A Preliminary Study of FTIR Spectroscopy as a Potential Non-Invasive Screening Tool for Pediatric Precursor B Lymphoblastic Leukemia
Abstract
1. Introduction
2. Results
2.1. Exploratory Data Analysis
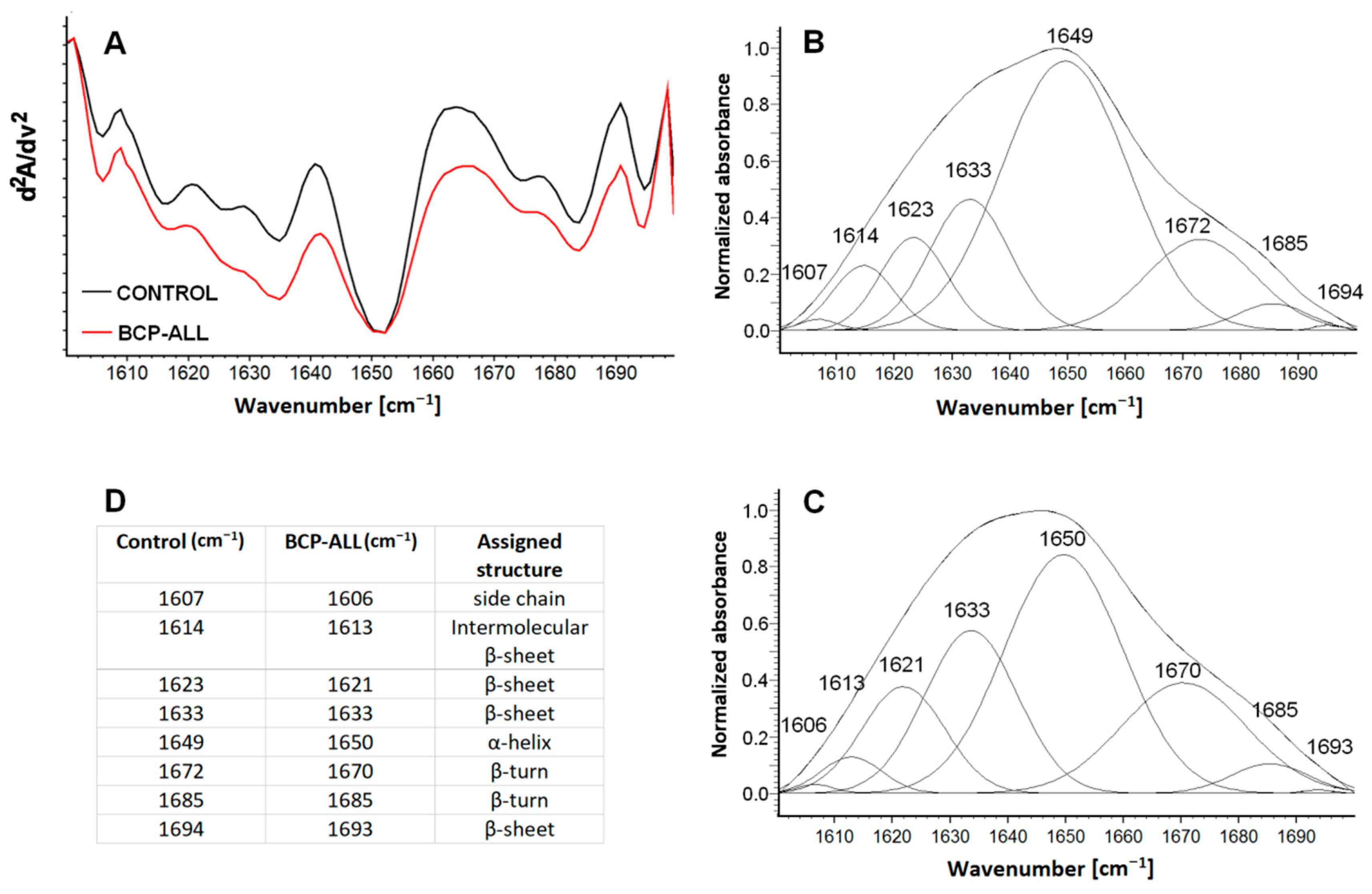
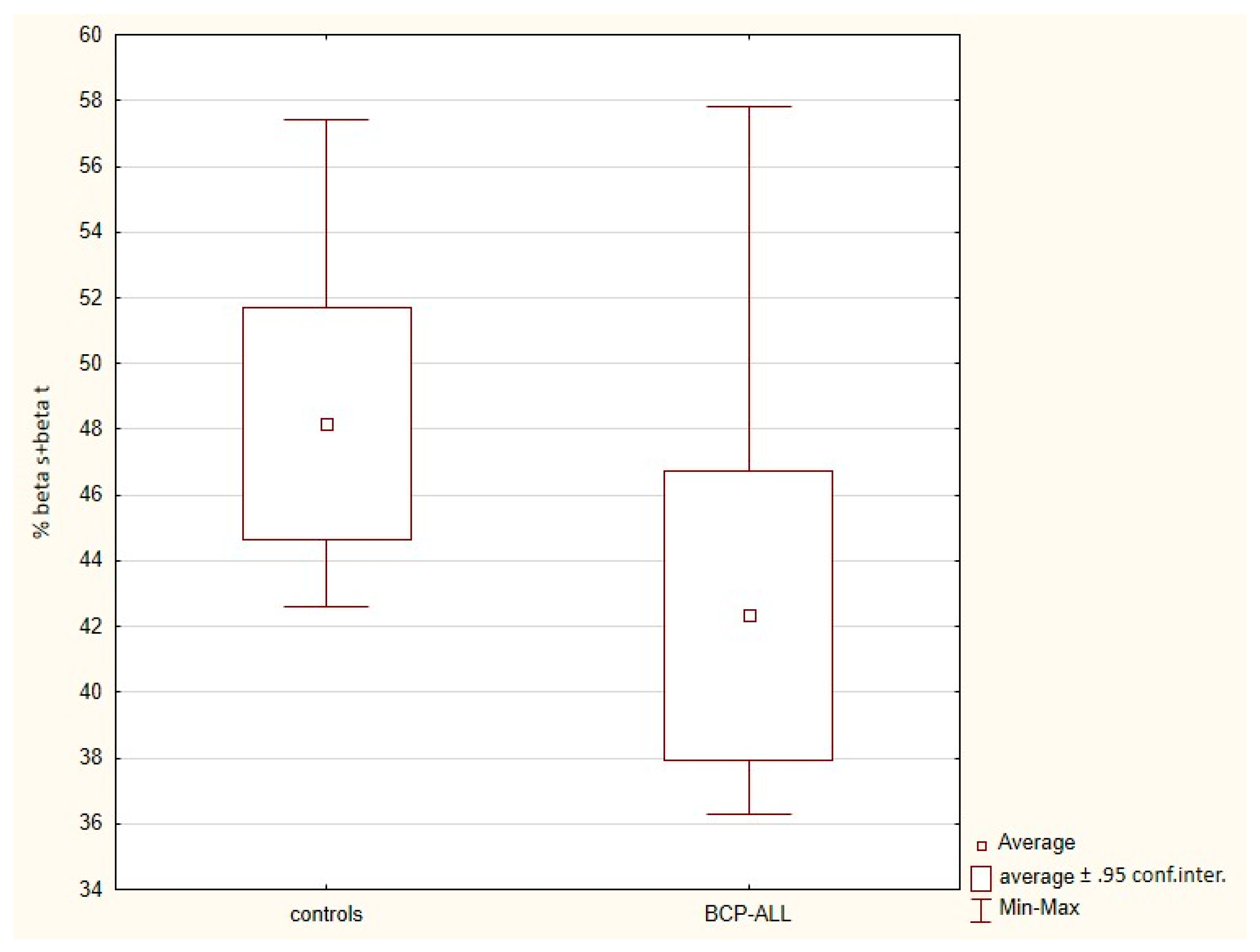
2.2. The Secondary Structure of Proteins
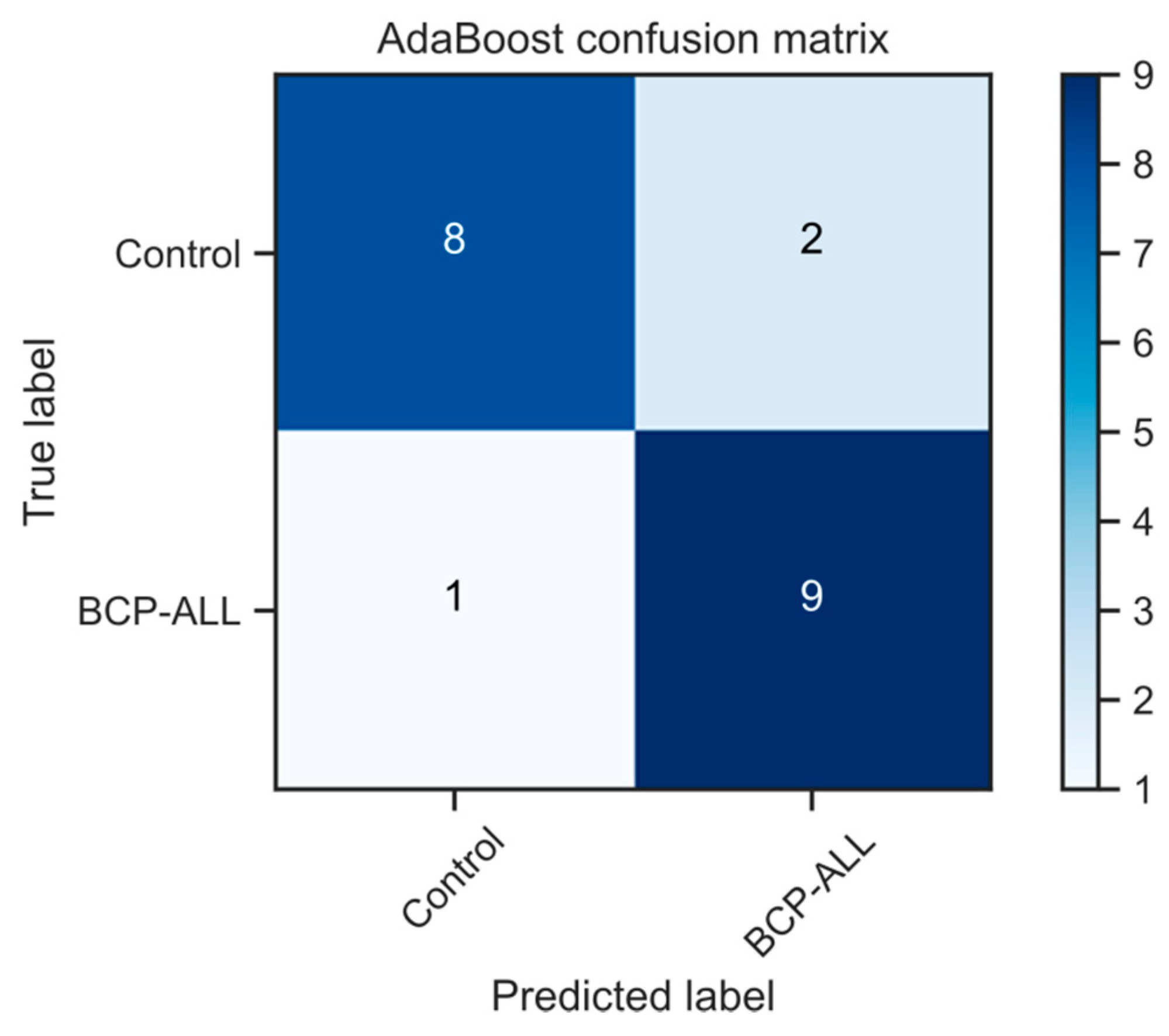
2.3. Methods for Dimensionality Reduction
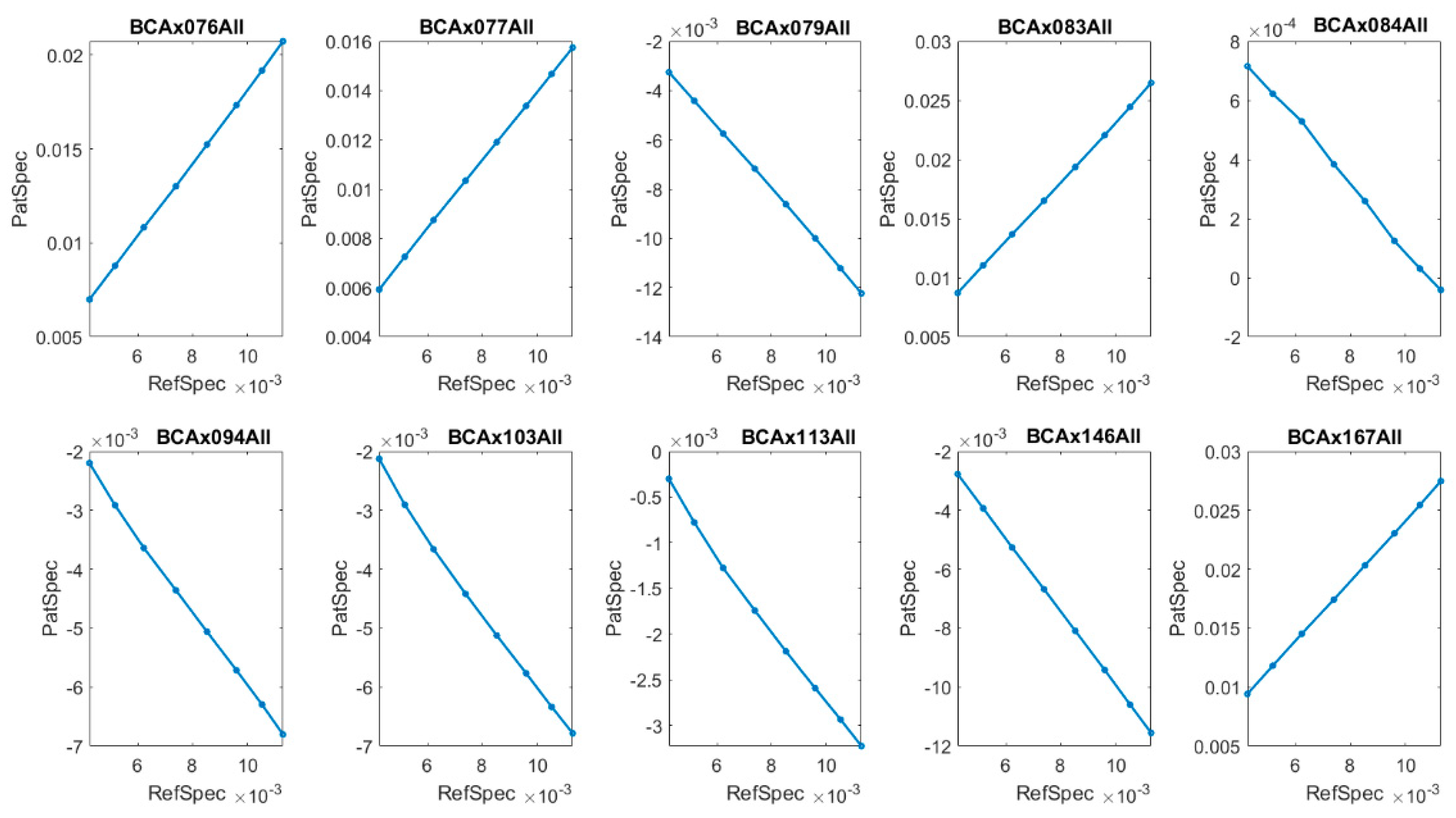
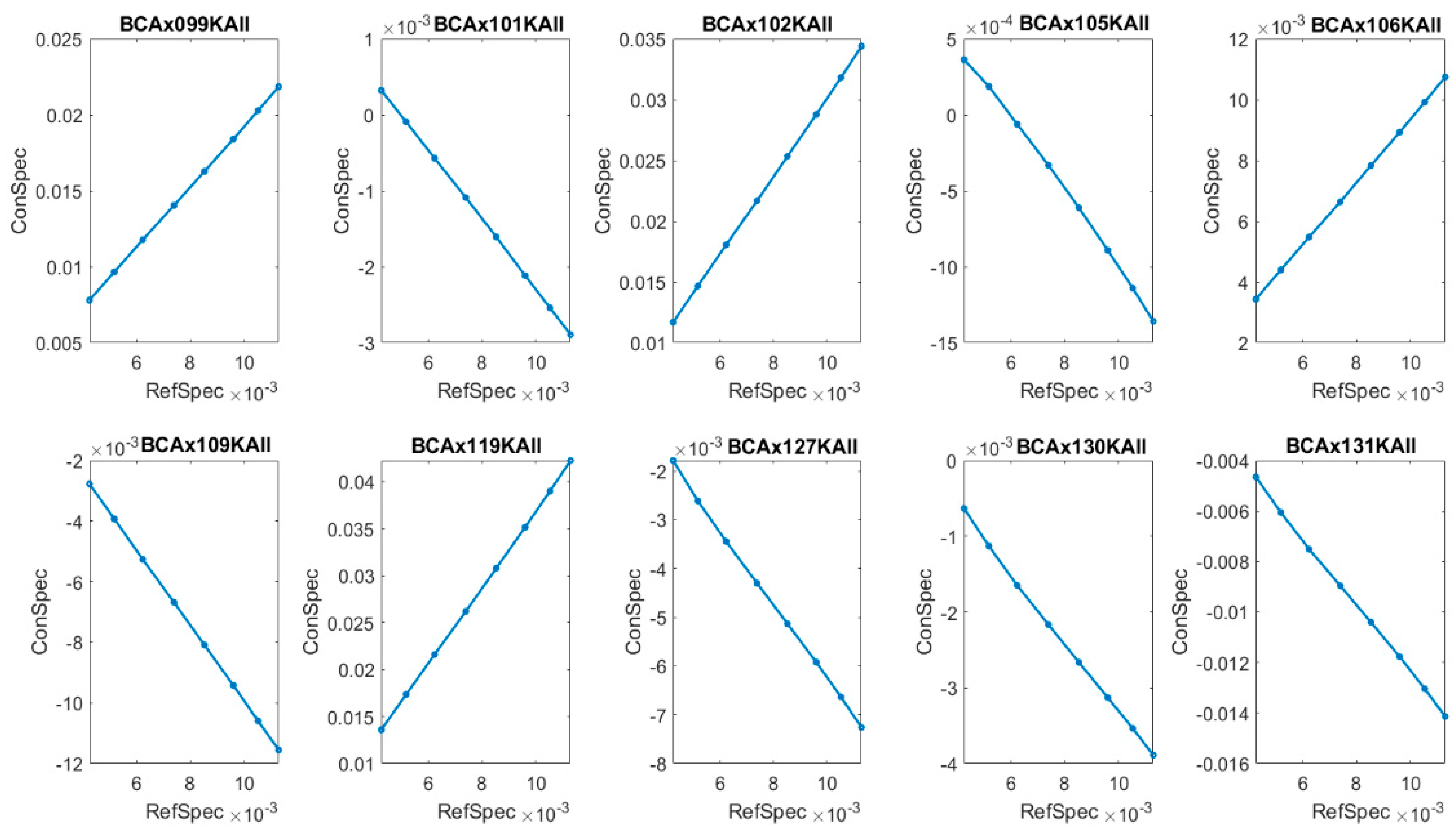
2.4. The Types of Absorbance Dynamics FTIR Spectra—Lissajous Curves Construction
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Sample Preparation
4.3. FTIR Spectroscopy
4.4. The Secondary Structure of Proteins
4.5. Data Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- PDQ Pediatric Treatment Editorial Board. Childhood Acute Lymphoblastic Leukemia Treatment (PDQ®): Health Professional Version. In PDQ Cancer Information Summaries [Internet]; National Cancer Institute: Bethesda, MD, USA, 2002. Available online: https://www.ncbi.nlm.nih.gov/books/NBK65763/ (accessed on 4 May 2020).
- Howlader, N.; Noone, A.M.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. SEER Cancer Statistics Review (CSR) 1975–2017; Cronin, K.A., Ed.; National Cancer Institute: Bethesda, MD, USA, 2020. Available online: https://seer.cancer.gov/csr/1975_2017/ (accessed on 15 April 2020).
- Kaplan, J.A. Leukemia in Children. Pediatr. Rev. 2019, 40, 319–331. [Google Scholar] [CrossRef]
- Su, K.Y.; Lee, W.L. Fourier Transform Infrared Spectroscopy as a Cancer Screening and Diagnostic Tool: A Review and Prospects. Cancers 2020, 12, 115. [Google Scholar] [CrossRef]
- Chaber, R.; Łach, K.; Szmuc, K.; Michalak, E.; Raciborska, A.; Mazur, D.; Machaczka, M.; Cebulski, J. Application of infrared spectroscopy in the identification of Ewing sarcoma: A preliminary report. Infrared Phys. Technol. 2017, 83, 200–205. [Google Scholar] [CrossRef]
- Chaber, R.; Arthur, C.J.; Depciuch, J.; Łach, K.; Raciborska, A.; Michalak, E.; Cebulski, J. Distinguishing Ewing sarcoma and osteomyelitis using FTIR spectroscopy. Sci. Rep. 2018, 8, 15081. [Google Scholar] [CrossRef]
- Chaber, R.; Łach, K.; Arthur, C.J.; Raciborska, A.; Michalak, E.; Ciebiera, K.; Bilska, K.; Drabko, K.; Cebulski, J. Prediction of Ewing Sarcoma treatment outcome using attenuated tissue reflection FTIR tissue spectroscopy. Sci. Rep. 2018, 8, 12299. [Google Scholar] [CrossRef] [PubMed]
- Chaber, R.; Arthur, C.J.; Łach, K.; Raciborska, A.; Michalak, E.; Bilska, K.; Drabko, K.; Depciuch, J.; Kaznowska, E.; Cebulski, J. Predicting Ewing Sarcoma Treatment Outcome Using Infrared Spectroscopy and Machine Learning. Molecules 2019, 24, 1075. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Yu, S. Fourier transform infrared spectroscopic analysis of protein secondary structures. Acta Biochim. Biophys. Sin. 2007, 39, 549–559. [Google Scholar] [CrossRef]
- Dovbeshko, G.I.; Chegel, V.I.; Gridina, N.Y.; Repnytska, O.P.; Shirshov, Y.M.; Tryndiak, V.P.; Todor, I.M.; Solyanik, G.I. Surface enhanced IR absorption of nucleic acids from tumor cells: FTIR reflectance study. Biopolymer 2002, 67, 470–486. [Google Scholar] [CrossRef] [PubMed]
- Movasaghi, Z.; Rehman, S.; ur Rehman, I. Fourier Transform Infrared (FTIR) Spectroscopy of Biological Tissues. Appl. Spectrosc. Rev. 2008, 43, 134–179. [Google Scholar] [CrossRef]
- Bellisola, G.; Sorio, C. Infrared spectroscopy and microscopy in cancer research and diagnosis. Am. J. Cancer Res. 2012, 2, 1–21. [Google Scholar] [PubMed]
- Wang, X.; Shen, X.; Sheng, D.; Chen, X.; Liu, X. FTIR spectroscopic comparison of serum from lung cancer patients and healthy persons. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2014, 122, 193–197. [Google Scholar] [CrossRef]
- Igci, N.; Sharafi, P.; Demiralp, D.O.; Yuce, A.; Emre, S.D. Application of Fourier transform infrared spectroscopy to biomolecular profiling of cultured fibroblast cells from Gaucher disease patients: A preliminary investigation. Adv. Clin. Exp. Med. 2017, 26, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Oleszko, A.; Hartwich, J.; Wójtowicz, A.; Gąsior-Głogowska, M.; Huras, H.; Komorowska, M. Comparison of FTIR-ATR and Raman spectroscopy in determination of VLDL triglycerides in blood serum with PLS regression. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2017, 183, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Borges, R.C.F.; Navarro, R.S.; Giana, H.E.; Tavares, F.G.; Fernandes, A.B.; Junior, L.S. Detecting alterations of glucose and lipid components in human serum by near-infrared Raman spectroscopy. Res. Biomed. Eng. 2015, 31. [Google Scholar] [CrossRef]
- Rohman, A.; Windarsih, A.; Lukitaningsih, E.; Rafi, M.; Betania, K.; Fadzillah, N. The use of FTIR and Raman spectroscopy in combination with chemometrics for analysis of biomolecules in biomedical fluids: A review. Biomed. Spectrosc. Imaging 2020, 8, 1–17. [Google Scholar] [CrossRef]
- Li, L.; Bi, X.; Sun, H.; Liu, S.; Yu, M.; Zhang, Y.; Weng, S.; Yang, L.; Bao, Y.; Wu, J.; et al. Characterization of ovarian cancer cells and tissues by Fourier transform infrared spectroscopy. J. Ovarian Res. 2018, 11, 64. [Google Scholar] [CrossRef]
- Theophanides, T. FT-IR Spectroscopy in Medicine. In Infrared Spectroscopy–Life and Biomedical Sciences; IntechOpen: Rijeka, Croatia, 2012; Available online: https://www.intechopen.com/books/infrared-spectroscopy-life-and-biomedical-sciences/ft-ir-spectroscopy-in-medicine (accessed on 4 November 2020).
- Sheng, D.; Liu, X.; Li, W.; Wang, Y.; Chen, X.; Wang, X. Distinction of leukemia patients’ and healthy persons’ serum using FTIR spectroscopy. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2013, 101, 228–232. [Google Scholar] [CrossRef]
- Barth, A. The infrared absorption of amino acid side chains. Prog. Biophys. Mol. Biol. 2000, 74, 141–173. [Google Scholar] [CrossRef]
- Malek, K. Spektroskopia Oscylacyjna; PWN: Warszawa, Poland, 2016; pp. 121–144. [Google Scholar]
- Usoltsev, D.; Sitnikova, V.; Kajava, A.; Uspenskaya, M. Systematic FTIR Spectroscopy Study of the Secondary Structure Changes in Human Serum Albumin under Various Denaturation Conditions. Biomolecules 2019, 9, 359. [Google Scholar] [CrossRef]
- Wojnarowska-Nowak, R.; Polit, J.; Sheregii, E.M. Interaction of gold nanoparticles with cholesterol oxidase enzyme in bionanocomplex—Determination of the protein structure by Fourier transform infrared spectroscopy. J. Nanopart. Res. 2020, 22, 107. [Google Scholar] [CrossRef]
- Abrosimova, K.V.; Shulenina, O.V.; Paston, S.V. FTIR study of secondary structure of bovine serum albumin and ovalbumin. J. Phys. Conf. Ser. 2016, 769, 01. [Google Scholar] [CrossRef]
- Mobili, P.; Londero, A.; Maria, T.M.R.; Eusebio, M.E.S.; De Antoni, G.L.; Fausto, R.; Gomez-Zavaglia, A. Characterization of S-layer proteins of Lactobacillus by FTIR spectroscopy and differential scanning calorimetry. Vib. Spectrosc. 2009, 50, 68–77. [Google Scholar] [CrossRef]
- Dores, G.M.; Devesa, S.S.; Curtis, R.E.; Linet, M.S.; Morton, L.M. Acute leukemia incidence and patient survival among children and adults in the United States, 2001–2007. Blood 2012, 119, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Erukhimovitch, V.; Talyshinsky, M.; Souprun, Y.; Huleihel, M. FTIR spectroscopy examination of leukemia patients plasma. Vib. Spectrosc. 2006, 40, 40–46. [Google Scholar] [CrossRef]
- Ramesh, J.; Kapelushnik, J.; Mordehai, J.; Moser, A.; Huleihel, M.; Erukhimovitch, V.; Levi, C.; Mordechai, S. Novel methodology for the follow-up of acute lymphoblastic leukemia using FTIR microspectroscopy. J. Biochem. Biophys. Methods 2002, 51, 251–261. [Google Scholar] [CrossRef]
- Abdel-Raouf, G.; Al Jaouni, S.K. Novel Methodology of Detecting Minimal Residual Disease in Acute Lymphoblastic Leukemia by Using FTIR Spectroscopy. J. Appl. Hematol. 2010, 1, 102–107. [Google Scholar]
- Mordechai, S.; Mordechai, J.; Ramesh, J.; Levi, C.; Huleihel, M.; Erukhimovitch, V.; Moser, A.; Kapelushnik, J. Application of FTIR microspectroscopy for the follow-up of childhood leukaemia chemotherapy. In Proceedings of the SPIE Subsurface and Surface Sensing Technologies and Applications III, San Diego, CA, USA, 30 July–1 August 2001; Volume 4491, pp. 243–250. [Google Scholar]
- Raouf, G.A.; Elkhateeb, W.F.; Toumah, H.; Quari, M.; Jaouni, S.; Elkebba, K.; Kumosani, T.A. Infrared spectroscopy of human bone marrow: Evidence of structural changes during acute leukemia. Int. J. Nano Biomater. 2009, 2, 289–298. [Google Scholar] [CrossRef]
- Musharraf, S.G.; Siddiqui, A.J.; Shamsi, T.; Choudhary, M.I.; Rahman, A.U. Serum metabonomics of acute leukemia using nuclear magnetic resonance spectroscopy. Sci. Rep. 2016, 6, 30693. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, L.; Chen, W.L.; Wang, J.H.; Li, N.; Li, J.M.; Mi, J.Q.; Zhang, W.N.; Li, Y.; Wu, S.F.; et al. Rapid diagnosis and prognosis of de novo acute myeloid leukemia by serum metabonomic analysis. J. Proteome Res. 2013, 12, 4393–4401. [Google Scholar] [CrossRef]
- Machana, S.; Weerapreeyakul, N.; Barusrux, S.; Thumanu, K.; Tanthanuch, W. FTIR microspectroscopy discriminates anticancer action on human leukemic cells by extracts of Pinus kesiya; Cratoxylum formosum ssp. pruniflorum and melphala. Talanta 2012, 93, 371–382. [Google Scholar] [CrossRef] [PubMed]
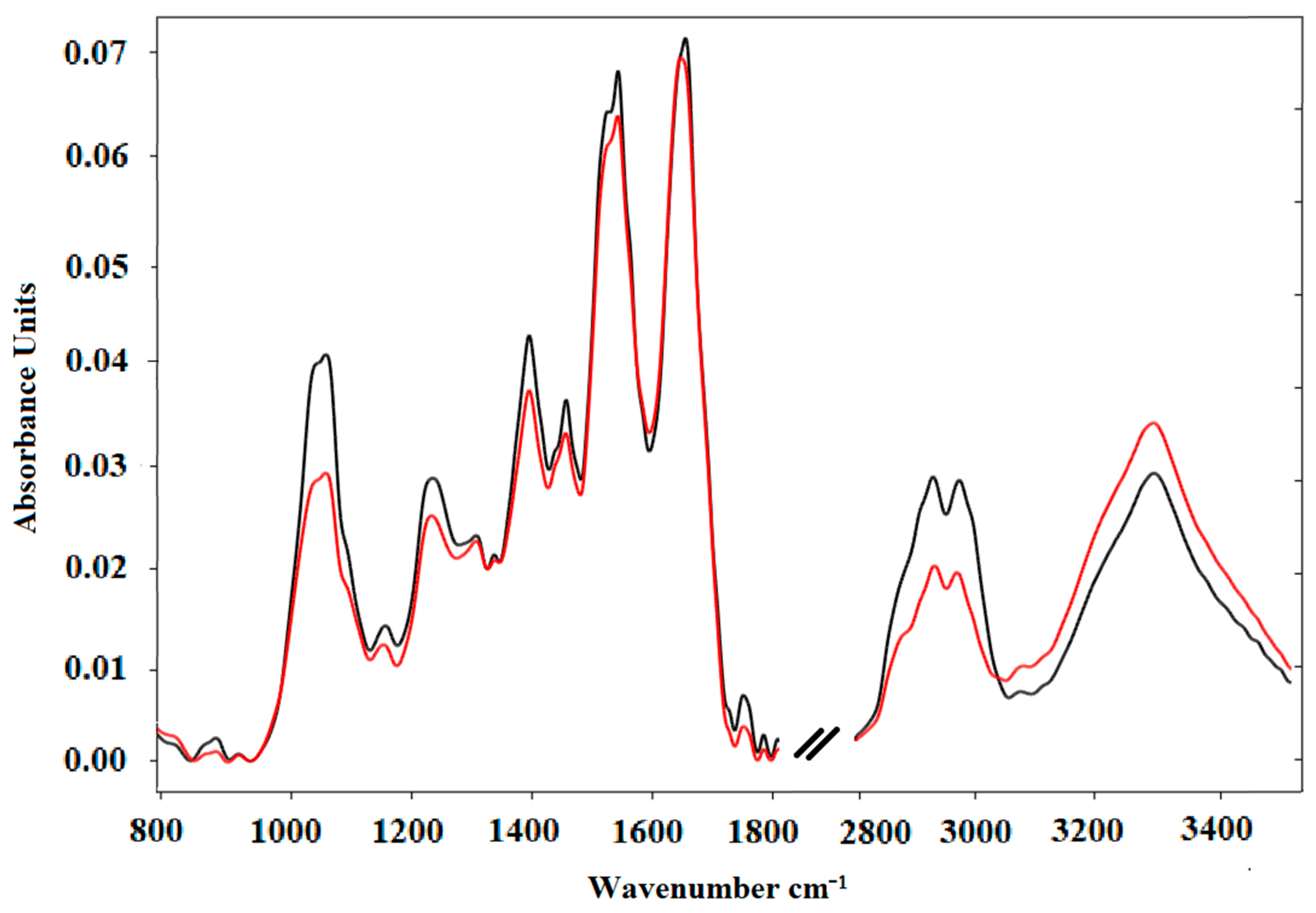
| FTIR Spectroscopy Peaks | ||||
|---|---|---|---|---|
| Control Sample | ALL Sample | ASSIGNMENT | ||
| Peaks [cm−1] | Average [A.U.] | Peaks [cm−1] | Average [A.U.] | |
| 894 | 0.002 | 893 | 0.001 | C-C, C-O deoxyribose, fatty acid, saccharide [10] |
| 931 | 0.001 | 932 | 0.001 | Left-handed helix DNA (Z form) [11] |
| 1071 | 0.039 | 1070 | 0.029 | vs(PO2−) DNA, RNA phospholipid, phosphorylated protein [12] |
| 1166 | 0.013 | 1163 | 0.012 | C-O group from groups of serine, threonine, and tyrosine of protein [10] |
| 1241 | 0.027 | 1239 | 0.025 | PO2− asymmetric and symmetric stretching (nucleic acids, phosphorylated proteins, and phospholipids) [13,14] |
| 1311 | 0.022 | 1311 | 0.022 | Amide III: proteins [15] |
| 1340 | 0.02 | 1340 | 0.02 | CH3, CH2 wagging: lipids/proteins [16] |
| 1396 | 0.041 | 1396 | 0.037 | νs(CH3): proteins, COO- symmetric stretching: fatty acids [15,16] |
| 1455 | 0.034 | 1454 | 0.033 | CH3, CH2 bending modes: lipids/proteins [16] |
| 1538 | 0.066 | 1537 | 0.064 | Amide II due to N-H bending of proteins [15,17] |
| 1645 | 0.07 | 1641 | 0.071 | Amide I due to C=O stretching of α-helix proteins [17] |
| 2924 | 0.028 | 2926 | 0.02 | asymmetric stretching symmetric CH2: lipids [18] |
| 2965 | 0.027 | 2962 | 0.019 | asymmetric stretching vibrations of CH3 [17] |
| 3278 | 0.028 | 3277 | 0.034 | ʋ-NH stretching of the peptide bond (-NHCO) of proteins and ʋ-OH stretching of functional groups of water [19] |
| Sample | Secondary Structure | ||
|---|---|---|---|
| α-Helix (%) | β-Sheet + β-Turn (%) | Other Structure (%) | |
| Control | 44.55 | 48.19 | 7.26 |
| BCP-ALL | 50.42 | 42.34 | 7.24 |
| Patients | BCAx076 ALL | BCAx077 ALL | BCAx079 ALL | BCAx083 ALL | BCAx084 ALL | BCAx094 ALL | BCAx103 ALL | BCAx113 ALL | BCAx146 ALL | BCAx167 ALL |
|---|---|---|---|---|---|---|---|---|---|---|
| Phase Shift | 0 | 0 | π | 0 | π | π | π | π | π | 0 |
| WBC [103/µL] | 205.8 | 21.08 | 1.7 | 9.08 | 3.33 | 2.22 | 0.13 | 1.62 | 4.15 | 22.43 |
| Blast Cells in Peripheral Blood [103/µL] | 183.16 | 11.80 | 0.24 | 2.81 | 0.66 | 0 | 0 | 0.19 | 0.33 | 10.99 |
| Controls | BCAx099KAll | BCAx101KAll | BCAx102KAll | BCAx105KAll | BCAx106KAll | BCAx109KAll | BCAx119KAll | BCAx127KAll | BCAx130KAll | BCAx131KAll |
|---|---|---|---|---|---|---|---|---|---|---|
| Phase Shift | 0 | π | 0 | π | 0 | π | 0 | π | π | π |
| WBC [103/µL] | 3.98 | 7.38 | 4.86 | 5.37 | 10.63 | 5.61 | 10.50 | 7.99 | 3.6 | 5.24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaber, R.; Kowal, A.; Jakubczyk, P.; Arthur, C.; Łach, K.; Wojnarowska-Nowak, R.; Kusz, K.; Zawlik, I.; Paszek, S.; Cebulski, J. A Preliminary Study of FTIR Spectroscopy as a Potential Non-Invasive Screening Tool for Pediatric Precursor B Lymphoblastic Leukemia. Molecules 2021, 26, 1174. https://doi.org/10.3390/molecules26041174
Chaber R, Kowal A, Jakubczyk P, Arthur C, Łach K, Wojnarowska-Nowak R, Kusz K, Zawlik I, Paszek S, Cebulski J. A Preliminary Study of FTIR Spectroscopy as a Potential Non-Invasive Screening Tool for Pediatric Precursor B Lymphoblastic Leukemia. Molecules. 2021; 26(4):1174. https://doi.org/10.3390/molecules26041174
Chicago/Turabian StyleChaber, Radosław, Aneta Kowal, Paweł Jakubczyk, Christopher Arthur, Kornelia Łach, Renata Wojnarowska-Nowak, Krzysztof Kusz, Izabela Zawlik, Sylwia Paszek, and Józef Cebulski. 2021. "A Preliminary Study of FTIR Spectroscopy as a Potential Non-Invasive Screening Tool for Pediatric Precursor B Lymphoblastic Leukemia" Molecules 26, no. 4: 1174. https://doi.org/10.3390/molecules26041174
APA StyleChaber, R., Kowal, A., Jakubczyk, P., Arthur, C., Łach, K., Wojnarowska-Nowak, R., Kusz, K., Zawlik, I., Paszek, S., & Cebulski, J. (2021). A Preliminary Study of FTIR Spectroscopy as a Potential Non-Invasive Screening Tool for Pediatric Precursor B Lymphoblastic Leukemia. Molecules, 26(4), 1174. https://doi.org/10.3390/molecules26041174






