Abstract
Fungi can synthesize a wealth of secondary metabolites, which are widely used in the exploration of lead compounds of pharmaceutical or agricultural importance. Beauveria, Metarhizium, and Cordyceps are the most extensively studied fungi in which a large number of biologically active metabolites have been identified. However, relatively little attention has been paid to Purpureocillium lilacinum. P. lilacinum are soil-habituated fungi that are widely distributed in nature and are very important biocontrol fungi in agriculture, providing good biological control of plant parasitic nematodes and having a significant effect on Aphidoidea, Tetranychus cinnbarinus, and Aleyrodidae. At the same time, it produces secondary metabolites with various biological activities such as anticancer, antimicrobial, and insecticidal. This review attempts to provide a comprehensive overview of the secondary metabolites of P. lilacinum, with emphasis on the chemical diversity and biological activity of these secondary metabolites and the biosynthetic pathways, and gives new insight into the secondary metabolites of medical and entomogenous fungi, which is expected to provide a reference for the development of medicine and agrochemicals in the future.
1. Introduction
The genus Purpureocillium in the Ophiocordycipitaceae family was structured by Luangsa-Ard et al. In 2011, based on the medical importance, the Purpureocillium lilacinum was designated as the type species of the Paecilomyces genus [1]. This species was nominated as Penicillium lilacinum by Thom in 1901, and then it was revised as Paecilomyces lilacinus by Samson in 1974 [2]. After comparing the 18S rRNA gene, internal transcribed spacer, and partial translation elongation factor 1-a sequences with P. lilacinus, Luangsa-Ard proposed a new genus name Purpureocillium and made the new combination P. lilacinum in 2011. The fungus was found in a wide range of land and marine environments [3,4,5]. They are often isolated from insects, nematodes, and the rhizosphere of many crops [6,7,8]. The species can grow in a wide range of temperatures from 8 to 38 °C with optimal temperatures of 26–30 °C [3]. It also has a wide pH tolerance and can grow on a variety of substrates [9]. This fungus has promising potential as a biocontrol agent to control crops‘ root-knot nematodes [10,11]. The parasitism of nematodes is that the hyphae directly invade the surface of nematodes’ eggs and then produce appressoria on the surface, which infects the nematodes’ eggs after adsorption. In the process of infection, P. lilacinum secretes a variety of enzymes, such as serine protease and chitinase, which can lead to the degradation of protein and chitin components of the nematode epidermis, which is conducive to the invasion of fungi and destruction of cell components. It has been shown that the fermentation filtrate of P. lilacinum can inhibit the mycelial growth of the pathogenic fungi Helminthosporium maydis and Fusarium graminearum, and has a significant inhibitory effect on the spore germination of Fusarium oxysporum [12,13]. Currently, there are eight registered pesticide products of P. lilacinum in China used to control root-knot nematodes (http://www.chinapesticide.org.cn/hysj/index.jhtml, accessed on 23 February 2021); similar pesticides are also registered in the USA (https://iaspub.epa.gov/apex/pesticides, accessed on 23 February 2021) and European Union (http://www.efsa.europa.eu/, accessed on 23 February 2021). In addition, P. lilacinum has been shown to be effective against Phyllotreta striolata, Thrips palmi, and predatory mite [14,15]. However, the P. lilacinum strains used for biocontrol agents have a high identity with those strains causing infections in humans [16,17].
Secondary metabolites are produced in a certain growth period of plants and microorganisms. They are small molecules with complex chemical structures that are not necessary for growth and reproduction, such as pigments, hormones, toxins, and antibiotics [18]. Fungi are important organisms that produce active secondary metabolites. Different kinds of fungi produce different secondary metabolites. The discovery of fungal secondary metabolites has become an important source of new drugs and pesticides [19]. Fumosorinone was isolated from the Isaria fumosorosea, and it is a potential medicine for the treatment of type II diabetes and other associated metabolic syndromes [20]. Diorcinol K, D, and I were isolated from Aspergillus, displaying significant antibacterial activities against Staphylococcus aureus and methicillin-resistant S. aureus [21]. Pyrenocine A was produced by Paecilomyces and showed a significant antitrypanosomal activity against Trypanosoma brucei [22]. Paeciloxanthone was isolated from the extracts of Paecilomyces sp. and showed significant cytotoxicity against HepG2 cell lines [23]. The research on the synthesis and regulation of secondary metabolites is helpful to develop new active compounds and increase the output of active compounds. The common secondary metabolites of fungi are polyketones, nonribosome peptides, sterols, alkaloids, and terpenes.
Several interesting reviews related to various aspects of Paecilomyces species have been published. For example, Weng reviewed the risks of Isaria fumosorosea (formerly P. fumosoroseus) and I. farinose (formerly P. farinosus) and their mycotoxins, including their structures, bioactivities, and toxicities [24]. Zhang summarized the mycotoxins of I. cicadae (formerly P. cicadae) and I. tenuipes (formerly P. tenuipes), as well as their risk evaluation [25]. As far as we know, a comprehensive overview of P. lilacinum, with an emphasis on the chemical diversity, relevant biological activities, and biosynthesis of these metabolites, remains untouched. In this paper, according to the published research reports in recent years, we have sorted out the secondary metabolites of P. lilacinum and described the sources, chemical structures, and bioactivities of the reported compounds with particular emphasis on their potential use as drug lead compounds and general biosynthesis pathways. We provide a reference for the follow-up study and ensure more secure and efficient use of fungal products.
2. Leucinostatins
Leucinostatins is a class of peptide mycotoxins that have some potent effects on liver cells after oral administration, and they were used as both antimicrobial and antitumor agents through interactions with the membrane phospholipids [26].
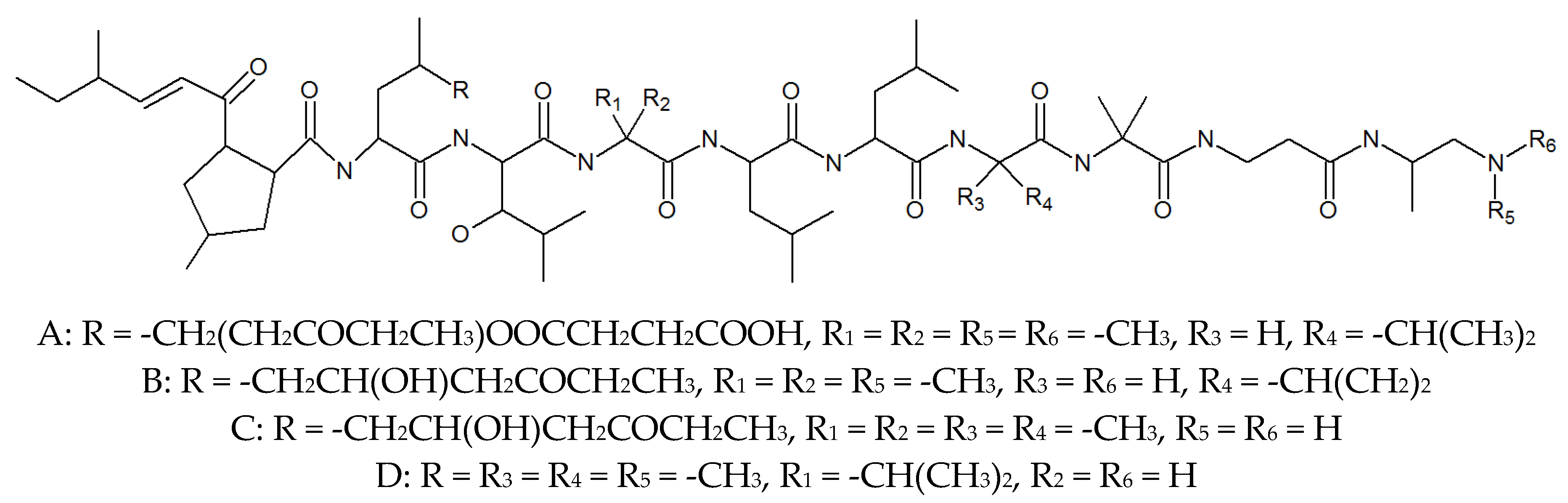
In the early 1970s, Tadashi and his team isolated a new antibiotic from the culture medium of P. lilacinum, named leucinostatin (Figure 1, Table 1). It was found that leucinostatin A, B, C, and D were active against yeasts including pathogenic and nonpathogenic strains and filamentous fungi, and were moderately active against Gram-positive bacteria, but more important is its anticancer activity, which is cytotoxic to the HeLa cell culture and inhibits Ehrlich subcutaneous solid tumors and prostate cancer [27,28]. A new report indicated that leucinostatin has a significant antihypertensive effect on rabbit blood pressure, but does not affect the reaction of adrenaline and acetylcholine [29]. It is worth mentioning that leucinostatin is one of the active substances to kill nematodes. Manabu suggested that Leucinostatin A inhibited prostate cancer cell growth through the reduction in insulin-like growth factor I expression in prostate stromal cells [30]. In addition, the use of leucinostatin A-loaded nanospheres could represent a new promising therapeutic system against Candida infection [31]. Leucinostatin Y exhibited the promising importance of the C-terminal of leucinostatins on the preferential cytotoxicity and inhibition of mitochondrial function of cancer cells in the absence of glucose [32]. It is not difficult to see that leucinostatins are potential anticancer compounds, but it should also be noted that the acute toxicities determined by intraperitoneal LD50 values for leucinostatins A and B hydrochlorides were found to be 1.8 mg/kg in mice body weight. Thus, it should be evaluated more carefully when it comes to drug use [33,34]. In addition, Yuzuru separated to obtain leucinostatin A, B, C, D, H, and K in P. lilacinum and found that the different isolates all produced leucinostatins, which means that they may play an important role not only in the infection process of mycoses in the human case, but also with insects and nematodes [26].
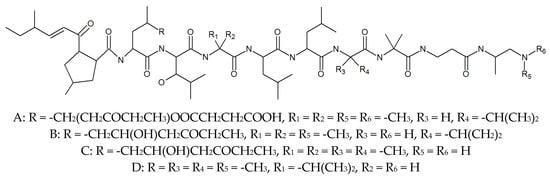
Figure 1.
The structures of leucinostatins.
3. PK Metabolites
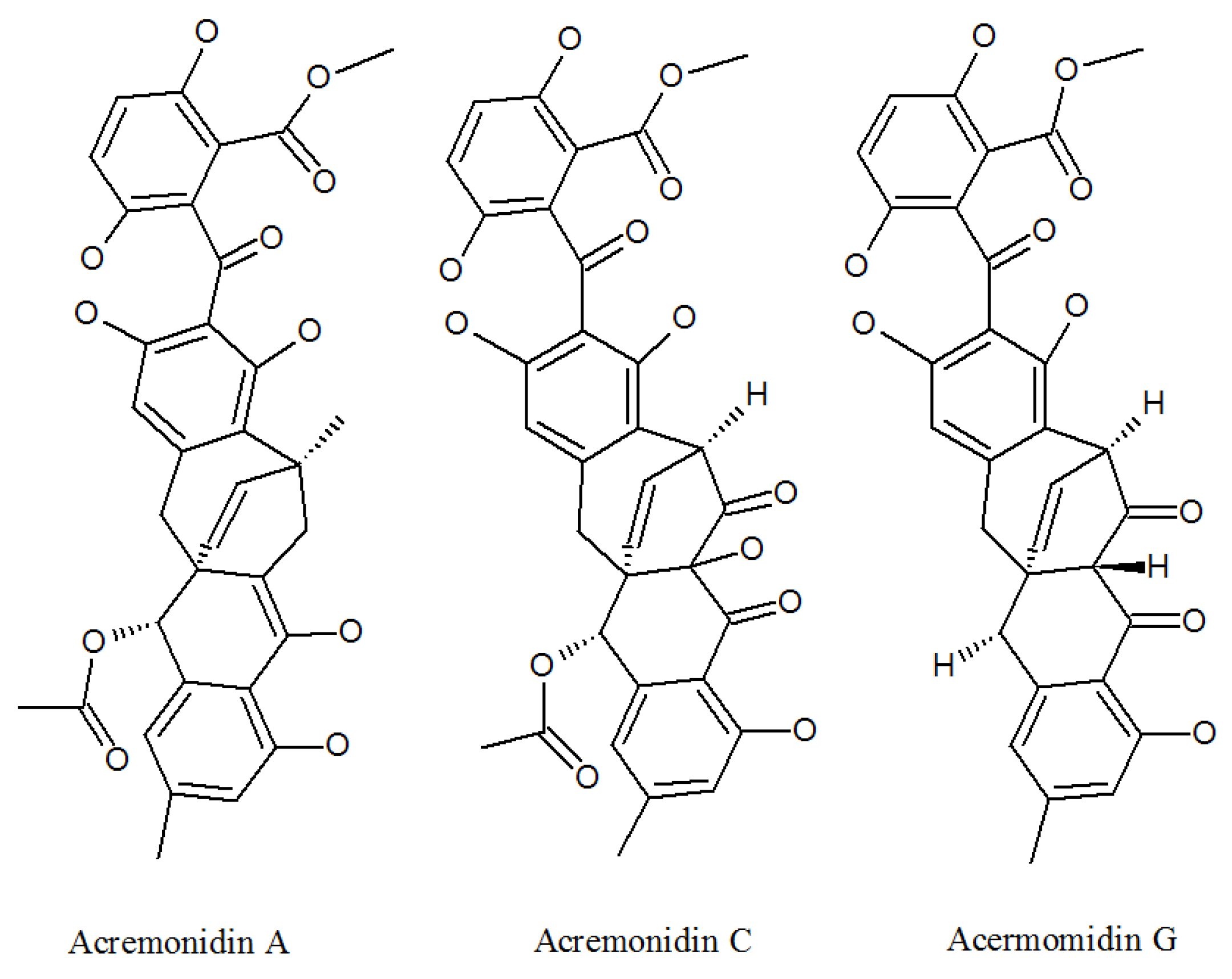
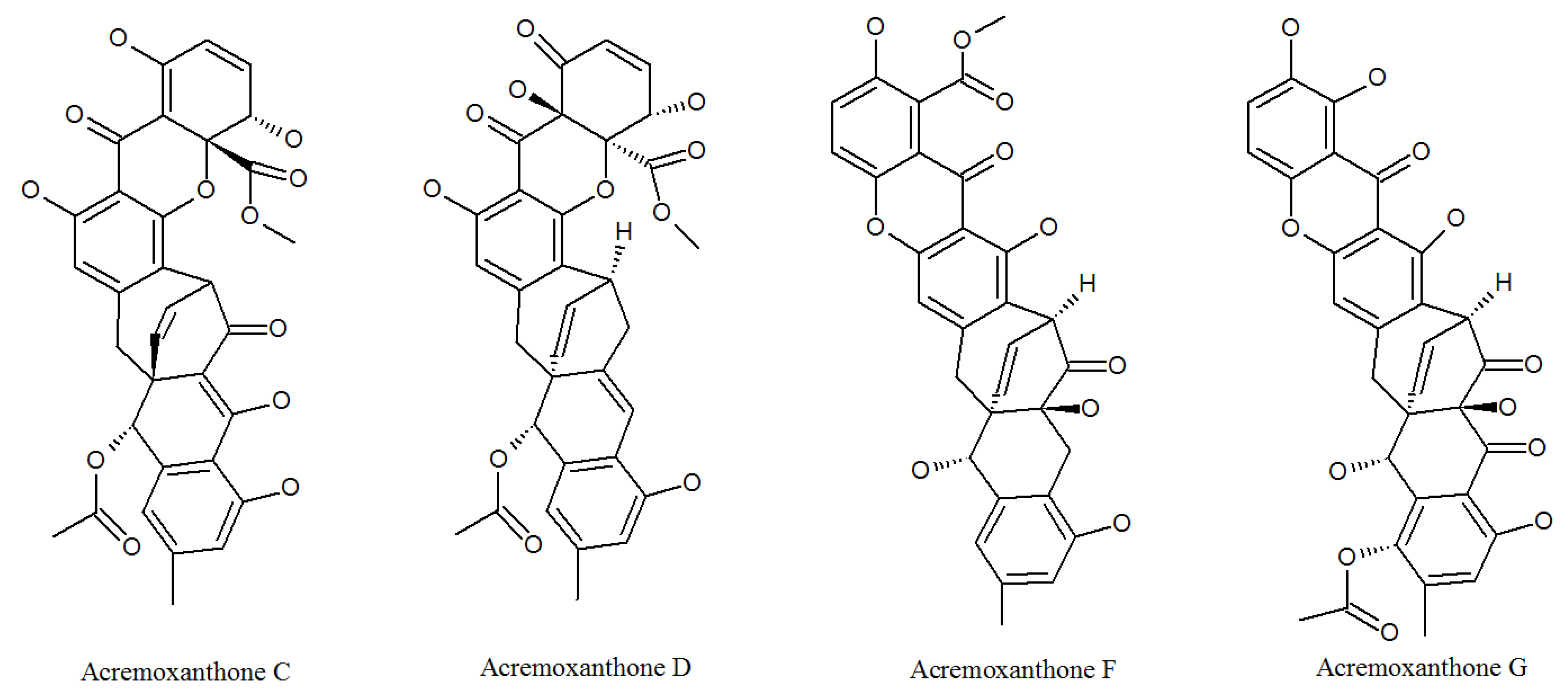
3.1. Acremonidins and Acremoxanthones
Acremonidins (Figure 2, Table 1) and acremoxanthones (Figure 3, Table 1) are kinds of polyketides (PKs), which contain alternating carbonyl and methylene groups, usually involved in cell defense or intercellular communication.
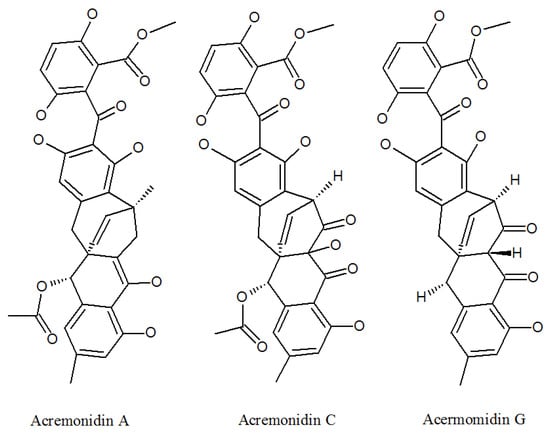
Figure 2.
The structures of acremonidins.
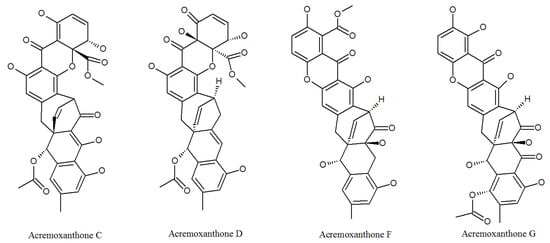
Figure 3.
The structures of acremoxanthones.
Acremoxanthone and acremonidin are xanthone-anthraquinone heterodimers, both calmodulin inhibitors produced by P. lilacinum [35]. Both of them exhibited anti-Bacillus cereus, antibacterial, antifungal, antiplasmodial, and cytotoxic activity [36]. In addition, acremonidin A and C, and acremoxanthone C and D were found to be moderate for 20 s proteasome inhibitory activity. Acremonidin A and Acremoxanthone C also have high affinity with human calmodulin biosensors. This means that they are also calmodulin inhibitors [37]. In addition, researchers found that acremoxanthone C has anti-oomycete activities [38]. Two new compounds acremoxanthones F and G represented antimalarial activity against the Plasmodium falciparum K1 strain, a multidrug-resistant strain [39]. These studies indicate that acremonidins and acremoxanthones all have high medicinal and economic value, but their toxicological effects need to be evaluated in more detail.
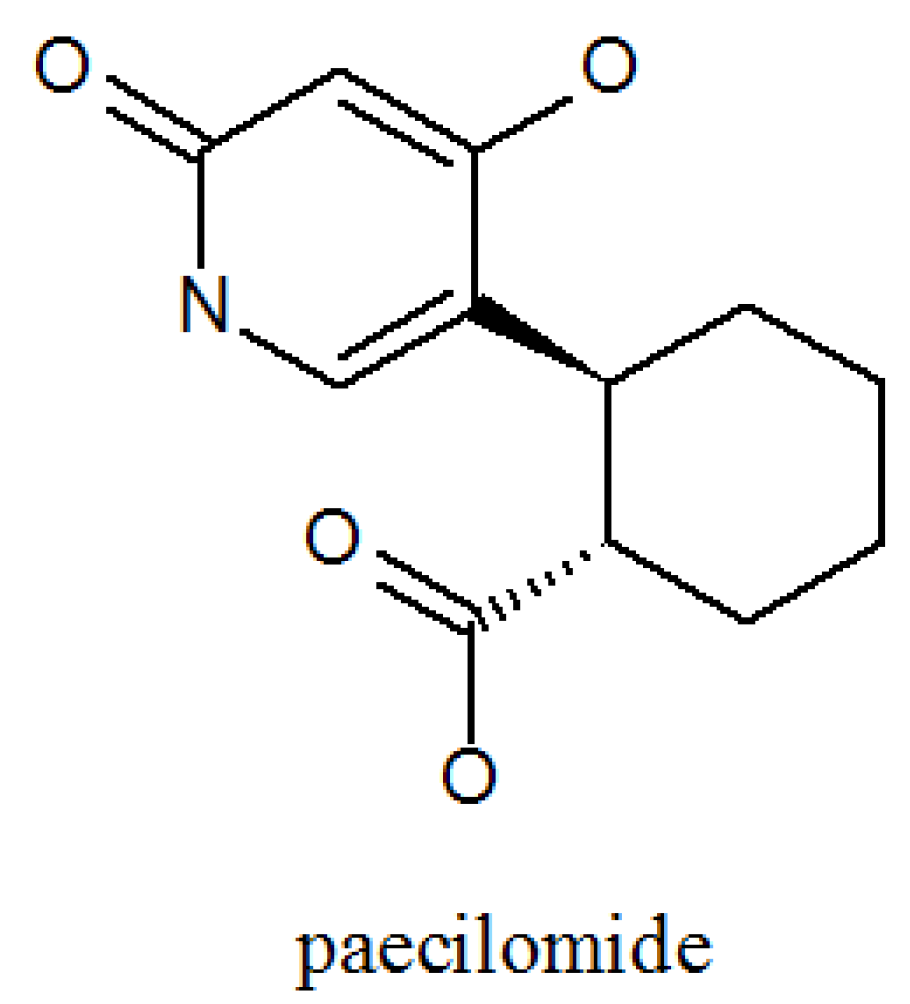
3.2. Paecilomide
Teles found a new α-pyridone Paecilomide (Figure 4, Table 1) by adding salmonella typhimurium to a flask containing P. lilacinum in two different concentrations and three different forms at two different stages of the development of P. lilacinum. He observed that adding a small amount of inoculum produced a living extract, while adding a large amount of inoculum led to the extraction of active extract, paecilomide [40]. It is an acetylcholinesterase inhibitor [41,42].
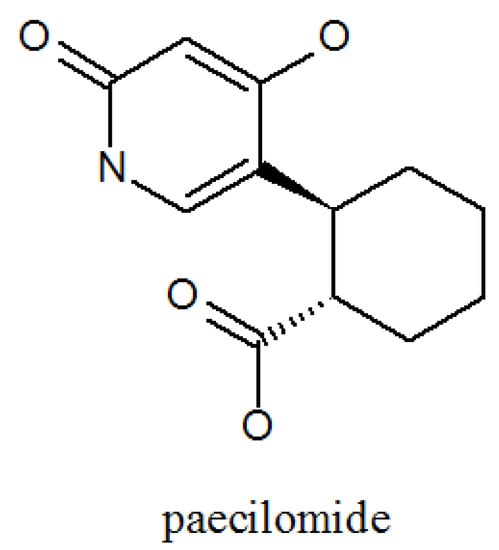
Figure 4.
The structure of paecilomide.
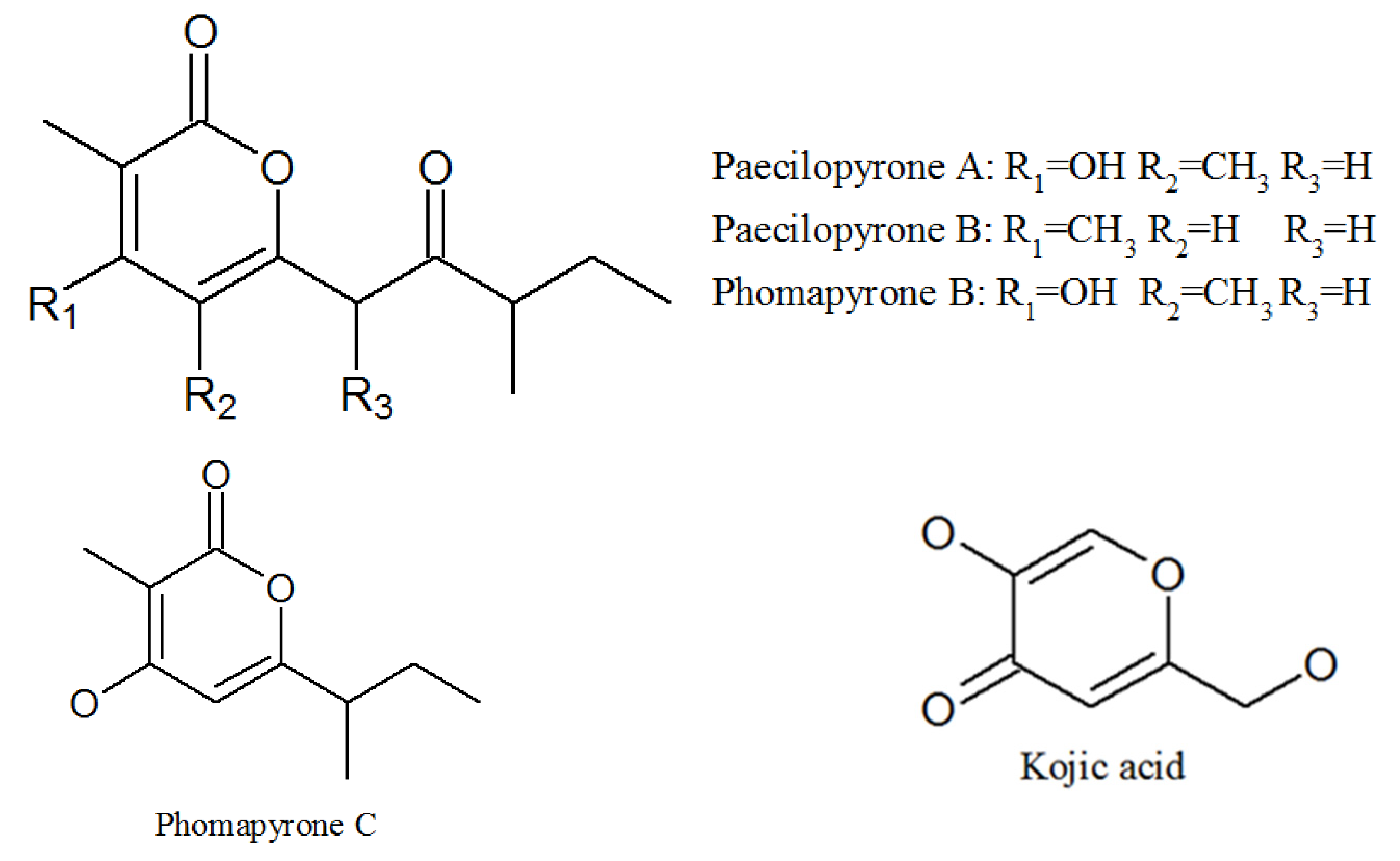
3.3. Pyrones
Elbandy isolated 13 compounds from the sponge-derived fungus P. lilacinum in 2009, four of which were α-pyrones: paecilopyrone A, paecilopyrone B, phomapyrone B, and phomapyrone C; and one γ-pyrone: kojic acid (Figure 5, Table 1). Paecilopyrone A and its linear analog paecilopyrone B may be derived from pentaketide; unfortunately, the detailed synthetic pathway is still unclear [43]. Kojic acid showed antibacterial activities and tyrosinase inhibitory activity [44,45].
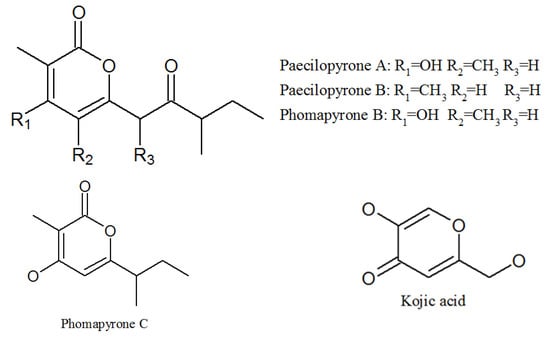
Figure 5.
The structures of pyrones.
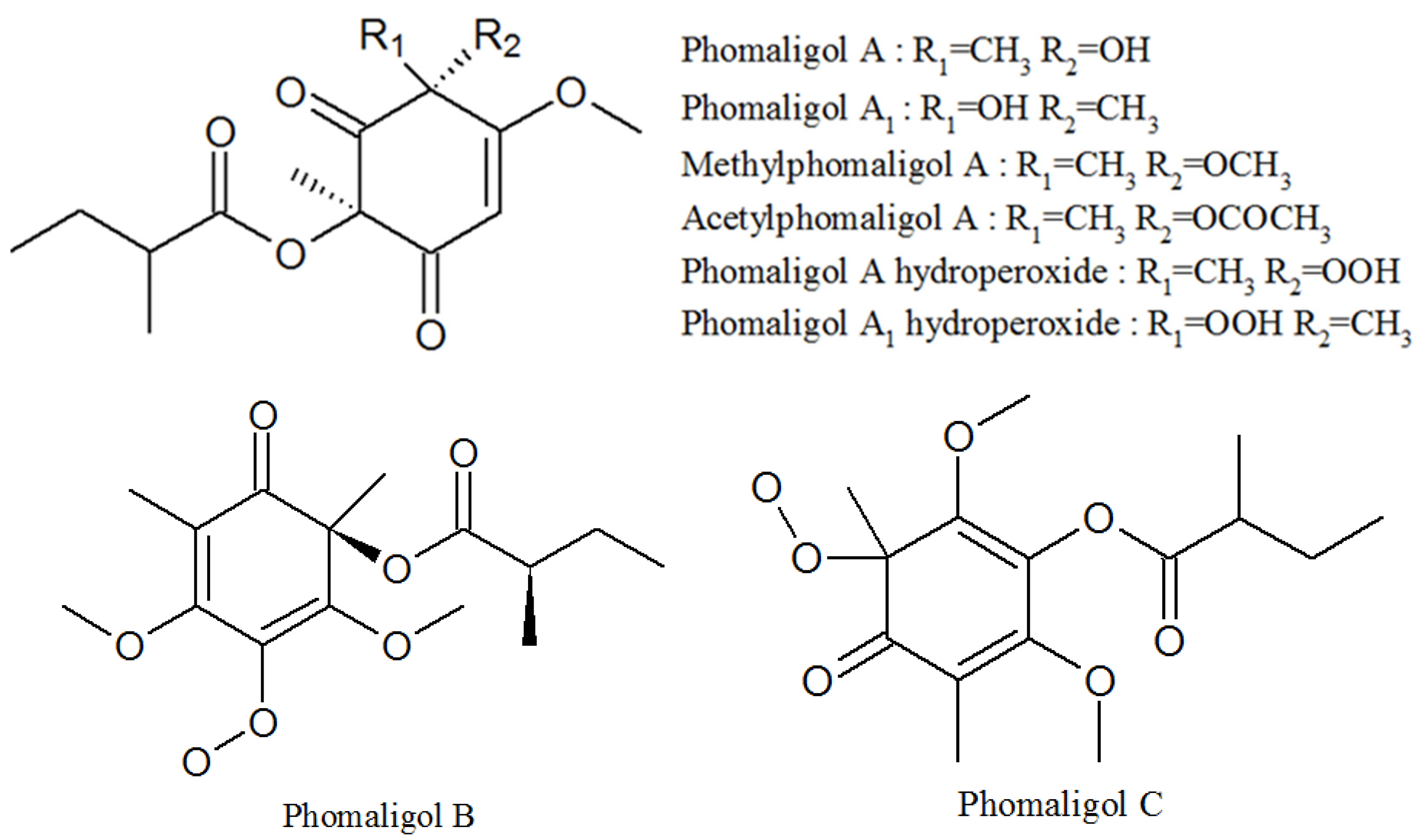
3.4. Phomaligols
Phomaligol A, phomaligol A1, methylphomaligol A, acetylphomaligol A, phomaligol A hydroperoxide, phomaligol A1 hydroperoxide, phomaligol B, and phomaligol C were all isolated from the culture of P. lilacinum (Figure 6, Table 1). All of them are yellow oil. Phomaligol A and Methylphomaligol A both showed cytotoxicity against a small panel of human solid tumor cell lines [46]. Phomaligol A, phomaligol A1, phomaligol A hydroperoxide, and phomaligol A1 hydroperoxide were previously isolated from Phoma lingam and Phoma wasabiae, but their biological activity has not been reported yet [47,48].
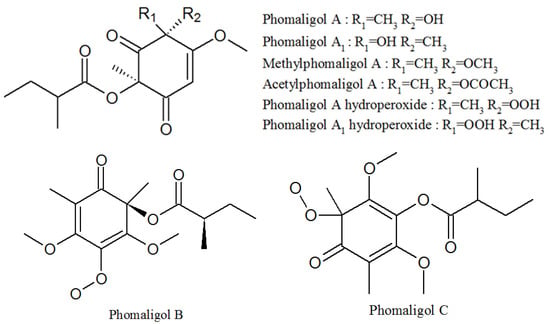
Figure 6.
The structures of phomaligols.
3.5. Pigment
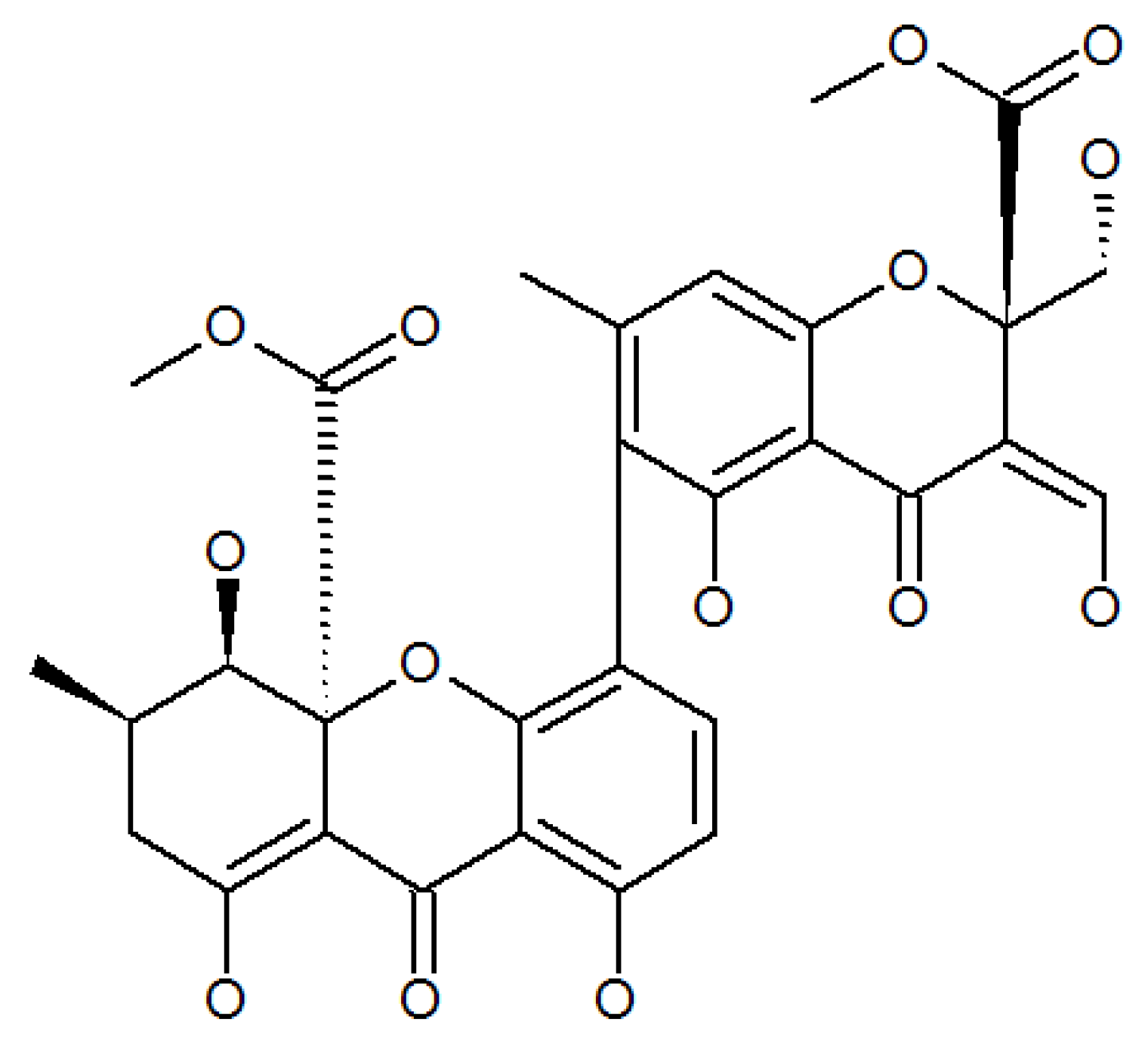
Lenta investigated the ethyl acetate extract of the mycelium of P. lilacinum isolated from the pigment purpureone (Figure 7, Table 1), which was found to possess potent antileishmanial activity and antibacterial activity [49].
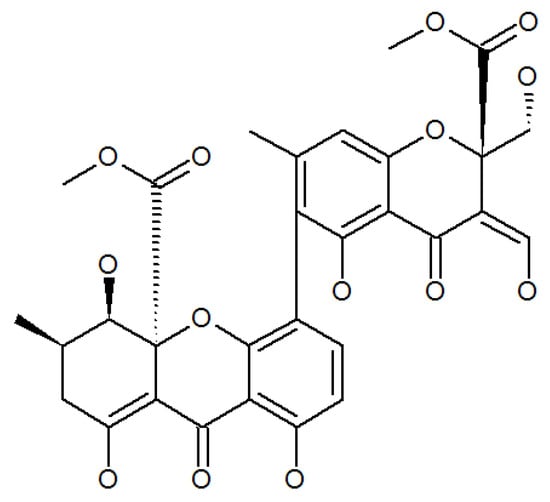
Figure 7.
The structure of purpureone.
4. Other Compounds
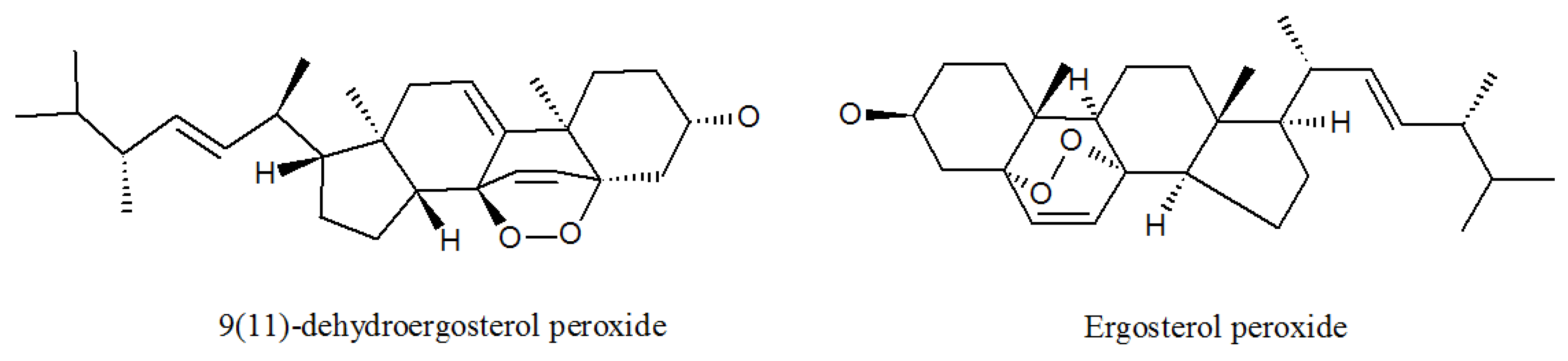
4.1. Ergosterols
Professor Cui and his team isolated seven compounds from the metabolites of P. lilacinum ZBY-1 identified as 9(11)-dehydroergosterol peroxide, ergosterol peroxide (Figure 8, Table 1), (22E,24R)-5α,6α-epoxy-3β-hydroxyergosta-22-ene-7-one, and cerebrosides A, B, C, and D. 9(11)-dehydroergosterol peroxide, ergosterol peroxide, and (22E,24R)-5α,6α-epoxy-3β-hydroxyergosta-22-ene-7-one had the inhibitory effect of human cancer K562, MCF-7, HL-60, and BGC-823 cells, with their IC50 values on these cell lines ranging from 9.5 mg/L to 59.6 mg/L [50]. 9(11)-dehydroergosterol peroxide and ergosterol peroxide were found to be useful for developing a therapeutic candidate for lung cancer complications [51,52]. These three compounds all show high medical value and provide good materials for the research and development of anti-cancer drugs.
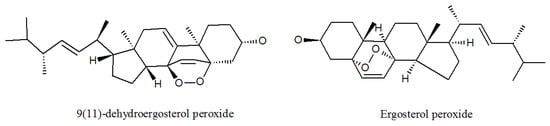
Figure 8.
The structures of ergosterols.
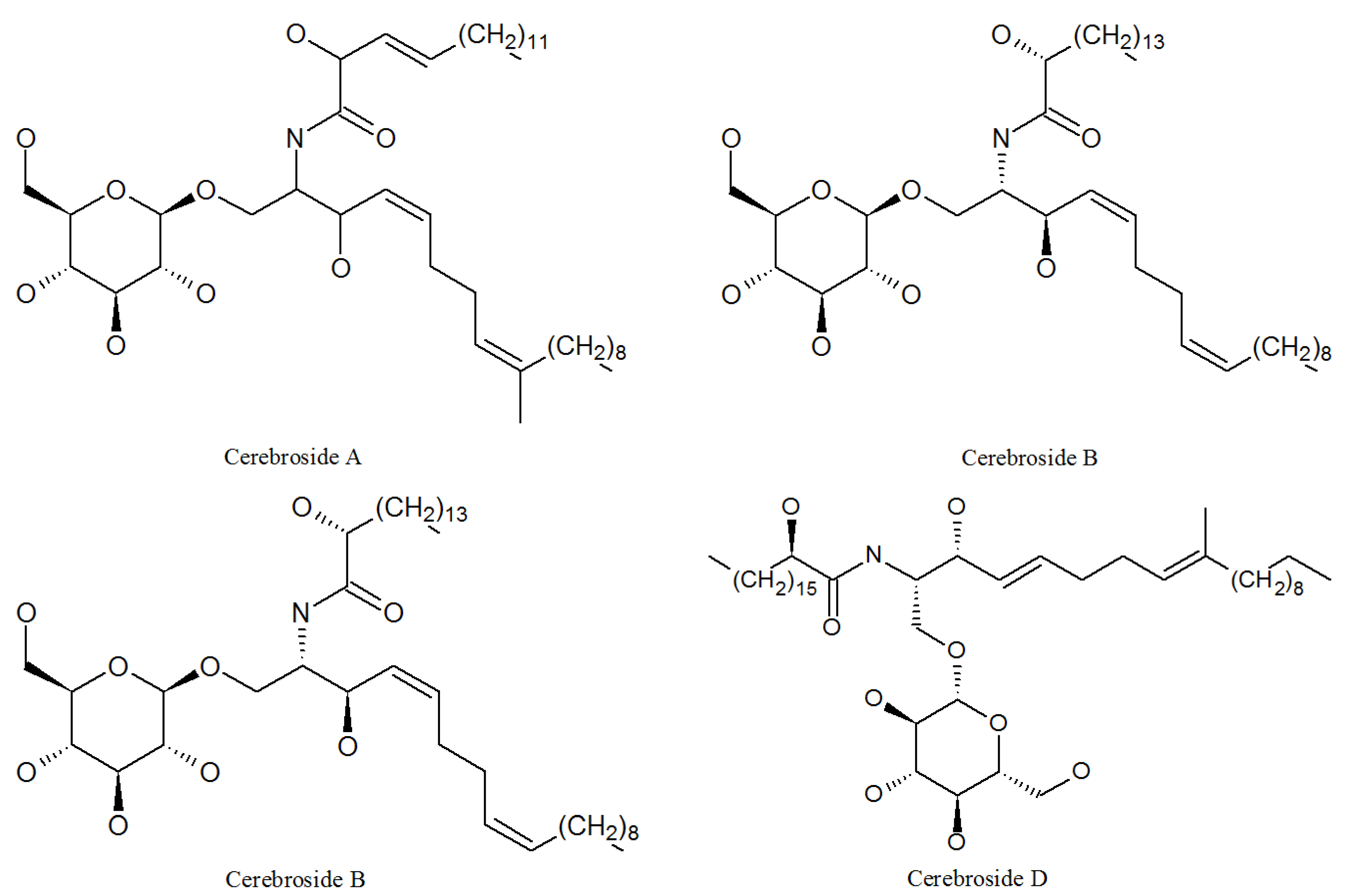
4.2. Cerebrosides
Cerebrosides A, B, C, and D (Figure 9, Table 1) were isolated from the P. lilacinum ZBY-1 strain by professor Cui in 2013, and they are all linear analogs. Cerebrosides function as a non-race-specific elicitor in a wide range of plant-phytopathogenic fungus interactions [53]; cerebrosides A and B have significant effects of analgesia and brain protection [54]. Cerebrosides C and D were known to potentiate the activity of cell wall-active antibiotics [55]. In addition, cerebrosides A and C play a role in cell growth, differentiation, and apoptosis in animals [56].
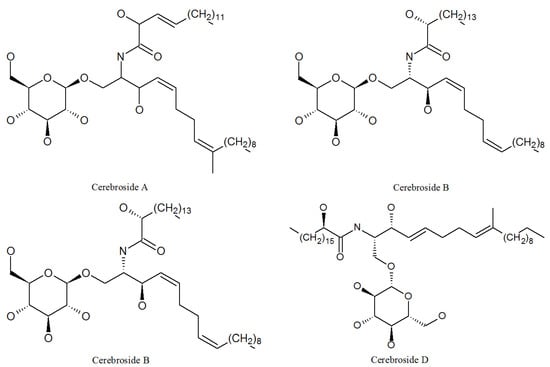
Figure 9.
The structures of cerebrosides.
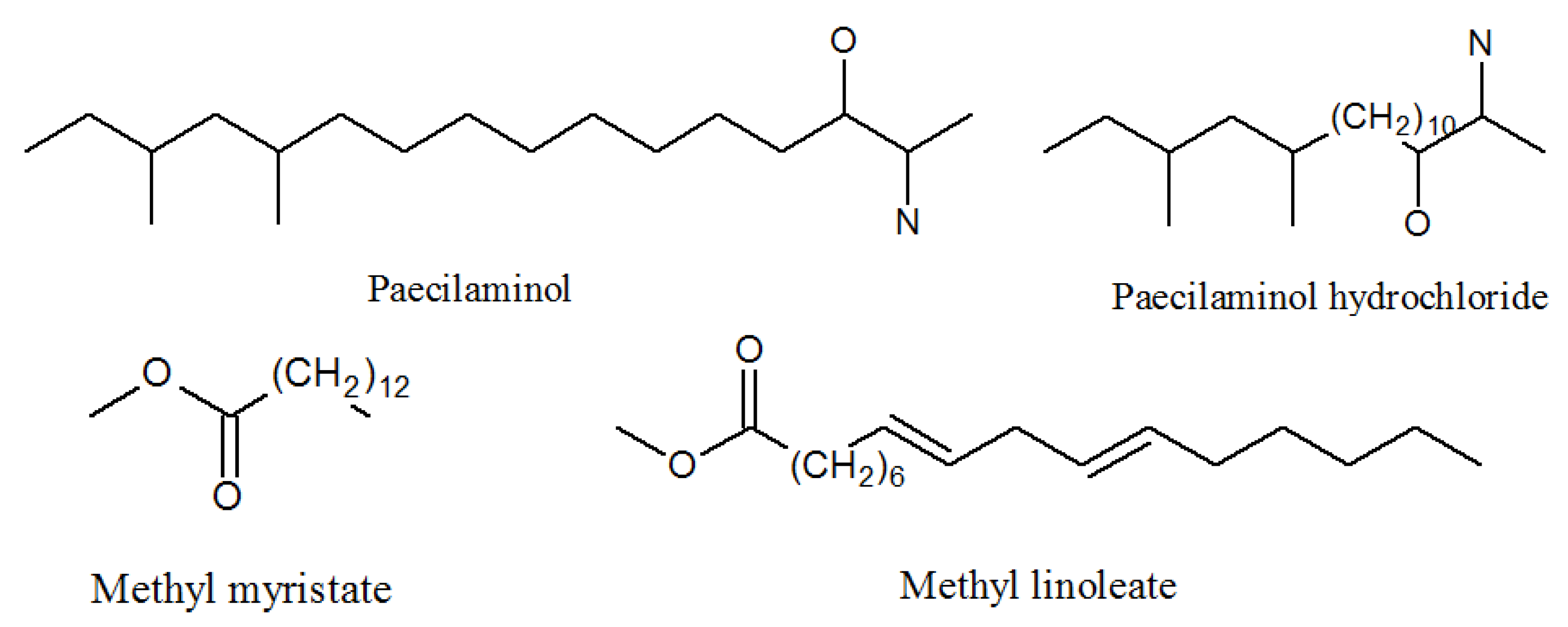
4.3. Paecilaminols and Others
Cui found 11 compounds in the year of 2012 identified as paecilaminol, paecilaminol hydrochloride, 1(2)-linolyl-2(1)-palmityl-glycero-O-4′-(N,N,N-trimethyl) homoserine, 1,2-dilinolylglycero-O-4′-(N,N,N-trimethyl) homoserine, Me myristate, Me linoleate, linoleate, oleic acid, indole-3-carboxaldehyde, indolyl-3-carboxylic acid, and 4-hydroxybenzoic acid (Figure 10, Table 1). Compounds paecilaminol and paecilaminol hydrochloride have the ability to inhibit human cancer K562, MCF-7, HL-60, and BGC-823 cells. Compound paecilaminol was a major antitumor metabolite of the strain P. lilacinum ZBY-1 and it is also a NADH-fumarate reductase inhibitor [57].
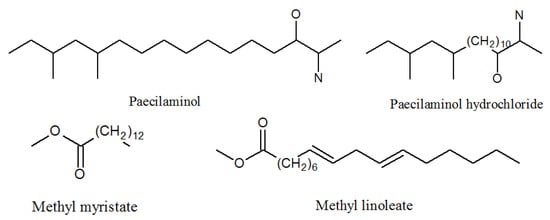
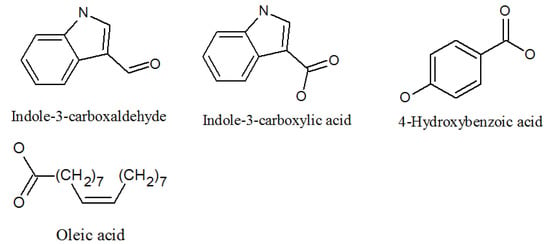
Figure 10.
The structures of paecilaminols and others.
Me myristate was promised to be exploited as a hydrophobic medical carrier [58]. Me linoleate exhibited cytotoxic antibacterial activities against Bacillus subtilis and Staphylococcus aureus [59,60]. Modern medicine often makes acute respiratory distress syndrome models by injecting oleic acid into rabbits or rats [61].
Indole-3-carboxaldehyde has useful antimicrobial properties, and it can inhibit the atopic dermatitis-like inflammation induced by MC903 [62,63]. Hydroxybenzoic acids such as 4-hydroxybenzoic acid and 3,4-dihydroxybenzoic acid have various functional biological properties, including anticancer, antibacterial, antiaging, antidiabetic, anti-inflammatory, and antiviral activities. They are widely used in food, cosmetic, and pharmaceutical industries [64]. In addition, 4-hydroxybenzoic acid increased after an organic intervention diet, and it may help with health-promoting qualities in the near future [65,66].

Table 1.
SMs isolated from Purpureocillium lilacinum and their biological activities.
Table 1.
SMs isolated from Purpureocillium lilacinum and their biological activities.
| Metabolites | CAS. No | Material Source | Biological Activity |
|---|---|---|---|
| Leucinostatin A | 76600-38-9 | P. lilacinus ZBY-1 from deep sea water | Inhibited prostate cancer cells [29], nematocidal activity [26], activity against Gram-positive bacteria [27]. |
| Leucinostatin B | 159544-15-7 | Culture medium of P. lilacinm | Treatment of systemic candidiasis, nematocidal activity [26], activity against Gram-positive bacteria [27]. |
| Leucinostatin C | 110483-88-0 | Culture medium of P. lilacinm | Drug-related side-effects and adverse reactions activity against Gram-positive bacteria [27], nematocidal activity [26]. |
| Leucinostatin D | 100334-47-2 | Cultivated, mycelia complex of P. marquandii | Activity against Gram-positive bacteria [27], nematocidal activity [26]. |
| Leucinostatin F | Culture medium of P. lilacinm | Unknown | |
| Leucinostatin H | 109539-58-4 | Culture medium of P. lilacinm | Nematocidal activity [26]. |
| Leucinostatin K | 109539-57-3 | Culture medium of P. lilacinm | Nematocidal activity [26]. |
| Leucinostatin Y | Mycelia, cultivated complex of P. linacinus 40-H-28 | Preferential cytotoxicity to cancer cells under glucose-deprived conditions and inhibition of mitochondrial function [32]. | |
| Acremoxanthone C | 1360445-63-1P | Cultivated, mycelia complex of P. lilacinm | Cytotoxicity and 20 s proteasome inhibitory activity; high affinity with human calmodulin biosensors [37]; anti-oomycete activities [38]; exhibited anti-Bacillus cereus, antibacterial, antifungal, antiplasmodial, and cytotoxic activity; Gram-positive bacteria [36]. |
| Acremoxanthone D | 1360445-62-0P | Cultivated, mycelia complex of P. lilacinm | Moderate 20 s proteasome inhibitory activity [37]. |
| Acremoxanthone F | 1882150-25-5P | Cultivated, mycelia complex of P. lilacinm | Antimalarial activity against plasmodium falciparum K1 strain and multidrug-resistant strain [39]. |
| Acremoxanthone G | 1882150-26-6P | Cultivated, mycelia complex of P. lilacinm | Antimalarial activity against plasmodium falciparum K1 strain and multidrug-resistant strain [39]. |
| Acremonidin A | 701914-77-4P | Cultivated, mycelia complex of P. lilacinm | Moderate activity Against Gram-positive bacteria [36]. |
| Acremonidin C | 701914-79-6P | Cultivated, mycelia complex of P. lilacinm | Antibacterial activity [36]. |
| Acremonidin G | 1882150-23-3P | P. lilacinus ZBY-1 from deep sea water | Anti-enterococcus faecium activity [39]. |
| Paecilomide | 1538575-22-2P | Cultivated, mycelia complex of P. lilacinm | Acetylcholinesterase inhibitor [41]. |
| 9(11)-dehydroergosterolperoxide | 91579717 | P. lilacinus ZBY-1 from deep sea water | Cytotoxic effect [51]. |
| Ergosterol peroxide | 2061-64-5 | P. lilacinus ZBY-1 from deep sea water | Exhibits antimycobacterial, trypanocidal, and antineoplastic activities [51]. |
| (22E,24R)-5α, 6α-epoxy-3β-hydroxyergosta-22-ene-7-one | P. lilacinus ZBY-1 from deep sea water | Inhibitory effect of human cancer K562, MCF-7, HL-60, and BGC-823 cells [50]. | |
| Cerebroside A | 115681-40-8 | P. lilacinus ZBY-1 from deep sea water | Induction of cell growth, differentiation, and apoptosis in animals [56]. |
| Cerebroside B | 88642-46-0 | P. lilacinus ZBY-1 from deep sea water | Causes disease such as fusariosis, colitis, and apnea |
| Cerebroside C | 98677-33-9 | P. lilacinus ZBY-1 from deep sea water | Activity of cell wall-active; antibiotics; induction of cell growth, differentiation, and apoptosis in animals [55]. |
| Cerebroside D | 113773-89-0 | P. lilacinus ZBY-1 from deep sea water | Activity of cell wall-active antibiotics [55]. |
| Paecilopyrone A | 1173292-70-0 | Cultivated, mycelia complex of P. lilacinm | Unknown |
| Paecilopyrone B | 1173292-71-1 | Same as above | Unknown |
| Phomapyrone B | 157744-25-7 | Same as above | Unknown |
| Micropyrone | 54682570 | Same as above | Unknown |
| Phomapyrone C | 157744-26-8 | Same as above | Unknown |
| Kojic acid | 501-30-4 | Same as above | Antibacterial activities; tyrosinase inhibitory activity [44]. |
| Phomaligol A | 152204-32-5 | Same as above | Unknown |
| Phomaligol A1 | 152053-11-7 | Same as above | Unknown |
| Methylphomaligol A | 152159-01-8 | Same as above | Unknown |
| Acetylphomaligol A | 1173292-72-2 | Same as above | Unknown |
| Phomaligol A hydroperoxide | 181798-75-4 | Same as above | Unknown |
| Phomaligol A1 hydroperoxide | 182072-72-6 | Same as above | Unknown |
| Phomaligol B | 1173292-73-3 | Same as above | Unknown |
| Phomaligol C | 1173292-74-4 | Same as above | Unknown |
| Paecilaminol | 540770-33-0 | Same as above | Inhibits human cancer cell K562, MCF-7, HL-60, and BGC-823 cells [50]. |
| Paecilaminol Hydrochloride | 1650570-79-8 | Same as above | Inhibits human cancer cell K562, MCF-7, HL-60, and BGC-823 cells |
| Me myristate | 124-10-7 | Same as above | Medical carrier [50]. |
| Me linoleate | 112-63-0 | Same as above | Exhibited cytotoxic antibacterial activities against Bacillus subtilis and Staphylococcus aureus [59]. |
| Indole-3-carboxaldehyde | 487-89-8 | Same as above | Antimicrobial properties [62]. |
| Indolyl-3-carboxylic acid | 771-50-6 | Same as above | Potential in vitro antimalarial, anticancer activity [63]. |
| 4-hydroxybenzoic acid | 99-96-7 | Same as above | Inhibits LPS-induced protein [64]. |
| Purpureone | 2231079-10-8P | Mycelium of P. lilacinm | Antileishmanial activity; antibacterial activity [49]. |
5. Biosynthesis of Secondary Metabolites in Purpureocillium lilacinum
In 2015, Prasad sequenced the TERIBC-1 strain of P. lilacinus with a genome size of 40.02 Mb by using Illumina Hiseq technology, and predicted 30 secondary metabolite synthesis genes: 12 polyketide syntheses (PKs, details of all abbreviations are in Table S1), 2 PKs-like, 7 nonribosome peptide synthetases, 7 NRPSs-like, 1 PK-NRPS, and 1 dimethylallyl tryptophan synthases (DMATs) gene [67]. In 2016, Wang sequenced P. lilacinus PLBJ-1 and PLFJ-1 strains. The genome sizes of the two strains were 38.14 Mb and 38.53 Mb, respectively [18]. Using SMURF [68] and anti-SMASH [69] software to predict the secondary metabolite synthesis gene cluster, PLBJ-1 and PLFJ-1 strains were found to encode 13 PKs, 2 PKs-like, 10 NRPSs, 10 NRPSs-like, 1 PK-NRPS, 4 terpene synthases (TSs), and 1 DMAT genes. It can be seen that the secondary metabolites produced by different species of P. lilacinum are not identical, but in general, P. lilacinum has great potential in the synthesis of secondary metabolites.
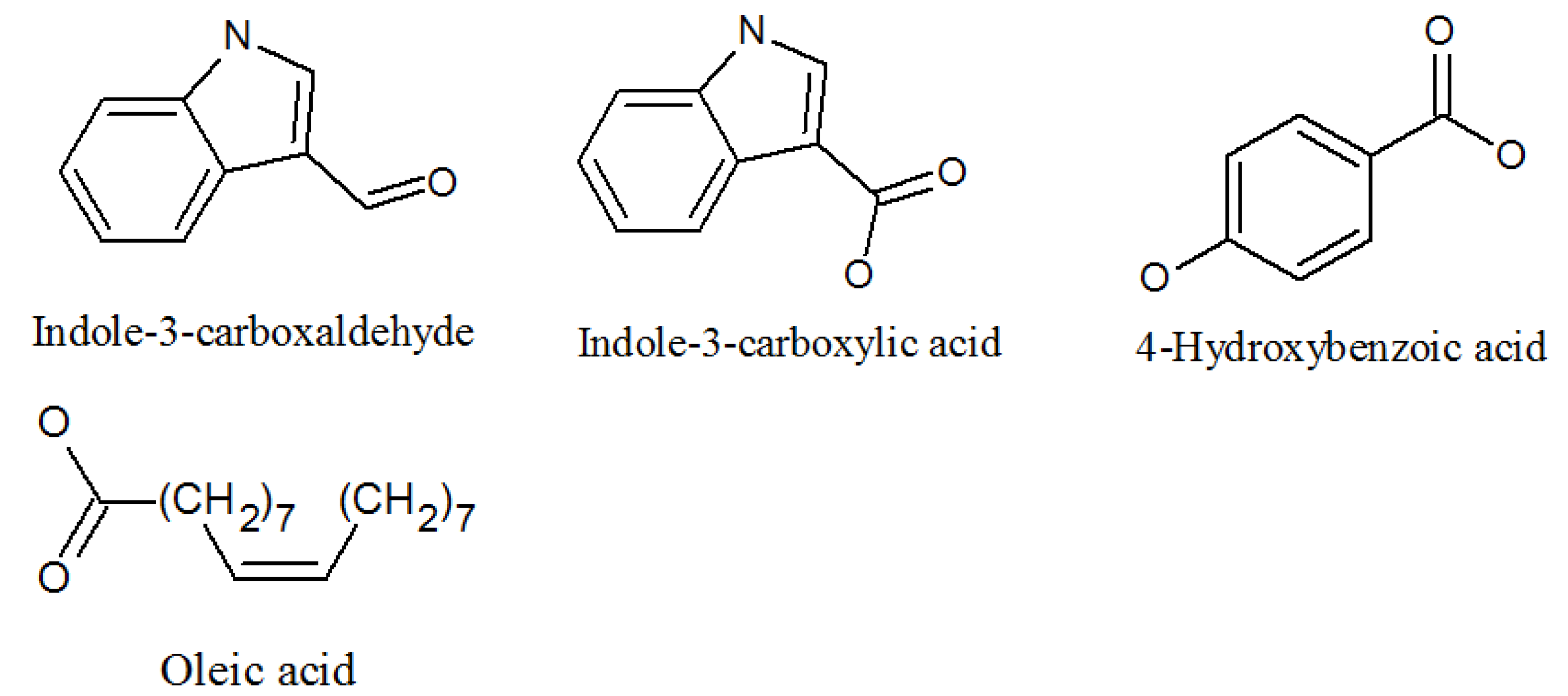
We know that the typical NRPS modules have adenylation (A), thiolation (T) or peptidyl carrier (PCP), condensation (C), and thioesterase (TE) domains [70,71], which are, respectively, responsible for the activation of amino acids, the extension of peptide chains, the formation of amide bonds, and the release of peptide chains [72,73]. The synthesis mechanism of NRPSs is shown in Figure 11. Generally speaking, the A domain combines with the amino acid substrate under the action of ATP to form the corresponding aminoacyl AMP, and the aminoacyl AMP combines with the sulfhydryl group of the T domain to form the aminoacyl-s-carrier complex. Finally, the carriers carrying the aminoacyl group and the peptide acyl group combine with the specific region of the C domain, and the amino group on the aminoacyl-s-carrier complex attacks the acyl group on the peptidyl-s-carrier complex, forming a new peptide bond, and finally forming a complete peptide chain, through the action of multiple modules, wherein the amino acids in the peptide chain correspond to the modules in the NRPS one by one. Some NRPS modules also contain epimerization (E), formylation (F), methylation (M), heterocyclization (CY) [74], reduction (R), and oxidation (OX) domains, which are involved in the structural modification of peptide chains. Finally, mature peptide chains are released from the NRP assembly line under the action of the TE domain [75].
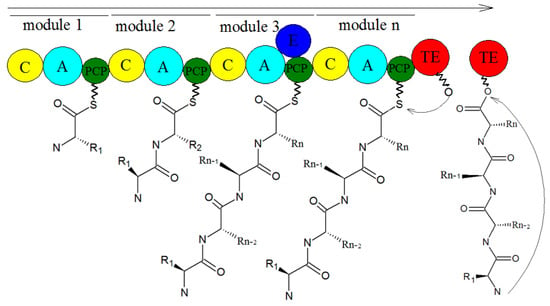
Figure 11.
The biosynthesis of NRPSs [76].
In 2016, Wang sequenced and analyzed the whole genome of P. lilacinum, and predicted the knock-out of the NRPS synthetic gene (LcsA), PK synthetase (LcsC), Acyl CoA ligase (LcsD), and thioesterase (LcsE), using high-performance liquid chromatography (HPLC) to compare the crude extracts of wild-type and mutant strains of P. lilacinum. It was found that the crude extracts of ΔLcsA, ΔLcsC, ΔLcsD, and ΔLcsE had a lack of Leucinostatin A and Leucinostatin B, and then these enzymes were found to play a key role in the synthesis of Leucinostatin, and the synthesis of leucinostatin of P. lilacinum was suggested. This hypothetical biosynthesis is initiated by the assembly of 4-methylhex-2-enoic acid via reductive PKs. However, they were unable to estimate which PKs were responsible for 4-methylhex-2-enoic acid [18].
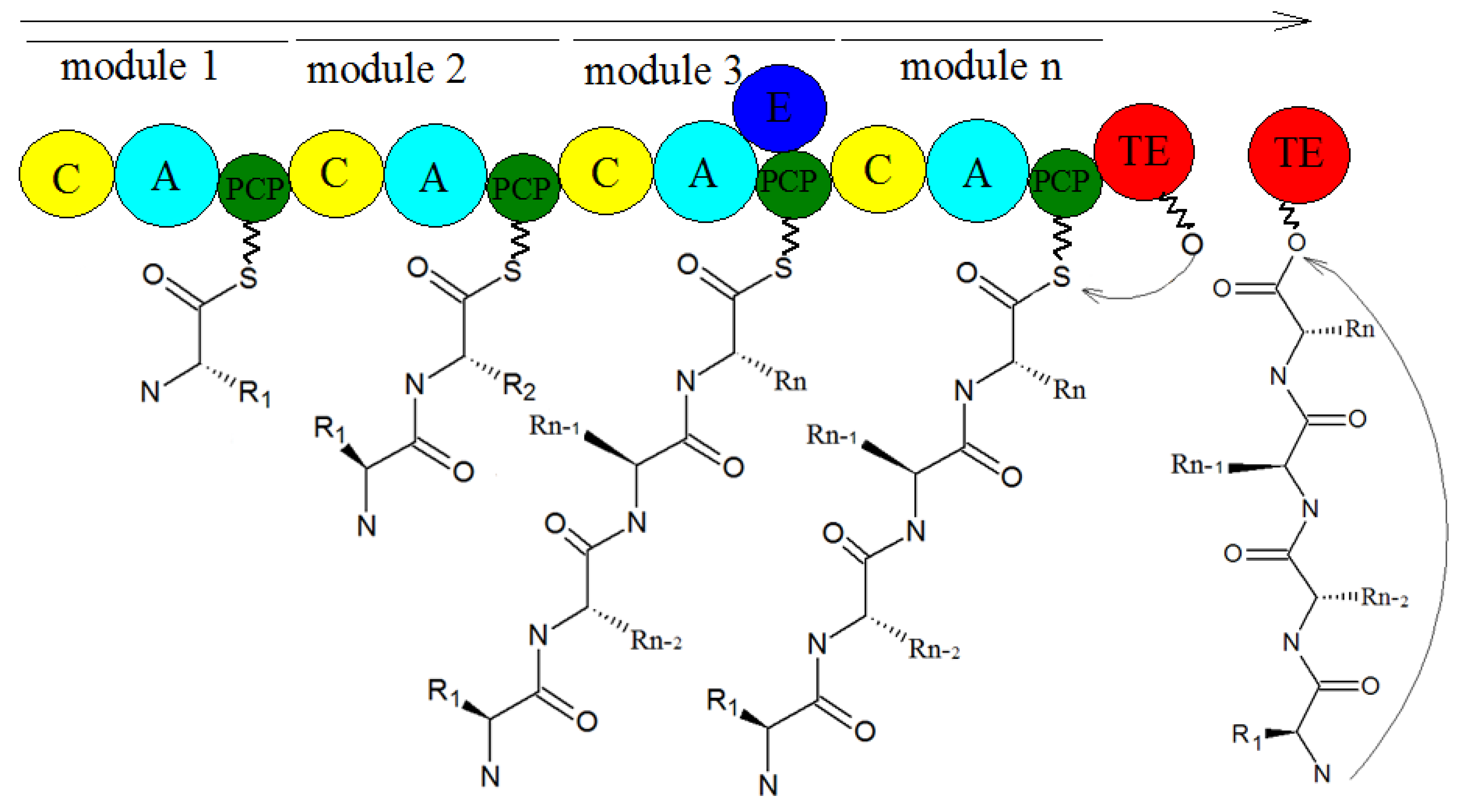
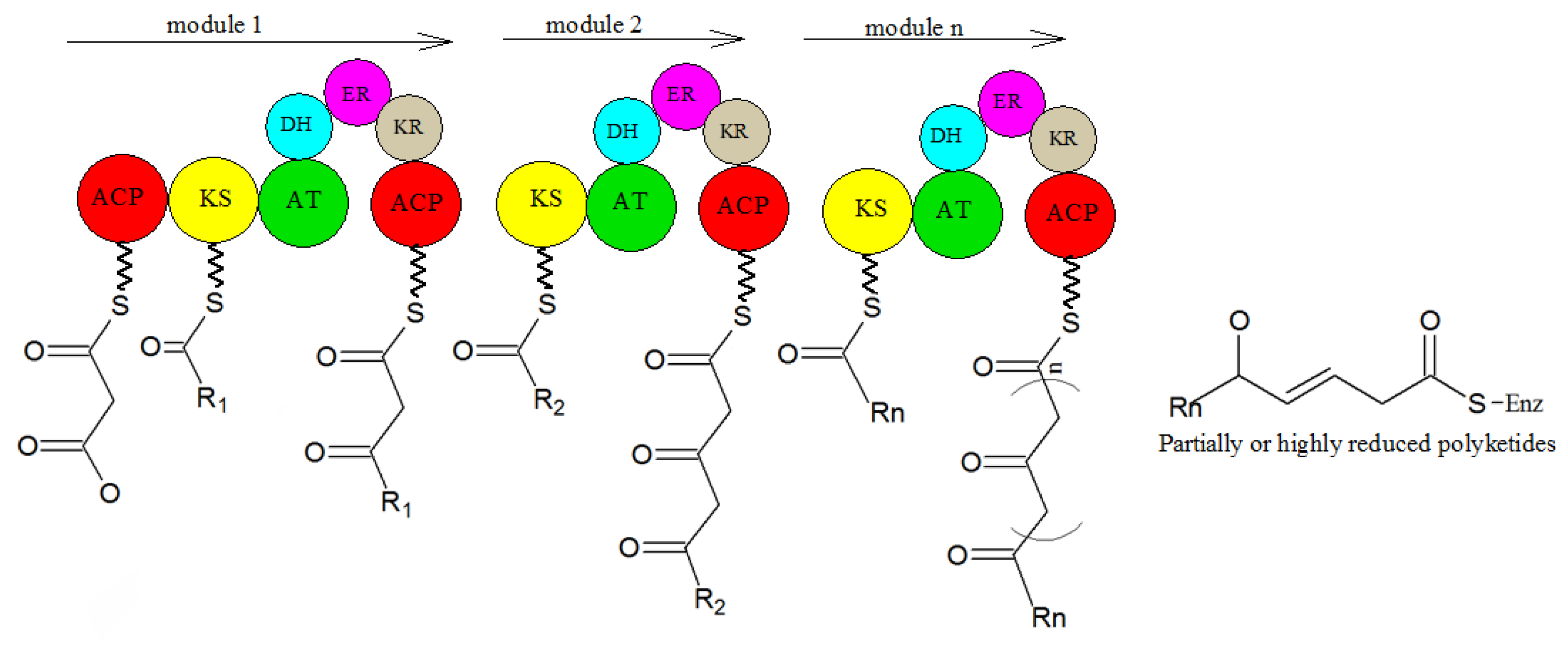
In microorganisms, PK comes from the independent hypothesis of a variety of compounds. Polyketide compounds are assembled by repeated Claisen condensations between the activated acyl initiation unit and the chain extender unit derived from malonyl-CoA. This process is catalyzed by the synergistic action of keto synthase (KS), acyltransferase (AT), and phosphopan ethylation acyl carrier protein (ACP) or CoA linked to the primary chain. After each extension step, the functionality of β-keto can be reduced by further involved enzymes [76]. This general PK catalytic mechanism is realized by different enzyme mechanisms (Figure 12). Three types of PKs are described below, which are responsible for the biosynthesis of polyketide chains.
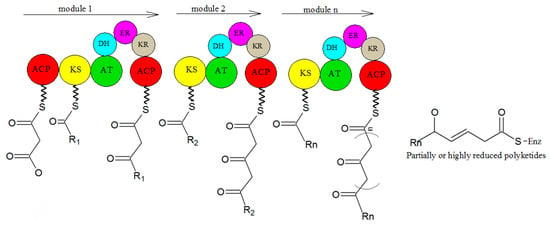
Figure 12.
The biosynthesis of PKs [77].
PKs can be divided into three types: type I PKs are modular enzymes composed of several functional domains, which are arranged linearly and covalently. Any functional domain is not reused in the process of chain synthesis and extension. They mainly synthesize polyether, polyene, and macrolides. PKs of type II are aromatic, starting from acetyl CoA. Polyketones with an aromatic ring structure are synthesized with malonyl coenzyme A as an extension unit. Type III PKs are chalcone synthetases, a kind of homologous dimer enzyme that can be reused. It catalyzes the condensation of acetyl-CoA molecules to synthesize one ring or multi-ring aromatic polyketones [74].
It is generally believed that most α-pyrones are synthesized through the polyketide pathway [78]. Terpenoids are a kind of chain or cyclic secondary metabolites, which are composed of isoprene as the basic unit. Terpenoids are synthesized by terpene synthase and can be divided into: monoterpenes, with geranyl diphosphate as the synthetic precursor; sesquiterpenes, with farnesyl diphosphate as the synthetic precursor; diterpenes, with geranyl pyrophosphate as the precursor. According to the degree of reduction, it can be divided into reduced terpenoids and nonreduced terpenoids [79].
6. Problems and Perspectives
Among the more than 40 metabolites reviewed in this paper, we can see that most SMs of P. lilacinus that have been reported so far have the functions of anticancer activity, antimicrobial activity, insecticidal activity, cytotoxicity, drug carriers, and so on. Most importantly, some of the compounds showed potent activities compared to those of the positive controls, which indicates that they could be used to develop new medicines. These include the anticancer lead compound leucinostatins, ergosterol peroxide, (22E,24R)-5α, 6α-epoxy-3β-hydroxyergosta-22-ene-7-one, and paecilaminol. Leucinostatins is cytotoxic to HeLa cells, Ehrlich subcutaneous solid tumors, and prostate cancer. However, it was found to be toxic to rats by intraperitoneal injection, so more attention should be paid to its safety assessment when developing the drug. The other three compounds have the ability to inhibit human cancer K562, MCF-7, HL-60, and BGC-823 cells, but their safety for other species is still unknown. Acremoxanthone and acremonidin were both calmodulin inhibitors; paecilomide is an acetylcholinesterase inhibitor and kojic acid showed tyrosinase inhibitory activity, indicating their potential as insecticides. These remarkable activities make many of these compounds suitable candidates for new drugs and insecticides discovery and may lead to future synthesis studies. However, some of the SMs of P. lilacinus are toxic to animals and humanity. Hocquette, Dr. Qian, Pastor, and others have reported infections caused by P. lilacinus in immunocompromised patients [80,81].
With the development of society, more and more attention has been paid to biological control, more and more fungal products will come out, and the safety of related products has also received great attention. Therefore, how to ensure the safety of fungal products has become particularly important.
Generally, in production and in life, there are six destinations (i.e., target organisms, nontarget organisms, soil, water, atmosphere, and humans) involved in the production and application of P. lilacinum pesticide formulations. The most important destination is target organisms, including pests and crops when preparations are released in fields. Soil is another important destination, especially when it is released through soil treatments for nematodes. Water and the atmosphere are the destinations of the drifting formulations. Humans contact P. lilacinum through direct and indirect pathways. There is no doubt that the biosafety risks of P. lilacinum are closely related to the sources and fates of the SMs produced by entomopathogenic fungi [24].
Surveying the SMs will be beneficial to improving the safety of P. lilacinum fungal products. Thus, developing the discovery, structure, function, and synthesis pathway of secondary metabolites of P. lilacinum are of great significance to biomedicine, human health, and agricultural disease control. For a long time, due to the gene silencing or low expression of most gene clusters in common culture medium, the research of fungal secondary metabolites has been hindered to some extent. There are only a few kinds of research on SMs of P. lilacinum, which are leucinostatins, acremoxanthones, and paecilomides, and their synthetic pathway and regulatory mechanism are still unclear. Therefore, it is necessary to use a super-expressing transcription factor, to replace the promoter in the synthetic gene cluster with an inducible strong promoter, to modify the histone, to heterologously express the gene cluster to activate the silent gene cluster, and to further discover that the structure is novel and biologically active. The SMs production yield of P. lilacinum needs to be improved by changing the culture conditions. First, gene knockout methods need to be used to further clarify the synthesis mechanism of secondary metabolites. In addition, it is necessary to continuously improve the efficiency and precision of chemical separation detection, in order to be more conducive to the separation of secondary metabolites and the identification of structural functions.
Supplementary Materials
The following are available online. Table S1: Information of all abbreviations.
Author Contributions
Conceptualization, W.C. and Q.H.; methodology, W.C.; investigation, W.C. and Q.H.; data curation, W.C. and Q.H.; writing—original draft preparation, W.C. and Q.H.; writing—review and editing, Q.H.; supervision, Q.H.; funding acquisition, Q.H. All authors have read and agreed to the published version of the manuscript.
Funding
This project was supported by the Guangzhou Science and Technology Project (201903010067).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Luangsa-Ard, J.; Houbraken, J.; van Doorn, T.; Hong, S.B.; Borman, A.M.; Hywel-Jones, N.L.; Samson, R.A. Purpureocillium, a new genus for the medically important Paecilomyces lilacinus. FEMS Microbiol. Lett. 2011, 321, 141–149. [Google Scholar] [CrossRef]
- Sampson, R.A. Paecilomyces and Some Allied Hyphomycetes. Cent. Voor Schimmelcultures 1975, 64, 174. [Google Scholar] [CrossRef]
- Srilakshmi, A.; Sai Gopal, D.V.R.; Narasimha, G. Impact of bioprocess parameters on cellulase production by Purpureocillium lilacinum isolated from forest soil. Int. J. Pharma Bio Sci. 2017, 8, 157–165. [Google Scholar] [CrossRef]
- Zhu, Y.; Ai, D.; Zhang, W. Difference of soil microbiota in perennial ryegrass turf before and after turning green using high-throughput sequencing technology. Res. J. BioTechnol. 2017, 12, 50–60. [Google Scholar]
- Redou, V.; Navarri, M.; Meslet-Cladiere, L.; Barbier, G.; Burgaud, G. Species richness and adaptation of marine fungi from deep-subseafloor sediments. Appl. Environ. Microbiol. 2015, 81, 3571–3583. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zhang, C.; Fan, H.; Guo, Z.; Yang, H.; Chen, M.; Han, J.; Cao, Y.; Xu, J.; Zhang, K.; et al. An efficient gene disruption system for the nematophagous fungus Purpureocillium lavendulum. Fungal. Biol. 2019, 123, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.D.; Carneiro, R.M.D.G.; Faria, M.; Souza, D.A.; Monnerat, R.G.; Lopes, R.B. Evaluation of Pochonia chlamydosporia and Purpureocillium lilacinum for suppression of Meloidogyne enterolobii on tomato and banana. J. Nematol. 2017, 49, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Gine, A.; Sorribas, F.J. Effect of plant resistance and BioAct WG (Purpureocillium lilacinum strain 251) on Meloidogyne incognita in a tomato-cucumber rotation in a greenhouse. Pest Manag. Sci. 2017, 73, 880–887. [Google Scholar] [CrossRef]
- Cavello, I.A.; Hours, R.A.; Rojas, N.L.; Cavalitto, S.F. Purification and characterization of a keratinolytic serine protease from Purpureocillium lilacinum LPS # 876. Process. Biochem. 2013, 48, 972–978. [Google Scholar] [CrossRef]
- Desaeger, J.A.; Watson, T.T. Evaluation of new chemical and biological nematicides for managing Meloidogyne javanica in tomato production and associated double-crops in Florida. Pest Manag. Sci. 2019, 75, 3363–3370. [Google Scholar] [CrossRef] [PubMed]
- Jiao, Y.; Li, Y.; Li, Y.; Cao, H.; Mao, Z.; Ling, J.; Yang, Y.; Xie, B. Functional genetic analysis of the leucinostatin biosynthesis transcription regulator lcsL in Purpureocillium lilacinum using CRISPR-Cas9 technology. Appl. Microbiol. Biotechnol. 2019, 103, 6187–6194. [Google Scholar] [CrossRef]
- Wang, M.; Zhou, H.; Fu, Y.; Wang, C. The Antifungal Activities of the Fungus 36–1 to Several Plant Pathogens. Chin. J. Biol. Control. 1996, 12, 20–23. [Google Scholar]
- Li, F.; Chen, J.; Shi, H.; Liu, B. Anatgoinstic effect of biocontrol fungus, Paecilomyces lilacinus strain NH-PL-3 and its mechainsm against Fusairum oxyspourm. J. Plant Prot. 2005, 32, 373–378. [Google Scholar]
- Hotaka, D.; Amnuaykanjanasin, A.; Maketon, C.; Siritutsoontorn, S.; Maketon, M. Efficacy of Purpureocillium lilacinum CKPL-053 in controlling Thrips palmi (Thysanoptera: Thripidae) in orchid farms in Thailand. Appl. Entomol. Zool. 2015, 50, 317–329. [Google Scholar] [CrossRef]
- Yoder, J.A.; Fisher, K.A.; Dobrotka, C.J. A report on Purpureocillium lilacinum found naturally infecting the predatory mite, Balaustium murorum (Parasitengona: Erythraeidae). Int. J. Acarol. 2018, 44, 139–145. [Google Scholar] [CrossRef]
- Deng, J.X.; Paul, N.C.; Sang, H.K.; Lee, J.H.; Hwang, Y.S.; Yu, S.H. First Report on Isolation of Penicillium adametzioides and Purpureocillium lilacinum from Decayed Fruit of Cheongsoo Grapes in Korea. Mycobiology 2012, 40, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.-N.; Wang, H.; Hsueh, P.-R.; Meis, J.F.; Chen, H.; Xu, Y.-C. Endophthalmitis caused by Purpureocillium lilacinum. J. Microbiol. Immunol. Infect. 2019, 52, 170–171. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Liu, Z.; Lin, R.; Li, E.; Mao, Z.; Ling, J.; Yang, Y.; Yin, W.-B.; Xie, B. Biosynthesis of antibiotic leucinostatins in bio-control fungus Purpureocillium lilacinum and their inhibition on Phytophthora revealed by genome mining. PLoS Pathog. 2016, 12, e1005685. [Google Scholar] [CrossRef] [PubMed]
- Bode, H.B.; Bethe, B.; Hofs, R.; Zeeck, A. Big effects from small changes: Possible ways to explore nature’s chemical diversity. Chembiochem 2002, 3, 619–627. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, J.; Chen, C.; Teng, J.; Wang, C.; Luo, D. Structure and biosynthesis of fumosorinone, a new protein tyrosine phosphatase 1B inhibitor firstly isolated from the entomogenous fungus Isaria fumosorosea. Fungal Genet. Biol. 2015, 81, 191–200. [Google Scholar] [CrossRef]
- Yurchenko, A.N.; Girich, E.V.; Yurchenko, E.A. Metabolites of Marine Sediment-Derived Fungi: Actual Trends of Biological Activity Studies. Mar. Drugs 2021, 19, 88. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-Q.; Xu, K.; Liu, X.-M.; Zhang, P. A Systematic Review on Secondary Metabolites of Paecilomyces Species: Chemical Diversity and Biological Activity. Planta Medica 2020, 86, 805–821. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.; Lin, Y.C.; She, Z.G.; Du, D.S.; Chan, W.L.; Zheng, Z.H. Paeciloxanthone, a new cytotoxic xanthone from the marine mangrove fungus Paecilomyces sp. (Tree1–7). J. Asian Nat. Prod. Res. 2008, 10, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Weng, Q.; Zhang, X.; Chen, W.; Hu, Q. Secondary Metabolites and the Risks of Isaria fumosorosea and Isaria farinosa. Molecules 2019, 24, 664. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, Q.; Weng, Q. Secondary metabolites (SMs) of Isaria cicadae and Isaria tenuipes. RSC Adv. 2019, 9, 172–184. [Google Scholar] [CrossRef]
- Mikami, Y.; Yazawa, K.; Fukushima, K.; Arai, T.; Samson, R.A.J.M. Paecilotoxin production in clinical or terrestrial isolates of Paecilomyces lilacinus strains. Mycopathologia 1989, 108, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Rossi, C.; Tuttobello, L.; Ricci, M.; Casinovi, C.G.; Radios, L. Leucinostatin D, a novel peptide antibiotic from Paecilomyces marquandii. J. Antibiot. 1987, 40, 130–133. [Google Scholar] [CrossRef]
- Momose, I.; Onodera, T.; Doi, H.; Adachi, H.; Iijima, M.; Yamazaki, Y.; Sawa, R.; Kubota, Y.; Igarashi, M.; Kawada, M. Leucinostatin Y: A Peptaibiotic Produced by the Entomoparasitic Fungus Purpureocillium lilacinum 40-H-28. J. Nat. Prod. 2019, 82, 1120–1127. [Google Scholar] [CrossRef]
- Kawada, M.; Inoue, H.; Momose, I.; Masuda, T.; Ikeda, D. 188 POSTER Leucinostatins suppress prostate cancer cell growth through the tumour-stromal cell interactions. Eur. J. Cancer Suppl. 2008, 6, 59–60. [Google Scholar] [CrossRef]
- Kawada, M.; Inoue, H.; Ohba, S.I.; Masuda, T.; Momose, I.; Ikeda, D. Leucinostatin A inhibits prostate cancer growth through reduction of insulin-like growth factor-I expression in prostate stromal cells. Int. J. Cancer 2010, 126, 810–818. [Google Scholar] [CrossRef]
- Ricci, M.; Blasi, P.; Giovagnoli, S.; Perioli, L.; Vescovi, C.; Rossi, C. Leucinostatin-A loaded nanospheres: Characterization and in vivo toxicity and efficacy evaluation. Int. J. Pharm. 2004, 275, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Arai, T.; Mikami, Y.; Fukushima, K.; Utsumi, T.; Yazawa, K. A new antibiotic, leucinostatin, derived from Penicillium lilacinum. J. Antibiot. 1973, 26, 157–161. [Google Scholar] [CrossRef]
- Fukushima, K.; Arai, T.; Mori, Y.; Tsuboi, M.; Suzuki, M. Studies on peptide antibiotics, leucinostatins. I. Separation, physico-chemical properties and biological activities of leucinostatins A and B. J. Antibiot. 1983, 36, 1606–1612. [Google Scholar] [CrossRef] [PubMed]
- Ishiyama, A.; Otoguro, K.; Iwatsuki, M.; Namatame, M.; Nishihara, A.; Nonaka, K.; Kinoshita, Y.; Takahashi, Y.; Masuma, R.; Shiomi, K.; et al. In vitro and in vivo antitrypanosomal activities of three peptide antibiotics: Leucinostatin A and B, alamethicin I and tsushimycin. J. Antibiot. 2009, 62, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Madariaga-Mazón, A.; González-Andrade, M.; González, M.d.C.; Glenn, A.E.; Cerda-García-Rojas, C.M.; Mata, R. Absolute Configuration of Acremoxanthone C, a Potent Calmodulin Inhibitor from Purpureocillium lilacinum. J. Nat. Prod. 2013, 76, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Ayers, S.; Graf, T.N.; Adcock, A.F.; Kroll, D.J.; Shen, Q.; Swanson, S.M.; Matthew, S.; de Blanco, E.; Wani, M.C.; Darveaux, B.A.; et al. Cytotoxic xanthone-anthraquinone heterodimers from an unidentified fungus of the order Hypocreales (MSX 17022). J. Antibiot. 2012, 65, 3–8. [Google Scholar] [CrossRef]
- Melendez-Gonzalez, C.; Muria-Gonzalez, M.J.; Anaya, A.L.; Hernandez-Bautista, B.E.; Hernandez-Ortega, S.; Gonzalez, M.C.; Glenn, A.E.; Hanlin, R.T.; Macias-Rubalcava, M.L. Acremoxanthone E, a Novel Member of Heterodimeric Polyketides with a Bicyclo[3.2.2]nonene Ring, Produced by Acremonium camptosporum W. Gams (Clavicipitaceae) Endophytic Fungus. Chem. Biodivers. 2015, 12, 133–147. [Google Scholar] [CrossRef]
- Isaka, M.; Palasarn, S.; Auncharoen, P.; Komwijit, S.; Gareth Jones, E.B. Acremoxanthones A and B, novel antibiotic polyketides from the fungus Acremonium sp. BCC 31806. Tetrahedron Lett. 2009, 50, 284–287. [Google Scholar] [CrossRef]
- He, H.; Bigelis, R.; Solum, E.H.; Greenstein, M.; Carter, G.T. Acremonidins, new polyketide-derived antibiotics produced by Acremonium sp., LL-Cyan 416. J. Antibiot. 2003, 56, 923–930. [Google Scholar] [CrossRef]
- Teles, A.P.C.; Takahashi, J.A. Paecilomide, a new acetylcholinesterase inhibitor from Paecilomyces lilacinus. Microbiol. Res. 2013, 168, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Tumiatti, V.; Bolognesi, M.L.; Minarini, A.; Rosini, M.; Milelli, A.; Matera, R.; Melchiorre, C. Progress in acetylcholinesterase inhibitors for Alzheimer’s disease: An update. Expert Opin. Ther. Pat. 2008, 18, 387–401. [Google Scholar] [CrossRef]
- Kulshreshtha, A.; Piplani, P. Current pharmacotherapy and putative disease-modifying therapy for Alzheimer’s disease. Neurol. Sci. 2016, 37, 1403–1435. [Google Scholar] [CrossRef]
- Seibert, S.F.; Eguereva, E.; Krick, A.; Kehraus, S.; Voloshina, E.; Raabe, G.; Fleischhauer, J.; Leistner, E.; Wiese, M.; Prinz, H.; et al. Polyketides from the marine-derived fungus Ascochyta salicorniae and their potential to inhibit protein phosphatases. Org. Biomol. Chem. 2006, 4, 2233–2240. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Xie, W.; Zhao, Y.; Lv, X.; Yang, H.; Zeng, Q.; Zheng, Z.; Yang, X. Synthesis, antimicrobial, moisture absorption and retention activities of kojic acid-grafted konjac glucomannan oligosaccharides. Polymers 2019, 11, 1979. [Google Scholar] [CrossRef]
- Li, X.; Jeong, J.H.; Lee, K.T.; Rho, J.R.; Choi, H.D.; Kang, J.S.; Son, B.W. γ-pyrone derivatives, kojic acid methyl ethers from a marine-derived fungus Altenaria sp. Arch. Pharmacal Res. 2003, 26, 532–534. [Google Scholar] [CrossRef]
- Elbandy, M.; Shinde, P.B.; Hong, J.; Bae, K.S.; Kim, M.A.; Lee, S.M.; Jung, J.H. α-pyrones and yellow pigments from the sponge-derived fungus Paecilomyces lilacinus. Bull. Korean Chem. Soc. 2009, 30, 188–192. [Google Scholar] [CrossRef]
- Pedras, M.S.C.; Taylor, J.L.; Morales, V.M. Phomaligin A and other yellow pigments in Phoma lingam and P. wasabiae. Phytochemistry 1995, 38, 1215–1222. [Google Scholar] [CrossRef]
- Soga, O.; Iwamoto, H.; Hata, K.; Maeba, R.; Takuwa, A.; Fujiwara, T.; Hsu, Y.H.; Nakayama, M. New oxidation product of was abidienone-A. Agric. Biol. Chem. 1988, 52, 865–866. [Google Scholar] [CrossRef]
- Lenta, B.N.; Ngatchou, J.; Frese, M.; Ladoh-Yemeda, F.; Voundi, S.; Nardella, F.; Michalek, C.; Wibberg, D.; Ngouela, S.; Tsamo, E.; et al. Purpureone, an antileishmanial ergochrome from the endophytic fungus Purpureocillium lilacinum. Z. Für Nat. B J. Chem. Sci. 2016, 71, 1159–1167. [Google Scholar] [CrossRef]
- Cui, X.; Li, C.; Wu, C.; Hua, W.; Cui, C.; Zhu, T.; Gu, Q.-Q. Metabolites of Paecilomyces lilacinus zby-1 from deep-sea water and their antitumor activity. J. Int. Pharm. Res 2013, 40, 177–186. [Google Scholar]
- Wu, H.; Yang, F.; Li, L.; Rao, Y.K.; Ju, T.; Wong, W.; Hsieh, C.; Pivkin, M.V.; Hua, K.; Wu, S. Ergosterol peroxide from marine fungus Phoma sp. induces ROS-dependent apoptosis and autophagy in human lung adenocarcinoma cells. Sci. Rep. 2018, 8, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, S.; Roh, H.-S.; Song, S.-S.; Ryoo, R.; Pang, C.; Baek, K.-H.; Kim, K.H. Cytotoxic constituents from the sclerotia of Poria cocos against human lung adenocarcinoma cells by inducing mitochondrial apoptosis. Cells 2018, 7, 116. [Google Scholar] [CrossRef] [PubMed]
- Umemura, K.; Tanino, S.; Nagatsuka, T.; Koga, J.; Iwata, M.; Nagashima, K.; Amemiya, Y. Cerebroside elicitor confers resistance to Fusarium disease in various plant species. Phytopathology 2004, 94, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Hua, W.; Miao, Y.; Chen, J.; You, Y.; Sun, C.; Yuan, L.; Xu, L. Identification and growth characterization of a cerebroside producing Termitomyces clypeatus CTM-1. Shengwu Jiagong Guocheng 2015, 13, 67–73. [Google Scholar] [CrossRef]
- Wicklow, D.T.; Joshi, B.K.; Gamble, W.R.; Gloer, J.B.; Dowd, P.F. Antifungal metabolites (monorden, monocillin IV, and cerebrosides) from Humicola fuscoatra traaen NRRL 22980, a mycoparasite of Aspergillus flavus sclerotia. Appl. Environ. Microbiol. 1998, 64, 4482–4484. [Google Scholar] [CrossRef] [PubMed]
- Koga, J. Induction of Rice Disease Resistance by Fungal Sphingolipids and Bile Acids. Am. Chem. Soc. 2009, 237, 100. [Google Scholar]
- Ui, H.; Shiomi, K.; Suzuki, H.; Hatano, H.; Morimoto, H.; Yamaguchi, Y.; Masuma, R.; Sakamoto, K.; Kita, K.; Miyoshi, H.; et al. Paecilaminol, a new NADH-fumarate reductase inhibitor, produced by Paecilomyces sp. FKI-0550. J. Antibiot. 2006, 59, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Guo, J.; Liu, W. The synthesis and property research of nanoparticles based on hydrophobic modified inulin. Shandong Huagong 2015, 44, 10–15. [Google Scholar]
- Khentoul, H.; Bensouici, C.; Reyes, F.; Albanese, D.; Sarri, D.; Ratiba, M.; Fadila, B.; Seghiri, R.; Boumaza, O. Chemical constituents and HRESI-MS analysis of an Algerian endemic plant—Verbascum atlanticum Batt—extracts and their antioxidant activity. Nat. Prod. Res. 2019, 34, 3008–3012. [Google Scholar] [CrossRef]
- Abd-Ellatif, A.E.S.; Abdel-Razek, A.S.; Hamed, A.; Soltan, M.M.; Soliman, H.S.M.; Shaaban, M. Bioactive compounds from marine Streptomyces sp.: Structure identification and biological activities. Vietnam. J. Chem. 2019, 57, 628–635. [Google Scholar] [CrossRef]
- Goncalves-de-Albuquerque, C.F.; Silva, A.R.; Burth, P.; Castro-Faria, M.V.; Castro-Faria-Neto, H.C. Acute Respiratory Distress Syndrome: Role of Oleic Acid-Triggered Lung Injury and Inflammation. Mediat. Inflamm. 2015, 2015, 1–9. [Google Scholar] [CrossRef]
- Balaz, M.; Kudlickova, Z.; Vilkova, M.; Imrich, J.; Balazova, L.; Daneu, N. Mechanochemical synthesis and isomerization of N-substituted indole-3-carboxaldehyde oximes. Molecules 2019, 24, 3347. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Yu, J.; Yao, X. Application of Indole-3-Carboxaldehyde in Preparation of Cosmetic or Drug for Treating Atopic Dermatitis. CN110368385A, 25 October 2019. China National Intellectual Property Administration, Beijing, China. [Google Scholar]
- Kim, H.; Kim, S.Y.; Sim, G.Y.; Ahn, J.-H. Synthesis of 4-Hydroxybenzoic Acid Derivatives in Escherichia coli. J. Agric. Food Chem. 2020, 68, 9743–9749. [Google Scholar] [CrossRef]
- Hurtado-Barroso, S.; Quifer-Rada, P.; Marhuenda-Munoz, M.; de Alvarenga, J.F.R.; Tresserra-Rimbau, A.; Lamuela-Raventos, R.M. Increase of 4-hydroxybenzoic, a bioactive phenolic compound, after an organic intervention diet. Antioxidants 2019, 8, 340. [Google Scholar] [CrossRef] [PubMed]
- Maia, N.J.L.; Correa, J.A.F.; Rigotti, R.T.; da Silva Junior, A.A.; Luciano, F.B. Combination of natural antimicrobials for contamination control in ethanol production. World J. Microbiol. Biotechnol. 2019, 35, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Prasad, P.; Varshney, D.; Adholeya, A. Whole genome annotation and comparative genomic analyses of bio-control fungus Purpureocillium lilacinum. BMC Genom. 2015, 16, 1004. [Google Scholar] [CrossRef]
- Khaldi, N.; Seifuddin, F.T.; Turner, G.; Haft, D.; Nierman, W.C.; Wolfe, K.H.; Fedorova, N.D. SMURF: Genomic mapping of fungal secondary metabolite clusters. Fungal Genet. Biol. 2010, 47, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Weber, T.; Blin, K.; Duddela, S.; Krug, D.; Kim, H.U.; Bruccoleri, R.; Lee, S.Y.; Fischbach, M.A.; Muller, R.; Wohlleben, W.; et al. antiSMASH 3.0-a comprehensive resource for the genome mining of biosynthetic gene clusters. Nucleic Acids Res. 2015, 43, W237–W243. [Google Scholar] [CrossRef]
- Takeda, K.; Kemmoku, K.; Satoh, Y.; Ogasawara, Y.; Shinya, K.; Dairi, T.J.A.C.B. N-Phenylacetylation and Nonribosomal Peptide Synthetases with Substrate Promiscuity for Biosynthesis of Heptapeptide Variants, JBIR-78 and JBIR-95. ACS Chem. Biol. 2017, 12, 1813. [Google Scholar] [CrossRef]
- Han, M.; Chen, J.; Qiao, Y.; Zhu, P. Advances in the nonribosomal peptide synthetases. Yaoxue Xuebao 2018, 53, 1080–1089. [Google Scholar] [CrossRef]
- Sung, C.T.; Chang, S.; Entwistle, R.; Ahn, G.; Lin, T.; Petrova, V.; Yeh, H.; Praseuth, M.B.; Chiang, Y.; Oakley, B.R.; et al. Overexpression of a three-gene conidial pigment biosynthetic pathway in Aspergillus nidulans reveals the first NRPS known to acetylate tryptophan. Fungal Genet. Biol. 2017, 101, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.A.E.; Schoppet, M.; Hansen, M.H.; Cryle, M.J. Diversity of nature’s assembly lines—recent discoveries in non-ribosomal peptide synthesis. Mol. Biosyst. 2017, 13, 9–22. [Google Scholar] [CrossRef]
- Sun, Y.-H.; Deng, Z.-X. Polyketides and combinatorial biosynthetic approaches. Zhongguo Kangshengsu Zazhi 2006, 31, 6. [Google Scholar]
- Bloudoff, K.; Fage, C.D.; Marahiel, M.A.; Schmeing, T.M. Structural and mutational analysis of the nonribosomal peptide synthetase heterocyclization domain provides insight into catalysis. Proc. Natl. Acad. Sci. USA 2017, 114, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Strieker, M.; Tanovic, A.; Marahiel, M.A. Nonribosomal peptide synthetases: Structures and dynamics. Curr. Opin. Struct. Biol. 2010, 20, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Hertweck, C. The Biosynthetic Logic of Polyketide Diversity. Angew. Chem. Int. Ed. 2009, 48, 4688–4716. [Google Scholar] [CrossRef] [PubMed]
- Schaeberle, T.F. Biosynthesis of alpha-pyrones. Beilstein J. Org. Chem. 2016, 12, 571–588. [Google Scholar] [CrossRef]
- Sun, J.; Bu, J.; Cui, G.; Ma, Y.; Zhao, H.; Mao, Y.; Zeng, W.; Guo, J.; Huang, L. Accumulation and biosynthetic of curcuminoids and terpenoids in turmeric rhizome in different development periods. Zhongguo Zhong Yao Za Zhi 2019, 44, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Hocquette, A.; Grondin, M.; Bertout, S.; Mallié, M. Les champignons des genres Acremonium, Beauveria, Chrysosporium, Fusarium, Onychocola, Paecilomyces, Penicillium, Scedosporium et Scopulariopsis responsables de hyalohyphomycoses. J. De Mycol. Médicale 2005, 15, 136–149. [Google Scholar] [CrossRef]
- Okhravi, N.; Lightman, S. Clinical manifestations, treatment and outcome of Paecilomyces lilacinus infections. Clin. Microbiol. Infect. 2007, 13, 554. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).