Discovery of New Coumarin-Based Lead with Potential Anticancer, CDK4 Inhibition and Selective Radiotheranostic Effect: Synthesis, 2D & 3D QSAR, Molecular Dynamics, In Vitro Cytotoxicity, Radioiodination, and Biodistribution Studies
Abstract
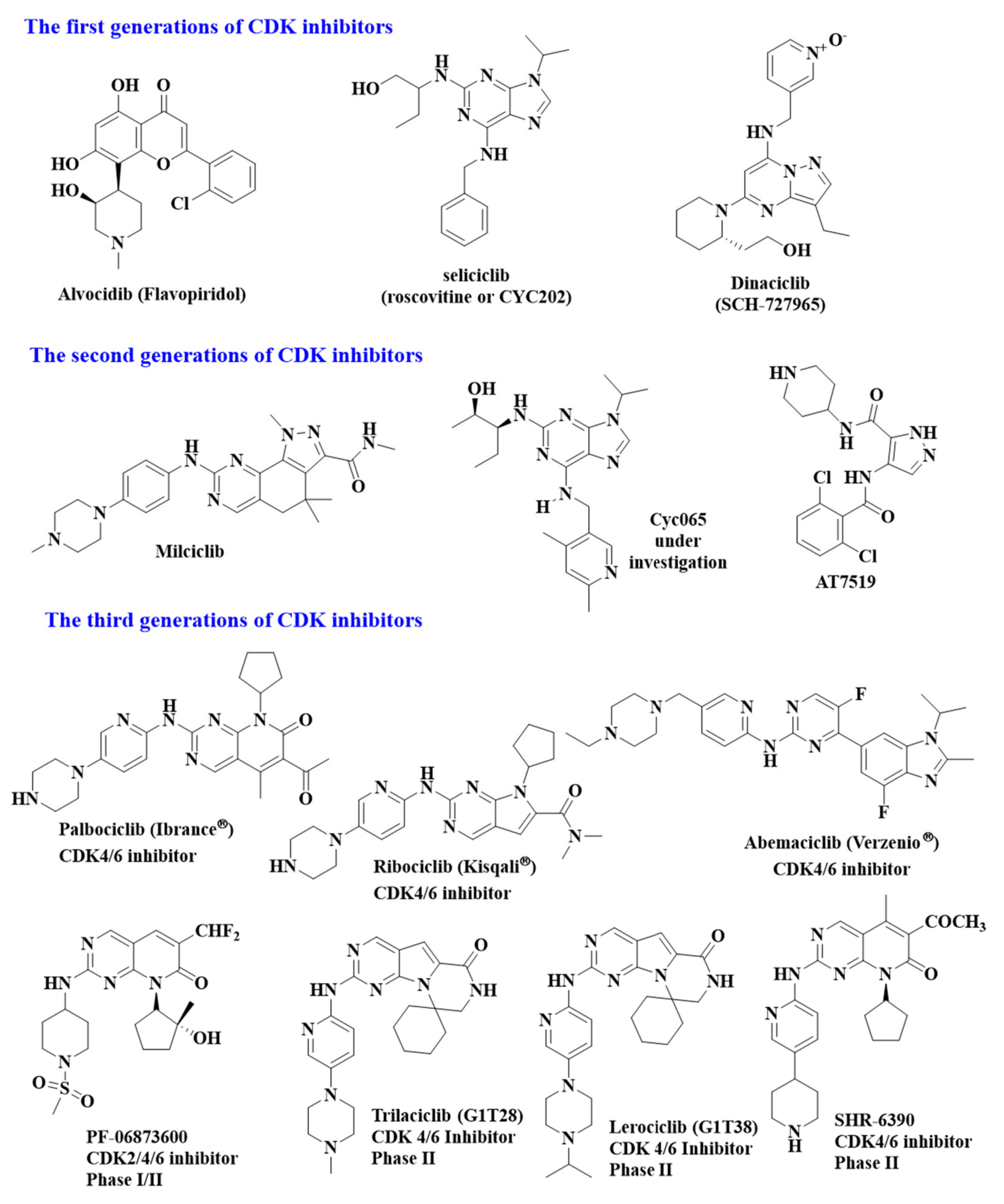
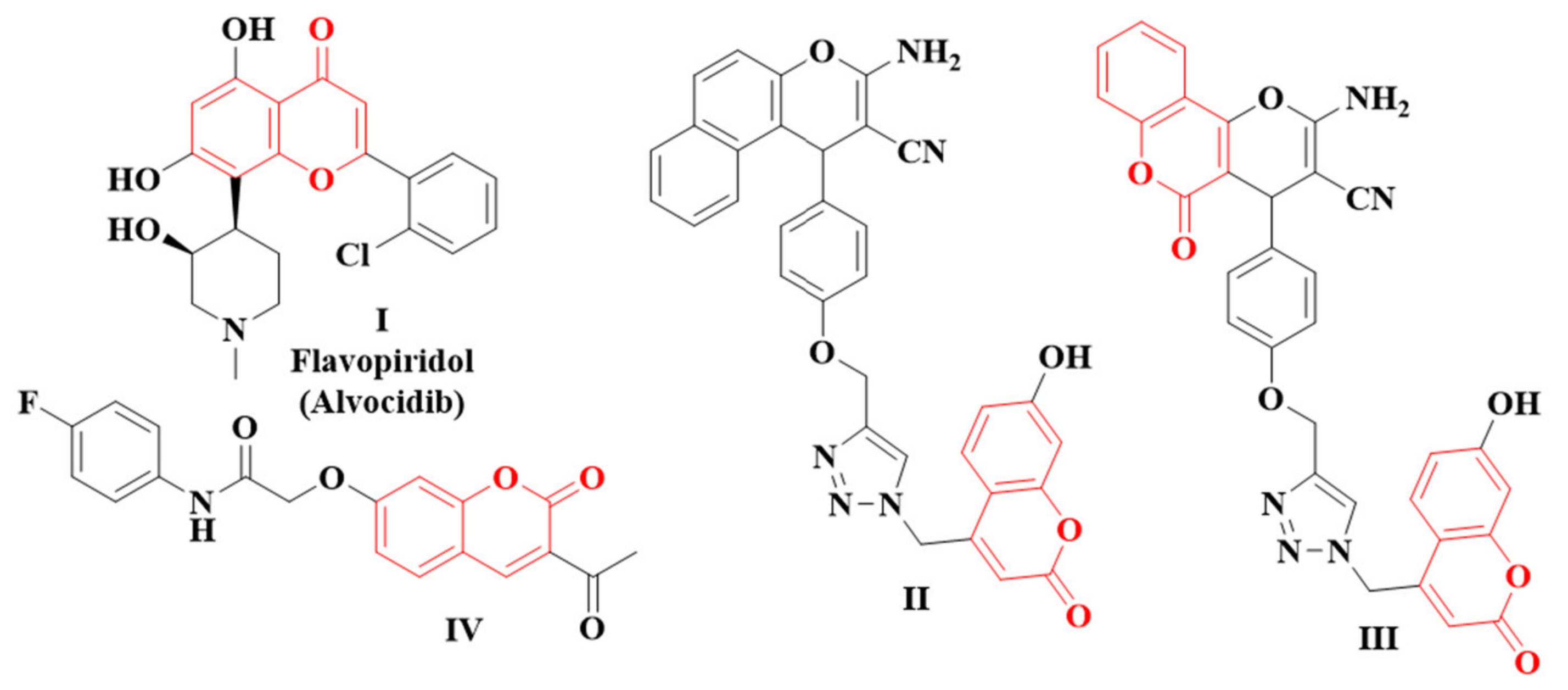
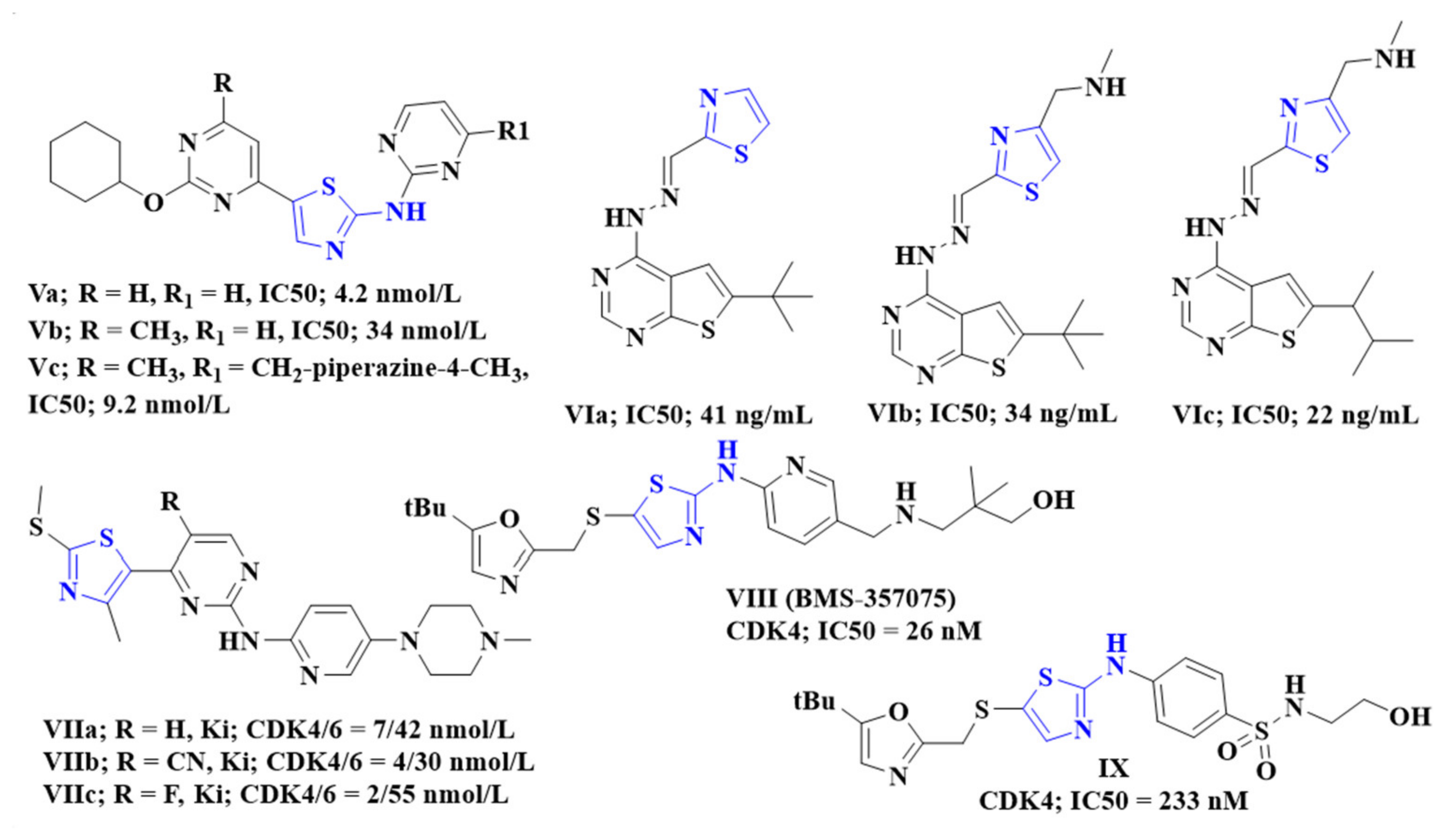
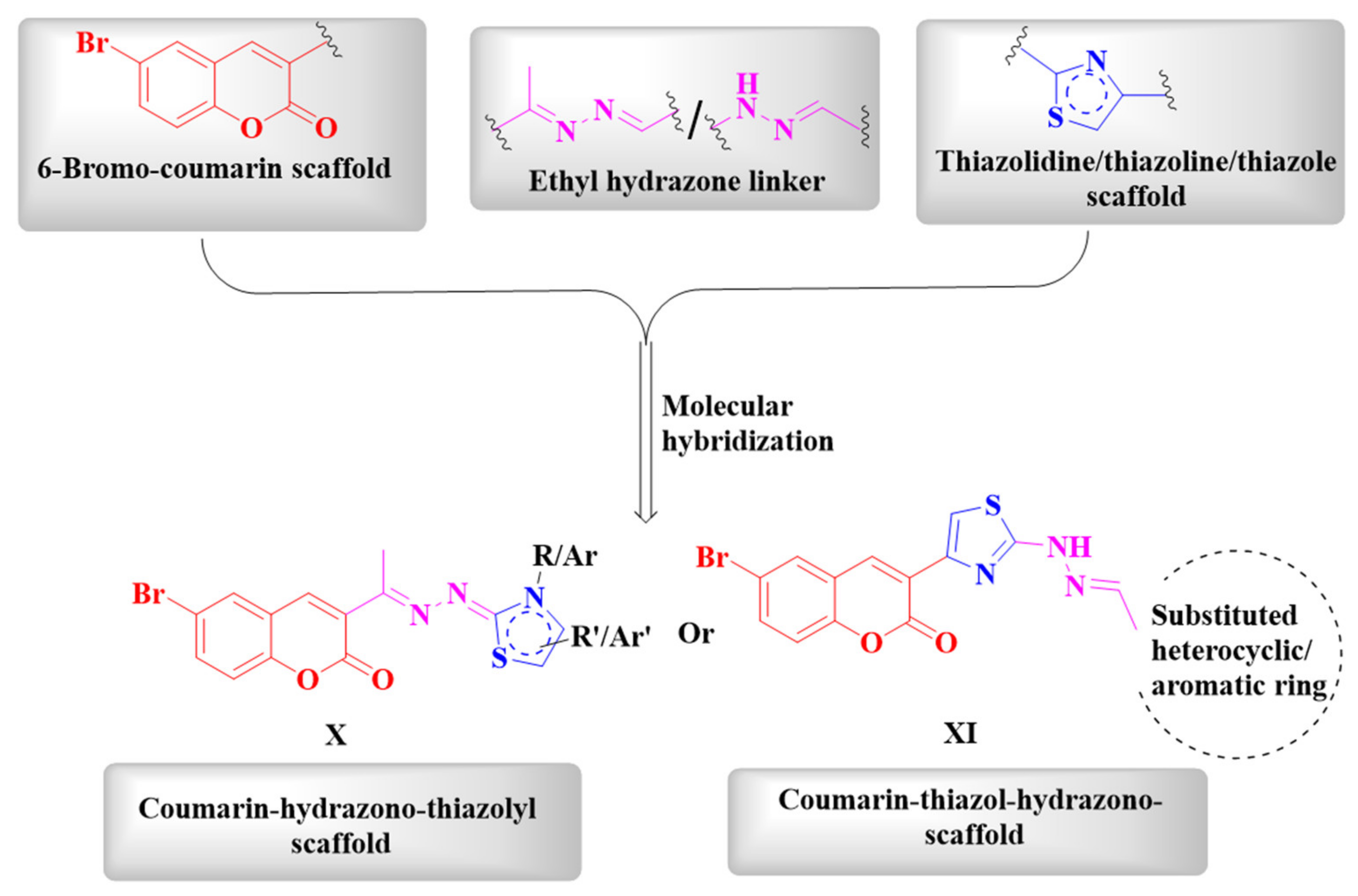
1. Introduction
2. Results and Discussion
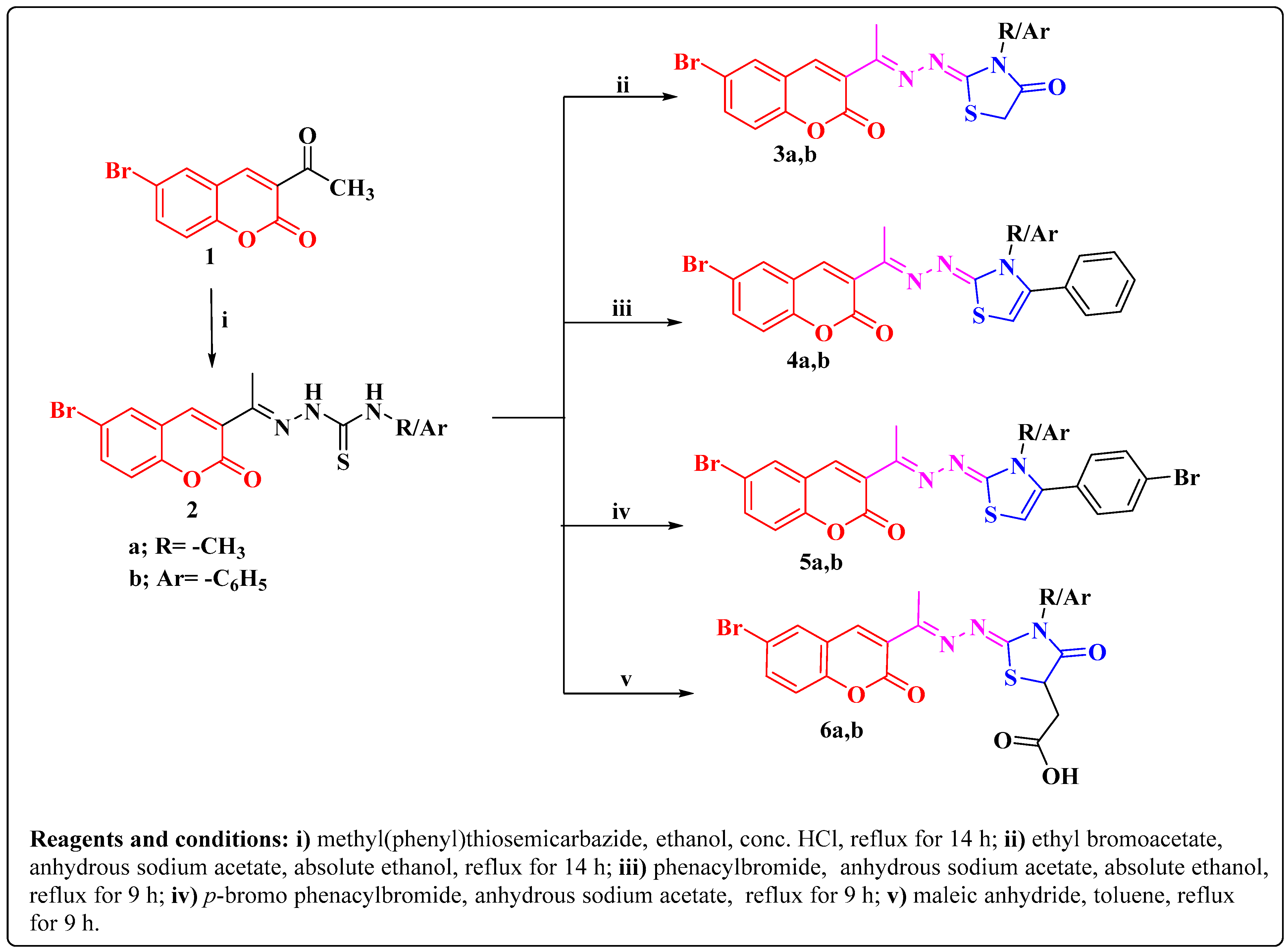
2.1. Chemistry
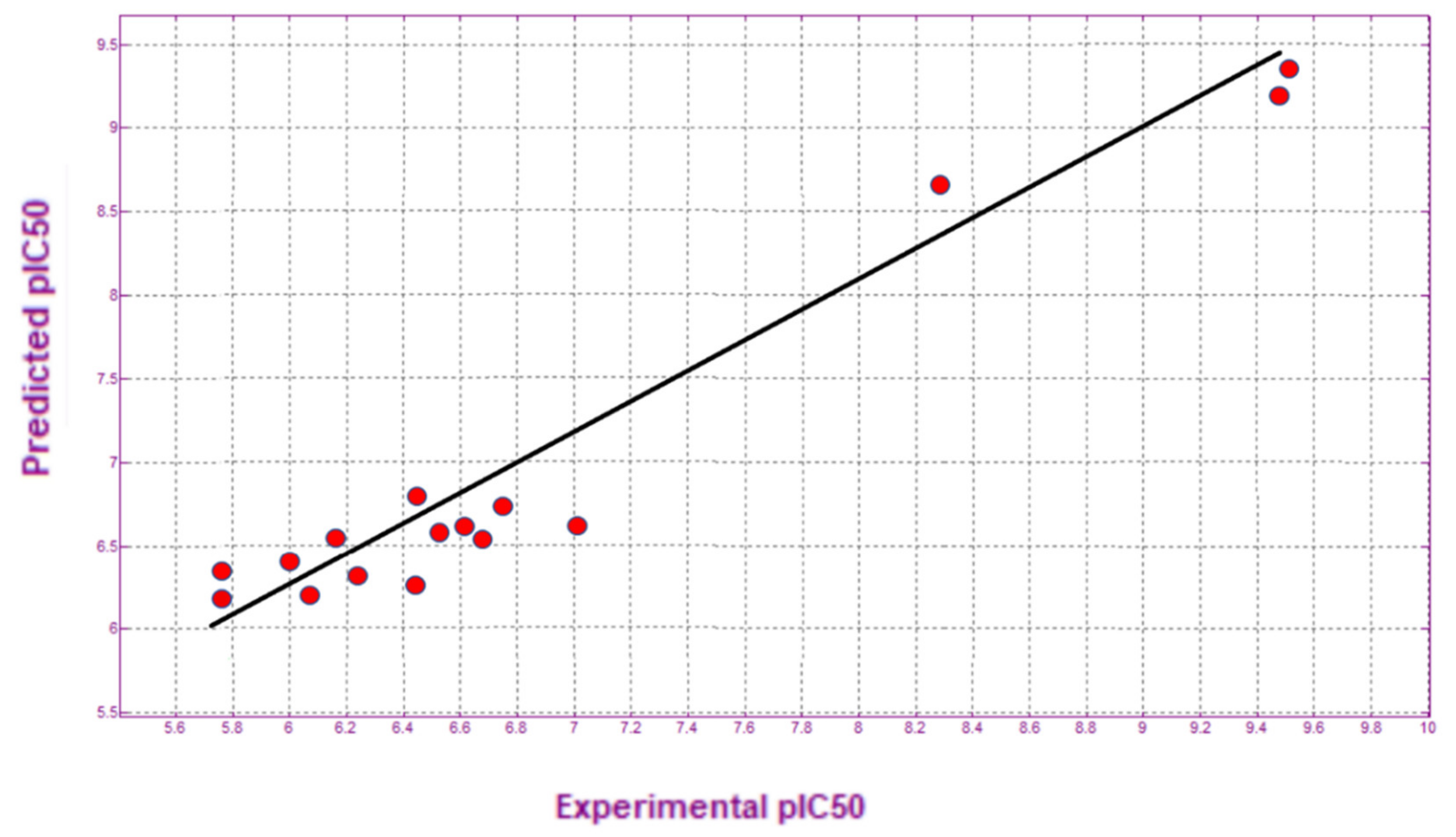
2.2. Quantitative Structure Activity Relationship model (QSAR-Model)
2.3. QSAR-Based Prediction of the Anticancer Activity of the New Compounds
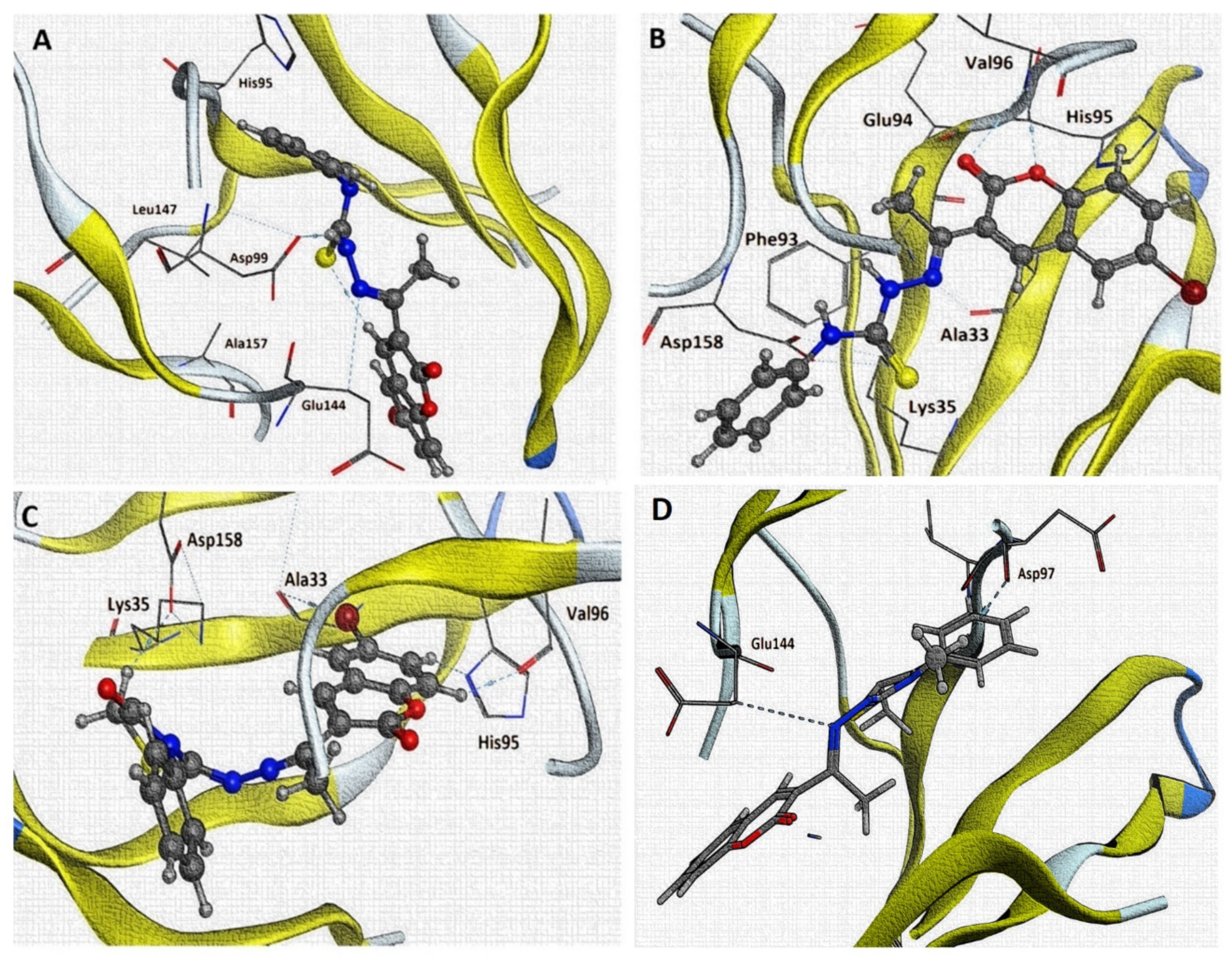
2.4. Molecular Docking Results
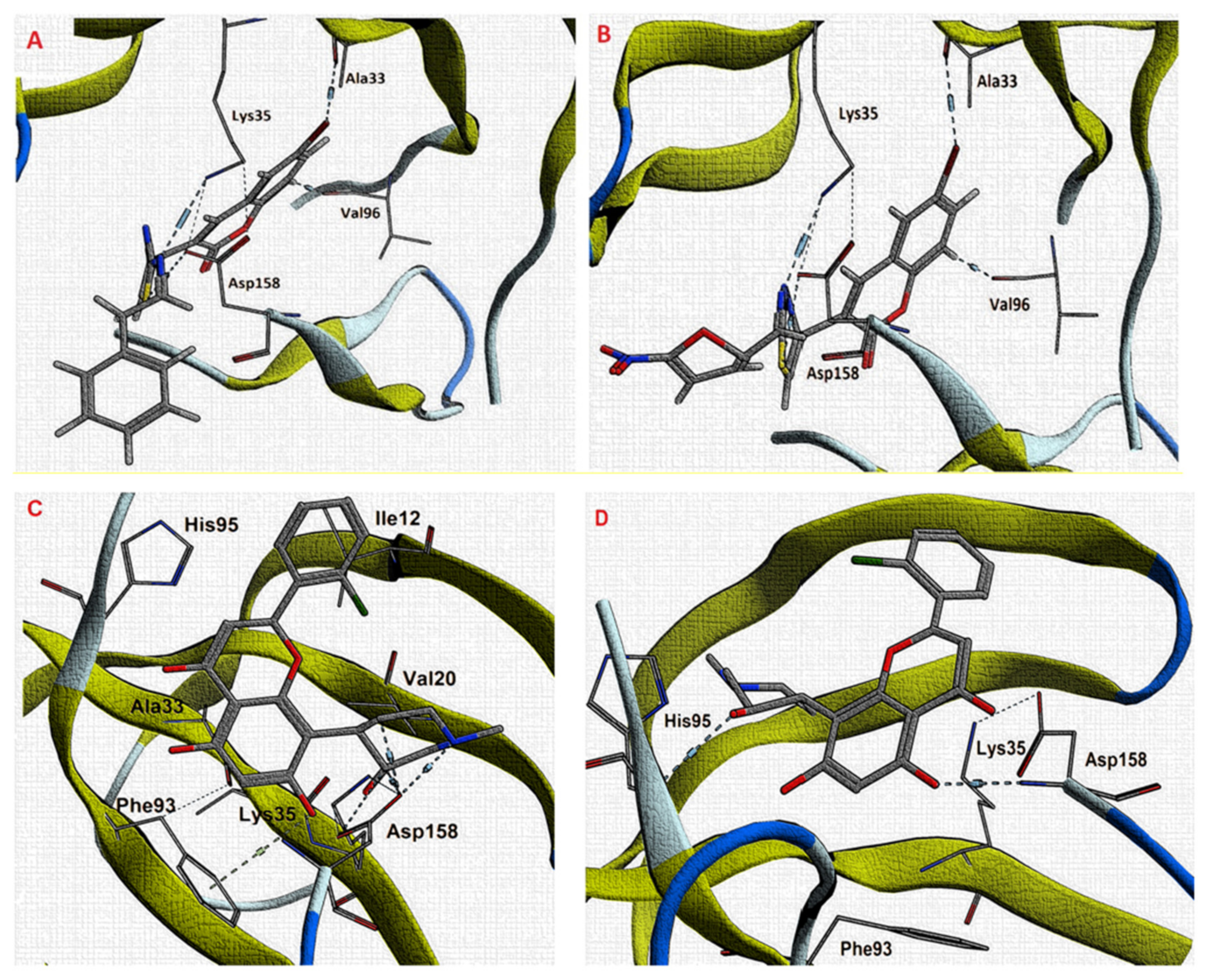
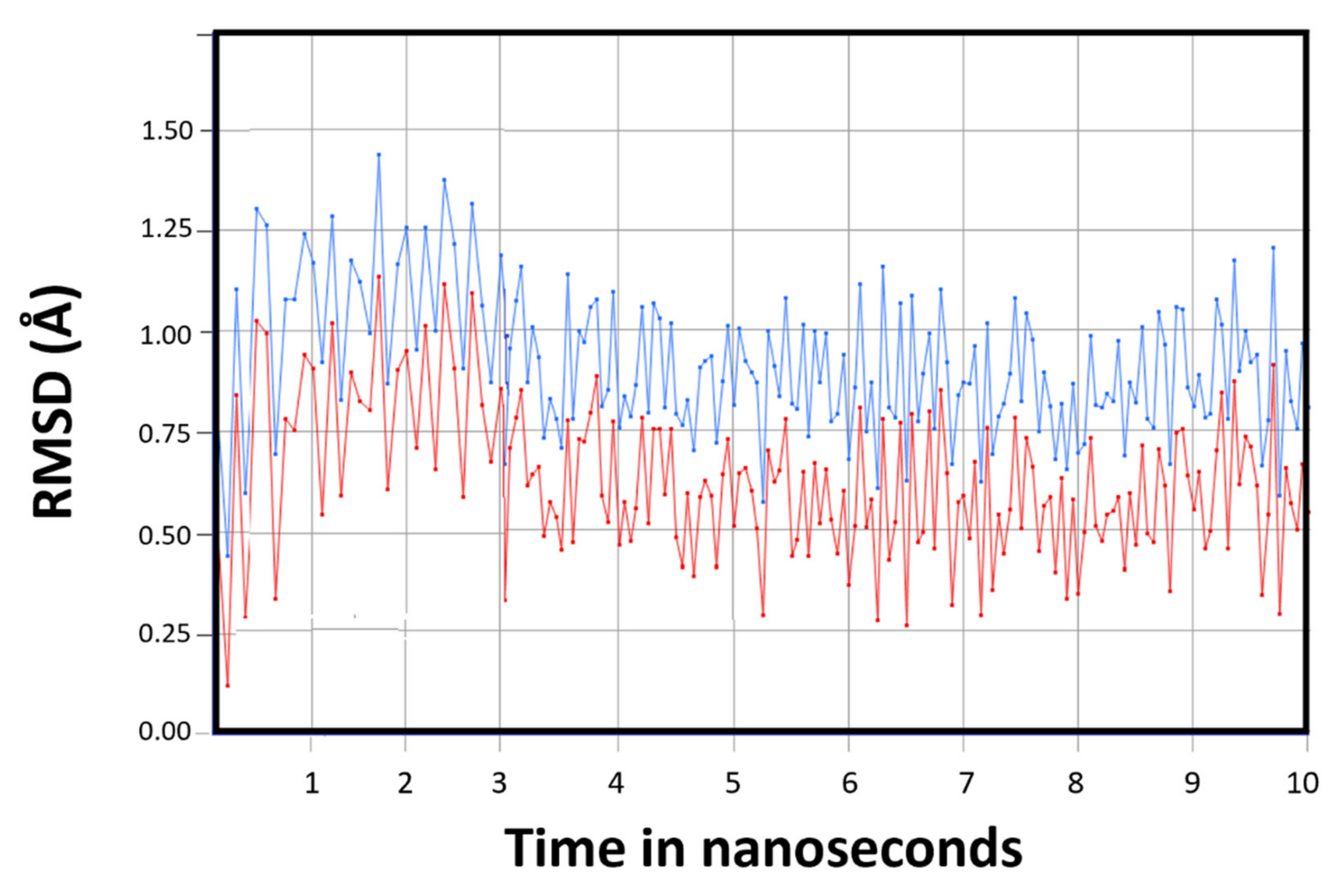
2.5. Molecular Dynamic Simulations
2.6. Biological Evaluation of the Synthesized Compounds
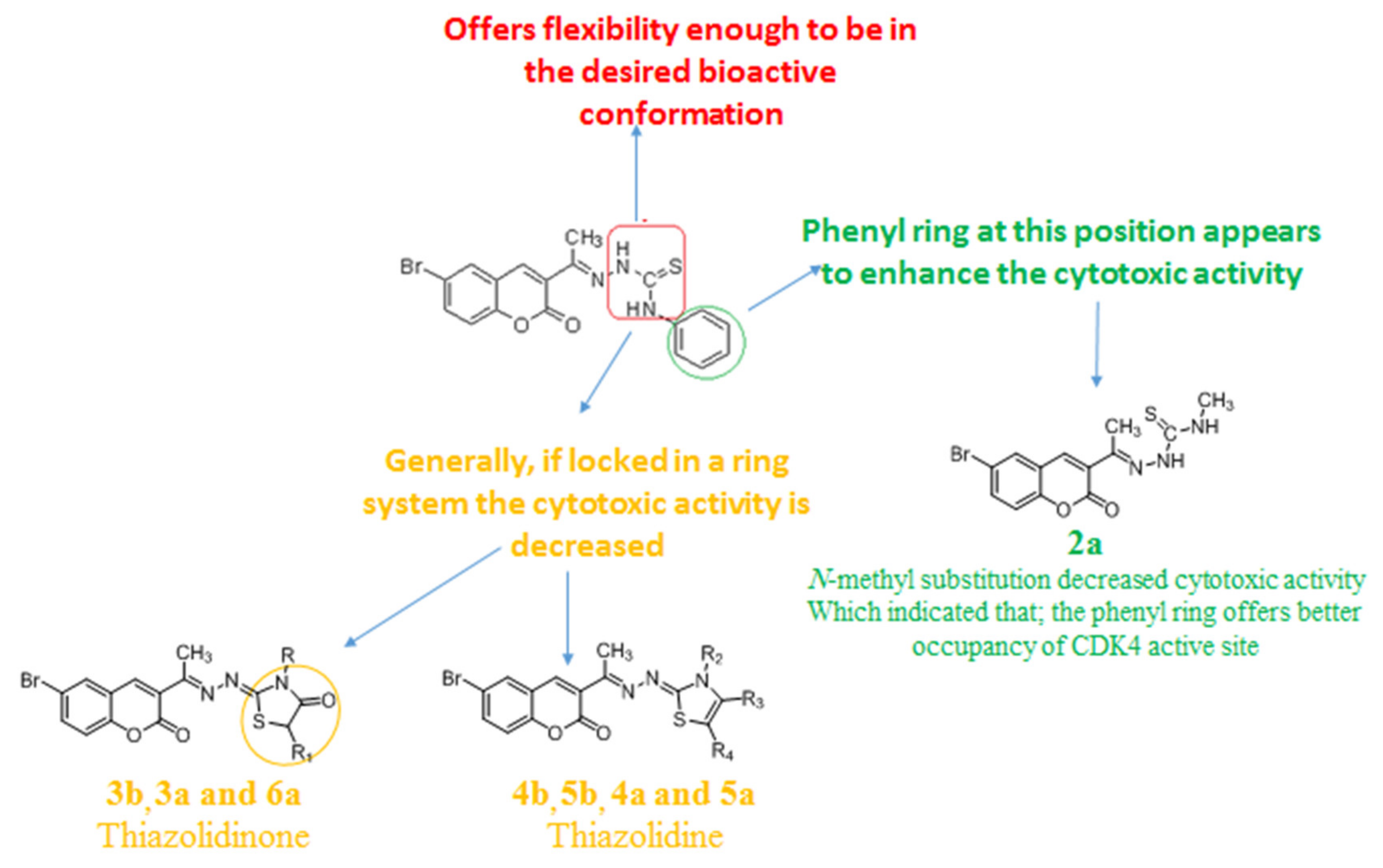
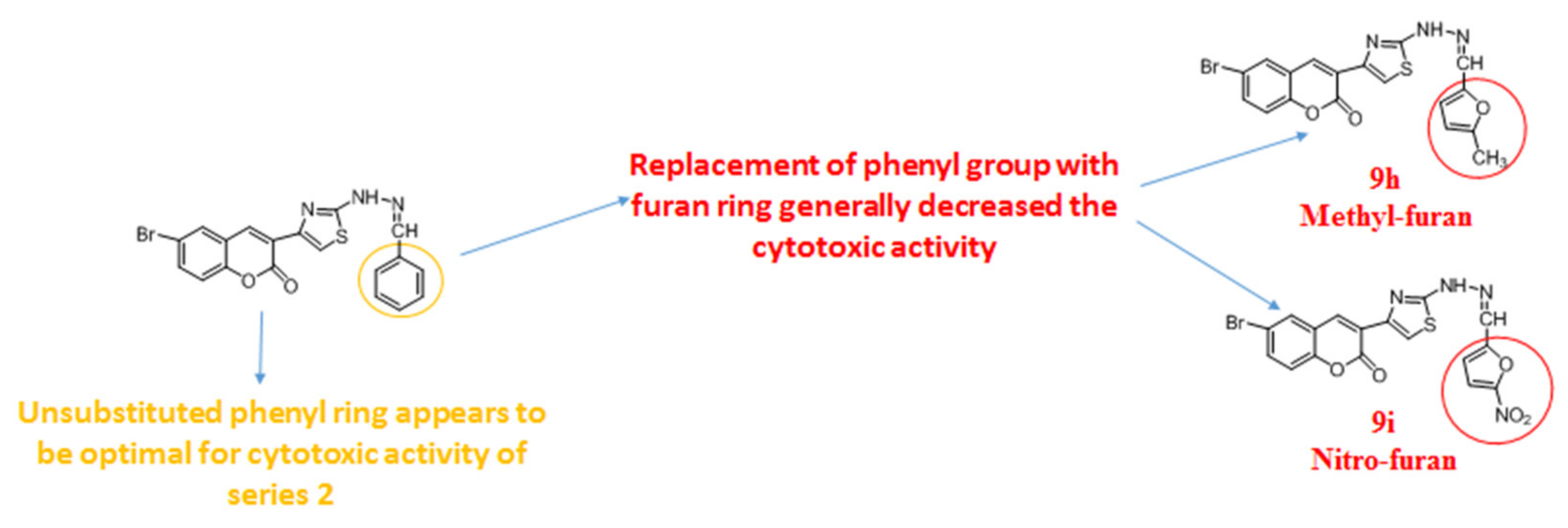
2.6.1. In Vitro Anticancer Effect and Structure Activity Relationship
2.6.2. In Vitro Activity against CDK4 Enzyme
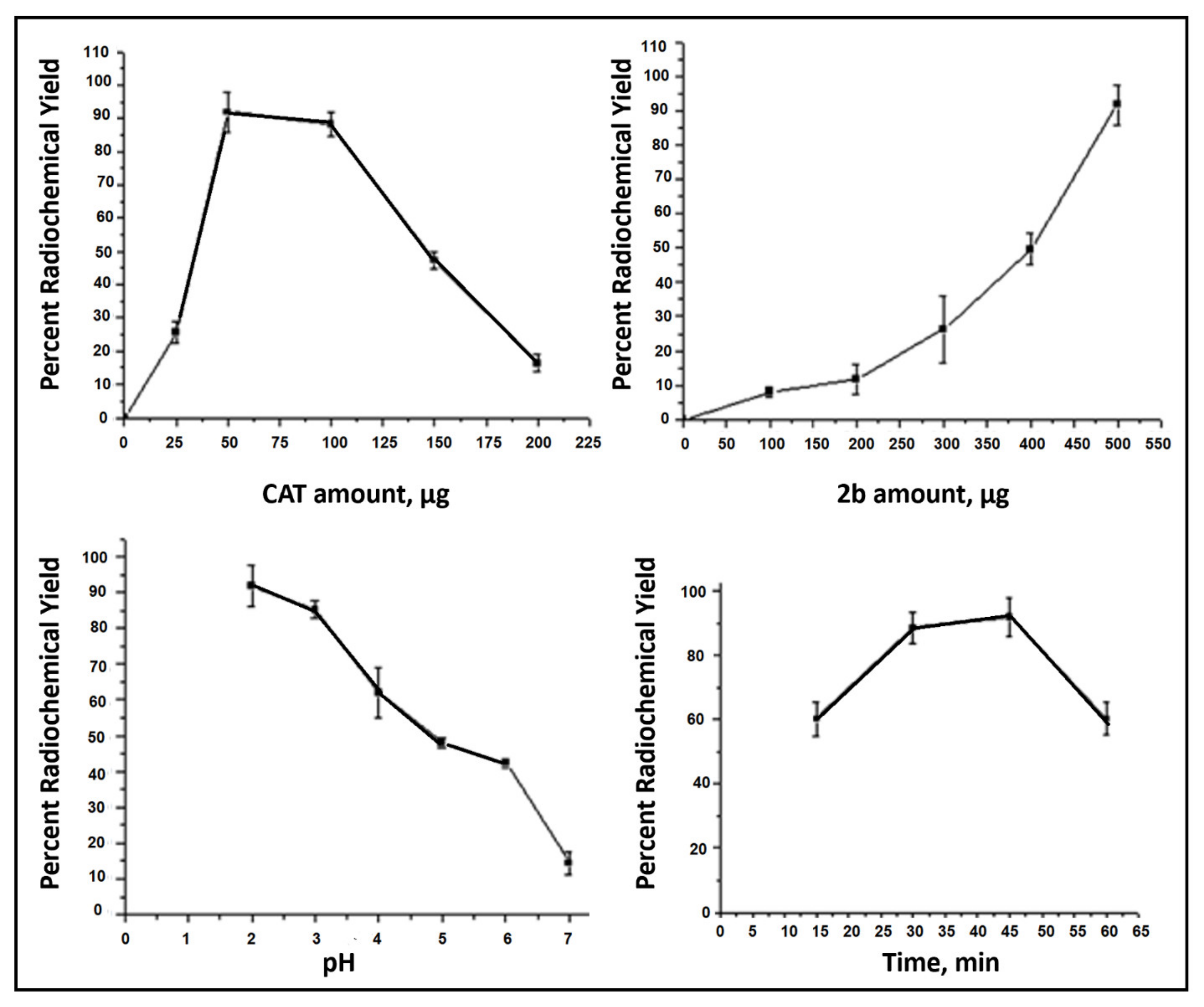
2.6.3. Radioiodination of Compound 2b
2.6.4. Chromatographic Determination of the RCY
2.6.5. Purification of 131I-2b by Column Chromatography
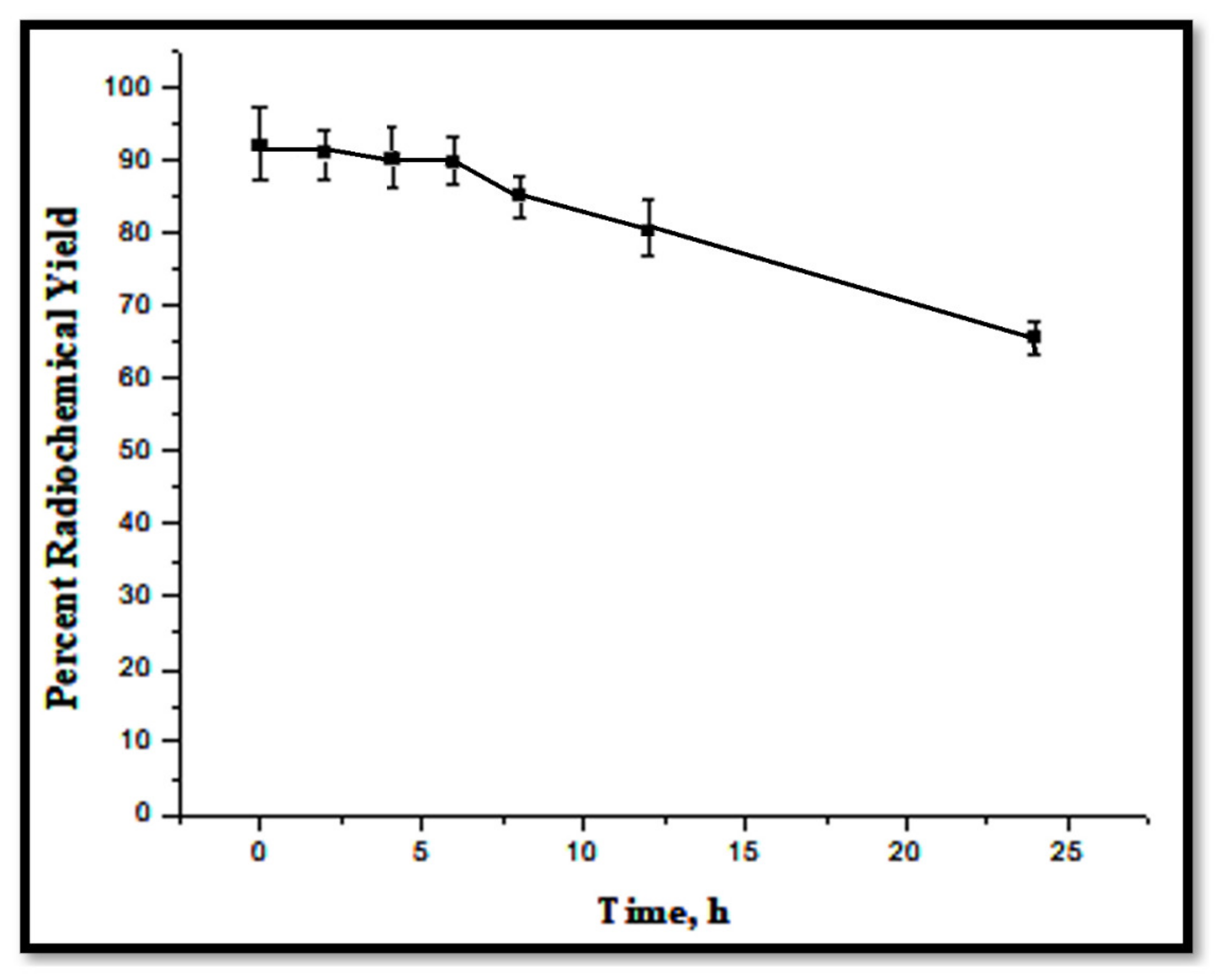
2.6.6. In Vitro Stability of 131I-2b
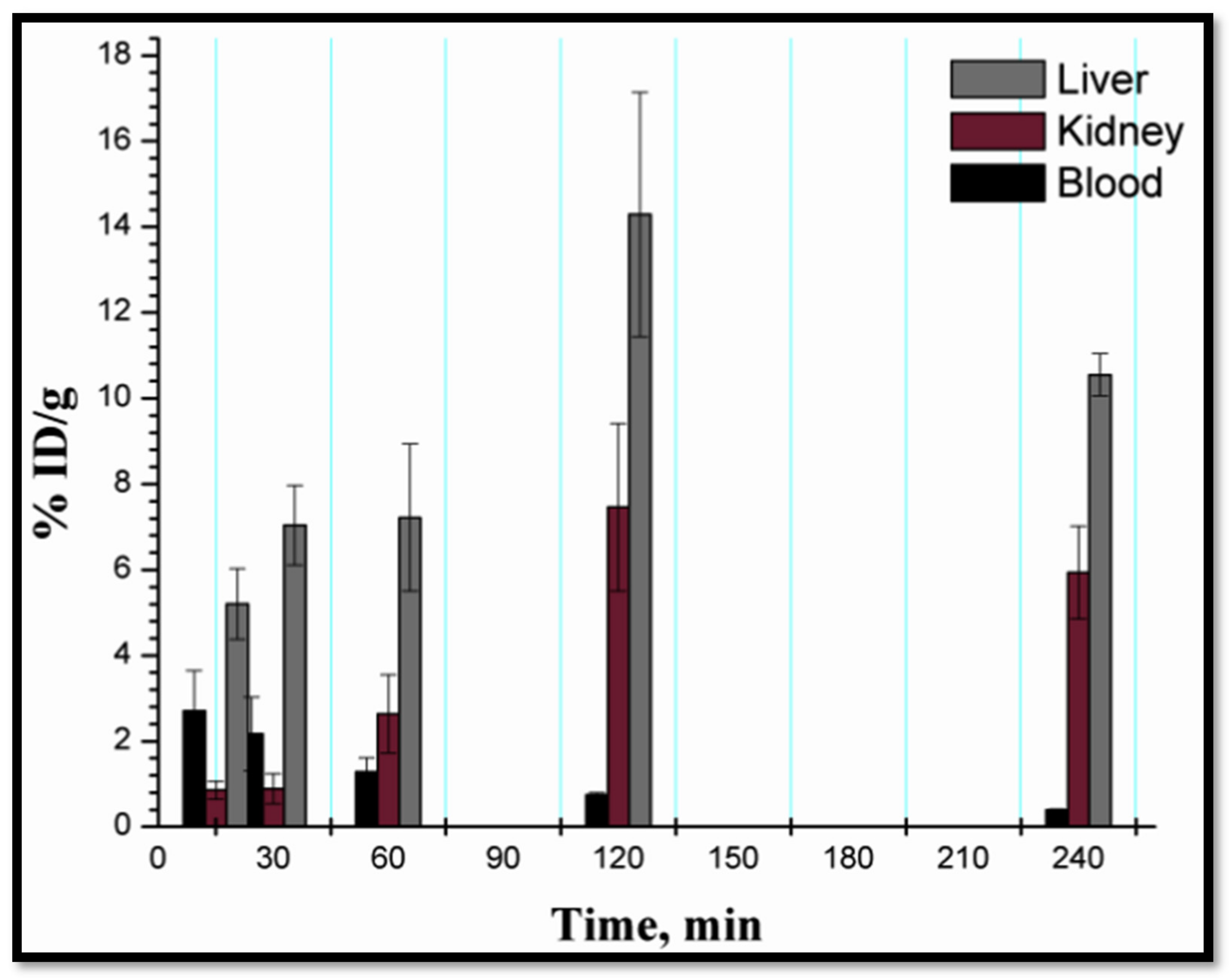
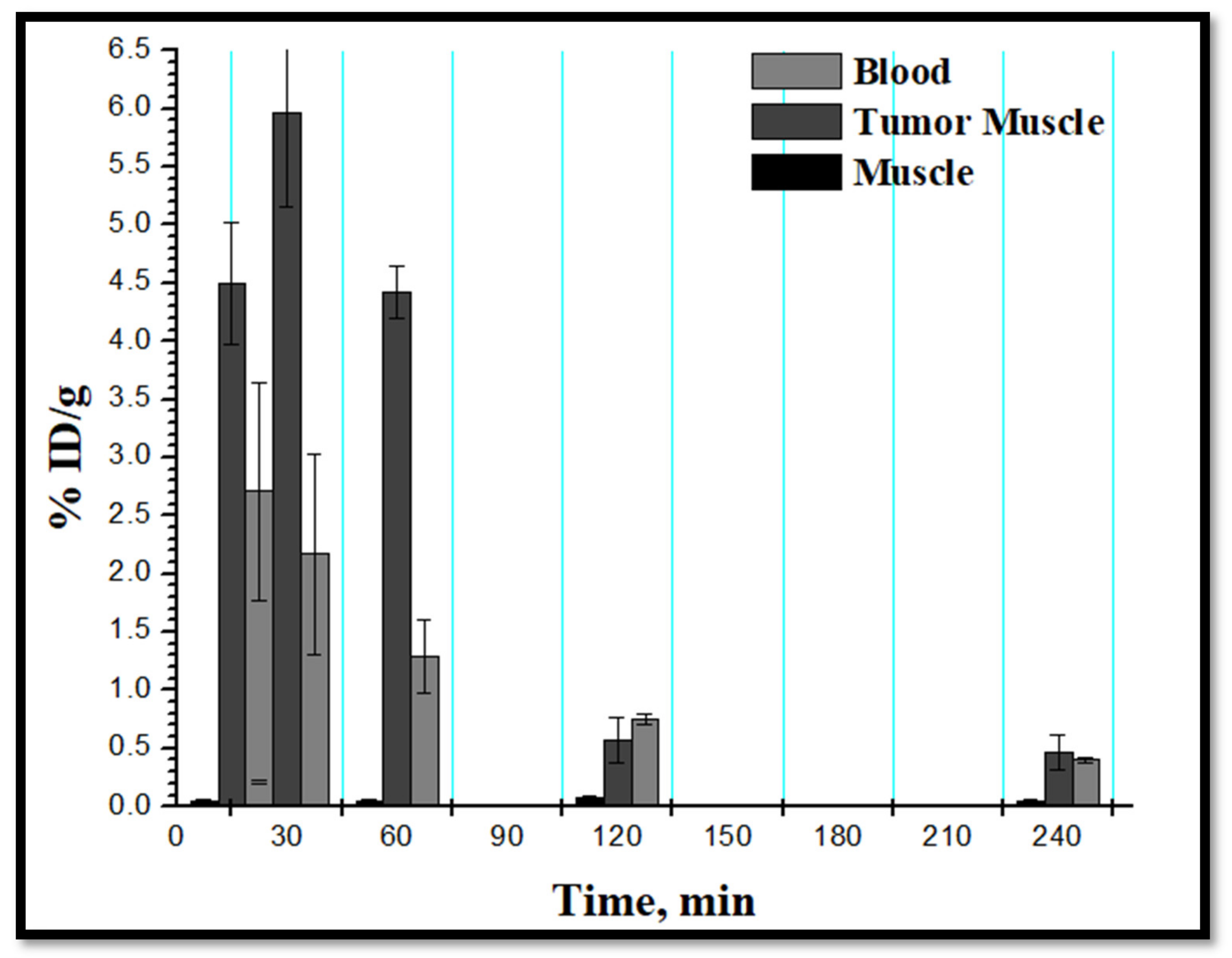
2.6.7. Biodistribution Study
3. In Silico Evaluation of ADMET
4. Materials and Methods
4.1. Chemical Synthesis
4.2. QSAR Study
4.3. Molecular Docking
4.4. Molecular Dynamic Simulations
4.5. Cytotoxic Evaluation
4.6. CDK4 Enzyme Inhibition Assay
4.7. Radioiodination of 2b
4.8. Determination of the Radiochemical Yield
4.9. Purification of 131I-2b
4.10. In-Vitro Stability Study
4.11. Biodistribution Study
4.12. In Silico Prediction of ADMET
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marak, B.N.; Dowarah, J.; Khiangte, D.; Singha, V.P. A Comprehensive Insight on the Recent Development of Cyclic Dependent Kinase Inhibitors as Anticancer Agents. Eur. J. Med. Chem. 2020, 203, 112571. [Google Scholar] [CrossRef]
- WHO. Global Cancer Report. Available online: https://www.who.int/health-topics/cancer#tab=tab_1 (accessed on 12 March 2020).
- Wan, Y.; Li, Y.; Yan, C.; Yan, M.; Tang, Z. Indole: A privileged scaffold for the design of anti-cancer agents. Eur. J. Med. Chem. 2019, 183, 111691. [Google Scholar] [CrossRef]
- Global Initiative for Childhood Cancer. Available online: https://www.who.int/news-room/detail/04-10-2018-global-initiative-for-childhood-cancer (accessed on 12 March 2020).
- Huang, Z.; Zhao, B.; Qin, Z.; Li, Y.; Wang, T.; Zhou, W.; Zheng, J.; Yang, S.; Shi, Y.; Fan, Y.; et al. Novel dual inhibitors targeting CDK4 and VEGFR2 synergistically suppressed cancer progression and angiogenesis. Eur. J. Med. Chem. 2019, 181, 111541. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.; Sicinski, P.; Hinds, P.W. Cyclins and cdks in development and cancer: A perspective. Oncogene 2005, 24, 2909–2915. [Google Scholar] [CrossRef]
- Malumbres, M.; Barbacid, M. Cell cycle, CDKs and cancer: A changing paradigm. Nat. Rev. Cancer 2009, 9, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Deng, K.; Wang, C.; Li, Y.; Wang, T.; Huang, Z.; Ma, Y.; Sun, P.; Shi, Y.; Yang, S.; et al. Novel CDKs inhibitors for the treatment of solid tumour by simultaneously regulating the cell cycle and transcription control. J. Enzym. Inhib. Med. Chem. 2020, 35, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Wells, C.I.; Vasta, J.D.; Corona, C.R.; Wilkinson, J.; Zimprich, C.A.; Ingold, M.R.; Pickett, J.E.; Drewry, D.H.; Pugh, K.M.; Schwinn, M.K.; et al. Quantifying CDK inhibitor selectivity in live cells. Nat. Commun. 2020, 11, 1–11. [Google Scholar] [CrossRef]
- Asghar, U.; Witkiewicz, A.K.; Turner, N.C.; Knudsen, E.S. The history and future of targeting cyclin-dependent kinases in cancer therapy. Nat. Rev. Drug Discov. 2015, 14, 130–146. [Google Scholar] [CrossRef]
- Peyressatre, M.; Prével, C.; Pellerano, M.; Morris, M.C. Targeting Cyclin-Dependent Kinases in Human Cancers: From Small Molecules to Peptide Inhibitors. Cancers 2015, 7, 179–237. [Google Scholar] [CrossRef]
- Ding, L.; Cao, J.; Lin, W.; Chen, H.; Xiong, X.; Ao, H.; Yu, M.; Lin, J.; Cui, Q. The Roles of Cyclin-Dependent Kinases in Cell-Cycle Progression and Therapeutic Strategies in Human Breast Cancer. Int. J. Mol. Sci. 2020, 21, 1960. [Google Scholar] [CrossRef]
- Kalra, S.; Joshi, G.; Munshi, A.; Kumar, R. Structural insights of cyclin dependent kinases: Implications in design of selective inhibitors. Eur. J. Med. Chem. 2017, 142, 424–458. [Google Scholar] [CrossRef]
- Harbour, J.; Luo, R.X.; Santi, A.D.; A Postigo, A.; Dean, D.C. Cdk Phosphorylation Triggers Sequential Intramolecular Interactions that Progressively Block Rb Functions as Cells Move through G1. Cell 1999, 98, 859–869. [Google Scholar] [CrossRef]
- Abdel Latif, N.A.; Batran, R.Z.; Khedr, M.A.; Abdalla, M.M. 3-Substituted-4-hydroxycoumarin as a new scaffold with potent CDK inhibition and promising anticancer effect: Synthesis, molecular modeling and QSAR studies. Bioorg. Chem. 2016, 67, 116–129. [Google Scholar] [CrossRef]
- Sherr, C.J.; Beach, D.H.; Shapiro, G.I. Targeting CDK4 and CDK6: From Discovery to Therapy. Cancer Discov. 2016, 6, 353–367. [Google Scholar] [CrossRef]
- Lim, J.S.; Turner, N.C.; Yap, T.A. CDK4/6 inhibitors: Promising opportunities beyond breast cancer. Cancer Discov. 2016, 6, 697–699. [Google Scholar] [CrossRef]
- Van Arsdale, T.; Bosho, C.; Arndt, K.T.; Abraham, R.T. Molecular pathways: Targeting the cyclin D–CDK4/6 axis for cancer treatment. Clin. Cancer Res. 2015, 21, 2905–2910. [Google Scholar] [CrossRef]
- Parylo, S.; Vennepureddy, A.; Dhar, V.; Patibandla, P.; Sokolo, A. Role of cyclin-dependent kinase 4/6 inhibitors in the current and future eras of cancer treatment. J. Oncol. Pharm. Pract. 2019, 25, 110–129. [Google Scholar] [CrossRef]
- Vinay, S.; Mohd, S.M.U.; Singh, J.S.; Nayan, S.B.; Venkatesan, J.; Bhabatosh, C. Cink4T, a quinazolinone-based dual inhibitor of Cdk4 and tubulin polymerization, identified via ligand-based virtual screening, for efficient anticancer therapy. Eur. J. Med. Chem. 2019, 165, 115–132. [Google Scholar]
- Sánchez-Martínez, C.; Lallena, M.J.; Sanfeliciano, S.G.; de Dios, A. Cyclin dependent kinase (CDK) inhibitors as anticancer drugs: Recent advances (2015–2019). Bioorg. Med. Chem. Lett. 2019, 29, 126637. [Google Scholar] [CrossRef]
- Losiewicz, M.D.; Carlson, B.A.; Kaur, G.; Sausville, E.A.; Worland, P.J. Potent inhibition of cdk2 kinase activity by the flavonoid L86-8275. Biophys. Res. Commun. 1994, 201, 589–595. [Google Scholar] [CrossRef]
- Meijer, L.; Borgne, A.; Mulner, O.; Chong, J.P.J.; Blow, J.J.; Inagaki, N.; Inagaki, M.; Delcros, J.-G.; Moulinoux, J.-P. Biochemical and Cellular Effects of Roscovitine, a Potent and Selective Inhibitor of the Cyclin-Dependent Kinases cdc2, cdk2 and cdk5. Eur. J. Biochem. 1997, 243, 527–536. [Google Scholar] [CrossRef]
- Brasca, M.G.; Amboldi, N.; Ballinari, D.; Cameron, A.; Casale, E.; Cervi, G.; Colombo, M.; Colotta, F.; Croci, V.; D’Alessio, R.; et al. Identification of N,1,4,4-Tetramethyl-8-{[4-(4-methylpiperazin-1-yl)phenyl]amino}-4,5-dihydro-1H-pyrazolo[4,3-h]quinazoline-3-carboxamide (PHA-848125), a Potent, Orally Available Cyclin Dependent Kinase Inhibitor. J. Med. Chem. 2009, 52, 5152–5163. [Google Scholar] [CrossRef]
- Parry, D.; Guzi, T.; Shanahan, F.; Davis, N.; Prabhavalkar, D.; Wiswell, D.; Seghezzi, W.; Paruch, K.; Dwyer, M.P.; Doll, R.; et al. Dinaciclib (SCH 727965), a Novel and Potent Cyclin-Dependent Kinase Inhibitor. Mol. Cancer Ther. 2010, 9, 2344–2353. [Google Scholar] [CrossRef]
- Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Cyc065#section=Information-Sources (accessed on 1 April 2021).
- Squires, M.S.; Feltell, R.E.; Wallis, N.G.; Lewis, E.J.; Smith, D.-M.; Cross, D.M.; Lyons, J.F.; Thompson, N.T. Biological characterization of AT7519, a small-molecule inhibitor of cyclin-dependent kinases, in human tumor cell lines. Mol. Cancer Ther. 2009, 8, 324–332. [Google Scholar] [CrossRef]
- O’Leary, B.; Finn, R.S.; Turner, N.C. Treating cancer with selective CDK4/6 inhibitors. Nat Rev. Clin. Oncol. 2016, 13, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Toogood, P.L.; Harvey, P.J.; Repine, J.T.; Sheehan, D.J.; VanderWel, S.N.; Zhou, H.; Keller, P.R.; McNamara, D.J.; Sherry, D.; Zhu, T.; et al. Discovery of a potent and selective inhibitor of cyclin dependent kinase 4/6. J. Med. Chem. 2005, 48, 2388–2406. [Google Scholar] [CrossRef]
- Rader, J.; Russell, M.R.; Hart, L.S.; Nakazawa, M.S.; Belcastro, L.T.; Martinez, D.; Li, Y.; Carpenter, E.L.; Attiyeh, E.F.; Diskin, S.J.; et al. Dual CDK4/CDK6 Inhibition Induces Cell-Cycle Arrest and Senescence in Neuroblastoma. Clin. Cancer Res. 2013, 19, 6173–6182. [Google Scholar] [CrossRef]
- Finn, R.S.; Dering, J.; Conklin, D.; Kalous, O.; Cohen, D.J.; Desai, A.J.; Ginther, C.; Atefi, M.; Chen, I.; Fowst, C.; et al. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res. 2009, 11, R77. [Google Scholar] [CrossRef]
- Baughn, L.B.; Di Liberto, M.; Wu, K.; Toogood, P.L.; Louie, T.; Gottschalk, R.; Niesvizky, R.; Cho, H.; Ely, S.; Moore, M.A.; et al. A novel orally active small molecule potently induces G1 arrest in primary myeloma cells and prevents tumor growth by specific inhibition of Cdk4/6. Blood 2006, 108, 113a–114a. [Google Scholar] [CrossRef]
- Im, S.-A.; Mukai, H.; Park, I.H.; Masuda, N.; Shimizu, C.; Kim, S.-B.; Im, Y.-H.; Ohtani, S.; Bartlett, C.H.; Lu, D.R.; et al. Palbociclib Plus Letrozole as First-Line Therapy in Postmenopausal Asian Women with Metastatic Breast Cancer: Results From the Phase III, Randomized PALOMA-2 Study. J. Glob. Oncol. 2019, 5, 1–19. [Google Scholar] [CrossRef]
- Meattini, I.; Desideri, I.; Scotti, V.; Simontacchi, G.; Livi, L. Ribociclib plus letrozole and concomitant palliative radiotherapy for metastatic breast cancer. Breast 2018, 42, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Heptinstall, A.B.; Adiyasa, I.; Cano, C.; Hardcastle, I.R. Recent advances in CDK inhibitors for cancer therapy. Futur. Med. Chem. 2018, 10, 1369–1388. [Google Scholar] [CrossRef] [PubMed]
- Wiernik, P.H. Alvocidib (flavopiridol) for the treatment of chronic lymphocytic leukemia. Expert Opin. Investig. Drugs 2016, 25, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Shankar, E.P.S.; Bahulayan, D. Chemistry, chemical biology and photophysics of certain new chromene–triazole–coumarin triads as fluorescent inhibitors of CDK2 and CDK4 induced cancers. N. J. Chem. 2019, 43, 13863–13872. [Google Scholar] [CrossRef]
- Umar, S.; Soni, R.; Durgapal, S.D.; Soman, S.; Balakrishnan, S. A synthetic coumarin derivative (4-flourophenylacetamide-acetyl coumarin) impedes cell cycle at G0/G1 stage, induces apoptosis, and inhibits metastasis via ROS-mediated p53 and AKT signaling pathways in A549 cells. J. Biochem. Mol. Toxicol. 2020, 34, e22553. [Google Scholar] [CrossRef] [PubMed]
- Farghaly, T.A.; Masaret, G.S.; Muhammad, Z.A.; Harras, M.F. Discovery of thiazole-based-chalcones and 4-hetarylthiazoles as potent anticancer agents: Synthesis, docking study and anticancer activity. Bioorganic Chem. 2020, 98, 103761. [Google Scholar] [CrossRef] [PubMed]
- Shimamura, T.; Shibata, J.; Kurihara, H.; Mita, T.; Otsuki, S.; Sagara, T.; Hirai, H.; Iwasawa, Y. Identification of potent 5-pyrimidinyl-2-aminothiazole CDK4, 6 inhibitors with significant selectivity over CDK1, 2, 5, 7, and 9. Bioorganic Med. Chem. Lett. 2006, 16, 3751–3754. [Google Scholar] [CrossRef]
- Horiuchi, T.; Takeda, Y.; Haginoya, N.; Miyazaki, M.; Nagata, M.; Kitagawa, M.; Akahane, K.; Uoto, K. Discovery of Novel Thieno[2,3-d]pyrimidin-4-yl Hydrazone-Based Cyclin-Dependent Kinase 4 Inhibitors: Synthesis, Biological Evaluation and Structure-Activity Relationships. Chem. Pharm. Bull. 2011, 59, 991–1002. [Google Scholar] [CrossRef] [PubMed]
- Tadesse, S.; Zhu, G.; Mekonnen, L.B.; Lenjisa, J.L.; Yu, M.; Brown, M.P.; Wang, S. A novel series of N-(pyridin-2-yl)-4-(thiazol-5-yl)pyrimidin-2-amines as highly potent CDK4/6 inhibitors. Future Med. Chem. 2017, 9, 1495–1506. [Google Scholar] [CrossRef]
- Tadesse, S.; Bantie, L.; Tomusange, K.; Yu, M.; Islam, S.; Bykovska, N.; Noll, B.; Zhu, G.; Li, P.; Lam, F.; et al. Discovery and pharmacological characterization of a novel series of highly selective inhibitors of cyclin-dependent kinases 4 and 6 as anticancer agents. Br. J. Pharmacol. 2018, 175, 2399–2413. [Google Scholar] [CrossRef]
- Misra, R.N.; Xiao, H.-Y.; Williams, D.K.; Kim, K.S.; Lu, S.; Keller, K.A.; Mulheron, J.G.; Batorsky, R.; Tokarski, J.S.; Sack, J.S.; et al. Synthesis and biological activity of N-aryl-2-aminothiazoles: Potent pan inhibitors of cyclin-dependent kinases. Bioorganic Med. Chem. Lett. 2004, 14, 2973–2977. [Google Scholar] [CrossRef]
- Al-Warhi, T.; El Kerdawy, A.M.; Aljaeed, N.; Ismael, O.E.; Ayyad, R.R.; Eldehna, W.M.; Abdel-Aziz, H.A.; Al-Ansary, G.H. Synthesis, Biological Evaluation and In Silico Studies of Certain Oxindole–Indole Conjugates as Anticancer CDK Inhibitors. Molecules 2020, 25, 2031. [Google Scholar] [CrossRef]
- Ding, Z.; Zhou, M.; Zeng, C. Recent advances in isatin hybrids as potential anticancer agents. Arch. Pharm. 2020, 353, e1900367. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Karima, S.S.; Syama, Y.M.; El Kerdawy, A.M.; Abdelghany, T.M. New thiazol-hydrazono-coumarin hybrids targeting human cervical cancer cells: Synthesis, CDK2 inhibition, QSAR and molecular docking studies. Bioorg. Chem. 2019, 86, 80–96. [Google Scholar] [CrossRef]
- Nasr, T.; Bondock, S.; Youns, M. Anticancer activity of new coumarin substituted hydrazide–hydrazone derivatives. Eur. J. Med. Chem. 2014, 76, 539–548. [Google Scholar] [CrossRef]
- Motaleb, M.A.; Ibrahim, I.T.; Sarhan, M.O.; Zaghary, W.A. Radioiodination and biological distribution of a new s -triazine derivative for tumor uptake evaluation. J. Label. Compd. Radiopharm. 2018, 61, 1058–1068. [Google Scholar] [CrossRef]
- Liu, J.; Wu, F.; Chen, L.; Zhao, L.; Zhao, Z.; Wang, M.; Lei, S. Biological evaluation of coumarin derivatives as mushroom tyrosinase inhibitors. Food Chem. 2012, 135, 2872–2878. [Google Scholar] [CrossRef] [PubMed]
- Kasumbwe, K.; Venugopala, K.N.; Mohanlall, V.; Odhav, B. Antimicrobial and antioxidant activities of substituted halogenated coumarins. J. Med. Plants Res. 2014, 8, 274–281. [Google Scholar] [CrossRef]
- Chopra, D.; Venugopal, K.N.; Jayashree, B.S.; Row, T.N.G. 3-Acetyl-6-chloro-2H-chromen-2-one. Acta Crystallogr. Sect. E Struct. Rep. Online 2006, 62, o2310–o2312. [Google Scholar] [CrossRef]
- Venugopala, K.N.; Jayashree, B.S.; Attimarad, M. Synthesis and evaluation of some substituted 2-arylaminocoumarinylthiazoles as potential NSAIDs. Asian J. Chem. 2004, 16, 872–876. [Google Scholar]
- Veerabhadraia, U. Synthesis of some 2-(arylamino)-5-heteroaryl-6H-1,3,4-thiadiazines. Part VI J. Indian Chem. Soc. 1990, 67, 81–82. [Google Scholar]
- Chimenti, F.; Bolasco, A.; Secci, D.; Chimenti, P.; Granese, A.; Carradori, S.; Yáñez, M.; Orallo, F.; Ortuso, F.; Alcaro, S. Investigations on the 2-thiazolylhydrazyne scaffold: Synthesis and molecular modeling of selective human monoamine oxidase inhibitors. Bioorganic Med. Chem. 2010, 18, 5715–5723. [Google Scholar] [CrossRef] [PubMed]
- Refat, M.S.; El-Deen, I.M.; Anwer, Z.M.; El-Ghol, S. Bivalent transition metal complexes of coumarin-3-ylthiosemicarbazone derivatives: Spectroscopic, antibacterial activity and thermogravimetric studies. J. Mol. Struct. 2009, 920, 149–162. [Google Scholar] [CrossRef]
- Zoltewicz, J.A.; Deady, L.W. Quaternization of Heteroaromatic Compounds: Quantitative Aspects. Adv. Heterocyclic Chem. 1978, 22, 71–121. [Google Scholar] [CrossRef]
- Molecular Operating Environment (MOE); Chemical Computing Group Inc.: Montreal, QC, Canada, 2016.
- Mahmoud, A.F.; Aboumanei, M.; Abdelhalim, S.; Hassan, Y.A.; Ibrahim, I. Radioiodination and in vivo assessment of the potential of newly synthesized pyrrolizine-5-carboxamides derivative in tumor model. Appl. Radiat. Isot. 2020, 166, 109369. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.B.; Salem, M.A.; Fasih, T.W.; Brown, A.; Sakr, T.M. Radioiodinated doxorubicin as a new tumor imaging model: Preparation, biological evaluation, docking and molecular dynamics. J. Radioanal. Nucl. Chem. 2018, 317, 1243–1252. [Google Scholar] [CrossRef]
- Zhou, L.; Chen, L.; Yang, L.; Cai, L.; Liu, L.; Zhao, Y.; Feng, Y.; Liu, N.; Zhao, Y.; Xia, Y.; et al. Preliminary Studies of 177Lu-Diethylenetriamine Penta-Acetic Acid-Deoxyglucose in Hepatic Tumor-Bearing Mice. Cancer Biother. Radiopharm. 2020, 35, 33–40. [Google Scholar] [CrossRef]
- Shi, D.; Liu, W.; Zhao, S.; Zhang, C.; Liang, T.; Hou, G. TLR5 is a new reporter for triple-negative breast cancer indicated by radioimmunoimaging and fluorescent staining. J. Cell. Mol. Med. 2019, 23, 8305–8313. [Google Scholar] [CrossRef] [PubMed]
- Motaleb, M.A.; Selim, A.A.; El-Tawoosy, M.; El-Hashash, M.A.; Sanad, M.H. Synthesis, radiolabeling and biological distribution of a new dioxime derivative as a potential tumor imaging agent. J. Radioanal. Nucl. Chem. 2017, 314, 1517–1522. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Elaasser, M.M.; Morsi, M.K.; Galal, S.M.; El-Rahman, M.K.A.; Katry, M.A. Antioxidant, anti-inflammatory and cytotoxic activities of the unsaponifiable fraction of extra virgin olive oil. Grasas y Aceites 2020, 71, 386. [Google Scholar] [CrossRef]
- Monteiro, L.O.; Fernandes, R.S.; Castro, L.C.; Cardoso, V.N.; Oliveira, M.C.; Townsend, D.M.; Ferretti, A.; Rubello, D.; Leite, E.A.; De Barros, A.L. Technetium-99 m radiolabeled paclitaxel as an imaging probe for breast cancer in vivo. Biomed. Pharmacother. 2017, 89, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Motaleb, M.A.; El-Tawoosy, M.; Mohamed, S.B.; Borei, I.H.; Ghanem, H.M.; Massoud, A.A. 99m Tc-labeled teicoplanin and its biological evaluation in experimental animals for detection of bacterial infection. Radiochemistry 2014, 56, 544–549. [Google Scholar] [CrossRef]




| Scheme I | Scheme II | ||
|---|---|---|---|
| Compound | Predicted pIC50 | Compound | Predicted pIC50 |
| 2a | 6.734 | 9a | 8.475 |
| 2b | 8.525 | 9b | 6.871 |
| 3a | 6.541 | 9c | 7.053 |
| 3b | 8.687 | 9d | 7.809 |
| 4a | 6.168 | 9e | 6.554 |
| 4b | 12.524 | 9f | 6.736 |
| 5a | 8.889 | 9g | 7.980 |
| 5b | 12.493 | 9h | 6.947 |
| 6a | 7.840 | 9i | 8.365 |
| 6b | 7.381 | ||
| Docking by MOE 2016.08 | Computed Affinity | |
|---|---|---|
| Compound | ΔG (kcal/mol) | Affinity pKi |
| 2a | −10.97 | 30.27 |
| 2b | −15.34 | 40.05 |
| 3a | −11.04 | 29.57 |
| 3b | −15.28 | 39.78 |
| 4a | −10.75 | 29.68 |
| 4b | −10.64 | 30.77 |
| 5a | −15.07 | 39.94 |
| 5b | −10.08 | 30.98 |
| 6a | −11.52 | 32.72 |
| 6b | −11.34 | 32.82 |
| 9a | −12.10 | 34.71 |
| 9b | −11.63 | 34.36 |
| 9c | −11.95 | 34.48 |
| 9d | −11.68 | 33.90 |
| 9e | −11.86 | 34.39 |
| 9f | −12.03 | 34.52 |
| 9g | −11.70 | 34.12 |
| 9h | −11.75 | 34.33 |
| 9i | −12.24 | 35.11 |
| Flavopiridol | −19.91 | 45.50 |
| Compound | MCF-7 (IC50, µM) | A-549 (IC50, µM) | CHO-K1 (IC50, µM) |
|---|---|---|---|
| 2a | 0.161 | 0.451 | 0.604 |
| 2b | 0.0314 | 0.015 | 0.054 |
| 3a | 0.138 | 0.560 | 0.735 |
| 3b | 0.116 | 0.056 | 0.127 |
| 4a | 0.360 | 0.537 | 0.757 |
| 4b | 0.861 | 0.784 | 0.968 |
| 5a | 0.102 | 0.054 | 0.075 |
| 5b | 0.305 | 0.305 | 0.414 |
| 6a | 0.055 | 0.095 | 0.131 |
| 6b | 0.055 | 0.077 | 0.101 |
| Flavopiridol | 0.00445 | 0.00114 | 0.00241 |
| Compound | MCF-7 (IC50, µM) | A549 (IC50, µM) | CHO-K1 (IC50, µM) |
|---|---|---|---|
| 9a | 0.060 | 0.034 | 0.091 |
| 9b | 0.295 | 0.386 | 0.522 |
| 9c | 0.479 | 0.244 | 0.649 |
| 9d | 0.780 | 0.513 | 0.901 |
| 9e | 0.432 | 0.242 | 0.507 |
| 9f | 0.276 | 0.200 | 0.495 |
| 9g | 0.488 | 0.441 | 0.744 |
| 9h | 0.534 | 0.34 | 0.574 |
| 9i | 0.124 | 0.075 | 0.189 |
| Flavopiridol | 0.00445 | 0.00114 | 0.00241 |
| Compound | IC50 (µM) |
|---|---|
| 2b | 0.036 |
| 3b | 0.127 |
| 5a | 0.142 |
| 9a | 0.131 |
| 9i | 0.193 |
| Flavopiridol | 0.001 |
| Models | 2b | 3b | 5a | 9a | 9i | |
|---|---|---|---|---|---|---|
| Absorption | Blood-Brain Barrier | BBB+ | BBB+ | BBB+ | BBB+ | BBB- |
| Human Intestinal Absorption | HIA+ | HIA+ | HIA+ | HIA+ | HIA+ | |
| Renal Organic Cation Transporter | Non-inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | |
| Metabolism | CYP450 3A4 Substrate | Non-substrate | Substrate | Substrate | Non-substrate | Substrate |
| CYP450 1A2 Inhibitor | Inhibitor | Inhibitor | Inhibitor | Inhibitor | Inhibitor | |
| CYP450 2D6 inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | |
| CYP450 3A4 Inhibitor | Inhibitor | Non-inhibitor | Non-inhibitor | Inhibitor | Inhibitor | |
| Toxicity | Human Ether-a-go-go-Related Gene Inhibition I | Weak inhibitor | Weak inhibitor | Weak inhibitor | Weak inhibitor | Weak inhibitor |
| Human Ether –a-go-go Related Gene Inhibition II | Non-inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | Non-inhibitor | |
| AMES Toxicity | Non AMES toxic | Non AMES toxic | Non AMES toxic | Non AMES toxic | AMES toxic | |
| Carcinogens | Non-carcinogens | Non-carcinogens | Non-carcinogens | Non-carcinogens | Non-carcinogens | |
| Honey Bee Toxicity | Low HBT | Low HBT | Low HBT | Low HBT | Low HBT | |
| Acute Oral Toxicity | III | III | III | III | III | |
| Carcinogenicity (three class) | Non-required | Non-required | Non-required | Non-required | Danger | |
| Rat Acute Toxicity (LD50, mol/kg) | 2.6533 | 2.4214 | 2.3609 | 2.5460 | 2.4924 | |
| Aqueous solubility (Log s) | −4.2840 | −4.0964 | −4.2184 | −4.2955 | −3.8523 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarhan, M.O.; Abd El-Karim, S.S.; Anwar, M.M.; Gouda, R.H.; Zaghary, W.A.; Khedr, M.A. Discovery of New Coumarin-Based Lead with Potential Anticancer, CDK4 Inhibition and Selective Radiotheranostic Effect: Synthesis, 2D & 3D QSAR, Molecular Dynamics, In Vitro Cytotoxicity, Radioiodination, and Biodistribution Studies. Molecules 2021, 26, 2273. https://doi.org/10.3390/molecules26082273
Sarhan MO, Abd El-Karim SS, Anwar MM, Gouda RH, Zaghary WA, Khedr MA. Discovery of New Coumarin-Based Lead with Potential Anticancer, CDK4 Inhibition and Selective Radiotheranostic Effect: Synthesis, 2D & 3D QSAR, Molecular Dynamics, In Vitro Cytotoxicity, Radioiodination, and Biodistribution Studies. Molecules. 2021; 26(8):2273. https://doi.org/10.3390/molecules26082273
Chicago/Turabian StyleSarhan, Mona O., Somaia S. Abd El-Karim, Manal M. Anwar, Raghda H. Gouda, Wafaa A. Zaghary, and Mohammed A. Khedr. 2021. "Discovery of New Coumarin-Based Lead with Potential Anticancer, CDK4 Inhibition and Selective Radiotheranostic Effect: Synthesis, 2D & 3D QSAR, Molecular Dynamics, In Vitro Cytotoxicity, Radioiodination, and Biodistribution Studies" Molecules 26, no. 8: 2273. https://doi.org/10.3390/molecules26082273
APA StyleSarhan, M. O., Abd El-Karim, S. S., Anwar, M. M., Gouda, R. H., Zaghary, W. A., & Khedr, M. A. (2021). Discovery of New Coumarin-Based Lead with Potential Anticancer, CDK4 Inhibition and Selective Radiotheranostic Effect: Synthesis, 2D & 3D QSAR, Molecular Dynamics, In Vitro Cytotoxicity, Radioiodination, and Biodistribution Studies. Molecules, 26(8), 2273. https://doi.org/10.3390/molecules26082273






