 3CLpro: Implications for Drug Design of Quercetin Analogs. Biomedicines 2021, 9, 375. [Google Scholar] [CrossRef]
- Diniz, L.R.L.; Perez-Castillo, Y.; Elshabrawy, H.A.; de Sousa, D.P. Bioactive Terpenes and Their Derivatives as Potential SARS-CoV-2 Proteases Inhibitors from Molecular Modeling Studies. Biomolecules 2021, 11, 74. [Google Scholar] [CrossRef]
- Bohlmann, F.; Zdero, C. Nue Anol-Derivate Aus Ophryosporus Angustifolius. Phytochemistry 1979, 18, 145–147. [Google Scholar] [CrossRef]
- Akihisa, T.; Yamamoto, K.; Tamura, T.; Kimura, Y.; Iida, T.; Nambara, T.; Chang, F.C. Triterpenoid Ketones from Lingnania Chungii MoClure: Arborinone, Friedelin and Glutinone. Chem. Pharm. Bull. 1992, 40, 789–791. [Google Scholar] [CrossRef] [Green Version]
- Ahiahonu, P.W.K.; Goodenowe, D.B. Triterpenoids from Leaves of Elaeophorbia Drupifera. Fitoterapia 2007, 78, 337–341. [Google Scholar] [CrossRef]
- Hui, W.-H.; Li, M.-M. Neutral Triterpenoids from Melaleuca Leucadendron. Phytochemistry 1976, 15, 563. [Google Scholar] [CrossRef]
- Oliveira, R.C.; Bandeira, P.N.; Lemos, T.L.G.; dos Santos, H.S.; Scherf, J.R.; Rocha, J.E.; Pereira, R.L.S.; Freitas, T.S.; Freitas, P.R.; Pereira-Junior, F.N. In Silico and in Vitro Evaluation of Efflux Pumps Inhibition of α, β-Amyrin. J. Biomol. Struct. Dyn. 2021, 1–15. [Google Scholar] [CrossRef]
- Heupel, R.C. Varietal Similarities and Differences in the Polycyclic Isopentenoid Composition of Sorghum. Phytochemistry 1985, 24, 2929–2937. [Google Scholar] [CrossRef]
- Szakiel, A.; Pączkowski, C.; Koivuniemi, H.; Huttunen, S. Comparison of the Triterpenoid Content of Berries and Leaves of Lingonberry Vaccinium Vitis-Idaea from Finland and Poland. J. Agric. Food Chem. 2012, 60, 4994–5002. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, T.; Akihisa, T.; Tokuda, H.; Ukiya, M.; Watanabe, K.; Nishino, H. Cancer Chemopreventive Effects of Cycloartane-Type and Related Triterpenoids in in Vitro and in Vivo Models. J. Nat. Prod. 2007, 70, 918–922. [Google Scholar] [CrossRef] [PubMed]
- Connolly, J.D.; Hill, R.A. Triterpenoids. Nat. Prod. Rep. 2010, 27, 79–132. [Google Scholar] [CrossRef] [PubMed]
- Toume, K.; Nakazawa, T.; Hoque, T.; Ohtsuki, T.; Arai, M.A.; Koyano, T.; Kowithayakorn, T.; Ishibashi, M. Cycloartane Triterpenes and Ingol Diterpenes Isolated from Euphorbia neriifolia in a Screening Program for Death-Receptor Expression-Enhancing Activity. Planta Med. 2012, 78, 1370–1377. [Google Scholar] [CrossRef] [Green Version]
- Bah, C.S.F.; Fang, E.F.; Ng, T.B. Medicinal Applications of Plant Lectins. In Antitumor Potential and Other Emerging Medicinal Properties of Natural Compounds; Springer: Berlin/Heidelberg, Germany, 2013; pp. 55–74. [Google Scholar]
- Liu, Y.; Liu, J.; Pang, X.; Liu, T.; Ning, Z.; Cheng, G. The Roles of Direct Recognition by Animal Lectins in Antiviral Immunity and Viral Pathogenesis. Molecules 2015, 20, 2272–2295. [Google Scholar] [CrossRef] [Green Version]
- Keyaerts, E.; Vijgen, L.; Pannecouque, C.; van Damme, E.; Peumans, W.; Egberink, H.; Balzarini, J.; van Ranst, M. Plant Lectins Are Potent Inhibitors of Coronaviruses by Interfering with Two Targets in the Viral Replication Cycle. Antivir. Res. 2007, 75, 179–187. [Google Scholar] [CrossRef]
- Zhang, H.; Zhou, G.; Zhi, L.; Yang, H.; Zhai, Y.; Dong, X.; Zhang, X.; Gao, X.; Zhu, Y.; He, F. Association between Mannose-Binding Lectin Gene Polymorphisms and Susceptibility to Severe Acute Respiratory Syndrome Coronavirus Infection. J. Infect. Dis. 2005, 192, 1355–1361. [Google Scholar] [CrossRef] [Green Version]
- Baslas, R.K.; Agrawal, R. Chemical Examination of the Bark of Euphorbia neriifolia Linn. Indian J. Pharm. Sci. 1980, 42, 66–67. [Google Scholar]
- Camarda, L.; di Stefano, V.; Pitonzo, R. Natural Resins: Chemical Constituents and Medicinal Uses. In Resin Composites Properties, Production and Applications; Nova Science Pub Inc.: London, UK, 2011; Volume 1, pp. 353–374. [Google Scholar]
- Mokoka, T.A.; McGaw, L.J.; Mdee, L.K.; Bagla, V.P.; Iwalewa, E.O.; Eloff, J.N. Antimicrobial Activity and Cytotoxicity of Triterpenes Isolated from Leaves of Maytenus Undata (Celastraceae). BMC Complement. Altern. Med. 2013, 13, 111. [Google Scholar] [CrossRef] [Green Version]
- Mead, J.R.; McNair, N. Antiparasitic Activity of Flavonoids and Isoflavones against Cryptosporidium Parvum and Encephalitozoon Intestinalis. FEMS Microbiol. Lett. 2006, 259, 153–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Annan, K.; Adu, F.; Gbedema, S.Y. Friedelin: A Bacterial Resistance Modulator from Paulinia pinnata L. J. Sci. Technol. 2009, 29, 152–159. [Google Scholar] [CrossRef] [Green Version]
- di Petrillo, A.; Orrù, G.; Fais, A.; Fantini, M.C. Quercetin and Its Derivates as Antiviral Potentials: A Comprehensive Review. Phytother. Res. 2022, 36, 266–278. [Google Scholar] [CrossRef]
- Cachola, E.R. Phytochemical and Microbiological Analysis of “Karimbuaya”, Euphorbia neriifolia Linn. In Proceedings of the 29th Annual Convention of the Philippine Society for Microbiology, Laoag, Philippines, 10–11 May 2000. [Google Scholar]
- Desta, B. Ethiopian Traditional Herbal Drugs. Part II: Antimicrobial Activity of 63 Medicinal Plants. J. Ethnopharmacol. 1993, 39, 129–139. [Google Scholar] [CrossRef]
- Chanda, S.; Baravalia, Y. Novel Leads from Herbal Drugs for Infectious Skin Diseases. Curr. Res. Technol. Educ. Top. Appl. Microbiol. Microbial. Biotechnol. 2010, 1, 451–456. [Google Scholar]
- Raghuwanshi, M.G.; Patil, P.S.; Shaikh, A.A.; Nazim, S.; Majaz, Q. Evaluation of antimicrobial activity of dried juice of Euphorbia neriifolia. J. Sci. Inform. 2013, 7, 51–55. [Google Scholar]
- Mishra, A.; Parida, S. Phytochemical and antimicrobial significance of few species of Euphorbia. Bi-Ling. Int. Res. J. 2020, 10, 82–89. [Google Scholar]
- Sumathi, S.; Hamsa, D.; Dharani, B.; Sivaprabha, J.; Malathy, N.; Radha, P.; Padma, P.R. Isolation and Characterization of Chitin from Prawn Shell Waste and Incorporation into Medical Textiles. Int. J. Recent Sci. Res. 2012, 3, 676–680. [Google Scholar]
- Samaresh, D.; NS, S.; DS, C. Exploration of Antimicrobial Potential of Methanol Extract of Stems of Euphorbia neriifolia. Int. Res. J. Pharm. 2013, 4, 271–273. [Google Scholar]
- Pokharen, N.; Dahal, S.; Anuradha, M. Phytochemical and Antimicrobial Studies of Leaf Extract of Euphorbia neriifolia. J. Med. Plants Res. 2011, 5, 5785–5788. [Google Scholar]
- Chaudhary, P.; Janmeda, P. Quantification of phytochemicals and in vitro antioxidant activities from various parts of Euphorbia neriifolia Linn. J. Appl. Biol. Biotechnol. 2022, 10, 133–145. [Google Scholar]
- Cowan, M.M. Plant Products as Antimicrobial Agents. Clin. Microbiol. Rev. 1999, 12, 564–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Draughon, F. Use of Botanicals as Biopreservatives in Foods. Food Technol. 2004, 58, 20–28. [Google Scholar]
- Tripathi, K.D. Essentials of Medical Pharmacology, 5th ed.; Jaypee Brothers Medical Publishers (P) Ltd.: New Delhi, India, 2003; pp. 145–155. [Google Scholar]
- Prichard, R.K. Anthelmintic Resistance in Nematodes: Extent, Recent Understanding and Future Directions for Control and Research. Int. J. Parasitol. 1990, 20, 515–523. [Google Scholar] [CrossRef]
- Hertzberg, H.; Bauer, C. Anthelminthika-Resistenzen Bei Magen-Darm-Strongyliden von Schafen Und Ziegen: Aktuelles Über Verbreitung, Epidemiologie, Vorbeugemassnahmen Und Alternativen Zum Anthelminthika-Einsatz. Berl. Münch. Tierärztl. Wschr. 2000, 113, 122–128. [Google Scholar]
- Swargiary, A.; Daimari, M.; Roy, M.K. Putative Anthelmintic Plants Used in Traditional Medicine System of Kokrajhar District, India. Ethnobot. Res. Appl. 2021, 22, 1–18. [Google Scholar] [CrossRef]
- Thiberville, S.-D.; Moyen, N.; Dupuis-Maguiraga, L.; Nougairede, A.; Gould, E.A.; Roques, P.; de Lamballerie, X. Chikungunya Fever: Epidemiology, Clinical Syndrome, Pathogenesis and Therapy. Antivir. Res. 2013, 99, 345–370. [Google Scholar] [CrossRef]
- Morrison, T.E. Reemergence of Chikungunya Virus. J. Virol. 2014, 88, 11644–11647. [Google Scholar] [CrossRef] [Green Version]
- Powers, A.M. Chikungunya Virus Outbreak Expansion and Microevolutionary Events Affecting Epidemiology and Epidemic Potential. Res. Rep. Trop. Med. 2015, 6, 11–19. [Google Scholar] [CrossRef] [Green Version]
- Nothias-Scaglia, L.-F.; Dumontet, V.; Neyts, J.; Roussi, F.; Costa, J.; Leyssen, P.; Litaudon, M.; Paolini, J. LC-MS2-Based Dereplication of Euphorbia Extracts with Anti-Chikungunya Virus Activity. Fitoterapia 2015, 105, 202–209. [Google Scholar] [CrossRef]
- Chang, F.-R.; Yen, C.-T.; Ei-Shazly, M.; Lin, W.-H.; Yen, M.-H.; Lin, K.-H.; Wu, Y.-C. Anti-Human Coronavirus (Anti-HCoV) Triterpenoids from the Leaves of Euphorbia neriifolia. Nat. Prod. Commun. 2012, 7, 1415–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.-X.; Liu, C.-P.; Qi, W.-Y.; Han, M.-L.; Han, Y.-S.; Wainberg, M.A.; Yue, J.-M. Eurifoloids A–R, Structurally Diverse Diterpenoids from Euphorbia neriifolia. J. Nat. Prod. 2014, 77, 2224–2233. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M. Phytochemical Virucidal Potential of Therapeutic Plants Indigenous to Rajasthan: A Review. Asian J. Adv. Med. Sci. 2021, 3, 22–34. [Google Scholar]
- Liu, Q.; Li, W.; Huang, L.; Asada, Y.; Morris-Natschke, S.L.; Chen, C.-H.; Lee, K.-H.; Koike, K. Identification, Structural Modification, and Dichotomous Effects on Human Immunodeficiency Virus Type 1 (HIV-1) Replication of Ingenane Esters from Euphorbia Kansui. Eur. J. Med. Chem. 2018, 156, 618–627. [Google Scholar] [CrossRef]
- Dang, Z.; Zhu, L.; Lai, W.; Bogerd, H.; Lee, K.-H.; Huang, L.; Chen, C.-H. Aloperine and Its Derivatives as a New Class of HIV-1 Entry Inhibitors. ACS Med. Chem. Lett. 2016, 7, 240–244. [Google Scholar] [CrossRef]
- Chinsembu, K.C. Coronaviruses and Nature’s Pharmacy for the Relief of Coronavirus Disease 2019. Rev. Bras. Farmacogn. 2020, 30, 603–621. [Google Scholar] [CrossRef]
- Ngwa, W.; Kumar, R.; Thompson, D.; Lyerly, W.; Moore, R.; Reid, T.-E.; Lowe, H.; Toyang, N. Potential of Flavonoid-Inspired Phytomedicines against COVID-19. Molecules 2020, 25, 2707. [Google Scholar] [CrossRef]
- Siddiqui, A.J.; Danciu, C.; Ashraf, S.A.; Moin, A.; Singh, R.; Alreshidi, M.; Patel, M.; Jahan, S.; Kumar, S.; Alkhinjar, M.I.M. Plants-Derived Biomolecules as Potent Antiviral Phytomedicines: New Insights on Ethnobotanical Evidences against Coronaviruses. Plants 2020, 9, 1244. [Google Scholar] [CrossRef]
- Khaerunnisa, S.; Kurniawan, H.; Awaluddin, R.; Suhartati, S.; Soetjipto, S. Potential Inhibitor of COVID-19 Main Protease (Mpro) from Several Medicinal Plant Compounds by Molecular Docking Study. Preprints 2020, 2020, 2020030226. [Google Scholar]
- Sumaryada, T.; Pramudita, C.A. Molecular Docking Evaluation of Some Indonesian’s Popular Herbals for a Possible COVID-19 Treatment. Biointerface Res. Appl. Chem. 2020, 11, 9827–9835. [Google Scholar]
- Srivastava, A.K.; Kumar, A.; Misra, N. On the Inhibition of COVID-19 Protease by Indian Herbal Plants: An in Silico Investigation. arXiv 2020, arXiv:2004.03411. [Google Scholar]
- Tazikeh-Lemeski, E.; Moradi, S.; Raoufi, R.; Shahlaei, M.; Janlou, M.A.M.; Zolghadri, S. Targeting SARS-CoV-2 Non-Structural Protein 16: A Virtual Drug Repurposing Study. J. Biomol. Struct. Dyn. 2020, 39, 4633–4646. [Google Scholar] [CrossRef]
- Sakib, R.; Prottay, A.A.S.; Rahman, N.; Rabbani, G.; Akter, K. In-Silico Molecular Docking Study of Afzelin and Its Derivatives Against 6m0j for Treatment Of COVID-19. Int. J. Evergr. Sci. Res. 2019, 3, 62–77. [Google Scholar]
- Chen, X.; Lu, J.; Zhang, Y.; He, J.; Guo, X.; Tian, G.; Jin, L. Studies of Macrophage Immuno-Modulating Activity of Polysaccharides Isolated from Paecilomyces Tenuipes. Int. J. Biol. Macromol. 2008, 43, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.D.; Ochsenbauer-Jambor, C.; Smythies, L.E. Intestinal Macrophages: Unique Effector Cells of the Innate Immune System. Immunol. Rev. 2005, 206, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Xue, Y.; Li, J.; Rao, K.; Yan, S.; Li, H.; Chen, X.; Li, R.; Liu, D. PKCδ/MAPKs and NF-ΚB Pathways Are Involved in the Regulation of Ingenane-Type Diterpenoids from Euphorbia neriifolia on Macrophage Function. J. Inflamm. Res. 2021, 14, 2681. [Google Scholar] [CrossRef]
- Gaur, K.; Rana, A.C.; Chauhan, L.S.; Sharma, C.S.; Nema, R.K.; Kori, M.L. Investigation of Immunomodulatory Potential of Euphorbia neriifolia Linn. Against Betamethasone Induced Immunosuppression. Int. J. Pharm. Phytochem. Res 2009, 2, 8–11. [Google Scholar]
- Basak, S.K.; Bakshi, P.K.; Basu, S.; Basak, S. Keratouveitis Caused by Euphorbia Plant Sap. Indian J. Ophthalmol. 2009, 57, 311. [Google Scholar] [CrossRef]
- Krishna, M.C.; Gupta, V.; Bansal, P.; Kumar, S.; Sannd, R.; Narayana, A. Review on Plants Mainly Used for the Preparation of Kshar Sutra. Int. J. Ayurvedic Med. 2010, 1, 12–22. [Google Scholar]
- Bigoniya, P.; Rana, A.C. Protective Effect of Euphorbia neriifolia Saponin Fraction on CCl4-Induced Acute Hepatotoxicity. Afr. J. Biotechnol. 2010, 9, 7148–7156. [Google Scholar]
- Mansuri, M.I.; Patel, V.M. Anti-Diabetic Potential of Euphorbia neriifolia Linn. Alloxan Induced Diabetic Rats. J. Pharm. Res. 2012, 5, 2571–2573. [Google Scholar]
- Naik, B.S. Common Milk Hedge (Euphorbia neriifolia) Juice Ingestion: A Clinical Case Report; IMSEAR: Goodyear, AZ, USA, 2009; pp. 30–31. [Google Scholar]
- Mitra, S.; Lami, M.S.; Uddin, T.M.; Das, R.; Islam, F.; Anjum, J.; Hossain, M.J.; Emran, T.B. Prospective multifunctional roles and pharmacological potential of dietary flavonoid narirutin. Biomed. Pharmacother. 2022, 150, 112932. [Google Scholar] [CrossRef] [PubMed]
- Noor-E-Tabassum; Das, R.; Lami, M.S.; Chakraborty, A.J.; Mitra, S.; Tallei, T.E.; Idroes, R.; Mohamed, A.A.; Hossain, M.J.; Dhama, K.; et al. Ginkgo biloba: A Treasure of Functional Phytochemicals with Multimedicinal Applications. Evid.-Based Complement. Altern. Med. ECAM 2022, 2022, 8288818. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.J.; Uddin, T.M.; Matin Zidan, B.; Mitra, S.; Das, R.; Nainu, F.; Dhama, K.; Roy, A.; Hossain, M.J.; Khusro, A.; et al. Allium cepa: A Treasure of Bioactive Phytochemicals with Prospective Health Benefits. Evid.-Based Complement. Altern. Med. ECAM 2022, 2022, 4586318. [Google Scholar] [CrossRef]
- Guo, J.; Huang, Z.; Sun, J.; Cui, X.; Liu, Y. Research Progress and Future Development Trends in Medicinal Plant Transcriptomics. Front. Plant Sci. 2021, 12, 691838. [Google Scholar] [CrossRef]

| Disease | Traditional Background | Reference |
|---|---|---|
| Whole plant | ||
| Respiratory stimulant, arthritis, local anesthetic, paronychia, antibacterial, antiviral, and interferolick | Unani medicine | [31] |
| Exerts “Katu” and “Tikta” action | Caraka Samhita | [50] |
| Exerts “Virya” properties with “Usna” action | Susruta Samhita | [50] |
| Gives “Guna”, “Vipaka”, and “Karma” properties | Vagbhata Geeta | [50] |
| Deep cracks in feet soles | Used with castor oil by locals of Chhattisgarh | [46] |
| Insecticide | Used as a spray by local farmers in India | [46] |
| As a fence full of spines | Used by local farmers in India | [46] |
| Allelopathic effect in weed control | Used by local farmers in India | [46] |
| Latex | ||
| Used in aphrodisiac mixture | Chhattisgarh region of India | [33] |
| Earache | Malay | [33] |
| Obstinate skin disease, urinary disorders, and diabetes | Shusruta | [33] |
| Coughs, skin problems | Used in Rajputana | [31] |
| Piles | Used with turmeric in Indian medicine | [26] |
| Ophthalmic use | Indian Medicine | [26] |
| Cathartic, earache | Used by Indian Vaidya | [43] |
| Whooping cough, leprosy, dyspepsia, jaundice, dropsy, colic, enlarged liver, and spleen | Used with salt by Indian Vaidya | [43] |
| Removes warts | Used by Indian Vaidya | [43] |
| External application for rheumatic limbs | Used with margosa oil or neem oil by Indian Vaidya | [43] |
| Prevents the attack of red weevils in palms | Gujarat | [43] |
| Anal fistulae | Indian medicine | [51] |
| Asthma | Ayurveda | [43] |
| Syphilis, visceral obstruction, spleen, and liver enlargement | Used with ghee in Rural area in India | [43] |
| Leaves | ||
| Ear problems | Sarawak | [33] |
| Wound healing, CNS problems, and immunomodulatory effects | Used in Malaya | [49] |
| Bronchitis, bleeding piles | Indian traditional medicine | [39] |
| Earache | Used in Malaya and Philippines | [40] |
| Wound-healing | The steamed leaves used in Indian medicine | [35] |
| Respiratory trouble in children | Used with common salt an honey in localised areas in India | [46] |
| Stem | ||
| Deroots skin warts | Indian traditional medicine | [42] |
| Coughs and colds | Used with honey in Indian traditional medicine | [42] |
| Chronic respiratory problems | Used with black pepper locally in India | [46] |
| Promotes the expectoration of phlegm | Used with honey and borax by Indian Vaidya | [43] |
| Hydrophobia | Used with fresh ginger by Indian Vaidya | [43] |
| Roots | ||
| Antispasmodic activity | Used in Indian medicine | [43] |
| Snake bites, scorpion stings | Used with black pepper in Indian medicine | [26] |
| Dropsy | Used after boiling with rice water by Indian Vaidya | [43] |
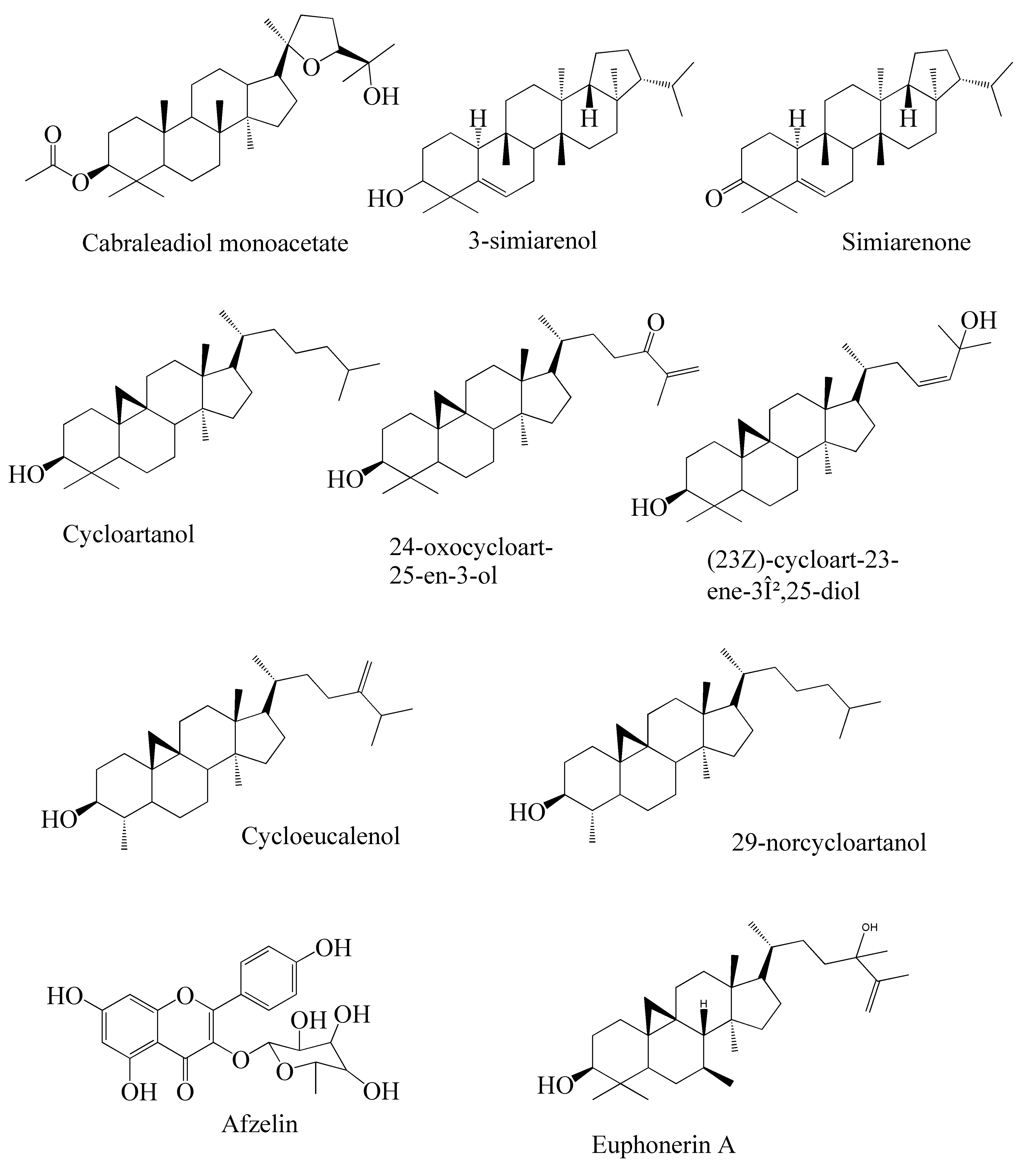
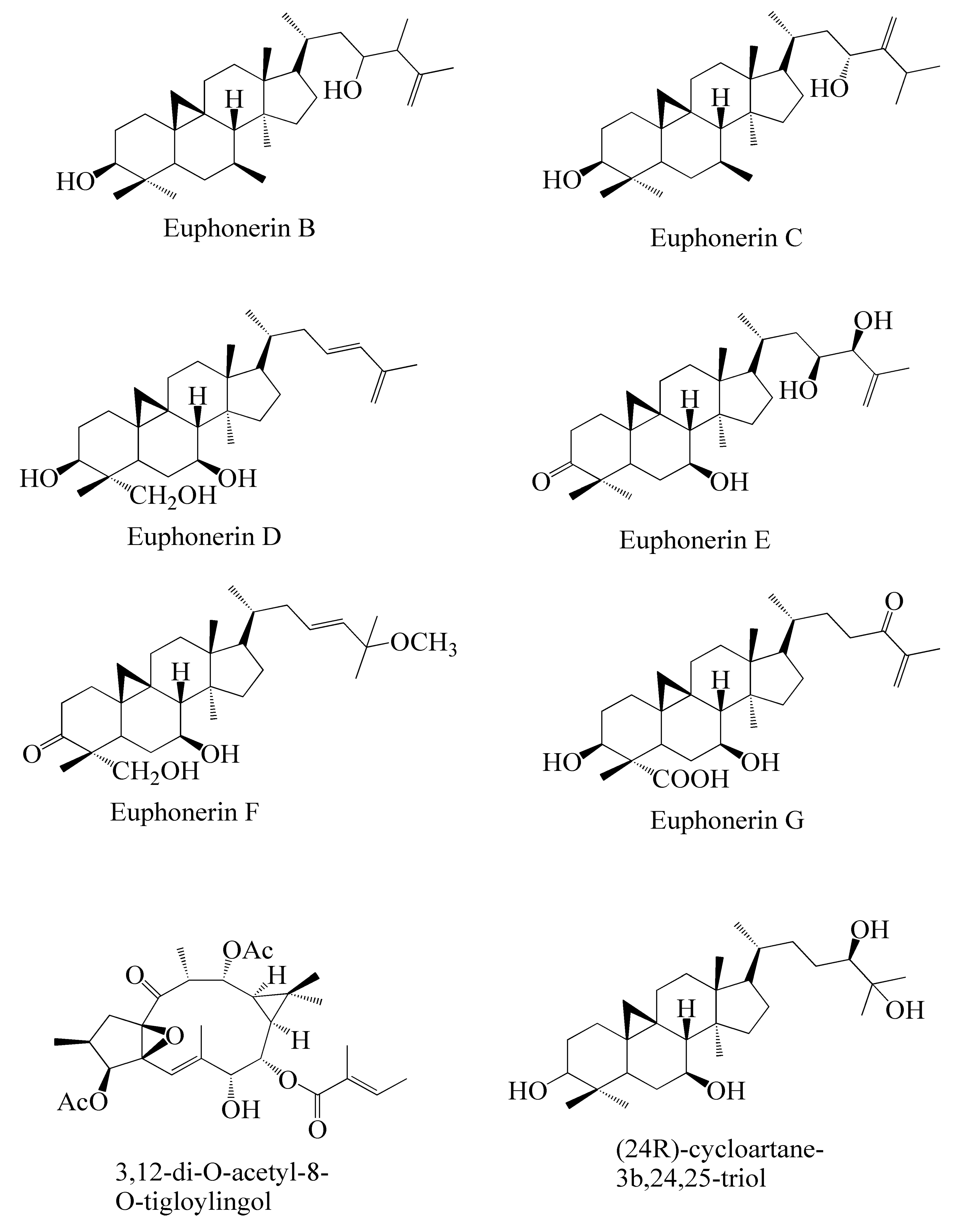
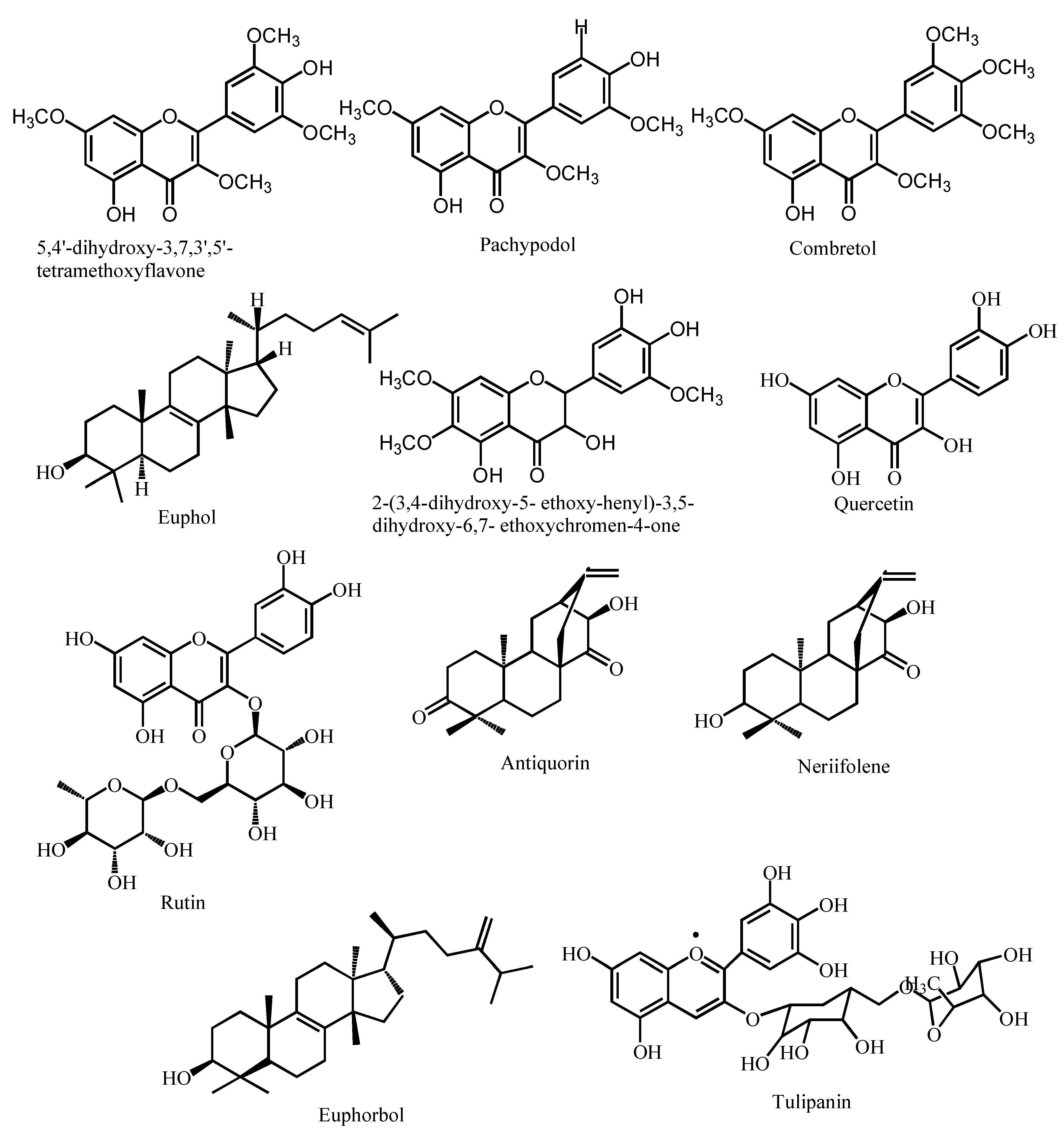
| Name of the Compound | Structure | Plant Part | Pharmacological Activities | References | |||
|---|---|---|---|---|---|---|---|
| Antibacterial Activity | Antifungal Activity | Antiviral Activity | Antiparasitic Activity | ||||
| Quercetin | 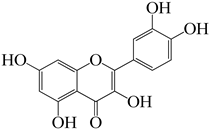 | Leaves | Potent bacteriostatic activity against P. aeruginosa, P. fluorescens, H. pylori, S. epidermidis, S. aureus, Y. enterocolitica, M. luteus, C. jejuni, and E. coli. | - Inhibits C. albicans - Acted as adjuvant for amphotericin B against C. neoformans at 0.25–0.125 μg/mL | - Inhibitory percentage is 82% at a 200 µM concentration - Binds with SARS-CoV 3CLpro protease - Active against human T-Lymphotropic virus 1, Japanese Encephalitis virus (JEV), dengue virus type-2, and hepatitis C virus. | Exerts potential antiparasitic activities against Toxoplasma, Babesia, Theileria, Trypanosoma, and Leishmania. | [61,62,63] |
| Rutin |  | Leaves | Active against E. coli, P. vulgaris, S. sonnei, P. auruginosa, B. subtilis and Klebsiella sp. | - Inhibits C. gattii with a MIC value of 60 µg/mL. - Acted as adjuvant for amphotericin B against C. neoformans at 0.0625 μg/mL | - Useful for treating retroviruses, herpes viruses, orthomyxoviruses, hepatitis B, and hepatitis C - Effective against avian influenza, strain H5N1 | Demonstrates antimycobacterialactivity against Mycobacterium smegmatis | [61,64,65] |
| 3β-friedelanol | 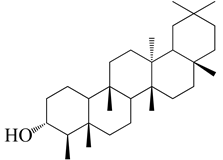 | Leaves | Not found | Not found | - Greater anti-HCoV activity than positive control actinomycin D with 132.4% survival rate - Inhibts hepatitis B virus (HBV) by inhibiting HBeAg secretion | Not found | [48,66] |
| 3β-acetoxy friedelane | 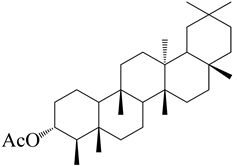 | Leaves | Not found | Not found | Anti-HCoV activity with 80.9% survival rate | Not found | [67] |
| Friedelin | 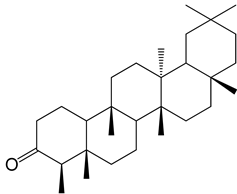 | Leaves | Active against S. faecalis, S. aureus, B. cereus, B. megaterium, B. stearothermophilus, B. subtilis | Active against C. albicans (MIC = 2.44 μg/mL) | Anti-HCoV activity with 80.9% survival rate | Not found | [66,68] |
| Lupenone | 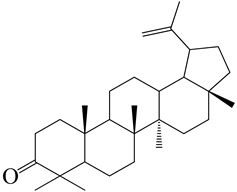 | Leaves | Not found | Not found | Against herpes simplex virus | Not found | [69] |
| Epitaraxerol | 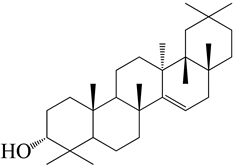 | Leaves | Inhibits A. niger, S. aureus, E. coli, P. aeruginosa, B. subtilis, T. mentagrophytes. | Inhibits C. albicans | Anti-HCoV activity with 111.0% survival rate | Not found | [69] |
| Epitaraxeryl acetate | 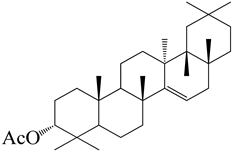 | Leaves | Not found | Not found | Antivirus activity against Epistein–Barr virus. | Not found | [70] |
| Taraxeryl acetate | 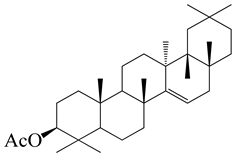 | Leaves | MIC for E. coli is 78 µg/mL, B. cereus 156 µg/mL, S. faecalis 78µg/mL | MIC for C. albicans is 156 µg/mL, M. audouinii 78 µg/mL | Not found | Not found | [52] |
| β-amyrin | 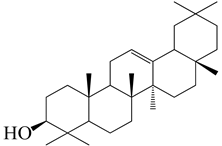 | Leaves | Contribute in the antibacterial activity of E. neriifolia plant | Inhibits the growth of Candida spp. | Inhibits Peste des Petits Ruminants virus. Exerts virucidal potential | Not found | [52,71] |
| 3β-simiarenol | 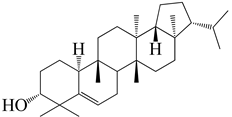 | Leaves | Not found | Not found | Anti-HCoV activity | Not found | [72] |
| Cycloartenol | 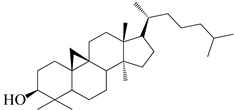 | Leaves, Roots, and Latex | Not found | Not found | Inhibits the migration of glioma cells and inhibits the phosphorylation of p38 MAP kinase. | Not found | [73] |
| Cycloeucalenol | 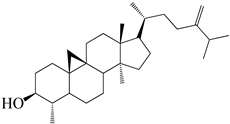 | Leaves | Inhibits P. aeruginosa (ZOI 24 mm) | Not found | Not found | Not found | [74] |
| Afzelin | 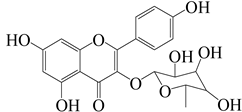 | Leaves | Not found | Not found | Binds with the SARS-CoV 3CLpro protease and inhibits viral replication | Not found | [75] |
| Euphonerin A | 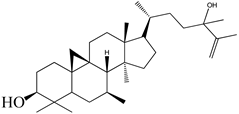 | Leaves | Not found | Not found | Anti-HIV | Not found | [76] |
| Euphonerin B | 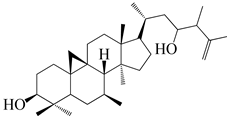 | Leaves | Not found | Not found | Anti-HIV | Not found | [76] |
| Euphonerin C | 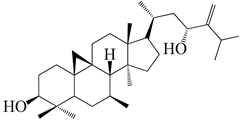 | Leaves | Not found | Not found | Anti-HIV | Not found | [76] |
| Euphonerin D |  | Leaves | Not found | Not found | Anti-HIV activity with EC50 of 34 µM | Not found | [76] |
| Lectin | Latex | Active against E. coli, S. dysenteriae, S. aureus, P. aeruginosa, B. subtilis, and Klebsiella sp. | Active against A. flavus, T. viride, F. oxysporum, F. moniliforme, C. comatus, R. olani, P. digitatum, A. alternata, and V. mali. | - Anti-HIV activity - exerts Anti-SARS-CoV-2 activity by attaching with viral spike protein | Not found | [57,77,78,79,80] | |
| Pachypodol (5,40-dihydroxy-3,7,30-trimethoxyflavone) | 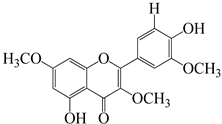 | Leaves | Active against B. subtilis, S. aureus, S. faecalis, E. coli, P. aeruginosa | Good activity against C. albicans, C. krusei, and C. galabrata | Not found | Not found | [76] |
| Taraxerol |  | Leaves and Stem | Exerted inhibition on E. coli in vitro with MIC value of 1.20 mg/mL | Not found | Antivirus activity against Epistein–Barr virus. | Not found | [76,77] |
| 24-Methylenecycloarenol |  | Root and Bark | Not found | Not found | Interacts with binding site residues that are known to interfere with the activity of ACE2 in SARS-CoV-2 | Not found | [25] |
| Ingenol triacetate | 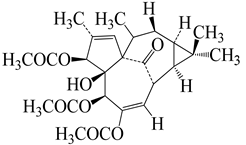 | Root | Not found | Not found | Prevent HIV replication in MT-4 cells at 0.051–0.65 µM | Not found | [25] |
| 12-Deoxyphorbol-13,20-diacetate | 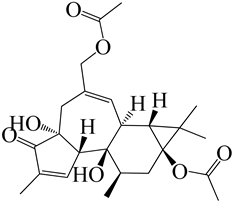 | Root | Not found | Not found | Causes HIV-1 expression in latently infected T-cell and increases sensitivity to killing through immunotoxins. | Not found | [25] |
| Tulipanin | 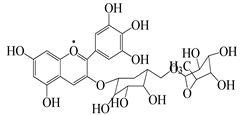 | Bark and Root | Active against S. aureus, P. aeruginosa, E. coli, and B. subtilis | Not found | Not found | Not found | [25] |
| n-hexacosanol | CH3(CH2)24CH2OH | Bark | Hexacosanol compounds exerted significant activities against M. smegmatis, S. faecium, L. monocytogenes, C. albicans, D. kl oackeri, and R. rubra | [81] | |||
| Wax, Resin, Caoutchouc, Gum | Bark and Latex | Wax, resin, gum, and caoutchouc from different origins exert various pharmacological activities, including antibacterial, antifungal, antiviral, and antiparasitic activities | [65,82] | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sultana, A.; Hossain, M.J.; Kuddus, M.R.; Rashid, M.A.; Zahan, M.S.; Mitra, S.; Roy, A.; Alam, S.; Sarker, M.M.R.; Naina Mohamed, I. Ethnobotanical Uses, Phytochemistry, Toxicology, and Pharmacological Properties of Euphorbia neriifolia Linn. against Infectious Diseases: A Comprehensive Review. Molecules 2022, 27, 4374. https://doi.org/10.3390/molecules27144374
Sultana A, Hossain MJ, Kuddus MR, Rashid MA, Zahan MS, Mitra S, Roy A, Alam S, Sarker MMR, Naina Mohamed I. Ethnobotanical Uses, Phytochemistry, Toxicology, and Pharmacological Properties of Euphorbia neriifolia Linn. against Infectious Diseases: A Comprehensive Review. Molecules. 2022; 27(14):4374. https://doi.org/10.3390/molecules27144374
Chicago/Turabian StyleSultana, Arifa, Md. Jamal Hossain, Md. Ruhul Kuddus, Mohammad A. Rashid, Miss Sharmin Zahan, Saikat Mitra, Arpita Roy, Safaet Alam, Md. Moklesur Rahman Sarker, and Isa Naina Mohamed. 2022. "Ethnobotanical Uses, Phytochemistry, Toxicology, and Pharmacological Properties of Euphorbia neriifolia Linn. against Infectious Diseases: A Comprehensive Review" Molecules 27, no. 14: 4374. https://doi.org/10.3390/molecules27144374
APA StyleSultana, A., Hossain, M. J., Kuddus, M. R., Rashid, M. A., Zahan, M. S., Mitra, S., Roy, A., Alam, S., Sarker, M. M. R., & Naina Mohamed, I. (2022). Ethnobotanical Uses, Phytochemistry, Toxicology, and Pharmacological Properties of Euphorbia neriifolia Linn. against Infectious Diseases: A Comprehensive Review. Molecules, 27(14), 4374. https://doi.org/10.3390/molecules27144374









